Abstract
Objective
Hospitalisation due to medication-related problems is a major health concern, particularly for those with pre-existing, or those at high risk of developing cardiovascular disease (CVD). Postdischarge medication reviews (PDMRs) may form a core component of reducing hospital readmissions due to medication-related problems. This study aimed to explore postdischarge CVD patients’ perspectives of, and experiences with, pharmacist-led medication management services. A secondary aim explored attitudes towards the availability of PDMRs.
Design
An interpretative qualitative study involving 16 semistructured interviews. Data were analysed using an inductive thematic approach.
Setting
Patients with CVD discharged to a community setting from the John Hunter Hospital, an 820-bed tertiary referral hospital based in New South Wales, Australia.
Participants
Patients with pre-existing or newly diagnosed CVD who were recently discharged from the hospital.
Results
A total of 16 interviews were conducted to reach thematic saturation. Nine participants (56%) were male. The mean age of participants was 57.5 (±13.2) years. Three emergent themes were identified: (1) poor medication understanding impacts transition from the hospital to home; (2) factors influencing medication concordance following discharge and (3) perceived benefits of routine PDMRs.
Conclusions
There is a clear need to further improve the quality use of medicines and health literacy of transition-of-care patients with CVD. Our findings indicate that the engagement of transition-of-care patients with CVD with pharmacist-led medication management services is minimal. Pharmacists are suitable to provide essential and tailored medication review services to patients with CVD as part of a multidisciplinary healthcare team. The implementation of routine, pharmacist-led PDMRs may be a feasible means of providing patients with access to health education following their transition from hospital back to community, improving their health literacy and reducing rehospitalisations due to medication-related issues.
Keywords: Pharmacists, Medication Reconciliation, Cardiovascular Disease, Hospital to Home Transition, Medication Review, CARDIOLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The strength of this study lies in the exploration of a heterogeneous sample of people with cardiovascular disease across their transition of care.
The inductive thematic analysis approach used in this study enables the richness of the qualitative data to be captured through a more flexible and reflective process.
Our study recruited patients who live outside major capital city area(s) of Australia, and therefore, may represent unique challenges due to their geographical location, often having poorer health outcomes than those living in major capital cities.
Potential reporting bias: responding participants may have had different experiences from non-responders, including access to primary care where differing models of care exist.
Introduction
Cardiovascular disease (CVD) is a leading cause of death and disability in Australia. In 2021 alone, CVD was the underlying cause of death in 42 700 individuals, representing 25% of all deaths. During this same year, coronary heart disease was the leading single cause of death in Australia, accounting for the deaths of 17 300 Australians, representing 10% of all deaths and 41% of CVD deaths.1 Internationally, medication-related issues are a common contributor to hospitalisations and mortality for patients with CVD who often have a high drug burden consisting of multiple medications and complex dosing regimens.2 This is compounded in patients with poor health literacy: the inability to understand and act on medical information.3
Rehospitalisation due to poor medication management presents a significant issue for cardiology patients. The likelihood of hospital readmission for patients with CVD has been shown to increase by 28% in the following month because of poorly managed medication regimens.4 Suboptimal medication concordance is closely associated with adverse outcomes in patients with CVD of whom many are elderly and take five or more medications.5 Poor medication concordance, the use of harmful medications and withdrawal of beneficial medications have been identified as precipitating factors for 20% of heart failure hospitalisations.6 Patients with poor medication concordance also have 36% higher mortality from ischaemic heart disease, and a twofold increased risk of mortality from cerebral haemorrhage and cerebral infarction than those with good concordance.7
Internationally, the provision of pharmacist-led medication reconciliation programmes during hospital transitions has been established as a means for improving posthospital healthcare utilisation.8–11 Growing evidence highlights that comprehensive medication reviews improve health literacy and reduce the number of medication-related errors and inappropriate use of medicines.12–17 In Australia, medication review services were first introduced for residents of aged care facilities in 1997, expanded to include those living in a community setting in 2001,18 19 and further revised in 2020 to include referrals from the hospital-based medical practitioners. The latest amendment enables the initiation of comprehensive medication reviews through hospital networks along with the allowance for pharmacist-initiated follow-up reviews; promoting a patient-centred cycle-of-care whereby pharmacists are directly involved in the follow-up of medication-specific problems.
To date, previous research has explored pharmacist and general practitioner (GP) perspectives of comprehensive medication reviews, including more recently pharmacist perspectives on the implementation of postdischarge medication reviews (PDMRs).20–25 There remains a lack of evidence relating to patient’s perspectives on PDMRs, particularly those with existing CVD or those who are at high risk of CVD complications. Patient’s perspectives are invaluable in assessing the effectiveness of healthcare service implementations aimed at improving health literacy and self-management. Some research exploring pharmacist-led medication reconciliation reviews suggests there is improved health literacy and sustained self-management on returning to a community setting in patients with CVD who receive pharmacist intervention.26 27 To our knowledge, this is the first study exploring these perspectives of transition-of-care (ToC) patients with CVD and their experiences with pharmacist-led medication management services. We aimed to explore the experiences of patients during their ToC from the hospital to home probing their understanding of medication-related changes and subsequent medicine review referral.
Method
Study design, participant selection and recruitment
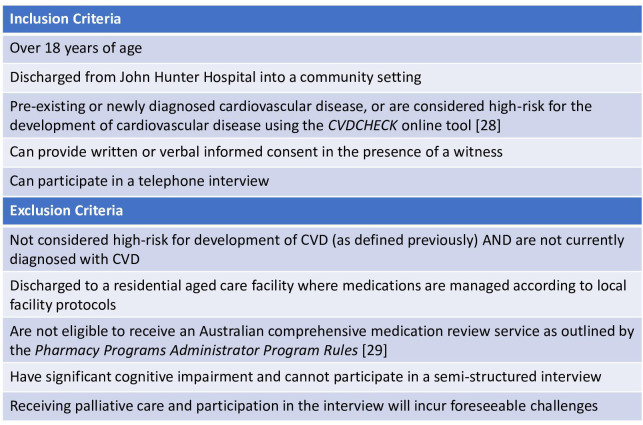
An interpretive qualitative approach was deemed appropriate to explore our research question. Participants were recruited from the John Hunter Hospital (JHH): a major referral hospital for the Hunter New England Local Health District (HNELHD) servicing over 920 000 people. To reduce the risk of recruitment bias, a clear set of inclusion criteria—partly informed by the Australian Chronic Disease Prevention Alliance28 and the Pharmacy Programs Administrator Program Rules29—as shown in figure 1 was created to assist with identifying potential participants. Patients meeting our inclusion criteria being discharged from the JHH with either newly diagnosed or pre-existing CVD were identified by, and invited to participate, by cardiology nurses and pharmacists from the cardiology ward and cardiac rehabilitation clinic (CRC) at the JHH. Purposive sampling was used when identifying and selecting patients with CVD as potential participants for the study to create a diverse and heterogeneous cohort.
Figure 1.
Inclusion and exclusion. CVD, cardiovascular disease.
Potential participants were provided with detailed study information and had the opportunity to ask questions about the research. Candidates were aware of the voluntary nature of their participation in the study and were not reimbursed for their participation. All participants provided informed consent. Interviews were conducted between 1 September 2022 and 30 September 2023. This study employed the use of semistructured interviews and was informed by the COnsolidated criteria for REporting Qualitative research checklist.30 The interview guide was designed by a subgroup of the investigators (JB, HC, JC and DN) following a review of existing literature. The subgroup then constructed questions based on this literature review that address the central aim of the study as shown in online supplemental file 1. However, considering the semistructured interview design, participants had the freedom to express views and experiences in their own words and diverge from the interview guide.
bmjopen-2023-082228supp001.pdf (83.2KB, pdf)
Patient and public involvement
Patient and public involvement was not deemed necessary for the design and implementation of this study.
Data collection and analysis
Semistructured telephone interviews (n=16), ranging from 30 to 60 min, were conducted by a member of the research team (JB) at a mutually convenient time between 1 September 2022 and 30 September 2023. Interviews were audio recorded with the participant’s consent and transcribed ad verbatim by JB with all identifying data removed. Guided by an interview schedule, questions aimed to probe participant experiences of their recent hospitalisation experiences and subsequent implementation and management of medications, as well as attitudes towards pharmacist-led medication management services including availability of PDMR services. Identified themes informed continuing data collection and sampling continued until thematic saturation (two co-coders agreeing that no new themes were emerging) was achieved. Coding was performed independently by two authors (JB and JW), following an inductive thematic approach.31 Analysis followed a three-phase approach: (1) initial familiarisation of the data following a systematic identification of salient themes within each interview transcript; (2) generation of a coding scheme with distinct boundaries linked to sections of the written transcript and (3) collation of codes into larger themes by examining relationships between each code. Transcripts were coded line by line, describing and interpreting emerging categories, and searching for differences and similarities. The next step involved examining the relationship between categories in the context of the research question to form themes. Consistency of findings was upheld through immersion within the data, and peer debriefing with data coding reflexivity and discussion with the research team.32 33 Coders captured exemplar quotes supporting each theme.
Results
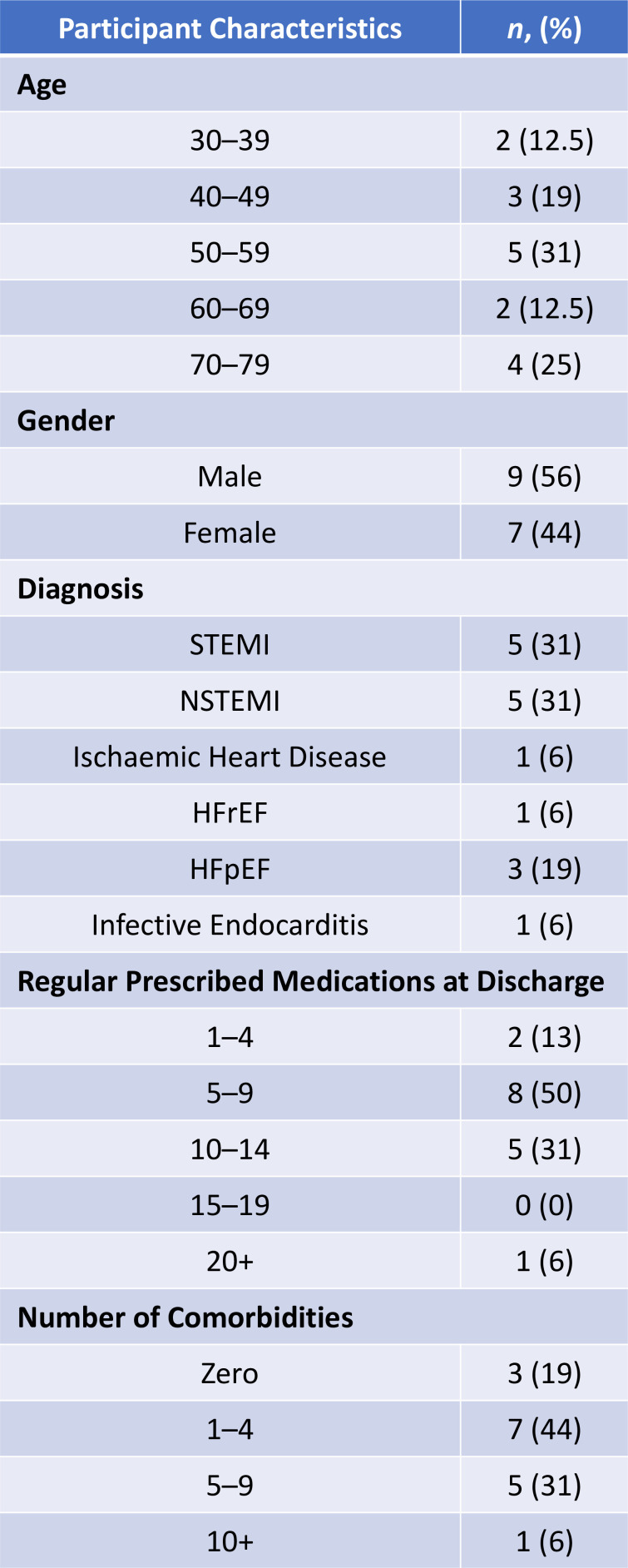
A total of 18 participants provided written informed consent to be interviewed, with 16 completing the interview process. One participant declined the interview and another participant passed away prior to being interviewed. Demographics for the 16 participants (mean age 57.5 (±13.2) years, 9 (56%) male) are shown in figure 2.
Figure 2.
Demographics of interviewed cardiovascular disease patients. Regular medications at discharge denote medications taken daily by patient (excludes ‘when required’ or ‘pro re nata’ medications). The number of comorbidities according to patient’s hospital discharge paperwork. HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; NSTEMI, non-STEMI; STEMI, ST-elevated myocardial infarction.
Three emergent themes were identified:
Poor medication understanding impacts the transition from the hospital to home.
Factors influencing medication concordance following discharge.
Perceived benefits of routine PDMRs.
Poor medication understanding impacts transition from hospital to home
The overwhelming hospital experience
Many participants reported difficulties comprehending health-related information during their hospital admission, including understanding the cause of their cardiovascular event, and subsequent medication and lifestyle changes recommended following their discharge. Participants reflected on their feelings of anxiety and being overwhelmed in response to the experience of a life-threatening cardiovascular event. Participants reportedly attributed anxiety to difficulties in comprehending the initiation of, or changes to, medications during their acute hospital admission.
[It’s] obviously a very stressful situation I was in, being so young and having a cardiac thing go on. So, I didn’t take everything in those first couple of days. (P1)
Because when you’re in hospital and they’re telling you what tablets to take, you’re going ‘okay, there’s just so much going on in hospital.’ Yeah, it’s not until you get home that you think ‘okay, what was that all about?’ It was just a whirlwind I went through. (P4)
Participants reported that understanding copious amounts of new medication-related information was more difficult to comprehend while trying to grasp the extensiveness of medications now required.
…so, they gave me a week’s medication from the pharmacy at the hospital and this big, two A4 sheets of all the tablets that you get. I go ‘oh s**t’ because you don’t know this. I’m going to check-out, and they go ‘oh, here are all your tablets’ and I go ‘oh s**t, look at all this!’ (P5)
Challenges associated with education within a hospital environment
Participants’ understanding of their medication regimen was experienced on a spectrum where some readily grasped changes with new information while others struggled. Difficulty understanding was compounded among participants who had no prior experience with taking regular medications.
My big problem—like, I’ve never had anything before—is knowing what all these tablets do…you know nothing, you’re learning it all. (P5)
Participants recounted varying experiences with education during their hospital admission. Most participants reported they received a combination of verbal and/or written medication instructions during their hospitalisation or at discharge. Participants valued staff who took the time to explain their medication regimen and ‘were nice enough to write down’ (P4) or provide written information. Information sources included physicians, nurses and pharmacists although some participants reported they were unsure as to who provided the information.
…the last doctor I’d seen there [in hospital], he explained to me all the way through me tablets… and it was all written out for me. (P17)
I mean, …there was a person, or some nurse, or doctor came around and explained the situation. (P5)
However, other participants commented on the lack of information provided during their admission and the limited reinforcement of what medication to take and why, especially during medication rounds. Participants’ reports suggested they were passive during medication rounds and only a few pressed staff for information. Many participants perceived limited education was due to staff time constraints and being unable to take time to engage and deliver education in an impactful manner.
None really. It was just, I guess, the nurses coming and saying either ‘this is due’ or ‘how are you feeling? Do you need pain relief?’ (P9)
…you know, when you’re in hospital, it’s so busy, full-on. The doctors and nurses are running from patient-to-patient. So, there’s not a lot of time to actually sit and really talk about medications and sort of similar things like that. (P6)
Participants’ reports suggested the negative impact of receiving differing information from multiple sources. Some participants reported a lack of consistency between staff members which accentuated anxiety and confusion.
So, I guess it’s probably a little bit of anxiousness where you get little snippets of information…you’ve got no idea… I think it’s because the message isn’t coming from the one person all the time. Like it’s coming from various different people. (P7)
Implementing medication self-management
Many participants described the difficulties engaging with self-management education when they felt unwell, distracted by an unfamiliar environment or were focused on ‘wanting to get home.’ (P5)
The thing is, you’ve been sick in hospital, you don’t think. So, your mind’s all muddled up or you go ‘whatever, I don’t want to listen to you.’ (P17)
Being a passive recipient of medications in hospital, alongside struggling to understand a new medication regimen, reportedly impacted participants’ confidence to manage their medications on discharge. Participants reported that they were most unsure during the first few weeks postdischarge as they attempted to establish routines with either taking medications for the first time or implementing a new medication regimen.
But at the time it’s a bit, like, I’m a bit confused about what is what, going though boxes and reading my list. So yeah, the first few weeks was a bit confusing with what I was taking. (P4)
While some participants reported ongoing feelings of anxiety and being overwhelmed by a lack of familiarity with medication terminology and understanding the purpose of their medication, others embraced self-education. For many, this involved conducting online research or talking to family members who were health professionals, especially in relation to side effects.
I came home without too much insight into what they [medications] are and that sort of thing. It’s been kind of left up to my own accord to basically prepare myself. (P9)
I asked my sister—she’s a cardiothoracic nurse. So, I asked her, you know, side effects I was having that I got on the weekend. (P2)
Factors influencing medication concordance following discharge
Discharge home
For many participants, the reality of needing to take life-saving medication became apparent on their return home when they were confronted with the seriousness of the situation and the need to develop new daily medication routines. Many were grateful they were on sick leave or had time postdischarge to establish a routine, including being mindful of when medications needed to be taken and if they needed to be taken with meals or not.
And generally, I get up at the same time each day. Having said that, I am on sick leave at the moment. So that will take time and breakfast will change when I go back to work. But that’s down the track management. (P1)
For participants, especially those without prior experience with taking medication, remembering to administer doses, manage prescriptions and medication supply, and follow-up appointments with GPs while balancing prior commitments with family or work was an additional burden.
I’m just a really busy person. I work full-time and then I’ve got two kids. So, by having to throw medication in on that…I guess it’s like when you’re a new person to start taking medication…you’ve got to take the medication seriously. Like it’s not the first thing that’s on my mind which is not good. I need to change that. (P7)
Cardiac rehabilitation
Several participants reported they continued to lack understanding of their medication regimen, which was apparent when engaging with other health professionals such as dentists or rehabilitation therapists.
I even went to the dentist, and they said: ‘what are you on, we need to update your records’, and I didn’t even know. (P9)
I was just at Cardio Rehab [CRC]…and they asked me if I was on a beta-blocker, and I actually didn’t know what a beta-blocker was. I was, like, not sure! (P7)
Nine participants were recruited through the CRC at the JHH and reported increased accessibility and reinforcement of medication information through the clinic. Participation in the CRC provided participants with an opportunity for further engagement with specialists in cardiology and ask questions or raise concerns related to medications or management of their CVD.
…I was going to have a chat with one of the guys at the pharmacy, but I thought I’m at rehab [CRC] today, I’ll chat with them [the nurses] about the cholesterol medication I’m on. (P6)
External support
Many participants relied on others to help manage their medications and adhere to their schedule, be that family members, carers or community pharmacists. While this was most evident in the weeks following discharge, others reported an ongoing reliance on family members or carers. As such, some participants acknowledged they had less opportunity to engage with community pharmacists for ongoing education, information or intervention if necessary.
My son sort of gets them out and gives them to me, and I just take them as I’m supposed to. I’m a bit foggy at the moment, but he’s looking after it. I’ll have to get more involved very shortly. (P15)
Because, say I say to my wife: ‘I’m too sick to get my tablets today, can you pick them up for me?’ So, if someone else goes and picks up your tablets for you, you don’t have any interaction with the pharmacist. (P5)
Engagement with pharmacist-led medication management services
Many participants stated that their experience with pharmacist-led medication management services was limited to medication supply and prescription management, predominantly delivered in a community setting.
So, you know, I guess their role is pretty broad. But personally, I use them for prescriptions and information around that and that’s probably about it. (P12)
Sort of nothing really. Just when it comes to medication-wise. Like that’s the only time I sort of have anything to do with pharmacists, it’s when I’ve gotta pick up medication. (P14)
Participants readily identified the importance of community pharmacies managing their prescriptions and medications, including the use of dose administration aids (DAAs).
So obviously looking at things of whether Webster-paks or blister packs [medication compliance packaging]—pre-made medications—that sort of thing as well I think is really important. (P1)
However, some participants acknowledged that by relying on an external source there was the potential for error or oversight if they were not familiar with changes to their medications.
I gave my prescriptions actually to the pharmacist. You don’t have to think about sitting at the table and dividing them all up and hoping that they’re not all wrong…which has happened a couple of times. I’ve gone a couple of weeks without realising I wasn’t taking one particular [medication]. (P18)
Engagement with community care
Participants who followed through with an appointment to see their GP on discharge indicated the benefit of gaining further understanding of their recent hospitalisation and medication changes, including accessing new prescriptions.
I was told to go to my GP a week after which I did yesterday…she reinforced what [medications] they had sent me home with. (P11)
Overall, participants reported a wide range of challenges adhering to a medication regimen on discharge. Many participants were not supplied with sufficient medication quantities on discharge to see them through to their follow-up GP appointment, who were often required to wait several weeks.
…because my GP is booked out that far ahead, I’m looking at two to three weeks. When I rang up to say that I need an appointment to arrange some medications after I had a heart attack, they had to put me on an emergency waiting list, and even then, it took them seven days to get me in. (P3)
Participants were reportedly confronted with the concept of taking multiple medications, highlighting their embarrassment and the stigma associated with medication use. Some participants were reluctant to seek pharmacist-led medication management services, such as DAAs, due to its perceived association with advanced age.
…going into the pharmacy and just slapping them [the prescriptions] down on the counter, it’s just going to feel like I’m a walking medication taker! Once I get over the initial embarrassment…I’m actually going to be calling them and saying, ‘I need to fill my medication’. (P7)
And for me, personally, I still consider myself still fairly young, and I think this [DAA] is an old person’s thing. So, getting your head around it all, you know, it’s a little new. (P2)
Many participants commented on the benefit of accessing a community pharmacist for medication-related information and health advice prior to escalating any concerns to their GP.
I wouldn’t go and pick up a multivitamin or something without talking to the chemist [pharmacist]: ‘this is what I take. Could there be any interactions?’ (P12)
Because sometimes it’s hard to get into see your GP. And sometimes it’s not necessary to see your GP. I feel that [the community pharmacist] is the ‘first port-of-call’; unless you’re really, really sick. (P6)
Conversations with a community pharmacist on discharge home provided many participants with the reassurance they needed to better manage their medications. However, some participants reported they were reticent to speak to their community pharmacist due to privacy concerns associated with discussing personal medical information in public or being a burden when the pharmacist was perceived to be ‘busy’. (P11)
But what I really hate when I go to the chemist [pharmacy] is…they want to talk to you—and there are so many people around… I actually feel uncomfortable talking about that in front of other people…it’s probably not actually sinking in because I’m like ‘who’s standing behind me, is there someone here that I know’ you know? And I think that’s probably why I didn’t know a lot about my medications. (P7)
For some participants, accessing a community pharmacist and pharmacy services centred around medication cost whereby participants would seek multiple pharmacies to obtain the best price for their medications. Participants acknowledged this had potential to impact continuity of care facilitated by seeing the same pharmacist.
So, we try to keep costs down where we can…at least by going to that [discount pharmacy] kind of thing…but in a way of a relationship, I wouldn’t know any of the people in there. (P9)
Perceived benefits of routine PDMRs
Most participants acknowledged the importance of taking responsibility for their medications. However, all participants could foresee circumstances where the availability of PDMRs would prove beneficial.
I think it [PDMRs] would be really valuable. For me who’s never really taken any medication, you know, it’s all a bit daunting all of a sudden having to take medication. (P2)
As a nurse, there are a lot of people out there who have no clue what their medications are or how they should be working, or when they should be taking them. So, I can see the benefits of it—even for myself. (P16)
Incorporation of PDMRs into standard of care
Participants reported that PDMR would provide an opportunity for a tailored provision of information. Some participants suggested incorporating a ‘triage’ system to account for each patient’s individual social situation and educational needs, along with assessing those who may be at high risk for medication misadventure.
There could be benefits from them [PDMRs] that you don’t see until you actually have someone come to have a look. I think that you would probably ideally…make contact with a person in hospital, so you understand what their circumstances are. And then you could make the decision from there. It’s very person orientated. (P12)
…then maybe from that phone call going ‘okay you sound really stressed about your medication we’ll try and squeeze you in tomorrow’…I guess maybe, like, a phone call to kinda like “triage” how urgently they need it. (P1)
The option for a PDMR with a pharmacist was perceived as a means of easing the anxiety experienced during and after discharge home. Participants reported that a PDMR would benefit their transition back into a community setting to reinforce information and provide ongoing monitoring, reassurance and support. Similarly, participants perceived that receiving a PDMR at home gave them time to process their hospitalisation and any changes implemented, which might raise issues to be discussed.
And also, when you’re in the hospital, you might not be thinking of these things to ask either because it’s all new and stuff. So, by the time you get home you can all of a sudden sit down and sort of absorb the information. (P2)
…like you feel quite safe while in hospital. But when you come home, it’s a little bit daunting. (P6)
Home visitation for a PDMR was also perceived to be more conducive for medication-related education, away from the time pressures experienced in other settings.
You’re not in the pharmacy with people glaring at you thinking ‘hurry, hurry up, get out of the way.’ And even you’re not sitting in the doctor’s surgery thinking ‘I’m getting charged for every 5 minutes I’m sitting here.’ (P9)
And when you go to the GP, it’s very transactional. Like, it’s just like you’re in, out. They’re really busy to the point that you don’t feel confident that they really listen. (P7)
Discussion
Summary of main findings
Our study explored perspectives of patients with CVD on their experiences with medication management and pharmacist-led medication review services during their ToC, including attitudes towards having access to PDMRs. Cardiology patients’ ToC following a hospital admission is often associated with a period of vulnerability that may be ameliorated through pharmacist medication reconciliation.34 Our findings identified that the hospital environment presented several challenges which impacted the effective delivery of education for inpatients. Participants detailed difficulties understanding and retaining medication-related information during their admission for a significant health event. Feelings of anxiety and being overwhelmed contributed to poor information retention and meant participants returned home lacking confidence in managing their medications. Despite these feelings, many participants received minimal support through pharmacist-led medication management services across their ToC. Overall, while participants took time to establish a routine back home, many gradually became confident and expressed value in a medication review to monitor and provide support on their return to a community setting.
Comparison with existing literature
The impact of time pressures on the quality and efficacy of hospital-delivered education for inpatients has been extensively covered in the published literature.35–38 In response, patients may be less equipped to manage their medications on discharge to a community setting, thus affecting their quality use of medicines (QUM)—the safe, effective and appropriate use of medicines—and increasing the risks of future hospitalisations.
Obtaining the patient’s perspective is a critically important phase of implementing new health services. Our results provide the perspectives of patients with CVD, thus building on existing literature.39 For example, White et al 40 conducted a qualitative study that identified four key benefits of medication reviews as perceived by eligible patients: (1) acquisition of personalised medication information and advice; (2) reassurance regarding medications and coordination of their care; (3) feeling valued and cared for by a healthcare provider and (4) enhancing the patient–provider and pharmacist–GP relationships. Our study mirrors these observations concerning the perceived benefits of PDMRs, particularly the need for postdischarge follow-up and the reassurance that patients experience when receiving pharmacist input into their care.
However, the White et al study identified patient concerns around the potential for pharmacist medication reviews to be perceived as undermining the authority of the GP, thus having a negative impact on the patient’s relationship with their GP.40 Participants in our study did not share these same perspectives, and instead felt that PDMRs would have potential to improve access to primary care postdischarge through pharmacists due to difficulties experienced with accessing their GPs. Our study demonstrated PDMRs were considered an opportunity to ask questions and more actively engage in education within the security of their own home. We posit that PDMRs have the potential to bridge education deficits that emerge on discharge home and promote communication between hospital and community-based medical practitioners.
The timing of service provision is crucial to ensure that QUM is maintained, and the risk of medication-related problems is minimised. Evidence detailing the incidence of medication-related problems ranges from 18.4% 2 weeks postdischarge to 37.5% 4 weeks postdischarge.41 Recently, Daliri et al demonstrated that pharmacy-led transitional care education programmes reduced the proportion of patients experiencing self-reported medication-related problems 4 weeks postdischarge.42 Participants in our study highlighted their desire for early pharmacist follow-up, within the first 7 days postdischarge being the most common request. This demonstrates the importance of early postdischarge follow-up to promote the safe and effective use of medicines for ToC patients.
Participants in the study experienced issues engaging with primary care once discharged from the hospital, identifying a potential role for pharmacists to bridge this gap. GP access for prescription resupply was the most common challenge experienced by participants when returning home. The limited quantities of tablets provided to participants at the time of discharge was sometimes insufficient to sustain them until their GP appointment. The HNELHD is part of the New South Wales (NSW) public health system which stipulates that take home supplies of regular medications must not exceed 7 days’ supply when discharged from the hospital.43 Unfortunately, this restriction imposes significant challenges for patients discharged from NSW public hospitals. This varies considerably to other states within Australia—for example, both Queensland and Victorian public hospital networks allow a 1-month supply of regular medications under the Pharmaceutical Benefits Scheme.44 45 Given that access to a GP may be difficult on discharge due to lengthy wait times, we advocate that pharmacists may in fact play an important role in ensuring the continuity of care and appropriate access to medications through the incorporation of a PDMR as standard of care for ToC patients.
Strengths, limitations and implications on future research and practice
The strength of this study lies in the exploration of a heterogeneous sample of cardiology patients. A diverse cohort of participants was purposively selected to capture the broadest range of perspectives possible. Furthermore, the inductive thematic analysis approach used in this study enables the richness of the qualitative data to be captured through a more flexible and reflective process. This method aims to remove a researcher’s analytic preconceptions, ensuring thematic analysis is data driven rather than researcher driven. We acknowledge that many patients were reflecting on the prospect of a PDMR across their ToC rather than having received one. A limitation of this study includes the potential for reporting bias. It is possible that ToC patients with CVD who engaged with the study may in fact have a differing experience with pharmacist-led medication management services compared with those who did not participate. The relatively young mean age of participants (57.5 years of age) may also not accurately reflect the views and experiences of ‘older’ adult patients (over the age of 65 years) surrounding their need for pharmacist-led medication management services. It is well documented that patients living outside major Australian capital cities have poorer health outcomes.46 Our study recruited patients who predominantly live outside the major capital city area(s) of Australia. Hence, their inclusion may, therefore, represent unique health outcome challenges associated with their geographical location. Our results provide a baseline understanding of the perspectives of ToC patients with CVD in terms of the implementation of PDMRs. Future research is needed to evaluate the clinical benefit of routine PDMRs for patients with CVD, investigating the acceptability of the service but also its impact on key CVD outcome markers, including 30-day hospital readmission rates and the incidence of major adverse cardiovascular events. In addition, future research should explore the perspectives of other population groups and their engagement with pharmacist-led medication management services. This may include the perspectives of patients who are not immediately engaged with the hospital system, along with culturally and linguistically diverse patients and those residing in regional, rural and remote localities.
Conclusion
Pharmacists are ideally positioned to assist patients with CVD across their ToC journeys as part of a broader multidisciplinary team. PDMRs are viewed by ToC patients with CVD as an acceptable means of improving their health literacy and QUM when transitioning from the hospital back home. However, our study indicates that patients with CVD do not frequently engage with pharmacist-led medication management services during their ToC. Routine service implementation may address the patient’s desire for postdischarge follow-up and provision for education away from the busy hospital environment. Service implementation may benefit from an initial ‘triage’ to individualise the delivery by assessing the patient’s own needs and expectations of the service while screening for those who may be at high risk of medication misadventure.
Supplementary Material
Acknowledgments
The authors would like to thank the participants for their time and willingness to partake in the interviews.
Footnotes
@JD_Bennetts
Contributors: Study design was conducted by JB, HC, JC, JW and DN. Recruitment was conducted by JB, DM, NE and MA. Interviews and interview transcription were performed by JB. Data analysis was completed by JB and JW. JB drafted the manuscript for publication and DN, ALS, HC, JW and JC contributed to the content and revision of the manuscript. Revisions, literature and manuscript checking were managed by JB. DN is acting as guarantor for this research. All authors read and approved the final version.
Funding: JB is the recipient of an Australian Government Research Training Programme Scholarship (University of Newcastle Vice-Chancellor’s Scholarship) and would like to thank the Commonwealth of Australia for their financial contribution to this research (Award ID not assigned). ALS is supported by Heart Foundation Australia Future Leader Fellowships (Award IDs 101918 and 106025). DN is supported by the NSW Ministry of Health EMC Fellowship, Australia (Grant ID G1701368) and Heart Foundation Australia Future Leader Fellowship (Award ID 104814). This work is supported in part by the Piggotts Family Trust from the Hunter Medical Research Institute (DN, JB; Grant ID G2100856); Royal Australasian College of Physicians (RACP) Foundation Research Establishment Awards (ALS; Grant ID G1801367); NSW Ministry of Health Translational Research Grant (ALS; Grant ID G1901542) and 2022 John Hunter Hospital Charitable Trust Grant (ALS, JB; Grant ID G2200585).
Competing interests: JB is a credentialed pharmacist who can provide domiciliary medication management reviews funded by the Australian Government Department of Health and Aged Care.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. All data relevant to the study was included either in the manuscript or as online supplemental material. Selected anonymised qualitative interview data may be made available on request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Hunter New England Human Research Ethics Committee of Hunter New England Local Health District (reference—2022/ETH00872). Participants gave informed consent to participate in the study before taking part.
References
- 1. Health AIo, Welfare . Heart, Stroke and Vascular Disease: Australian Facts. Canberra: AIHW, 2023. [Google Scholar]
- 2. Abolbashari M, Macaulay TE, Whayne TF, et al. Polypharmacy in cardiovascular medicine: problems and promises. CHAMC 2017;15:31–9. 10.2174/1871525715666170529093442 [DOI] [PubMed] [Google Scholar]
- 3. Mixon AS, Myers AP, Leak CL, et al. Characteristics associated with postdischarge medication errors. Mayo Clin Proc 2014;89:1042–51. 10.1016/j.mayocp.2014.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Organization WH . Medication without harm. World Health Organization; 2017. [Google Scholar]
- 5. Mastromarino V, Casenghi M, Testa M, et al. Polypharmacy in heart failure patients. Curr Heart Fail Rep 2014;11:212–9. 10.1007/s11897-014-0186-8 [DOI] [PubMed] [Google Scholar]
- 6. Formiga F, Chivite D, Manito N, et al. Hospitalization due to acute heart failure. role of the precipitating factors. Int J Cardiol 2007;120:237–41. 10.1016/j.ijcard.2006.10.004 [DOI] [PubMed] [Google Scholar]
- 7. Kim S, Shin DW, Yun JM, et al. Medication adherence and the risk of cardiovascular mortality and hospitalization among patients with newly prescribed antihypertensive medications. Hypertension 2016;67:506–12. 10.1161/HYPERTENSIONAHA.115.06731 [DOI] [PubMed] [Google Scholar]
- 8. Mekonnen AB, McLachlan AJ, Brien J-AE. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open 2016;6:e010003. 10.1136/bmjopen-2015-010003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ramalho de Oliveira D, Brummel AR, Miller DB. Medication therapy management: 10 years of experience in a large integrated health care system. J Manag Care Pharm 2010;16:185–95. 10.18553/jmcp.2010.16.3.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee E, Braund R, Tordoff J. Examining the first year of medicines use review services provided by pharmacists in New Zealand: 2008. N Z Med J 2009;122. [PubMed] [Google Scholar]
- 11. Blenkinsopp A, Bond C, Raynor DK. Medication reviews. Br J Clin Pharmacol 2012;74:573–80. 10.1111/j.1365-2125.2012.04331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chen TF. Pharmacist-led home medicines review and residential medication management review: the Australian model. Drugs Aging 2016;33:199–204. 10.1007/s40266-016-0357-2 [DOI] [PubMed] [Google Scholar]
- 13. Renaudin P, Boyer L, Esteve M-A, et al. Do Pharmacist‐Led medication reviews in hospitals help reduce hospital readmissions? A systematic review and meta‐analysis. Br J Clin Pharmacol 2016;82:1660–73. 10.1111/bcp.13085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burgess LH, Kramer J, Castelein C, et al. Pharmacy-led medication reconciliation program reduces adverse drug events and improves satisfaction in a community hospital. HCA Healthc J Med 2021;2:411–21. 10.36518/2689-0216.1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Abdulghani KH, Aseeri MA, Mahmoud A, et al. The impact of pharmacist-led medication reconciliation during admission at tertiary care hospital. Int J Clin Pharm 2018;40:196–201. 10.1007/s11096-017-0568-6 [DOI] [PubMed] [Google Scholar]
- 16. Kramer J, Hayley Burgess L, Warren C, et al. Impact of pharmacist-led admission medication reconciliation on patient outcomes in a large health system. J Patient Saf Risk Manag 2023;28:260–7. 10.1177/25160435231193584 [DOI] [Google Scholar]
- 17. Tan JP, Cheng KKF, Siah RCJ. A systematic review and meta‐analysis on the effectiveness of education on medication adherence for patients with hypertension, hyperlipidaemia and diabetes. J Adv Nurs 2019;75:2478–94. 10.1111/jan.14025 [DOI] [PubMed] [Google Scholar]
- 18. Pharmaceutical Society of Australia . Guidelines for pharmacists providing residential medication management review (RMMR) and quality use of medicines (QUM) services. 2011.
- 19. Australian Government . Third community Pharmacy agreement between the Commonwealth of Australia and the pharmacy Guild of Australia. Commonwealth of Australia; 2000. [Google Scholar]
- 20. Czarniak P, Hattingh L, Sim TF, et al. Home medicines reviews and residential medication management reviews in Western Australia. Int J Clin Pharm 2020;42:567–78. 10.1007/s11096-020-01001-8 [DOI] [PubMed] [Google Scholar]
- 21. Weir KR, Naganathan V, Bonner C, et al. Pharmacists’ and older adults’ perspectives on the benefits and barriers of home medicines reviews–a qualitative study. J Health Serv Res Policy 2020;25:77–85. 10.1177/1355819619858632 [DOI] [PubMed] [Google Scholar]
- 22. Weir KR, Naganathan V, Rigby D, et al. Home medicines reviews: a qualitative study of Gps’ experiences. Aust J Prim Health 2020;26:24. 10.1071/PY19072 [DOI] [PubMed] [Google Scholar]
- 23. Patounas M, Lau ET, Chan V, et al. Home medicines reviews: a national survey of Australian accredited pharmacists’ health service time investment. Pharm Pract (Granada) 2021;19:2376. 10.18549/PharmPract.2021.3.2376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Spinks J, Birch S, Wheeler AJ, et al. Provision of home medicines reviews in Australia: linking population need with service provision and available pharmacist workforce. Aust Health Rev 2020;44:973–82. 10.1071/AH19207 [DOI] [PubMed] [Google Scholar]
- 25. Angley M, Criddle D, Rigby D, et al. Hospital‐initiated post‐discharge medication reviews in Australia: expert opinion on the barriers and enablers to implementation. Pharmacy Practice and Res 2022;52:446–53. 10.1002/jppr.1832 [DOI] [Google Scholar]
- 26. Cawthon C, Walia S, Osborn CY, et al. Improving care transitions: the patient perspective. J Health Commun 2012;17 Suppl 3:312–24. 10.1080/10810730.2012.712619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Parajuli DR, Franzon J, McKinnon RA, et al. Role of the pharmacist for improving self-care and outcomes in heart failure. Curr Heart Fail Rep 2017;14:78–86. 10.1007/s11897-017-0323-2 [DOI] [PubMed] [Google Scholar]
- 28. Australian Chronic Disease Prevention Alliance . Australian Guideline for Assessing and Managing Cardiovascular Disease Risk. Canberra, ACT: Commonwealth of Australia, 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pharmacy Programs Administrator . Medication management programs. 2021. Available: https://www.ppaonline.com.au/programs/medication-management-programs
- 30. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 31. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 32. Krefting L. Rigor in qualitative research: the assessment of trustworthiness. Am J Occup Ther 1991;45:214–22. 10.5014/ajot.45.3.214 [DOI] [PubMed] [Google Scholar]
- 33. Pandit NR. The creation of theory: a recent application of the grounded theory method. TQR 1996;2:1–15. 10.46743/2160-3715/1996.2054 [DOI] [Google Scholar]
- 34. Al Sattouf A, Farahat R, Khatri AA. Effectiveness of transitional care interventions for heart failure patients: a systematic review with meta-analysis. Cureus 2022;14:e29726. 10.7759/cureus.29726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Deccache A, Aujoulat I. A European perspective: common developments, differences and challenges in patient education. Patient Educ Couns 2001;44:7–14. 10.1016/s0738-3991(01)00096-9 [DOI] [PubMed] [Google Scholar]
- 36. Badiyepeymaiejahromi Z, Isfahani SS, Parandavar N, et al. Nursing students' perspectives regarding challenges of patient education in clinical settings. Bangladesh J Med Sci 2016;15:615–20. 10.3329/bjms.v15i4.30719 [DOI] [Google Scholar]
- 37. Tsiga E, Panagopoulou E, Sevdalis N, et al. The influence of time pressure on adherence to guidelines in primary care: an experimental study. BMJ Open 2013;3:e002700. 10.1136/bmjopen-2013-002700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cooper JM, Garrett T. Providing medicines information and education to hospital in‐patients: patients’ experiences and preferences. J Pharm Pract Res 2014;44:213–9. 10.1002/jppr.1035 [DOI] [Google Scholar]
- 39. Australian Commission on Safety and Quality in Health Care . Patient-centred care: improving quality and safety through partnerships with patients and consumers. Sydney: Australian Commission on Safety and Quality in Health Care; 2011. [Google Scholar]
- 40. White L, Klinner C, Carter S. Consumer perspectives of the Australian home medicines review program: benefits and barriers. Res Social Adm Pharm 2012;8:4–16. 10.1016/j.sapharm.2010.11.003 [DOI] [PubMed] [Google Scholar]
- 41. Garcia-Caballos M, Ramos-Diaz F, Jimenez-Moleon JJ, et al. Drug-related problems in older people after hospital discharge and interventions to reduce them. Age Ageing 2010;39:430–8. 10.1093/ageing/afq045 [DOI] [PubMed] [Google Scholar]
- 42. Daliri S, Hugtenburg JG, Ter Riet G, et al. The effect of a pharmacy-led transitional care program on medication-related problems post-discharge: a before—after prospective study. PLOS ONE 2019;14:e0213593. 10.1371/journal.pone.0213593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. NSW Government . Medication Handling. St Leonards, New South Wales: NSW Government, 2022. [Google Scholar]
- 44. Queensland Government . Commonwealth funding of medicines Brisbane. QLD: Queensland Health; 2019. Available: https://www.health.qld.gov.au/clinical-practice/guidelines-procedures/medicines/commonwealth-funding [Google Scholar]
- 45. Victorian government Department of health . Pharmaceutical benefits scheme in Victoria’s public hospitals. 2015. Available: https://www.health.vic.gov.au/patient-care/pharmaceutical-benefits-scheme-in-victorias-public-hospitals
- 46. Health AIo, Welfare . Health AIo, Welfare. Rural and Remote Health. Canberra: AIHW, 2023. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-082228supp001.pdf (83.2KB, pdf)
Data Availability Statement
Data are available on reasonable request. All data relevant to the study was included either in the manuscript or as online supplemental material. Selected anonymised qualitative interview data may be made available on request.