Abstract
Purpose
To investigate the long-term effect of sitting time and physical activity after a skin cancer diagnosis.
Methods
A cohort of a nationally representative sample of skin cancer survivors (n=862) and non-cancer adults (n=13691) ≥50 years from the US National Health and Nutrition Examination Survey. Mortality data were linked through December 31, 2019.
Results
During up to 13.2 years of follow-up (median, 6.3 years; 94,093 person-years), 207 deaths (cancer: 53) occurred in skin cancer survivors and 1970 (cancer: 414) in non-cancer adults. After adjusting for covariates and skin cancer type, being active was associated with lower risks of all-cause (HR=0.69; 95% CI: 0.47 to 1.00) and non-cancer (HR=0.59; 95% CI: 0.36 to 0.97) mortality compared to being inactive among skin cancer survivors. Meanwhile, sitting 8 h/d was associated with higher risks of all-cause (HR=1.72; 95% CI: 1.11 to 2.67) and non-cancer (HR=1.76; 95% CI: 1.07 to 2.92) mortality compared to sitting <6 h/d. In the joint analysis, inactive skin cancer survivors sitting >8 h/d had the highest mortality risks from all-cause (HR=2.26; 95% CI: 1.28 to 4.00) and non-cancer (HR=2.11; 95% CI,1.10 to 4.17). Additionally, the associations of LTPA and sitting time with all-cause and cause-specific mortality did not differ between skin cancer survivors and non-cancer adults (all P for interaction>0.05)
Conclusion
The combination of prolonged sitting and lack of physical activity was associated with elevated risks of all-cause and non-cancer deaths among US skin cancer survivors. Skin cancer survivors could benefit from maintaining a physically active lifestyle.
Keywords: Sitting time, Physical activity, Skin cancer, Cancer survivorship, Mortality
Introduction
Skin cancer is the most common cancer in the USA [1, 2]. Nearly all diagnoses are non-melanoma skin cancer (estimated 5.4 million cases/year) [3], while 1% are melanoma but causing the majority of skin cancer deaths [3]. Most skin cancers are curable. The 5-year relative survival rates for all stages combined were lower in male than females [4], exceeding 95% for non-melanoma skin cancer and 93% for melanoma [5]. The incidence of both non-melanoma skin cancer and melanoma continued to increase [4], resulting in a large number of survivors [6]. Nevertheless, the knowledge base for improving skin cancer survivorship is lacking despite these survivors experience dramatic life changes and physical and psychosocial stress associated with cancer and its treatments [7–11].
The 2022 American Cancer Society (ACS) guidelines recommended cancer survivors engage in leisure-time physical activity (LTPA) and limit time spent sitting based on evidence generated primarily from cancer survivors of the breast, colorectal, and prostate, with no evidence from skin cancer [12]. New research conducted in mixed-type non-skin cancer survivors suggested the combination of prolonged sitting and lack of physical activity was associated with elevated mortality risks [13]. However, no study has evaluated the impact of LTPA and sitting time on mortality outcomes specifically in survivors of skin cancers. Recognizing the potential health benefits, making specific recommendations for skin cancer survivors to increase LTPA and limit sitting remains under debate [14]. LTPA, particularly outdoor LTPA, may increase ultraviolet exposure and therefore the risk of skin cancer recurrence [15, 16]. However, skin cancer survivors often die from sedentary lifestyle-related chronic diseases, such as cardiovascular diseases, rather than skin cancer [17]. Therefore, skin cancer survivors might be negatively affected by sedentary lifestyle similarly to non-cancer adults. The uncertainty about these lifestyle practices and long-term health outcomes among skin cancer survivors may constrain their physical activity participation and lead to a sedentary lifestyle, which places skin cancer survivors at elevated risks of comorbidities and death [14]. Thus, an in-depth investigation on the impacts of LTPA and sitting time on cancer and non-cancer mortality outcomes among skin cancer survivors is needed to address this knowledge gap.
This study aimed to examine associations of LTPA and daily sitting time with all-cause, cancer-specific, and non-cancer mortality among a US nationally representative sample of skin cancer survivors and non-cancer adults.
Methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is a major research study conducted by the National Center for Health Statistics (NCHS) to monitor the health and nutritional status of the US population. NHANES consists of nationally representative samples in two-year cycles starting in 1999. All NHANES protocols were approved by the NCHS ethics review board and written informed consent was obtained from all participants. Each participant was invited to an in-person interview and completed a set of physical examinations and laboratory tests in a mobile examination center (MEC). Herein, data on sociodemographic characteristics, lifestyle factors, and medical history in skin cancer survivors and non-cancer adults aged ≥50 years with available information on physical activity and daily sitting time during the six NHANES cycles from 2007 to 2018 were analyzed. This investigation, based on published data containing no personally identifiable information, was exempt from human subjects review. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement guidelines.
Diagnosis of skin cancer
Data on cancer diagnosis and cancer type were collected during the in-person interview, which included cancer type(s) up to three diagnoses and age at each diagnosis. Participants were asked, “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?” Individual who responded “Yes” was defined as cancer survivors and then was asked, “What kind of cancer was it?” and “How old were you when this cancer was first diagnosed?” [18]. Years since the first cancer diagnosis were calculated as the difference between current age and age at first diagnosis. Individuals who were ever diagnosed with melanoma, skin (non-melanoma), and skin (don’t know what kind) cancer were defined as skin cancer survivors [19]. Current analyses were restricted to aged 50 years or older at the time of the survey because most skin cancer cases were diagnosis after age 50 [3]. All adults aged 50 years or older in the analyzed cycles from NHANES who did not have any cancer diagnosis at baseline were defined as non-cancer adults.
Ascertainment of mortality
The NCHS provided mortality data that were linked to the National Death Index through December 31, 2019. The International Classification of Diseases, 10th Revision (ICD-10) was used to record the underlying cause of death. Cancer mortality was classified as death caused by malignant neoplasms (ICD-10 codes C00-C97) and non-cancer mortality was classified as death caused by other causes. The duration of follow-up was defined as the interval (months) from the survey date (2007 to 2018) to death date or to December 31, 2019 for those who were censored [20]. To reduce the probability of reverse causation, deaths occurring during the first year of follow-up were excluded [21].
Leisure-time physical activity and daily sitting time
Information on leisure-time physical activity (LTPA) and total daily sitting time were self-reported by participants responding to the Global Physical Activity Questionnaire (GPAQ). The GPAQ has been previously validated to collect information related to daily activities, leisure-time activities, and sedentary behaviors [22]. During the in-person interview, participants were asked to report moderate- and vigorous-intensity aerobic PA in a typical week. The total amount of LTPA was estimated as minutes of moderate-intensity activity plus twice the minutes of vigorous-intensity activity from recreational activities [23, 24]. Based on the 2018 Physical Activity Guidelines for Americans, participants without any LTPA, with LTPA >0 but <150 minutes/week, and with LTPA ≥150 min/week in the past week were classified as inactive, insufficiently active and sufficiently active, respectively [23, 24]. Furthermore, participants were asked “On a typical day, how much time do you usually spend sitting at school, at home, getting to and from places, or with friends including time spent sitting at a desk, traveling in a car or bus, reading, playing cards, watching television, or using a computer?” Responses were converted to hours per day then further categorized into <6, 6–8, and ≥8 hours/day (h/d) according to recent studies [13, 25, 26].
Sociodemographic characteristics, lifestyle behaviors, and chronic conditions
Self-reported sociodemographic characteristics included sex (male vs. female), race/ethnicity (Non-Hispanic White and other than Non-Hispanic White), and educational attainment (less than high school, high school, and beyond high school), family income-to-poverty ratio (<1.3 [lowest income], 1.3 ≤ 3.5, ≥3.5 [highest income]). Participants’ weight and height were measured during the physical examination at the MEC. Body mass index (BMI, kg/m2) was categorized into three groups (<25, 25.0–29.9, ≥30 kg/m2). Lifestyle factors included smoking status (never, former, and current), alcohol use (never, former, current, unknown), and the Healthy Eating Index-2015 (derived from 24-hour dietary recall interviews). The Healthy Eating Index-2015 indicates the overall dietary quality with a score ranging from 0 to 100 (worst to best-quality diet) [27].
Co-morbid conditions, including hypertension, hypercholesterolemia, cardiovascular disease (CVD) and diabetes were determined either through a health professional diagnosis or by direct measurements following the NHANES protocol. Hypertension was defined as blood pressure ≥130 mm Hg systolic or ≥80 mm Hg diastolic. Hypercholesterolemia was defined as total cholesterol level ≥240 mg/dL (to convert to mmol/L, multiply by 0.0259). A further identification of CVD and diabetes was participants instructed to take prescribed medications for these conditions [20].
Statistical analysis
All analyses were conducted following the NHANES analytic guidelines and accounted for the unequal probability of selection, over-sampling of certain subpopulations, and non-response adjustments to ensure nationally representative estimates. All analyses were done using Stata, version 17.0 (StataCorp LLC). Statistical tests were two-sided and statistical significance was set at p <0.05.
Sample sizes and weighted percentages were estimated by participants’ sociodemographic and lifestyle factors. Multivariable Cox proportional hazards regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for associations of LTPA and daily sitting time with all-cause, cancer-specific, and non-cancer mortality, respectively. Final-stage multivariable models were adjusted for age, sex, race/ethnicity, education, family poverty ratio, BMI, smoking status, alcohol use, and Healthy Eating Index-2015, hypertension, hypercholesterolemia, history of diabetes, and CVD for non-cancer adults and additionally adjusted for years since the first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown) for skin cancer survivors. To examine joint associations, participants were classified based on LTPA and sitting time to estimate mortality risks using multivariable Cox proportional hazards regression models. All analyses were conducted in skin cancer survivors and non-cancer adults, respectively. Stratified analyses were conducted by sex, BMI, smoking status, history of diabetes and CVD, and years since cancer diagnosis among skin cancer survivors.
Results
A total of 862 skin cancer survivors (184 melanoma, 459 non-melanoma and 249 unknown type) and 13691 non-cancer adults were included (Table 1). Skin cancer survivors were more likely to be Non-Hispanic White (96.9% vs 46.4%) and male (55.9% vs 46.4%) than non-cancer adults. Most (62.5%) survivors lived with cancer for >5 years and 16.2% of participants were diagnosed with skin cancer within 1 year. Patterns of LTPA and sitting time were similar in skin cancer survivors and non-cancer adults (Fig. 1). Among all skin cancer survivors, 46.3% reported no LTPA (inactive), 15.6% reported <150 min/week LTPA (insufficiently active), and 38.1% reported ≥150 min/week LTPA (sufficiently active) in the past week, while 38.1% reported sitting 6–8 h/d and 22.1% reported sitting >8 h/d. Of note, 29.6% of survivors reported no LTPA and concurrently sitting >6 h/d. More non-melanoma skin cancer survivors (43.2%) reported being sufficiently active than those with melanoma (33.9%), while their sitting time did not differ. After adjusting for sociodemographic and lifestyle factors and health conditions, levels of physical activity and daily sitting time were not significantly different between skin cancer survivors and non-cancer adults (all P>0.05).
Table 1.
Sample size for association of daily sitting time and physical activity level with mortality among US skin cancer survivors and non-cancer adults aged 50 years or older, NHANES 2007–2019a
| No. of Participants (Weighted %) |
|||||
|---|---|---|---|---|---|
| Skin Cancer Survivors |
Non-Cancer Adults | ||||
| Allb | Melanoma | Non-melanoma | Unknown | ||
|
| |||||
| Overall | 862 (100) | 184 (100) | 459 (100) | 249 (100) | 13691 (100) |
| Sex | |||||
| Male | 506 (55.9) | 114 (62.4) | 262 (54.2) | 149 (55.5) | 6662 (46.4) |
| Female | 356 (44.1) | 70 (37.6) | 197 (45.8) | 100 (44.5) | 7029 (53.6) |
| Age group, y | |||||
| 50–64 | 230 (40.0) | 49 (34.1) | 122 (42.3) | 64 (37.1) | 7771 (63.7) |
| ≥65 | 632 (60.0) | 135 (65.9) | 337 (57.7) | 185 (62.9) | 5920 (36.3) |
| Race/ethnicity | |||||
| Non-Hispanic White | 798 (96.9) | 166 (96.8) | 430 (96.6) | 230 (97.8) | 8304 (29.2) |
| Other than Non-Hispanic White | 64 (3.1) | 18 (3.2) | 29 (3.4) | 19 (2.2) | 5387 (70.8) |
| Family poverty ratio | |||||
| <1.3 | 168 (11.4) | 41 (11.8) | 75 (10.1) | 53 (12.1) | 4448 (20.6) |
| 1.3–<3.5 | 350 (36.3) | 77 (40.0) | 175 (32.6) | 115 (41.1) | 5532 (37.3) |
| ≥3.5 | 344 (52.3) | 66 (48.2) | 209 (57.3) | 81 (46.8) | 3711 (42.1) |
| Education | |||||
| <High school | 120 (9.2) | 21 (6.0) | 51 (7.6) | 51 (13.6) | 4160 (18.2) |
| High school | 187 (18.8) | 31 (15.5) | 96 (18.2) | 64 (22.1) | 3232 (24.9) |
| >High school | 555 (72.0) | 132 (78.5) | 312 (74.2) | 134 (64.3) | 6299 (56.9) |
| Weight status | |||||
| <25 kg/m2 | 248 (29.6) | 44 (22.0) | 140 (31.8) | 69 (28.7) | 3469 (25.3) |
| 25–<30 kg/m2 | 312 (35.8) | 69 (38.2) | 164 (35.0) | 90 (33.6) | 4742 (34.6) |
| ≥30 kg/m2 | 302 (34.6) | 71 (39.8) | 155 (33.2) | 90 (37.7) | 5480 (40) |
| Smoking status | |||||
| Never | 384 (47.2) | 77 (44.3) | 213 (49.4) | 103 (43.0) | 7045 (51.9) |
| Past | 391 (42.0) | 85 (44.2) | 200 (39.7) | 127 (48.6) | 4312 (32) |
| Current | 87 (10.8) | 22 (11.5) | 46 (10.9) | 19 (8.4) | 2334 (16.1) |
| Diabetes | |||||
| No | 699 (83.3) | 142 (76.6) | 393 (86.5) | 187 (79.2) | 10692 (83) |
| Yes | 162 (16.7) | 42 (23.4) | 66 (13.5) | 61 (20.8) | 2988 (16.9) |
| Cardiovascular Disease | |||||
| No | 649 (81.0) | 140 (81.4) | 341 (80.5) | 192 (83.0) | 11270 (84.8) |
| Yes | 213 (19.0) | 44 (18.6) | 118 (19.5) | 57 (17.0) | 2421 (15.2) |
| Time since cancer | |||||
| 0<1 | 144 (16.2) | 11 (5.3) | 84 (17.4) | 53 (21.0) | |
| 2–5 | 172 (21.3) | 17 (7.1) | 114 (27.8) | 45 (16.6) | |
| >5 | 546 (62.5) | 156 (87.6) | 261 (54.8) | 151 (62.5) | |
| Total Sitting Time, h/d | |||||
| <6 | 346 (39.8) | 71 (38.0) | 189 (41.8) | 94 (34.5) | 7226 (47.3) |
| 6–8 | 333 (38.1) | 79 (41.0) | 179 (37.9) | 95 (41.0) | 4003 (30.9) |
| >8 | 183 (22.1) | 34 (21.0) | 91 (20.3) | 60 (24.5) | 2462 (21.8) |
| Physical Activity Level | |||||
| Inactive | 454 (46.2) | 93 (50.5) | 234 (41.3) | 144 (53.6) | 8375 (54.2) |
| Insufficient Active | 129 (15.6) | 31 (15.6) | 64 (15.5) | 38 (15.5) | 1991 (16.7) |
| Physically Active | 278 (38.2) | 60 (33.9) | 160 (43.2) | 67 (30.9) | 3315 (29.1) |
Sample size was weighted to be nationally representative
One participant may have more than one type of skin cancer
Fig. 1.
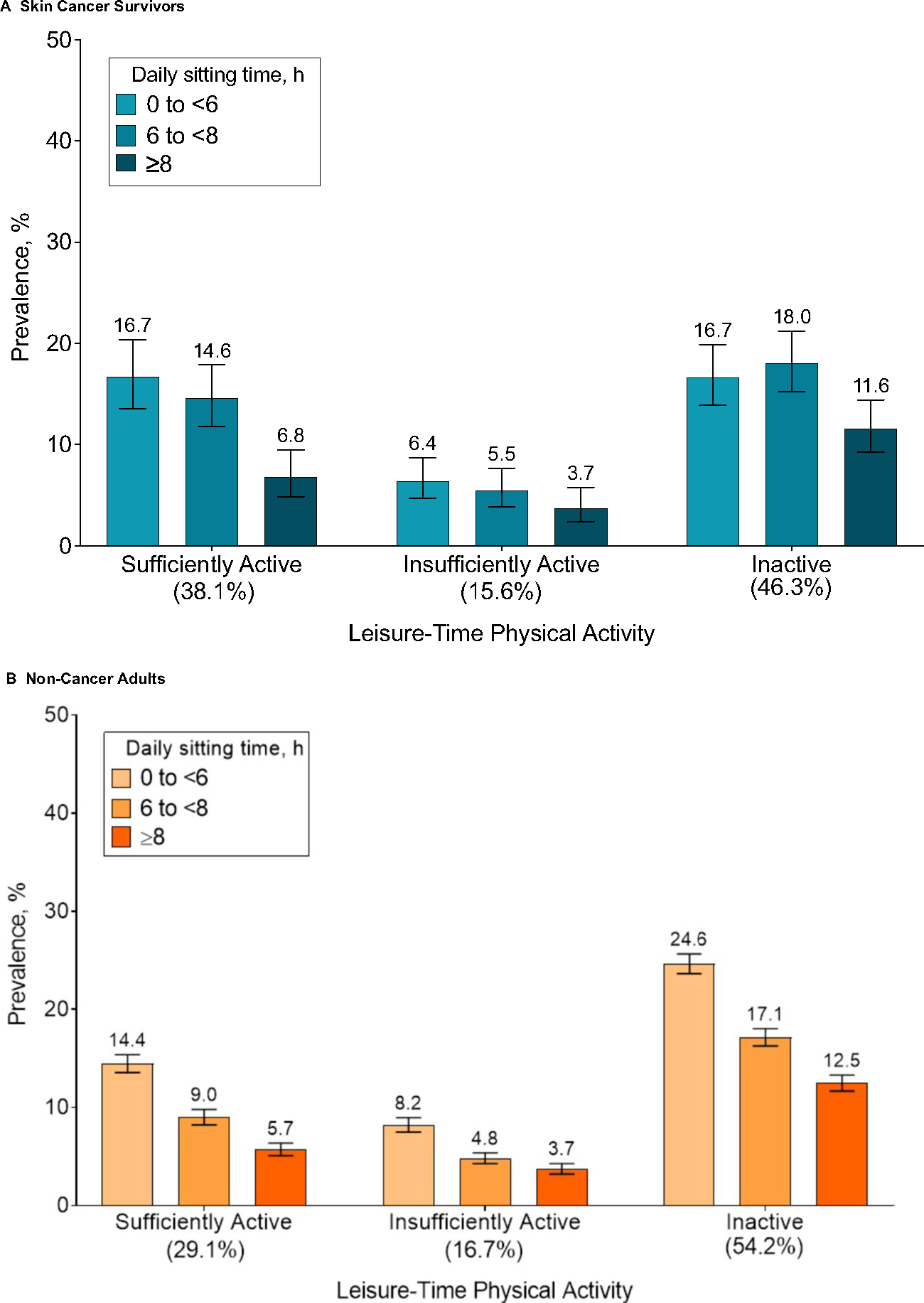
Patterns of leisure-time physical activity and daily sitting time among US skin cancer survivors and non-cancer adults aged 50 years or older, NHANES 2007–2019
During up to 13.2 years of follow-up (median, 6.3 years; 94,093 person-years), 207 deaths (cancer: 53) occurred in skin cancer survivors and 1970 (cancer: 414) in non-cancer adults. All-cause mortality did not differ across skin cancer type (Supplementary Figure 1). The all-cause death likelihood was higher in skin cancer survivors and non-cancer adults who were physically inactive compared to those who were active and raised as daily sitting hour increased (Table 2). After adjusting for covariates and skin cancer type, being active was associated with lower risks of all-cause (HR=0.69; 95% CI: 0.47 to 1.00) and non-cancer (HR=0.59; 95% CI: 0.36 to 0.97) mortality compared to being inactive in skin cancer survivors. Meanwhile, sitting 8 h/d was associated with higher risks of all-cause (HR=1.72; 95% CI: 1.11 to 2.67) and non-cancer (HR=1.76; 95% CI: 1.07 to 2.92) mortality compared to sitting <6 h/d (Table 3) in skin cancer survivors. Furthermore, daily sitting time was associated with higher risks of all-cause (HR per 1-h increase, 1.08 [95% CI, 1.01 to 1.15]) and non-cancer (HR per 1-h increase, 1.08 [95% CI, 1.02 to 1.15]) mortality in a dose-response manner in adults with skin cancers. No association of physical activity (HR=0.90; 95% CI: 0.46 to 1.78) and sitting time (HR=1.07; 95% CI: 0.92 to 1.25) with cancer-specific mortality was observed. In the joint analysis, inactive skin cancer survivors sitting >8 h/d had the highest mortality risks from all-cause (HR=2.26; 95% CI: 1.28 to 4.00) and non-cancer (HR=2.11; 95% CI,1.10 to 4.17) (Tables 4–5). Additionally, the associations of LTPA and sitting time with all-cause and cause-specific mortality did not differ between skin cancer survivors and non-cancer adults (all P for interaction>0.05, Fig. 2).
Table 2.
Association of total sitting time and physical activity level with all-cause mortality among US skin cancer survivors and non-cancer adults aged 50 years or older, NHANES 2007–2019
| Death/No. | Weighted death (%) | Hazard Ratio (95% CI) |
|||
|---|---|---|---|---|---|
| Age-adjusteda | MV model 1a,b | MV model 2a,b,c | |||
|
| |||||
| Skin Cancer Survivors | |||||
| Total Sitting Time, h/d | |||||
| <6 | 75/346 | 442529 (13.8) | 1 [reference] | 1 [reference] | 1 [reference] |
| 6–8 | 79/333 | 476866 (15.6) | 1.04 (0.71 to 1.50) | 1.03 (0.71 to 1.51) | 1.03 (0.71 to 1.51) |
| >8 | 53/183 | 325918 (18.4) | 1.73 (1.13 to 2.65) | 1.77 (1.16 to 2.70) | 1.72 (1.11 to 2.67) |
| per 1 h/d increase | NA | NA | 1.07 (1.01 to 1.14) | 1.08 (1.02 to 1.15) | 1.08 (1.01 to 1.15) |
| Physical Activity Level | |||||
| Inactive | 135/454 | 798621 (21.5) | 1 [reference] | 1 [reference] | 1 [reference] |
| Active | 72/408 | 446692 (10.3) | 0.52 (0.37 to 0.74) | 0.66 (0.45 to 0.98) | 0.69 (0.47 to 1.00) |
| Insufficient Active | 22/129 | 114580 (9.1) | 0.43 (0.25 to 0.71) | 0.53 (0.31 to 0.90) | 0.55 (0.31 to 0.97) |
| Physically Active | 50/278 | 332112 (10.9) | 0.57 (0.38 to 0.85) | 0.74 (0.47 to 1.15) | 0.75 (0.49 to 1.15) |
| Non-Cancer Adults | |||||
| Total Sitting Time, h/d | |||||
| <6 | 878/7226 | 5422310 (9.4) | 1 [reference] | 1 [reference] | 1 [reference] |
| 6–8 | 640/4003 | 4287795 (11.4) | 1.24 (1.09 to 1.42) | 1.28 (1.12 to 1.46) | 1.24 (1.08 to 1.42) |
| >8 | 452/2462 | 3532486 (13.3) | 1.72 (1.48 to 1.99) | 1.83 (1.57 to 2.13) | 1.74 (1.50 to 2.03) |
| per 1 h/d increase | NA | NA | 1.07 (1.06 to 1.09) | 1.08 (1.06 to 1.10) | 1.07 (1.06 to 1.09) |
| Physical Activity Level | |||||
| Inactive | 1490/8385 | 9927965 (15.0) | 1 [reference] | 1 [reference] | 1 [reference] |
| Active | 480/5306 | 3314626 (5.9) | 0.47 (0.41 to 0.54) | 0.56 (0.49 to 0.65) | 0.60 (0.52 to 0.69) |
| Insufficient Active | 209/1991 | 1373957 (6.8) | 0.52 (0.44 to 0.63) | 0.61 (0.47 to 0.81) | 0.64 (0.53 to 0.78) |
| Physically Active | 271/3315 | 1940669 (5.5) | 0.44 (0.37 to 0.52) | 0.43 (0.33 to 0.57) | 0.56 (0.47 to 0.67) |
Adjusted for age (years)
Multivariable (MV) model additionally adjusted for sex (male or female), race/ethnicity (Non-Hispanic White and other than Non-Hispanic White), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), Healthy Eating Index-2015
Additionally adjusted for hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), history of CVD (yes or no), years after first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown)
Table 3.
Association of daily sitting time and physical activity level with cancer and non-cancer mortality among US skin cancer survivors and non-cancer adults aged 50 years or older, NHANES 2007–2019
| Skin Cancer Survivors |
Non-Cancer Adults |
|||||
|---|---|---|---|---|---|---|
| Death/No. | Weighted death (%) | Hazard Ratio (95% CI)a | Death/No. | Weighted death (%) | Hazard Ratio (95% CI)b | |
|
| ||||||
| Cancer Mortality | ||||||
| Total Sitting Time, h/d | ||||||
| <6 | 24/346 | 139216 (4.4) | 1 [reference] | 212/7226 | 950296 (2.5) | 1 [reference] |
| 6–8 | 19/333 | 97594 (3.2) | 0.72 (0.34 to 1.52) | 132/4003 | 617691 (2.5) | 1.07 (0.80 to 1.44) |
| >8 | 10/183 | 87307 (4.9) | 1.65 (0.64 to 4.23) | 70/2462 | 360171 (2.0) | 1.04 (0.71 to 1.52) |
| per 1 h/d increase | NA | NA | 1.07 (0.92 to 1.25) | 1.01 (0.97 to 1.06) | ||
| Physical Activity Level | ||||||
| Inactive | 27/454 | 161683 (4.4) | 1 [reference] | 276/8385 | 1210214 (2.7) | 1 [reference] |
| Active | 26/408 | 162434 (3.8) | 0.90 (0.46 to 1.78) | 138/5306 | 717945 (1.9) | 0.97 (0.71 to 1.34) |
| Insufficient Active | 11/129 | 55448 (4.4) | 0.85 (0.31 to 2.34) | 45/1991 | 205130 (1.5) | 0.75 (0.49 to 1.13) |
| Physically Active | 15/278 | 106987 (3.5) | 0.93 (0.43 to 2.01) | 93/3315 | 512816 (2.2) | 1.12 (0.78 to 1.62) |
| Non-Cancer Mortality | ||||||
| Total Sitting Time, h/d | ||||||
| <6 | 51/346 | 303312 (9.5) | 1 [reference] | 666/7226 | 2664577 (6.9) | 1 [reference] |
| 6–8 | 60/333 | 379272 (12.4) | 1.20 (0.76 to 1.89) | 508/4003 | 2240839 (8.9) | 1.30 (1.12 to 1.51) |
| >8 | 43/183 | 238611 (13.4) | 1.76 (1.07 to 2.92) | 382/2462 | 1994819 (11.2) | 1.99 (1.69 to 2.34) |
| per 1 h/d increase | NA | NA | 1.08 (1.02 to 1.15) | 1.09 (1.07 to 1.11) | ||
| Physical Activity Level | ||||||
| Inactive | 108/454 | 636938 (17.2) | 1 [reference] | 1214/8385 | 8112644 (12.3) | 1 [reference] |
| Active | 46/408 | 284257 (6.6) | 0.59 (0.36 to 0.97) | 342/5306 | 2237708 (4.0) | 0.51 (0.43 to 0.59) |
| Insufficient Active | 11/129 | 59132 (4.7) | 0.41 (0.20 to 0.83) | 164/1991 | 1066262 (5.2) | 0.62 (0.51 to 0.77) |
| Physically Active | 35/278 | 225125 (7.4) | 0.68 (0.38 to 1.19) | 178/3315 | 1171446 (3.3) | 0.43 (0.35 to 0.52) |
Adjusted for for age, sex (male or female), race/ethnicity (non-Hispanic White and other than Non-Hispanic White), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), and Healthy Eating Index-2015, hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), history of CVD (yes or no), years after first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown)
Adjusted for for age, sex (male or female), race/ethnicity (Non-Hispanic White and other than Non-Hispanic White), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), and Healthy Eating Index-2015, hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), and history of CVD (yes or no)
Table 4.
Joint association of total sitting time and physical activity level with all-cause mortality among US skin cancer survivors and non-cancer adults aged 50 years or older, NHANES 2007–2019
| Total Sitting Time, h/d | Death/No. | Weighted death (%) | Hazard Ratio (95% CI) |
|||
|---|---|---|---|---|---|---|
| Age-adjusteda | MV model 1a,b | MV model 2a,b,c | ||||
|
| ||||||
| Skin Cancer Survivors | ||||||
| Insufficient/Physically Active | <6 | 34/181 | 330574 (11.8) | 1 [reference] | 1 [reference] | 1 [reference] |
| 6–8 | 28/155 | 235449 (9.8) | 0.77 (0.43 to 1.39) | 0.74 (0.42 to 1.33) | 0.83 (0.46 to 1.50) | |
| >8 | 10/72 | 104015 (8.2) | 0.92 (0.38 to 2.23) | 0.98 (0.42 to 2.32) | 1.02 (0.40 to 2.56) | |
| Inactive | <6 | 41/165 | 333219 (16.6) | 1.26 (0.74 to 2.15) | 0.98 (0.55 to 1.74) | 1.01 (0.56 to 1.81) |
| 6–8 | 51/178 | 479850 (22.1) | 1.64 (0.98 to 2.74) | 1.32 (0.78 to 2.22) | 1.33 (0.78 to 2.27) | |
| >8 | 43/111 | 384863 (27.6) | 3.04 (1.76 to 5.25) | 2.40 (1.36 to 4.25) | 2.26 (1.28 to 4.00) | |
| Non-Cancer Adults | ||||||
| Insufficient/Physically Active | <6 | 260/2909 | 1683915 (6.1) | 1 [reference] | 1 [reference] | 1 [reference] |
| 6–8 | 152/1493 | 1093657 (6.5) | 1.18 (0.92 to 1.52) | 1.22 (0.95 to 1.57) | 1.23 (0.96 to 1.57) | |
| >8 | 68/904 | 537054 (4.7) | 1.06 (0.76 to 1.48) | 1.23 (0.88 to 1.71) | 1.27 (0.91 to 1.77) | |
| Inactive | <6 | 618/4317 | 3738395 (12.4) | 1.82 (1.51 to 2.19) | 1.57 (1.29 to 1.91) | 1.54 (1.26 to 1.88) |
| 6–8 | 488/2510 | 3194138 (15.3) | 2.32 (1.91 to 2.81) | 2.05 (1.68 to 2.51) | 1.93 (1.58 to 2.36) | |
| >8 | 384/1558 | 2995432 (19.7) | 3.56 (2.90 to 4.36) | 3.19 (2.58 to 3.93) | 2.92 (2.36 to 3.59) | |
Adjusted for age (years)
Multivariable (MV) model additionally adjusted for sex (male or female), race/ethnicity (Non-Hispanic White and other than Non-Hispanic White), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), Healthy Eating Index-2015
Additionally adjusted for hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), and history of CVD (yes or no) in addition to years after first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown) for skin cancer survivors
Table 5.
Joint association of total sitting time and physical activity level with cancer and non-cancer mortality among US non-cancer adults aged 50 years or older, NHANES 2007–2019
| Total Sitting Time, h/d | Skin Cancer Survivors |
Non-Cancer Adults |
|||||
|---|---|---|---|---|---|---|---|
| Death/No. | Weighted death (%) | Hazard Ratio (95% CI)a | Death/No. | Weighted death (%) | Hazard Ratio (95% CI)b | ||
|
| |||||||
| Cancer Mortality | |||||||
| Insufficient/Physically Active | <6 | 76/2889 | 1110874 (6.1) | 1 [reference] | 76/2889 | 1110874 (6.1) | 1 [reference] |
| ≥6 | 62/2397 | 1087141 (5.8) | 0.58 (0.19 to 1.78) | 62/2397 | 1087141 (5.8) | 1.14 (0.74 to 1.75) | |
| Inactive | <6 | 131/4247 | 2406006 (12.2) | 0.59 (0.20 to 1.72) | 131/4247 | 2406006 (12.2) | 1.08 (0.70 to 1.67) |
| ≥6 | 140/4068 | 4126380 (17.2) | 1.04 (0.43 to 2.55) | 140/4068 | 4126380 (17.2) | 1.10 (0.73 to 1.64) | |
| Non-Cancer Mortality | |||||||
| Insufficient /Physically Active | <6 | 182/2889 | 741630 (4.1) | 1 [reference] | 182/2889 | 741630 (4.1) | 1 [reference] |
| ≥6 | 158/2397 | 738440 (3.9) | 1.05 (0.53 to 2.09) | 158/2397 | 738440 (3.9) | 1.27 (0.98 to 1.65) | |
| Inactive | <6 | 474/4247 | 1835592 (9.3) | 1.25 (0.56 to 2.78) | 474/4247 | 1835592 (9.3) | 1.71 (1.38 to 2.12) |
| ≥6 | 732/4068 | 3497218 (14.6) | 2.11 (1.10 to 4.17) | 732/4068 | 3497218 (14.6) | 2.88 (2.35 to 3.54) | |
Adjusted for for age, sex (male or female), race/ethnicity (Non-Hispanic White and other than Non-Hispanic White), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), and Healthy Eating Index-2015, hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), history of CVD (yes or no), years after first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown)
Adjusted for for age, sex (male or female), race/ethnicity (Non-Hispanic White and other than Non-Hispanic White), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), and Healthy Eating Index-2015, hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), and history of CVD (yes or no)
Fig. 2.
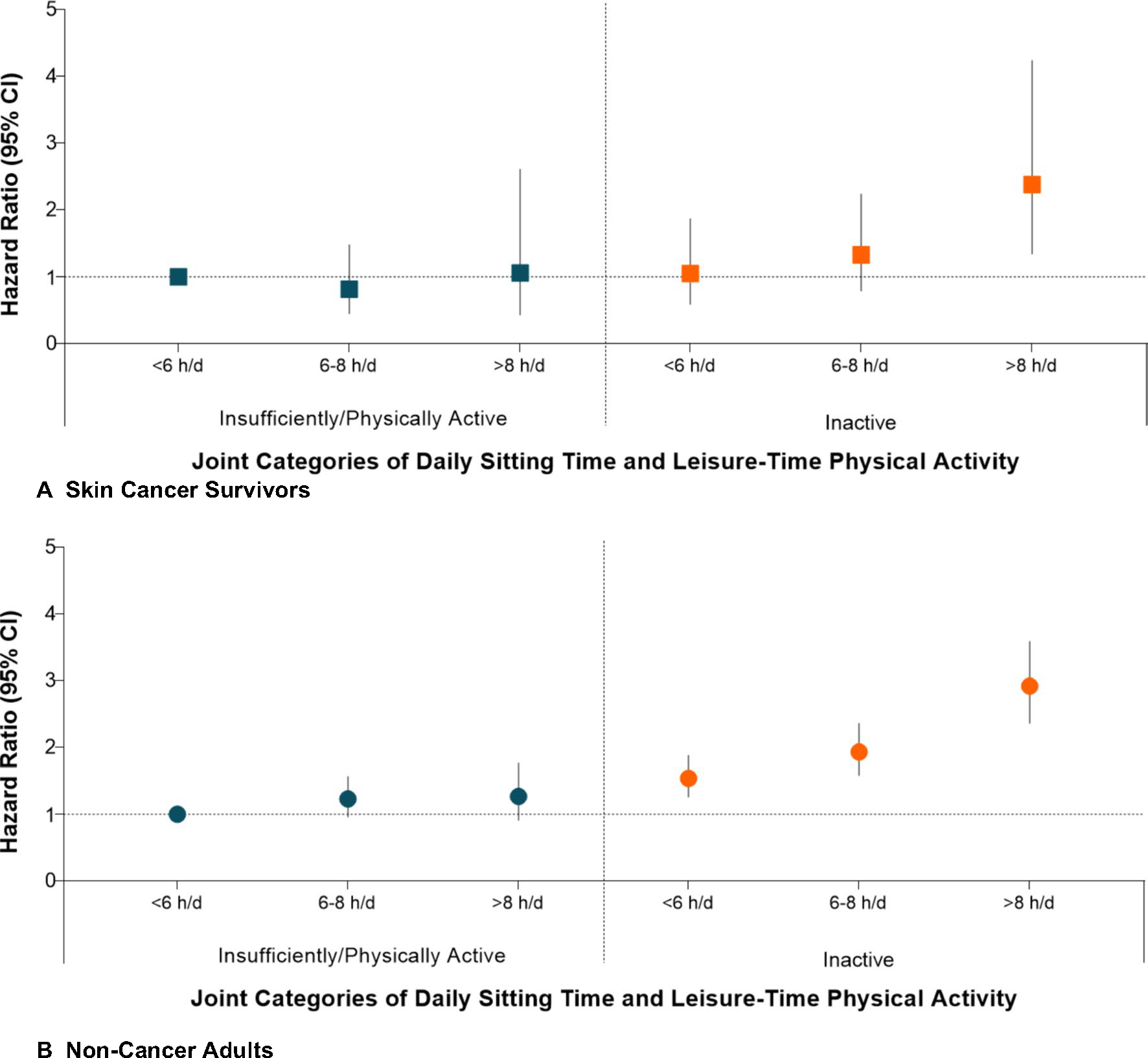
Association of leisure-time physical activity and daily sitting time with all-cause mortality among US skin cancer survivors and non-cancer adults aged 50 years or older, NHANES 2007–2019a. aEstimates were adjusted for age, sex (male or female), race/ethnicity (non-Hispanic white and other), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), and Healthy Eating Index-2015, hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), history of CVD (yes or no), years after first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown)
Results were similar when restricting to non-melanoma skin cancers (Supplementary Table 1) and stratified by BMI, smoke status, history of diabetes and CVD, and years since cancer diagnosis (Fig. 3). The association between LTPA and all-cause mortality was more apparent in females (HR=0.36; 95% CI: 0.18 to 0.69) than in males (HR=0.72; 95% CI: 0.44 to 1.18) after skin cancer diagnoses (Pinteraction<.05) (Supplementary Table 2). Similarly, the combination of prolonged sitting >8 h/d and physical inactivity was strongly associated with increased all-cause mortality among female survivors (HR=4.00; 95% CI, 1.69 to 9.42) but emerged as a statistically non-significant association (HR=1.54; 95% CI, 0.86 to 2.76) among male survivors (Pinteraction<.001) ((Supplementary Table 3).
Fig. 3.
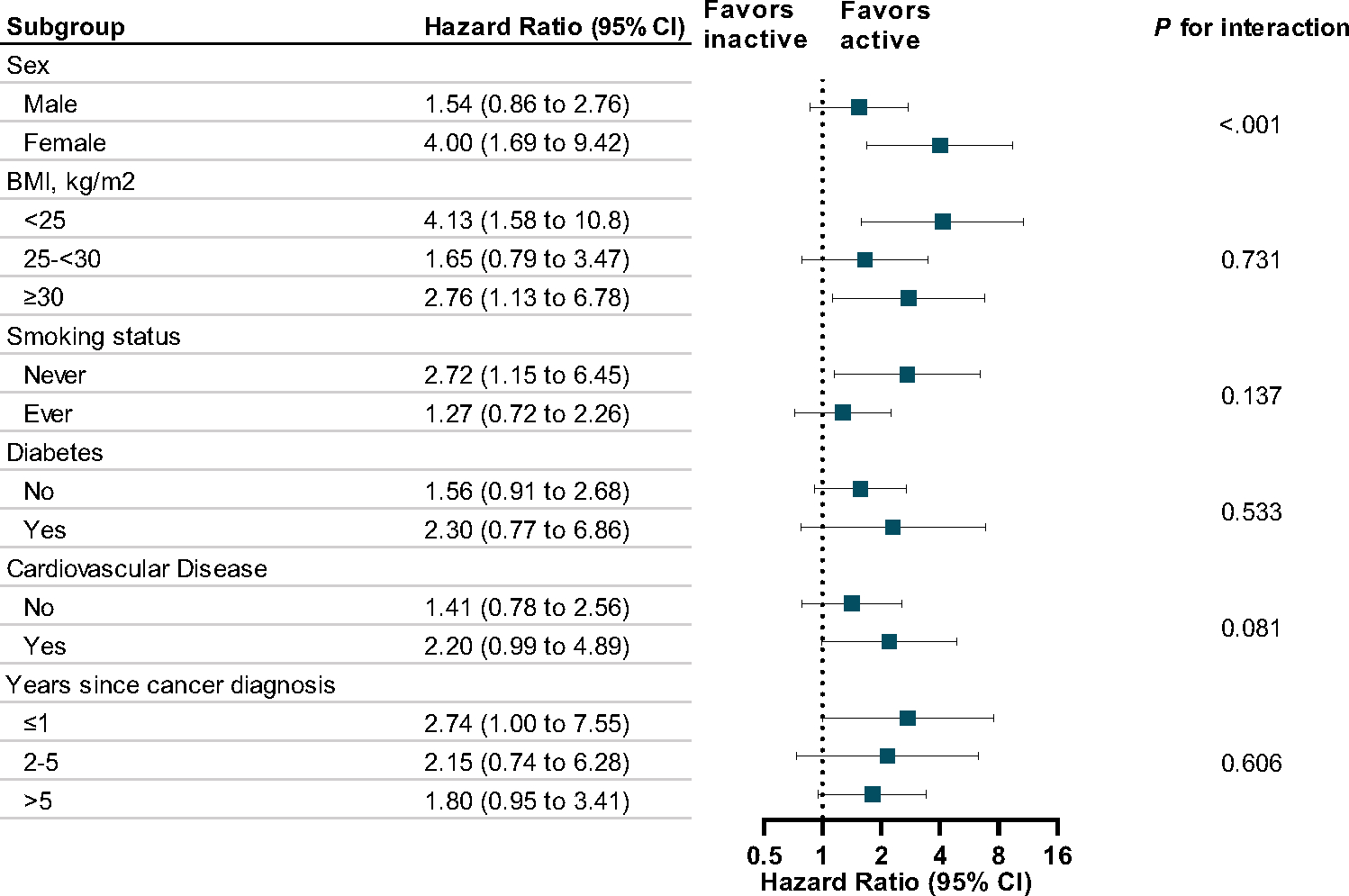
Stratified hazard ratios of all-cause mortality comparing most inactive (no physical activity and sitting >8 h/d) with most active (any physical activity and sitting <6 h/d) skin cancer survivors aged 50 years or older, NHANES 2007–2019a. aEstimates were adjusted for age, sex (male or female), race/ethnicity (non-Hispanic white and other), education attainment (less than high school, high school graduate, above high school), family poverty ratio (<1.30, 1.30–3.49, or ≥3.5), body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) (<18.5, 18.5–24.9, 25–29.9, and ≥30), smoking status (never, former, and current), alcohol use (never, former, and current), and Healthy Eating Index-2015, hypertension (yes or no), hypercholesterolemia (yes or no), history of diabetes (yes or no), history of CVD (yes or no), years after first diagnosis of cancer, and skin cancer type (melanoma, non-melanoma, unknown)
Discussion
In this US nationally representative sample of skin cancer survivors and non-cancer adults, nearly half reported no LTPA and more than half reported sitting >6 h/d. Notably, over 1/3 of skin cancer survivors reported no LTPA and concurrently sitting >6 h/d. During up to 13.2 years of follow-up, skin cancer survivors and non-cancer adults who reported participation in any LTPA and a shorter sitting time both had lower all-cause and non-cancer mortality risks. No associations were found for cancer mortality. In the joint analyses of LTPA and sitting time, inactive skin cancer survivors and non-cancer adults with the longest sitting time (>8 h/d) had a two-fold increase in all-cause mortality risk. The association of LTPA and mortality risks were more apparent in female than in male skin cancer survivors. Particularly, female skin cancer survivors with no LTPA and sitting >6 h/d had as much as a four-fold increase in the risk of all-cause mortality compared to those with any LTPA and sitting <6h/d.
The long-term health impacts of LTPA and daily sitting time among skin cancer survivors had been largely unknown previously. To our knowledge, this study is the first to investigate the associations of LTPA and daily sitting time with mortality in a nationally representative sample of skin cancer survivors. Previous studies suggested an association of LTPA, particularly in the outdoor setting, with increased risks of skin cancer recurrence [15, 16, 28], which may discourage skin cancer survivors to engage in LTPA. However, most skin cancer survivors die from chronic diseases related to a sedentary lifestyle [17]. The present study revealed that LTPA participation and limited sitting time were associated with decreased mortality risks driven by non-cancer causes but not cancer. The impacts of LTPA and sitting time on mortality risks were similar in skin cancer survivors and non-cancer adults.
The association of sitting time and LTPA with mortality has been investigated in the general population and survivors of non-skin cancer. Evidence to date suggests that the combination of low LTPA and prolonged sitting increase the risk of all-cause and CVD mortality in diverse populations [25, 26, 29, 30]. Several studies found a dose-response relationship between daily sitting time and mortality risks, which was more apparent in physically inactive adults. We have previously found that survivors of non-skin cancer who did not meet the PA guidelines (LTPA <150 min/week) and sat >8 h/d had a five-fold increase in the risk of death from all-cause, cancer, and non-cancer compared with those who met PA guidelines and sat <4 h/d [13]. Our present study revealed that prolonged sitting combined with a lack of LTPA was strongly associated with risks of death from all-cause and non-cancer but not cancer particularly in female skin cancer survivors. Previous studies also found sex-specific effects of LTPA on mortality outcomes, suggesting an inverse association between LTPA and CVD and respiratory disease mortality in females but not in males [31], and a stronger association of LTPA and survival in female than in male cancer non-skin cancer survivors [32].
The 2022 ACS guidelines highlighted that cancer survivors who are disease free or who have stable disease following their treatment and recovery need to engage in LTPA, and limit time spent sitting to improve long-term survivorship [12]. The current evidence on health benefits of regular LTPA and limiting sitting time was largely derived from cancer survivors of the breast, colorectal and prostate, while few investigations were conducted among skin cancer survivors despite being the most common type of cancer. The present analysis provides direct evidence on the associations of LTPA and sitting in skin cancer survivors and suggests the potential to reduce excess mortality risks through participation in LTPA and limiting sitting time. Furthermore, the observed sex-specific associations suggest that future development of strategies and interventions need to take consideration of sex.
The potential mechanisms underlying observed associations could be behavioral and biologic. Previous research suggested that skin cancer survivors who had low LTPA could experience psychosocial impairments from complications (e.g., scarring due to surgeries to treat tumors) that lead to a lower motivation of LTPA and an association with poor health status and worse survivorship [11]. Physical activity can improve metabolic regulation, boost immunity, improve cardiometabolic health, and reduce the risk of chronic and infectious diseases [33–35]. Cancer survivors, particularly long term survivors, experience increased risks of cardiovascular diseases and diabetes [36]. The growing evidence from experimental and epidemiologic studies indicates that low LTPA and prolonged sitting are associated with insulin resistance, impaired glucose control, and unfavorable profiles of cardiometabolic biomarkers [37]. These biologic mechanisms could explain how LTPA and sitting time are associated with all-cause and non-cancer mortality driven by CVD. Sex differences observed in this study can be explained by similar findings in general populations that men need to expend more energy through exercise than women to achieve equal mortality benefits [38]. Regular LTPA can promote the regulation of bioavailable sex hormones (e.g., estradiol) that lead to differential effects on mortality, particularly in adults 50 years or older [39]. Future studies are needed to confirm the mechanisms of these sex-specific associations.
Strengths and limitations
The study used a nationally representative sample of skin cancer survivors and non-cancer adults, which allows the findings to be generalized to the US population. Some limitations need to be considered. First, information on sun exposure (i.e., risk factor of skin cancer occurrence and recurrence), such as LTPA setting (outdoor vs. indoor), and sun protective behavior were not available for most participants and were not adjusted. Nevertheless, the current findings suggested a statistically significant association of LTPA with mortality risks that was mainly driven by non-cancer causes. Second, LTPA and sitting time were self-reported and not device measured. However, the GPAQ is a valid tool to assess LTPA and sitting time in epidemiologic studies [22]. Third, detailed information on skin cancer stages and treatment was not collected in the NHANES. Nevertheless, most skin cancer cases in the US were detected at early stages. Additionally, skin cancer type (melanoma, non-melanoma, unknown) did not affect the results.
Conclusion
In this prospective cohort of US skin cancer survivors and non-cancer adults, participating in LTPA and limiting sitting time were associated with decreased all-cause and non-cancer mortality risks. The impacts of LTPA and sitting time on mortality risks were similar in skin cancer survivors and non-cancer adults. The association of the combination of lack of LTPA and prolonged sitting with elevated mortality was more noticeable in female skin cancer survivors. This study provides evidence to support recommendations that skin cancer survivors should avoid sedentary lifestyle for long-term health benefits.
Supplementary Material
Funding information
Chao Cao is supported by the U.S. National Cancer Institute grant 5T32CA092203
Footnotes
Competing interests The authors declare no competing interests.
Ethical approval This study involves secondary data analysis utilizing unidentified data, obviating the need for IRB approval.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s00520-023-08192-6.
Data availability
The data underlying this article are availably publicly through https://www.cdc.gov/nchs/nhanes/index.htm
References
- 1.Stern RS (2010) Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol 146(3):279–282 [DOI] [PubMed] [Google Scholar]
- 2.Guy GP Jr, Thomas CC, Thompson T et al. (2015) Vital signs: melanoma incidence and mortality trends and projections - United States, 1982–2030. MMWR Morb Mortal Wkly Rep 64(21):591–596 [PMC free article] [PubMed] [Google Scholar]
- 3.American Cancer Society. Skin Cancer. https://www.cancer.org/cancer/skin-cancer.html. Accessed 8 Aug 2023
- 4.Joosse A, de Vries E, Eckel R et al. (2011) Gender Differences in Melanoma Survival: Female Patients Have a Decreased Risk of Metastasis. J Investig Dermatol 131(3):719–726 [DOI] [PubMed] [Google Scholar]
- 5.American Cancer Society. Survival Rates for Melanoma Skin Cancer. https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html. Accessed 8 Aug 2023
- 6.Le HV, Le CHH, Le PHUUU et al. (2020) Incidence and trends of skin cancer in the United States, 1999–2016. J Clin Oncol 38(15_suppl):10077–10077 [Google Scholar]
- 7.Stein KD, Syrjala KL, Andrykowski MA (2008) Physical and psychological long-term and late effects of cancer. Cancer 112(11 Suppl):2577–2592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cornish D, Holterhues C, van de Poll-Franse LV et al. (2009) A systematic review of health-related quality of life in cutaneous melanoma. Ann Oncol 20:vi51–vi58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Miller CJ, O’Malley V et al. (2018) Patient quality of life fluctuates before and after Mohs micrographic surgery: A longitudinal assessment of the patient experience. J Am Acad Dermatol 78(6):1060–1067 [DOI] [PubMed] [Google Scholar]
- 10.Lukowiak TM, Perz AM, Veerabagu SA et al. (2021) Patient Quality of Life After Interpolated Flap Repair of Nasal Mohs Surgery Defects: A Multicenter Prospective Cohort Study. JAMA Dermatol 157(10):1213–1216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sobanko JF, Sarwer DB, Zvargulis Z, Miller CJ (2015) Importance of physical appearance in patients with skin cancer. Dermatol Surg 41(2):183–188 [DOI] [PubMed] [Google Scholar]
- 12.Rock CL, Thomson CA, Sullivan KR et al. (2022) American Cancer Society nutrition and physical activity guideline for cancer survivors. CA Cancer J Clin 72(3):230–262 [DOI] [PubMed] [Google Scholar]
- 13.Cao C, Friedenreich CM, Yang L (2022) Association of Daily Sitting Time and Leisure-Time Physical Activity With Survival Among US Cancer Survivors. JAMA Oncol 8(3):395–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabatabaie S, Litt JS, Crane LA (2020) The experience of outdoor physical activity for skin cancer survivors: understanding the importance of the built and natural environments. J Cancer Surviv 14(5):739–756 [DOI] [PubMed] [Google Scholar]
- 15.Lynn J, Urda J, Pierce P (2016) Sun exposure and exercise: the good, the bad, and the behavior change. ACSMs Health Fit J 20(3):11–15 [Google Scholar]
- 16.Betof AS, Dewhirst MW, Jones LW (2013) Effects and potential mechanisms of exercise training on cancer progression: a translational perspective. Brain Behav Immun 30 Suppl(0):S75–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewis KG, Weinstock MA (2004) Nonmelanoma Skin Cancer Mortality (1988–2000): The Rhode Island Follow-Back Study. Arch Dermatol 140(7):837–842 [DOI] [PubMed] [Google Scholar]
- 18.Cao C, Patel AV, Liu R, Cao Y, Friedenreich CM, Yang L (2023) Trends and cancer-specific patterns of physical activity, sleep duration, and daily sitting time among US cancer survivors, 1997–2018. J Natl Cancer Inst. 10.1093/jnci/djad146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lauby-Secretan B, Scoccianti C, Loomis D et al. (2016) Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med 375(8):794–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao C, Cade WT, Li S et al. (2021) Association of Balance Function With All-Cause and Cause-Specific Mortality Among US Adults. JAMA Otolaryngol Head Neck Surg 147(5):460–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sattar N, Preiss D (2017) Reverse Causality in Cardiovascular Epidemiological Research. Circulation 135(24):2369–2372 [DOI] [PubMed] [Google Scholar]
- 22.Armstrong T, Bull F (2006) Development of the world health organization Global Physical Activity Questionnaire (GPAQ). J Public Health 14(2):66–70 [Google Scholar]
- 23.Ussery EN, Fulton JE, Galuska DA et al. (2018) Joint Prevalence of Sitting Time and Leisure-Time Physical Activity Among US Adults, 2015–2016. JAMA 320(19):2036–2038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piercy KL, Troiano RP, Ballard RM et al. (2018) The Physical Activity Guidelines for Americans. JAMA 320(19):2020–2028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ekelund U, Steene-Johannessen J, Brown WJ et al. (2016) Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388(10051):1302–1310 [DOI] [PubMed] [Google Scholar]
- 26.Stamatakis E, Gale J, Bauman A et al. (2019) Sitting Time, Physical Activity, and Risk of Mortality in Adults. J Am Coll Cardiol 73(16):2062–2072 [DOI] [PubMed] [Google Scholar]
- 27.Krebs-Smith SM, Pannucci TE, Subar AF et al. (2018) Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet 118(9):1591–1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Behrens G, Niedermaier T, Berneburg M et al. (2018) Physical activity, cardiorespiratory fitness and risk of cutaneous malignant melanoma: Systematic review and meta-analysis. PLOS ONE 13(10):e0206087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Q, Liu F, Li J et al. (2020) Sedentary behavior and risk of incident cardiovascular disease among Chinese adults. Sci Bull 65(20):1760–1766 [DOI] [PubMed] [Google Scholar]
- 30.Li S, Lear SA, Rangarajan S et al. (2022) Association of Sitting Time With Mortality and Cardiovascular Events in High-Income, Middle-Income, and Low-Income Countries. JAMA Cardiol. 10.1001/jamacardio.2022.1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.El Saadany T, Richard A, Wanner M et al. (2017) Sex-specific effects of leisure-time physical activity on cause-specific mortality in NHANES III. Prev Med 101:53–59 [DOI] [PubMed] [Google Scholar]
- 32.Friedenreich CM, Stone CR, Cheung WY et al. (2020) Physical Activity and Mortality in Cancer Survivors: A Systematic Review and Meta-Analysis. JNCI Cancer. Spectrum 4(1):pkz080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nieman DC, Wentz LM (2019) The compelling link between physical activity and the body’s defense system. J Sport Health Sci 8(3):201–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Exercise MJ, Health C (2003) Circulation 107(1):e2–e5 [DOI] [PubMed] [Google Scholar]
- 35.Liao J, Hu M, Imm K et al. (2022) Association of daily sitting time and leisure-time physical activity with body fat among US adults. J Sport Health Sci. 10.1016/j.jshs.2022.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Florido R, Daya Natalie R, Ndumele Chiadi E et al. (2022) Cardiovascular Disease Risk Among Cancer Survivors. J Am Coll Cardiol 80(1):22–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunstan DW, Dogra S, Carter SE et al. (2021) Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol 18(9):637–648 [DOI] [PubMed] [Google Scholar]
- 38.Al-Mallah MH, Juraschek SP, Whelton S et al. (2016) Sex Differences in Cardiorespiratory Fitness and All-Cause Mortality: The Henry Ford ExercIse Testing (FIT) Project. Mayo Clin Proc 91(6):755–762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choudhury F, Bernstein L, Hodis HN, et al. Physical activity and sex hormone levels in estradiol- and placebo-treated postmenopausal women. Menopause (New York, N.Y.) 2011;18(10):1079–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are availably publicly through https://www.cdc.gov/nchs/nhanes/index.htm


