Abstract
This retrospective study aimed to analyze the treatment effect and prognostic factors of pediatric acute myeloid leukemia (AML) patients with t(8;21). A total of 268 newly diagnosed pediatric AML (pAML) enrolled from 1 January 2005 to 31 December 2022 were retrospectively reviewed, and 50 (18.7%) patients harbored t(8;21) translocation. CR rate, OS, EFS, and RFS were assessed by multivariate Logistic and Cox regression models in these patients. Of the 50 patients, 2 patients abandoned treatment during the first induction course. Of the remaining 48 patients who received double-induction therapy and were included in the final analyses, CR1 and CR2 were 75.0% (36/48) and 95.8% (46/48), respectively. The overall three-year OS, EFS, and RFS were 68.4% (95% CI, 55.0–85.1), 64.2% (95% CI, 50.7–81.4), and 65.5% (95% CI, 51.9–82.8), respectively. The presence of loss of sex chromosome (LOS) at diagnosis (n = 21) was associated with a better 3-year OS [87.5% (95% CI, 72.7–100) vs. 52.7% (95% CI, 35.1–79.3), p = 0.0089], 3-year EFS [81.6% (95% CI, 64.7–100) vs. 49.7% (95% CI, 32.4–76.4), p = 0.023], and 3-year RFS [81.6% (95% CI, 64.7–100) vs. 51.7% (95% CI, 33.9–78.9), p = 0.036] than those without LOS (n = 27), and it was also an independent good prognostic factor of OS (HR, 0.08 [95% CI, 0.01–0.48], p = 0.005), EFS (HR, 0.22 [95% CI, 0.05–0.85], p = 0.029), and RFS (HR, 0.21 [95% CI, 0.05–0.90], p = 0.035). However, extramedullary leukemia (EML) featured the independent risk factors of inferior OS (HR, 10.99 [95% CI, 2.08–58.12], p = 0.005), EFS (HR, 4.75 [95% CI, 1.10–20.61], p = 0.037), and RFS (HR, 6.55 [95% CI, 1.40–30.63], p = 0.017) in pediatric individuals with t(8;21) AML. Further analysis of combining LOS with EML indicated that the EML+LOS− subgroup had significantly inferior OS (92.9%, [95% CI, 80.3–100]), EFS (86.2%, [95% CI, 70.0–100]), and RFS (86.2%, [95% CI, 80.3–100]) compared to the other three subgroups (all p < 0.001). LOS and EML are independent prognostic factors of OS, EFS, and RFS with t(8;21) pAML patients. LOS combined with EML may help improve risk stratification.
Keywords: t(8;21), pediatric acute myeloid leukemia, prognosis, loss of sex chromosome, extramedullary leukemia
1. Introduction
Acute myeloid leukemia (AML) constitutes 20% of pediatric leukemias, with 5.1% of AML patients being diagnosed at an age younger than 20 years [1,2,3]. AML1::ETO (also known as RUNX1::RUNX1T1) resulting from t(8;21) (q22;q22) is one of the most frequent genetic aberrations, with a incidence of 20% in newly diagnosed pAML patients [4,5,6,7]. Although t(8;21) AML is generally categorized as a favorable subgroup, 20%–35% of patients with this genotype experience relapse, and the outcomes of this genotype are heterogeneous [8,9,10]. We conducted a single-center retrospective study of children with this genotype from 1 January 2005 to 31 December 2022 to search for prognostic factors that could potentially be useful to further improve outcomes and update therapy strategies.
2. Materials and Methods
2.1. Study Design and Patients
Individuals aged ≤eighteen years with a confirmed diagnosis of AML were enrolled in the retrospective study. Data from individuals without proof of t(8;21) presence and individuals without treatment during the first induction course were excluded from analyses. All patients were treated in the Children’s Hospital of Fudan University between 2005 and 2023, receiving risk-stratified therapy without prophylactic cranial irradiation. Patients treated in our institution from 2005 to 2014 received the CHFU-AML 2005 regimen, and CCLG-AML-2015 and CALSIII-AML18 regimens were used in 2015–2018 and 2018–2023, respectively [11,12]. The study was approved by the institutional review board of the Children’s Hospital of Fudan University, and informed consent was obtained from all patients or their legal guardians. Outcome data reported here were updated on 21 March 2023.
2.2. Morphology, Cytogenetics and Immunophenotyping
The morphologic assessment was founded on May-Grünwald–Giemsa stains, myeloperoxidase reactions, and nonspecific esterases utilizing α-naphthyl acetate following the FAB and WHO classifications [13,14,15]. A chromosome G-banding analysis was conducted on all cases according to standard procedures [16,17]. The description of karyotypes followed the ISCN [18]. Loss of sex chromosomes (LOS) was defined as the presence of a -X/-Y clone in more than 3 of the 20 cells analyzed [19]. Complex karyotype (CK) was defined as ≥3 chromosomal aberrations [20]. Monosomal karyotype (MK) was defined as ≥2 separate autosomal monosomies or 1 monosomy plus ≥ 1 structural aberrations [21,22]. Immunophenotyping was conducted in bone marrow (BM) specimens of all cases following previous descriptions [23,24]. Quantification of minimal residual disease (MRD) in the BM (after induction therapy I and II, or other later timepoint) using multiparameter flow cytometry (MFCM) commenced in June 2018.
2.3. Molecular Biology Analysis
Molecular studies were performed from June 2018, and the results for 20 patients are available. Mononuclear cells were isolated, and both DNA and mRNA were extracted from BM and peripheral blood samples. Additionally, random-primed cDNA synthesis was conducted according to the protocols [25]. As for fusion genes, interphase fluorescence in situ hybridization (FISH) with probes for RUNX1 and RUNX1T1 was conducted using commercially available probes. Investigations for FLT3-ITD, C-KIT/D816, NPM1 (Exon12), and CEBPA were carried out in these patients [26].
2.4. Statistical Analysis
Each statistical assessment was performed utilizing R software (version 4.1.0). Outcomes were evaluated by using complete remission (CR), overall survival (OS), event-free survival (EFS), and relapse-free survival (RFS) (Table S1) [27]. Categorical variables were compared between groups utilizing the χ2 test and continuous variables by the Mann–Whitney U test. To identify factors associated with CR and prognosis, variables with p < 0.2 [28] in univariate analyses entered a multivariate Logistic regression model and a multivariate Cox regression model, respectively. Results were presented as OR or HR and 95% CI. Survival outcomes were determined utilizing the Kaplan–Meier method, and comparisons between groups were conducted utilizing the logrank test. Statistical importance was denoted by two-sided p < 0.05.
3. Results
3.1. Clinical Characteristics
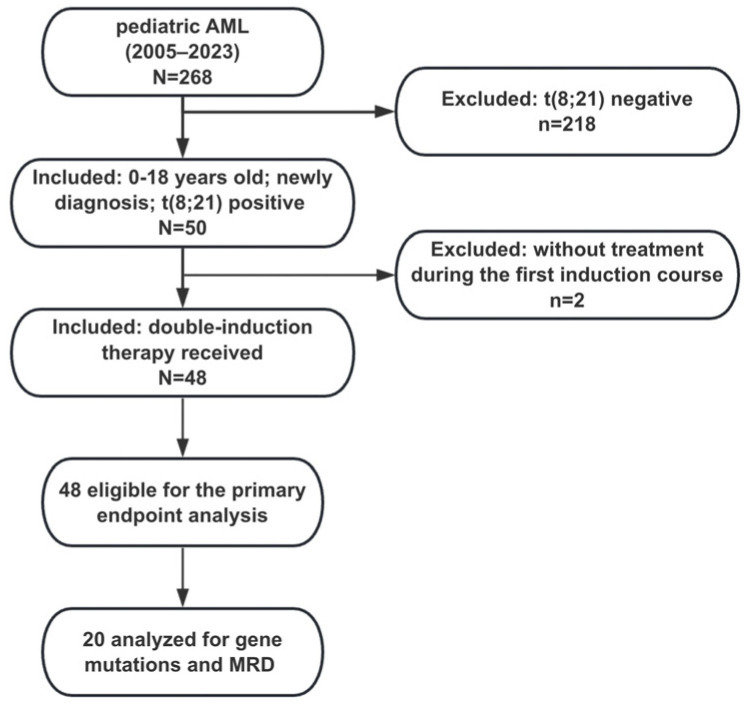
From 1 January 2005 to 31 December 2022, 268 evaluable individuals were enrolled from a Chinese children’s medical center. Data from 218 individuals without proven t(8;21) presence and two individuals without treatment during the first induction course were excluded (Figure 1). An amount of 48 individuals with t(8;21) AML were included in the final analyses, with a male-to-female ratio of 1.8:1. The median age at diagnosis was 8.6 years (range, 2.5–16.7), with 46 patients (95.8%) aged between 3 and 14 years and only one patient (2.1%) in each age group younger than three years and older than fourteen years, respectively. The median white blood cell (WBC) count was 15.9 × 109/L (range, 1.7–123.0). The median platelet count was 28.5 × 109/L (range, 4–265). The median hemoglobin (Hb) count was 78.6 g/L (38.2–122.0). The median follow-up time was 35.5 months (IQR, 12.8–74.8). According to MFCM, the sums of the percentage of positive cells for CD34 plus CD117 or HLA-DR were greater than 95% in these cases. CD19 antigen and CD56 antigen were detected in 23 (47.9%) and 21 (43.6%) of these cases, respectively. As for additional chromosome abnormality (ACA), t(8;21) was the sole cytogenetic aberration in 13 patients (27.1%), while 35 (72.9%) harbored other ACAs, 21 (43.8%) had loss of sex chromosome (LOS), 7 (14.6%) had CK, 11 (22.9%) had MK, 3 (6.3%) had deletion of chromosome 9q [del(9q)], only one (2.1%) had trisomy 4, and no one had trisomy 8. Of the 20 patients analyzed for genetic mutation, two (10.0%) were FLT3-ITD positive, 12 (60.0%) were C-KIT positive, and none of them had CEBPA and NPM1 mutations. Within the same cohort evaluable for MRD analysis, 7 (35%) and 18 (90%) had a negative MRD status (defined by <0.1%) after induction therapy I and II, respectively (Table 1).
Figure 1.
Flow diagram.
Table 1.
Baseline features of 48 pediatric acute myeloid leukemia (pAML) patients with t(8;21).
| Characteristics | n = 48 |
|---|---|
| Gender, n (%) | |
| Male | 31 (64.6) |
| Female | 17 (35.4) |
| Age (M[range]) (years), n (%) | 8.6 (2.5–16.7) |
| <3 | 1 (2.1) |
| 3–14 | 45 (93.8) |
| >14 | 2 (4.2) |
| HB (M[range]) (g/L) | 78.6 (38.2–122.0) |
| ≤60 | 10 (20.8) |
| 60–90 | 24 (50.0) |
| >90 | 14 (29.2) |
| PLT (M[range]) (×109/L) | 28.5 (4.0–265.0) |
| ≤20 | 11(22.9) |
| 20–100 | 34 (70.8) |
| >100 | 3 (6.3) |
| PB blast (M[range]) (%) 1, n (%) | 45.0 (5.0–88.0) |
| BM blast (M[range]) (%), n (%) | 51.25 (5.0–87.0) |
| FAB | |
| M2 | 33 (68.8) |
| M4 | 10 (20.8) |
| M5 | 3 (6.2) |
| NOS | 2 (4.2) |
| Immunological classification, n (%) | |
| CD19 (+) | 23 (47.9) |
| CD56 (+) | 21 (43.6) |
| CD34 (+) | 47 (97.9) |
| HLA-DR (+) | 48 (100) |
| CD117 (+) | 48 (100) |
| MPO (+) | 34 (70.8) |
| CD13 (+) | 20 (41.7) |
| CD33 (+) | 35 (72.9) |
| Karyotype, n (%) | |
| CK | 7 (14.6) |
| LOS | 21 (43.8) |
| MK | 11(22.9) |
| del(9q) | 3 (6.3) |
| trisomy 4 | 1 (2.1) |
| Genetic mutations 2, N (%) | from 2018, N = 20 |
| C-KIT (+) | 12 (60.0) |
| FLT3-ITD (+) | 2 (10.0) |
| Induction I MRD (%) 3, n (%) | from 2018, N = 20 |
| <0.1 | 7 (35.0) |
| ≥0.1 | 13 (65.0) |
| Induction II MRD (%) 3, n (%) | from 2018, N = 20 |
| <0.1 | 18 (90.0) |
| ≥0.1 | 2 (10.0) |
| EML 4, n (%) | 8 (16.7) |
| CR1, n (%) | |
| CR | 36 (75.0) |
| NR | 5 (10.4) |
| PR | 7 (14.6) |
| CR2, n (%) | |
| CR | 46 (95.8) |
| NR | 2 (4.2) |
| Year of diagnosis, n (%) | |
| 2005–2014 | 18 (37.5) |
| 2015–2018 | 10 (20.8) |
| 2019–2023 | 20 (41.7) |
| HSCT, n (%) | 9 (18.8) |
| Relapse, n (%) | 13 (27.1) |
| Death, n (%) | 13 (27.1) |
Abbreviations: WBC: white blood cell counts; MRD: minimal residual disease; BM blast: bone marrow leukemic blast percentage; PLT: platelets; LOS: loss of sex chromosome; CR1: first complete remission; HB: hemoglobin; MK: monosomal karvotype; EML: extramedullary leukemia; PR: partial remission; NR: no remission; PB blast: peripheral blast percentage; del(9q), Deletion of chromosome 9q; M: median; CR2: second complete remission; CK: complex karyotype. 1 Missing data are due to being not submitted to the statistics center. N = 46. 2 Genetic mutation detection has been available since June 2018. N = 20. 3 MRD detection has been available since June 2018. N = 20. 4 EML was defined as the process whereby malignant leukemic cells from the BM infiltrate into tissues outside the BM at diagnosis, including the central nervous system, cutis, and periosteum, leading to the formation of an extramedullary mass.
3.2. Treatment Outcome
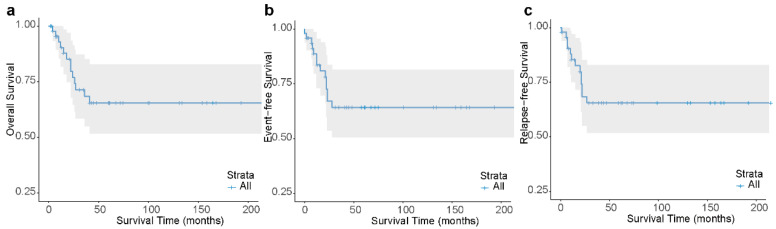
Overall, first complete remission (CR1) and second complete remission (CR2) were achieved by 75.0% (n = 36) and 95.8% (n = 46) of the patients, respectively. CR was achieved in 20 (100.0%) patients treated with the CALSIII-AML18 protocol, of whom 18 (90.0%) had a negative MRD status at the end of induction therapy. The 3-year OS, EFS, and RFS were 68.4% (95% CI, 55.0–85.1), 64.2% (95% CI, 50.7–81.4), and 65.5% (95% CI, 51.9–82.8), respectively (Figure 2a–c). The 3-year OS, EFS, and RFS of 18 cases treated with the CHFU-AML 2005 protocol were 72.2% (95% CI, 54.2–96.2), 61.1% (95% CI, 42.3–88.3), and 64.7% (95% CI, 45.5–91.9), respectively. The 3-year OS, EFS, and RFS of 10 cases treated with the CCLG-AML 2015 protocol were 60.0% (95% CI, 36.2–99.5), 60.0% (95% CI, 36.2–99.5), and 60.0% (95% CI, 36.2–99.5), respectively. The 3-year OS, EFS, and RFS of 20 cases treated with the CALSIII-AML18 protocol were 68.2% (95% CI, 43.8–100), 71.1% (95% CI, 47.5–100), and 71.1% (95% CI, 47.5–100), respectively. No significant differences were found in the outcomes (Figure S1) and CR rate among these protocols (Tables S2 and S3).
Figure 2.
Outcomes of t(8;21) pAML patients. Kaplan–Meier analysis of overall survival (OS) (a), event-free survival (EFS) (b) and relapse-free survival (RFS) (c) for all patients. Three-year OS, EFS and RFS: 0.68 ± 0.08, 0.64 ± 0.08, 0.66 ± 0.08, respectively.
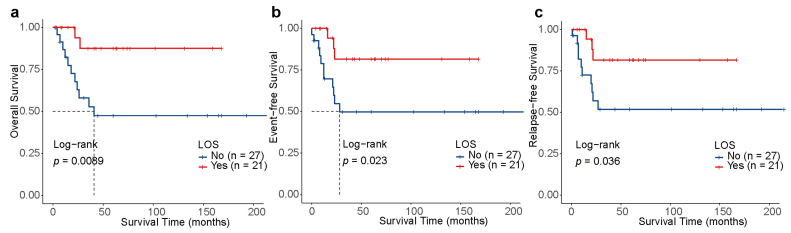
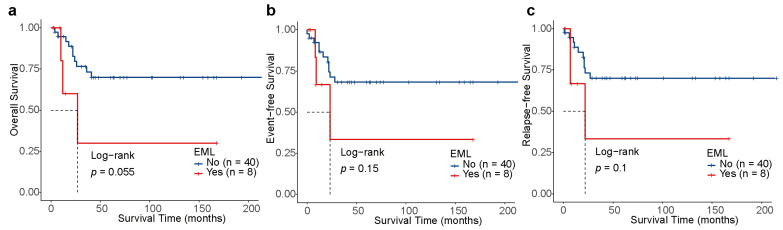
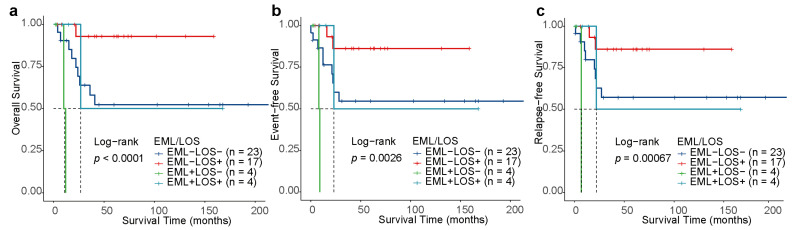
Of note, patients with LOS (n = 21) had significantly better 3-year OS [87.5% (95% CI, 72.7–100) vs. 52.7% (95% CI, 35.1–79.3), p = 0.0089], 3-year EFS [81.6% (95% CI, 64.7–100) vs. 49.7% (95% CI, 32.4–76.4), p = 0.023], and 3-year RFS [81.6% (95% CI, 64.7–100) vs. 51.7% (95% CI, 33.9–78.9), p = 0.036] than those without LOS (n = 27, Figure 3a–c). Additionally, the OS, EFS, and RFS of patients with EML did not have any significant differences to those without EML (p > 0.05, Figure 4a–c), which may be associated with the limited quantity of individuals with EML (n = 8). For the 20 patients treated under the CALSIII-AML18 regimen, there was no significant difference in prognosis between those with and without C-KIT/negative MRD status, respectively (all p > 0.05, Figures S2–S4).
Figure 3.
Outcomes depending on the loss of sex chromosomes (LOS) in t(8;21) AML. Kaplan–Meier analysis of OS (a), EFS (b) and RFS (c) for patients stratified by LOS.
Figure 4.
Outcomes depending on the extramedullary leukemia (EML) in t(8;21) AML. Kaplan–Meier analysis of OS (a), EFS (b) and RFS (c) for patients stratified by EML.
3.3. Impact of Clinical and Biological Characteristics on CR Achievement
We assessed the association of clinical and biological features with CR achievement in a logistic regression model. As shown in Table 2, age at diagnosis, WBC, PB blast, FAB, CD19, MK, and Year of diagnosis were significantly linked to CR achievement of those patients. We then included these seven variables in the multivariate logistic analysis and revealed that none of these values remained significantly different for CR achievement.
Table 2.
Univariate and multivariate logistic analyses of first complete remission (CR1) in 48 patients with t(8;21) AML.
| Characteristics | CR | CRR | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |||
| Gender | ||||||||
| Female | 11 | 64.7 | Ref | |||||
| Male | 25 | 80.6 | 2.27 | 0.59–8.89 | 0.228 | |||
| Age at diagnosis (years) | ||||||||
| ≤8.6 | 21 | 84.0 | Ref | Ref | ||||
| >8.6 | 15 | 65.2 | 0.36 | 0.08–1.35 | 0.141 | 0.55 | 0.08–3.25 | 0.514 |
| WBC (×109/L) | ||||||||
| >20 | 11 | 61.1 | Ref | Ref | ||||
| ≤20 | 25 | 83.3 | 3.18 | 0.84–12.99 | 0.093 | 1.86 | 0.34–10.32 | 0.464 |
| PB blast (%) | ||||||||
| <45 | 20 | 83.3 | Ref | Ref | ||||
| ≥45 | 14 | 58.3 | 0.23 | 0.05–0.94 | 0.053 | 0.24 | 0.03–1.29 | 0.119 |
| BM blast (%) | ||||||||
| <50 | 16 | 0.8 | Ref | |||||
| ≥50 | 20 | 71.4 | 0.62 | 0.15–2.37 | 0.501 | |||
| FAB | ||||||||
| M2 | 27 | 81.8 | Ref | Ref | ||||
| M4 | 5 | 50.0 | 0.22 | 0.05–1.02 | 0.053 | 0.22 | 0.03–1.41 | 0.120 |
| M5 | 2 | 66.7 | 0.44 | 0.04–10.47 | 0.534 | 0.90 | 0.03–36.68 | 0.988 |
| NOS | 2 | 100 | 3,478,080 | 0–NA | 0.993 | 1,881,857 | 0-NA | 0.996 |
| CD19 | ||||||||
| No | 21 | 84.0 | Ref | Ref | ||||
| Yes | 15 | 65.2 | 0.36 | 0.08–1.35 | 0.141 | 0.66 | 0.04–7.82 | 0.752 |
| CD56 | ||||||||
| No | 21 | 77.8 | Ref | |||||
| Yes | 15 | 71.4 | 0.71 | 0.19–2.70 | 0.615 | |||
| LOS | ||||||||
| No | 21 | 77.8 | Ref | |||||
| Yes | 15 | 71.4 | 0.71 | 0.19–2.70 | 0.615 | |||
| CK | ||||||||
| No | 29 | 70.7 | Ref | |||||
| Yes | 7 | 100 | 4,785,467 | 0-NA | 0.996 | |||
| MK | ||||||||
| No | 26 | 70.3 | Ref | Ref | ||||
| Yes | 10 | 90.9 | 4.23 | 0.68–82.44 | 0.193 | 3.62 | 0.36–87.81 | 0.318 |
| EML | ||||||||
| No | 29 | 72.5 | Ref | |||||
| Yes | 7 | 87.5 | 2.66 | 0.40–52.62 | 0.386 | |||
| Year of diagnosis | ||||||||
| 2005–2014 | 16 | 88.9 | Ref | Ref | ||||
| 2015–2018 | 6 | 60.0 | 0.19 | 0.02–1.21 | 0.091 | 0.42 | 0.02–7.38 | 0.540 |
| 2019–2023 | 14 | 70.0 | 0.29 | 0.04–1.5 | 0.168 | 0.48 | 0.02–16.72 | 0.666 |
Abbreviations: WBC: white blood cell counts; LOS: loss of sex chromosome; HB: hemoglobin; MK: monosomal karvotype; PB_blast: peripheral blast percentage; EML: extramedullary leukemia; BM blast: bone marrow leukemic blast percentage; CRR: complete remission rate; PLT: platelets; CI: confidence interval; CK: complex karyotype; OR: odds ratio.
3.4. Prognostic Factors for OS, EFS, and RFS
To assess the significant prognostic factors, Cox regression modeling was performed. As shown in Table 3 and Tables S4–S8, EML and LOS were significantly correlated with the OS, EFS, and RFS of t(8;21) pAML patients. Individuals with EML had lower OS (p = 0.071), EFS (p = 0.164), and RFS (p = 0.108), while those with LOS had higher OS (p = 0.022), EFS (p = 0.036), and RFS (p = 0.051). We then included the two covariates in the multivariate analyses and demonstrated that EML was an independent risk factor for inferior OS (hazard ratio [HR], 10.99 [95% CI, 2.08–58.12], p = 0.005), EFS (HR, 4.75 [95% CI, 1.10–20.61], p = 0.037), and RFS (HR, 6.55 [95% CI, 1.40–30.63], p = 0.017), while LOS was an independent good prognostic factor that influenced OS (HR, 0.08 [95% CI, 0.01–0.48], p = 0.005), EFS (HR, 0.22 [95% CI, 0.05–0.85], p = 0.029), and RFS (HR, 0.21 [95% CI, 0.05–0.90], p = 0.035).
Table 3.
Univariate and multivariate COX analyses of event-free survival (EFS) in 48 patients with t(8;21) AML.
| Characteristics | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Gender | ||||||
| Female | Ref | |||||
| Male | 1.63 | 0.51–5.20 | 0.412 | |||
| Age at diagnosis (years) | ||||||
| ≤8.6 | Ref | |||||
| >8.6 | 1.55 | 0.54–4.42 | 0.417 | |||
| WBC (×109/L) | ||||||
| >20 | Ref | |||||
| ≤20 | 0.76 | 0.25–2.28 | 0.623 | |||
| PB blast (%) | ||||||
| <45 | Ref | |||||
| ≥45 | 1.48 | 0.47–4.67 | 0.502 | |||
| BM blast (%) | ||||||
| <50 | Ref | |||||
| ≥50 | 1.10 | 0.38–3.17 | 0.864 | |||
| FAB | ||||||
| M2 | Ref | |||||
| M4 | 0.29 | 0.04–2.25 | 0.236 | |||
| M5 | 0.98 | 0.13–7.61 | 0.984 | |||
| NOS | 1.83 | 0.24–14.21 | 0.564 | |||
| CD19 | ||||||
| No | Ref | |||||
| Yes | 0.53 | 0.17–1.68 | 0.28 | |||
| CD56 | ||||||
| No | Ref | |||||
| Yes | 0.65 | 0.22–1.95 | 0.443 | |||
| LOS | ||||||
| No | Ref | Ref | ||||
| Yes | 0.26 | 0.07–0.92 | 0.036 | 0.22 | 0.05–0.85 | 0.029 |
| CK | ||||||
| No | Ref | |||||
| Yes | 1.12 | 0.25–5.04 | 0.878 | |||
| MK | ||||||
| No | Ref | |||||
| Yes | 0.57 | 0.13–2.56 | 0.464 | |||
| C-KIT | ||||||
| No | Ref | |||||
| Yes | 1.99 | 0.2–19.39 | 0.554 | |||
| FLT3-ITD | ||||||
| No | Ref | |||||
| Yes | NA | NA | NA | |||
| Induction I MRD (%) | ||||||
| <0.1 | Ref | |||||
| ≥0.1 | 0 | 0-Inf | 0.999 | |||
| Induction II MRD (%) | ||||||
| <0.1 | Ref | |||||
| ≥0.1 | 4.29 | 0.38–48.77 | 0.241 | |||
| EML | ||||||
| No | Ref | Ref | ||||
| Yes | 2.52 | 0.69–9.24 | 0.164 | 4.75 | 1.10–20.61 | 0.037 |
| CR1 | ||||||
| CR | Ref | |||||
| not in CR | 0.91 | 0.25–3.27 | 0.885 | |||
| CR2 | ||||||
| CR | Ref | |||||
| not in CR | ∞ | 0-Inf | 1.00 | |||
| Year of diagnosis | ||||||
| 2005–2014 | Ref | |||||
| 2015–2018 | 1.21 | 0.35–4.13 | 0.766 | |||
| 2019–2023 | 0.64 | 0.16–2.5 | 0.523 | |||
Abbreviations: WBC: white blood cell counts; MK: monosomal karvotype; BM blast: bone marrow leukemic blast percentage; CK: complex karyotype; PLT: platelets; LOS: loss of sex chromosome; HB: hemoglobin; CR1: first complete remission; PB blast: peripheral blast percentage; EML: extramedullary leukemia; HR: hazard ratio; CR2: second complete remission; CI: confidence interval.
3.5. Risk Stratification
To provide an estimation of prognostic stratification, we classified individuals into four risk groups based on EML and LOS: the EML+LOS+ (n = 4), EML+LOS− (n = 4), EML−LOS+ (n = 17), and EML−LOS− (n = 23) subgroups. As for other secondary ACAs that accompany t(8;21), one out of four individuals in the EML+LOS− subgroup had trisomy 4, 1 out of 23 individuals in the EML−LOS− group and 2 out of 17 patients in the EML−LOS+ subgroup had del(9q), and no patients had trisomy 8. Kaplan–Meier survival analysis unveiled that t(8;21) pAML patients with EML+LOS− had the most inferior outcome, while those with EML−LOS+ had the best prognosis, showing the following statistically significant survivals: the 3-year OS [0 vs. 92.9% (95% CI, 80.3–100), p < 0.001], the 3-year EFS [0 vs. 86.2% (95% CI, 70.0–100), p < 0.001], and the 3-year RFS [0 vs. 86.2% (95% CI, 80.3–100), p < 0.001] (Figure 5a–c). Given that the number of patients in the EML+LOS− and EML+LOS− subgroups was too small, we need to exercise caution when explaining the impact of risk stratification on prognosis. The observation of distinct prognostic effects between the two groups based on risk stratification suggested that EML+LOS− should be differentiated from EML−LOS+ in future research.
Figure 5.
Kaplan–Meier curves for risk stratification. Kaplan–Meier analysis of OS (a), EFS (b) and RFS (c) for patients stratified by risk levels depending on EML and LOS.
4. Discussion
This study demonstrated that, among a large cohort of 268 pAML individuals, 50 (18.7%) harbored t(8;21) translocation. This finding aligns with the range reported in other studies [29,30]. We explored the prognostic factors of t(8;21) pAML patients at a single Chinese children’s medical center. Previous studies demonstrated that t(8;21) pAML individuals likely benefit from regimens incorporating high doses of Ara-C during induction therapy [29]. In this study, the three-year OS, EFS, and RFS were 68.4% (95% CI, 55.0–85.1), 64.2% (95% CI, 50.7–81.4), and 65.5% (95% CI, 51.9–82.8), respectively, which were greater than that in the research by Wu et al. [31], comparable with the research by Che et al. [32], and obviously lower than that reported by a Japanese team [8]. Their better therapeutic effect may be attributed to a higher cumulative dose of Ara-C (59.4–78.4 g/m2) and adequate supportive care.
There was no difference in CR rate among different induction protocols [33,34]. In accordance with these studies, our cohort showed that patients treated with CHFU-AML 2005, CCLG-AML 2015, and CALSIII-AML18 regimens also showed no significant difference in CR rate (p > 0.05). Walter et al. [35] demonstrated that CR is a unique clinical significance factor in trials of de novo AML. Fang et al. [34] observed that AML individuals achieving CR1 showed better prognoses than those without CR1. In our study, however, we did not verify their finding that the clinical and biological features of individuals between CR1 and PR/NR groups were compared, but there was no statistical difference in CR rate among all factors (p > 0.05). Our results were slightly different from previous studies, considering that the sample size included in our study was small and needs to be further expanded in future studies.
In line with prior reports, the prevalence of ACAs was high (72.9%), and the most common cytogenetic aberration was LOS [36,37,38,39,40,41]. According to the Cox model, EML and LOS were independent prognostic factors for t(8;21) pAML individuals. Previous studies found that loss of Y chromosome (LOY) was linked to a high relapse risk and shorter OS [42,43]. However, some studies demonstrated that LOS had no significant associations with survival probabilities [19,36,44,45]. Mitterbauer et al. [46] suggested that LOS was linked to a significantly better EFS outcome. In our study, LOS was correlated with significantly better OS, EFS, and RFS, aligning with the research by Chen et al. [47].
The prognostic values of EML remain controversial across studies. Previous studies found that t(8;21) pAML patients with EML were linked to a low CR rate and poor RFS and OS [48,49,50]. However, Bisschop et al. [51] did not find significant associations with survival outcomes. The differences in results between studies may relate to the small-scale cohort, differences in race, and the wide range of case cohorts. In our study, EML was identified as an independent prognostic factor that is correlated with worse OS, EFS, and RFS, in line with the findings reported by Stove et al. [49] In addition, some reports claimed that patients with EML involving different sites had different survival outcomes [52,53]. In our study, subgroup analysis for the prognosis effect of EML at different sites could not be conducted due to the insufficient number of cases. Furthermore, individuals were categorized into four risk groups based on the two independent prognostic factors, LOS and EML, enabling the refinement of patients with different survival outcomes and suggesting that MRD should be closely monitored, as well as that HSCT should be considered in time among those subgroups with worse outcomes. To enhance the robustness of the findings, a larger cohort involving multiple medical centers is required for further verification of the results.
C-KIT mutations are reported to occur in 12−46% of adult t(8;21) AML patients [52,53,54,55], whereas they account for approximately 17−43% in pediatric t(8;21) patients [29,53,56,57,58,59]. The frequency of C-KIT in this study reached 60.0% (12/20), surpassing previous pediatric series [30,60]. This discrepancy could be owing to factors such as the small-sized sample from a single center, as well as the variations in the detection method and sequencing depth and coverage. Although C-KIT mutations mediate an adverse prognostic impact on the prognosis of adults with AML [61,62], the impact of C-KIT on pAML is still inconclusive [57,63]. Chen et al. [30] observed that C-KIT mutations are genetic markers linked to inferior prognoses in pAML patients. Another study indicated that C-KIT mutations were strongly correlated with poor outcome in t(8;21) pAML individuals [58]. In our study, despite the high frequency of C-KIT in t(8;21) pAML, it did not impact long-term prognosis, in line with previous pediatric reports [29,34]. This suggests potential differences in prognostic factors between pediatric and adult individuals diagnosed with this disease.
MRD is a pivotal marker in modern studies of pAML, with a commonly accepted threshold set at 0.1% [64]. MRD levels exceeding this threshold are linked to an elevated risk of relapse and unfavorable prognosis. In our study, MRD levels were quantified using MFCM following the first and second induction therapy phases in the CALSIII-AML18 protocol. However, the definitive prognostic value of MRD status derived from our findings may be inconclusive, likely due to the limited sample size.
The primary limitation of our study stems from its retrospective design, which may lead to missing data and an unavoidable bias. The power of the subsequent stratified analysis is constrained by the relatively small size of the subgroups and prospective research with a large-scale sample size is warranted to be practicable.
5. Conclusions
In conclusion, LOS is prognostically favorable, whereas EML is deemed to be strongly correlated with adverse prognoses in pediatric patients with t(8;21) AML. LOS combined with EML may help improve risk stratification and potentially facilitate the customization of future therapies.
Acknowledgments
We thank the pediatricians, patients and their guardians for participation in the study. This work was supported by the Medical Science Data Center in Shanghai Medical College of Fudan University.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children11050605/s1. Figure S1. Probability of survival for patients with t(8;21) AML in the protocols. Figure S2. Probability of survival depending on the C-KIT mutation in t(8;21) AML. Kaplan–Meier survival curves of OS (a), EFS (b) and RFS (c) for patients stratified by C-KIT mutation. Figure S3. Probability of survival depending on the Induction I MRD status in t(8;21) AML. Kaplan–Meier survival curves of OS (a), EFS (b) and RFS (c) for patients stratified by Induction I MRD status. Figure S4. Probability of survival depending on the Induction II MRD status in t(8;21) AML. Kaplan–Meier survival curves of OS (a), EFS (b) and RFS (c) for patients stratified by Induction II MRD status. Table S1. Definitions of end points. Table S2. Comparison of characteristics for patients with t(8;21) AML in differrent consecutive protocols. Table S3. Univariate and multivariate COX analyses of OS in 48 patients with t(8;21) AML. Table S4. Univariate and multivariate COX analyses of RFS in 48 patients with t(8;21) AML. Table S5. Univariate and multivariate COX analyses of overall survival (OS) in 48 patients with t(8;21) AML. Table S6. Univariate and multivariate COX analyses of overall survival (OS) in 20 t(8;21) AML patients who enrolled after 2018. Table S7. Univariate and multivariate COX analyses of relapse-free survival (RFS) in 48 patients with t(8;21) AML. Table S8. Univariate and multivariate COX analyses of relapse-free survival (RFS) in 20 t(8;21) AML patients who enrolled after 2018.
Author Contributions
Conceptualization, J.Y. and X.Z. (Xiaowen Zhai); methodology, J.Y. and H.W.; validation, J.Y., X.Z. (Xiaohua Zhu) and H.Z.; formal analysis, J.Y.; investigation, J.Y., X.Z. (Xiaohua Zhu) and H.Z.; resources, Y.F., Z.L. and Z.X.; data curation, Y.Y., P.C., J.L. (Jun Le), J.L. (Jun Li) and J.J.; writing—original draft preparation, J.Y.; writing—review and editing, J.Y., X.Z. (Xiaohua Zhu) and H.Z.; visualization, J.Y.; supervision, X.Z. (Xiaowen Zhai) and H.W.; project administration, X.Z. (Xiaohua Zhu) and H.Z.; funding acquisition, X.Z. (Xiaowen Zhai). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Children’s Hospital of Fudan University (9 December 2021; 2021-436).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are provided within the manuscript or Supplementary Information files.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
The work was supported by the National Key Research and Development Program of China (2022YFC2705003, 2023YFC2706301); the National Natural Science Foundation of China (82141125); Shanghai Municipal Committee of Science and Technology (21Y31900302); Shanghai Hospital Development Center (SHDC12019121); the Cyrus Tang Foundation (ZSBK0070).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Short N.J., Rytting M.E., Cortes J.E. Acute myeloid leukaemia. Lancet. 2018;392:593–606. doi: 10.1016/s0140-6736(18)31041-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Rooij J.D., Zwaan C.M., van den Heuvel-Eibrink M. Pediatric AML: From Biology to Clinical Management. J. Clin. Med. 2015;4:127–149. doi: 10.3390/jcm4010127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolouri H., Farrar J.E., Triche T., Jr., Ries R.E., Lim E.L., Alonzo T.A., Ma Y., Moore R., Mungall A.J., Marra M.A., et al. The molecular landscape of pediatric acute myeloid leukemia reveals recurrent structural alterations and age-specific mutational interactions. Nat. Med. 2018;24:103–112. doi: 10.1038/nm.4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pui C.H., Carroll W.L., Meshinchi S., Arceci R.J. Biology, risk stratification, and therapy of pediatric acute leukemias: An update. J. Clin. Oncol. 2011;29:551–565. doi: 10.1200/jco.2010.30.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arber D.A., Orazi A., Hasserjian R., Thiele J., Borowitz M.J., Le Beau M.M., Bloomfield C.D., Cazzola M., Vardiman J.W. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–2405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 6.Sood R., Kamikubo Y., Liu P. Role of RUNX1 in hematological malignancies. Blood. 2017;129:2070–2082. doi: 10.1182/blood-2016-10-687830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu H.H., Zhang X.H., Qin Y.Z., Liu D.H., Jiang H., Chen H., Jiang Q., Xu L.P., Lu J., Han W., et al. MRD-directed risk stratification treatment may improve outcomes of t(8;21) AML in the first complete remission: Results from the AML05 multicenter trial. Blood. 2013;121:4056–4062. doi: 10.1182/blood-2012-11-468348. [DOI] [PubMed] [Google Scholar]
- 8.Imamura T., Iwamoto S., Kanai R., Shimada A., Terui K., Osugi Y., Kobayashi R., Tawa A., Kosaka Y., Kato K., et al. Outcome in 146 patients with paediatric acute myeloid leukaemia treated according to the AML99 protocol in the period 2003-06 from the Japan Association of Childhood Leukaemia Study. Br. J. Haematol. 2012;159:204–210. doi: 10.1111/bjh.12030. [DOI] [PubMed] [Google Scholar]
- 9.Tomizawa D., Yoshida M., Kondo T., Miyamura T., Taga T., Adachi S., Koh K., Noguchi M., Kakuda H., Watanabe K., et al. Allogeneic hematopoietic stem cell transplantation for children and adolescents with high-risk cytogenetic AML: Distinctly poor outcomes of FUS-ERG-positive cases. Bone Marrow Transplant. 2019;54:393–401. doi: 10.1038/s41409-018-0273-7. [DOI] [PubMed] [Google Scholar]
- 10.Kellaway S., Chin P.S., Barneh F., Bonifer C., Heidenreich O. t(8;21) Acute Myeloid Leukemia as a Paradigm for the Understanding of Leukemogenesis at the Level of Gene Regulation and Chromatin Programming. Cells. 2020;9:2681. doi: 10.3390/cells9122681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Creutzig U., Zimmermann M., Ritter J., Reinhardt D., Hermann J., Henze G., Jürgens H., Kabisch H., Reiter A., Riehm H., et al. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia. 2005;19:2030–2042. doi: 10.1038/sj.leu.2403920. [DOI] [PubMed] [Google Scholar]
- 12.Yang W., Qin M., Jia C., Yang J., Chen W., Luo Y., Jing Y., Wang B. Pediatric acute myeloid leukemia patients with KMT2A rearrangements: A single-center retrospective study. Hematology. 2022;27:583–589. doi: 10.1080/16078454.2022.2071797. [DOI] [PubMed] [Google Scholar]
- 13.Bennett J.M., Catovsky D., Daniel M.T., Flandrin G., Galton D.A., Gralnick H.R., Sultan C. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br. J. Haematol. 1976;33:451–458. doi: 10.1111/j.1365-2141.1976.tb03563.x. [DOI] [PubMed] [Google Scholar]
- 14.Bennett J.M., Catovsky D., Daniel M.T., Flandrin G., Galton D.A., Gralnick H.R., Sultan C. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann. Intern. Med. 1985;103:620–625. doi: 10.7326/0003-4819-103-4-620. [DOI] [PubMed] [Google Scholar]
- 15.Arber D., Brunning R., Le Beau M. Acute myeloid leukemia with recurrent genetic abnormalities. In: Swerdlow S.H., Campo E., Harris N.L., Jaffe E.S., Pileri S.A., Stein H., Thiele J., Vardiman J.W., editors. World Health Organization Classification of Tumors of Haematopoietic and Lymphoid Tissues. 4th ed. WHO Press; Geneva, Switzerland: 2008. pp. 116–117. [Google Scholar]
- 16.Haferlach C., Rieder H., Lillington D.M., Dastugue N., Hagemeijer A., Harbott J., Stilgenbauer S., Knuutila S., Johansson B., Fonatsch C. Proposals for standardized protocols for cytogenetic analyses of acute leukemias, chronic lymphocytic leukemia, chronic myeloid leukemia, chronic myeloproliferative disorders, and myelodysplastic syndromes. Genes. Chromosomes Cancer. 2007;46:494–499. doi: 10.1002/gcc.20433. [DOI] [PubMed] [Google Scholar]
- 17.Schoch C., Schnittger S., Bursch S., Gerstner D., Hochhaus A., Berger U., Hehlmann R., Hiddemann W., Haferlach T. Comparison of chromosome banding analysis, interphase- and hypermetaphase-FISH, qualitative and quantitative PCR for diagnosis and for follow-up in chronic myeloid leukemia: A study on 350 cases. Leukemia. 2002;16:53–59. doi: 10.1038/sj.leu.2402329. [DOI] [PubMed] [Google Scholar]
- 18.Shaffer L.G., Tommerup N. ISCN 2005: An International System for Human Cytogenetic Nomenclature (2005): Recommendations of the International Standing Committee on Human Cytogenetic Nomenclature. Karger Medical and Scientific Publishers; Basel, Switzerland: 2005. [Google Scholar]
- 19.Wiktor A., Rybicki B.A., Piao Z.S., Shurafa M., Barthel B., Maeda K., Van Dyke D.L. Clinical significance of Y chromosome loss in hematologic disease. Genes. Chromosomes Cancer. 2000;27:11–16. doi: 10.1002/(SICI)1098-2264(200001)27:1<11::AID-GCC2>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 20.Döhner H., Estey E., Grimwade D., Amadori S., Appelbaum F.R., Büchner T., Dombret H., Ebert B.L., Fenaux P., Larson R.A., et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–447. doi: 10.1182/blood-2016-08-733196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breems D.A., Van Putten W.L., De Greef G.E., Van Zelderen-Bhola S.L., Gerssen-Schoorl K.B., Mellink C.H., Nieuwint A., Jotterand M., Hagemeijer A., Beverloo H.B., et al. Monosomal karyotype in acute myeloid leukemia: A better indicator of poor prognosis than a complex karyotype. J. Clin. Oncol. 2008;26:4791–4797. doi: 10.1200/jco.2008.16.0259. [DOI] [PubMed] [Google Scholar]
- 22.Weinberg O.K., Ohgami R.S., Ma L., Seo K., Ren L., Gotlib J.R., Seetharam M., Cherry A., Arber D.A. Acute myeloid leukemia with monosomal karyotype: Morphologic, immunophenotypic, and molecular findings. Am. J. Clin. Pathol. 2014;142:190–195. doi: 10.1309/ajcpmlo84jdnvlnk. [DOI] [PubMed] [Google Scholar]
- 23.Kern W., Voskova D., Schoch C., Hiddemann W., Schnittger S., Haferlach T. Determination of relapse risk based on assessment of minimal residual disease during complete remission by multiparameter flow cytometry in unselected patients with acute myeloid leukemia. Blood. 2004;104:3078–3085. doi: 10.1182/blood-2004-03-1036. [DOI] [PubMed] [Google Scholar]
- 24.Kern W., Bacher U., Haferlach C., Schnittger S., Haferlach T. The role of multiparameter flow cytometry for disease monitoring in AML. Best. Pract. Res. Clin. Haematol. 2010;23:379–390. doi: 10.1016/j.beha.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Schnittger S., Schoch C., Dugas M., Kern W., Staib P., Wuchter C., Löffler H., Sauerland C.M., Serve H., Büchner T., et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: Correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood. 2002;100:59–66. doi: 10.1182/blood.v100.1.59. [DOI] [PubMed] [Google Scholar]
- 26.O’Donnell M.R., Tallman M.S., Abboud C.N., Altman J.K., Appelbaum F.R., Arber D.A., Attar E., Borate U., Coutre S.E., Damon L.E., et al. Acute myeloid leukemia, version 2.2013. J. Natl. Compr. Canc. Netw. 2013;11:1047–1055. doi: 10.6004/jnccn.2013.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheson B.D., Bennett J.M., Kopecky K.J., Büchner T., Willman C.L., Estey E.H., Schiffer C.A., Doehner H., Tallman M.S., Lister T.A., et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J. Clin. Oncol. 2003;21:4642–4649. doi: 10.1200/jco.2003.04.036. [DOI] [PubMed] [Google Scholar]
- 28.Hosmer D.W., Jr., Lemeshow S., Sturdivant X.R. Applied Logistic Regression, Third Edition. Technometrics. 1992;34:358–359. [Google Scholar]
- 29.Klein K., Kaspers G., Harrison C.J., Beverloo H.B., Reedijk A., Bongers M., Cloos J., Pession A., Reinhardt D., Zimmerman M., et al. Clinical Impact of Additional Cytogenetic Aberrations, cKIT and RAS Mutations, and Treatment Elements in Pediatric t(8;21)-AML: Results From an International Retrospective Study by the International Berlin-Frankfurt-Münster Study Group. J. Clin. Oncol. 2015;33:4247–4258. doi: 10.1200/jco.2015.61.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen X., Dou H., Wang X., Huang Y., Lu L., Bin J., Su Y., Zou L., Yu J., Bao L. KIT mutations correlate with adverse survival in children with core-binding factor acute myeloid leukemia. Leuk. Lymphoma. 2018;59:829–836. doi: 10.1080/10428194.2017.1361025. [DOI] [PubMed] [Google Scholar]
- 31.Wu J., Zhang L.P., Lu A.D., Wang B., Cheng Y.F., Liu G.L. [Clinical features and prognosis of t (8; 21)/AML1-ETO-positive childhood acute myeloid leukemia] Zhongguo Dang Dai Er Ke Za Zhi. 2011;13:931–935. [PubMed] [Google Scholar]
- 32.Che L., Xu Y., Pang L., He H., Hu S., Wang Y., Lu J., Ji Z., He Y., Huang Y., et al. Clinical characteristics and prognosis of core binding factor positive acute myeloid leukemia in children. Chin. J. Appl. Clin. Pediatr. 2014;29:207–211. [Google Scholar]
- 33.Gibson B.E., Webb D.K., Howman A.J., De Graaf S.S., Harrison C.J., Wheatley K. Results of a randomized trial in children with Acute Myeloid Leukaemia: Medical research council AML12 trial. Br. J. Haematol. 2011;155:366–376. doi: 10.1111/j.1365-2141.2011.08851.x. [DOI] [PubMed] [Google Scholar]
- 34.Fan G.L., Jiang P.J., Yuan M. [Clinical Prognostic Factors Analysis of Initially Treated AML Children with t(8;21)/RUNX1-RUNX1T1] Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2020;28:1510–1515. doi: 10.19746/j.cnki.issn.1009-2137.2020.05.014. [DOI] [PubMed] [Google Scholar]
- 35.Walter R.B., Kantarjian H.M., Huang X., Pierce S.A., Sun Z., Gundacker H.M., Ravandi F., Faderl S.H., Tallman M.S., Appelbaum F.R., et al. Effect of complete remission and responses less than complete remission on survival in acute myeloid leukemia: A combined Eastern Cooperative Oncology Group, Southwest Oncology Group, and M. D. Anderson Cancer Center Study. J. Clin. Oncol. 2010;28:1766–1771. doi: 10.1200/jco.2009.25.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grimwade D., Walker H., Oliver F., Wheatley K., Harrison C., Harrison G., Rees J., Hann I., Stevens R., Burnett A., et al. The importance of diagnostic cytogenetics on outcome in AML: Analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood. 1998;92:2322–2333. doi: 10.1182/blood.V92.7.2322. [DOI] [PubMed] [Google Scholar]
- 37.von Neuhoff C., Reinhardt D., Sander A., Zimmermann M., Bradtke J., Betts D.R., Zemanova Z., Stary J., Bourquin J.P., Haas O.A., et al. Prognostic impact of specific chromosomal aberrations in a large group of pediatric patients with acute myeloid leukemia treated uniformly according to trial AML-BFM 98. J. Clin. Oncol. 2010;28:2682–2689. doi: 10.1200/jco.2009.25.6321. [DOI] [PubMed] [Google Scholar]
- 38.Raimondi S.C., Chang M.N., Ravindranath Y., Behm F.G., Gresik M.V., Steuber C.P., Weinstein H.J., Carroll A.J. Chromosomal abnormalities in 478 children with acute myeloid leukemia: Clinical characteristics and treatment outcome in a cooperative pediatric oncology group study-POG 8821. Blood. 1999;94:3707–3716. [PubMed] [Google Scholar]
- 39.Rubnitz J.E., Raimondi S.C., Halbert A.R., Tong X., Srivastava D.K., Razzouk B.I., Pui C.H., Downing J.R., Ribeiro R.C., Behm F.G. Characteristics and outcome of t(8;21)-positive childhood acute myeloid leukemia: A single institution’s experience. Leukemia. 2002;16:2072–2077. doi: 10.1038/sj.leu.2402633. [DOI] [PubMed] [Google Scholar]
- 40.Creutzig U., Zimmermann M., Bourquin J.P., Dworzak M.N., Fleischhack G., Graf N., Klingebiel T., Kremens B., Lehrnbecher T., von Neuhoff C., et al. Randomized trial comparing liposomal daunorubicin with idarubicin as induction for pediatric acute myeloid leukemia: Results from Study AML-BFM 2004. Blood. 2013;122:37–43. doi: 10.1182/blood-2013-02-484097. [DOI] [PubMed] [Google Scholar]
- 41.Betts D.R., Ammann R.A., Hirt A., Hengartner H., Beck-Popovic M., Kuhne T., Nobile L., Caflisch U., Wacker P., Niggli F.K. The prognostic significance of cytogenetic aberrations in childhood acute myeloid leukaemia. A study of the Swiss Paediatric Oncology Group (SPOG) Eur. J. Haematol. 2007;78:468–476. doi: 10.1111/j.1600-0609.2007.00854.x. [DOI] [PubMed] [Google Scholar]
- 42.Schlenk R.F., Benner A., Krauter J., Büchner T., Sauerland C., Ehninger G., Schaich M., Mohr B., Niederwieser D., Krahl R., et al. Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: A survey of the German Acute Myeloid Leukemia Intergroup. J. Clin. Oncol. 2004;22:3741–3750. doi: 10.1200/jco.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 43.Zhou W., Chen G., Gong D., Li Y., Huang S., Wang N., Xu Q., Xiong Q., Jing Y., Lv N., et al. Loss of the Y chromosome predicts a high relapse risk in younger adult male patients with t(8;21) acute myeloid leukemia on high-dose cytarabine consolidation therapy: A retrospective multicenter study. Leuk. Lymphoma. 2020;61:820–830. doi: 10.1080/10428194.2019.1683734. [DOI] [PubMed] [Google Scholar]
- 44.Schoch C., Haase D., Haferlach T., Gudat H., Büchner T., Freund M., Link H., Lengfelder E., Wandt H., Sauerland M.C., et al. Fifty-one patients with acute myeloid leukemia and translocation t(8;21)(q22;q22): An additional deletion in 9q is an adverse prognostic factor. Leukemia. 1996;10:1288–1295. [PubMed] [Google Scholar]
- 45.Wu J., Lu A.D., Zhang L.P., Zuo Y.X., Jia Y.P. [Study of clinical outcome and prognosis in pediatric core binding factor-acute myeloid leukemia] Zhonghua Xue Ye Xue Za Zhi. 2019;40:52–57. doi: 10.3760/cma.j.issn.0253-2727.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mitterbauer M., Kusec R., Schwarzinger I., Haas O.A., Lechner K., Jaeger U. Comparison of karyotype analysis and RT-PCR for AML1/ETO in 204 unselected patients with AML. Ann. Hematol. 1998;76:139–143. doi: 10.1007/s002770050378. [DOI] [PubMed] [Google Scholar]
- 47.Chen G., Zhou W., Gong D., Li Y., Huang S., Wang N., Xu Q., Xiong Q., Jing Y., Lv N., et al. Loss of X chromosome predicts favorable prognosis in female patients with t(8;21) acute myeloid leukemia. Leuk. Lymphoma. 2020;61:1168–1177. doi: 10.1080/10428194.2019.1709836. [DOI] [PubMed] [Google Scholar]
- 48.Byrd J.C., Weiss R.B., Arthur D.C., Lawrence D., Baer M.R., Davey F., Trikha E.S., Carroll A.J., Tantravahi R., Qumsiyeh M., et al. Extramedullary leukemia adversely affects hematologic complete remission rate and overall survival in patients with t(8;21)(q22;q22): Results from Cancer and Leukemia Group B 8461. J. Clin. Oncol. 1997;15:466–475. doi: 10.1200/jco.1997.15.2.466. [DOI] [PubMed] [Google Scholar]
- 49.Støve H.K., Sandahl J.D., Abrahamsson J., Asdahl P.H., Forestier E., Ha S.Y., Jahnukainen K., Jónsson Ó.G., Lausen B., Palle J., et al. Extramedullary leukemia in children with acute myeloid leukemia: A population-based cohort study from the Nordic Society of Pediatric Hematology and Oncology (NOPHO) Pediatr. Blood Cancer. 2017;64 doi: 10.1002/pbc.26520. [DOI] [PubMed] [Google Scholar]
- 50.Hu G., Lu A., Wu J., Jia Y., Zuo Y., Ding M., Zhang L. Characteristics and prognosis of pediatric myeloid sarcoma in the cytogenetic context of t(8;21) Pediatr. Hematol. Oncol. 2021;38:14–24. doi: 10.1080/08880018.2020.1803462. [DOI] [PubMed] [Google Scholar]
- 51.Bisschop M.M., Révész T., Bierings M., van Weerden J.F., van Wering E.R., Hählen K., van der Does-van den Berg A. Extramedullary infiltrates at diagnosis have no prognostic significance in children with acute myeloid leukaemia. Leukemia. 2001;15:46–49. doi: 10.1038/sj.leu.2401971. [DOI] [PubMed] [Google Scholar]
- 52.Krauth M.T., Eder C., Alpermann T., Bacher U., Nadarajah N., Kern W., Haferlach C., Haferlach T., Schnittger S. High number of additional genetic lesions in acute myeloid leukemia with t(8;21)/RUNX1-RUNX1T1: Frequency and impact on clinical outcome. Leukemia. 2014;28:1449–1458. doi: 10.1038/leu.2014.4. [DOI] [PubMed] [Google Scholar]
- 53.Shih L.Y., Liang D.C., Huang C.F., Chang Y.T., Lai C.L., Lin T.H., Yang C.P., Hung I.J., Liu H.C., Jaing T.H., et al. Cooperating mutations of receptor tyrosine kinases and Ras genes in childhood core-binding factor acute myeloid leukemia and a comparative analysis on paired diagnosis and relapse samples. Leukemia. 2008;22:303–307. doi: 10.1038/sj.leu.2404995. [DOI] [PubMed] [Google Scholar]
- 54.Chen W., Xie H., Wang H., Chen L., Sun Y., Chen Z., Li Q. Prognostic Significance of KIT Mutations in Core-Binding Factor Acute Myeloid Leukemia: A Systematic Review and Meta-Analysis. PLoS ONE. 2016;11:e0146614. doi: 10.1371/journal.pone.0146614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cairoli R., Beghini A., Grillo G., Nadali G., Elice F., Ripamonti C.B., Colapietro P., Nichelatti M., Pezzetti L., Lunghi M., et al. Prognostic impact of c-KIT mutations in core binding factor leukemias: An Italian retrospective study. Blood. 2006;107:3463–3468. doi: 10.1182/blood-2005-09-3640. [DOI] [PubMed] [Google Scholar]
- 56.Tarlock K., Alonzo T.A., Wang Y.C., Gerbing R.B., Ries R., Loken M.R., Pardo L., Hylkema T., Joaquin J., Sarukkai L., et al. Functional Properties of KIT Mutations Are Associated with Differential Clinical Outcomes and Response to Targeted Therapeutics in CBF Acute Myeloid Leukemia. Clin. Cancer Res. 2019;25:5038–5048. doi: 10.1158/1078-0432.Ccr-18-1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pollard J.A., Alonzo T.A., Gerbing R.B., Ho P.A., Zeng R., Ravindranath Y., Dahl G., Lacayo N.J., Becton D., Chang M., et al. Prevalence and prognostic significance of KIT mutations in pediatric patients with core binding factor AML enrolled on serial pediatric cooperative trials for de novo AML. Blood. 2010;115:2372–2379. doi: 10.1182/blood-2009-09-241075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shimada A., Taki T., Tabuchi K., Tawa A., Horibe K., Tsuchida M., Hanada R., Tsukimoto I., Hayashi Y. KIT mutations, and not FLT3 internal tandem duplication, are strongly associated with a poor prognosis in pediatric acute myeloid leukemia with t(8;21): A study of the Japanese Childhood AML Cooperative Study Group. Blood. 2006;107:1806–1809. doi: 10.1182/blood-2005-08-3408. [DOI] [PubMed] [Google Scholar]
- 59.Manara E., Bisio V., Masetti R., Beqiri V., Rondelli R., Menna G., Micalizzi C., Santoro N., Locatelli F., Basso G., et al. Core-binding factor acute myeloid leukemia in pediatric patients enrolled in the AIEOP AML 2002/01 trial: Screening and prognostic impact of c-KIT mutations. Leukemia. 2014;28:1132–1134. doi: 10.1038/leu.2013.339. [DOI] [PubMed] [Google Scholar]
- 60.Mao X., Yin R., Liu L., Zhou Y., Yang C., Fang C., Jiang H., Guo Q., Tian X. Clinical impact of c-KIT and CEBPA mutations in 33 patients with corebinding factor (Non-M3) acute myeloid leukemia. Pediatr. Neonatol. 2023;64:435–441. doi: 10.1016/j.pedneo.2022.05.020. [DOI] [PubMed] [Google Scholar]
- 61.Shimoni A., Labopin M., Savani B., Volin L., Ehninger G., Kuball J., Bunjes D., Schaap N., Vigouroux S., Bacigalupo A., et al. Long-term survival and late events after allogeneic stem cell transplantation from HLA-matched siblings for acute myeloid leukemia with myeloablative compared to reduced-intensity conditioning: A report on behalf of the acute leukemia working party of European group for blood and marrow transplantation. J. Hematol. Oncol. 2016;9:118. doi: 10.1186/s13045-016-0347-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ishikawa Y., Kawashima N., Atsuta Y., Sugiura I., Sawa M., Dobashi N., Yokoyama H., Doki N., Tomita A., Kiguchi T., et al. Prospective evaluation of prognostic impact of KIT mutations on acute myeloid leukemia with RUNX1-RUNX1T1 and CBFB-MYH11. Blood Adv. 2020;4:66–75. doi: 10.1182/bloodadvances.2019000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Forghieri F., Comoli P., Marasca R., Potenza L., Luppi M. Minimal/Measurable Residual Disease Monitoring in NPM1-Mutated Acute Myeloid Leukemia: A Clinical Viewpoint and Perspectives. Int. J. Mol. Sci. 2018;19:3492. doi: 10.3390/ijms19113492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schuurhuis G.J., Heuser M., Freeman S., Béné M.C., Buccisano F., Cloos J., Grimwade D., Haferlach T., Hills R.K., Hourigan C.S., et al. Minimal/measurable residual disease in AML: A consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–1291. doi: 10.1182/blood-2017-09-801498. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are provided within the manuscript or Supplementary Information files.