Abstract
Purpose
To examine the association of sociodemographic and health-related determinants with social isolation in relation to family and friends in the oldest-old.
Methods
Database was the multi-center prospective AgeCoDe/AgeQualiDe cohort study assessed at follow-up wave 5 (N = 1148; mean age 86.6 years (SD 3.0); 67% female). Social isolation was assessed using the short form of the Lubben Social Network Scale (LSNS-6). The LSNS-6 contains two sets of items establishing psychometrically separable subscales for isolation from family and friends (ranges 0–15 points), with lower scores indicating higher isolation. Cross-sectional linear (OLS) regression analyses were used to examine multivariate associations of sociodemographic and health-related determinants with social isolation from family and friends.
Results
Overall, n = 395 participants (34.6%) were considered socially isolated. On average, isolation was higher from friends (mean 6.0, SD 3.8) than from family (mean 8.0, SD 3.5). Regression results revealed that in relation to family, males were more socially isolated than females (β = − 0.68, 95% CI − 1.08, − 0.28). Concerning friends, increased age led to more isolation (β = − 0.12, 95% CI − 0.19, − 0.05) and functional activities of daily living to less isolation (β = 0.36, 95% CI 0.09, 0.64). Independent of the social context, depression severity was associated with more social isolation, whereas cognitive functioning was associated with less social isolation.
Conclusions
Different determinants unequally affect social isolation in relation to family and friends. The context of the social network should be incorporated more strongly regarding the detection and prevention of social isolation to sustain mental and physical health.
Keywords: Social isolation, Social network, Family, Friends, Cohort study, Oldest-old, Risk factor, Prevalence
Introduction
Increasing life expectancy worldwide accounts for a steadily increasing proportion of older people in the demographic composition of Western societies. In Germany, the percentage of people over 80 years of age is estimated to triple between 2040 and 2060, as compared to 2008 [1]. Therefore, it is of crucial importance to pay attention especially to the concerns, challenges and needs of the oldest-old.
Social isolation is one of the major challenges for older adults due to decreasing economic and social resources, impaired mobility and the death of spouses and friends, all leading to a reduction in older people’s network size [2]. Socially isolated older individuals in particular face a variety of challenges that can adversely affect their mental and physical health [3]. A wide range of concomitant diseases are associated with social isolation, including depression [4], cardiovascular diseases [5], and cognitive decline [6], as well as a higher risk of chronic illnesses [7], suicidal behaviour [8] and premature mortality [9]. It has been argued that social isolation as a risk factor for mortality is comparable to the deleterious effects of smoking and greater than the risk of obesity [9].
Research on social integration as the opposite of social isolation corroborates these findings, indicating that positive social ties and support have beneficial influences on mental and physical health among older adults. For example, social relationships and support are associated with greater life satisfaction and self-esteem [10] and prevent depression after a loss experience and bereavement [11]. The significance of social integration has become even more important as a result of the COVID-19 pandemic [12].
Two main social network types and sources of integration among older adults are family and friends [13]. The social networks of family and friends vary in their structural and functional characteristics, quality and quantity [14]. The quantity of a social network displays aspects such as the size of social network and the frequency of contacts, the quality includes closeness, satisfaction and expectations of the relationship [15]. Friendships are made voluntarily, usually based on common interests and life stages, and they are likely to include people of the same age and provide companionship. In contrast, family relationships are obligatory, based on family history, and might be maintained partly because of cultural norms and formal obligations [16].
Multiple studies state that the quality of a social network is more strongly correlated with social isolation than the quantity [10, 14, 17]. A good quality of relationships was associated with well-being and physical health, whereas the quantity of relationships had little influence on physical and psychological health [14].
Nevertheless, the quantity of social contact with friends was more closely related to well-being than the quantity of contact with adult children [10]. This is consistent with evidence suggesting that friendships may contribute more to well-being than family relationships [14]. The absence of family in the context of friends was less detrimental than the absence of friends in the context of family. For instance, the friend’s network seems to be more beneficial than the family network in terms of physical but not mental health [18].
In sum, there is evidence that the social network of friends and family may vary among older adults and that social isolation resulting from any of these sources may have different effects on physical and mental health. At the same time, prevalence figures on social isolation in the particularly vulnerable group of oldest-olds (80+ years) are lacking [19], specifically with regard to the differentiation of isolation from family and friends. In addition, there is a lack of knowledge about context-specific determinants of social isolation, which are fundamental to prevention efforts to maintain physical and mental health among older adults. In this study, we attempt to address these gaps by (1) estimating the prevalence of social isolation from family and friends in a group of older adults, and (2) assessing the impact of sociodemographic and health-related determinants on social isolation from family and friends in this subgroup.
Methods
Study design and sample
Data analysis is based on general practitioner (GP) patients who participated in the longitudinal, prospective studies German study on ageing, cognition and dementia in primary care patients (AgeCoDe) and Needs, health service use, costs and health-related quality of life in a large sample of oldest-old primary care patients (85+) (AgeQualiDe). The AgeQualiDe study is a continuation (follow-ups 7–9) and extension of the AgeCoDe study.
Patients were recruited in six cities throughout Germany including Hamburg, Bonn, Düsseldorf, Leipzig, Mannheim and Munich via general practitioners. Selection requirements for participation in the baseline study were 75+ years of age, no dementia according to the GP’s diagnosis and at least one contact with the GP during the last 12 months. In Germany, approximately 94% of people above 65 years regularly seek medical advice from their GP [20]. Therefore, participants can be considered representative of the majority of community-dwelling older individuals. Following the recruitment, participants were contacted by the study centers and asked to complete the baseline assessment.
Data collection of the AgeCoDe/AgeQualiDe study took place between 2003 and 2017 including nine follow-up assessments that were scheduled approximately every 18 months. This study includes data from follow-up wave 5 only, conducted in 2011, since data on social isolation was not assessed in earlier waves. Data collection took place in the participants’ homes by trained research assistants.
The AgeCoDe/AgeQualiDe Study was conducted in accordance with the ethical standards embodied in the Declaration of Helsinki of 1975 and was approved by the local ethics committees of the participating study sites in Germany.
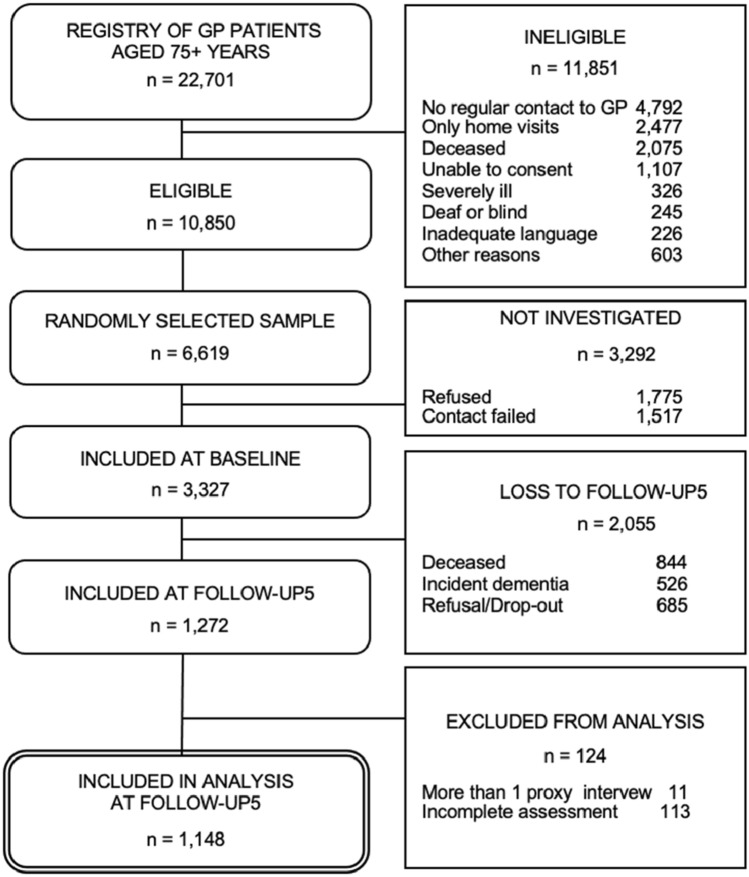
A flowchart of sample selection is shown in Fig. 1. A total of N = 3327 participants gave written informed consent and were included in the baseline sample (Fig. 1). Up to follow-up wave 5, n = 844 (25.4%) participants deceased, n = 526 (15.8%) had developed dementia and n = 685 (20.6%) refused or dropped-out due to other reasons. Of the remaining n = 1272 participants included in follow-up 5, n = 124 (9.7%) had to be excluded from the analyses due to incomplete assessments or because they had more than one proxy interview in the previous follow-ups. The resulting analytical sample consisted of n = 1148 participants.
Fig. 1.
Flowchart of analytical sample at baseline
Assessments
Social isolation
Social isolation was assessed using the Lubben Social Network Scale 6 (LSNS-6), which examines the social network and the quality of social support of older individuals. The LSNS-6 is a statistically well evaluated six-item, self-report questionnaire [21]. The measurement displays frequency, size, and closeness of contacts in the respondent’s social network. Each LSNS-6 question is scored on a 0–5 Likert scale, the total score is an equally weighted sum of the six items, with a total score between 0 and 30. A cut-off score of 12 points was established for the LSNS-6, with respondents scoring lower being defined as socially isolated [21, 22]. The LSNS-6 is set up in two times three questions, in which each set of three questions form two subscales for social isolation from family (e.g., “How many relatives do you see or hear from at least once a month?”) and friends (e.g., “How many friends do you feel close to such that you could call on them for help?”). The two subscales of family and friends are statistically well justified with high levels of internal consistency and stable factor structures [21]. Cut-off scores for the two subscales family and friends were validated at score 6 to best discriminate between isolated and not isolated people; respondents with a score of less than 6 points are defined as socially isolated with regard to the respective context.
In an explorative factor analysis in our study, the two-dimensional structure of the LSNS-6 with the family and friends subscales was confirmed. The eigenvalues suggested strong principal components. Initial eigenvalues indicated that the first two factors explained 38.8% and 33.2% of the variance, respectively. Factor 1 represented the LSNS-6 family subscale. These items had primary factor loadings ranging from 0.87 to 0.88. Factor 2 represented the LSNS-6 friend’s subscale. These items had primary factor loadings ranging from 0.79 to 0.82. The item rest correlation for the two subscales family and friends ranged between 0.71 and 0.73 and 0.54 and 0.58, respectively. The resulting overall Cronbachs alpha for the family and friends subscales was α = 0.85 and α = 0.75, respectively.
Determinants
To cover potential risk factors of social isolation, a number of determinants were collected including sociodemographics, somatic and psychological aspects. Data on these determinants was provided in a standardized interview and by patient’s GPs.
Sociodemographic determinants included age, gender, marital status (married vs. not married/widowed/divorced), living situation (living alone vs. not alone), children (yes vs. no) and level of education. To constitute the determinant of education, the CASMIN classification with the educational level of low, medium or high was chosen [23]. Due to sparsely populated cells, medium and high education were collapsed into one category.
Furthermore, a number of health-related determinants were considered as risk factors of social isolation. First, impairments in vision, hearing and mobility were assessed as self-reported ratings and categorized as indicator variables (impaired vs. not impaired). To collect the data on somatic comorbidities, the general physician completed a questionnaire regarding the health of the participants. The following somatic comorbidities were requested: cardiac diseases, insult, hypertension, kidney insufficiency, diabetes mellitus, atherosclerosis, Parkinson's disease and illnesses of the thyroid gland. For simplicity, we used this information to generate a determinant indicating the number of somatic comorbidities in a patient (range 0–8). In addition, we used the Mini-Mental State Examination (MMSE) test to screen for cognitive functioning [24]. The MMSE results in a sum score ranging from 0 to 30, with higher scores indicating better cognitive performance. Moreover, we assessed depressive symptoms with the Geriatric depression scale (GDS), a self-report assessment consisting in its short form of 15 items (GDS-15). The GDS-15 is a reliable and valid screening instrument for detecting depressive symptom severity in elderly people, as well being sensitive to depression among elderly people suffering from mild to moderate dementia and physical illness [25].
Finally, difficulties in instrumental activities of daily living (IADL) were assessed via the 8-item Lawton and Brody IADL scale [26]. The analyses included only data on the five items common to both males and females, excluding the frequently female-associated items of food preparation, housekeeping and laundry. The resulting total score ranged from 0 to 5 points, with higher scores indicating less difficulties in activities of daily living.
Statistical analysis
Sociodemographic and health-related determinants as well as figures on the prevalence and distribution of social isolation are reported as means with standard deviation or frequencies with percentages, as appropriate. Gender differences in social isolation were tested using Pearson chi-square tests for prevalence variables and t tests for LSNS-6 scores. Multivariate linear (OLS) regression models were conducted to test the association of sociodemographic and health-related determinants with social isolation related to family and friends, as measured by LSNS-6 subscales. The assumptions for the linear model were tested and confirmed psychometrically.
All statistical analyses were performed using STATA 16.0 SE (Stata Corp LP, College Station, TX) and used an alpha level of 0.05 (two-tailed) for statistical significance. The clustered design of the study was accounted for by adjusting the standard errors in the regression models using the practice ID as a cluster variable.
Results
Sample characteristics
Sample characteristics are shown in Table 1. The mean age of the analytical sample of 1,148 participants was 86.6 years (SD 3.0). Two in three participants were female (67.3%). The majority of participants were unmarried or widowed, was living alone, had children and low school education. With regard to physical impairments, the majority of participants reported walking difficulties (60.5%), almost half (48.8%) had a hearing impairment and a quarter (26.3%) had visual impairment. On average, participants had normal cognition (MMSE mean score 27.8, SD 1.9), hardly had any deficits in activities of daily living (IADL mean score 4.2, SD 1.1) and no signs of depression (GDS-15 mean score 2.6, SD 2.5). Moreover, participants reported on average 2–3 somatic comorbidities, with arterial hypertension (86.0%) and cardiac diseases (55.4%) being reported most frequently.
Table 1.
Distribution of sociodemographic and health-related determinants
| Total | |
|---|---|
| N = 1148 | |
| Sociodemographic | |
| Gender, n (%) | |
| Male | 376 (33.7) |
| Age, mean (SD) | 86.6 (3.0) |
| Marital status, n (%) | |
| Unmarried/widowed | 806 (70.2) |
| Married | 342 (29.8) |
| Level of education, n (%) | |
| Low | 643 (56.0) |
| Medium/high | 505 (44.0) |
| Living situation, n (%) | |
| Living alone | 638 (55.6) |
| Living with spouse/relatives | 510 (44.4) |
| Having children, n (%) | 931 (81.1) |
| Health-related | |
| Difficulties walking, n (%) | 694 (60.5) |
| Sensory impairment, n (%) | |
| Vision | 302 (26.3) |
| Hearing | 560 (48.8) |
| MMSE, mean (SD) | 27.8 (1.9) |
| IADL, mean (SD) | 4.2 (1.0) |
| Depressive symptoms, mean (SD) | 2.6 (2.5) |
| Somatic comorbidities, n (%) | 2.4 (1.3) |
SD standard deviation, MMSE mini-mental state examination, IADL instrumental activities of daily living
Prevalence and distribution of social isolation
Overall, one in three participants was socially isolated (34.6%). Participants reported more frequent isolation from friends (44.3%) than from their family (21.8%). Although females had significantly lower mean scores than males on the LSNS-6 total and the friend’s subscale, there were no gender differences in these prevalence figures of social isolation (Table 2).
Table 2.
Prevalence and distribution of social isolation (total, family, friends) according to LSNS-6
| Total | Gender | |||||
|---|---|---|---|---|---|---|
| N = 1.148 | Female (n = 772) | Male (n = 376) | ||||
| n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | |
| Prevalence | ||||||
| Total, cut-off < 12 | 397 (34.6) | 277 (35.9) | 120 (31.9) | |||
| Friends, cut-off < 6 | 508 (44.3) | 345 (44.7) | 163 (43.4) | |||
| Family, cut-off < 6 | 250 (21.8) | 185 (24.0) | 65 (17.3) | |||
| Distribution | ||||||
| Total score | 14.0 (5.58) | 13.7 (5.4)* | 14.6 (5.9) | |||
| Friends subscore | 6.0 (3.8) | 7.8 (3.6)* | 8.3 (3.3) | |||
| Family subscore | 8.0 (3.5) | 5.9 (3.7) | 6.2 (4.0) | |||
T test or Chi2 test for comparison between females and males
SD standard deviation, CI confidence interval
*p < 0.05, **p < 0.01 ***p < 0.001
Determinants of social isolation related to family
Analysis of determinants of social isolation related to family showed that males were significantly more socially isolated than females (β = − 0.68, 95% CI − 1.08, − 0.28; Table 3). In comparison, participants who reported being married were less socially isolated than those who reported being widowed or divorced (β = 0.96, 95% CI 0.22, 1.70). Moreover, lower education (β = 0.42, 95% CI 0.08, 0.76) and having children (β = 3.21, 95% CI 2.64, 3.78) were depicted as protective factors for social isolation related to the family. With regard to health-related determinants, impairment in walking had a significant impact on social isolation (β = − 0.42, 95% CI − 0.84, − 0.01), whereas better cognitive functioning was a protective factor against social isolation related to the family (β = 0.11, 95% CI 0.01, 0.22). Finally, depressive symptom severity was significantly associated with more social isolation in the family context (β = − 0.28, 95% CI − 0.36, − 0.20).
Table 3.
Linear Regression of social isolation in the context of family and friends
| Family | Friends | |||
|---|---|---|---|---|
| N = 1148 | N = 1148 | |||
| B | 95% CI | B | 95% Cl | |
| Sociodemographic | ||||
| Gender | ||||
| Male | − 0.68*** | [− 1.08, − 0.28] | − 0.09 | [− 0.57, 0.39] |
| Age | − 0.01 | [− 0.08, 0.06] | − 0.12** | [− 0.19, − 0.05] |
| Marital status | ||||
| Married | 0.96* | [0.22, 1.70] | 0.54 | [− 0.19, 1.26] |
| Level of education | ||||
| Low | 0.42* | [0.08, 0.76] | − 0.51* | [− 0.93, − 0.09] |
| Living situation | ||||
| Living alone | − 0.56 | [− 1.15, 0.03] | 0.53 | [− 0.03, 1.09] |
| Having children | 3.21*** | [2.64, 3.78] | − 0.08 | [− 0.69, 0.53] |
| Health-related | ||||
| Difficulties walking | − 0.42* | [− 0.84, − 0.01] | 0.27 | [− 0.24, 0.78] |
| Sensory impairment | ||||
| Vision | − 0.32 | [− 0.70, 0.06] | − 0.04 | [− 0.51, 0.44] |
| Hearing | 0.01 | [− 0.30, 0.31] | 0.22 | [− 0.22, 0.67] |
| MMSE | 0.11* | [0.00, 0.22] | 0.22*** | [0.11, 0.34] |
| IADL | − 0.20 | [− 0.40, 0.00] | 0.36** | [0.09, 0.64] |
| Depressive symptoms | − 0.28*** | [− 0.36, − 0.20] | − 0.30*** | [− 0.39, − 0.20] |
| Somatic comorbidities | 0.01 | [− 0.11, 0.13] | − 0.07 | [− 0.23, 0.08] |
| R2 | 0.24 | 0.12 | ||
B unstandardized regression coefficient, CI confidence interval, MMSE Mini-Mental State Examination, IADL instrumental activities of daily living
Determinants of social isolation related to friends
Analyses of determinants of social isolation related to friends yielded somewhat different results. First, it was found that social isolation from friends was associated with higher age (β = − 0.12, 95% CI − 0.19, − 0.05) and lower education (β = − 0.51, 95% CI − 0.93, − 0.09). With regard to health-related determinants, results further indicated that less difficulties in handling daily activities were associated with less social isolation from friends (β = 0.36, 95% CI 0.09, 0.64). In addition, similar to the family context, cognitive functioning (β = 0.22, 95% CI 0.11, 0.34) proved protective against social isolation in relation to friends, while depressive symptom severity appeared to be associated with more social isolation (β = − 0.30, 95% CI − 0.39, − 0.20; Table 3).
Discussion
Main findings
This study aimed to estimate the prevalence of social isolation in the oldest-old as well as to examine the impact of multiple determinants on social isolation in relation to family and friends. We found that about one in three adults over 80, regardless of gender, were socially isolated, with isolation from friends being reported twice as often as isolation related to the family.
We also found that differences in the social context of isolation were predominantly determined by demographics, while health-related determinants were largely associated with social isolation in general, regardless of its context.
Our study adds significantly to the evidence for the high prevalence of social isolation in old age by expanding the age group studied to include the oldest-old. In previous population-based studies, the prevalence of social isolation in Germany was assessed only up to the age of 79 years, ranging between 12–13% before the COVID-19 pandemic [27, 19]. In our sample of 80+ year-olds, the prevalence of social isolation was more than twice as high at 34.6%. When distinguishing by context, we further found considerable differences in the prevalence of social isolation in relation to friends (44.3%) and family (21.8%). This underlines that social isolation in old age is a serious concern and there is a need to establish context-specific interventions to reduce social isolation especially in relation to friends in order to maintain health long-term.
We found several differences in the severity of social isolation from family and friends related to sociodemographic characteristics. First, in the multivariate analysis, male gender was associated with social isolation in the family, but not in friends. This is consistent with a study indicating that males are significantly more socially isolated in the family than in friends [28]. In general, the social networks of males and females may differ in that females have a larger social network and tend to be more satisfied with their network than males. Moreover, with increasing age the size of the social network diminishes substantially [13], and this was more prone in males than in females [29]. The gender difference may affect the consequences of social isolation as well. According to a population-based 18-year follow-up study from the US, social isolation has a greater impact on chronic illnesses and mortality in males than in females, possibly due to a heightened inflammatory response to the disruption of social ties [30]. Altogether, older males with their smaller social network seem more vulnerable to social isolation and its consequences, especially when related to the family.
Although age is regarded as one of the main risk factors for social isolation [31], our results indicated that this is only true in relation to friends. This could indicate changes and transitions in the social network of older adults from friends to family as they grow older. This is corroborated by the findings of Wrzus et al. [32] showing a decrease in the network size of friends, whereas the family network size remains stable. However, conflicting findings [28] show that age as a risk factor for social isolation is more complex than previously thought. Further research considering the social context of isolation among older adults is needed to unravel the role of aging in older adults’ family and friends networks.
Marital status is often considered in research on social isolation, as it provides a first insight into the everyday social interactions of respondents. The protective effect of marriage on family-related social isolation that we found is not surprising and has been confirmed more generally in several studies [33]. Likewise, having children also protected against isolation in the family context, certainly due to the emotional, physical, and financial support that (adult) children can provide [34]. What is interesting, though, is that marriage did not play a substantial role in social isolation from friends. Moreover, living alone was not associated with social isolation, neither related to family nor to friends. Despite possible health restrictions, married or cohabitating people seem to focus no less on friends (in favour to their own partnerships) than people who are widowed or live alone do.
Another interesting, yet contrastive finding for social isolation related to family and friends was found with regard to educational attainment. A low level of education was protective against social isolation related to the family, whereas it was a risk factor for social isolation related to friends. This complements previous studies suggesting that low education is associated with higher levels of social isolation in general [35]. It may be that the family environment is generally more inclusive and tolerant, while education promotes protection against isolation from friends, particularly in older age.
We also found evidence for several health-related determinants of social isolation, with the results often being similar in the family and friends' contexts. First, cognitive functioning was associated with lower social isolation related to both family and friends. This complies with other studies showing that dementia impairs communication and social interactions, eventually leading to social isolation [27]. In addition, reverse causation is also conceivable: socially isolated individuals have less social interaction and therefore receive less cognitive stimulation, ultimately resulting in cognitive decline [36]. Taken together, the results underline the importance of the association between cognition and social isolation, which in our study appeared to be even more pronounced in the context of friends than in the family.
Next, depressive symptoms were a strong determinant of social isolation both from family and friends, lining up with more general studies on depression and social isolation [4]. Depression is not only a frequent result of declining health and functional impairment in older adults [37] but also an important correlate of loneliness and social isolation [4]. The relationship between depression and social isolation is complex; some claim it is sequential [4], some say it is likely to be reciprocal [38].
Our study further revealed an association of difficulties in instrumental activities of daily living (IADL) with social isolation from friends. Restrictions in IADL appear to pose a serious obstacle to social contacting and participation outside the family. Interestingly, another study [28] found the opposite, reporting that impairments in IADL were associated with less isolation from friends. The authors assumed that an increased need for care entails more social interactions with caregivers, which ultimately leads to more friendships. However, participants in our study were on average 20 years older and more often widowed/living alone than in the mentioned study. It is very likely that the particular role of difficulties in daily care routines substantially affects the social network with increasing age.
Contrary to intuition, walking difficulties were another independent predictor of social isolation in the family but not in the friend’s context. The inability to participate in family social gatherings due to physical disabilities may be associated with a kind of (unwanted) self-isolation. In contrast, activities in the friends’ context could be planned better and more specifically despite existing physical disabilities.
Unlike other studies looking at sensory impairments and somatic comorbidities [39], we did not find significant associations with social isolation in relation to family or friends. One explanation could be that we did not consider the severity of disabilities in our study; a more severe and clinically relevant condition is more likely to be associated with social isolation, regardless of context. In addition, the selection of examined diseases may have been too small, since various somatic comorbidities undoubtedly differ in their degree of impairment and limitation. A broader range, including neurological and cancer diseases and information on the extent of medical control should be included in further research.
Limitations
Our study was not without limitations. First, data were collected prior to the Covid-19 pandemic. Due to social distancing, quarantine measures and decreasing social interaction, increasing levels of loneliness and social isolation were found among all age groups during the pandemic [40]. One study found a perceived isolation of even 59% in the age group between 18 and 70 years [41], almost five times as high as the mentioned range of 12–13% found prior to the COVID-19 pandemic [19, 27]. Changes in determinants, prevalence and patterns of social isolation post-pandemically remain unclear in this study. Second, an inherent selection bias in our analyses cannot be ruled out with certainty, as some participants could not be contacted, were excluded from the data due to lack of information, or declined participation in the beginning or during the follow-up studies. The analyses may particularly omit more severely ill cases since these participants either did not meet the inclusion criteria or have already dropped out in the first four waves of the cohort study. Third, data were drawn only from self-administered questionnaires, which is prone to reporting bias. Since social isolation is possibly attached to stigma, individuals may underreport social isolation and the prevalence may be underestimated. Our aim was to consider as many determinants of social isolation as possible, but the selection of determinants was limited to those chosen during the planning and conduction process of the study. There may be more determinants, such as income and demographic factors (e.g. metropolitan vs. non-metropolitan) [42], which have not yet been assessed. Finally, due to the cross-sectional design, our study cannot conclude causality. A longitudinal approach is required to depict developments in the social network of older people, e.g. after critical life events such as the loss of a partner or hospitalization.
Conclusion
Given the multitude of health implications, preventing social isolation in old age should be of paramount health and societal concern [43–45]. With a 35% prevalence of social isolation among people aged 80+, the urgency to address this issue is particularly evident. Due to demographic change and the long-term effects of the COVID-19 pandemic, the importance of the social integration of older people into society might increase even more in the future. Our study further provides evidence of contextual and independent factors influencing social isolation. Older males with low education, cognitive impairment and depressive symptoms are particularly at risk and should receive special attention in terms of prevention. Initiatives such as intergenerational programs, making communities more age-friendly, or facilitating access to services and public spaces for the elderly population could help prevent social isolation, improve quality of life and health in old age, and avert psychological and physical harm [44, 46].
Acknowledgements
We want to thank both all participating patients and their general practitioners for their good collaboration. We would like to thank all members of the AgeCoDe Study Group. Members of the AgeCoDe & AgeQualiDe study group: Principal Investigators1: Wolfgang Maier, Martin Scherer, Steffi G. Riedel-Heller, Heinz-Harald Abholz, Christian Brettschneider, Cadja Bachmann, Horst Bickel, Wolfgang Blank, Hendrik van den Bussche, Sandra Eifflaender-Gorfer, Marion Eisele, Annette Ernst, Angela Fuchs, André Hajek, Kathrin Heser, Frank Jessen, Hanna Kaduszkiewicz, Teresa Kaufeler, Mirjam Köhler, Hans- Helmut König, Alexander Koppara, Diana Lubisch, Tobias Luck, Dagmar Lühmann, Melanie Luppa, Tina Mallon, Manfred Mayer, Edelgard Mösch, Michael Pentzek, Jana Prokein, Susanne Röhr, Anna Schumacher, Janine Stein, Susanne Steinmann, Franziska Tebarth, Carolin van der Leeden, Michael Wagner, Klaus Weckbecker, Dagmar Weeg, Jochen Werle, Siegfried Weyerer, Birgitt Wiese, Steffen Wolfsgruber, Thomas Zimmermann. 1Hendrik van den Bussche (2002–2011).
Author contributions
KM and AP made substantial contributions to the conception and design of the study, did the data analyses and interpretation, and drafted and edited the manuscript. H-HK and SR-H designed the cohort study, contributed to data acquisition, drafting and revision of the manuscript and were responsible for supervision. FB, ML, HK, CvdL, AH, CB, KH, LK, JW, AF, DW, HB, MP, SW, BW, MW, WM, MS, revised and contributed to the manuscript. All authors approved the final version of the manuscript to be published.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study is part of the German Research Network on Dementia (KND), the German Research Network on Degenerative Dementia (KNDD; German Study on Aging, Cognition and Dementia in Primary Care Patients; AgeCoDe), and the Health Service Research Initiative (Study on Needs, health service use, costs and health-related quality of life in a large sample of oldest- old primary care patients (85+; AgeQualiDe)) and was funded by the German Federal Ministry of Education and Research (grants KND: 01GI0102, 01GI0420, 01GI0422, 01GI0423, 01GI0429, 01GI0431, 01GI0433, 01GI0434; grants KNDD: 01GI0710, 01GI0711, 01GI0712, 01GI0713, 01GI0714, 01GI0715, 01GI0716; grants Health Service Research Initiative: 01GY1322A, 01GY1322B, 01GY1322C, 01GY1322D, 01GY1322E, 01GY1322F, 01GY1322G). The study is published in affiliation with the study “Healthy Aging—gender specific trajectories into latest life (AgeDifferent.de)” that was funded by the German Federal Ministry of Education and Research (BMBF; grant numbers: 01GL1714A, 01GL1714B, 01GL1714C, 01GL1714D). This paper was further supported by a grant from the Hans and Ilse Breuer Foundation.
Availability of data and material
The data used and analyzed in this study can be made available to researchers on reasonable request to the correspondent author.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The AgeCoDe/AgeQualiDe Study was conducted in accordance with the ethical standards embodied in the Declaration of Helsinki of 1975 and was approved by the local ethics committees of the participating study sites in Germany.
Consent to participate
All participants provided informed consent prior to their inclusion in the study.
Consent of publication
Not applicable.
Footnotes
Katharina Isabelle Moormann and Alexander Pabst shared first authorship.
Hans-Helmut König and Steffi G. Riedel-Heller shared last authorship.
References
- 1.Federal Statistical Office (2019) Germany’s population by 2060. Results 14th Coord Popul Proj. 48. https://www.destatis.de/EN/Publications/Specialized/Population/GermanyPopulation2060_5124206159004.pdf?__blob=publicationFile
- 2.Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Heal Soc Care Community. 2017;25(3):799–812. doi: 10.1111/hsc.12311. [DOI] [PubMed] [Google Scholar]
- 3.Park C, Majeed A, Gill H, et al. The effect of loneliness on distinct health outcomes: a comprehensive review and meta-analysis. Psychiatry Res. 2020;294:113514. doi: 10.2139/ssrn.3463317. [DOI] [PubMed] [Google Scholar]
- 4.Van As BAL, Imbimbo E, Franceschi A, et al. The longitudinal association between loneliness and depressive symptoms in the elderly: a systematic review. Int Psychogeriatr. 2021 doi: 10.1017/S1041610221000399. [DOI] [PubMed] [Google Scholar]
- 5.Valtorta NK, Kanaan M, Gilbody S, et al. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Röhr S, Löbner M, Gühne U, et al. Changes in social network size are associated with cognitive changes in the oldest-old. Front Psychiatry. 2020;11(May):1–10. doi: 10.3389/fpsyt.2020.00330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cantarero-Prieto D, Pascual-Sáez M, Blázquez-Fernández C. Social isolation and multiple chronic diseases after age 50: a European macro-regional analysis. PLoS ONE. 2018;13(10):1–12. doi: 10.1371/journal.pone.0205062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClelland H, Evans JJ, Nowland R, et al. Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta-analysis of prospective studies. J Affect Disord. 2020;274:880–896. doi: 10.1016/j.jad.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. 2000;15(2):187–224. doi: 10.1037/0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- 11.Förster F, Stein J, Löbner M, et al. Loss experiences in old age and their impact on the social network and depression—results of the Leipzig Longitudinal Study of the Aged (LEILA 75+) J Affect Disord. 2018;241:94–102. doi: 10.1016/j.jad.2018.07.070. [DOI] [PubMed] [Google Scholar]
- 12.Riedel-Heller SG. Social integration and health. Psychiatr Prax. 2022;49(2):64–66. doi: 10.1055/a-1736-4190. [DOI] [PubMed] [Google Scholar]
- 13.Harasemiw O, Newall N, Shooshtari S, et al. From social integration to social isolation: the relationship between social network types and perceived availability of social support in a national sample of older Canadians. Res Aging. 2017;40(8):715–739. doi: 10.1071/AH080468. [DOI] [PubMed] [Google Scholar]
- 14.Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. J Gerontol Ser B Psychol Sci Soc Sci. 2006;61(1):25–32. doi: 10.1093/geronb/61.1.P25. [DOI] [PubMed] [Google Scholar]
- 15.Routasalo PE, Savikko N, Tilvis RS. Social contacts and their relationship to loneliness among aged people—a population-based study. Gerontology. 2006;52(3):181–187. doi: 10.1159/000091828. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen AW, Chatters LM, Taylor RJ, et al. Social support from family and friends and subjective well-being of older African Americans. J Happiness Stud. 2016;17(3):959–979. doi: 10.1007/s10902-015-9626-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryan AK, Willits FK. Family ties, physical health, and psychological well-being. J Aging Health. 2007;19(6):907–920. doi: 10.1177/0898264307308340. [DOI] [PubMed] [Google Scholar]
- 18.Li T, Zhang Y. Social network types and the health of older adults: Exploring reciprocal associations. Soc Sci Med. 2015;130:59–68. doi: 10.1016/j.socscimed.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Röhr S, Wittmann F, Engel C, et al. Social factors and the prevalence of social isolation in a population-based adult cohort. Soc Psychiatry Psychiatr Epidemiol. 2021 doi: 10.1007/s00127-021-02174-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prütz F, Rommel A. Inanspruchnahme ambulanter ärztlicher Versorgung in Deutschland. J Heal Monit. 2017;2(4):88–94. doi: 10.17886/RKI-GBE-2017-116. [DOI] [Google Scholar]
- 21.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the lubben social network scale among three European community-dwelling older adult populations. Gerontologist. 2006;46(4):503–513. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- 22.Rubinstein M. Implied binomial trees. J Financ. 1994;49(3):771–818. doi: 10.1111/j.1540-6261.1994.tb00079.x. [DOI] [Google Scholar]
- 23.Brauns H, Steinmann S. Educational reform in France, West-Germany and the United Kingdom: updating the CASMIN educational classification. ZUMA Nachrichten. 1999;23(44):7–44. [Google Scholar]
- 24.Folstein MF, Folstein SE, Mc Hugh PR. Mini-mental state: a practical method for grading the cognitive status of patients for clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS) Jerome. Clin Gerontol. 1986;5(1–2):165–173. [Google Scholar]
- 26.Lawton M, Brody E. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi: 10.1093/geront/9.3_Part_1.179. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez FS, Schroeter ML, Witte AV, et al. Could high mental demands at work offset the adverse association between social isolation and cognitive functioning? Results of the population-based LIFE-adult-study. Am J Geriatr Psychiatry. 2017;25(11):1258–1269. doi: 10.1016/j.jagp.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 28.Chatters LM, Taylor HO, Nicklett EJ, et al. Correlates of objective social isolation from family and friends among older adults. Healthcare. 2018;6(1):24. doi: 10.3390/healthcare6010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McLaughlin D, Vagenas D, Pachana NA, et al. Gender differences in social network size and satisfaction in adults in their 70s. J Health Psychol. 2010;15(5):671–679. doi: 10.1177/1359105310368177. [DOI] [PubMed] [Google Scholar]
- 30.Yang Claire Y, McClintock KM, Kozloski M, et al. Social isolation and adult mortality: the role of chronic inflammation and sex differences. J Heal Soc Behav. 2013;54(2):183–203. doi: 10.1177/0022146513485244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Key W, Culliney M. The oldest old and the risk of social exclusion. Soc Policy Soc. 2018;17(1):47–63. doi: 10.1017/S1474746416000518. [DOI] [Google Scholar]
- 32.Wrzus C, Hänel M, Wagner J, et al. Social network changes and life events across the life span: a meta-analysis. Psychol Bull. 2013;139(1):53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- 33.Victor CR, Yang K. The prevalence of loneliness among adults: a case study of the United Kingdom. J Psychol Interdiscip Appl. 2012;146:85–104. doi: 10.1080/00223980.2011.613875. [DOI] [PubMed] [Google Scholar]
- 34.Grenade L, Boldy D. Social isolation and loneliness among older people: Issues and future challenges in community and residential settings. Aust Heal Rev. 2008;32(3):468–478. doi: 10.1071/AH080468. [DOI] [PubMed] [Google Scholar]
- 35.Hawkley LC, Hughes ME, Waite LJ, et al. From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. J Gerontol B Psychol Sci Soc Sci. 2008;68(8):375–384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Evans IEM, Llewellyn DJ, Matthews FE, et al. Social isolation, cognitive reserve, and cognition in healthy older people. PLoS ONE. 2018;13(8):1–14. doi: 10.1371/journal.pone.0201008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maier A, Riedel-Heller SG, Pabst A, et al. Risk factors and protective factors of depression in older people 65+. A systematic review. PLoS ONE. 2021;16:1–38. doi: 10.1371/journal.pone.0251326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luanaigh CÓ, Lawlor BA. Loneliness and the health of older people. Int J Geriatr Psychiatry Sci. 2008;23(12):1213–1221. doi: 10.1002/gps.2054. [DOI] [PubMed] [Google Scholar]
- 39.Cohen-Mansfield J, Hazan H, Lerman Y, et al. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychoger. 2016;28(557):76. doi: 10.1017/S1041610215001532. [DOI] [PubMed] [Google Scholar]
- 40.Berger K, Riedel-Heller S, Pabst A, et al. Loneliness during the first wave of the SARS-CoV-2 pandemic—results of the German National Cohort (NAKO) Bundesgesundheitsblatt Gesundheitsforsch Gesundheitsschutz. 2021;64(9):1157–1164. doi: 10.1007/s00103-021-03393-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hajek A, König H-H. Prevalence and correlates of loneliness, perceived and objective social isolation during the COVID-19 pandemic. Evidence from a representative survey in Germany. Soc Psychiatry Psychiatr Epidemiol. 2022;57(10):1969–1978. doi: 10.1007/s00127-022-02295-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cudjoe TKM, Roth DL, Szanton SL, et al. The epidemiology of social isolation: national health and aging trends study. J Gerontol Ser B Psychol Sci Soc Sci. 2020;75(1):107–113. doi: 10.1093/geronb/gby037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Heal Soc Behav. 2009;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cotterell N, Buffel T, Phillipson C. Preventing social isolation in older people. Maturitas. 2018;113(April):80–84. doi: 10.1016/j.maturitas.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 45.Findlay RA. Interventions to reduce social isolation amongst older people: where is the evidence? Ageing Soc. 2003;23(5):647–658. doi: 10.1017/S0144686X03001296. [DOI] [Google Scholar]
- 46.Vitman A, Iecovich E, Alfasi N. Ageism and social integration of older adults in their neighborhoods in Israel. Gerontologist. 2014;54(2):177–189. doi: 10.1093/geront/gnt008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used and analyzed in this study can be made available to researchers on reasonable request to the correspondent author.