Summary:
Superior orbital fissure syndrome (SOFS) is a rare complication of craniofacial fracture, caused by damage to cranial nerves Ⅲ, Ⅳ, Ⅴ, and Ⅵ, which typically is associated with ophthalmoplegia, blepharoptosis, pupil dilatation and fixation, and upper eyelid and forehead hypesthesia. However, we here describe a very unusual case of craniofacial fracture with SOFS in the absence of pupil symptoms, involving a patient who was injured when he fell while riding his bicycle. Upon medical examination, we observed mild blepharoptosis and ophthalmoplegia of the right eye without pupillary symptoms. Computed tomography (CT) revealed basal skull and zygomatic fractures. After the patient had been treated conservatively for his skull base fracture, facial bone reduction was performed at our hospital. Because ophthalmoplegia and blepharoptosis remained after the surgery, we checked the preoperative CT images again and discovered stenosis of the superior orbital fissure. Postoperative CT revealed a widening of the superior orbital fissure after the facial bone reduction, and therefore, the patient was given steroid treatment without additional surgery. At 6 months postoperatively, the cranial nerves had completely recovered. Our finding emphasizes that, in contrast to common theory, trauma-induced SOFS can result in pupil-sparing oculomotor nerve palsy.
Traumatic superior orbital fissure syndrome (SOFS) is a rare condition, representing only 0.3% of craniofacial traumatic injuries.1 It is characterized by the narrowing of the superior orbital fissure, resulting in damage to cranial nerves III, IV, V, and VI, which traverse this structure. Common manifestations are blepharoptosis, ophthalmoplegia, dilatation and fixation of the pupil, and hypesthesia of the upper eyelid and forehead.1,2 Pupil-sparing oculomotor nerve palsy, in which there are no pupillary symptoms and only ophthalmoplegia, is well known as a characteristic of diabetic oculomotor nerve palsy.3,4 However, we here present a rare case of traumatic SOFS with pupil-sparing oculomotor nerve palsy.
CASE DESCRIPTION
A 40-year-old man fell from his bicycle and was taken to the emergency department of a local hospital. A computed tomography (CT) scan revealed basal skull and zygomatic fractures, and epidural hematoma. Because of the absence of symptom aggravation, neurosurgical intervention was deemed unnecessary, and conservative treatment was provided. The patient was transferred to our department for treatment of his right zygomatic fracture on the seventh day after the injury. For his right eye, preserved abduction together with mild blepharoptosis and impairments in adduction, depression, and elevation were observed (Fig. 1). (See figure, Supplemental Digital Content 1, which shows a photograph of the patient at the initial examination. http://links.lww.com/PRSGO/D214.) His pupillary light reflex was normal and anisocoria was absent, but sensory deficits in the infraorbital nerve region, trismus, and malocclusion were observed. A CT scan revealed skull base and right zygomatic fractures. Observations included a fracture line on the right greater wing of the sphenoid bone, medial displacement of the zygomatic body, and an alveolar fracture of the right maxilla. The skull base fracture was reevaluated by our neurosurgery department, who, as did the neurosurgeons before them, decided that it did not require surgery. As for the facial bone fractures, our department decided that surgical treatment was necessary, and facial bone reduction and fixation were performed on the 14th day after the injury.
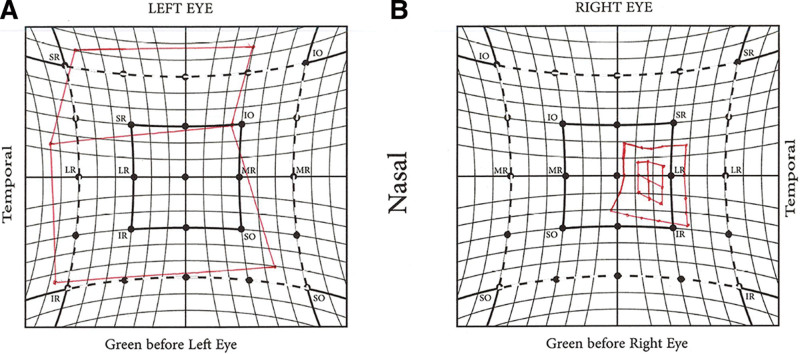
Fig. 1.
Hess chart examination at the initial examination. The Hess chart examination showed ophthalmoplegia. A, Left eye. B, Right eye.
Under general anesthesia, the operative field was approached using infrabrow, subciliary, and oral vestibular incisions. The zygomatic bone was elevated and repositioned, and also the alveolar fracture area was repositioned and intermaxillary fixed using a preoperatively prepared arch bar. The frontozygomatic suture and infraorbital rim were then fixed with a 0.6-mm-thick titanium plate, and a 2.0-mm Kirschner-wire was inserted among the right and left zygomatic bodies for additional stabilization.
Given that there was no significant improvement in adduction, depression, and elevation, CT and MRI scans were conducted on the second postoperative day to check for additional pathologies; however, no suggestions for neoplastic, inflammatory, cerebrovascular, or other diseases were found. Furthermore, the patient’s standard preoperative blood tests (for cell counts, inflammatory response, HbA1c and glucose, etc.), to determine if the patient was fit to undergo general anesthesia surgery, showed no abnormalities. After another consultation with the neurosurgeon and a review of the preoperative CT images, the superior orbital fissure on the injured side was found to be narrowed, concluding that the ophthalmoplegia was caused by SOFS (Fig. 2). Because CT images showed that the superior orbital fissure of the injured side became wider postoperatively, we decided against additional surgical treatment for dislocation of the skull base and, for treating SOFS, intravenous betamethasone injection 4 mg per day was started (Fig. 3). After 14 days of inpatient treatment with intravenous betamethasone injection, the patient was prescribed oral administration of hydrocortisone for 2 months as part of outpatient treatment. At 6 months postoperatively, his subjective symptoms had improved, and movements of both eyes and his perception were normal (Fig. 4). (See figure, Supplemental Digital Content 2, which shows the patient at 6 months postoperatively. http://links.lww.com/PRSGO/D215.)
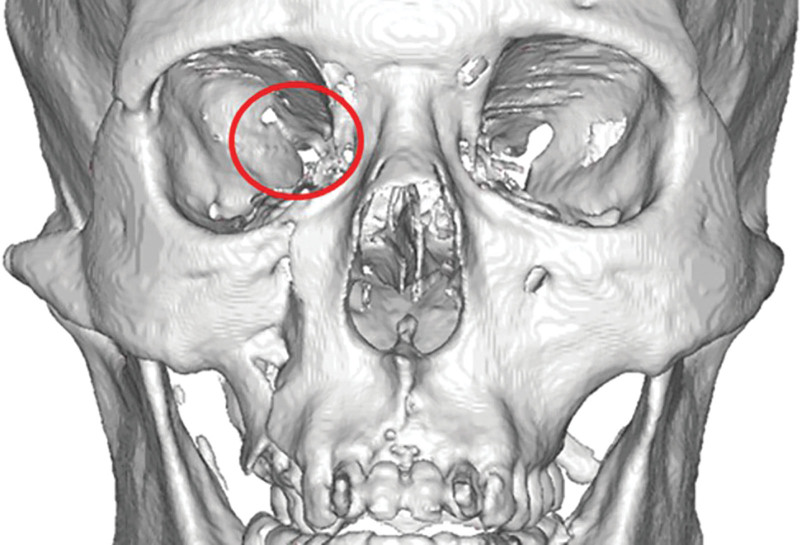
Fig. 2.
Preoperative 3D CT. The superior orbital fissure on the injured side was narrowed (red circle).
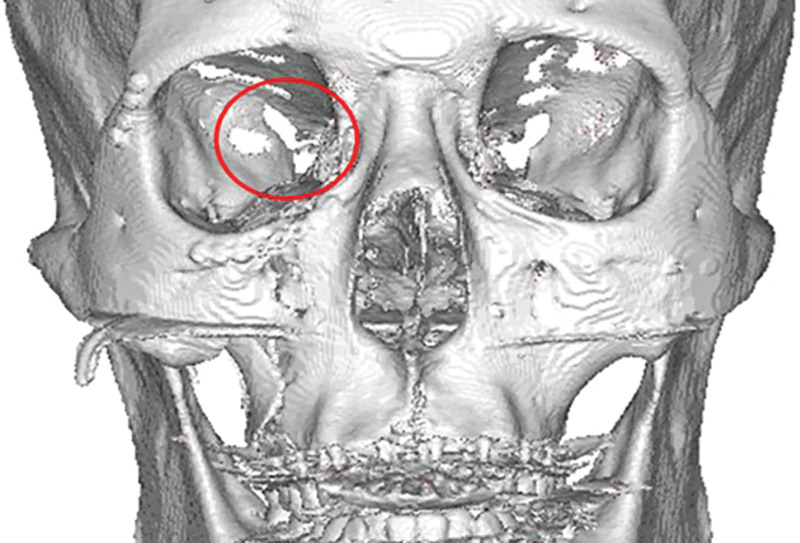
Fig. 3.
Postoperative 3D CT. The superior orbital fissure became wider postoperatively (red circle).
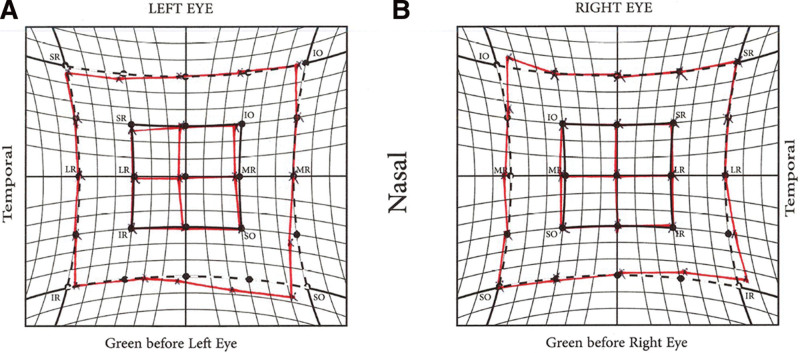
Fig. 4.
Hess chart examination at 6 months postoperatively. The Hess chart examination revealed no abnormalities. A, Left eye. B, Right eye.
DISCUSSION
The main causes of SOFS can be divided into traumatic and nontraumatic, with traumatic causes being (1) direct compression of nerves due to displacement of bone fragments associated with fractures or (2) secondary nerve damage due to increased internal pressure around the superior orbital fissure caused by hematoma, swelling, or other factors associated with trauma.1,5 Although there are no clear treatment guidelines for traumatic SOFS due to its infrequency, there are scattered reports describing various treatment modalities.1,5–10 Between them, surgery was shown beneficial for cases involving narrowing of the superior orbital fissure due to dislocation of bone fragments, with the note that this should be performed as early as possible.1,7 Steroid therapy, on the other hand, is mainly used to improve soft tissue swelling around the superior orbital fissure, and recently there have been many reports showing good results with megadose steroid therapy using an initial dose of approximately 30 mg per kg of methylprednisolone followed by continuous or intermittent high-dose steroid therapy for the first 2 or 3 days after injury.1,5,6,8
In the present case, the diagnosis of SOFS was delayed because there were no pupillary symptoms typically associated with oculomotor nerve palsy. Pupil-sparing oculomotor nerve palsy is conventionally linked with diabetic neuropathy, and then attributed to vascular vitrification and subsequent nerve ischemia; the herewith associated demyelination proceeds from the center of the oculomotor nerve, which receives its blood supply from the periphery, so pupillary symptoms are unlikely to occur.3,4 In our patient, we hypothesize that the displacement of the greater wing of the sphenoid bone caused physical stenosis and impaired venous return on the surface of the oculomotor nerve. Consequentially, blood flow stagnated, affecting primarily the central part of the oculomotor nerve, which may explain why, similar to in diabetic neuropathy, pupillary symptoms did not occur. Because it has been reported that, in traumatic SOFS cases, steroid treatment improves recovery from postinjury nerve damage, we postoperatively also provided steroid therapy, although at a lower dose than used in megadose steroid therapy because more than 2 weeks had passed since the injury.1,5,10
When performing the right zygomatic fracture reduction, inadvertently, the patient’s skull base also moved outward, improving the stenosis of the superior orbital fissure. However, we consider this a dangerous technique that could further aggravate the skull fracture because it is performed unintentionally. We believe that in skull base fractures with stenosis of the supraorbital fissure, a craniotomy procedure to the skull base is necessary to reposition the stenosis of the superior orbital fissure associated with the displacement of the bone fragments. On the other hand, when a zygomatic fracture is not accompanied by stenosis of the supraorbital fissure and an approach to the skull base is not necessary, dissection of the sphenozygomatic suture is indispensable for the selective reduction of only the zygomatic fracture. In the present case, the diagnosis of SOFS was delayed because the symptoms were not typical, but, in hindsight, it should have been diagnosed in the preoperative stage based on preoperative CT.
CONCLUSION
In cases of craniofacial fractures, even without pupillary symptoms, clinicians should remain aware of the possibility of supraorbital fissure syndrome.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 17 May 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Chen CT, Wang TY, Tsay PK, et al. Traumatic superior orbital fissure syndrome: assessment of cranial nerve recovery in 33 cases. Plast Reconstr Surg. 2010;126:205–212. [DOI] [PubMed] [Google Scholar]
- 2.Hirschfeld L. Epanchement de sang dans le sinus caverneux du cote gauche diagnostique pendant la vie [in French]. Compt Rend Soc Biol. 1858;5. [Google Scholar]
- 3.Asbury AK, Aldredge H, Hershberg R, et al. Oculomotor palsy in diabetes mellitus: a clinico-pathological study. Brain. 1970;93:555–566. [DOI] [PubMed] [Google Scholar]
- 4.Dreyfus PM, Hakim S, Adams RD. Diabetic ophthalmoplegia; report of case, with postmortem study and comments on vascular supply of human oculomotor nerve. AMA Arch Neurol Psychiatry. 1957;77:337–349. [PubMed] [Google Scholar]
- 5.Chen CT, Chen YR. Traumatic superior orbital fissure syndrome: current management. Craniomaxillofac Trauma Reconstr. 2010;3:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Acarturk S, Sekucoglu T, Kesiktas E. Mega dose corticosteroid treatment for traumatic superior orbital fissure and orbital apex syndromes. Ann Plast Surg. 2004;53:60–64. [DOI] [PubMed] [Google Scholar]
- 7.Bun RJ, Vissink A, Bos RR. Traumatic superior orbital fissure syndrome: report of two cases. J Oral Maxillofac Surg. 1996;54:758–761. [DOI] [PubMed] [Google Scholar]
- 8.Caldarelli C, Benech R, Iaquinta C. Superior orbital fissure syndrome in lateral orbital wall fracture: management and classification update. Craniomaxillofac Trauma Reconstr. 2016;9:277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Postma MP, Seldomridge GW, Vines FS. Superior orbital fissure syndrome and bilateral internal carotid pseudoaneurysms. J Oral Maxillofac Surg. 1990;48:503–508. [DOI] [PubMed] [Google Scholar]
- 10.Rohrich RJ, Hackney FL, Parikh RS. Superior orbital fissure syndrome: current management concepts. J Craniomaxillofac Trauma. 1995;1:44–48. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.