Abstract
Background
Canadians are engaged in an intense debate about the relative merits of private for-profit versus private not-for-profit health care delivery. To inform this debate, we undertook a systematic review and meta-analysis of studies comparing the mortality rates of private for-profit hospitals and those of private not-for-profit hospitals.
Methods
We identified studies through an electronic search of 11 bibliographical databases, our own files, consultation with experts, reference lists, PubMed and SciSearch. We masked the study results before determining study eligibility. Our eligibility criteria included observational studies or randomized controlled trials that compared private for-profit and private not-for-profit hospitals. We excluded studies that evaluated mortality rates in hospitals with a particular profit status that subsequently converted to the other profit status. For each study, we calculated a relative risk of mortality for private for-profit hospitals relative to private not-for-profit hospitals and pooled the studies of adult populations that included adjustment for potential confounders (e.g., teaching status, severity of illness) using a random effects model.
Results
Fifteen observational studies, involving more than 26 000 hospitals and 38 million patients, fulfilled the eligibility criteria. In the studies of adult populations, with adjustment for potential confounders, private for-profit hospitals were associated with an increased risk of death (relative risk [RR] 1.020, 95% confidence interval [CI] 1.003–1.038; p = 0.02). The one perinatal study with adjustment for potential confounders also showed an increased risk of death in private for-profit hospitals (RR 1.095, 95% CI 1.050–1.141; p < 0.0001).
Interpretation
Our meta-analysis suggests that private for-profit ownership of hospitals, in comparison with private not-for-profit ownership, results in a higher risk of death for patients.
Canadian health policy-makers are considering an expansion of private for-profit health care delivery, including private for-profit hospitals.1 Most of the debate has focused on whether private for-profit health care facilities can contain costs more effectively,2,3,4,5 avoid differential access to health services (i.e., two-tier medicine)6 and avoid letting foreign investors influence Canadian health care policy through the North American Free Trade Agreement (NAFTA).7 What has been missing from this debate is consideration of the potential health outcomes of the proposed expansion of private for-profit health services.
Health care can be separated into 2 essential and distinct components: funding (i.e., who pays for health care) and delivery (i.e., who owns and administers the institutions or services that provide the care). Both funding and delivery can be public or private. Public funding means paid for by government (e.g., through the use of tax dollars); public delivery means government ownership and administration of health care facilities. Private funding and private delivery can both be for-profit or not-for-profit. On the funding side, insurance companies that channel premiums to pay for health care can be private for-profit or private not-for-profit. On the delivery side, hospitals and other health care delivery institutions that are private for-profit corporations are owned by shareholders or investors. Private hospitals can also be not-for-profit institutions that are owned by religious organizations, communities, regional health authorities or the hospital boards.
Public funding is the main method by which Canadian hospitals obtain revenue. However, 95% of Canadian hospitals are private not-for-profit institutions.8 Because Canadians commonly use the term “public hospitals” to refer to private not-for-profit hospitals, many are unaware of the private ownership and administration of our hospitals.9
This study addresses issues of health care delivery, rather than health care funding. We undertook a systematic review and a meta-analysis to address the following question: What is the relative effect of private for-profit versus private not-for-profit delivery of hospital care on patient mortality?
Methods
We evaluated hospital mortality rates as a component of a larger systematic review that we are undertaking to compare health outcomes, quality and appropriateness of care, and cost in private for-profit versus private not-for-profit health care delivery systems. This publication presents the results of the hospital mortality review. The study process is outlined in Fig. 1.
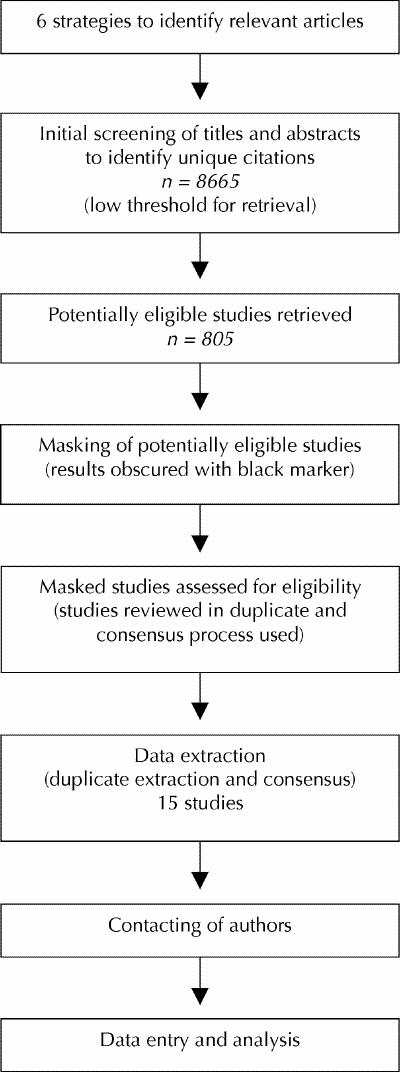
Fig. 1: Study process.
We used 6 strategies to identify studies: an electronic search of 11 bibliographical databases; our own files; consultation with experts from several continents; a review of reference lists from articles that fulfilled our eligibility criteria; PubMed, using the “related articles” feature for all studies meeting our entry criteria; and SciSearch, for publications that cited any studies that fulfilled our entry criteria.
We used all the studies that we were initially aware of to identify medical subject heading terms and key words for the search. A librarian (N.B.) undertook an iterative process, for each database, to refine the search strategy through testing of several search terms and incorporation of new search terms as new relevant citations were identified. The search included the following databases: EMBASE (1980–2001), MEDLINE (1966–2001), HEALTHSTAR (1975–2001), CINAHL (1982–2001), BIOETHICSLINE (1973–2000), Wilson Business Abstracts (1997–2001), EconLit (1969–2001), Cochrane Library (2001, issue 3), Dissertation Abstracts Ondisc (1861–2001), ABI/ INFORM (1970–2001) and NTIS (1964–2002). Complete listings of the database search strategies are available from the authors.
Our 6 strategies identified 8665 unique citations. Teams consisting of 2 individuals independently screened the titles and abstracts of each citation and identified all citations for full review when there was any possibility that the study contained a comparison we were interested in. This screening process yielded 805 full-text publications identified by one or both of the individuals in each team for full review (Fig. 1).
We masked the results (i.e., obscured them with a black marker from the tables and text) of all publications selected for full review. Teams of 2 individuals independently evaluated each masked article to determine eligibility. Our agreement on studies evaluated within teams was excellent (κ 0.83, 95% confidence interval [CI] 0.73–0.93). All disagreements were resolved by consensus. The consensus process required individuals to discuss the reasoning for their decisions. If one individual realized that she or he had made an error, then the process was complete. This occurred in all cases, and therefore an independent third adjudicator was never required to resolve disagreements. Teams reviewed masked articles that they had not assessed during the screening process.
We included observational studies or randomized controlled trials (RCTs) that compared patient mortality in private for-profit and private not-for-profit hospitals. We excluded studies that evaluated health care delivery systems with a particular profit status (e.g., private not-for-profit) that subsequently converted to another profit status (e.g., private for-profit), because the comparisons are confounded by potential differences in patient populations and medical interventions over time and uncertainty regarding the time required to create functional change after an alteration in ownership status.
We assessed the following characteristics in all the observational studies that met the eligibility criteria: sampling method, type of hospitals evaluated (e.g., general medical and surgical hospitals, hospitals with maternity services), date when data collection was initiated and completed, duration of patient follow-up, source(s) of health care financing (e.g., public, private insurance), case mix of patients (e.g., medical disorders, surgical disorders), source of data (e.g., administrative database, patient chart), number of hospitals and patients evaluated, mortality results and whether there was adjustment for potential confounders in the analyses. Teams of 2 individuals independently abstracted data from all the studies that fulfilled our eligibility criteria. Disagreements were resolved by consensus using the same process discussed earlier. Our overall agreement was 93% for the data abstraction. We attempted to contact all authors when data were missing.
To eliminate hospital teaching status as a potential confounder, we included the results from private for-profit nonteaching and private not-for-profit nonteaching hospitals when these data were available. If a study reported 2 separate adjusted analyses, we included the results from the analysis with the most appropriate adjustment. We considered it appropriate to adjust for patients' severity of illness and socioeconomic status, hospital teaching status and other variables that could confound the comparison of interest. Where possible, we avoided adjustment for variables that are under the control of hospital administrators, which may be influenced by profit status and may affect mortality. These variables include hospital staffing levels (e.g., the number of registered nurses per bed, registered pharmacists per bed) after adjustment for patients' severity of illness has already been undertaken.
Before carrying out the analysis, we specified several hypotheses to test potential explanations for variability (i.e., heterogeneity) in the direction and magnitude of effect among studies. We hypothesized that the effect size may differ based on whether the analysis adjusted for potential confounders; whether we incorporated an estimate of the sample size into the calculation to determine the effect size; the duration of patient follow-up (i.e., in hospital, or for 30 days or 90 days after admission); the source of health care funding; the data source; whether the hospitals belonged to a chain or were free-standing organizations; whether the patient population was adult or pediatric; and, for studies involving US Medicare patients, whether the data collection occurred before 1984 (when US Medicare switched from a cost-based reimbursement scheme, whereby hospitals were reimbursed for the costs associated with a patient's care, to a prospective payment system whereby hospitals are reimbursed based on the patient's designated diagnosis).
For each study, we computed the relative risk of mortality in private for-profit hospitals relative to private not-for-profit hospitals (see the Appendix on the CMAJ Web site for details). We pooled these relative risks using a random effects model10 and tested for heterogeneity using a χ2 test. A meta-analysis program written by one of the authors (B.W.) was used. We evaluated a funnel plot for evidence of publication bias.11
The Hamilton Health Sciences Research Ethics Board in Hamilton, Ont., approved this study protocol.
Results
We identified 13 publications that reported 15 observational studies that met our eligibility criteria.12,13,14,15,16,17,18,19,20,21,22,23,24 Three publications identified as fulfilling our eligibility criteria were subsequently excluded, because 2 were duplicate publications of included studies, and in one publication the patient population was a subset of a larger population from an included study.25,26,27 We also identified 19 publications that we felt might be eligible but required further information or data, or both, from the authors. After contacting authors, we confirmed that these studies either did not address our study question or the authors could not provide the necessary data. Studies that did address our question but did not contain data that we could use all suggested an advantage for private not-for-profit hospitals (Table 1).28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46
Table 1
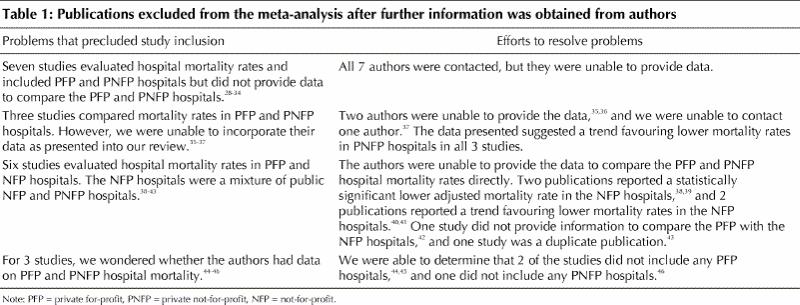
Tables 2 and 3 (Table 3 is available in electronic format on the CMAJ Web site) present the study characteristics and the study methodology respectively for the 15 observational studies included in our systematic review. These studies were all conducted in the United States, and in most studies patient health care was publicly funded through Medicare. Most studies included general acute care, medical and surgical patients, and one study specifically examined maternity services.18 Data in these studies came from about 38 million patients admitted from 1982 to 1995 to 26 000 hospitals, and the most frequent patient follow-up period was 30 days after admission to hospital. All studies used administrative data.
Table 2
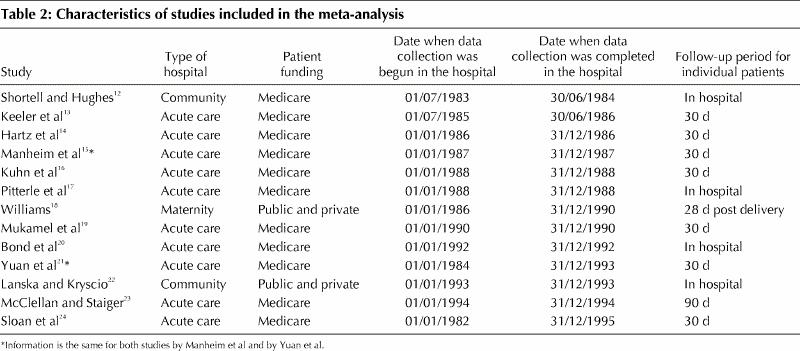
Of the 14 studies that evaluated adult populations and adjusted for potential confounders, 6 had a statistically significant lower relative risk of death in the private not-for-profit hospitals,14,16,17,20,21,23 and one had a statistically significant lower relative risk of death in the private for-profit hospitals (Fig. 2).19 Meta-analysis of these 14 studies demonstrated that private for-profit hospitals were associated with an increased risk of death (relative risk [RR] 1.020, 95% CI 1.003–1.038; p = 0.02).
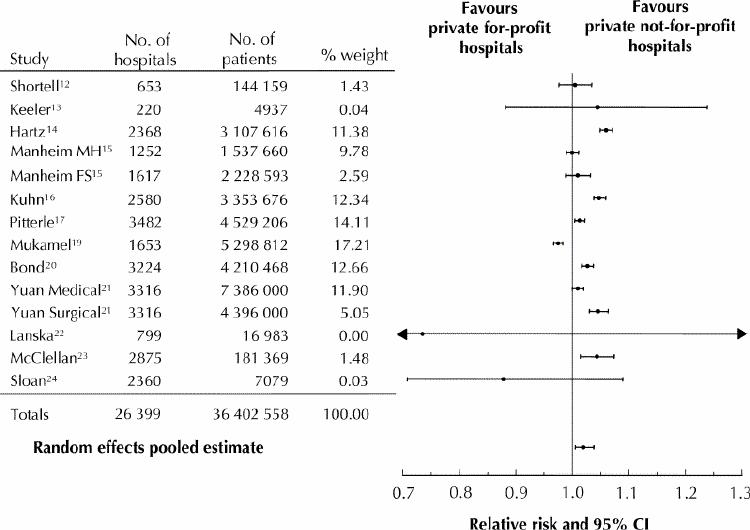
Fig. 2: Relative risk of hospital mortality for adult patients in private for-profit hospitals relative to private not-for-profit hospitals. CI = confidence intervals.
One study of perinatal mortality that evaluated 1 642 002 patients in 243 hospitals and adjusted for potential confounders also demonstrated an increased risk of death in private for-profit hospitals (RR 1.095, 95% CI 1.050–1.141; p < 0.0001).18
Two studies reported analyses that appropriately adjusted for patients' severity of illness and separate analyses that also adjusted for staffing levels (e.g., registered nurses as a proportion of all nurses, board-certified specialists as a proportion of all physicians, registered pharmacists per occupied bed).14,20 In both studies, the risk of higher mortality associated with private for-profit hospitals decreased in the latter analysis. Hartz and colleagues reported a decrease in relative risk from 1.06 to 1.04, and Bond and coworkers reported a decrease from 1.03 to 1.01, in the analysis that adjusted for variables under the control of hospital administrators.14,20
We explored potential sources of variability in the study results based on our predefined hypotheses. We found different summary estimates for the studies that evaluated adult populations compared with the study that evaluated a perinatal population (p = 0.002); the impact of the private not-for-profit hospitals in lowering mortality was larger in the perinatal study. Because of these findings, we did not include the study that evaluated a perinatal population in the pooled analysis. The p values for the difference in summary estimates in each pair of subgroups defined in our other hypotheses were all greater than 0.10, indicating no significant difference in subgroup summary estimates. Our pooled estimate of the adult population studies with adjustment for confounding had heterogeneity (p = 0.02) that we could not explain. The funnel plot did not suggest publication bias (Fig. 3).
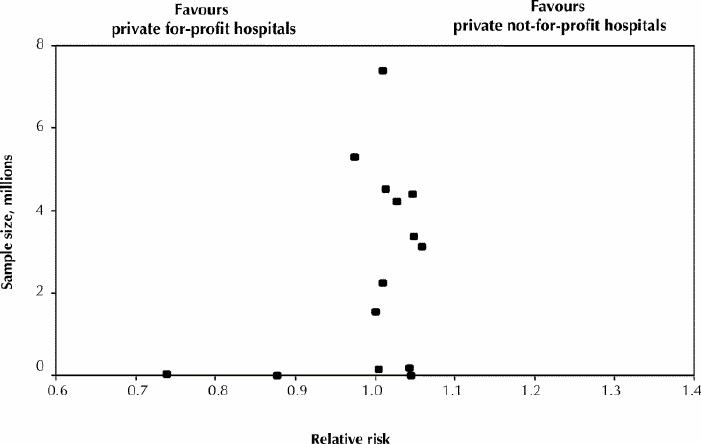
Fig. 3: Funnel plot of relative risk, in adult studies, of death in private for-profit hospitals relative to private not-for-profit hospitals.
Interpretation
Our systematic review identified 15 observational studies that compared private for-profit with private not-for-profit hospital mortality. These studies uniformly met quality criteria regarding adjustment for potential confounders, in particular, patients' severity of illness or surrogate markers of severity of illness, and complete accounting of deaths. Our pooled analysis of the adult population studies demonstrated that private for-profit hospitals were associated with a statistically significant increase in the risk of death.
We are aware of 2 earlier reviews in this area. The New York Academy of Medicine has reported a qualitative review that compared access, costs, quality of care, education and research in for-profit and not-for-profit hospitals, managed care organizations and nursing homes.47 This review only included 4 of the 15 studies we identified and reached the general conclusion that the studies evaluated provided no clear indication as to the superiority of either hospital system regarding the quality of care and health outcomes.47 The second review focused on the public purchasing of private surgical services.48 This qualitative review identified 7 of the 15 studies we included and reached the general conclusion that more research was needed.
We undertook multiple strategies to identify studies, including searching 11 bibliographical databases, and found a number of studies not included in earlier reviews (see preceding paragraph). We masked study results before determining study eligibility. Our agreement on study inclusion was high as was our agreement during data abstraction. We were also successful in confirming and obtaining information from authors (see Appendix49). We were able to identify 15 studies with very large sample sizes that adjusted for potential confounders.
Our systematic review has several limitations. The most important is that we were unable to identify any RCTs. It is unlikely that RCTs will ever be undertaken to study this question, thus the strongest feasible design for addressing our question is observational. However, all 15 studies we identified did adjust for potential confounders, including teaching hospital status and markers of patients' severity of illness.
A major threat to the validity of observational studies is residual confounding. Is it possible that there are factors other than private not-for-profit hospital status that explain such institutions' lower mortality rates? One such factor could be teaching status, because a much higher proportion of private not-for-profit than private for-profit hospitals are teaching hospitals. However, 3 of the studies conducted analyses that excluded teaching hospitals altogether and found a statistically significant increase in mortality in the private for-profit hospitals (RR 1.01, 1.05 and 1.05).16,21
Inevitably, large administrative databases have a limited ability to adjust for disease severity. Is it possible that patients in private not-for-profit hospitals were, on average, less sick? Most of the studies considered here used the Health Care Financing Administration (HCFA) database that includes data on all US hospitals that serve Medicare patients and generates risk-adjusted mortality rates that are highly correlated with detailed clinical risk–adjusted mortality rates.33 Moreover, in the studies that reported both unadjusted and adjusted results for disease severity, the adjusted analysis consistently led to effect estimates that were more favourable to the private not-for-profit institutions, suggesting that private not-for-profit hospitals serve a population of patients with greater disease severity.13,14,16,22 Under these circumstances, we would anticipate that residual confounding would make the private not-for-profit institutions look worse, rather than better, than the private for-profit institutions. These considerations suggest that, if anything, our results may represent an underestimate of the potential increase in mortality associated with private for-profit hospital care.
Ideally, studies would have adjusted for, or considered as explanatory factors, other variables for which data were not available. These variables include whether the physicians wre hospital employees or corporate employees, or independent contractors, and their relationships with local health maintenance organizations. Finally, studies have done little to adjust for the proportion of Medicare patients versus privately insured patients in the institutions being analyzed. With respect to this last variable, however, it is likely that for-profit hospitals attracted a larger proportion of privately insured individuals. If this is the case, private for-profit providers would have more resources available, and one might expect a “spillover” effect of improved care to Medicare patients. To the extent that this is the case, our pooled estimate again biases the results against the private not-for-profit institutions.
When studies show important differences in results, rigorous systematic reviewers explore the data to see if they can identify cogent explanations for the differences. How they should proceed if they fail to find an explanation for the differences remains controversial. Some argue that under these circumstances, pooling is inappropriate. Others argue that clinicians, and in this case health policy-makers, must still make decisions, and their decisions should be driven by the best available estimate of treatment effect.50 In the presence of unexplained heterogeneity, while inferences associated with pooled estimates are weaker, these estimates nevertheless provide the best estimate of the average effect, and thus constitute useful information for decision-makers.
The studies we pooled used similar methods to examine similar populations. Moreover, one does not require a pooled analysis to generate concern about the impact of for-profit status on hospital mortality: 7 studies provided statistically significant results that favoured lower mortality in private not-for-profit hospitals, whereas only one study had a statistically significant finding in the opposite direction.
We have no satisfactory explanation for the one study that demonstrated a statistically significant lower risk of death in private for-profit hospitals.19 Other large studies that used data from the same database before and after this study reached the opposite conclusion.14,16,17,20,21,23 We contacted the authors of this study and asked them to undertake further analyses to determine what may have accounted for this discrepant finding.19 The authors declined our request.
Why is there an increase in mortality in for-profit institutions? Typically, investors expect a 10%–15% return on their investment. Administrative officers of private for-profit institutions receive rewards for achieving or exceeding the anticipated profit margin. In addition to generating profits, private for-profit institutions must pay taxes and may contend with cost pressures associated with large reimbursement packages for senior administrators that private not-for-profit institutions do not face. As a result, when dealing with populations in which reimbursement is similar (such as Medicare patients), private for-profit institutions face a daunting task. They must achieve the same outcomes as private not-for-profit institutions while devoting fewer resources to patient care.
Considering these issues one might feel concern that the profit motive of private for-profit hospitals may result in limitations of care that adversely affect patient outcomes. Our results suggest that this concern is justified. Studies included in our review that conducted an initial analysis adjusting for disease severity, and another analysis with further adjustment for staffing levels, support this explanation for our results. The private for-profit hospitals employed fewer highly skilled personnel per risk-adjusted bed.14,20 The number of highly skilled personnel per hospital bed is strongly associated with hospital mortality rates,14,17,20 and differences in mortality between private for-profit and private not-for-profit institutions predictably decreased when investigators adjusted for staffing levels. Therefore, lower staffing levels of highly skilled personnel are probably one factor responsible for the higher risk-adjusted mortality rates in private for-profit hospitals.
Given the differences in the organization of the Canadian and US health care systems, one might question whether our results can be applied to Canada. The structure of US health care has, however, shifted dramatically over time. With the exception of a single study, the results are remarkably consistent over time, suggesting that the adverse effect of private for-profit hospitals is manifest within a variety of health care contexts. Furthermore, whatever the context within which they function, for-profit care providers face the problem of holding down costs while delivering a profit. One would, therefore, expect the resulting problems in health care delivery to emerge whatever the setting. Finally, should Canada open its doors to private for-profit hospitals, it is the very same large US hospital chains that have generated the data included in this study that will soon be purchasing Canadian private for-profit hospitals. In summary, we think it plausible, indeed likely, that our results are generalizable to the Canadian context.
The Canadian health care system is at a crucial juncture with many individuals suggesting that we would be better served by private for-profit health care delivery. Our systematic review raises concerns about the potential negative health outcomes associated with private for-profit hospital care. Canadian policy-makers, the stakeholders who seek to influence them and the public whose health will be affected by their decisions should take this research evidence into account.
β See related articles pages 1416 and 1418
Acknowledgments
We want to acknowledge the outstanding work of Deborah Maddock who coordinated this study.
Footnotes
Fast-tracked article
This article has been peer reviewed.
Contributors: P.J. Devereaux is the principal investigator for this study. He had the original idea for this study and led all aspects including design and data acquisition and interpretation. He wrote the first draft of the manuscript. Peter Choi is the co-principal investigator for this study. He made substantial contributions to its design and execution and made critical revisions to the manuscript. Christina Lacchetti made substantial contributions to the design and execution of this study and made critical revisions to the manuscript. Bruce Weaver was involved in the study design, data acquisition and analysis, and provided critical revisions to the manuscript. Holger Schünemann, Ted Haines, Brydon Grant, David Haslam, Mohit Bhandari, Stephen Walter, Humaira Khan, Neera Bhatnagar and Gordon Guyatt were involved in the study design, data acquisition and interpretation, and provided critical revisions to the manuscript. Stephen Taylor also undertook data analysis. Gordon Guyatt also provided supervisory support throughout the study. John Lavis, Terrence Sullivan, Deborah Cook, Maureen Meade were involved in the study design, interpretation of data and provided critical revisions to the manuscript.
This study was supported by an Atkinson Foundation Research Grant and a Hamilton Health Sciences Research Development Grant. Dr. Devereaux is supported by a Heart and Stroke Foundation of Canada/Canadian Institutes of Health Research Fellowship Award. Dr. Lavis holds a Canada Research Chair in Knowledge Transfer and Uptake. He also receives partial salary support as Liberty Health Scholar, Canadian Institute for Advanced Research. Dr. Cook is a Chair of the Canadian Institutes for Health Research. Dr. Meade is an MRC/CIHR/Peter Lougheed Scholar.
Competing interests: None declared.
Correspondence to: Dr. P.J. Devereaux, Department of Clinical Epidemiology & Biostatistics, McMaster University, Rm. 2C12, 1200 Main St. W, Hamilton ON L8N 3Z5; fax 905 524-3841; philipj@mcmaster.ca
References
- 1.Lewis S, Donaldson C, Mitton C, Currie G. The future of health care in Canada. BMJ 2001;323:926-9. [DOI] [PMC free article] [PubMed]
- 2.Gray C. Alberta is back at it, goading the feds. CMAJ 2000;162(3):411. Available: www.cmaj.ca/cgi/content/full/162/3/411
- 3.Klein's surgical strike at medicare [editorial]. CMAJ 2000;162(3):309. Available:www.cmaj.ca/cgi/content/full/162/3/309 [PMC free article] [PubMed]
- 4.Rebick J. Klein Bill 11 threatens medicare. CBC front page news 2000. Available: http://cbc.ca/news/viewpoint/columns/rebick/rebick000330.html (accessed 2002 Apr 18).
- 5.Zelder M. Public policy sources: How private hospital competition can improve the Canadian health care system. Public Policy Sources 2000;35:1-21. Available: www.fraserinstitute.ca/admin/books/files/priv-hosp(v8).pdf (accessed 2002 Apr 17).
- 6.Cairney R. Alberta ignores vocal opposition, presses ahead with law to expand role of private clinics. CMAJ 2000;162(11):1606-7. Available: www.cmaj.ca/cgi/content/full/162/11/1606 [PMC free article] [PubMed]
- 7.Shortt SED. Alberta's Bill 11: Will trade tribunals set domestic health policy? CMAJ 2001;164(6):798-9. Available: www.cmaj.ca/cgi/content/full/164/6/798 [PMC free article] [PubMed]
- 8.Commission on the Future of Health Care in Canada, Minister of Public Works and Government. Shape the future of health care. Consultation workbook. 2002. p. 1-29. Available: www.healthcarecommission.ca/Suite247/Common/GetMedia_WO.asp?MediaID=604&Filename=consultation_workbook.pdf (accessed 2002 Apr 18).
- 9.Deber RB. Getting what we pay for: myths and realities about financing Canada's health care system. 2000. p.1-52. Available: www.utoronto.ca/hpme/dhr/pdf/atrevised3.pdf (accessed 2002 Apr 18).
- 10.Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res 1993; 2:121-45. [DOI] [PubMed]
- 11.Egger M, Smith GD. Misleading meta-analysis. Lessons from “an effective, safe, simple” intervention that wasn't. BMJ 1995;310:752-4. [DOI] [PMC free article] [PubMed]
- 12.Shortell SM, Hughes EF. The effects of regulation, competition, and ownership on mortality rates among hospital inpatients. N Engl J Med 1988; 318(17):1100-7. [DOI] [PubMed]
- 13.Keeler EB, Rubenstein LV, Kahn KL, Draper D, Harrison ER, McGinty MJ, et al. Hospital characteristics and quality of care. JAMA 1992;268:1709-14. [PubMed]
- 14.Hartz AJ, Krakauer H, Kuhn EM, Young M, Jacobsen SJ, Gay G, et al. Hospital characteristics and mortality rates. N Engl J Med 1989;321:1720-5. [DOI] [PubMed]
- 15.Manheim LM, Feinglass J, Shortell SM, Hughes EF. Regional variation in Medicare hospital mortality. Inquiry 1992;29:55-66. [PubMed]
- 16.Kuhn EM, Hartz AJ, Krakauer H, Bailey RC, Rimm AA. The relationship of hospital ownership and teaching status to 30- and 180-day adjusted mortality rates. Med Care 1994;32:1098-108. [DOI] [PubMed]
- 17.Pitterle ME, Bond CA, Raehl CL, Franke T. Hospital and pharmacy characteristics associated with mortality rates in United States hospitals. Pharmacotherapy 1994;14:620-30. [PubMed]
- 18.Williams RL. 1986–1990: Maternal and child health data base descriptive narrative. Santa Barbara (CA): University of California at Santa Barbara; 1994. MCH contract no. 91-12638.
- 19.Mukamel DB, Zwanziger J, Tomaszewski KJ. HMO penetration, competition, and risk-adjusted hospital mortality. Health Serv Res 2001;36:1019-35. [PMC free article] [PubMed]
- 20.Bond CA, Raehl CL, Pitterle ME, Franke T. Health care professional staffing, hospital characteristics, and hospital mortality rates. Pharmacotherapy 1999;19:130-8. [DOI] [PubMed]
- 21.Yuan Z, Cooper GS, Einstadter D, Cebul RD, Rimm AA. The association between hospital type and mortality and length of stay. A study of 16.9 million hospitalized Medicare beneficiaries. Med Care 2000;38:231-45. [DOI] [PubMed]
- 22.Lanska DJ, Kryscio RJ. In-hospital mortality following carotid endarterectomy. Neurology 1998;51:440-7. [DOI] [PubMed]
- 23.McClellan M, Staiger D. Comparing hospital quality at for-profit and not-for-profit hospitals. In: Cutler DM, editor. The changing hospital industry: comparing not-for-profit and for-profit institutions. Chicago: University of Chicago Press; 2001. p. 93-112.
- 24.Sloan FA, Picone GA, Taylor DH Jr, Chou SY. Hospital ownership and cost and quality of care: Is there a dime's worth of difference? J Health Econ 2001;20:1-21. [DOI] [PubMed]
- 25.Sloan FA, Picone GA, Taylor DH, Chou SY. Does where you are admitted make a difference? An analysis of Medicare data. Cambridge (MA): National Bureau of Economic Research; 1999. NBER working paper no. 6896.
- 26.McClellan M, Staiger D. Comparing hospital quality at for-profit and not-for-profit hospitals. Cambridge (MA): National Bureau of Economic Research; 1999. NBER working paper no. 7324.
- 27.Taylor DH Jr, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med 1999;340:293-9. [DOI] [PubMed]
- 28.Ettner SL, Hermann RC. The role of profit status under imperfect information: evidence from the treatment patterns of elderly Medicare beneficiaries hospitalized for psychiatric diagnoses. J Health Econ 2001;20:23-49. [DOI] [PubMed]
- 29.Siddiqui RI, Rizvi T, Jafarey S. Situation analysis of emergency obstetric care (EOC) in four districts of Sindh. J Coll Physicians Surg Pakistan 1999;9:187-9.
- 30.George E, Hunsberger S, Savitha D, Pais P. Treatment of acute myocardial infarction: Does the type of hospital make a difference? Indian Heart J 1999; 51:161-6. [PubMed]
- 31.Ferrier GD, Valdmanis V. Rural hospital performance and its correlates. J Productivity Analysis 1996;7:63-80.
- 32.Burns LR, Wholey DR. The effect of patient, hospital, and physician characteristics on length of stay and mortality. Med Care 1991;29:251-71. [DOI] [PubMed]
- 33.Krakauer H, Bailey RC, Skellan KJ, Stewart JD, Hartz AJ, Kuhn EM, et al. Evaluation of the HCFA Model for the analysis of mortality following hospitalization. Health Serv Res 1992;27:317-35. [PMC free article] [PubMed]
- 34.Luft HS, Hunt SS, Maerki SC. The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res 1987;22:157-82. [PMC free article] [PubMed]
- 35.Aiken LH, Smith HL, Lake ET. Lower Medicare mortality among a set of hospitals known for good nursing care. Med Care 1994;32:771-87. [DOI] [PubMed]
- 36.Hannan EL, O'Donnell JF, Kilburn H, Bernard HR, Yazici A. Investigation of the relationship between volume and mortality for surgical procedures performed in New York State hospitals. JAMA 1989;262:503-10. [PubMed]
- 37.Sorrentino EA. Hospitals vary by LOS, charges, reimbursements and death rates. Nurs Manage 1989;20:54–6. [PubMed]
- 38.Williams RL. Measuring the effectiveness of perinatal medical care. Med Care 1979;17:95-110. [DOI] [PubMed]
- 39.Al-Haider AS, Wan TTH. Modeling organizational determinants of hospital mortality. Health Serv Res 1991;26:303-23. [PMC free article] [PubMed]
- 40.Silverman EM, Skinner JS, Fisher ES. The association between for-profit hospital ownership and increased Medicare spending. N Engl J Med 1999; 341:420-6. [DOI] [PubMed]
- 41.Schultz MA, van Servellen G, Chang BL, McNeese-Smith D, Waxenberg E. The relationship of hospital structural and financial characteristics to mortality and length of stay in acute myocardial infarction patients. Outcomes Manage Nurs Practice 1998;2:130-6. [PubMed]
- 42.Iezzoni LI, Mackiernan YD, Cahalane MJ, Phillips RS, Davis RB, Miller K. Screening inpatient quality using post-discharge events. Med Care 1999; 37:384-98. [DOI] [PubMed]
- 43.Schultz MA, van Servellen G, Litwin MS, McLaughlin EJ, Uman GC. Can hospital structural and financial characteristics explain variations in mortality caused by acute myocardial infarction? Appl Nurs Res 1999;12:210-4. [DOI] [PubMed]
- 44.Shortell SM, LoGerfo J. Hospital medical staff organization and quality of care: results for myocardial infarction and appendectomy. Med Care 1980; 19:1041-55. [DOI] [PubMed]
- 45.Kelly JV, Hellinger FJ. Physician and hospital factors associated with mortality of surgical patients. Med Care 1986;24:785-800. [DOI] [PubMed]
- 46.Matshidze KP, Richter LM, Ellison GTH, Levin JB, McIntyre JA. Caesarean section rates in South Africa: evidence of bias among different ‘population groups’. Ethn Health 1998;3:71-9. [DOI] [PMC free article] [PubMed]
- 47.Division of Health and Science Policy, New York Academy of Medicine. The empirical literature comparing for-profit and nonprofit hospitals, managed care organizations and nursing homes: updating the Institute of Medicine Study. New York: The Academy; 1999. p. 1-65. Available: www.cnhc.org/Report3.pdf (accessed 2002 Apr 23).
- 48.Donaldson C, Currie G. The public purchase of private surgical services: a systematic review of the evidence of efficiency and equity. Ottawa: National Library of Canada; 2000. Institute of Health Economics working paper no. 00-9.
- 49.Armitage P, Colton T. Encyclopedia of biostatistics. vol 6. London: John Wiley & Son; 1998. p.4245.
- 50.Montori V, Hatala R, Guyatt GH. Evaluating differences in study results. In: Guyatt G, Rennie D, editors. The users' guides to the medical literature: a manual for evidence-based clinical practice. Chicago: American Medical Association; 2002.


