Key Teaching Points.
-
•
The presence of a left atrial band can lead to incomplete block lines in atrial fibrillation ablation, and it can be a part of the tachycardia circuit in supraventricular arrhythmias.
-
•
The presence of a left atrial band can increase technical difficulties during catheter ablation for atrial fibrillation because of anatomical difficulties.
-
•
An intracardiac echocardiography catheter is useful for delineating abnormal structures in the left atrium, including the left atrial band, and allows visual confirmation of contact between the structure and the ablation catheter.
-
•
It is important to assess not only a left atrial appendage thrombus and pulmonary vein structural abnormalities but also the left atrial band in preoperative computed tomography (CT).
-
•
The present case emphasizes the role of preoperative CT in demonstrating the complete anatomy of the left atrium and associated abnormalities.
Introduction
A left atrial band is a congenital anomaly with an incidence of 2% based on autopsy studies.1 However, based on transesophageal echocardiography (TEE), only 1 case of a left atrial band was reported from more than 20,000 examinations in the past 20 years.2 A left atrial band, composed of fibromuscular tissue, connects the left atrial side of the fossa ovalis to other areas of the left atrium.1 An additional association between the left atrial band and presence of a patent foramen ovale and Chiari network has been reported, and an increased incidence of premature atrial complexes has also been observed.1 Another study reported an association between left atrial bands and cardiogenic stroke.3 However, the clinical significance of left atrial bands remains largely unknown. Here, we report a case of atrial fibrillation (AF) ablation with evidence of electrical conduction through the left atrial band.
Case report
A 65-year-old man with a 7-year history of AF was referred to our hospital for catheter ablation owing to associated shortness of breath upon exertion. The patient was scheduled to undergo catheter ablation after providing informed consent. His medications included bisoprolol (2.5 mg) and rivaroxaban (15 mg/day), although other medical history was unremarkable. Physical examination revealed a heart rate of 60 beats per minute, a blood pressure of 117/75 mm Hg, an oxygen saturation of 95%, and a body temperature of 35.8°C. Chest radiography revealed a cardiothoracic ratio of 48%. Electrocardiography revealed AF rhythm and no significant ST-T changes. Laboratory tests revealed a mild elevated B-type natriuretic peptide level of 96.7 pg/mL. Transthoracic echocardiography showed a left ventricular ejection fraction in the normal range at 65% and no significant valvular disease. The left atrial diameter increased to 51 mm. Preoperative cardiac computed tomography (CT) revealed a left atrial band adhering from the atrial septum to the posterior wall of the left atrium (Figure 1A and 1B). There was no evidence of a left atrial appendage thrombus, pulmonary vein structural abnormalities, patent foramen ovale, or coronary artery stenosis.
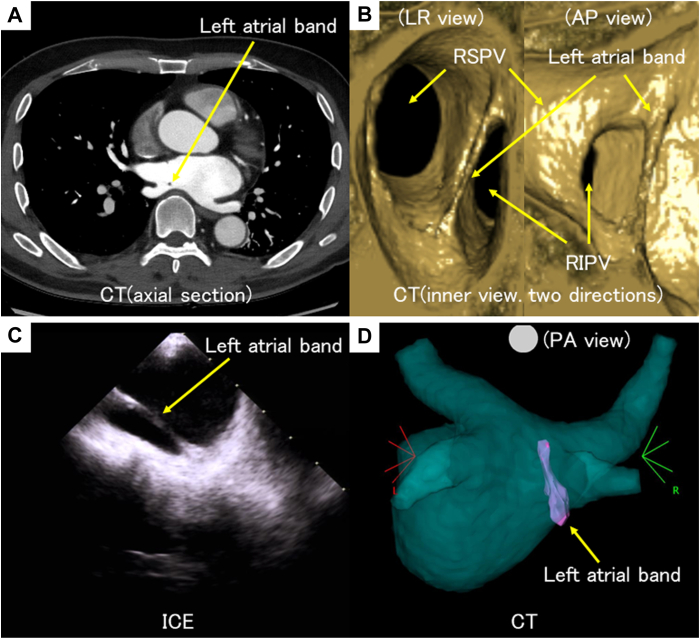
Figure 1.
Preoperative cardiac computed tomography (CT) reveals a left atrial band adhering from the atrial septum to the posterior wall of the left atrium (A: axial section; B: inner view). A SoundStar intracardiac echocardiography (ICE) catheter (Biosense Webster, Diamond Bar, CA) was used to merge the left atrium and left atrial band before the transseptal puncture (C: ICE; D: CT merge). RIPV = right inferior pulmonary vein; RSPV = right superior pulmonary vein.
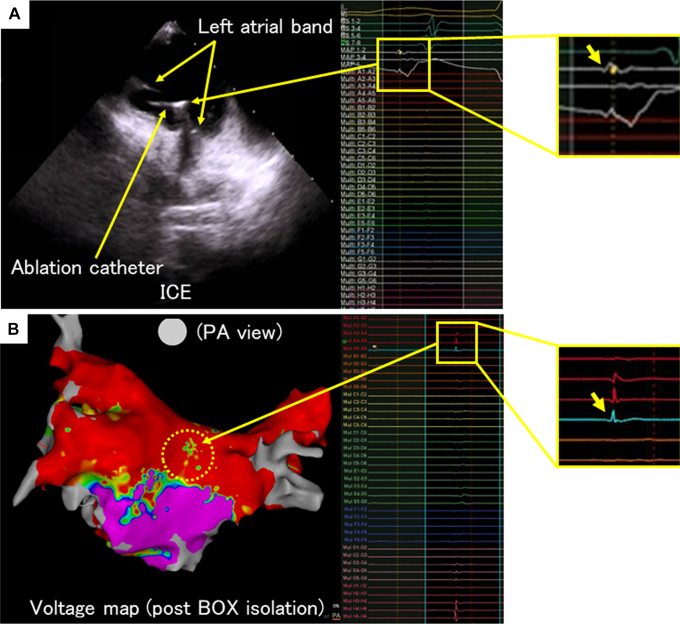
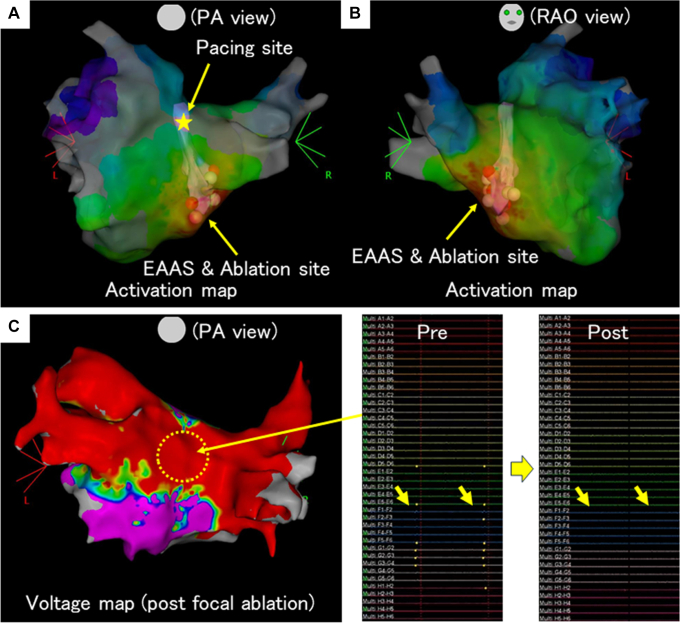
During the catheter ablation, the CARTO 3D electroanatomical mapping system (Biosense Webster, Diamond Bar, CA) was used. A SoundStar intracardiac echocardiography (ICE) catheter (Biosense Webster) was used to merge the left atrium and left atrial bands before the transseptal puncture was performed (Figure 1C and 1D). After mapping of the left atrium using an OCTARAY catheter (Biosense Webster) in sinus rhythm, the ablation catheter was placed in contact with the central part of the left atrial band under the ICE catheter and contact force guide. The local potential was confirmed (Figure 2A). Pulmonary vein and posterior wall isolation was performed, although residual local potentials were observed in the middle of the posterior wall, and the bidirectional block was not completed in the voltage map (Figure 2B). However, a bidirectional block was observed on the roof and bottom lines. Pacing was performed at the site of the local potentials recorded in the middle of the posterior wall, and the left atrium was mapped. The activation map showed a centrifugal pattern with the atrial septum and contralateral attachment end of the left atrial band as the earliest atrial activation site, suggesting incomplete pulmonary vein and posterior wall isolation by electrical conduction through the left atrial band (Figure 3A and 3B). When focal ablation of the left atrial septum attached to the left atrial band was performed while the OCTARAY catheter was placed in the posterior wall, the local potential recorded by the OCTARAY catheter disappeared. When voltage mapping was performed again, the local potentials in the posterior wall disappeared, confirming the completion of the bidirectional block and pulmonary vein and posterior wall isolation (Figure 3C). The session was completed without any left atrial band damage resulting from catheter manipulation. No complications were observed. Three months have passed since the catheter ablation, and no recurrence of AF or other supraventricular arrhythmias has been observed.
Figure 2.
A: The ablation catheter is contacted with the central part of the left atrial band under the intracardiac echocardiography (ICE) catheter and contact force guide, and local potentials are confirmed. B: Pulmonary vein and posterior wall isolation was performed, although residual local potentials were observed in a part of the middle of the posterior wall, and the bidirectional block was not completed in the voltage map.
Figure 3.
The activation map shows a centrifugal pattern with the atrial septum, the contralateral attachment end of the left atrial band, as the earliest atrial activation site (EAAS), suggesting incomplete pulmonary vein and posterior wall isolation by electrical conduction through the left atrial band (A: posteroanterior view; B: right anterior oblique view). C: When the voltage mapping was performed after focal ablation for the left atrial septum, the local potentials in the posterior wall disappeared, confirming the completion of the bidirectional block, and pulmonary vein and posterior wall isolation was completed.
Discussion
No previous report has verified and proven left atrial band electrical conduction during catheter ablation, and, to our knowledge, this is the first demonstration of electrical conduction through the left atrial band. The presence of a left atrial band can lead to incomplete block lines in AF ablation and can be part of the tachycardia circuit in supraventricular arrhythmias. Moreover, the presence of a left atrial band can pose technical difficulties during catheter ablation for AF because of anatomical difficulties.4
The ICE catheter is widely used during ablation procedures, primarily for transseptal puncture and CT merging of the left atrium, ventricle, and aortic cusp. In addition, an ICE catheter is useful for delineating abnormal structures in the left atrium, including left atrial bands, and allows visual confirmation of contact between the structure and ablation catheter.
Various modalities, such as echocardiography, CT, and magnetic resonance imaging, are useful for assessing left atrial bands. Before AF ablation, CT or TEE is usually performed for preoperative assessment, including that for a left atrial appendage thrombus. According to previous studies, a left atrial band may be overlooked on TEE.2 The present case emphasizes the role of preoperative CT in demonstrating the complete anatomy of the left atrium and associated abnormalities.
There was 1 limitation in this case. In the ablation procedure, the ablation catheter was placed in contact with the central part of the left atrial band under the ICE catheter and contact force guide. A left atrial band is a thin structure, and owing to the respiratory motion of the patient, the catheter contact was slightly unstable. For the evaluation of residual local potentials in a left atrial band, reliability was obtained by checking the reproducibility many times.
Conclusion
In this case, the left atrial band was shown to exhibit electrical conduction properties for the first time. The presence of a left atrial band can lead to incomplete block lines in AF ablation and can be a part of the tachycardia circuit in supraventricular arrhythmias. An ICE catheter is useful for delineating abnormal structures in the left atrium, including the left atrial band, and allows visual confirmation of contact between the structure and ablation catheter.
Disclosures
We have no conflicts of interest to disclosure concerning this report.
Acknowledgments
We are grateful to the members of our laboratory for helpful discussions and comments on the manuscript.
Written informed consent was obtained from the patient.
Funding Sources
None.
References
- 1.Yamashita T., Ohkawa S., Imai T., Ide H., Watanabe C., Ueda K. Prevalence and clinical significance of anomalous muscular band in the left atrium. Am J Cardiovasc Pathol. 1993;4:286–293. [PubMed] [Google Scholar]
- 2.Liou K., Premaratne M., Mathur G. Left atrial band: a rare congenital anomaly. Ann Card Anaesth. 2014;17:318–319. doi: 10.4103/0971-9784.142077. [DOI] [PubMed] [Google Scholar]
- 3.Ozer O., Sari I., Davutoglu V., Yigiter R., Akkoyun C. Cryptogenic stroke in two cases with left atrial band: coincidence or cause? Eur J Echocardiogr. 2009;10:360–361. doi: 10.1093/ejechocard/jen302. [DOI] [PubMed] [Google Scholar]
- 4.Okajima K., Imamura K., Kanda G., Shimane A. Left atrial anomalous muscular band detected by computed tomography before catheter ablation in a patient with atrial fibrillation. J Arrhythm. 2015;31:64–65. doi: 10.1016/j.joa.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]