Abstract
Highly purified subunit vaccines require potent adjuvants in order to elicit optimal immune responses. In a previous phase I trial, an alum formulation of ICC-1132, a malaria vaccine candidate comprising hepatitis B core (HBc) virus-like particle containing Plasmodium falciparum circumsporozoite (CS) protein epitopes, was shown to elicit Plasmodium falciparum-specific antibody and cellular responses. The present study was designed as a single-blind, escalating-dose phase I trial to evaluate the safety and immunogenicity of single intramuscular doses of ICC-1132 formulated in the more potent water-in-oil adjuvant Montanide ISA 720 (ICC-1132/ISA 720). The vaccine was safe and well tolerated, with transient injection site pain as the most frequent complaint. All vaccinees that received either 20 μg or 50 μg of ICC-1132/ISA 720 developed antiimmunogen and anti-HBc antibodies. The majority of volunteers in these two groups developed sporozoite-specific antibodies, predominantly of opsonizing immunoglobulin G subtypes. Peak titers and persistence of parasite-specific antibody following a single injection of the ISA 720 formulated vaccine were comparable to those obtained following two to three immunizations with alum-adsorbed ICC-1132. Peripheral blood mononuclear cells of ICC-1132/ISA 720 vaccinees proliferated and released cytokines (interleukin 2 and gamma interferon) when stimulated with recombinant P. falciparum CS protein, and CS-specific CD4+ T-cell lines were established from volunteers with high levels of antibodies to the repeat region. The promising results obtained with a single dose of ICC-1132 formulated in Montanide ISA 720 encourage further clinical development of this malaria vaccine candidate.
Analysis of protective immunity induced by immunization with irradiated sporozoites has identified the circumsporozoite (CS) protein as a major protective antigen of the infectious sporozoite stage of the Plasmodium parasite (21, 24). High levels of antibody to the immunodominant repeat region of CS protein can neutralize sporozoite infectivity and block invasion of host liver cells. In experimental systems, gamma interferon (IFN-γ) produced by CS-specific T cells inhibited development of the intracellular hepatic stages of the parasite and prevented initiation of the erythrocytic cycle responsible for clinical disease.
A number of Plasmodium falciparum CS subunit vaccines, comprised of recombinant proteins, synthetic peptides, viral vectors, or naked DNA, have undergone phase I/II trials in an effort to elicit optimal levels of antibody and cells specific for protective CS epitopes (reviewed in reference 27). Although a standard correlate of protective immunity has not yet been defined for preerythrocytic stage malaria vaccines, high antibody titers to CS repeats and IFN-γ-producing CS-specific T cells have been associated with protection in volunteers immunized with a malaria vaccine candidate designated RTS,S (33, 36, 37). RTS,S is a virus-like particle (VLP) vaccine comprised of a mixture of native hepatitis B virus surface antigen (HBsAg) and hybrid HBsAg protein containing 200 amino acids (aa) of the CS protein. In recent phase I-IIa/b studies, RTS,S elicited short-lived protective immunity in approximately 40% of vaccinated adults and children 1 to 4 years old (2, 5, 14, 35, 36). Induction of protective immunity by RTS,S required a potent adjuvant formulation, SBAS2, consisting of a combination of Salmonella enterica serovar Typhimurium monophosphoryl lipid A (MPL) and a purified saponin adjuvant (QS-21) in a proprietary oil-in-water emulsion (36).
VLPs comprised of recombinant hepatitis B core (HBc) protein also provide a promising vaccine delivery system for malaria, as well as other pathogens (23, 29-31, 32, 40). In recent preclinical studies, an Escherichia coli-expressed HBc VLP containing P. falciparum CS epitopes, designated ICC-1132, elicited high levels of humoral and cellular immunity in mice and monkeys when formulated in adjuvants suitable for human use (3, 4, 17). The ICC-1132 vaccine candidate contains the immunodominant B-cell epitope, (NANP)3, and a T-helper epitope termed T1, NANPNVDPNANP, from the conserved central repeat region of the CS protein (Fig. 1). A synthetic peptide vaccine containing only the T1 and B epitopes elicited high levels of antibody and CD4+ T cells in individuals with a limited number of HLA-DR and -DQ genotypes (22). The ICC-1132 vaccine also contains the CS T* epitope, considered to be a universal T-cell epitope, as it is restricted by a broad range of HLA class II alleles in vivo and in vitro (7, 18). A small phase I trial of a triepitope T1BT* peptide vaccine demonstrated that the T* epitope can elicit CD4+ T-helper cells in individuals of diverse genetic backgrounds (19).
FIG. 1.
(A) Schematic representation of P. falciparum CS protein showing the B-cell epitope, (NANP)3, and T1 epitope within the repeat region and the universal T* epitope in the C terminus. (B) Schematic representation of ICC-1132, showing malaria T1 and B epitopes inserted in the HBc loop region and the T* epitope at the truncated C terminus of the HBc monomer (adapted from Nature [6] with permission from the publisher).
The first phase I study to assess the safety and immunogenicity of the ICC-1132 malaria vaccine was carried out using an alum (Alhydrogel) formulation (20). Three immunizations with the highest dose (50 μg) of alum-adsorbed ICC-1132 elicited anti-CS repeat antibodies, as well as anti-HBc antibodies, in the majority of vaccinees. Cellular assays carried out in this first clinical trial demonstrated that CS-specific IFN-γ-producing cells were detectable by enzyme-linked immunospot assay in expanded peripheral blood mononuclear cells (PBMC) of several of the immunized volunteers.
ICC-1132 administered in water-in-oil adjuvants, such as Freund's adjuvant or Montanide ISA 720, was significantly more immunogenic than alum formulations in preclinical studies in mice and monkeys (3). Antirepeat antibody titers of >1 × 106 were elicited by ICC-1132 in Montanide ISA 720, while alum formulations elicited titers that were 1 to 2 log units lower. Potent adjuvants are frequently associated with reactogenicity due to their strong immunostimulatory properties. Thus, Freund's complete adjuvant, although the most potent adjuvant for many antigens, elicits unacceptable reactogenicity that precludes its use for human vaccines. In phase I studies, injections of ISA 720 alone were well tolerated (14); however, some vaccine formulations of ISA 720 were reactogenic depending on the antigen and the immunizing dose (11, 12, 16, 28, 38). In preclinical studies of ICC-1132 formulated in ISA 720, no reactogenicity was noted in mice, rabbits, or Macaca fascicularis (cynomolgous) monkeys (3; A. Birkett, unpublished). However, Macaca mulatta (rhesus) monkeys immunized with ICC-1132 in the adjuvant Montanide ISA 720 (ICC-1132/ISA 720) developed sterile abscesses at the site of injection, more frequently after booster immunization (14a). No other local or systemic reactions were noted in any of the experimental primate hosts. The present phase I trial was therefore designed to examine the safety and immunogenicity of a single immunization with 5, 20, or 50 μg ICC-1132 emulsified in Montanide ISA 720.
MATERIALS AND METHODS
Vaccine.
ICC-1132 vaccine is a virus-like particle, produced in E. coli, comprising recombinant hepatitis B core protein with strategically positioned B- and T-cell epitopes of the Plasmodium falciparum CS protein (NF 54 isolate) (3, 4, 17) (Fig. 1). Tandem T1 and B repeat sequences were inserted in the HBc loop region between amino acids 78 and 79, an optimal position for antibody production (29, 39). The CS-derived universal T* epitope was fused to the C terminus of the truncated HBc from which the nucleic acid binding region (HBc aa 150 to 183) had been deleted. The ICC-1132 vaccine was formulated in ISA 720 (Seppic S.A., France), a metabolizable oil adjuvant containing a mannide mono-oleate emulsifier, at a ratio of 70% of ISA 720 to 30% aqueous phase containing ICC-1132.
Study design.
A total of 30 healthy adult volunteers were recruited at the University of Tuebingen, Germany. The study protocol was approved by the ethics committee of the Medical Faculty of the University of Tuebingen and Program for Appropriate Technologies in Health (PATH), and written informed consent was obtained from all volunteers prior to screening for eligibility. Medical history, physical examination, and routine laboratory tests were performed to exclude subjects with evidence of renal, cardiovascular, or gastrointestinal disease, history of cancer, or past malaria infection. Serology for hepatitis B surface antigen or core antigen, hepatitis C, and human immunodeficiency virus (HIV) were used to exclude subjects with hepatitis or HIV infection. The volunteers in the study had previously received HBsAg vaccine as part of routine immunizations and had seroprotective antibody levels (>10 IU/liter).
The study was a single-blind, escalating-dose trial designed to test the safety and immunogenicity of a single injection of ICC-1132 formulated in ISA 720. Ten volunteers were randomly assigned to one of the three dose cohorts receiving 5, 20, or 50 μg vaccine. In each group, eight individuals received a single intramuscular injection with 0.5 ml ICC-1132/ISA 720, and two individuals received saline injections (placebo controls). A staged progression to each successively higher dose was carried out only after review of all safety data from the lower-dose group by a medical monitor and an independent data safety monitoring committee. After injection, volunteers remained overnight at the Clinical Trial Ward of the University Hospital of Tuebingen for a 24-h observation period for local or systemic reactions. Volunteers returned to the clinic for examination on days 2, 7, 14, and 28 and were interviewed by phone on day 4. Local and systemic adverse events were recorded daily for 14 days on preprinted diary cards. Blood samples for cellular and humoral studies were drawn prior to immunization and 14, 28, 56, 112, and 168 days after immunization.
Serological assays. (i) ELISA.
CS- and hepatitis B core-specific enzyme-linked immunosorbent assay (ELISA) titers were measured using as coating antigens ICC-1132, HBc amino acid 1 to 49 without CS inserts (HBc149), or tetrabranched peptides containing CS repeats (T1B)4 or (T*)4 sequences. Immulon-2 plates (Dynatech Laboratories, Inc., Chantilly, VA) were coated overnight with agitation at 4°C, blocked with bovine serum albumin, and incubated with twofold serum dilutions for 1 h, at 37°C. Specific antibodies were detected by reaction with peroxidase-labeled anti-human immunoglobulin G(γ heavy chain) [(IgG)(γ)] or IgM(μ) (Cappel Research Products, Durham, NC) followed by enzyme substrate H2O2/2,2′-azinobis (3-ethylbenzthiazoline-6-sulfonic acid) (ABTS) (Kirkegaard and Perry Laboratories, Inc., Gaithersburg, MD). The endpoint titer was the highest serum dilution giving an optical density greater than the mean plus 2 standard deviations, obtained using preimmune sera. Antigen-specific IgG subgroups were determined by ELISA using serum at a 1:100 dilution and peroxidase-labeled IgG1 to IgG4 subtype-specific monoclonal antibodies (Southern Biotechnology, Birmingham, AL).
(ii) Immunofluorescence antibody assay (IFA).
Multiwell slides containing air-dried P. falciparum (NF54 strain) sporozoites were incubated with twofold serum dilutions, followed by reaction with fluorescein isothiocyanate-conjugated anti-human IgG(γ) (Kirkegaard and Perry Laboratories, Inc., Gaithersburg, MD) diluted in phosphate-buffered saline-0.4% Evans blue. The endpoint titer was the highest serum dilution giving positive fluorescence as determined by two independent readers.
(iii) CSP assay.
Circumsporozoite precipitin (CSP) assays were carried out using transgenic Plasmodium berghei sporozoites expressing P. falciparum CS repeat sequences (25). Viable sporozoites were incubated for 30 min at 37°C with an equal volume of sera from ICC-1132-immunized volunteers. CSP reactions, visible by phase-contrast microscopy as a long terminal precipitin on the sporozoite, were scored on 20 individual parasites. Serum was considered positive if 2/20 sporozoites exhibited a clear CSP reaction.
Cellular assays. (i) Proliferation and cytokine assays.
CS- and hepatitis B core-specific T-cell responses were measured by proliferation using Ficoll-purified peripheral blood mononuclear cells (PBMC). Briefly, PBMC in medium (complete RPMI plus 10% human sera) were incubated in 96-well plates with or without 10-fold dilutions of ICC-1132, HBc (aa 1 to 149) or recombinant P. falciparum CS (rCS) protein. Purified E. coli-expressed murine dihydrofolate reductase (DHFR) protein served as a negative control. Tetrabranched peptides representing the T1, B, and T* epitopes were used to detect CS-specific T-cell responses. Mitogens (phytohemagglutinin [PHA] [Difco, Detroit, MI] and pokeweed mitogen [Sigma, St. Louis, MO]) and a recall antigen, tetanus toxoid (kindly provided by Wyeth Labs), were included as positive controls. After 5 days, culture wells were pulsed with 1 μCi [3H]thymidine and incubated for an additional 16- to 18-h period before harvesting and scintillation counting.
ICC-1132 stimulated proliferation of preimmune PBMC (day 0) in approximately 30% of volunteers (data not shown). Results were therefore expressed as fold increase in stimulation index (SI), calculated as postvaccination SI divided by preimmune SI. The presence of interleukin 2 in 72-h culture supernatants was measured by bioassay, based on proliferation of an IL-2-dependent T-cell line CTLL-2 (19). The concentration of IFN-γ in 5-day culture supernatants was measured by using a commercial ELISA kit (BD Biosciences Pharmingen, San Diego, CA).
(ii) TCL.
Short-term T-cell lines (TCL) were established from PBMC prior to immunization (day 0) and 14, 28, and 56 days postvaccination, as previously described (19, 22). Briefly, 1 × 106 cells/ml in complete RPMI plus 10% human serum were cultured with rCS protein (10 μg/ml) for 3 days and expanded, without further antigen stimulation, by twice weekly addition of fresh medium containing recombinant IL-2 (100 U/ml). After 3 to 4 weeks in vitro, the TCL were washed and assayed in a 3-day proliferation assay. TCL at 4 × 105/ml were incubated with 10-fold dilutions of rCS protein, malaria peptides, or DHFR control, using irradiated autologous PBMC as antigen-presenting cells. IL-2 and IFN-γ cytokine production were measured in 24- and 48-h supernatants, respectively, as described above.
RESULTS
Safety of ICC-1132/ISA 720.
ICC-1132 formulated in Montanide ISA 720 was safe and well tolerated. The majority of adverse events (74%) were graded as “mild,” 25% were rated as “moderate,” and one was graded as “severe.” The sole serious adverse event was an appendectomy occurring 81 days after injection in the 5-μg-dose group and was unrelated to vaccination. There were no withdrawals from the study.
The majority of acute local reactions consisted of pain and tenderness at the injection site, and no serious acute local reactions were noted (Table 1). No convincing pattern of dose dependency was observed. Reactions consistent with vaccination, such as injection site erythema, swelling, and induration, were noted with similar frequencies in recipients of vaccine or saline control.
TABLE 1.
Adverse events associated with ICC-1132/ISA 720
| Adverse event | No. of volunteers (%)a
|
|||
|---|---|---|---|---|
| ICC-1132/ISA 720
|
Saline (n = 6) | |||
| 5 μg (n = 8) | 20 μg (n = 8) | 50 μg (n = 8) | ||
| Local | ||||
| Tenderness | 6 (75) | 1 (13) | 5 (63) | 2 (33) |
| Injection site pain | 4 (50) | 3 (38) | 7 (88) | 1 (17) |
| Arm limitation | 1 (13) | 0 (0) | 0 (0) | 0 (0) |
| Erythema | 0 (0) | 0 (0) | 2 (25) | 2 (33) |
| Swelling | 0 (0) | 1 (13) | 0 (0) | 0 (0) |
| Induration | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lymphadenopathy | 1 (13) | 0 (0) | 2 (25) | 1 (17) |
| Systemic | ||||
| Fever (>37.5°C) | 1 (13) | 1 (13) | 0 (0) | 1 (17) |
| Headache | 4 (50) | 5 (63) | 3 (38) | 4 (67) |
| Malaise | 2 (25) | 3 (38) | 0 (0) | 0 (0) |
| Fatigue | 1 (13) | 1 (13) | 0 (0) | 0 (0) |
| Nausea | 1 (13) | 1 (13) | 1 (13) | 2 (33) |
| Diarrhea | 1 (13) | 0 (0) | 0 (0) | 0 (0) |
| URIb | 4 (50) | 2 (25) | 5 (63) | 4 (67) |
Results shown as the number of volunteers in each group experiencing immediate or systemic adverse events following a single vaccination with ICC-1132/ISA 720 or saline as a control.
URI, upper respiratory infection.
Four volunteers in the 20-μg-dose group and two volunteers in the 50-μg-dose group reported local injection site reactions that presented in a delayed manner (Table 2), similar to those previously described in vaccinees receiving an ISA 720 formulated blood-stage vaccine (28). In the ICC-1132/ISA 720 vaccinees, the delayed reactions occurred 12 to 24 days after vaccination and spontaneously resolved within 1 to 5 days with no sequelae. All of the delayed local reactions were scored as “mild” or “moderate,” with the exception of one volunteer in the 20-μg-dose group who reported pain and “severe swelling” on day 22 (resolved within 48 h). One volunteer in the 50-μg-dose group reported mild pain on days 16 and 17, which resolved and recrudesced on days 24 to 26.
TABLE 2.
Delayed local reactions associated with ICC-1132/ISA 720a
| Volunteer | Dose (μg) | Symptom | Day of onset | Day of resolution | Maximum severity |
|---|---|---|---|---|---|
| 13 | 20 | Tenderness | 16 | 21 | Moderate |
| Injection site pain | 16 | 21 | Moderate | ||
| Arm limitation | 18 | 19 | Mild | ||
| Erythema | 18 | 19 | Moderate | ||
| Induration | 18 | 19 | Moderate | ||
| 16 | 20 | Injection site pain | 12 | 14 | Mild |
| 18 | 20 | Injection site pain | 22 | 24 | Mild |
| Swelling | 22 | 24 | Severe | ||
| 20 | 20 | Tenderness | 15 | 16 | Mild |
| Injection site pain | 12 | 16 | Mild | ||
| Swelling | 12 | 14 | Moderate | ||
| 26 | 50 | Injection site pain | 16 | 17 | Mild |
| Injection site painb | 24 | 26 | Mild | ||
| 29 | 50 | Injection site pain | 22 | 24 | Mild |
| Erythema | 23 | 24 | Mild |
Symptoms experienced by volunteers >10 days after vaccination.
Symptom resolved on day 17 and recurred on day 24.
Systemic adverse events consisted mainly of headache and malaise which resolved with symptomatic treatment (Table 1). None of the systemic adverse events were categorized as serious or severe. A consistent proportion of volunteers reported upper respiratory infection symptoms during the study. The frequencies of other systemic complaints were similar in vaccinees and saline controls. The systemic symptoms did not appear to be associated with either the immediate or delayed local reactions.
One subject in the 20-μg-dose group presented with a constellation of symptoms, including hyperventilation, weakness, and dizziness on study day 7 and was reported to have two electrocardiogram (ECG) abnormalities (“QTc prolongation” and “nonspecific T wave changes”). Both events resolved on the day of onset, no action was taken, and no concomitant medications were administered. The adverse events were scored as possibly related to vaccination due to temporal association. Neither the symptoms nor ECG findings could be correlated to organic disease.
All results of biochemical analysis were normal, except for a single volunteer in the 20-μg dosage group who had mild transient elevation of liver enzymes noted on day 15. The event was scored as “possibly related” and considered not clinically significant.
Humoral immunity in ICC-1132/ISA 720 vaccinees. (i) Fine specificity of antibody response.
The vaccine was highly immunogenic, and a single immunization with 20 μg or 50 μg of ICC-1132 formulated in ISA 720 elicited IgG antibody responses to the immunogen and to HBc in 100% of the volunteers (Table 3). The seroconversion rate was dose dependent; in the 5-μg-dose group, only 63% of the vaccinees developed IgG antibodies to ICC-1132 and 38% to HBc. In the seropositive individuals, antibody titers to ICC-1132 were seven- to eightfold-higher than antibody titers to HBc, but peak titers were not significantly different in the various dosage groups.
TABLE 3.
Antibody responses in ICC-1132/ISA 720-immunized seropositive volunteers
| Dose (μg) | ICC-1132
|
HBc
|
CS repeats
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IgM
|
IgG
|
IgM
|
IgG
|
IgM
|
IgG
|
|||||||
| Pos/total (%)a | GMT (range)b | Pos/total (%) | GMT (range) | Pos/total (%) | GMT (range) | Pos/total (%) | GMT (range) | Pos/total (%) | GMT (range) | Pos/total (%) | GMT (range) | |
| 5 | 1/8 (13) | 80 | 5/8 (63) | 2,874 (160-20,480) | 1/8 (13) | 320 | 3/8 (38) | 640 | 3/8 (38) | 320 | 5/8 (63) | 844 (160-5,120) |
| 20 | 7/8 (88) | 353 (160-640) | 8/8 (100) | 5,120 (640-40,960) | 0/8 | 8/8 (100) | 761 (320-2,560) | 6/8 (75) | 285 (160-320) | 7/8 (88) | 1,050 (320-10,240) | |
| 50 | 6/8 (75) | 359 (160-640) | 8/8 (100) | 6,640 (1,280-20,480) | 1/8 (13) | 160 | 8/8 (100) | 830 (320-2,560) | 6/8 (75) | 285 (160-640) | 8/8 (100) | 905 (320-2,560) |
Results shown as number of positive vaccinees (ELISA titers ≥80) to the total number of volunteers in each group with the percentage positive in parentheses.
ELISA GMT of seropositive vaccinees were determined using sera obtained on day 56 and are shown in bold type.
At the highest dose, 100% IgG seroconversion to CS repeats was also obtained. The IgG antirepeat seroconversion rate was dose dependent, with 88% and 63% seropositivity in the 20-μg- and 5-μg-dose groups, respectively. In seropositive individuals, the peak antirepeat titers were not significantly different for different doses, as noted in the response to ICC-1132 and HBc. The CS-specific antibodies were directed against the CS repeats, with little or no antibody to the T* sequence located at the C terminus of the recombinant ICC-1132 protein (data not shown).
IgM antibodies to ICC-1132 and to CS repeats were detected in the majority of volunteers (75% to 88%) in the 20-μg- and 50-μg-dose groups (Table 3). The IgM response was dose dependent with <40% seroconversion in the in the 5-μg-dose group. Minimal IgM antibodies specific for HBc were detected in all dose groups, with 0 to 13% seroconversion.
(ii) Antibody reactivity with Plasmodium sporozoites.
The ELISA titers were highly correlated with IFA reactivity to P. falciparum sporozoites (r2 = 0.92), indicating that a single dose of ICC-1132 induced antibodies reactive with native CS protein on the sporozoite surface (Fig. 2). For the majority of volunteers, the IFA titer was within fourfold of the antirepeat ELISA titer. The peak IFA levels in seropositive volunteers in the 20-μg- and 50-μg-dose groups were not significantly different, with IFA geometric mean titers (GMT) of 580 and 761, respectively. Sera of vaccinees with high antirepeat ELISA and IFA titers induced positive circumsporozoite precipitin reactions when the sera were allowed to react with viable transgenic sporozoites expressing P. falciparum CS repeats (Fig. 2).
FIG. 2.
ELISA and IFA antibody titers in day 56 sera of volunteers receiving a single immunization with 5-μg, 20-μg, or 50-μg dose of ICC-1132/ISA 720. Asterisks indicate the two volunteers in each group injected with saline placebo. All sera were tested for CSP reactivity using viable sporozoites expressing P. falciparum CS repeats (25). CSP-positive sera (+) are indicated.
(iii) Kinetics of IgG antibody responses.
The kinetics of the anti-CS and anti-HBc IgG antibody response was followed for 6 months after the single injection of ICC-1132/ISA 720 (Fig. 3). Although the magnitude of the response to ICC-1132 was higher than the response to CS repeats or HBc, the kinetics of the antibody responses to all three antigens were similar. Peak antibody titers were observed at day 56, followed by a gradual decline in titer. The dose of vaccine did not alter the kinetics of the response with similar patterns observed for the 5-μg dose and higher doses.
FIG. 3.
Kinetics of IgG antibody response following a single injection of various doses of ICC-1132/ISA 720. The results are shown as ELISA GMT for all volunteers in each dose group using ICC-1132, HBc protein, or CS repeat peptide as the antigen in ELISA.
Remarkably, a single immunization with ICC-1132 formulated in ISA 720 induced a persistent antibody response to all three antigens that was still detectable 6 months after immunization. Anti-ICC-1132 antibodies were present on day 168 in 95% (20/21) of the seropositive volunteers and 63% (12/19) of anti-HBc seropositive volunteers in all dosage groups. Although the magnitude of the response to CS repeats was lower, the antibody response was similarly persistent. On day 168, antirepeat antibodies were still detectable in 70% (14/20) of all seropositive volunteers.
(iv) Antibody IgG subtypes.
The antigen-specific antibodies in sera of the vaccinees were predominately IgG1 and IgG3, with no IgG2 or IgG4 detected (Fig. 4). The patterns of IgG1/IgG3 responses to ICC-1132 or CS repeats were similar in each individual. Predominance of Th1-type antibodies was also noted in response to all antigens in the 5-μg-dose group (volunteer 9) and 50-μg-dose group (data not shown).
FIG. 4.
IgG subtypes in volunteers with high antibody titers in 5-μg (volunteer 9) and 20-μg dose cohorts as measured by ELISA using ICC-1132 or CS repeat peptide as the antigen. Results at 1:100 serum dilution are shown as optical density (OD), calculated as the OD in wells coated with antigen minus the OD in wells coated with bovine serum albumin. Positive-control serum (MAP #1) was from a volunteer immunized with a (T1B)4 multiple antigen peptide (MAP) vaccine (22). OD values of <0.1 were obtained with sera from saline-injected controls (data not shown).
Cellular immunity in ICC-1132/ISA 720 vaccinees. (i) PBMC proliferation and cytokine responses.
PBMC obtained at various time points following immunization were assayed for response to ICC-1132 immunogen, HBc, and rCS proteins. Optimal proliferative responses were obtained with cells from the 20-μg-dose group (Fig. 5), with lower responses in the 5-μg- and 50-μg-dose cohorts (data not shown). At one or more time points after immunization, the majority (five of eight volunteers) in the 20-μg-dose group showed positive proliferative responses to the ICC-1132 immunogen (Fig. 5A). Peak proliferation was detected in cells obtained 14 to 56 days postimmunization, depending on the individual. Low levels of IL-2 were detected in culture supernatants (data not shown). Positive ICC-1132 responses at lower levels were detectable by proliferation and/or IL-2 assays in 28% to 38% of all volunteers at 4 and 6 months postimmunization, respectively (data not shown).
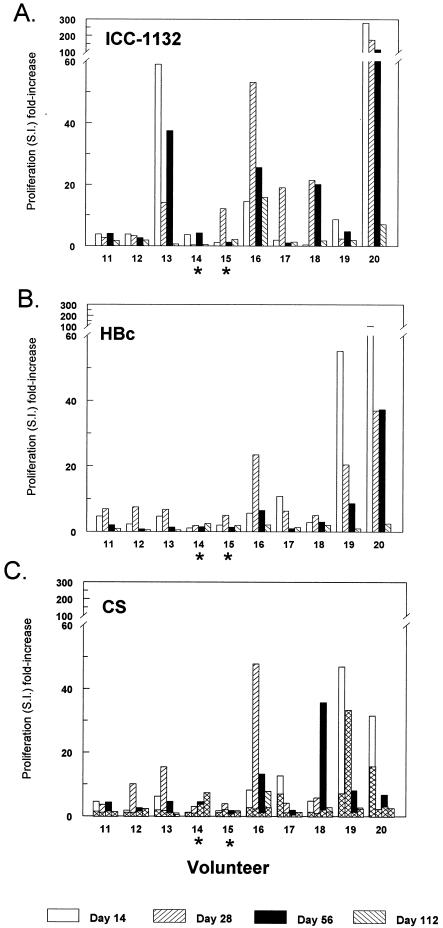
FIG. 5.
Proliferative responses of PMBC obtained 14, 28, 56 and 112 days postimmunization with 20 μg ICC-1132/ISA 720 when stimulated with ICC-1132, HBc, or rCS protein. Responses to DHFR control protein are shown as superimposed cross hatched bars in panel C. Results for each volunteer are shown as fold increase in stimulation index (SI) calculated as SI postimmunization divided by the SI at day 0. Asterisks indicate volunteers injected with saline placebo.
Although the numbers were too small for statistical analysis, there was a positive association between cellular and humoral responses to the ICC-1132 immunogen. PBMC of three of the four volunteers with high anti-ICC-1132 titers (≥104), volunteers 13, 16, and 20, gave strong proliferative responses following stimulation with ICC-1132 (Fig. 5A). Proliferation was antigen specific, as the magnitude of the response to ICC-1132 differed from the response to HBc, e.g., volunteer 13 gave high proliferative responses to ICC-1132 but not HBc (Fig. 5B).
Importantly for vaccine efficacy, the rCS protein also elicited positive proliferative responses in six of eight vaccinees in the 20-μg-dose group (Fig. 5C). These responses were CS specific, as an E. coli-expressed DHFR control protein did not stimulate PBMC from the majority of volunteers (Fig. 5C). Synthetic peptides representing the malaria T1, B, and T* epitopes contained in the ICC-1132 vaccine did not stimulate PBMC proliferation (data not shown).
As noted with ICC-1132, the majority (six of seven) of the volunteers who were seropositive for antirepeat antibodies had positive CS-specific cellular responses. The magnitude of the cellular response to rCS, however, did not predict the magnitude of the antirepeat antibody titers. Volunteer 19, who had strong CS-specific proliferation on day 14, had a peak antirepeat titer of 320. In contrast, volunteers 11 and 13 had antirepeat titers of 2,560 and 10,240, respectively, but low cellular responses to CS.
Consistent with the polarized Th1-type IgG1 and IgG3 antibody responses, IFN-γ was detected in PBMC culture supernatants following stimulation with ICC-1132 or HBc (Fig. 6A and B). The DHFR control protein did not stimulate IFN-γ production (data not shown). Incubation of PBMC with rCS also elicited IFN-γ production (Fig. 6C), indicating that parasite-specific Th-1 cells were induced by immunization with ICC-1132/ISA 720. The kinetics of the IFN-γ response was similar to that observed for the proliferative response (Fig. 6), with positive responses detected 14 to 56 days after immunization. In the 50-μg-dose group, increased proliferation and/or IFN-γ was observed in seven of eight vaccinees in response to ICC-1132, in three/eight vaccinees to rCS, and in none of the vaccinees to HBc (data not shown).
FIG. 6.
Detection of IFN-γ in culture supernatants obtained from PBMC proliferation assays described in the legend to Fig. 5. Mean proliferation SI (solid line) and IFN-γ (pg/ml) (dotted line) shown for all vaccinees in the 20-μg-dose group (closed symbols) or placebo controls (open symbols). In the vaccinees, the means ± standard errors of the means for peak responses to ICC-1132 were as follows: peak SI of 185 ± 71 and 744 ± 289 pg/ml IFN-γ; HBc peak SI of 39 ± 21 and 427 ± 231 pg/ml IFN-γ; and rCS peak SI of 40 ± 22 and 482 ± 17 pg/ml IFN-γ.
(ii) CD4+ T-cell lines specific for P. falciparum CS protein.
To examine the fine specificity of the cellular response, T-cell lines were derived by expanding PBMC with a single stimulation in vitro with rCS protein. TCL established from PBMC obtained 28 and 56 days following immunization with ICC-1132/ISA 720 proliferated and produced IL-2 and IFN-γ in response to stimulation with rCS protein (Table 4). Responses were antigen specific, as E. coli-expressed DHFR control protein did not stimulate TCL proliferation or cytokine production at any time point (data not shown). CS-specific TCL could not be established using PBMC obtained from volunteers on day 0 or from a placebo control (volunteer 14), indicating that the CS-specific TCL detected on days 28 and 56 were the result of in vivo immunization and not in vitro priming.
TABLE 4.
P. falciparum CS-specific TCL derived from ICC-1132/ISA 720 vaccinees
| Volunteer | ELISAb | TCLa
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0
|
Day 14
|
Day 28
|
Day 56
|
||||||||||
| Prol.c | IL-2d | IFN-γe | Prol. | IL-2 | IFN-γ | Prol. | IL-2 | IFN-γ | Prol. | IL-2 | IFN-γ | ||
| 11 | 2,560 | 1 | 1 | 22 | 1 | 3 | 0 | 79 | 54 | 274 | 21 | 70 | 447 |
| 12 | 320 | 2 | 2 | 0 | 1 | 1 | 0 | 6 | 23 | 152 | 15 | 27 | 508 |
| 13 | 10,240 | 2 | 1 | 20 | 1 | 1 | 0 | 165 | 523 | 2,298 | 21 | 20 | 444 |
| 14 | <80 | 1 | 1 | 12 | 5 | 3 | 52 | 1 | 1 | 14 | 9 | 4 | 140 |
TCL were established from PBMC obtained on days 0, 14, 28, and 56 postimmunization. Volunteer 14 received placebo saline injection. Values that were significantly higher than the value for volunteer 14 (control) are shown in bold type.
Peak CS repeat ELISA titer in sera obtained 56 days postimmunization.
SI in 3-day proliferation (Prol.) assay in wells stimulated with or without rCS (10 μg/ml). For all TCL, the mean value in triplicate wells without antigen was 640 ± 426 cpm. DHFR control protein elicited an SI of <5 for all TCL at all time points.
SI in IL-2 bioassay using 24-h culture supernatants from the proliferation assay. For all TCL, supernatants from wells without antigen gave a mean value of 349 ± 201 cpm.
IFN-γ (in pg/ml) in 48-h culture supernatants.
The fine specificity of the CS-specific T cells was determined using peptides representing the T1, B, and T* epitopes to stimulate TCL from a second group of volunteers (Table 5). Consistent with previous results, CS-specific TCL were established from cells of all seropositive volunteers, but not a seronegative vaccinee (volunteer 17) or placebo control (volunteer 15). CS-specific T cells were not detected in preimmune PBMC (day 0) or at 14 days postimmunization (data not shown). The TCL established on day 28 from volunteers 18 and 20 recognized the T* peptide, in addition to rCS protein. Volunteer 20 TCL from day 56 also proliferated and produced IL-2 when stimulated with T* peptide. The T1 and B peptides and DHFR control protein did not stimulate any of the TCL (data not shown).
TABLE 5.
Fine specificity of P. falciparum CS-specific TCL
| Volunteer | ELISAb | TCLa
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0
|
Day 28
|
Day 56
|
|||||||||||
| rCS
|
T*
|
rCS
|
T*
|
rCS
|
T*
|
||||||||
| Prol.c | IL-2c | Prol. | IL-2 | Prol. | IL-2 | Prol. | IL-2 | Prol. | IL-2 | Prol. | IL-2 | ||
| 15 | <80 | 13 | 2 | 3 | 1 | 6 | 2 | 1 | 1 | 16 | 1 | 1 | 1 |
| 16 | 2,560 | 2 | 1 | 1 | 1 | 68 | 79 | 1 | 1 | 59 | 106 | 1 | 1 |
| 17 | <80 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 4 | 1 | 1 | 1 |
| 18 | 320 | 6 | 1 | 1 | 1 | 42 | 108 | 17 | 50 | 8 | 1 | 1 | 1 |
| 19 | 320 | 13 | 6 | 2 | 1 | 27 | 15 | 1 | 1 | 19 | 8 | 1 | 1 |
| 20 | 640 | 5 | 1 | 2 | 2 | 32 | 36 | 24 | 71 | 26 | 160 | 37 | 364 |
TCL were established from PBMC obtained on days 0, 14, 28, and 56 postimmunization. Volunteer 15 (control) received only saline injection. Results for day 14 TCL proliferation and IL-2 responses to rCS were similar to day 0 TCL (<twofold increase) (data not shown). Values that were significantly higher than the value for volunteer 15 (control) are shown in bold type.
Peak CS repeat ELISA titer in sera obtained 56 days postimmunization.
SI in 3-day proliferation (Prol.) assay or in IL-2 bioassay in wells stimulated with rCS (10 μg/ml) or T* peptide (10 μg/ml). For all TCL, the mean value in triplicate wells without antigen was 572 ± 328 cpm in proliferation assay and 454 ± 193 cpm in IL-2 bioassay. TCL stimulated with DHFR control protein gave an SI of <5 for all time points (data not shown).
DISCUSSION
The present phase I trial demonstrates that ICC-1132 formulated in the water-in-oil adjuvant, ISA 720, was safe, well tolerated, and highly immunogenic. A single immunization with 20 μg or 50 μg ICC-1132/ISA 720 elicited IgG antibodies specific for CS repeats in 88% and 100% of the vaccinees. All of the vaccinees in these groups also seroconverted to ICC-1132 and HBc protein. The IgG antibody response was dose dependent, with lower seroconversion in the 5-μg-dosage group to CS (63%), ICC-1132 (63%), and HBc (38%).
The anti-CS repeat titers obtained following a single dose of ICC-1132/ISA 720 (Table 3) were comparable in magnitude to those obtained following two or three injections of alum-adsorbed ICC-1132 (GMT of 538 and 508 in the 20-μg- and 50-μg-dose groups, respectively) (20). Moreover, a single dose of the ISA 720 vaccine formulation elicited antirepeat antibody responses in 88% and 100% of vaccinees in the 20-μg- and 50-μg-dose group, compared to 40% and 75% of vaccinees receiving three doses of alum-adsorbed ICC-1132.
The ICC-1132/ISA 720 vaccine formulation also elicited 100% seroconversion to HBc, while a single dose of alum-adsorbed ICC-1132 elicited positive anticore responses in only one vaccinee. Since the immunodominant core epitope is disrupted by insertion of the CS repeats, the more potent ISA 720 adjuvant presumably enhanced antibody responses to minor or neo-epitopes in HBc. The presence of antibodies to only minor core protein epitopes is consistent with the low or negative results for sera from all vaccinees measured using a commercial anticore antibody assay (Corzyme; Abbott Laboratories) (data not shown).
There was a positive correlation between CS repeat ELISA titers and reactivity with P. falciparum sporozoites in sera of the ICC-1132/ISA 720 vaccinees (Fig. 2), consistent with the fine specificity of antibodies elicited by the ICC-1132/alum formulation and other CS repeat-based malaria vaccines (19, 20, 22). To be effective, vaccine-induced antibodies should react not only with repeat peptides and air-dried parasites but also with viable sporozoites, as binding of antibodies to CS on the surfaces of viable sporozoites leads to loss of sporozoite motility and infectivity (24, 34). In the present studies, a single immunization with ICC-1132/ISA 720 elicited antibodies that induced a positive CSP reaction (Fig. 2), indicating that the antibodies were of sufficient avidity/affinity to cross-link surface CS protein on viable parasites.
Consistent with alum-adsorbed ICC-1132 (20), the ICC-1132/ISA 720 formulation induced predominantly IgG1 and IgG3 antibody subtypes, suggesting that the ability of ICC-1132 particles to elicit Th1-type responses is not adjuvant dependent. This finding in humans contrasts with murine studies in which all IgG subtypes were detected following immunization with ICC-1132 in various adjuvants or with HBc VLP containing rodent malaria CS epitopes (3, 31).
The strong immunogenicity of HBc particles has been attributed to their ability to bind to B cells, leading to T-cell-independent antibody responses and enhanced B-cell antigen presentation to naïve T cells (17). Purified human B cells, when transferred into SCID/NOD mice, produced anti-HBc IgM antibodies in response to stimulation with HBc particles (7a). Several of the volunteers had positive anti-HBc antibodies or high levels of nonspecific proliferation to ICC-1132 on day 0. However, no correlation was found between day 0 responses and immune responses to the vaccine in these individuals. Moreover, only low IgM responses were noted in all vaccinees immunized with ICC-1132 formulated in ISA 720 (Table 3) or alum (20). These findings, combined with the strong IgG1 and IgG3 responses, which are characteristic of T-cell-dependent antibody responses to protein antigens, suggest that ICC-1132 does not function as a T-cell-independent B-cell antigen in humans.
The strong bias toward Th1-type antibodies in humans may be a unique property of virus-like particles based on HBc protein. In phase I trials of RTS,S malaria vaccine composed of HBsAg VLP, predominantly IgG1 and IgG2 antibodies, without significant IgG3 and IgG4, were detected (36). Similarly, antirepeat antibodies of all subtypes were elicited in phase I trials of a synthetic peptide malaria vaccine containing the same T1, B, and T* epitopes as contained in ICC-1132 (19, 22).
While antirepeat monoclonal antibodies of all isotypes have been shown to be protective in experimental models (1), Th1-type antibodies may provide advantages in vivo. IgG1 and IgG3, but not Th2-type IgG2 or IgG4, are strong opsonizing antibodies that can potentially enhance phagocytosis of sporozoites. The production of IFN-γ by Th1 cells not only provides a B-cell differentiation factor for IgG1 and IgG3 subtypes but also activates macrophages to enhance phagocytosis of opsonized sporozoites (9, 33).
The efficacy of preerythrocytic malaria vaccines may be further enhanced by the presence of parasite-specific CD4+ Th1 cells, since IFN-γ is a potent inhibitor of the Plasmodium intracellular hepatic stages (10, 21). In murine models, CD4+ T-cell IFN-γ-dependent protective immunity against sporozoite challenge can be elicited by malaria subunit vaccines (8, 41). In humans, IFN-γ production by CS-specific CD4+ T cells has been correlated with resistance to P. falciparum sporozoite challenge in vaccinated and naturally infected individuals (26, 37). In the present study, PBMC and TCL derived from volunteers immunized with ICC-1132/ISA 720 produced IFN-γ following stimulation with rCS protein (Fig. 5 and Table 4). CD4+ T cells that recognized the T* epitope, but not the T1 or B epitope, could also be detected in several volunteers (Table 5).
The immunized volunteers also developed HBc-specific cellular responses (Fig. 5B). The presence of HBc-specific T cells has been associated with protection against hepatitis B virus (HBV) challenge in animal models and with recovery from chronic HBV infection in humans (13, 15, 30). These findings raise the hope that the antiviral and antiplasmodial responses induced by ICC-1132 may prove beneficial in areas where both malaria and HBV infections are endemic.
Studies with malaria subunit vaccines, as well as vaccines for other infectious diseases, have shown that adjuvant plays a critical role in immunogenicity and protective immunity. Unlike vaccines based on attenuated or inactivated pathogens, highly purified vaccines lack intrinsic immunostimulatory properties necessary to stimulate innate immune responses required for development of strong antigen-specific adaptive immunity. The use of potent adjuvants in vaccine formulations increases immunogenicity but can be associated with increased reactogenicity (28, 36). The single immunization with ICC-1132 in ISA 720 was well tolerated; however, booster immunizations will be required to obtain optimal levels of parasite-specific immunity. The results of a recent phase I/II trial demonstrated that the low antibody titers induced by a single immunization with ICC 1132/ISA 720 were not protective (40a). Antirepeat titers an order of magnitude higher have been obtained following multiple immunizations with RTS,S and synthetic peptide malaria vaccines (14, 22). Booster inoculations with lower doses of ICC-1132/ISA 720 or with alum-adsorbed ICC-1132 can enhance immunogenicity without increasing reactogenicity in Rhesus monkeys (14a). These findings suggest that optimal ICC-1132 formulations can be defined that minimize reactogenicity of potent adjuvants while enhancing immunogenicity.
The present phase I trial demonstrates that the immunogenicity of a single dose of a core VLP malaria vaccine administered in a potent adjuvant, Montanide ISA 720, is comparable to the immunogenicity of multiple immunizations with alum-adsorbed vaccine. The encouraging results obtained in volunteers primed with ICC-1132/ISA 720 raises the expectation that booster immunizations will increase the magnitude of CS-specific responses and concomitant efficacy of malaria vaccines based on hepatitis virus core VLP.
Acknowledgments
We thank the volunteers who participated in the phase I trial and Victor Nussenzweig for review of the manuscript. Diana Barrios Rodriquez and Rita Altszuler are acknowledged for providing expert technical assistance. IL-2 was obtained from M. Gately through NIH AIDS Research and Reference Reagent Program.
Studies at New York University were supported by NIAID RO1 AI045138 and research funding from Apovia, Inc. The clinical trial at University of Tuebingen was supported by the Malaria Vaccine Initiative, PATH, Rockville, MD.
The phase I trial was carried out jointly at University of Tuebingen (P.G.K.) and New York University (E.H.N.).
Editor: J. D. Clements
REFERENCES
- 1.Ak, M., J. H. Bower, S. L. Hoffman, M. Sedegah, A. Lees, M. Carter, R. L. Beaudoin, and Y. Charoenvit. 1993. Monoclonal antibodies of three different immunoglobulin G isotypes produced by immunization with a synthetic peptide or native protein protect mice against challenge with Plasmodium yoelii sporozoites. Infect. Immun. 61:2493-2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alonso, P. L., J. Sacarlal, J. J. Aponte, A. Leach, E. Macete, J. Milman, I. Mandomando, B. Spiessens, C. Guinovart, M. Espasa, Q. Bassat, P. Aide, O. Ofori-Anyinam, M. M. Navia, S. Corachan, M. Ceuppens, M. C. Dubois, M. A. Demoitie, F. Dubovsky, C. Menendez, N. Tornieporth, W. R. Ballou, R. Thompson, and J. Cohen. 2004. Efficacy of the RTS,S/AS02A vaccine against Plasmodium falciparum infection and disease in young African children: randomised controlled trial. Lancet 364:1411-1420. [DOI] [PubMed] [Google Scholar]
- 3.Birkett, A., K. Lyons, A. Schmidt, D. Boyd, G. A. Oliveira, A. Siddique, R. Nussenzweig, J. M. Calvo-Calle, and E. Nardin. 2002. A modified hepatitis B virus core particle containing multiple epitopes of the Plasmodium falciparum circumsporozoite protein provides a highly immunogenic malaria vaccine in preclinical analyses in rodent and primate hosts. Infect. Immun. 70:6860-6870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birkett, A., B. Thornton, D. Milich, G. A. Oliveira, A. Siddique, R. Nussenzweig, J. M. Calvo-Calle, and E. H. Nardin. 2001. Hepatitis B virus core antigen particles containing minimal T and B cell epitopes of Plasmodium falciparum CS protein elicit high levels of malaria specific immune responses in mice and non-human primates. Am. J. Trop. Med. Hyg. 65:258. [Google Scholar]
- 5.Bojang, K. A., P. J. Milligan, M. Pinder, L. Vigneron, A. Alloueche, K. E. Kester, W. R. Ballou, D. J. Conway, W. H. Reece, P. Gothard, L. Yamuah, M. Delchambre, G. Voss, B. M. Greenwood, A. Hill, K. P. McAdam, N. Tornieporth, J. D. Cohen, and T. Doherty. 2001. Efficacy of RTS,S/AS02 malaria vaccine against Plasmodium falciparum infection in semi-immune adult men in The Gambia: a randomised trial. Lancet 358:1927-1934. [DOI] [PubMed] [Google Scholar]
- 6.Bottcher, B., S. A. Wynne, and R. A. Crowther. 1997. Determination of the fold of the core protein of hepatitis B virus by electron cryomicroscopy. Nature 386:88-91. [DOI] [PubMed] [Google Scholar]
- 7.Calvo-Calle, J. M., J. Hammer, F. Sinigaglia, P. Clavijo, Z. R. Moya-Castro, and E. H. Nardin. 1997. Binding of malaria T cell epitopes to DR and DQ molecules in vitro correlates with immunogenicity in vivo: identification of a universal T cell epitope in the Plasmodium falciparum circumsporozoite protein. J. Immunol. 159:1362-1373. [PubMed] [Google Scholar]
- 7a.Cao, T., U. Lazdina, I. Desombere, P. Vanlandschoot, D. R. Milich, M. Sallberg, and G. Leroux-Roels. 2001. Hepatitis B virus core antigen binds and activates naïve human B cells in vivo: studies with a human PBL-NOD/SCID mouse model. J. Virol. 75:6359-6366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charoenvit, Y., V. F. Majam, G. Corradin, J. B. Sacci, Jr., R. Wang, D. L. Doolan, T. R. Jones, E. Abot, M. E. Patarroyo, F. Guzman, and S. L. Hoffman. 1999. CD4+ T-cell- and gamma interferon-dependent protection against murine malaria by immunization with linear synthetic peptides from a Plasmodium yoelii 17-kilodalton hepatocyte erythrocyte protein. Infect. Immun. 67:5604-5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Danforth, H. D., M. Aikawa, A. H. Cochrane, and R. S. Nussenzweig. 1980. Sporozoites of mammalian malaria: attachment to, interiorization and fate within macrophages. J. Protozool. 27:193-202. [DOI] [PubMed] [Google Scholar]
- 10.Ferreira, A., L. Schofield, V. Enea, H. Schellekens, P. van der Meide, W. E. Collins, R. S. Nussenzweig, and V. Nussenzweig. 1986. Inhibition of development of exoerythrocytic forms of malaria parasites by gamma-interferon. Science 232:881-884. [DOI] [PubMed] [Google Scholar]
- 11.Genton, B., F. Al-Yaman, R. Anders, A. Saul, G. Brown, D. Pye, D. O. Irving, W. R. Briggs, A. Mai, M. Ginny, T. Adiguma, L. Rare, A. Giddy, R. Reber-Liske, D. Stuerchler, and M. P. Alpers. 2000. Safety and immunogenicity of a three-component blood-stage malaria vaccine in adults living in an endemic area of Papua New Guinea. Vaccine 18:2504-2511. [DOI] [PubMed] [Google Scholar]
- 12.Genton, B., F. Al-Yaman, I. Betuela, R. F. Anders, A. Saul, K. Baea, M. Mellombo, J. Taraika, G. V. Brown, D. Pye, D. O. Irving, I. Felger, H. P. Beck, T. A. Smith, and M. P. Alpers. 2003. Safety and immunogenicity of a three-component blood-stage malaria vaccine (MSP1, MSP2, RESA) against Plasmodium falciparum in Papua New Guinean children. Vaccine 22:30-41. [DOI] [PubMed] [Google Scholar]
- 13.Iwarson, S., E. Tabor, H. C. Thomas, P. Snoy, and R. J. Gerety. 1985. Protection against hepatitis B virus infection by immunization with hepatitis B core antigen. Gastroenterology 88:763-767. [DOI] [PubMed] [Google Scholar]
- 14.Kester, K. E., D. A. McKinney, N. Tornieporth, C. F. Ockenhouse, D. G. Heppner, T. Hall, U. Krzych, M. Delchambre, G. Voss, M. G. Dowler, J. Palensky, J. Wittes, J. Cohen, and W. R. Ballou. 2001. Efficacy of recombinant circumsporozoite protein vaccine regimens against experimental Plasmodium falciparum malaria. J. Infect. Dis. 183:640-647. [DOI] [PubMed] [Google Scholar]
- 14a.Langermans, J. A. M., S. Schmidt, R. A. W. Vervenne, A. J. Birkett, J. M. Calvo-Calle, M. Hensmann, G. B. Thornton, F. Dubovsky, H. Weiler, E. Nardin, and A. W. Thomas. 2005. Effect of adjuvant on reactogenicity and long-term immunogenicity of the malaria vaccine ICC-1132 in macaques. Vaccine, in press. [DOI] [PubMed]
- 15.Lau, G. K., D. Suri, R. Liang, E. I. Rigopoulou, M. G. Thomas, I. Mullerova, A. Nanji, S. T. Yuen, R. Williams, and N. V. Naoumov. 2002. Resolution of chronic hepatitis B and anti-HBs seroconversion in humans by adoptive transfer of immunity to hepatitis B core antigen. Gastroenterology 122:614-624. [DOI] [PubMed] [Google Scholar]
- 16.Lopez, J. A., C. Weilenman, R. Audran, M. A. Roggero, A. Bonelo, J. M. Tiercy, F. Spertini, and G. Corradin. 2001. A synthetic malaria vaccine elicits a potent CD8+ and CD4+ T lymphocyte immune response in humans. Implications for vaccination strategies. Eur. J. Immunol. 31:1989-1998. [DOI] [PubMed] [Google Scholar]
- 17.Milich, D. R., J. Hughes, J. Jones, M. Sallberg, and T. R. Phillips. 2001. Conversion of poorly immunogenic malaria repeat sequences into a highly immunogenic vaccine candidate. Vaccine 20:771-788. [DOI] [PubMed] [Google Scholar]
- 18.Moreno, A., P. Clavijo, R. Edelman, J. Davis, M. Sztein, F. Sinigaglia, and E. Nardin. 1993. CD4+ T cell clones obtained from Plasmodium falciparum sporozoite-immunized volunteers recognize polymorphic sequences of the circumsporozoite protein. J. Immunol. 151:489-499. [PubMed] [Google Scholar]
- 19.Nardin, E. H., J. M. Calvo-Calle, G. A. Oliveira, R. S. Nussenzweig, M. Schneider, J. M. Tiercy, L. Loutan, D. Hochstrasser, and K. Rose. 2001. A totally synthetic polyoxime malaria vaccine containing Plasmodium falciparum B cell and universal T cell epitopes elicits immune responses in volunteers of diverse HLA types. J. Immunol. 166:481-489. [DOI] [PubMed] [Google Scholar]
- 20.Nardin, E. H., G. A. Oliveira, J. M. Calvo-Calle, K. Wetzel, C. Maier, A. J. Birkett, P. Sarpotdar, M. L. Corado, G. B. Thornton, and A. Schmidt. 2004. Phase I testing of malaria vaccine composed of hepatitis B virus core particles expressing Plasmodium falciparum circumsporozoite epitopes. Infect. Immun. 72:6519-6527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nardin, E. H., and R. S. Nussenzweig. 1993. T cell responses to pre-erythrocytic stages of malaria: role in protection and vaccine development. Annu. Rev. Immunol. 11:687-727. [DOI] [PubMed] [Google Scholar]
- 22.Nardin, E. H., G. A. Oliveira, J. M. Calvo-Calle, Z. R. Castro, R. S. Nussenzweig, B. Schmeckpeper, B. F. Hall, C. Diggs, S. Bodison, and R. Edelman. 2000. Synthetic peptide malaria vaccine elicits high levels of antibodies in vaccinees of defined HLA genotypes. J. Infect. Dis. 182:1486-1496. [DOI] [PubMed] [Google Scholar]
- 23.Noad, R., and P. Roy. 2003. Virus-like particles as immunogens. Trends Microbiol. 11:438-444. [DOI] [PubMed] [Google Scholar]
- 24.Nussenzweig, V., and R. S. Nussenzweig. 1989. Rationale for the development of an engineered sporozoite malaria vaccine. Adv. Immunol. 45:283-334. [DOI] [PubMed] [Google Scholar]
- 25.Persson, C., G. A. Oliveira, A. A. Sultan, P. Bhanot, V. Nussenzweig, and E. Nardin. 2002. Cutting edge: a new tool to evaluate human pre-erythrocytic malaria vaccines: rodent parasites bearing a hybrid Plasmodium falciparum circumsporozoite protein. J. Immunol. 169:6681-6685. [DOI] [PubMed] [Google Scholar]
- 26.Reece, W. H., M. Pinder, P. K. Gothard, P. Milligan, K. Bojang, T. Doherty, M. Plebanski, P. Akinwunmi, S. Everaere, K. R. Watkins, G. Voss, N. Tornieporth, A. Alloueche, B. M. Greenwood, K. E. Kester, K. P. McAdam, J. Cohen, and A. V. Hill. 2004. A CD4+ T-cell immune response to a conserved epitope in the circumsporozoite protein correlates with protection from natural Plasmodium falciparum infection and disease. Nat. Med. 10:406-410. [DOI] [PubMed] [Google Scholar]
- 27.Richie, T. L., and A. Saul. 2002. Progress and challenges for malaria vaccines. Nature 415:694-701. [DOI] [PubMed] [Google Scholar]
- 28.Saul, A., G. Lawrence, A. Smillie, C. M. Rzepczyk, C. Reed, D. Taylor, K. Anderson, A. Stowers, R. Kemp, A. Allworth, R. F. Anders, G. V. Brown, D. Pye, P. Schoofs, D. O. Irving, S. L. Dyer, G. C. Woodrow, W. R. Briggs, R. Reber, and D. Sturchler. 1999. Human phase I vaccine trials of 3 recombinant asexual stage malaria antigens with Montanide ISA720 adjuvant. Vaccine 17:3145-3159. [DOI] [PubMed] [Google Scholar]
- 29.Schodel, F., A. M. Moriarty, D. L. Peterson, J. A. Zheng, J. L. Hughes, H. Will, D. J. Leturcq, J. S. McGee, and D. R. Milich. 1992. The position of heterologous epitopes inserted in hepatitis B virus core particles determines their immunogenicity. J. Virol. 66:106-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schodel, F., G. Neckermann, D. Peterson, K. Fuchs, S. Fuller, H. Will, and M. Roggendorf. 1993. Immunization with recombinant woodchuck hepatitis virus nucleocapsid antigen or hepatitis B virus nucleocapsid antigen protects woodchucks from woodchuck hepatitis virus infection. Vaccine 11:624-628. [DOI] [PubMed] [Google Scholar]
- 31.Schodel, F., D. Peterson, D. R. Milich, Y. Charoenvit, J. Sadoff, and R. Wirtz. 1997. Immunization with hybrid hepatitis B virus core particles carrying circumsporozoite antigen epitopes protects mice against Plasmodium yoelii challenge. Behring Inst. Mitt. 98:114-119. [PubMed] [Google Scholar]
- 32.Schodel, F., R. Wirtz, D. Peterson, J. Hughes, R. Warren, J. Sadoff, and D. Milich. 1994. Immunity to malaria elicited by hybrid hepatitis B virus core particles carrying circumsporozoite protein epitopes. J. Exp. Med. 180:1037-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwenk, R., L. V. Asher, I. Chalom, D. Lanar, P. Sun, K. White, D. Keil, K. E. Kester, J. Stoute, D. G. Heppner, and U. Krzych. 2003. Opsonization by antigen-specific antibodies as a mechanism of protective immunity induced by Plasmodium falciparum circumsporozoite protein-based vaccine. Parasite Immunol. 25:17-25. [DOI] [PubMed] [Google Scholar]
- 34.Stewart, M. J., R. J. Nawrot, S. Schulman, and J. P. Vanderberg. 1986. Plasmodium berghei sporozoite invasion is blocked in vitro by sporozoite-immobilizing antibodies. Infect. Immun. 51:859-864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stoute, J. A., K. E. Kester, U. Krzych, B. T. Wellde, T. Hall, K. White, G. Glenn, C. F. Ockenhouse, N. Garcon, R. Schwenk, D. E. Lanar, P. Sun, P. Momin, R. A. Wirtz, C. Golenda, M. Slaoui, G. Wortmann, C. Holland, M. Dowler, J. Cohen, and W. R. Ballou. 1998. Long-term efficacy and immune responses following immunization with the RTS,S malaria vaccine. J. Infect. Dis. 178:1139-1144. [DOI] [PubMed] [Google Scholar]
- 36.Stoute, J. A., M. Slaoui, D. G. Heppner, P. Momin, K. E. Kester, P. Desmons, B. T. Wellde, N. Garcon, U. Krzych, M. Marchand, W. R. Ballou, and J. D. Cohen for the RTS,S Malaria Vaccine Evaluation Group. 1997. A preliminary evaluation of a recombinant circumsporozoite protein vaccine against Plasmodium falciparum malaria. N. Engl. J. Med. 336:86-91. [DOI] [PubMed] [Google Scholar]
- 37.Sun, P., R. Schwenk, K. White, J. A. Stoute, J. Cohen, W. R. Ballou, G. Voss, K. E. Kester, D. G. Heppner, and U. Krzych. 2003. Protective immunity induced with malaria vaccine, RTS,S, is linked to Plasmodium falciparum circumsporozoite protein-specific CD4+ and CD8+ T cells producing IFN-gamma. J. Immunol. 171:6961-6967. [DOI] [PubMed] [Google Scholar]
- 38.Toledo, H., A. Baly, O. Castro, S. Resik, J. Laferte, F. Rolo, L. Navea, L. Lobaina, O. Cruz, J. Miguez, T. Serrano, B. Sierra, L. Perez, M. E. Ricardo, M. Dubed, A. L. Lubian, M. Blanco, J. C. Millan, A. Ortega, E. Iglesias, E. Penton, Z. Martin, J. Perez, M. Diaz, and C. A. Duarte. 2001. A phase I clinical trial of a multi-epitope polypeptide TAB9 combined with Montanide ISA 720 adjuvant in non-HIV-1 infected human volunteers. Vaccine 19:4328-4336. [DOI] [PubMed] [Google Scholar]
- 39.Ulrich, R., G. P. Borisova, E. Gren, I. Berzin, P. Pumpen, R. Eckert, V. Ose, H. Siakkou, E. J. Gren, R. von Baehr, et al. 1992. Immunogenicity of recombinant core particles of hepatitis B virus containing epitopes of human immunodeficiency virus 1 core antigen. Arch. Virol. 126:321-328. [DOI] [PubMed] [Google Scholar]
- 40.Ulrich, R., M. Nassal, H. Meisel, and D. H. Kruger. 1998. Core particles of hepatitis B virus as carrier for foreign epitopes. Adv. Virus Res. 50:141-182. [DOI] [PubMed] [Google Scholar]
- 40a.Walther, M., S. Dunachie, S. Keating, J. M. Vuola, T. Berthoud, A. Schmidt, C. Maier, L. Andrews, R. F. Andersen, S. Gilbert, I. Poulton, D. Webster, F. Dubovsky, E. Tierney, P. Sarpotdar, S. Correa, A. Huntcooke, G. Butcher, J. Willimas, R. E. Sinden, G. B. Thornton, and A. V. S. Hill. 2005. Safety, immunogenicity and efficacy of a pre-erythrocytic malaria candidate vaccine, ICC-1132 formulated in Seppic ISA 720. Vaccine 23:857-864. [DOI] [PubMed] [Google Scholar]
- 41.Wang, R., Y. Charoenvit, G. Corradin, P. De La Vega, E. D. Franke, and S. L. Hoffman. 1996. Protection against malaria by Plasmodium yoelii sporozoite surface protein 2 linear peptide induction of CD4+ T cell- and IFN-gamma-dependent elimination of infected hepatocytes. J. Immunol. 157:4061-4067. [PubMed] [Google Scholar]