Abstract
Background
Management of thalassemia major requires patients to have life-long access to a treatment regimen of regular blood transfusions coupled with iron chelation therapy. The objective of this study was to investigate patients' reasons for missing iron chelation therapy with desferrioxamine, and the support to sustain life-long adherence to treatment.
Methods
From October 1999 to May 2000 a survey of patients with thalassemia major was conducted in ten countries: Cyprus, Egypt, Greece, Hong Kong, India, Iran, Italy, Jordan, Taiwan, and the United States.
Results
1,888 questionnaires (65%) were returned. Most patients (1,573) used desferrioxamine, and 79% administered a dose at least 4 days a week. Inaccessibility of the drug was a common reason for missing a dose in India (51%), and in Iran (25%), whereas, in any other country, it was a reason for less than 17% of patients. Overall, 58% reported reasons for missing a dose related to their beliefs or feelings about the medication, and 42% drug-related side effects.
Conclusion
Many patients miss doses of desferrioxamine and an opportunity remains to develop interventions that provide more support to sustain use of desferrioxamine.
Background
Management of thalassemia major requires patients to have life-long access to a treatment regimen of regular blood transfusions coupled with iron chelation therapy [1,2]. Adequate chelation can be achieved by regular use of desferrioxamine infusions, which has been shown to be critical for long-term disease-free survival – reducing the risk of both iron overload and the associated life threatening complications [3,4]. Generally, regular blood transfusions and iron chelation treatment with desferrioxamine are initiated early in life; therefore, the patients and their families have to sustain regular treatment throughout their childhood, adolescent, and adult years.
Many patients and their families find it difficult to sustain compliance with chronic treatment regimens for other life threatening diseases that arise during childhood or adolescence, such as bone marrow or renal transplantations [5-7]. Patients receiving regular blood transfusions but administering less than two-thirds of the recommended desferrioxamine dose are known to increase their risk of developing complications later in life as a result of accumulating iron [8,9]. Consequently, a commitment to life-long adherence to regular administration of desferrioxamine is key to the long-term health of patients. To date research into alternative iron chelators has resulted in the marketing of one alternative agent, deferiprone. Desferrioxamine remains the mainstay of treatment, however, as there are concerns about the relative long-term efficacy and safety of deferiprone [10].
This survey was designed to collect data on the current patterns of desferrioxamine use by patients in ten countries: Cyprus, Egypt, Greece, Hong Kong, India, Iran, Italy, Jordan, Taiwan, and the United States. Patients were asked about the frequency of administration of desferrioxamine each week and their reasons for missing doses. In addition, this survey provided information about the support currently available to patients and their families to continue with this life saving, but complex, treatment regimen.
Methods
Questionnaires
Questionnaires were developed in collaboration with experts in the treatment of thalassemia and specifically designed to be self-administered by patients or, for children younger than 14 years old, by their caregivers. The questionnaires were distributed and returned by mail. The questionnaire distributed in India and the US was in English. For the remaining countries, it was translated by native speakers into Greek, Italian, Arabic, Farsi, or Chinese, as appropriate. The initial translations were back translated and corrections made accordingly. In the pilot study, translated questionnaires were completed by patients or their caregivers and their feedback was used to improve the design of the final questionnaire.
Data Collection
The survey was conducted in ten countries: Cyprus (CY), Egypt (EG), Greece (GR), Hong Kong (HK), India (IN), Iran (IR), Italy (IT), Jordan (JO), Taiwan (TA), and the United States (US). In each country, the Thalassemia International Federation (TIF) coordinators had access to the local patient organization membership lists. The coordinators randomly selected patients from these lists and distributed to them a copy of the patient and caregiver questionnaires. To ensure that the patients were randomly selected from the membership, the coordinators divided the total number of current members by the number of questionnaires, and then selected patients from their list at this interval. Patients or caregivers were asked to return the completed questionnaires to the coordinators by mail in the envelope provided (local postage was prepaid). Each questionnaire had a unique identifier code but did not include a patient's name; consequently, all the responses were anonymous. No letters were sent to ask the non-responders to complete the questionnaire and no remuneration was extended to participants for returning the questionnaire to the TIF coordinators.
Three hundred questionnaires were dispatched to each country between October 1999 and January 2000, except in Greece where two hundred were distributed. All responses returned by May 31, 2000 were translated, where necessary, and all patients prescribed desferrioxamine were included in these analyses (Table 1).
Table 1.
Response rates by country and proportions of the patients prescribed desferrioxamine from each country
| Country | CY | EG | GR | HK | IN | IR | IT | JO | TA | US | Total |
| Membership | 636 | 2,801 | 922 | 334 | 823 | 6,810 | 840 | 360 | 302 | 310 | 14,138 |
| Questionnaires dispatched | 300 | 300 | 200 | 300 | 300 | 300 | 300 | 300 | 300 | 300 | 2,900 |
| Questionnaires completed | 275 | 199 | 118 | 159 | 235 | 215 | 147 | 232 | 231 | 77 | 1,888 |
| Response rate (%) | 92 | 66 | 59 | 53 | 78 | 72 | 49 | 77 | 77 | 26 | 65 |
| Desferrioxamine use, N (%) | 267 (97) | 120 (60) | 112 (95) | 147 (93) | 128 (55) | 200 (93) | 132 (90) | 185 (80) | 212 (92) | 70 (91) | 1573 (83) |
Cyprus (CY), Egypt (EG), Greece (GR), Hong Kong (HK), India (IN), Iran (IR), Italy (IT), Jordan (JO), Taiwan (TA), United States (US)
The questionnaire asked respondents to provide information about the frequency of missed doses, taking a higher or lower dose of desferrioxamine than was prescribed during the preceding month, and the sources of help to continue taking the drug regularly (i.e., doctor, health care providers, family, friends, other patients, thalassemia association or other sources). In addition the patients' reasons for missing doses were investigated under five categories: (1) access to desferrioxamine, (2) related to adverse effects of desferrioxamine, (3) patient's beliefs and feelings about the treatment, (4) inadequate support to continue with the treatment, and (5) other reasons not listed on the questionnaire. The responses classified as issues related to access to desferrioxamine were those indicating that it was not available or too expensive. Responses indicating the reason for missing a dose was due to side effects or that the infusions were very uncomfortable were grouped as related to adverse effects of desferrioxamine. The questions pertaining to the patient's beliefs and feelings included the daily use of an infusion, taking too many medications, not believing treatment was necessary, using natural remedies, feeling healthy, making the patient feel different from their friends, and not liking to medicate in front of people. The questions relating to adequate support to continue taking desferrioxamine asked the patients whether doses were missed because health care providers, family, or friends did not seem to be concerned about the patient's treatment.
Analyses
The data collected from the questionnaires are summarized by reporting the proportions of patients answering each item or, when appropriate, the mean and standard deviation (SD). The analyses pool the responses from patients or caregivers, as questions were common to both questionnaires.
Analyses included the patient characteristics and details of the desferrioxamine treatment. The proportion of patients in each age group, males, patients with each type of iron related complication; as well as the mean age at diagnosis and first blood transfusion are reported. The details of the desferrioxamine treatment include mean age when first used and current dose, frequency, and method of administration. The analyses also determined the proportion missing at least one dose of desferrioxamine in the preceding month, as well as the sources of help for adherence to the prescribed regimen.
Comparisons were made using the chi square of the proportions missing at least one dose of desferrioxamine in the preceding month among: countries, age groups, patients with iron related complications, frequency of blood transfusions, and method and frequency of desferrioxamine administration. The odds of missing at least one dose were determined using logistic regression to adjust for both age and country. The following potential predictors were also investigated: gender, age when desferrioxamine was first used, frequency of administration per week, use of a pump, and presence of iron-related complications.
Results
There were 1,888 respondents (65%) out of 2,900 questionnaires sent (Table 1), and 1,573 indicated they used desferrioxamine. The demographic and clinical characteristics of the patients using desferrioxamine are summarized in Table 2. About half the respondents using desferrioxamine were over 18 years old. Over 90% of the patients responding to this survey in each country reported that blood transfusions are received at intervals of 2 to 6 weeks. Typically, they were diagnosed with thalassemia major before they were two years old, and started desferrioxamine treatment around the age of 6 years (Table 3). Amongst the 1,573 patients prescribed desferrioxamine, 47% (n = 665) missed at least one dose during the preceding month; the mean number of doses missed was 4.7 (SD 6.1). In addition, 23% (n = 335) indicated they took a lower dose at least once in the preceding month; the mean number of times a lower dose was taken was 3.9 (SD 4.7). Far fewer reported taking a higher dose (10%, n = 144) and the mean number of times a higher dose was taken was 5.4 (SD 7.2).
Table 2.
Characteristics of respondents using desferrioxamine
| 31. Characteristics | Respondents using desferrioxamine (N = 1573) |
| Age N (%) | |
| <10 | 329 (21.5) |
| 10–18 | 464 (30.3) |
| >18 | 739 (48.2) |
| Male N (%) | 765 (49.0) |
| Receiving blood transfusions N (%) | 1564 (99.6) |
| Complications N (%) | |
| Heart disease | 154 (11.2) |
| Liver disease | 258 (18.8) |
| Diabetes | 133 (9.7) |
| Thyroid problem | 85 (6.3) |
| 32. Mean age at diagnosis, months (SD) | 19.1 (28.4) |
Table 3.
Desferrioxamine administration and proportions missing at least one dose in the preceding month
| 33. Characteristics | Overall (N = 1573) | Desferrioxamine use last month | |
| Missed at least one dose (N = 665) | No doses missed (N = 761) | ||
| Mean age first used years (SD) | 6.3 (5.3) | 6.6 (5.3) | 6.0 (5.5) |
| >= 5 days per week, N (%) | 941 (62.3) | 397 (61.9) | 470 (64.0) |
| Administered by pump, N (%) | 1189 (81.6) | 472 (76.9) | 622 (85.8) |
| Mean daily dose (SD), g | 1.7 (0.9) | 1.7 (0.9) | 1.7 (0.9) |
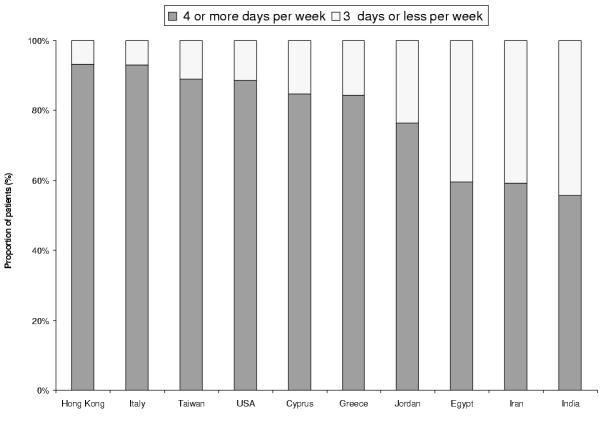
Desferrioxamine was administered at least five days per week by the majority of patients (62%, n = 941) (Table 3), and four or more days a week by most patients (79%, n = 1187). The proportion of patients administering desferrioxamine four or more days per week varied significantly among countries (chi square 163.5, p-value = 0.001). No more than 59% infused desferrioxamine on four days or more each week in Egypt, India, and Iran (Figure 1), compared to at least 76% in other countries.
Figure 1.
Proportion of patients administering desferrioxamine at least 4 days per week
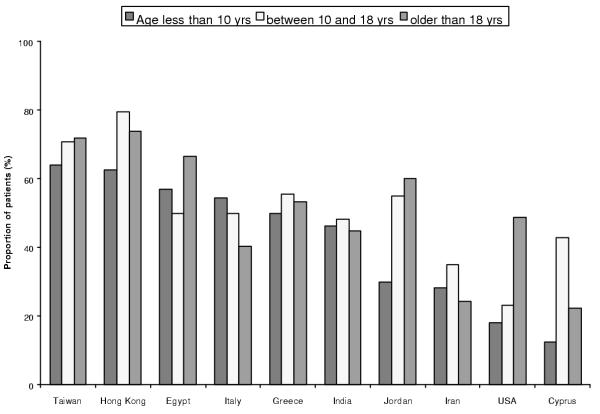
The proportion of patients that missed at least one dose also varied significantly among countries (Figure 2), (Chi square 159.8, p-value = 0.001). Hong Kong and Taiwan were the two countries with the highest risk of non-adherence and Cyprus the lowest. Amongst patients younger than 10 years old 19% missed at least one dose, age 10 to 18 years 33% and 48% of those older than 18 years. The patients younger than 10 years old had a significantly lower risk of missing the prescribed dose compared to the older age groups (Chi square 6.0, p = 0.05, df 2). Multivariate analyses using logistic regression to adjust for country and age revealed that both were significant predictors of the odds of missing at least one dose (Table 4). However, gender, age when desferrioxamine was first used, frequency of administration per week, use of a pump, and presence of iron-related complications were not associated with a significantly increased risk of missing a dose.
Figure 2.
Proportion of patients missing at least one desferrioxamine dose during preceding month by age group
Table 4.
Adjusted Odds Ratios (95% Confidence Intervals) for the association between age and country with missing at least one dose in the past month
| Variable | Odds Ratio | (95% CI) | P-value |
| Age group vs 18+years | |||
| < 10 years | 0.77 | (0.93, 0.63) | 0.01 |
| 10–18 years | 1.19 | (1.42, 1.00) | 0.05 |
| Country vs USA | |||
| Cyprus | 0.32 | (0.43, 0.23) | <0001 |
| Egypt | 1.51 | (2.24, 0.99) | 0.04 |
| Greece | 1.18 | (4.98, 3.56) | 0.39 |
| Hong Kong | 3.05 | (4.40, 0.47 | <0001 |
| India | 0.95 | (1.38, 1.52) | 0.79 |
| Iran | 0.49 | (0.67, 2.81) | <0001 |
| Italy | 0.80 | (1.13, 1.77) | 0.20 |
| Jordan | 0.94 | (1.30, 1.47) | 0.71 |
| Taiwan | 2.54 | (3.45, 0.54) | <0001 |
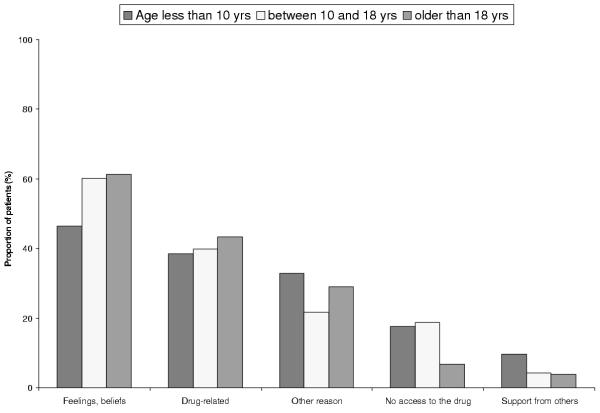
The most frequently reported category of reasons for patients missing a dose was related to their beliefs and feelings about the treatment (58%, n = 387) (Figure 3). The next most frequent reason was the adverse effects of infusing desferrioxamine (42%, n = 277). Problems accessing the drug (13%, n = 86), or feeling a lack of support from family, friends, or professional caregivers (5%, n = 35) were infrequent reasons (Figure 3). While access to the drug was the most common concern in India (51%, n = 26) and a frequent issue in Iran (25%, n = 15), it was a reason given for missing a desferrioxamine dose for less than 17% of the patients in any other country. Many patients (27%, n = 179) also indicated there were other reasons for missing a dose that were not covered by the list in the questionnaire.
Figure 3.
Reasons for missing a desferrioxamine dose according to age
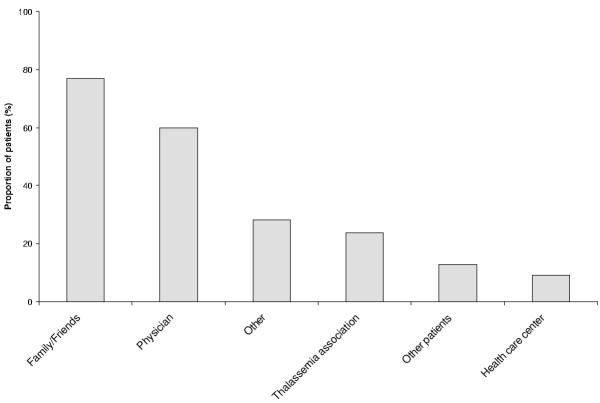
Family or friends (77%, n = 951) and physicians (60%, n = 660) were the most frequent sources of support for the patients to continue administering desferrioxamine (Figure 4). Further, the most helpful source of support identified by the patients was their family and friends (53%, n = 529) or their physicians (24%, n = 241). Other professionals and organizations were not frequently providing help to these patients in any of the countries.
Figure 4.
Sources of support to continue taking desferrioxamine regularly
Discussion
Evidence that the prognosis for patients diagnosed with thalassemia major is improved by regular blood transfusions and iron chelation has been available for more than 25 years [11,12]. Over 90% of the patients responding to this survey in each country reported that blood transfusions are received at regular intervals, and most respondents were infusing desferrioxamine at least four days per week. In Egypt, India, and Iran, however, nearly half of patients were using desferrioxamine three days or less each week and, from these responses, adequate access to desferrioxamine is still a common reason for missing a dose in India and Iran. These results suggest that there is a need for renewed efforts to create awareness within public health departments of this situation. It also provides additional data to support the local initiatives by patient organizations, as well as TIF, to ensure all patients gain access to an effective chelation regimen.
Regular blood transfusions with inadequate iron chelation therapy will not have immediate consequences for the patients, but will inevitably increase their risk of developing iron overload complications later in life [8,13]. Our study has shown that, overall, almost half of the patients had missed one or more doses in the preceding month and, on average a quarter were administering desferrioxamine three days or less each week. In our survey, children under ten years of age had a lower risk of missing a dose than the older age groups. This is consistent with other evidence that adolescents are generally less compliant than younger children [7,14]. Relatively few studies have been published on adherence to desferrioxamine, and different methodologies, countries, and age groups make direct comparisons between any studies of adherence inherently difficult. Three small studies of patients with thalassemia major found poor compliance with treatments, indicating patients administer as little as 54% of the prescribed desferrioxamine and, in one study, 23% of patients were taking less than 60% of the recommended dose [15-17]. In the UK, recent estimates suggest that only about half the patients are able to fully adhere to current iron chelation treatments and when compared to adherent patients the less adherent patients gain, on average, only ten years of life [18].
Our findings are consistent with studies of adherence to other chronic regimens for life threatening diseases that arise during childhood or adolescence [5-7,19,20]. For example, at least half of children receiving bone marrow transplants had significant problems with adherence to a long-term preventive antibiotic regimen [6]. Adults also have problems adhering to chronic preventive regimens for asymptomatic conditions. After a diagnosis of hypertension, for example, only 78% of patients persist with treatment for one year [21].
The physician and the family were the most frequent sources of support to continue administering desferrioxamine. Adherence has been related to young people's psychological adjustment to living with thalassemia and its treatment [15,22-24]. From our survey, the limited number of patients receiving support from local organizations suggests that there may be an opportunity to further expand their role. For example, these organizations could provide additional support groups where patients and parents can share their experiences, learn that they are not alone, and support each other. Such an approach has been found to be well received [25].
The reasons given by patients for missing desferrioxamine doses should be taken into account in developing interventions to enhance adherence. The most common reasons for missing a dose were those related to the patients' beliefs and feelings, rather than barriers to access the drug. This finding is in accord with other research on adherence. The most widely held theory is the "health belief model", according to which patients' perceived susceptibility to the illness or condition, its perceived severity, and perceived benefits and barriers to compliance are the most important factors determining their actions [26]. Another approach gaining currency is based on behavior change theory [27]. The results from our study indicate that interventions that increase adherence to chelation therapy should be pursued [28]. The reasons must be investigated further, however, given that at least a quarter of respondents indicated there were reasons for missing a dose that were not covered by the list included in the questionnaire.
One important limitation of this survey is that the respondents were all members of a patient organization and may therefore not be fully representative of patients with thalassemia. It is possible that those who seek membership are more involved in their illness and may thus reflect a greater commitment to treatment. Despite the good response rate (65%) for a survey like this, the rates did vary widely between countries. As responses were not linked with medical records, the data remain self-reports. Despite this limitation, we believe these data have value, especially regarding the patients' reasons for non-compliance and sources of support.
There were differences among countries in the ages of respondents. For example, in Cyprus, Greece, Italy, and the US, the majority of patients were adults, whereas in Egypt and Jordan, patients younger than 10 years old formed the largest age group. These differences may be a reflection of variations in TIF membership, of public health policies such as genetic screening, as well as of the impact of the type of treatment previously provided in each country. For example, during the last 30 years Cyprus, Greece, Italy, and the US introduced carrier and prenatal screening programs and the birth of affected children has decreased [10,29,30].
Conclusions
Adoption of life long adherence to regular administration of desferrioxamine is clearly very important for the long-term health of patients diagnosed with thalassemia major. There remains an opportunity to improve life-long use of desferrioxamine. Additional research to develop interventions to support adherence to this vital, treatment is therefore essential, until alternative oral chelation agents are developed.
Authors Contributions
Author 1 (AW) designed the draft questionnaires, performed the statistical analysis and drafted the manuscript. Author 2 (JJC) conceived of and designed the study, and participated in drafting the manuscript. Author 3 (TCG) managed the coordination of the surveys, data collection and analysis. Author 4 (KH) designed the study protocol and helped design the questionnaires. Author 5 (AA) participated in the design and coordination of the study. Author 6 (SW) participated in the design of the questionnaires and coordination and management of the study. Author 7 (AE) coordinated the TIF activities and participated in the design of the study and questionnaire development.
All authors read and approved the final manuscript.
Competing interests
Caro Research of which Jaime Caro is a shareholder, received a grant from Novartis Pharma AG (Basel, Switzerland), which provided funding for portions of the study. No editorial control was allowed.
At the time of the study, Alejandro Arana MD MSc MPH and Suzanne Wait PhD were employed by Novartis, which provided funding for portions of the study.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
Volunteers working with thalassemia patient organizations conducted the survey in each country, and the study was co-coordinated by the Thalassemia International Federation. The contribution of Thalassaemia International Federation's Scientific Collaborators is greatly acknowledged: Dr. M. Al-Fallah, Dr. De Sanctis, Prof. A. El-Beshlawy, Dr. S. Fucharoen, Ms. P. Gheissary, Dr. M. Hadjigavriel, Dr. M. Karageorga-Lagana, Dr. A. Kolnakou, Dr. V. Ladis, Dr. C.K. Li, Dr. H-S Lin, Dr. A. Mangiagli, Dr. I. Mirilla, Mrs. Z. Pakbaz, Dr. C. Politis, C. Papageorgiou, Dr. M. Sitarou, Sofianou, Dr. V.S. Tanphaichitr, and Mrs. S. Tuli. This research was supported in part by an unrestricted grant from Novartis Pharma AG, Basel, Switzerland.
Contributor Information
Alexandra Ward, Email: alexward@caroresearch.com.
J Jaime Caro, Email: jcaro@caroresearch.com.
Traci Craig Green, Email: tcraig@po-box.mcgillca.com.
Krista Huybrechts, Email: khuybrechts@carorresearch.com.
Alejandro Arana, Email: alejandro.arana@pharma.novartis.com.
Suzanne Wait, Email: suzanne.wait@bmc.com.
Androulla Eleftheriou, Email: thalassaemia@cytanet.com.cy.
References
- Modell B, ed Guidelines for the control of haemoglobin disorders. World Health Organization. 1994.
- Cao A, Gabutti V, Galanello R, Masera G, Modell B, Di Palma A, Piga A, Vullo C, Wonke B. Management protocol for the treatment of thalassemia patients. Thalassemia International Federation Nicosia, Cyprus. 1997.
- Olivieri NF, Nathan DG, MacMillan JH, Wayne AS, Liu PP, McGee A, Martin M, Koren G, Cohen AR. Survival in medically treated patients with homozygous beta-thalassemia. N Engl J Med. 1994;331:574–578. doi: 10.1056/NEJM199409013310903. [DOI] [PubMed] [Google Scholar]
- Zurlo MG, De Stefano P, Borgna-Pignatti C, Di Palma A, Piga A, Melevendi C, Di Gregorio F, Burattini MG, Terzoli S. Survival and causes of death in thalassemia major. Lancet. 1989;2:27–30. doi: 10.1016/S0140-6736(89)90264-X. [DOI] [PubMed] [Google Scholar]
- Blowey DL, Hebert D, Arbus GS, Pool R, Korus M, Koren G. Compliance with cyclosporine in adolescent renal transplant recipients. Pediatr Nephrol. 1997;11:547–551. doi: 10.1007/s004670050335. [DOI] [PubMed] [Google Scholar]
- Phipps S, DeCuir-Whalley S. Adherence issues in pediatric bone marrow transplantation. J Pediatr Psychol. 1990;15:459–475. doi: 10.1093/jpepsy/15.4.459. [DOI] [PubMed] [Google Scholar]
- Pidgeon V. Compliance with chronic illness regimens: school aged children and adolescents. J Pediatr Nurs. 1989;4:36–47. [PubMed] [Google Scholar]
- Brittenham G, Griffith PM, Nienhuis AW, McLaren CE, Young NS, Tucker EE, Allen CJ, Farrell DE, Harris JW. Efficacy of deferoxamine in preventing complications of iron overload in patients with thalassemia major. N Engl J Med. 1994;331:567–573. doi: 10.1056/NEJM199409013310902. [DOI] [PubMed] [Google Scholar]
- Gabutti V, Piga A. Results of long term iron chelating therapy. Acta Haematol. 1996;95:26–36. doi: 10.1159/000203853. [DOI] [PubMed] [Google Scholar]
- Olivieri NF. The beta-thalassemias. N Engl J Med. 1999;341:99–109. doi: 10.1056/NEJM199907083410207. [DOI] [PubMed] [Google Scholar]
- Hussain MA, Green N, Flynn DM, Hussein S, Hoffbrand AV. Subcutaneous infusion and intramuscular injection of desferrioxamine in patients with transfusional iron overload. Lancet. 1976;2:1278–1280. doi: 10.1016/S0140-6736(76)92035-3. [DOI] [PubMed] [Google Scholar]
- Modell B, Letsky EA, Flynn DM, Peto R, Weatherall DJ. Survival and desferrioxamine in thalassemia major. BMJ. 1982;284:1081–1084. doi: 10.1136/bmj.284.6322.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers KH, Levin AR, Markenson AL, Marcus JR, Klein AA, Hilgartner MW, Engle MA. Longitudinal study of cardiac function in thalassemia major. Ann N Y Acad Sci. 1980;344:397–404. doi: 10.1111/j.1749-6632.1980.tb33678.x. [DOI] [PubMed] [Google Scholar]
- Cromer B, Tarnowski KJ. Non-compliance in adolescents: a review. J Dev Behav Pediatr. 1989;10:207–215. [PubMed] [Google Scholar]
- Beratis S. Noncompliance with iron chelation therapy in patients with beta thalassaemia. J Psychosom Res. 1989;33:739–745. doi: 10.1016/0022-3999(89)90089-5. [DOI] [PubMed] [Google Scholar]
- McGee A, Koren G, Liu P, Freedman M, Rose V, Benson L, Olivieri N. Cardiac disease-free survival in patients with thalassemia major treated with subcutaneous deferoxamine: an update of the Toronto cohort. Blood. 1989;74:311a Abstract 1172. [Google Scholar]
- Olivieri N. Randomized trial of deferiprone (L1) and deferoxamine (DFO) in thalassemia major. Blood. 1996;88:651a Abstract 2593. [Google Scholar]
- Modell B, Khan M, Darlison M. Survival in beta-thalassemia major in the UK: data form the UK Thalassemia Register. Lancet. 2000;355:2051–2052. doi: 10.1016/S0140-6736(00)02357-6. [DOI] [PubMed] [Google Scholar]
- Rees L. Compliance with growth hormone therapy in chronic renal failure and post transplant. Pediatr Nephrol. 1997;11:752–754. doi: 10.1007/s004670050383. [DOI] [PubMed] [Google Scholar]
- Wolff G, Strecker K, Vester U, Latta K, Ehrich JH. Non-compliance following renal transplantation in children and adolescents. Pediatr Nephrol. 1998;12:703–708. doi: 10.1007/s004670050531. [DOI] [PubMed] [Google Scholar]
- Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. Can Med Assoc J. 1999;160:31–37. [PMC free article] [PubMed] [Google Scholar]
- Bush S, Mandel FS, Giardina PJ. Future orientation and life expectations of adolescents and young adults with thalassemia major. Ann N Y Acad Sci. 1998;850:361–369. doi: 10.1111/j.1749-6632.1998.tb10494.x. [DOI] [PubMed] [Google Scholar]
- Goldbeck L, Baving A, Kohne E. Psychosocial aspects of beta-thalassemia: distress, coping and adherence. Klin Padiatr. 2000;212:254–259. doi: 10.1055/s-2000-9683. [DOI] [PubMed] [Google Scholar]
- Sherman M, Koch D, Giardina P, Hymowitz P, Siegel R, Shapiro T. Thalassemic children's understanding of illness: a study of cognitive and emotional factors. Ann N Y Acad Sci. 1985;445:327–336. doi: 10.1111/j.1749-6632.1985.tb17203.x. [DOI] [PubMed] [Google Scholar]
- Yamashita R, Foote D, Weissman L. Patient cultures: thalassemia service delivery and patient compliance. Ann N Y Acad Sci. 1998;850:521–552. doi: 10.1111/j.1749-6632.1998.tb10540.x. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. The health belief model: explaining health behavior through expectancies. In: Ganz K, editor. Health Behavior and Health Education. 1. New York, Jossey-Bass; 1989. pp. 39–62. [Google Scholar]
- Willey C, Redding C, Stafford J, Garfield F, Geletko S, Flanigan T, Melbourne K, Mitty J, Caro JJ. Stages of change for adherence with medication regimens for chronic diseases: development and validation of a measure. Clin Ther. 2000;22:853–871. doi: 10.1016/S0149-2918(00)80058-2. [DOI] [PubMed] [Google Scholar]
- Koch DA, Giardina PJ, Ryan M, MacQueen M, Hilgartner MW. Behavioral contracting to improve adherence in patients with thalassemia. J Pediatr Nurs. 1993;8:106–111. [PubMed] [Google Scholar]
- Loukopoulos D. Current status of thalassemia and the sickle cell syndromes in Greece. Semin Hematol. 1996;33:76–86. [PubMed] [Google Scholar]
- Pearson HA, Guiliotis DK, Rink L, Wells JA. Patient age distribution in thalassemia major: changes from 1973 to 1985. Pediatrics. 1987;80:53–57. [PubMed] [Google Scholar]