Abstract
Toll-like receptors (TLR) play a key role in innate immunity. To examine the ability of diverse TLRs to modulate hepatitis B virus (HBV) replication, HBV transgenic mice received a single intravenous injection of ligands specific for TLR2, TLR3, TLR4, TLR5, TLR7, and TLR9. All of the ligands except for TLR2 inhibited HBV replication in the liver noncytopathically within 24 h in a α/β interferon-dependent manner. The ability of these TLR ligands to induce antiviral cytokines at the site of HBV replication suggests that TLR activation could represent a powerful and novel therapeutic strategy for the treatment of chronic HBV infection.
We have previously shown that hepatitis B virus (HBV)-specific CD8+ cytotoxic T lymphocytes and CD4+ helper T lymphocytes can inhibit HBV replication in the liver of HBV transgenic mice by secreting gamma interferon (IFN-γ) when they recognize viral antigen (6, 8). This antiviral effect could be also induced in response to IFN-α/β that was produced in the liver during lymphocytic choriomeningitis virus, murine cytomegalovirus, and adenovirus infections (2, 7). More recently, we have demonstrated that NKT cells, NK cells, and antigen-presenting cells inhibit HBV replication when they are activated by alpha-galactosylceramide (16), interleukin-12 (IL-12) (3), IL-18 (18), and an agonistic anti-CD40 antibody injection (17), respectively. Collectively, these results suggest that HBV replication can be controlled by innate immune response if it is activated in the liver.
Toll-like receptors (TLRs) are essential for the recognition of invading pathogens and serve as an important link between innate and adaptive immunity. TLRs can discriminate various microbial components, such as triacylated lipopeptides (recognized by TLR1/TLR2 heterodimer) (30), diacylated lipopeptides (recognized by TLR2/TLR6 heterodimer) (23), double-stranded RNA (dsRNA; recognized by TLR3) (1), lipopolysaccharide (LPS; recognized by TLR4) (27), flagellin from bacterial flagella (recognized by TLR5) (11), single-stranded RNA (ssRNA; recognized by TLR7/8) (4, 12), and bacterial DNA containing the unmethylated CpG motif (recognized by TLR9) (13). While the TLRs have been shown to play a crucial role in the innate recognition of bacterial and fungal pathogens, recent studies also suggest the importance of TLRs in antiviral immunity in vivo (14, 19, 20).
Although we have reported that poly(I · C) inhibits HBV replication by inducing IFN-α/β (21), little is known about the ability of other TLRs to control of HBV. Accumulating evidence suggests that each TLR transduces its signals by distinct but overlapping signaling pathways. For instance, TLR3 and TLR4 appear to signal mainly through a MyD88-independent, TRIF-dependent pathway, while TLR2, TLR5, TLR7, and TLR9 signaling appears to be MyD88 dependent and TRIF independent (14). Thus, to examine the potential antiviral effect of these different TLR signaling pathways, groups of three or more age-, sex-, and serum HBeAg-matched transgenic mice from lineage 1.3.32 (9) were injected intravenously with a panel of ligands specific for TLR2 (PGN and Pam3Cys), TLR3 [poly(I · C)], TLR4 (LPS), TLR5 (Flagellin), TLR7 (R848), and TLR9 (CpG oligodeoxynucleotides [ODN]), and they were sacrificed 24 h later. Total hepatic DNA was analyzed for HBV DNA by Southern blot analysis (8, 9). Total hepatic RNA was analyzed for HBV gene expression by Northern blot analysis and for the expression of various cytokines and 2′,5′-oligoadenylate synthetase (2′5′-OAS) (a marker of IFN-α/β induction) by RNase protection assay (8). The results were compared with those observed in mice that were injected intravenously with saline.
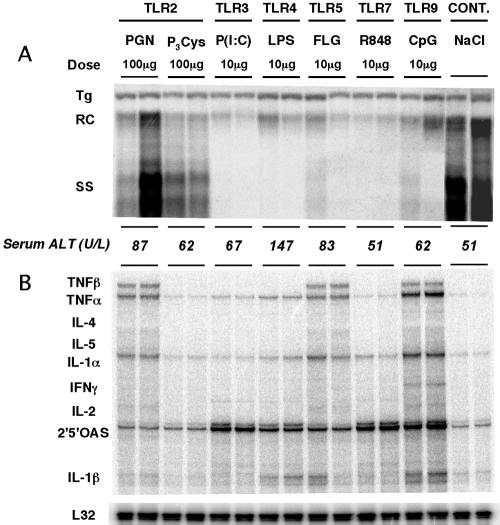
As shown in Fig. 1A for two representative mice per group, HBV replication was almost completely abolished by the administration of 10 μg of TLR3, -4, -5, -7, and -9 ligands. In contrast, the administration of 20 μg (data not shown) or 100 μg of TLR2 ligands had little effect on virus replication. As shown below the Southern blot in Fig. 1A, except for LPS, the administration of these ligands did not cause any elevation of serum alanine aminotransferase (ALT) activity (a manifestation of liver cell injury), nor did they induce the recruitment of intrahepatic lymphocytes (data not shown), indicating that the antiviral effect was essentially noninflammatory and noncytopathic. Importantly, the TLR ligands had no effect on the HBV RNA content of the livers (data not shown), indicating that the antiviral effect on HBV replication was posttranscriptional as previously reported (8). Importantly, as shown in Fig. 1B, the profound inhibition of HBV replication was accompanied by the intrahepatic induction of IFN-α/β (indicated by the induction of 2′5′-OAS mRNA expression) following TLR3, -4, -5, -7, and -9 ligand injection, and IFN-γ mRNA was also induced by activation of TLR9. These results indicate that the administration of these TLR ligands induced the production of cytokines in the liver (especially IFN-α/β and IFN-γ) that inhibit HBV replication by suppressing the assembly or stability of HBV RNA-containing capsids, within which HBV DNA synthesis occurs (8, 21, 32).
FIG. 1.
Toll-like receptor ligands inhibit HBV replication in vivo. Age-, sex-, and serum HBeAg-matched lineage 1.3.32 HBV transgenic mice were injected intravenously with 20 μg (not shown) and 100 μg of TLR2/6 (peptidoglycan [PGN] from Staphylococcus aureus; InvivoGen), TLR2/1 ligand N-α-palmitoyl-S-[2,3-bis(palmitoyloxy)-(2RS)-propyl]-l-cysteine (Pam3Cys; InvivoGen), 10 μg of TLR3 [polyinosinic-poly(I · C); P(I:C); Sigma]) TLR4 (LPS from Escherichia coli 011:B4 strain; InvivoGen), TLR5 (Flagellin from salmonella muenchen; Calbiochem), TLR7 (R848) (InvivoGen), or TLR9 (ODN 1826 CpG oligonucleotide [CpG]; InvivoGen) ligands and sacrificed 24 h later. Lineage 1.3.32 mice replicate HBV at high levels in the liver without any evidence of cytopathology (9). (A) Total hepatic DNA was isolated from frozen liver tissues and analyzed for HBV DNA by Southern blot analysis as previously described (9). Bands corresponding to the integrated transgene (Tg), relaxed circular double stranded (RC), and single-stranded (SS) HBV DNA replicative forms are indicated. The integrated transgene can be used to normalize the amount of DNA bound to the membrane. The mean serum ALT activity, measured at the time of autopsy, is indicated for each group and is expressed in units/liter. (B) Total hepatic RNA was also isolated from the same mice and analyzed by RNase protection assay for the expression of various cytokines as previously described (8). The RNA encoding the ribosomal protein L32 was used to normalize the amount of RNA loaded in each lane.
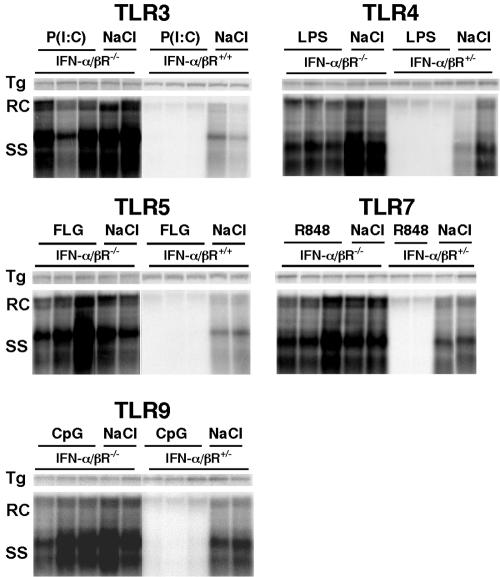
The results described above suggest that TLR signaling triggered the production of cytokines that inhibited HBV replication. It is possible, however, that TLR signaling per se could have directly inhibited viral replication by cytokine-independent mechanisms. To examine this question, the TLR ligands were injected into groups of HBV transgenic mice that were homozygous (IFN-α/βR−/−) for the IFN-α/βR-null mutation (21, 22), and the animals were sacrificed 24 h later. HBV transgenic mice that were either heterozygous (IFN-α/βR+/−) for the IFN-α/βR-null mutation or wild type with respect to the IFN-α/βR allele were treated with the TLR ligands at the same time as controls. As shown in Fig. 2, the baseline level of HBV replication was higher in IFN-α/βR−/− mice than the controls, indicating that constitutive levels of IFN-α/β regulate HBV replication under baseline conditions, as previously described (21). Importantly, the antiviral effect of all the TLR ligands was virtually abolished in the absence of the IFN-α/β receptor, indicating that the IFN-α/β pathway is primarily responsible for inhibiting HBV replication in these experiments.
FIG. 2.
The antiviral effect of TLRs is mediated by IFN-α/β. Age-, sex-, and serum HBeAg-matched transgenic mice (lineage 1.3.46) that were homozygous (−/−) for the IFN-α/β receptor null mutation (21, 22) were injected with 20 μg of TLRs as indicated and sacrificed 24 h later, and their livers were analyzed for HBV replication. Age-, HBeAg-, and sex-matched transgenic mice from lineage 1.3.46 that were heterozygous (+/−) for the IFN-α/β receptor null mutation or [in the case of poly(I · C) and flagellin] from wild-type lineage 1.3.32 were treated exactly the same as controls. The integrated transgene (Tg) can be used to normalize the amount of DNA bound to the membrane. P(I:C), poly(I · C).
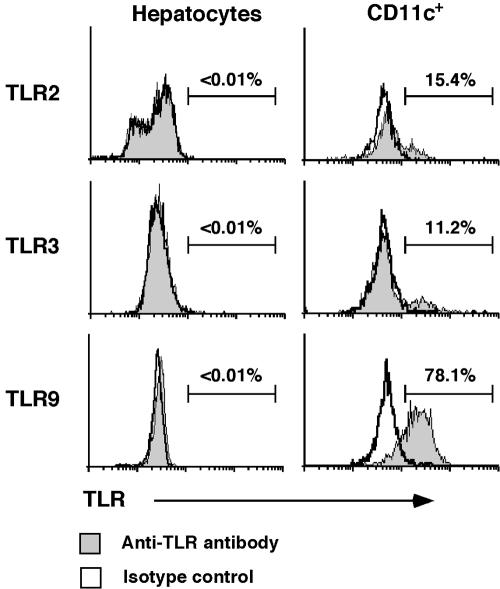
The source of IFN-α/β following TLR ligation could be any TLR+ cell in the liver. To determine if the TLR ligands target the hepatocytes directly, we treated an immortalized murine hepatocyte cell line derived from HBV transgenic mice (HBV-Met) (26) with TLR2, -3, -4, -5, and -9 ligands (5 μg/ml peptidoglycan [PGN], 100 μg/ml poly(I · C), 1 μg/ml LPS, 0.2 μg/ml flagellin, 6.6 μg/ml CpG oligonucleotide, respectively). Unlike IFN-α (2,000 U/ml), which efficiently suppresses HBV replication in these cells, the TLR ligands did not inhibit HBV replication (not shown), probably because these cells do not express the corresponding TLRs. Nonetheless, it is possible that hepatocytes express TLRs in vivo but not after immortalization and maintenance in vitro. Thus, we examined TLR2, -3, and -9 expression by flow cytometry in primary hepatocytes and CD11c-positive intrahepatic nonparenchymal cells isolated from the livers of HBV transgenic mice (16, 25). As shown in Fig. 3, none of these TLRs was expressed by freshly isolated hepatocytes. In contrast, 15.4%, 11.2%, and 78.1% of CD11c+ nonparenchymal cells (i.e., intrahepatic dendritic cells) expressed TLR2, TLR3, and TLR9, respectively. Collectively, these results suggest that in vivo the TLR ligands activate an antiviral program in the nonparenchymals cells, especially the dendritic cells, and not the hepatocytes. Since the TLRs examined in this study are known to highly expressed on monocytes, NK cells (29), endothelial cells (28), and hepatic stellate cells (24) as well as dendritic cells (15), all of which are abundant in the liver, it is likely that some or all of those nonparenchymal cells are activated by the TLR ligands, produce IFN-α/β, and thereby inhibit HBV replication in the hepatocyte in vivo.
FIG. 3.
Freshly isolated hepatocytes do not express TLRs. Primary hepatocytes and intrahepatic lymphocytes were isolated from HBV transgenic mice as previously described (16, 25) and stained with antibodies specific for TLR2, -3, and -9 (eBioscience) in combination with anti-CD11c (BD Pharmingen). Surface staining was performed to detect TLR2 expression, while intracellular staining was applied for TLR3 and -9 expressions (18). Cells were acquired using a FACSCalibur flow cytometer (Becton Dickinson), and data were analyzed using CELLQuest software (Becton Dickinson). Histograms represent TLR staining (gray) or isotype control staining (white) of hepatocytes (left panel). Corresponding TLR expression on CD11c+ cells of intrahepatic lymphocytes were shown as positive controls (right panel).
While ample evidence suggests the involvement of TLRs in the defense against bacterial infections, their role in viral infections is less understood. Recent studies suggest that TLR activation can both enhance human immunodeficiency virus (HIV) replication (5) and suppress respiratory syncytial virus (19), mouse cytomegalovirus (14), and vesicular stomatitis virus infection (20) in vivo. Furthermore, there is evidence that poxviruses have developed strategies to defeat TLR activation (10), suggesting a role for TLRs in the control of those infections as well. While the current results suggest that TLR activation could contribute to the control of HBV replication during natural infection, we have recently reported that IFN-α/β, 2′5′-OAS, and other genes associated with the innate immune response are not induced in the liver of acutely infected chimpanzees (31). While this implies that HBV probably does not activate TLRs per se, it also suggests that it hasn't evolved evasion strategies to defeat the antiviral signaling pathways TLRs induce. Thus, we suggest that therapeutic TLR activation could be used to treat chronic HBV infection, since local induction of IFN-α by TLR activation is likely to be more efficient than systemic IFN-α administration (21) and should therefore reduce the risk of the undesirable side effects of this cytokine. In this regard, it is particularly encouraging that multiple TLR ligands that utilize distinct signaling pathways inhibited HBV replication in the absence of cytopathology, implying that coadministration of various TLR ligands might induce additive or synergistic antiviral effects in chronically infected patients.
Acknowledgments
We thank Luca G. Guidotti and Stefan Wieland for helpful advice and Josan Chung and Sadie Medrano for excellent technical assistance.
This study was supported by grant CA40489 to F.V.C. from the National Institutes of Health and by a fellowship to M.I. from the Skaggs Foundation.
Footnotes
This is manuscript number 16835-MEM from The Scripps Research Institute.
REFERENCES
- 1.Alexopoulou, L., A. C. Holt, R. Medzhitov, and R. A. Flavell. 2001. Recognition of double-stranded RNA and activation of NF-kappaB by Toll-like receptor 3. Nature 413:732-738. [DOI] [PubMed] [Google Scholar]
- 2.Cavanaugh, V. J., L. G. Guidotti, and F. V. Chisari. 1998. Inhibition of hepatitis B virus replication during adenovirus and cytomegalovirus infections in transgenic mice. J. Virol. 72:2630-2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cavanaugh, V. J., L. G. Guidotti, and F. V. Chisari. 1997. Interleukin-12 inhibits hepatitis B virus replication in transgenic mice. J. Virol. 71:3236-3243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diebold, S. S., T. Kaisho, H. Hemmi, S. Akira, and C. Reis e Sousa. 2004. Innate antiviral responses by means of TLR7-mediated recognition of single-stranded RNA. Science 303:1529-1531. [DOI] [PubMed] [Google Scholar]
- 5.Feng, C. G., C. A. Scanga, C. M. Collazo-Custodio, A. W. Cheever, S. Hieny, P. Caspar, and A. Sher. 2003. Mice lacking myeloid differentiation factor 88 display profound defects in host resistance and immune responses to Mycobacterium avium infection not exhibited by Toll-like receptor 2 (TLR2)- and TLR4-deficient animals. J. Immunol. 171:4758-4764. [DOI] [PubMed] [Google Scholar]
- 6.Franco, A., L. G. Guidotti, M. V. Hobbs, V. Pasquetto, and F. V. Chisari. 1997. Pathogenetic effector function of CD4-positive T helper 1 cells in hepatitis B virus transgenic mice. J. Immunol. 159:2001-2008. [PubMed] [Google Scholar]
- 7.Guidotti, L. G., P. Borrow, A. Brown, H. McClary, R. Koch, and F. V. Chisari. 1999. Noncytopathic clearance of lymphocytic choriomeningitis virus from the hepatocyte. J. Exp. Med. 189:1555-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guidotti, L. G., T. Ishikawa, M. V. Hobbs, B. Matzke, R. Schreiber, and F. V. Chisari. 1996. Intracellular inactivation of the hepatitis B virus by cytotoxic T lymphocytes. Immunity 4:25-36. [DOI] [PubMed] [Google Scholar]
- 9.Guidotti, L. G., B. Matzke, H. Schaller, and F. V. Chisari. 1995. High-level hepatitis B virus replication in transgenic mice. J. Virol. 69:6158-6169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harte, M. T., I. R. Haga, G. Maloney, P. Gray, P. C. Reading, N. W. Bartlett, G. L. Smith, A. Bowie, and L. A. O'Neill. 2003. The poxvirus protein A52R targets Toll-like receptor signaling complexes to suppress host defense. J. Exp. Med 197:343-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayashi, F., K. D. Smith, A. Ozinsky, T. R. Hawn, E. C. Yi, D. R. Goodlett, J. K. Eng, S. Akira, D. M. Underhill, and A. Aderem. 2001. The innate immune response to bacterial flagellin is mediated by Toll-like receptor 5. Nature 410:1099-1103. [DOI] [PubMed] [Google Scholar]
- 12.Heil, F., H. Hemmi, H. Hochrein, F. Ampenberger, C. Kirschning, S. Akira, G. Lipford, H. Wagner, and S. Bauer. 2004. Species-specific recognition of single-stranded RNA via toll-like receptor 7 and 8. Science 303:1526-1529. [DOI] [PubMed] [Google Scholar]
- 13.Hemmi, H., O. Takeuchi, T. Kawai, T. Kaisho, S. Sato, H. Sanjo, M. Matsumoto, K. Hoshino, H. Wagner, K. Takeda, and S. Akira. 2000. A Toll-like receptor recognizes bacterial DNA. Nature 408:740-745. [DOI] [PubMed] [Google Scholar]
- 14.Hoebe, K., X. Du, P. Georgel, E. Janssen, K. Tabeta, S. O. Kim, J. Goode, P. Lin, N. Mann, S. Mudd, K. Crozat, S. Sovath, J. Han, and B. Beutler. 2003. Identification of Lps2 as a key transducer of MyD88-independent TIR signalling. Nature 424:743-748. [DOI] [PubMed] [Google Scholar]
- 15.Kadowaki, N., S. Ho, S. Antonenko, R. W. Malefyt, R. A. Kastelein, F. Bazan, and Y. J. Liu. 2001. Subsets of human dendritic cell precursors express different toll-like receptors and respond to different microbial antigens. J. Exp. Med. 194:863-869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kakimi, K., L. G. Guidotti, Y. Koezuka, and F. V. Chisari. 2000. Natural killer T cell activation inhibits hepatitis B virus replication in vivo. J. Exp. Med. 192:921-930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimura, K., K. Kakimi, S. Wieland, L. G. Guidotti, and F. V. Chisari. 2002. Activated intrahepatic antigen-presenting cells inhibit hepatitis B virus replication in the liver of transgenic mice. J. Immunol. 169:5188-5195. [DOI] [PubMed] [Google Scholar]
- 18.Kimura, K., K. Kakimi, S. Wieland, L. G. Guidotti, and F. V. Chisari. 2002. Interleukin-18 inhibits hepatitis B virus replication in the livers of transgenic mice. J. Virol. 76:10702-10707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kurt-Jones, E. A., L. Popova, L. Kwinn, L. M. Haynes, L. P. Jones, R. A. Tripp, E. E. Walsh, M. W. Freeman, D. T. Golenbock, L. J. Anderson, and R. W. Finberg. 2000. Pattern recognition receptors TLR4 and CD14 mediate response to respiratory syncytial virus. Nat. Immunol. 1:398-401. [DOI] [PubMed] [Google Scholar]
- 20.Lund, J. M., L. Alexopoulou, A. Sato, M. Karow, N. C. Adams, N. W. Gale, A. Iwasaki, and R. A. Flavell. 2004. Recognition of single-stranded RNA viruses by Toll-like receptor 7. Proc. Natl. Acad. Sci. USA 101:5598-5603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McClary, H., R. Koch, F. V. Chisari, and L. G. Guidotti. 2000. Relative sensitivity of hepatitis B virus and other hepatotropic viruses to the antiviral effects of cytokines. J. Virol. 74:2255-2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muller, U., U. Steinhoff, L. F. Reis, S. Hemmi, J. Pavlovic, R. M. Zinkernagel, and M. Aguet. 1994. Functional role of type I and type II interferons in antiviral defense. Science 264:1918-1921. [DOI] [PubMed] [Google Scholar]
- 23.Ozinsky, A., D. M. Underhill, J. D. Fontenot, A. M. Hajjar, K. D. Smith, C. B. Wilson, L. Schroeder, and A. Aderem. 2000. The repertoire for pattern recognition of pathogens by the innate immune system is defined by cooperation between toll-like receptors. Proc. Natl. Acad. Sci. USA 97:13766-13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paik, Y. H., R. F. Schwabe, R. Bataller, M. P. Russo, C. Jobin, and D. A. Brenner. 2003. Toll-like receptor 4 mediates inflammatory signaling by bacterial lipopolysaccharide in human hepatic stellate cells. Hepatology 37:1043-1055. [DOI] [PubMed] [Google Scholar]
- 25.Pasquetto, V., S. Wieland, and F. V. Chisari. 2000. Intracellular hepatitis B virus nucleocapsids survive cytotoxic T-lymphocyte-induced apoptosis. J. Virol. 74:9792-9796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pasquetto, V., S. F. Wieland, S. L. Uprichard, M. Tripodi, and F. V. Chisari. 2002. Cytokine-sensitive replication of hepatitis B virus in immortalized mouse hepatocyte cultures. J. Virol. 76:5646-5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poltorak, A., X. He, I. Smirnova, M. Y. Liu, C. Van Huffel, X. Du, D. Birdwell, E. Alejos, M. Silva, C. Galanos, M. Freudenberg, P. Ricciardi-Castagnoli, B. Layton, and B. Beutler. 1998. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282:2085-2088. [DOI] [PubMed] [Google Scholar]
- 28.Raschi, E., C. Testoni, D. Bosisio, M. O. Borghi, T. Koike, A. Mantovani, and P. L. Meroni. 2003. Role of the MyD88 transduction signaling pathway in endothelial activation by antiphospholipid antibodies. Blood 101:3495-3500. [DOI] [PubMed] [Google Scholar]
- 29.Sivori, S., M. Falco, M. Della Chiesa, S. Carlomagno, M. Vitale, L. Moretta, and A. Moretta. 2004. CpG and double-stranded RNA trigger human NK cells by Toll-like receptors: induction of cytokine release and cytotoxicity against tumors and dendritic cells. Proc. Natl. Acad. Sci. USA 101:10116-10121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takeuchi, O., S. Sato, T. Horiuchi, K. Hoshino, K. Takeda, Z. Dong, R. L. Modlin, and S. Akira. 2002. Cutting edge: role of Toll-like receptor 1 in mediating immune response to microbial lipoproteins. J. Immunol. 169:10-14. [DOI] [PubMed] [Google Scholar]
- 31.Wieland, S., R. Thimme, R. H. Purcell, and F. V. Chisari. 2004. Genomic analysis of the host response to hepatitis B virus infection. Proc. Natl. Acad. Sci. USA 101:6669-6674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wieland, S. F., L. G. Guidotti, and F. V. Chisari. 2000. Intrahepatic induction of alpha/beta interferon eliminates viral RNA-containing capsids in hepatitis B virus transgenic mice. J. Virol. 74:4165-4173. [DOI] [PMC free article] [PubMed] [Google Scholar]