Abstract
Background:
Hurricane Harvey made landfall in August 2017 and resulted in catastrophic flooding in Houston, Texas. Prior studies of hurricanes and preterm birth have found conflicting results. We tested the hypotheses that exposure to Hurricane Harvey was associated with a higher risk of spontaneous pre- and early-term birth and assessed vulnerable subpopulations.
Methods:
We conducted a retrospective study of singleton births using administrative birth records in the nine-county greater Houston area from 2015 to 2019. We estimated the likelihood of pre- and early-term births using logistic regression, comparing births occurring during or within 1, 2, or 4 weeks of Hurricane Harvey to unexposed reference periods encompassing the same dates 2 years prior and after. Stratified models assessed effect modification by degree of flooding, birth parent age, high- vs. low-risk pregnancy, race/ethnicity, and prenatal care.
Results:
Among 15,564 births, we found no association between exposure to Hurricane Harvey and spontaneous preterm birth within 1 week adjusted (odds ratio [OR], 1.06; 95% confidence interval [CI] = 0.91, 1.25) but a 14% higher odds of spontaneous early-term birth (OR, 1.14; 95% CI = 1.04, 1.25). The odds of early-term birth were even higher in neighborhoods with severe flooding (OR, 1.21; 95% CI = 1.05, 1.38), segregated neighborhoods (OR, 1.23; 95% CI = 1.03, 1.47), and among foreign-born Hispanics (OR, 1.21; 95% CI = 1.04, 1.53) and pregnant people receiving no prenatal care (OR, 1.37; 95% CI = 1.03, 1.82). Effect estimates were attenuated or null when considering 2-week or 4-week lags to define exposure.
Conclusions:
Hurricane Harvey was associated with higher odds of spontaneous early-term birth up to 1 week later, especially among socially marginalized populations.
What this study adds
Previous studies reached conflicting conclusions regarding the impact of hurricanes on preterm birth. No prior studies consider early-term birth, despite its high prevalence and potential for adverse health consequences. Using administrative birth records from the greater Houston, Texas area, we found that exposure to Hurricane Harvey in 2017 was associated with 14% higher odds of spontaneous early-term birth up to 1 week later, with greater effect sizes in more flooded and segregated neighborhoods, among foreign-born Hispanics, and among pregnant people who did not receive prenatal care. The results suggest hurricanes can shorten pregnancy and disproportionately impact immigrants and residents living in areas of concentrated racialized economic disadvantage.
Introduction
Climate change is projected to increase hurricane frequency and intensity in the continental United States1–3 and result in more extreme hurricane-season rainfall.4,5 In the United States, 60.2 million people live in hurricane-prone areas,6 and damages due to hurricanes have risen considerably over the last century, mainly due to increases in population and wealth in hurricane-affected areas.7,8 Prior studies suggest exposure to a hurricane during pregnancy may be associated with an increased risk of adverse birth outcomes,9 including preterm birth,10,11 fetal distress,12 low birth weight,11,13 and small for gestational age birth.13 Leading explanations include stress14 and limited access to prenatal care.15 However, the evidence is not consistent, with some studies reporting a null or protective effect for preterm birth and low birth weight.16 Marginalized populations with fewer resources to prepare and cope with extreme storms are disproportionately affected by hurricanes and may be at a higher risk of adverse birth outcomes.17
The sensitivity of adverse birth outcomes to climatic conditions is worrying considering their high prevalence and public health impact. Preterm birth (<37 completed weeks) is a primary predictor of infant mortality and morbidity.18,19 Infants born early-term (37–38 completed weeks) are also more likely to be admitted to neonatal intensive care and have respiratory complications than full-term infants.18,19 Both preterm and early-term births can lead to longer-term health consequences, including respiratory, infectious, neurocognitive, and emotional problems into adulthood.18,19 With approximately 10% of US infants born preterm and 30% born early term, the disease burden resulting from early delivery is substantial. Anxiety, air pollution, and diabetes are among the shared risk factors that have been identified for preterm and early-term births.18
Here we utilize a hurricane that struck the Texas Gulf Coast as a natural experiment by which to test the hypotheses that exposure to hurricanes increases the risk of spontaneous pre- and early-term birth. Hurricane Harvey made landfall in Southeast Texas on 25 August 2017 and resulted in heavy rain and catastrophic flooding, particularly in the Greater Houston metropolitan statistical area (MSA), a highly urbanized and industrialized region.20 Over one million people were displaced, and at least 70 deaths were directly or indirectly attributed to the storm, with more than half of the fatalities occurring in the greater Houston area.20,21 Declines in overall health care utilization, including primary care practitioner visits, emergency department visits, and hospitalizations, were observed during and post-Hurricane Harvey, indicating barriers to care.22 However, emergency department visits for carbon monoxide poisoning, insect bite, dehydration, hypothermia, pregnancy complications, and hospitalizations for respiratory and infectious diseases and injuries increased.23,24 A prior study of one public and one private hospital in Houston found that births occurring within 40 weeks of Harvey’s landfall were more likely to have adverse maternal (e.g., cesarean section and hypertensive disorders of pregnancy) and neonatal (e.g., respiratory distress syndrome and newborn sepsis) outcomes.25 However, no previous studies have examined acute spontaneous early-term birth risk in relation to Hurricane Harvey and whether marginalized populations were disproportionately affected using a representative sample. We used administrative greater Houston area birth records from 2015 to 2019 to assess relationships with hurricane exposure at multiple lags.
Methods
Cohort selection
The study population included singleton births in the Greater Houston MSA, which encompasses nine counties in southeastern Texas with a population of about 7.2 million people (Figure 1). We obtained geo-coded administrative birth records for all singleton live births from the Texas Department of State Health Services for the years 2015–2019. We excluded births with <20 or >42 completed gestational weeks and improbable combinations of birthweight and gestational age. Improbable combinations were defined as outside of the mean ±2.575 × standard deviation (SD) of a 2014 US national reference for each completed gestational week.26 Eligible births were those that took place within 4 weeks of the hurricane period (August 25–September 26) during 2015, 2016, 2017, 2018, or 2019. The final analytical sample included 15,564, 25,230, and 44,695 births for the 1- 2- and 4-week lag exposure definitions, respectively (Supplementary Figure S1; http://links.lww.com/EE/A277). The study protocol was approved by the institutional review boards of the University of California, Los Angeles (#23-000791) and the Texas Department of State Health Service (#14-044).
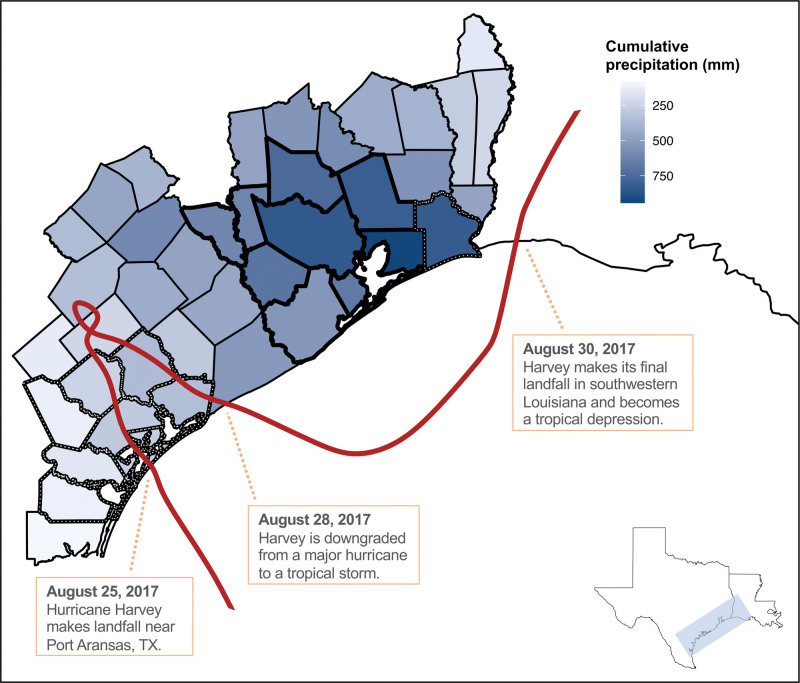
Figure 1.
Hurricane Harvey’s storm track and cumulative precipitation (mm) levels in counties designated for relief assistance by the US Federal Emergency Management Agency from August 25–29, 2017. Bolded boundaries indicate Houston MSA counties included in the main analysis (N = 9): Austin, Brazoria, Chamber, Fort Bend, Galveston, Harris, Liberty, Montgomery, Waller. Dotted boundaries indicate additional counties included in the sensitivity analysis (N = 9) that experienced >600 mm of precipitation during the study period or windspeed >64 knots: Aransas, Bee, Calhoun, Goliad, Jefferson, Nueces, Refugio, San Patricio, Victoria.
Hurricane exposure
We defined the Hurricane Harvey period as the 5 days of 25–29 August 2017, beginning on the day of the hurricane’s landfall between Port Aransas and Port O’Connor near Rockport, Texas, and ending on the day Harvey’s center moved offshore.27 26 and 27 August were two of the wettest days on record in Houston, with more than two feet of combined rainfall over the consecutive days.28 Tornadoes were a lesser hazard associated with the hurricane compared to heavy rainfall, however, a total of 52 tornadoes were documented, with many of them impacting the Houston area. Harris County was on a 60-hour tornado watch between 25 and 27 August.29
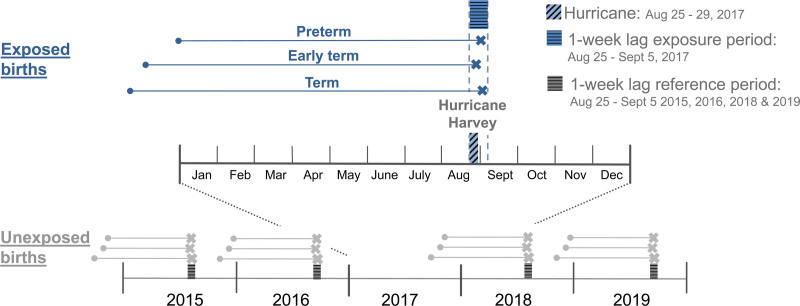
To evaluate the impact of acute exposure to Hurricane Harvey, we defined the exposed group as pregnancies resulting in births that occurred during the 5-day period or within 1 week after (primary exposure, 1-week lag, 25 August–5 September 2017, Figure 2). The unexposed group gave birth during the same dates in 2015, 2016, 2018, or 2019. The rationale for this approach is that if acute exposure to the hurricane and its immediate aftermath triggered the early onset of labor, we would observe higher rates of pre- and early-term births between the dates of 25 August and 5 September in 2017 relative to the 2 years before and after. We focused on acute exposure during the 1-week lag to reduce potential confounding resulting from the secular trend in preterm birth rates, which increased overall between 2015 and 2019 in our nine-county study area, and potential selection bias resulting from temporary or permanent migration out of the study area due to the storm. We secondarily considered the 5-day period plus 2 weeks (2-week lag, 25 August–12 September) or 4 weeks (4-week lag, 25 August–26 September) to define the exposed and unexposed groups.
Figure 2.
Illustration of the primary exposure definition comparing births during or within 1 week of Hurricane Harvey to births occurring during the same dates 2 years before or after the storm. Secondary analyses considered births within 2 weeks and 4 weeks of the hurricane.
We estimated the extent of flooding across census block groups using the Federal Emergency Management Administration’s Hurricane Harvey Inundation Footprint which has been utilized in a previous study.30 First, we used a high-resolution version of the National Hydrography Dataset for Texas31 to remove all permanent water features located within the 2010 Census block group boundaries of counties in the study area. We then overlaid this map layer representing tract land areas on the 3-meter by 3-meter resolution Hurricane Harvey Inundation Footprint raster grid. We counted the number of pixels with nonzero flood depth, the number of pixels with zero flood depth, and the total number of pixels without data within each block group to derive the percent of each block group’s land area that experienced flooding (median: 55%; range: 0–99%).
Outcomes
We used the obstetrician’s estimate of gestational age in weeks to define spontaneous preterm birth (<37 completed weeks) and early-term birth (37 and 38 completed weeks). We did not investigate spontaneous extremely (<28 completed weeks) or early (29–31 completed weeks) preterm birth separately due to a small number of events in the acute exposure period. We focused on spontaneous births since the etiology of provider-initiated births is likely to differ and particularly for preterm births, indicate an underlying severe medical condition that is unlikely to be related to hurricane exposure. Because we lacked information on labor, rupture of membranes, or cervical incompetence, we used noninduced labor to define spontaneous preterm birth and early-term birth.
Covariates
We adjusted for potential confounders derived from the birth records and selected a priori based on the literature, as well as known risk factors for our outcomes, which were included to improve the precision of our estimates: days from 1 January 2015 (to control for secular trends), maternal age (in 5 year increments from <20 to ≥40 years), race/ethnicity (Asian/Pacific Islander, Hispanic, non-Hispanic Black, non-Hispanic White, Multiple, or other), education (less than high school, high school, some college, or bachelor’s degree or above), marital status (married or other), nativity (US or foreign born), insurance (private/self-pay or other), smoking 3 months pre-/during pregnancy (yes or no), pre-pregnancy body mass index (BMI, underweight [≤18.5 kg/m2], normal [≥18.5–25 kg/m2], overweight [≥25–30 kg/m2], or obese [≥30 kg/m2]), high-risk pregnancy (any of the following: pregnancy-induced hypertension or preeclampsia, eclampsia, gestational diabetes, preexisting hypertension, preexisting diabetes, or previous preterm birth), parity (nulliparous or multiparous), prenatal care index (no care, inadequate, intermediate, adequate, or adequate plus), and infant sex (male or female). Race and ethnicity were conceived of as imperfect markers for experiences of discrimination and intergenerational marginalization resulting from interpersonal and structural racism.32–34 The Kotelchuck or Adequacy of Prenatal Care Utilization Index was used to characterize prenatal care. It combines the initiation time of prenatal care and the number of prenatal visits to derive a ratio of observed to expected visits.35 The number of expected visits was estimated based on the American College of Obstetricians and Gynecologists prenatal care standards for uncomplicated pregnancies adjusted for gestational age at delivery and the initiation time of care.
We utilized the 2010 census tract of residence to characterize neighborhood racialized economic segregation, which we previously found to confer greater risk to the effects of extreme heat on preterm birth.36 We calculated the Index of Concentration at the Extremes (ICE), which quantifies the degree to which marginalized and privileged populations are concentrated in particular neighborhoods, using 5 years (2007–2011) population estimates from the American Community Survey.37 We defined the marginalized group as people of color with an annual household income <$25,000 and the privileged group as non-Hispanic White people with an annual household income >$100,000, and categorized ICE, which ranges from −1 to 1, into quartiles.
Statistical analysis
We compared frequencies and percentages for categorical variables and means and standard deviations for continuous variables of interest between the exposed (1-week lag, 2-week lag, and 4-week lag) and their corresponding unexposed groups. We then applied logistic regression models to estimate the unadjusted and adjusted odds ratio (OR) and confidence intervals (CI) of spontaneous preterm birth and early-term birth in separate models comparing the exposed group vs. the corresponding unexposed group. Since the probability of birth increases exponentially with the length of gestation, this approach assumes minimal differences in the distribution of gestational ages at risk in the exposed and unexposed populations. We checked this assumption visually using boxplots (data not shown).
We then conducted a series of models to assess potentially vulnerable subgroups, focusing on the exposure period (i.e., 1-week lag) for which we observed the strongest associations. We ran stratified models for the following subgroups: neighborhood extent of flooding (high [≥55% flooded, median] and low [<55% flooded], each compared to the reference group of unexposed), maternal age (≤35 and >35 years), high-risk pregnancy (yes and no), race/ethnicity and nativity (Asian/Pacific Islander, non-Hispanic Black, non-Hispanic White, Foreign-born Hispanic, US-born Hispanic, and all others), prenatal care index (no care, inadequate, intermediate, adequate, and adequate plus), and ICE (quartiles). We considered foreign- and US-born Hispanics separately because foreign-born Hispanics have better birth outcomes in our population; stratifying by nativity among other racial/ethnic groups was not possible due to limitations of sample size.
Finally, to check the robustness of our main results, we performed a sensitivity analysis repeating the analyses of 1-week lag exposure using a larger area affected by Hurricane Harvey. This larger area (N = 18 counties) included nine additional counties designated for individual and public relief assistance by Federal Emergency Management Agency38 that experienced either (1) more than 600 mm of cumulative precipitation from August 25 to August 29 or (2) maximum sustained wind speed greater than 64 knots at the county centroid during any point of the hurricane. We obtained precipitation data from the PRISM Climate group.39 We obtained information on county-level windspeed from the hurricaneexposure R package,40,41 and defined the cutoff of >64 knots based on Category 1 (“very dangerous winds that will produce some damage”) of the Saffir-Simpson Hurricane Wind Scale.42
County-level hurricane exposure assignment was conducted in R. All statistical analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC). A two-sided P-value less than 0.05 was considered statistically significant.
Results
For the main analysis considering a 1-week lag, the final analytical sample included 15,564 births, with 18.4% of births in the exposed group and 81.6% births in the unexposed group. In general, the exposed and unexposed groups had similar baseline characteristics, including maternal age, race/ethnicity, and education for all exposure lags, except for prenatal care. A larger proportion of exposed births received no, inadequate, or intermediate levels of prenatal care, and a smaller proportion received more than adequate levels of prenatal care, possibly related to interruptions due to Hurricane Harvey (Table 1 and Supplementary Table 1; http://links.lww.com/EE/A277). Considering the 1-week lag, the crude rate of spontaneous preterm birth was similar in the exposed and unexposed groups (7.56% and 7.48%, respectively), while the crude rate of spontaneous early-term birth was slightly higher in the exposed group than in the unexposed group (26.20% and 24.23%, respectively) (Table 1).
Table 1.
Participant characteristics for 1-week lag definition of exposurea
| Exposed | Unexposed | |||
|---|---|---|---|---|
| N = 2,870 | N = 12,694 | |||
| Maternal age (years), mean (SD) | 28.69 | (5.94) | 28.80 | (5.96) |
| Missing | 1 | (0.03) | 0 | (0.00) |
| Race and ethnicity, N (%) | ||||
| Asian or Pacific Islander | 244 | (8.50) | 910 | (7.17) |
| Hispanic | 1,307 | (45.54) | 5,723 | (45.08) |
| Non-Hispanic Black | 484 | (16.86) | 2,167 | (17.07) |
| Non-Hispanic White | 749 | (26.10) | 3,538 | (27.87) |
| Multiple races | 38 | (1.32) | 120 | (0.95) |
| Other | 46 | (1.60) | 138 | (1.09) |
| Missing | 2 | (0.07) | 98 | (0.77) |
| Education, N (%) | ||||
| Less than high school | 588 | (20.49) | 2,438 | (19.21) |
| High school | 656 | (22.86) | 2,851 | (22.46) |
| Some college or associate degree | 724 | (25.23) | 3,472 | (27.35) |
| Bachelor’s degree or above | 894 | (31.15) | 3,914 | (30.83) |
| Missing | 8 | (0.28) | 19 | (0.15) |
| Private or self-pay, N (%) | ||||
| Yes | 1,337 | (46.70) | 5,815 | (45.89) |
| No | 1,526 | (53.17) | 6,856 | (54.01) |
| Missing | 7 | (0.24) | 23 | (0.18) |
| Foreign born, N (%) | ||||
| Yes | 1,091 | (38.04) | 4,637 | (36.55) |
| No | 1,777 | (61.92) | 8,049 | (63.41) |
| Missing | 2 | (0.07) | 8 | (0.06) |
| Married, N (%) | ||||
| Yes | 1,743 | (60.73) | 7,533 | (59.36) |
| No | 1,127 | (39.27) | 5,158 | (40.63) |
| Missing | 0 | (0.00) | 3 | (0.02) |
| Nulliparity, N (%) | ||||
| Yes | 1,071 | (37.34) | 4,854 | (38.25) |
| No | 1,797 | (62.61) | 7,835 | (61.72) |
| Missing | 2 | (0.07) | 5 | (0.04) |
| Pre-pregnancy BMI category, N (%) | ||||
| Underweight | 84 | (2.93) | 442 | (3.48) |
| Normal weight | 1,246 | (43.41) | 5,297 | (41.73) |
| Overweight | 799 | (27.84) | 3,581 | (28.21) |
| Obese | 718 | (25.02) | 3,245 | (25.56) |
| Missing | 23 | (0.80) | 129 | (1.02) |
| Prenatal care index, N (%) | ||||
| No care | 324 | (11.29) | 868 | (6.84) |
| Inadequate | 658 | (22.93) | 3,263 | (25.71) |
| Intermediate | 268 | (9.34) | 957 | (7.54) |
| Adequate | 950 | (33.10) | 4,205 | (33.13) |
| Adequate plus | 670 | (23.34) | 3,401 | (26.79) |
| Smoked 3 months pre-pregnancy or during pregnancy | 76 | (2.65) | 336 | (2.65) |
| Conception season | ||||
| Fall (September, October, November) | 1,564 | (54.49) | 6,677 | (52.60) |
| Winter (December, January, February) | 1,301 | (45.33) | 5,977 | (47.09) |
| Spring (March, April, May) | 5 | (0.17) | 40 | (0.32) |
| Summer (June, July, August) | 0 | (0.00) | 0 | (0.00) |
| High-risk pregnancyb, N (%) | 373 | (13.00) | 1,779 | (14.01) |
| Male infant, N (%) | 1,482 | (51.64) | 6,381 | (50.27) |
| Spontaneous preterm birth, N (%) | 217 | (7.56) | 949 | (7.48) |
| Spontaneous early-term birth, N (%) | 752 | (26.20) | 3,076 | (24.23) |
We defined the exposed group as births during Hurricane Harvey or within 1 week later (primary exposure, 1-week lag).
High-risk pregnancy included any of the following: pregnancy-induced hypertension or preeclampsia, eclampsia, gestational diabetes, preexisting hypertension, preexisting diabetes, or previous preterm birth.
BMI, body mass index; SD, standard deviations.
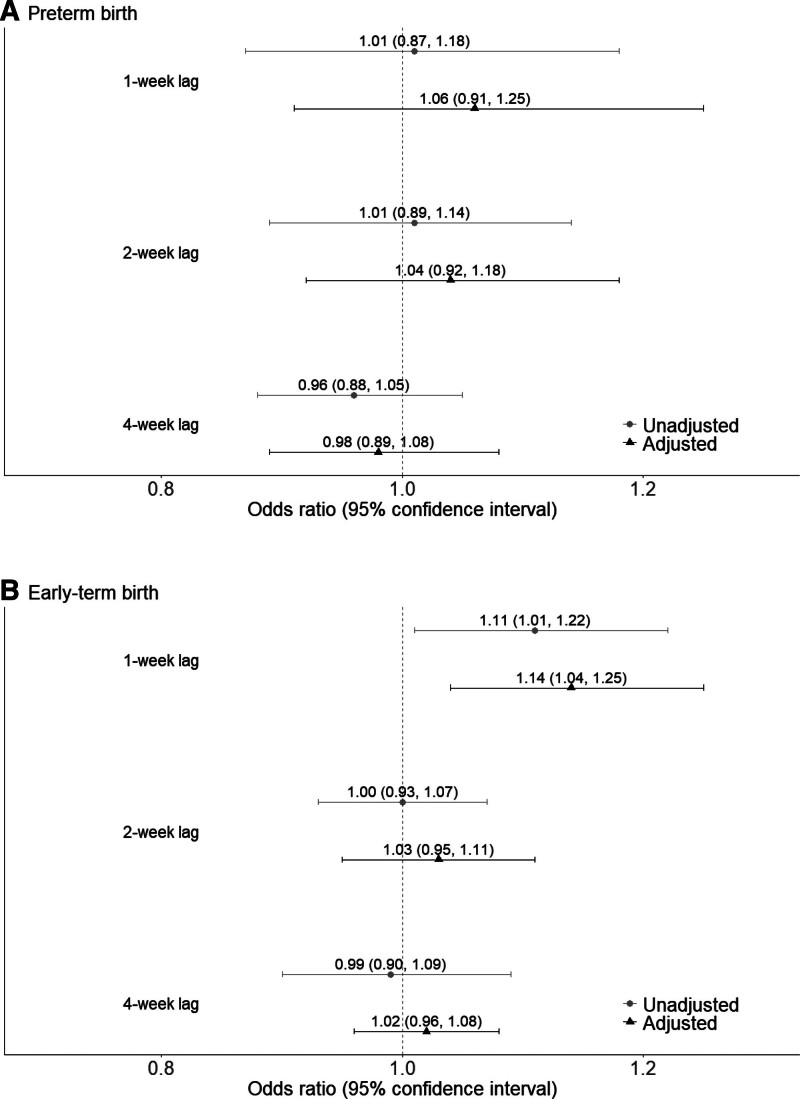
The results of the unadjusted and adjusted logistic models indicated no elevated odds of spontaneous preterm birth across any of the lags examined (Figure 3A and Supplemental Table 2; http://links.lww.com/EE/A277). The odds of spontaneous early-term birth were higher in the 1-week lag exposed group than in the corresponding unexposed group in both the unadjusted (OR, 1.11; 95% CI = 1.01, 1.22) and adjusted (OR, 1.14; 95% CI = 1.04, 1.25) models (Figure 3B and Supplementary Table 3; http://links.lww.com/EE/A277). The odds of spontaneous early-term birth were not elevated when considering the 2-week and 4-week lags (adjusted OR, 1.03; 95% CI = 0.95, 1.11 and 1.02; 95% CI = 0.96, 1.08, respectively) (Figure 3B and Supplementary Table 3; http://links.lww.com/EE/A277).
Figure 3.
Odds ratios and confidence intervals of spontaneous (A) preterm and (B) early-term birth associated with exposure to Hurricane Harvey.
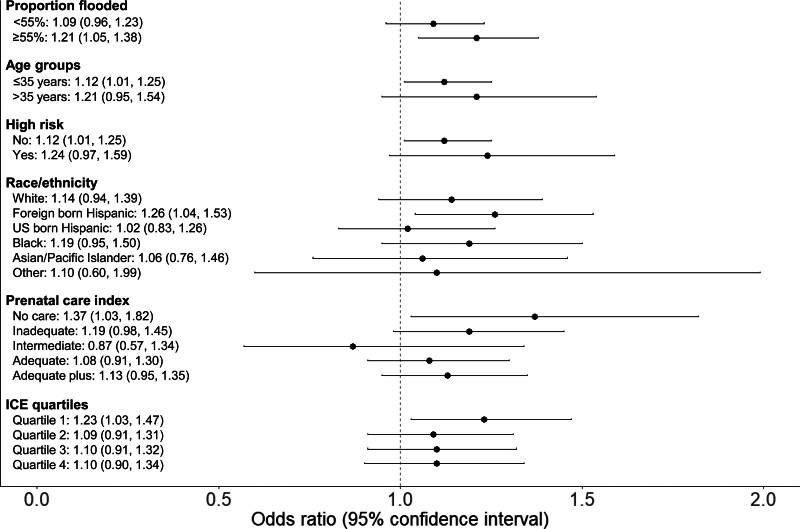
We found no evidence of vulnerable subgroups for spontaneous preterm birth when considering neighborhood extent of flooding, maternal age, race/ethnicity and nativity, high-risk pregnancy, or prenatal care (Supplementary Table 4; http://links.lww.com/EE/A277). CIs were wide and a limited number of cases in the exposed groups may have resulted in Type II error. Pregnancies in neighborhoods with a high extent of flooding had elevated odds of spontaneous early-term birth (OR, 1.21; 95% CI = 1.05, 1.38), while the association was attenuated in neighborhoods with less flooding (OR, 1.09; 95% CI = 0.96, 1.23) (Figure 4 and Supplementary Table 5; http://links.lww.com/EE/A277). In addition, foreign-born Hispanics had higher odds of spontaneous early-term birth than other racial/ethnic groups (OR, 1.26; 95% CI = 1.04, 1.53) (Figure 4 and Supplementary Table 5; http://links.lww.com/EE/A277). Birth parents who did not receive prenatal care and those who lived in neighborhoods of racialized economic segregation (lowest ICE quartile) also had higher odds of spontaneous early-term birth than other prenatal care groups (OR, 1.37; 95% CI = 1.03, 1.82 and 1.23; 95% CI = 1.03, 1.47, respectively) (Figure 4 and Supplementary Table 5; http://links.lww.com/EE/A277). Effect estimates for birth parents over age 35, and those with high-risk pregnancies were also elevated but not statistically significant (Figure 4 and Supplementary Table 5; http://links.lww.com/EE/A277).
Figure 4.
Adjusted odds ratios and confidence intervals of spontaneous early-term birth associated with exposure to Hurricane Harvey (1-week lag) by potentially vulnerable subgroups.
Effect estimates were similar when we expanded the study area to include additional counties in the sensitivity analysis (Supplementary Table 6; http://links.lww.com/EE/A277).
Discussion
In this retrospective cohort study of 15,564 births from Greater Houston, Texas 2015–2019, we found that births occurring during or within 1 week of Hurricane Harvey had 14% higher odds of spontaneous early-term birth compared to the unexposed. The association was attenuated when extending the definition of exposure to 2 weeks or 4 weeks after the hurricane, suggesting that the impact of Hurricane Harvey on spontaneous early-term birth was primarily acute. Pregnancies in neighborhoods with a greater extent of flooding were at elevated odds of spontaneous early-term birth than those with a lower extent of flooding (21% and 9% odds, respectively). Foreign-born Hispanic birth parents were also at greatest odds, with hurricane exposure within 1 week being associated with 26% higher odds of spontaneous early-term birth within this group as compared to 14% for non-Hispanic Whites. In addition, birth parents without prenatal care were at 37% higher odds of spontaneous early-term birth, much higher than other prenatal care index groups. We observed no association between exposure to Hurricane Harvey and spontaneous preterm birth.
We are unaware of prior studies of early-term birth in relation to hurricane exposure. Nevertheless, our results are in line with previous work showing shorter gestational age after exposure to Hurricane Irene (0.7 day)43 and injury during Hurricane Katrina (5 days).44 The underlying mechanisms for the association we observed could involve multiple pathways. Prenatal stress caused by Hurricane Harvey45,46 may have led to stress-related alterations in maternal-placental-fetal endocrine and immune processes.14 Additionally, Hurricane Harvey disrupted access to prenatal care,15 which may have also led to spontaneous early-term birth.47 Other adverse factors associated with Hurricane Harvey, including bodily injury,44 exposure to chemical and environmental pollutants,48,49 mold,50 and food insecurity,51 may also have contributed to the higher risk of spontaneous early-term birth.
With respect to preterm birth, our findings are consistent with a prior study of Hurricane Harvey using data from two Houston hospitals.25 The authors compared the risk of preterm birth (spontaneous and indicated) among exposed pregnancies, defined as those resulting in births within 40 weeks of 25 August 2017, versus births since 2011 (controlling for seasonality and secular trends) and found no evidence of an association. Multiple prior studies have explored associations between other hurricanes and preterm birth in the United States,9 yielding mixed findings with positive,10,11,52 null,53,54 and even negative54 associations. The conflicting results could relate to differences in hurricane characteristics, severity, impacts, and emergency response as well as the definitions utilized of hurricane exposure (e.g., acute or chronic, trimester-specific, and affected areas) and preterm birth (e.g., indicated or spontaneous).9 A study of 58 hurricanes from 1989 to 2002 in the eastern United States found that hurricane exposure was associated with a higher risk of spontaneous preterm birth within 1 month (1%, 2%, and 4% higher risk per 10,000 pregnancies, respectively).10 Our study lacked the statistical power to detect such a small association. Given our sample size, we estimate that we would have required over 200,000 births using a similar 1-month lag to detect an OR of 1.06 (two-sided test, power of 0.80, alpha of 0.05, 18% exposed, and 7% spontaneous preterm birth rate in the unexposed group). We were also unable to examine extreme or early preterm births, which are more severe and have been previously linked with hurricane exposure,10,53 due to sample size limitations.
Exposure to hurricanes and severe flooding has been shown to disproportionately impact the health of marginalized populations, including socially vulnerable counties,10 low-income communities,55 and people of color,56 including non-Hispanic Blacks,55,57 and Hispanics.53,58 In our study, we found that foreign-born Hispanics giving birth within a week of the storm had a higher risk of spontaneous early-term birth than other racial/ethnic groups, although they had a lower crude rate of early-term birth compared to other racial/ethnic groups except for non-Hispanic Whites. A previous study conducted in the Houston and Miami MSAs found that foreign-born Hispanics exhibited lower levels of self-protection and knowledge of flood and hurricane hazards and higher perceived risk than US-born Hispanics and non-Hispanic Whites.58 These disparities might be due to factors like limited English language proficiency, which can hinder access to information and resources, and precarious immigration status and housing tenure. Another study on the respiratory health impacts of a 2006 flood event in El Paso, Texas, a majority Hispanic population, found increased risk among those lacking US citizenship, suggesting postdisaster health disparities among politically marginalized groups.59 Research has shown that non-US citizen Hispanic people are more likely to experience constraints in accessing resources like public assistance or healthcare, which contributes to poor health outcomes, particularly following a disaster.60 Apart from these social vulnerabilities, there is also evidence that shows marginalized Hispanic immigrants in the Houston MSA have a greater likelihood of living in a 100-year flood zone compared to non-Hispanic Whites, and therefore face disproportionate flood and related health risks due to place of residence.61
Our study also found that birth parents who resided in neighborhoods of racialized economic disadvantage (ICE quartile 1), as well as those who did not receive prenatal care were more negatively impacted by Hurricane Harvey regarding spontaneous early-term birth. In a prior study, we found that racialized economic segregation increased the risk of preterm birth due to extreme heat exposure in this population.36 Together, these findings suggest more frequent extreme weather events due to climate change may worsen social disparities in pre- and early-term births. Several factors, including young age, low education level, low socioeconomic status, and unintended pregnancy, are associated with a lack of use of prenatal care.62 In our 1-week lag sample, individuals in the no prenatal care group were more likely to identify as Hispanic or non-Hispanic Black, have lower educational attainment, have public insurance, be unmarried, and have smoked pre-pregnancy or during pregnancy (Supplementary Table 7; http://links.lww.com/EE/A277). In addition, prenatal care may have been directly interrupted by Hurricane Harvey.
Effect estimates in our study were attenuated with increasing time after the storm, indicating a waning influence of the hurricane on birth outcomes. However, it is possible that there were additional effects that manifested over longer time periods, which we did not consider in our study. This may be particularly true among displaced individuals, which we were unable to identify because administrative birth records only include residential address at birth, or if the storm impacted fertility or rates of fetal loss. Less than a third of conceptions are thought to result in live births,63 but our study lacked information on stillbirth or miscarriage. Previous studies suggested that exposure to hurricanes or flooding is associated with more stillbirths.25,64 If Hurricane Harvey resulted in stillbirth or miscarriage, our study may have underestimated the true association via differential fetal loss among those with underlying susceptibility, especially for vulnerable subgroups.65,66 Sample size limitations in our study may have also resulted in a lack of statistical power to detect a small change in preterm birth risks and elevated risks for the smaller subpopulations. Moreover, we relied on noninduced labor to define spontaneous births, which may have included medically indicated preterm deliveries, leading to outcome misclassification. Finally, this study was observational by design, so uncontrolled confounding, such as due to policy changes, may exist.
In conclusion, we found that Hurricane Harvey was associated with increased odds of spontaneous early-term birth, especially in neighborhoods with a greater extent of flooding or concentrated racialized economic disadvantage, among foreign-born Hispanics, and among birth parents who did not receive prenatal care, highlighting the importance of assessing the role of disparities in flood risk, segregation, and social marginalization in future work. If confirmed by future studies, our findings suggest that the increased frequency and severity of extreme weather events due to climate change may further exacerbate health disparities.
Conflicts of interest statement
The authors declare that they have no conflicts of interest with regard to the content of this report.
Supplementary Material
Footnotes
Published online 17 May 2024
Supported by grant 84003901 from the U.S. Environmental Protection Agency (EPA) and the Jonathan and Karin Fielding Presidential Chair in Health Equity. The contents of this document do not necessarily reflect the views and policies of the EPA, nor does the EPA endorse trade names or recommend the use of commercial products mentioned in this document.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.environepidem.com).
Computing code is available from the authors upon request. Data are confidential and cannot be shared in accordance with human subjects protections.
References
- 1.Wuebbles DJ, Fahey DW, Hibbard KA. Climate science special report: fourth national climate assessment, volume I; 2017. [Google Scholar]
- 2.Pant S, Cha EJ. Potential changes in hurricane risk profile across the United States coastal regions under climate change scenarios. Struct Saf. 2019;80:56–65. [Google Scholar]
- 3.First Street Foundation. The 7th National Risk Assessment: Worsening Winds; 2023. [Google Scholar]
- 4.Reed KA, Wehner MF, Zarzycki CM. Attribution of 2020 hurricane season extreme rainfall to human-induced climate change. Nat Commun. 2022;13:1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang SS, Zhao L, Yoon J-H, Klotzbach P, Gillies RR. Quantitative attribution of climate effects on Hurricane Harvey’s extreme rainfall in Texas. Environ Res Lett. 2018;13:054014. [Google Scholar]
- 6.Cohen D. About 60.2M Live in Areas Most Vulnerable to Hurricanes. Available at: https://www.census.gov/library/stories/2019/07/millions-of-americans-live-coastline-regions.html. [Google Scholar]
- 7.Klotzbach PJ, Bowen SG, Pielke R, Bell M. Continental US hurricane landfall frequency and associated damage: observations and future risks. Bull Am Meteorol Soc. 2018;99:1359–1376. [Google Scholar]
- 8.Grinsted A, Ditlevsen P, Christensen JH. Normalized US hurricane damage estimates using area of total destruction, 1900−2018. Proc Natl Acad Sci USA. 2019;116:23942–23946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeffers NK, Glass N. Integrative review of pregnancy and birth outcomes after exposure to a hurricane. J Obstet Gynecol Neonatal Nurs. 2020;49:348–360. [DOI] [PubMed] [Google Scholar]
- 10.Sun S, Weinberger KR, Yan M, Anderson GB, Wellenius GA. Tropical cyclones and risk of preterm birth: a retrospective analysis of 20 million births across 378 US counties. Environ Int. 2020;140:105825. [DOI] [PubMed] [Google Scholar]
- 11.Xiong X, Harville EW, Buekens P, Mattison DR, Elkind-Hirsch K, Pridjian G. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. Am J Med Sci. 2008;336:111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zahran S, Snodgrass JG, Peek L, Weiler S. Maternal hurricane exposure and fetal distress risk. Risk Anal. 2010;30:1590–1601. [DOI] [PubMed] [Google Scholar]
- 13.Harville EW, Pan K, Beitsch L, et al. Hurricane Michael and adverse birth outcomes in the Florida Panhandle: analysis of vital statistics data. Disaster Med Public Health Prep. 2022;17:e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Entringer S, Buss C, Wadhwa PD. Prenatal stress and developmental programming of human health and disease risk: concepts and integration of empirical findings. Curr Opin Endocrinol Diabetes Obes. 2010;17:507–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chambers KA, Husain I, Chathampally Y, et al. Impact of Hurricane Harvey on healthcare utilization and emergency department operations. West J Emerg Med. 2020;21:586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang W, Gao Y, Xu R, et al. Health effects of cyclones: a systematic review and meta-analysis of epidemiological studies. Environ Health Perspect. 2023;131:86001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zoraster RM. Vulnerable populations: Hurricane Katrina as a case study. Prehosp Disaster Med. 2010;25:74–78. [DOI] [PubMed] [Google Scholar]
- 18.Delnord M, Zeitlin J. Epidemiology of late preterm and early term births–an international perspective. Semin Fetal Neonatal Med. 2019;24:3–10. [DOI] [PubMed] [Google Scholar]
- 19.Sengupta S, Carrion V, Shelton J, et al. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr. 2013;167:1053–1059. [DOI] [PubMed] [Google Scholar]
- 20.Murphy JD. August/September 2017 Hurricane Harvey. In: Administration NOaA, ed; 2018. [Google Scholar]
- 21.Jonkman SN, Godfroy M, Sebastian A, Kolen B. Brief communication: loss of life due to Hurricane Harvey. Nat Hazards Earth Syst Sci. 2018;18:1073–1078. [Google Scholar]
- 22.Carrel M, Clore GS, Kim S, et al. Health care utilization among Texas Veterans Health Administration enrollees before and after Hurricane Harvey, 2016-2018. JAMA Netw Open. 2021;4:e2138535–e2138535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramesh B, Jagger MA, Zaitchik B, et al. Emergency department visits associated with satellite observed flooding during and following Hurricane Harvey. J Expo Sci Environ Epidemiol. 2021;31:832–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parks RM, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, Kioumourtzoglou M-A. Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat Commun. 2021;12:1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendez-Figueroa H, Chauhan SP, Tolcher MC, et al. Peripartum outcomes before and after Hurricane Harvey. Obstet Gynecol. 2019;134:1005–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Talge NM, Mudd LM, Sikorskii A, Basso O. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics. 2014;133:844–853. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Commerce National Oceanic and Atmospheric Association. Service Assessment: August/September 2017 Hurricane Harvey. Available at: https://www.weather.gov/media/publications/assessments/harvey6-18.pdf. [Google Scholar]
- 28.Liberto TD. Reviewing Hurricane Harvey’s catastrophic rain and flooding. Available at: https://www.climate.gov/news-features/event-tracker/reviewing-hurricane-harveys-catastrophic-rain-and-flooding. [Google Scholar]
- 29.Edwards R, Nowotarski CJO, Scott, Woodall GR. Tornadoes in Hurricane Harvey: Documentation and Environmental Analysis. [Google Scholar]
- 30.Chakraborty J, Collins TW, Grineski SE. Exploring the environmental justice implications of Hurricane Harvey flooding in Greater Houston, Texas. Am J Public Health. 2019;109:244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.United States Geological Survey. National Hydrography Dataset. Available at: https://www.usgs.gov/national-hydrography/access-national-hydrography-products. [Google Scholar]
- 32.Boyd RW, Lindo EG, Weeks LD, McLemore MR. On racism: a new standard for publishing on racial health inequities. Health Affairs Forefront. 2020. [Google Scholar]
- 33.Slaughter-Acey JC, Sealy-Jefferson S, Helmkamp L, et al. Racism in the form of micro aggressions and the risk of preterm birth among black women. Ann Epidemiol. 2016;26:7–13.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sudhinaraset M, Woofter R, Young M-EDT, Landrian A, Vilda D, Wallace SP. Analysis of state-level immigrant policies and preterm births by race/ethnicity among women born in the US and women born outside the US. JAMA Netw Open. 2021;4:e214482–e214482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kotelchuck M. An evaluation of the Kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health. 1994;84:1414–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cushing LJ, Morello-Frosch R, Hubbard A. Extreme heat and its association with social disparities in the risk of spontaneous preterm birth. Paediatr Perinat Epidemiol. 2022;36:13–22. [DOI] [PubMed] [Google Scholar]
- 37.Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2016;106:256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.FEMA. Designated Areas: Disaster 4332. Available at: https://www.fema.gov/disaster/4332/designated-areas. [Google Scholar]
- 39.PRISM Climate Group. PRISM Climate Data. Available at: https://prism.oregonstate.edu/. [Google Scholar]
- 40.Anderson G, Yan M, Ferreri J, et al. Hurricane exposure: explore and Map County-Level Hurricane Exposure in the United States. R package version 0.1. 1. 2020. [Google Scholar]
- 41.Anderson G, Schumacher A, Crosson W, et al. Hurricane exposure data: data Characterizing Exposure to Hurricanes in United States Counties. R package version 0.1. 0. 2020. [Google Scholar]
- 42.National Hurricane Center and Central Pacific Hurricane Center. Saffir-Simpson Hurricane Wind Scale. Available at: https://www.nhc.noaa.gov/aboutsshws.php. [Google Scholar]
- 43.Hochard J, Li Y, Abashidze N. Associations of hurricane exposure and forecasting with impaired birth outcomes. Nat Commun. 2022;13:6746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harville EW, Giarratano G, Savage J, Barcelona de Mendoza V, Zotkiewicz T. Birth outcomes in a disaster recovery environment: New Orleans women after Katrina. Matern Child Health J. 2015;19:2512–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oluyomi AO, Panthagani K, Sotelo J, et al. Houston Hurricane Harvey health (Houston-3H) study: assessment of allergic symptoms and stress after Hurricane Harvey flooding. Environ Health. 2021;20:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fitzpatrick KM. Post-traumatic stress symptomatology and displacement among Hurricane Harvey survivors. Soc Sci Med. 2021;270:113634. [DOI] [PubMed] [Google Scholar]
- 47.Debiec KE, Paul KJ, Mitchell CM, Hitti JE. Inadequate prenatal care and risk of preterm delivery among adolescents: a retrospective study over 10 years. Am J Obstet Gynecol. 2010;203:122.e1–122.e6. [DOI] [PubMed] [Google Scholar]
- 48.Du J, Park K, Yu X, Zhang YJ, Ye F. Massive pollutants released to Galveston Bay during Hurricane Harvey: understanding their retention and pathway using Lagrangian numerical simulations. Sci Total Environ. 2020;704:135364. [DOI] [PubMed] [Google Scholar]
- 49.Qin R, Khakzad N, Zhu J. An overview of the impact of Hurricane Harvey on chemical and process facilities in Texas. Int J Disaster Risk Reduct. 2020;45:101453. [Google Scholar]
- 50.Chow NA, Toda M, Pennington AF, et al. Hurricane-associated mold exposures among patients at risk for invasive mold infections after Hurricane Harvey—Houston, Texas, 2017. Morb Mortal Wkly Rep. 2019;68:469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clay LA, Ross AD. Factors associated with food insecurity following Hurricane Harvey in Texas. Int J Environ Res Public Health. 2020;17:762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Antipova A, Curtis A. The post-disaster negative health legacy: pregnancy outcomes in Louisiana after Hurricane Andrew. Disasters. 2015;39:665–686. [DOI] [PubMed] [Google Scholar]
- 53.Grabich SC, Robinson WR, Engel SM, Konrad CE, Richardson DB, Horney JA. Hurricane Charley exposure and hazard of preterm delivery, Florida 2004. Matern Child Health J. 2016;20:2474–2482. [DOI] [PubMed] [Google Scholar]
- 54.Harville EW, Tran T, Xiong X, Buekens P. Population changes, racial/ethnic disparities, and birth outcomes in Louisiana after Hurricane Katrina. Disaster Med Public Health Prep. 2010;4:S39–S45. [DOI] [PubMed] [Google Scholar]
- 55.Elliott JR, Pais J. Race, class, and Hurricane Katrina: social differences in human responses to disaster. Soc Sci Res. 2006;35:295–321. [Google Scholar]
- 56.Berberian AG, Gonzalez DJ, Cushing LJ. Racial disparities in climate change-related health effects in the United States. Curr Environ Health Rep. 2022;9:451–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fussell E, Lowe SR. The impact of housing displacement on the mental health of low-income parents after Hurricane Katrina. Soc Sci Med (1982). 2014;113:137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maldonado A, Collins TW, Grineski SE. Hispanic immigrants’ vulnerabilities to flood and hurricane hazards in two United States metropolitan areas. Geographical Review. 2016;106:109–135. [Google Scholar]
- 59.Jimenez AM, Collins TW, Grineski SE. Intra-ethnic disparities in respiratory health problems among Hispanic residents impacted by a flood. J Asthma. 2013;50:463–471. [DOI] [PubMed] [Google Scholar]
- 60.Carrasquillo O, Carrasquillo AI, Shea S. Health insurance coverage of immigrants living in the United States: differences by citizenship status and country of origin. Am J Public Health. 2000;90:917–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maldonado A, Collins TW, Grineski SE, Chakraborty J. Exposure to flood hazards in Miami and Houston: are Hispanic immigrants at greater risk than other social groups? Int J Environ Res Public Health. 2016;13:775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hajizadeh S, Ramezani Tehrani F, Simbar M, Farzadfar F. Factors influencing the use of prenatal care: a systematic review. JMRH. 2016;4:544–557. [Google Scholar]
- 63.Boklage CE. Survival probability of human conceptions from fertilization to term. Int J Fertil. 1990;35:75, 79–80, 81. [PubMed] [Google Scholar]
- 64.Mallett LH, Etzel RA. Flooding: what is the impact on pregnancy and child health? Disasters. 2018;42:432–458. [DOI] [PubMed] [Google Scholar]
- 65.Goin DE, Casey JA, Kioumourtzoglou M-A, Cushing LJ, Morello-Frosch R. Environmental hazards, social inequality, and fetal loss: implications of live-birth bias for estimation of disparities in birth outcomes. Environ Epidemiol. 2021;5:e131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harville EW, Xiong X, David M, Buekens P. The paradoxical effects of Hurricane Katrina on births and adverse birth outcomes. Am J Public Health. 2020;110:1466–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.