Abstract
Introduction:
Burns and fires in the operating room are a known risk and their prevention has contributed to many additional safety measures. Despite these safeguards, burn injuries contribute significantly to the medical malpractice landscape. The aim of the present study is to analyze malpractice litigation related to burn and fire injuries in plastic and reconstructive surgery, identify mechanisms of injury, and develop strategies for prevention.
Methods:
The Westlaw and LexisNexis databases were queried for jury verdicts and settlements in malpractice lawsuits related to burn and fire injuries that occurred during plastic surgery procedures. The Boolean terms included “burn & injury & plastic”, “fire & injury & “plastic surg!”” in Westlaw, and “burn & injury & “plastic surg!””, “fire & injury & “plastic surg!”” in LexisNexis.
Results:
A total of 46 cases met the inclusion criteria for this study. Overheated surgical instruments and cautery devices were the most common mechanisms for litigation. Plastic surgeons were defendants in 40 (87%) cases. Of the included cases, 43% were ruled in favor of the defendant, while 33% were ruled in favor of the plaintiff. Mishandling of cautery devices 6 (13%), heated surgical instruments 6 (13%), and topical acids 2 (4%) were the most common types of errors encountered.
Conclusion:
Never events causing burn injury in plastic and reconstructive surgery are ultimately caused by human error or neglect. The misuse of overheated surgical instruments and cauterizing devices should be the focus for improving patient safety and reducing the risk of medical malpractice. Forcing functions and additional safeguards should be considered to minimize the risk of costly litigation and unnecessary severe harm to patients.
Keywords: Burn Injury, Fire Injury, Plastic surgery, Never events, Malpractice in plastic surgery, Litigation
1. Introduction
Iatrogenic injury presents a serious issue in healthcare, with the opportunity to inflict physical harm, psychological trauma, and financial burdens on patients and their families. “Never events,” defined as incidents caused by a departure from the standard of care, represent one of the most severe forms of medical malpractice. [1] The National Health System states that the existence of robust systemic safeguards at both the national and healthcare provider levels are needed to prevent these incidents. [2].
Among medical errors, surgical errors carry direct and severe consequences, including death or permanent injury. [3] According to a 2022 annual summary published by The Joint Commission, a non-profit focused on healthcare organization accreditation, burn injuries are among the top ten sentinel event types within healthcare. [4] In an endeavor to incentivize surgical patient safety, pay-for-performance programs have introduced penalties for hospitals involved in such incidents since 2008, aiming to promote surgical patient safety. [3,5].
Severe burn and fire injuries are particularly significant never events, leading to potentially life-threatening complications and costly lawsuits that contribute to the annual $55.6 billion medical liability system in the United States. [4,6] Plastic and reconstructive surgeons face a 15% chance of being sued each year, [6] twice as likely as other physicians (13%–15% vs 7% each year). [7–12] The present study aims to review burn and fire injury malpractice litigations related to plastic and reconstructive surgery procedures with the goal of identifying the most common mechanisms of injury and proposing solutions to prevent these events from occurring.
2. Methods
2.1. Study design
Following an Institutional Review Board of the Icahn School of Medicine at Mount Sinai exemption, medical malpractice litigations were queried using the Westlaw (Thomson Reuters Corporation, Canada) and LexisNexis (RELX Group, New York) legal databases. The Westlaw database is a comprehensive online collection of court documents and records from over 40,000 legal databases in the United States. [7,13] The LexisNexis search engine contains a global legal and news database that has 139 billion documents and records. [14] Any single case within these two databases includes information such as the names of defendants and plaintiffs, expert witness identification if used, date of the incident in question, filing date of the lawsuit, and date of trial or settlement. Lastly, most entries include a synopsis of the case or injury.
A Boolean search was utilized to query medical malpractice cases related to burn injuries, specifically jury verdicts and settlements from federal and district court cases. The following Boolean terms were used: “burn & injury & plastic”, “fire & injury & ”plastic surg!” in Westlaw, and “burn & injury & ”plastic surg!”, “fire & injury & “plastic surg!” in LexisNexis. Cases were included if they were based in state court or federal court and related to burn or fire related surgical or medical-induced injuries during a plastic surgery procedure. For cases with limited information, local district clerk websites were queried to verify or obtain additional case details, if available. Duplicate cases, cases with insufficient information, and burn injuries caused by events or side effects disclosed in patient consent forms, such as chemical peels or laser burns, were excluded from the analysis.
2.2. Variables
The following data was collected for all cases: year of trial or filing, state of filing, state or federal filing status, type of physician involved in the lawsuit, chief complaint, outcome of the case, compensatory damages, and presence of an expert witness supporting the plaintiff and/or defendant. The mechanisms of burn injury were placed into eight major categories: grounding failure, overheated instrument, cauterizer, overheated saline bag, fire, acid burn, overheated lamp, or unknown. The types of human error were categorized, with mishandling defined as misuse of surgical instruments, chemical substances, or heating devices that fell outside of standard care. Misplacement of an instrument was defined as a situation in which a holstering device was present but not used, or situation in which a surgical device was placed inappropriately. A burn caused by any surgical instrument, chemical substance, or heating device that was not caused by mishandling or misplacement was defined as an accident/negligence.
3. Results
The Westlaw and LexisNexis databases yielded a total of 744 cases, 46 of which ultimately met the inclusion criteria for this study (Fig. 1). The 46 cases were filed between the years 1987 and 2018. The year with the most cases was 2009 (n = 6, 13%), followed by 2010 (n = 4, 9%) and 2015 (n = 4, 9%) (Fig. 2). Most plaintiffs were female (n = 34, 74%), with 6 (13%) cases involving male plaintiffs, and 6 (13%) cases reporting an unknown gender. The average plaintiff age was 36.8 years. New York and California had the most cases (n = 7 for each, 15%) (Fig. 3). Except for one federal case, all the included cases were filed in state court (n = 45).
Fig. 1 –
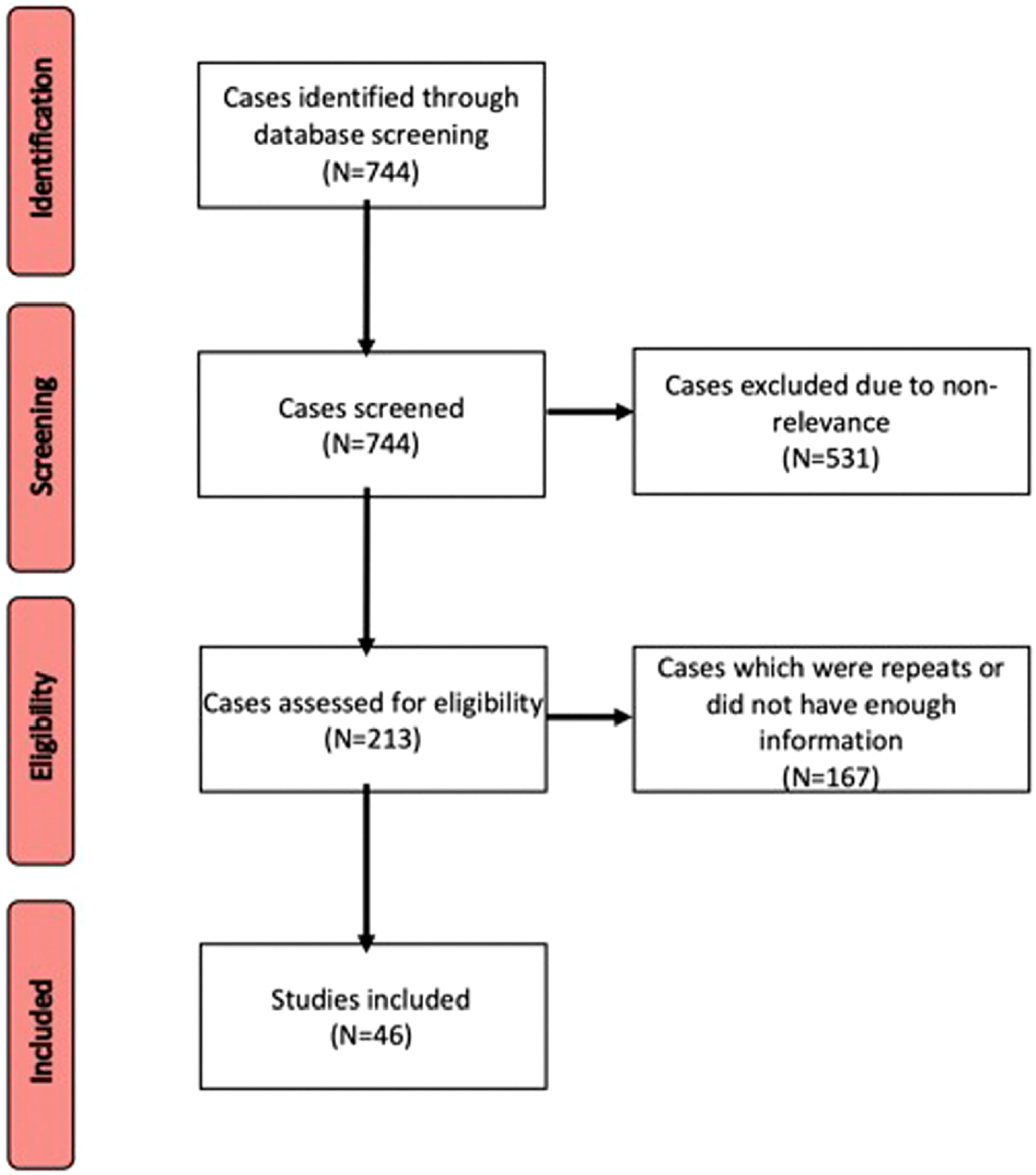
Flowchart of Cases Included in the Final Analysis.
Fig. 2 –
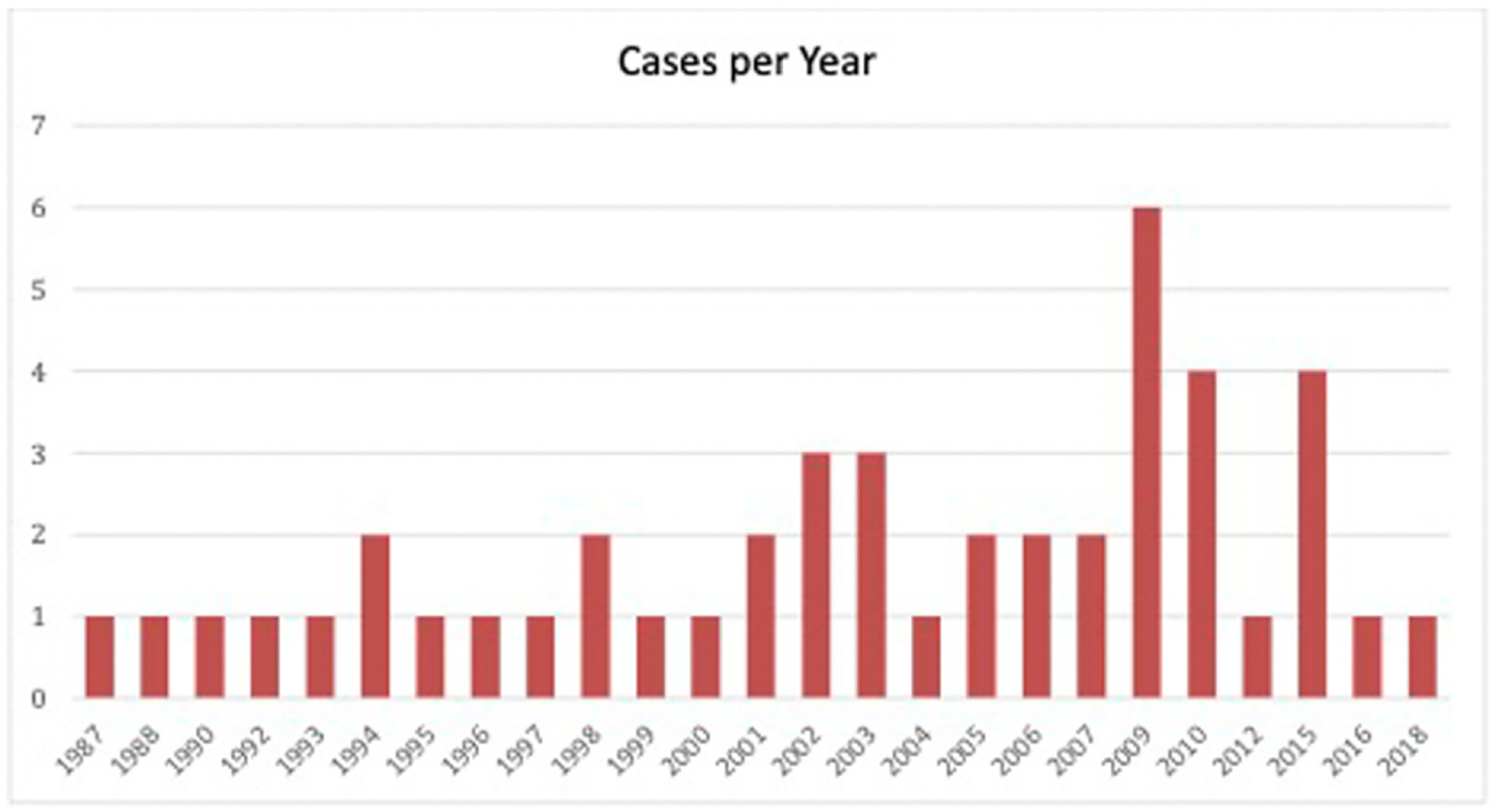
Cases per Year.
Fig. 3 –
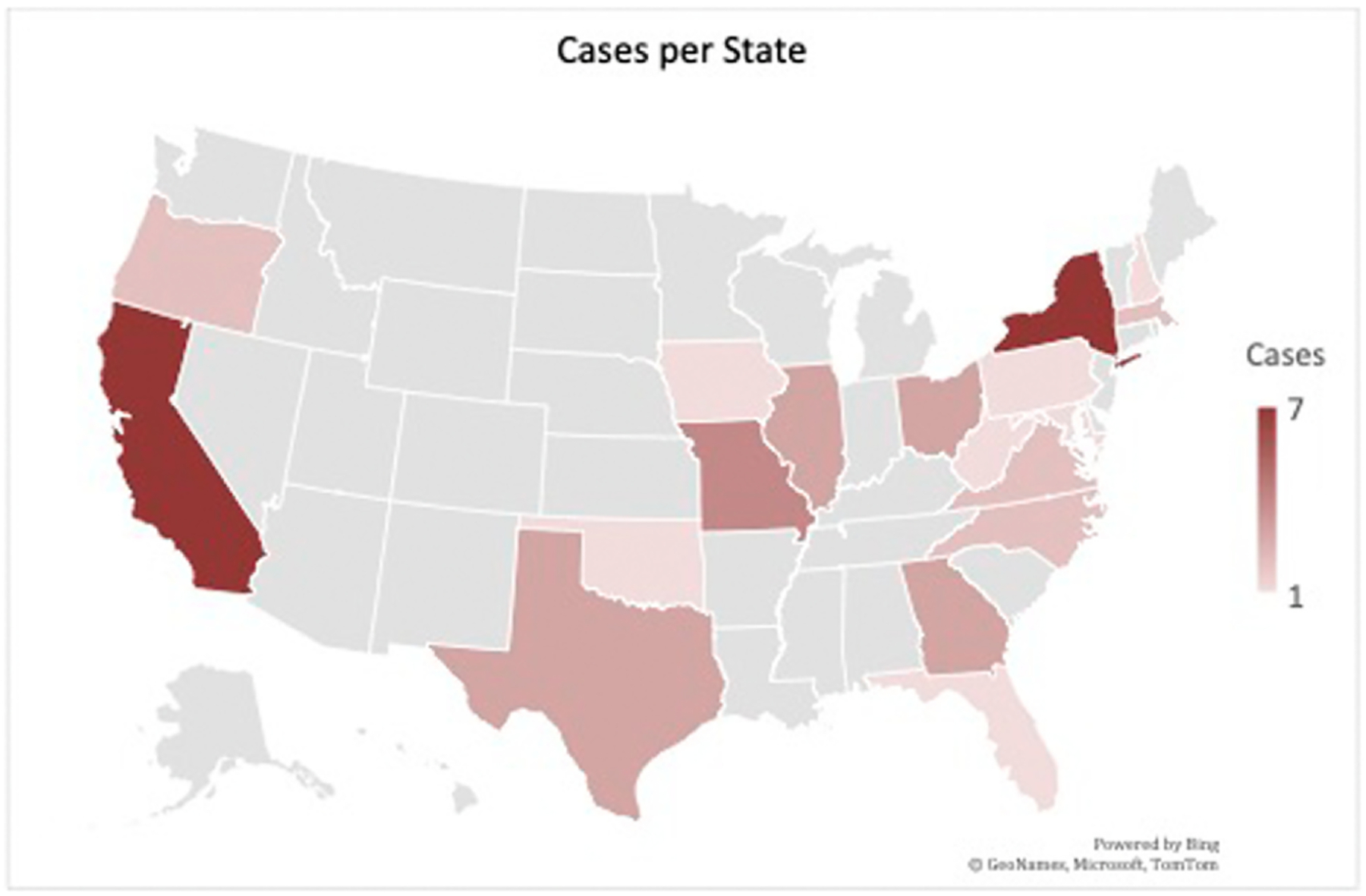
Total number of cases per state.
Injury from cautery devices (n = 10, 22%), fire injuries (n = 9, 20%), and overheated surgical instruments (n = 8, 17%) were the most common mechanisms of burn injury. Less common mechanisms included chemical burns (n = 4, 9%), overheated lamp burns (n = 2, 4%), electrical burns (n = 1, 2%), burns by an overheated saline bag (n = 1, 2%), or other causes (n = 1, 2%) (Fig. 4). In 18 cases, heated surgical instruments in contact with the skin caused burn injury. Electrocautery devices, breast sizers, retractors, and metal implants were among other tools listed. Breast sizers caused burns after undergoing sterilization and the temperature not being checked prior to use. In 15 of these cases, human error due to mishandling and misplacement were the most common cause of burn injuries from overheated instruments and cautery devices (n = 15, 33%) (Fig. 5). In the 9 cases where an operating room fire occurred, mishandling of a cautery device in proximity to an oxygenated nasal cannula caused (n = 7, 15%).
Fig. 4 –
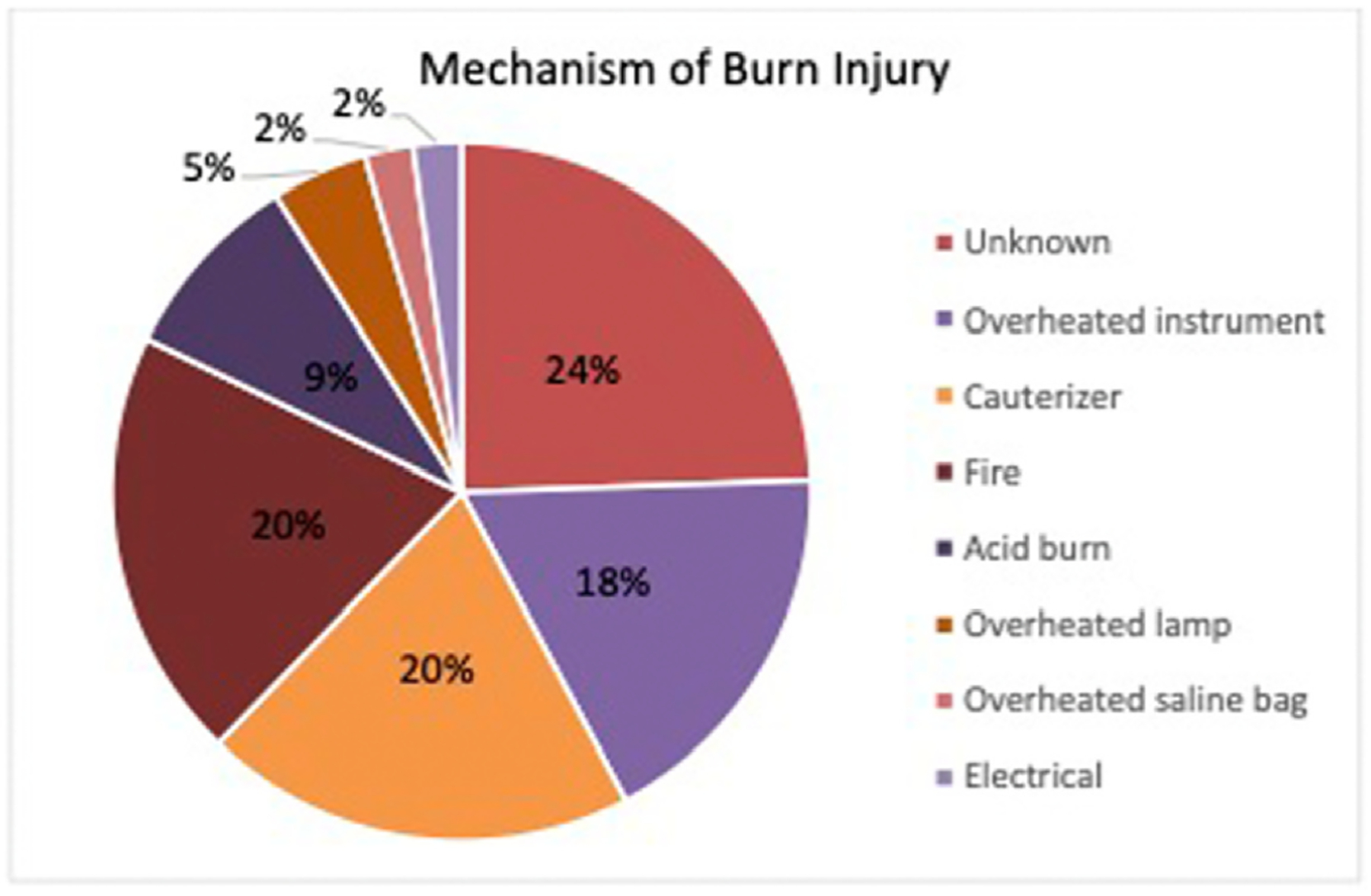
Mechanisms of Burn Involved in Litigation.
Fig. 5 –
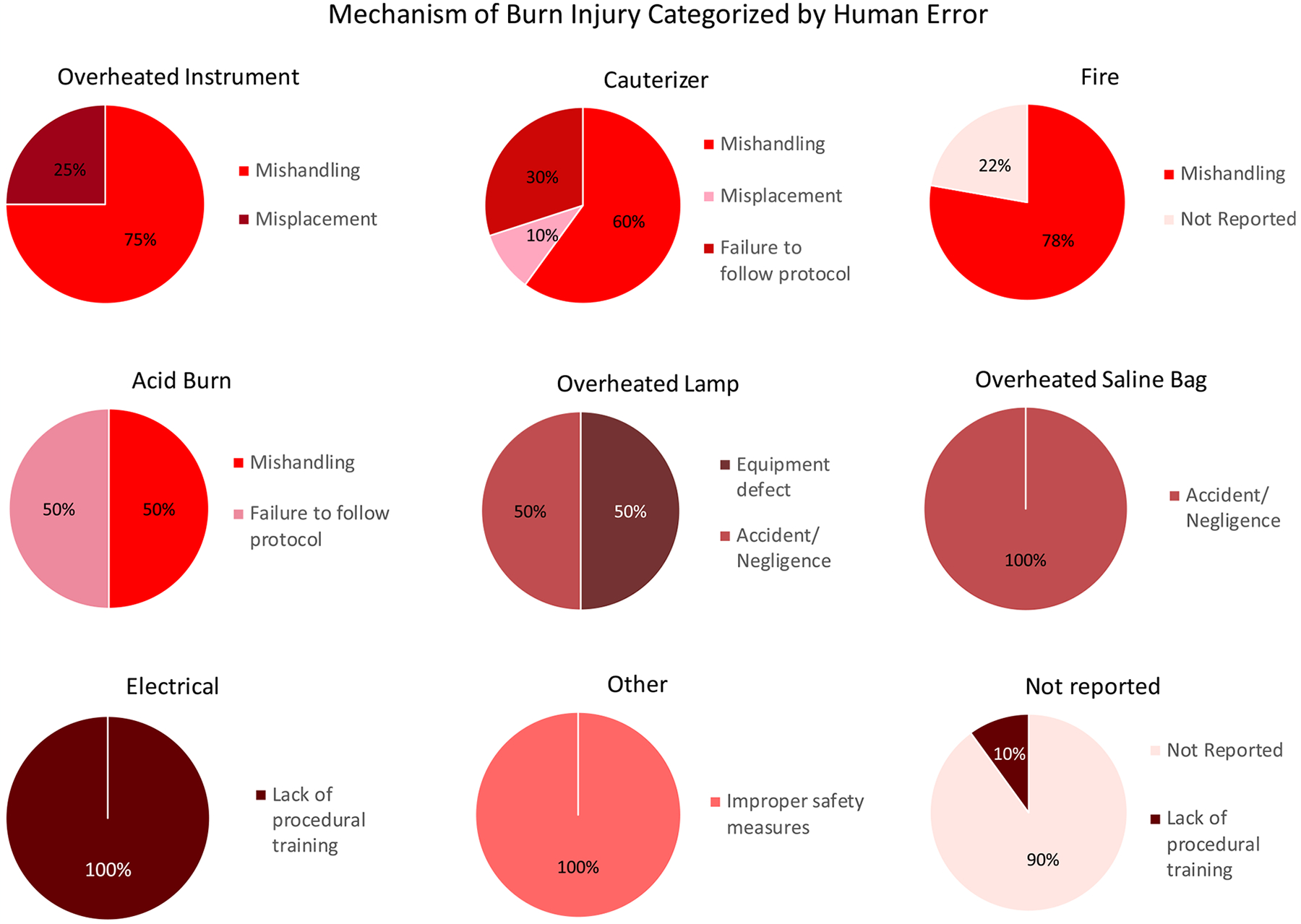
Mechanism of Burn Injury Categorized by Human Error.
Failure to follow proper protocol resulted in patient burns with an electrocautery tool in 3 cases and 2 cases where a caustic agent was used. The first electrocautery tool case involved a burn due to the current traveling through the improper path. In this case, a foley catheter was not placed in the patient prior to starting surgery and the patient urinated during the procedure. The patient claimed that the electrical current traveled through the urine that was on the operating table due to the newly created electrical path. In two other cases, a failure to ground the electrocautery device was found prior to the start of the procedure. Specifically, in one of these cases, failure to properly attach the grounding pad caused the current to run through the patient’s leg after passing along the peripheral nerve and spinal column. Chemical burns occurred in cases where a patient’s allergy was not recorded, and another occurred when a nasal cannula was not removed prior to a procedure, resulting in the caustic agent accumulation near the patient’s nose.
Several cases involved burns caused by various types of human error within the operating room. These cases involved burns caused by a hot saline bag placed in the patient’s axilla for heating and positioning, a corneal burn caused by a failure to use proper corneal protectors, and acid mishandling and spilling on a patient.
Certain specialties and surgical procedures had higher incidents of malpractice burn litigation than others. Breast surgery (n = 19, 41%) was the most common procedure in which these injuries occurred followed by blepharoplasty (n = 6, 13%) and liposuction (n = 5, 11%). Other types of surgery included in litigation were wart removal (n = 2, 4%), mole removal (n = 2, 4%), hand surgery (n = 2, 4%), lip repair (n = 1, 2%), flap surgery (n = 1, 2%), rhinoplasty (n = 1, 2%), abdominoplasty (n = 1, 2%), and face lift (n = 1, 2%) (Fig. 6). Plastic surgeons were defendants in 40 (87%) cases (Fig. 7). Ophthalmologists (n = 1, 2%), radiologists (n = 1, 2%), and otolaryngologists (n = 1, 2%) were less frequently named defendants in lawsuits (Fig. 7).
Fig. 6 –
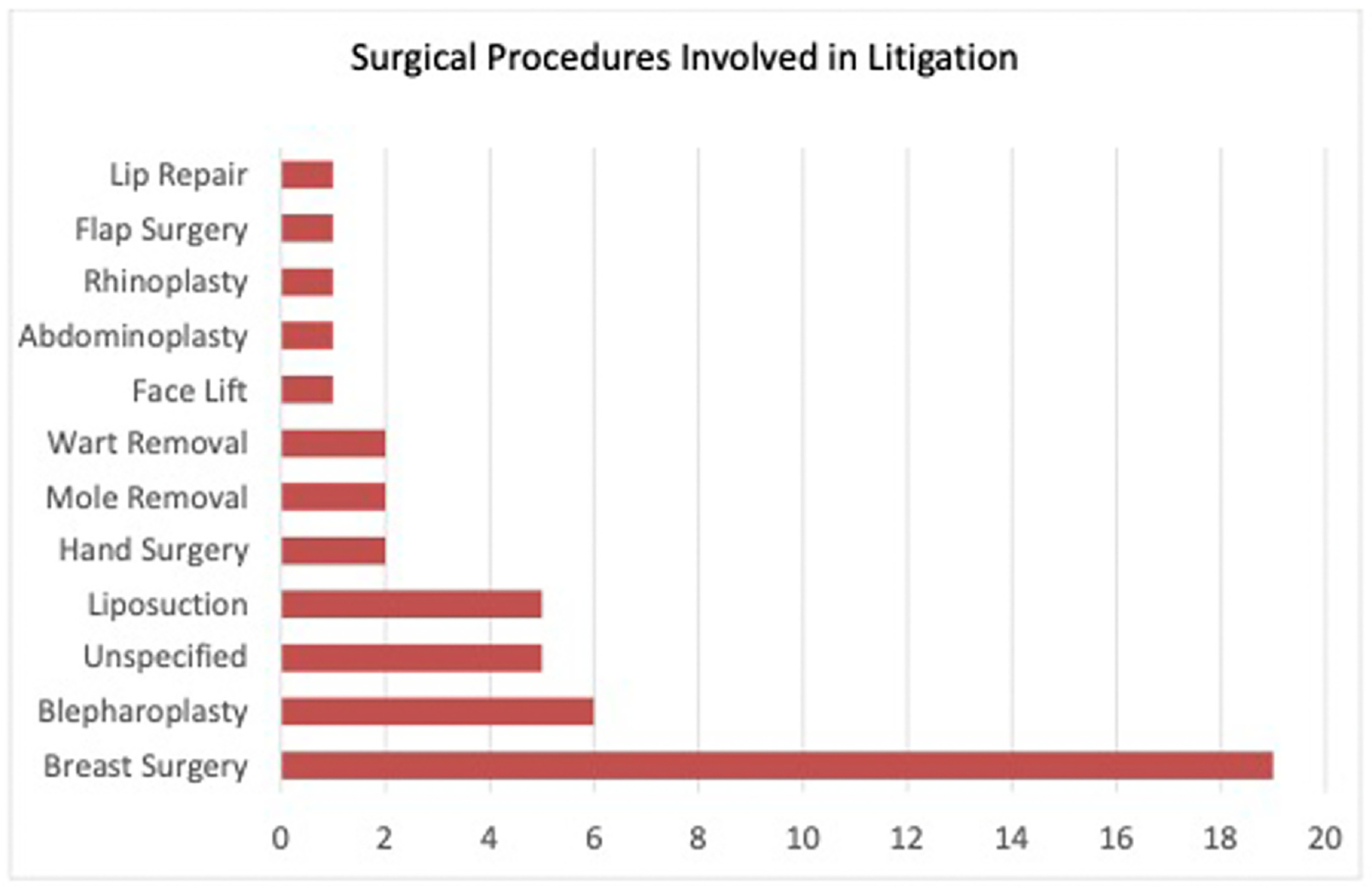
Surgical Procedures Involved in Litigation.
Fig. 7 –
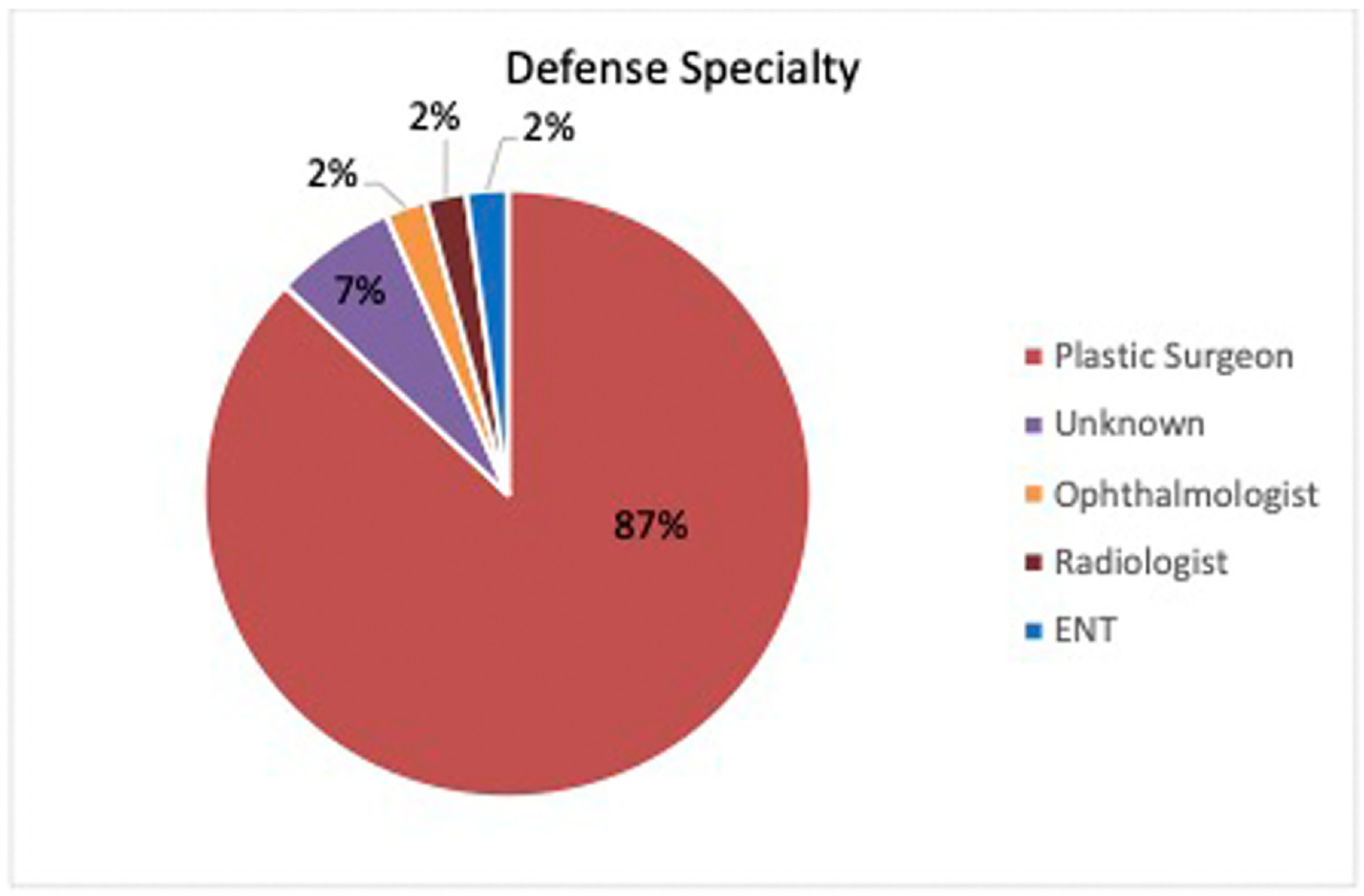
Surgical Specialty.
Of the 46 included cases, 20 (43%) were ruled in favor of the defendant physician or hospital, 15 (33%) were ruled in favor of the plaintiff, 7 (15%) ended in a settlement, 3 (7%) had an unknown outcome, 1 (2%) ended in arbitration, and no cases were dismissed (Fig. 8). The case with the highest payout for the plaintiff involved a patient who suffered third-degree burns on his chest from a lamp during a lip laceration procedure (Fig. 9). The plaintiff was awarded $3080,000. The defendant claimed that the lamp lacked a proper shield, which would have prevented the burns. The second highest amount paid in compensatory damages was $1296,659. In this case, a patient received a second-degree burn from an operating room fire during an eyebrow mole removal procedure. The third highest awarded case had compensatory damages of $690,000 and involved a patient who suffered second-degree thermal burns from a heated knife during a breast reconstruction procedure.
Fig. 8 –
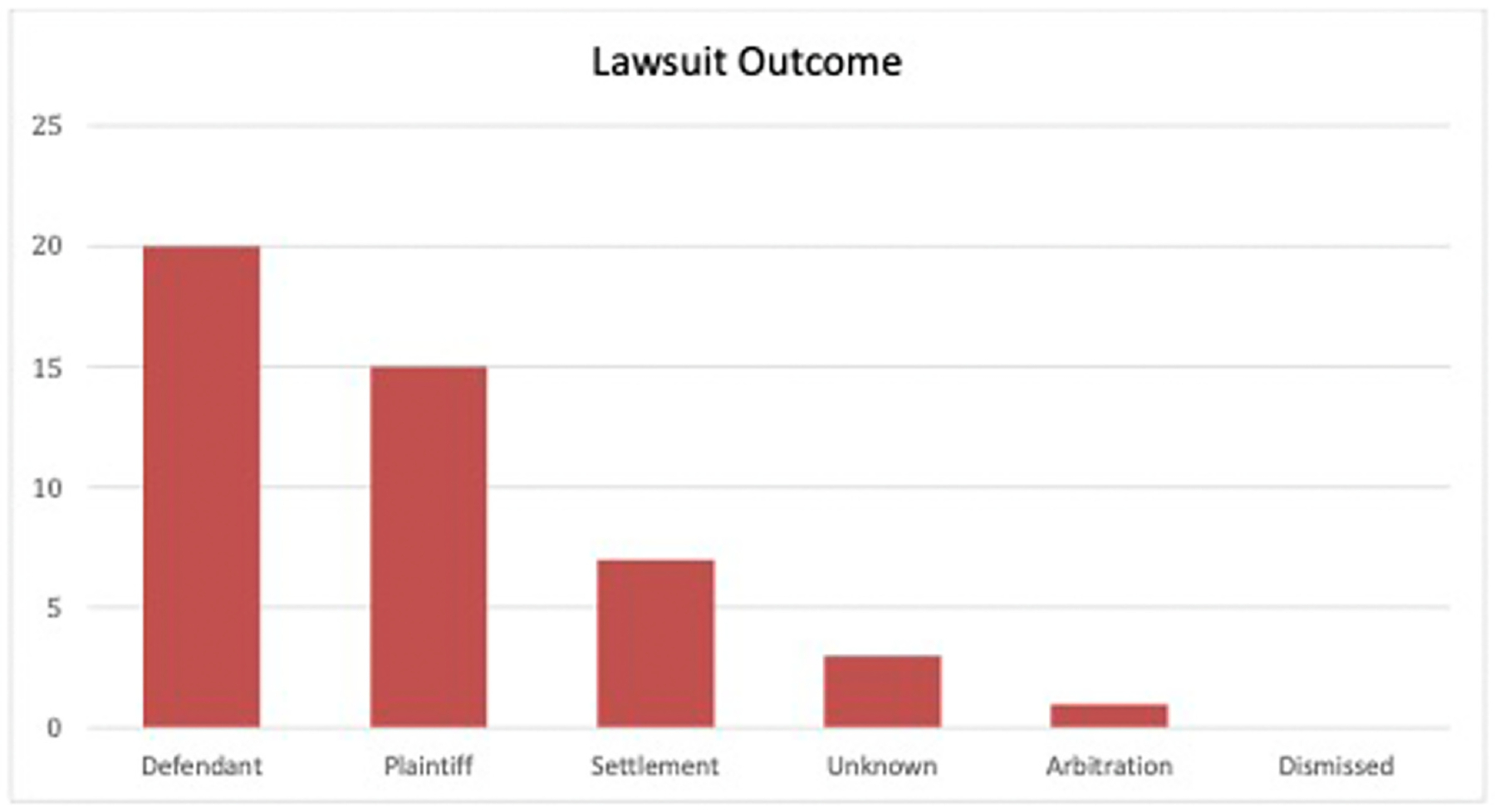
Lawsuit Outcome.
Fig. 9 –
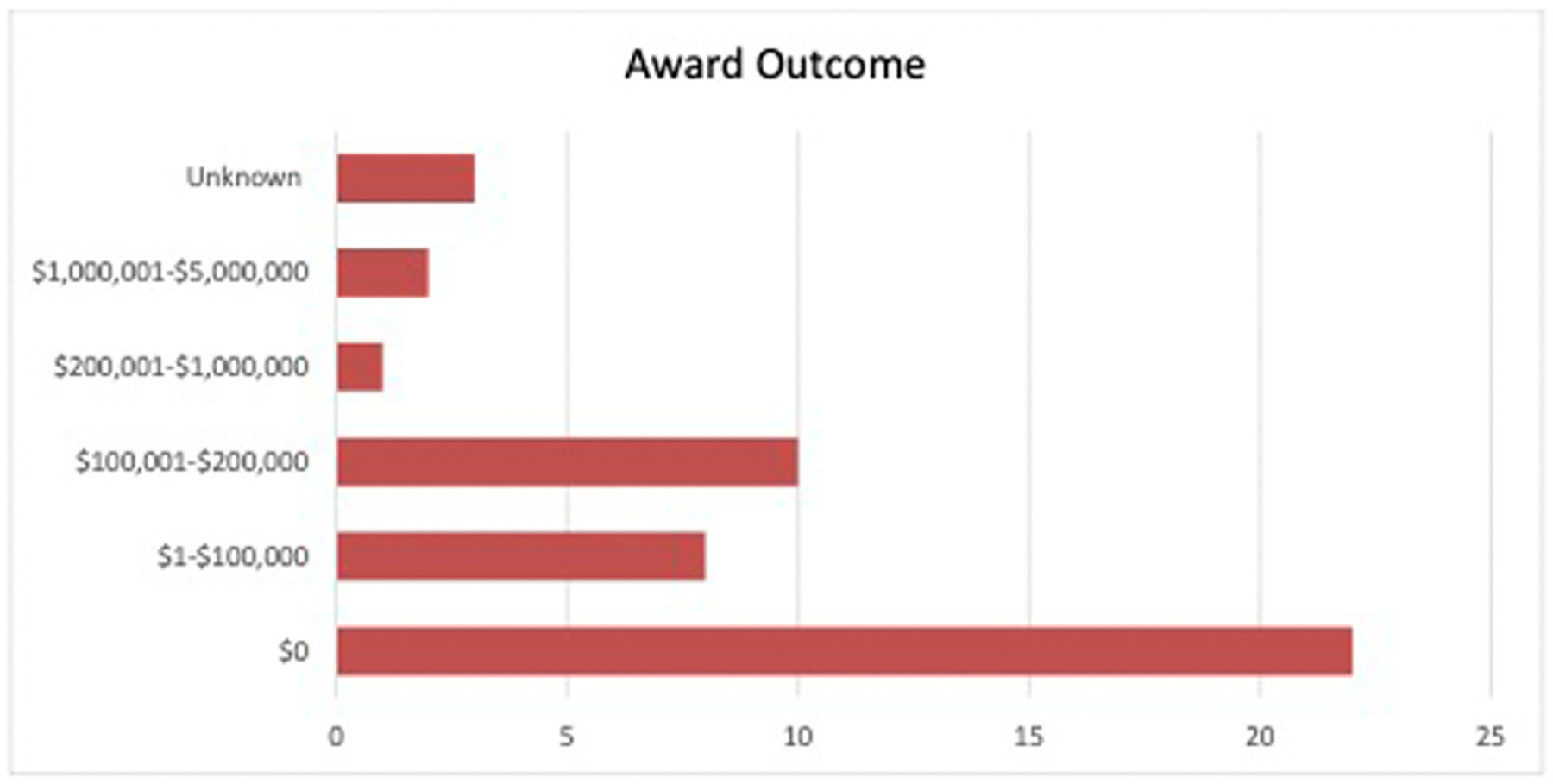
Award Outcome.
4. Discussion
Surgical never events are infrequent, occurring once in every 17,000 operations in England with comparable rates in the United States. [15,16] Furthermore, Moppett et al. found that the risk of serious harm after the occurrence of a never event is approximately 1 in 250,000. [15] Cohen et al. observed that intraoperative burns contributed to 11 never events (8.3%) of the 142 never events studied (rate of 1 in 200,000). Seven were caused by oxygen ignition via electrocautery near the face (63.6%) and two were caused by electrocautery burn to a nonsurgical area (18.2%). [17] The results of the present study indicate that this is an important area for improved safety measures in plastic surgery.
Results of the present study highlight the significant percentage of cauterizer induced burns and fire injury. In fact, electrosurgical units are the most common cause of operating room fires. [18] As the operation of a nasal cannula lies in the purview of the anesthesiologist and the operation of the cauterizer lies in the purview of the surgeon, miscommunication between these two physicians and improper safety procedures can lead to fire when these two pieces of equipment are used in proximity. This type of human error can be prevented in several ways. Both the surgeon and anesthesiologist should confirm no tunneling of drapes between the oxygen rich environment and the surgical field. [19] Additional communication should include discussion of possible risks during time-out. [19] Furthermore, clear communication is made prior to the use of the electrocautery device by the surgeon. [19] Anesthesiologists can minimize or discontinue oxygen prior to the use of the electrocautery device when possible and titrate oxygen to the lowest safe concentration. [19] All of the above suggestions can be reinforced by employing surgical checklists, which have been shown to be an effective intervention for preventing of never events. [20].
In instances in which burns were caused by mishandling or misplacement of overheated surgical instruments, no safeguards were in place to verify that the instrument was stored when not in use and that the instrument was not overheated prior to use or skin contact. To prevent burns from overheated instruments, systematic checks should be instilled to ensure safe temperatures during use, and the surgical team should always verify that electrocautery tools are placed in a holster when not in use. Electrocautery tools should be treated as scalpels in the surgical field; when not in use, the instrument should be handed to the surgical technician for safekeeping. A study by DeGirolamo et al. looked at safety in the operating room pertaining to scalpel use and discovered that the use of the “hands-free” technique has proven especially useful in decreasing accidental scalpel-induced injury. [21] Additional safeguards could include alerts that sound when the tool is inactive and outside of the holster for an extended period of time, or forcing functions that turn the equipment off after a certain period of inactivity.
In several of the presented cases, burns were caused by a deviation from standard operating procedures, such as the case in which a Foley catheter was placed after the start of surgery, or the case in which a grounding pad was not properly placed. These types of never events can be avoided by implementing surgical checklists while these devices and substances are in use. In 2022, The Joint Commission report showed that a lack of leadership and communication is a main contributor to sentinel events in healthcare. [4] Taking this into account, a study described how Johns Hopkins Hospital uses operating room briefings to prompt additional dialogue between the anesthesia care team, the nursing staff, and the surgical team to confirm the correct patient, procedure, and operative site. [22] These briefings should also include verification of the proper settings, operation, and use of surgical instruments and cauterizers to address burn never events. To reduce surgical error, California expert reviewers also proposed policy adherence monitoring, revision of existing policy, and policy education. [17].
Several cases involved either a defect in equipment, improper training of personnel, or improper use of equipment or chemicals. To prevent these never events, forcing functions on equipment and proper training of personnel is critical. For example, in the case where the patient was burned by the defective lamp, a forcing function could have been employed so that the lamp would not turn on at all.
One of the limitations of these databases is not encompassing the cases which do not reach the litigation and out-of-court settlements, which could potentially lead to underestimation of malpractice cases. The Bureau of Justice Statistics, the statistical agency of the U.S. Department of Justice, conducted a study evaluating medical malpractice insurance claims in seven states between 2000–2004. The study found that about 95% of medical malpractice insurance claims settled prior to trial. Additionally, claims that settled prior to trial saw median insurance payouts at least 2.5 times smaller compared to payouts for claims that reached a trial decision. Several reasons are present for why injured patients do not report such cases. One of the reasons could be due to the lack of resources to litigate a medical malpractice lawsuit. Medical malpractice lawsuits are usually fact intensive, require expensive experts to opine on the proper standards of care or procedures, and can be lengthy depending on the complexity of the injury and circumstances. Physicians and hospitals often have significantly more resources than patients and patients may be intimidated from suing or feel that their injury isn’t worth the expense or emotional stress that comes with litigation. When patients lack resources to fund a medical malpractice lawsuit on their own, a law firm may take on the lawsuit under a contingency fee agreement, meaning that the law firm advances the costs of litigation on behalf of the client but takes a percentage of the final monetary recovery ranging from 30–40%, if one is obtained. This allows patients who normally may not be able to afford the costs of litigation to pursue their medical malpractice claims. However, the law firm must also consider the economics of the lawsuit before agreeing to a contingency fee agreement. Some states have laws that cap the amount of monetary damages a plaintiff can receive in a medical malpractice case, which is another factor to consider when contemplating whether filing a lawsuit will be worthwhile. Furthermore, some states require by law that the injured patient give advance notice to the physician or hospital that they are planning to file a lawsuit. This pre-lawsuit notice lasts for a certain period of time before the lawsuit can be legally filed and typically must identify the allegations for the contemplated lawsuit, identify potential defendants, state the relief sought by the patient, and provide sufficient time for the potential defendant to cure the problem. The physician or hospital may take this opportunity to put their malpractice insurer on notice, investigate the issue, and attempt to negotiate a settlement with the patient before the lawsuit can be filed. Additionally, the frequency of cases settling before a lawsuit is even filed is impossible to determine as the agreements are private and often confidential, which prohibits the patient from discussion the details of the alleged malpractice publicly.
Another limitation of the Westlaw and LexisNexis is that these databases are public, and rules for public record disclosure differ by jurisdiction, which may have an impact on the cases that are eventually included in these databases. [23] Furthermore, the lack of a standardized database reporting format meant that some cases provided detailed information whereas other cases had to be excluded due to insufficient information and inability to determine if a case was relevant to this study despite containing the relevant search terms.
5. Conclusion
While never events are rare overall, never events causing burn injury in plastic surgery are ultimately caused by human error or neglect. The use of overheated surgical instruments and misuse of cauterizing devices should be the focus for improving patient safety to reduce the risk of medical malpractice during surgical procedures. Forcing functions and additional safeguards should be considered to minimize the risk of costly litigation and unnecessary severe harm to patients.
Footnotes
CRediT authorship contribution statement
All authors equally contributed to the manuscript preparation and revisions.
All authors were involved in reviewing and analyzing data, writing manuscript and revisions.
Conflict of Interest
None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript. No funding was received to assist with preparation of this manuscript.
REFERENCES
- [1].Adetayo OA, Salcedo SE, Biskup NI, Gupta SC. The battle of words and the reality of never events in breast reconstruction: incidence, risk factors predictive of occurrence, and economic cost analysis. Plast Reconstr Surg 2012;130(1):23–9. 10.1097/PRS.0b013e3182547b74 [DOI] [PubMed] [Google Scholar]
- [2].N.H.S. England Patient Safety Domain. Revised Never Events Policy and Framework. Published online March 27, 2015. Accessed May 2, 2023. 〈https://www.england.nhs.uk/wp-content/uploads/2015/04/never-evnts-pol-framwrk-apr.pdf〉. [Google Scholar]
- [3].Mehtsun WT, Ibrahim AM, Diener-West M, Pronovost PJ, Makary MA. Surgical never events in the United States. Surgery 2013;153(4):465–72. 10.1016/j.surg.2012.10.005 [DOI] [PubMed] [Google Scholar]
- [4].The Joint Commission. Sentinel Event Data 2022 Annual Review. Accessed May 3, 2023. 〈https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/03162023_sentinel-event-_annual-review_final.pdf〉. [Google Scholar]
- [5].Centers for Medicare & Medicaid Services. CMS Improves Patient Safety for Medicaid by Addressing Never Events. Published online August 4, 2008. Accessed May 3, 2023. 〈https://www.cms.gov/newsroom/fact-sheets/cms-improves-patient-safety-medicare-and-medicaid-addressing-never-events〉. [Google Scholar]
- [6].Boyd JB, Moon HK, Martin S, Mastrogiovanni DB. Plastic surgery and the malpractice industry. Plast Reconstr Surg 2021;147(1):239–47. 10.1097/PRS.0000000000007497 [DOI] [PubMed] [Google Scholar]
- [7].Gong JH, Kim DD, Mehrzad R. Medical malpractice litigations after hair restoration surgery in the United States. J Plast Reconstr Aesthetic Surg JPRAS 2022;75(8):2831–70. 10.1016/j.bjps.2022.06.097 [DOI] [PubMed] [Google Scholar]
- [8].Sarmiento S, Wen C, Cheah MA, Lee S, Rosson GD. Malpractice litigation in plastic surgery: can we identify patterns? Aesthet Surg J 2020;40(6):NP394–401. 10.1093/asj/sjz258 [DOI] [PubMed] [Google Scholar]
- [9].Mozeika AM, Sachdev D, Asri R, Farber N, Paskhover B. Sociological and Medical Factors Influence Outcomes in Facial Trauma Malpractice. J Oral Maxillofac Surg J Am Assoc Oral Maxillofac Surg 2019;77(5):1042.e1–1042.e10. 10.1016/j.joms.2019.01.005 [DOI] [PubMed] [Google Scholar]
- [10].Therattil PJ, Chung S, Sood A, Granick MS, Lee ES. An analysis of malpractice litigation and expert witnesses in plastic surgery. Eplasty 2017;17:e30. [PMC free article] [PubMed] [Google Scholar]
- [11].Paik AM, Mady LJ, Sood A, Eloy JA, Lee ES. A look inside the courtroom: an analysis of 292 cosmetic breast surgery medical malpractice cases. Aesthet Surg J 2014;34(1):79–86. [DOI] [PubMed] [Google Scholar]
- [12].Svider PF, Eloy JA, Folbe AJ, Carron MA, Zuliani GF, Shkoukani MA. Craniofacial surgery and adverse outcomes: an inquiry into medical negligence. Ann Otol Rhinol Laryngol 2015;124(7):515–22. 10.1177/0003489414567937 [DOI] [PubMed] [Google Scholar]
- [13].Sasor SE, Chung KC. Litigation in hand surgery: a 30-year review. Plast Reconstr Surg 2020;146(4):430e–8e. 10.1097/PRS.0000000000007157 [DOI] [PubMed] [Google Scholar]
- [14].About | LexisNexis. Accessed December 23, 2022. 〈https://www.lexisnexis.com/en-us/about-us/about-us.page〉. [Google Scholar]
- [15].Moppett IK, Moppett SH. The risk of surgical never events. Br J Hosp Med Lond Engl 2005 2016;77(2):64–5. 10.12968/hmed.2016.77.2.64 [DOI] [PubMed] [Google Scholar]
- [16].Neily J, Mills PD, Eldridge N, et al. Incorrect surgical procedures within and outside of the operating room: a follow-up report. Arch Surg Chic Ill 1960 2011;146(11):1235–9. 10.1001/archsurg.2011.171 [DOI] [PubMed] [Google Scholar]
- [17].Cohen AJ, Lui H, Zheng M, et al. Rates of serious surgical errors in California and plans to prevent recurrence. JAMA Netw Open 2021;4(5):e217058. 10.1001/jamanetworkopen.2021.7058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Culp WC, Kimbrough BA, Luna S, Maguddayao AJ. Mitigating operating room fires: development of a carbon dioxide fire prevention device. Anesth Analg 2014;118(4):772–5. 10.1213/ANE.0000000000000133 [DOI] [PubMed] [Google Scholar]
- [19].Jones TS, Black IH, Robinson TN, Jones EL. Operating Room Fires. Anesthesiology 2019;130(3):492–501. 10.1097/ALN.0000000000002598 [DOI] [PubMed] [Google Scholar]
- [20].Collins SJ, Newhouse R, Porter J, Talsma A. Effectiveness of the surgical safety checklist in correcting errors: a literature review applying reason’s swiss cheese model. AORN J 2014;100(1):65. 10.1016/j.aorn.2013.07.024 [DOI] [PubMed] [Google Scholar]
- [21].DeGirolamo KM, Courtemanche DJ, Hill WD, Kennedy A, Skarsgard ED. Use of safety scalpels and other safety practices to reduce sharps injury in the operating room: what is the evidence? Can J Surg J Can Chir 2013;56(4):263–9. 10.1503/cjs.003812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Michaels RK, Makary MA, Dahab Y, et al. Achieving the national quality forum’s “never events”: prevention of wrong site, wrong procedure, and wrong patient operations. Ann Surg 2007;245(4):526–32. 10.1097/01.sla.0000251573.52463.d2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kandinov A, Mutchnick S, Nangia V, et al. Analysis of factors associated with rhytidectomy malpractice litigation cases. JAMA Facial Plast Surg 2017;19(4):255–9. 10.1001/jamafacial.2016.1782 [DOI] [PMC free article] [PubMed] [Google Scholar]


