Abstract
Second-degree burn, the most common among burn degrees, underscores the importance of timely and proper treatment in influencing prognosis. Nutmeg (Myristica fragrans), renowned for its potent antibacterial and antifungal properties, also serves as an effective antiseptic for open wounds. The aim of this study was to identify the phytochemical constituents of nutmeg essential oil and analyze the wound healing effect of nutmeg cream on second-degree burns in an animal model. An experimental study with a completed randomized design was conducted on Rattus norvegicus strain Wistar rats with second-degree burn. This study had four groups and each group consisting of four rats: B (burn-treated base cream), B+N (burn-treated 3% nutmeg cream), B+SSD (burn-treated silver sulfadiazine (BSS)), and B+N+SSD (burn-treated 3% nutmeg cream and SSD in a 1:1 ratio). The phytochemical analysis of nutmeg essential oil was conducted by gas chromatography and mass spectroscopy (GC-MS). The burn diameter and burn wound healing percentage were measured from day 0 to 18. One-way ANOVA followed by post hoc analysis using the least significant difference (LSD) was employed to analysis the effect. The phytochemical analysis of nutmeg essential oil found that myristicin, terpinene-4-ol, terpinene, safrole and terpinolene were the most abundant putative compounds in nutmeg essential oil. On day 0, the average burn wound diameters were 1.4 cm in all groups and increases were observed in all groups on day 3. The wound diameter decreased until day 18 with the smallest burn wound diameter was found in the B+N group (0.86±0.37 cm), followed by B+SSD (0.93±0.29 cm). The B+SSD group exhibited the highest percentage of burn wound healing (56.80±14.05%), which was significantly different from the base cream (p<0.05). The percentage of burn wound healing in rats given 3% nutmeg cream was 41.88±13.81%, suggesting that nutmeg cream could promote burn wound healing in rats induced by second-degree burns.
Keywords: Burn, nutmeg, Myristica fragrans, wound healing, second-degree burn
Introduction
Burn is characterized by tissue damage from exposure to extreme temperatures in the form of heat, cold, electricity, chemicals, radiation, or friction on objects [1]. This damage is inflicted on the skin and underlying soft tissues, such as muscles, bones, blood vessels, and nerves, resulting in either temporary or permanent injuries [2]. The severity is categorized based on the depth the amount of tissue affected, these include first-degree (superficial) burns; second-degree (partial thickness) burns; third-degree (full-thickness) burns, and fourth-degree burns. Second-degree burns are further subcategorized into A (superficial partial) and B (deep partial) [3].
Approximately 90% of burn cases are concentrated in developing countries, particularly affecting low to middle-income communities [4]. Second-degree burns are the most prevalent among the other degrees of burns, emphasizing the crucial role of prompt and appropriate treatment in determining the prognosis [4]. While the gold standard in pharmacological burn management is the administration of silver sulfadiazine (SSD), its accessibility is often limited to urban centers, rendering the rural population reliant on traditional remedies for superficial burns [5,6].
Nutmeg (Myristica fragrans) is a traditional medicine recognized for its anti-inflammatory properties. Studies suggested that this medicinal plant has antimicrobial, antiseptic, and disinfectant effects, in addition to possessing antioxidant, analgesic, aphrodisiac, and stimulant properties [7,8]. Nutmeg has strong antibacterial and antifungal effects as well as its role as an antiseptic agent for open wounds [9]. The plant contains compounds such as monoterpene (sabinene, β-terpineol, p-menth-8-en-1-ol, and terpinene-4-ol), phenylpropene (eugenol, methyl eugenol, and myristicin), and sesquiterpene (germacrene D and β-bergamotene), which are associated as intermediaries to the biological activity [8,10]. The aim of this study was to identify the phytochemical constituents of nutmeg essential oils and analyze the wound healing effect of nutmeg cream on second-degree burns in an animal model.
Methods
Study design and study groups
An experimental study with a completed randomized design was conducted on Rattus norvegicus strain Wistar rats. The study used 3% nutmeg cream. Second-degree burns were induced in the rats and further divided into four groups: B (burn-treated base cream), B+N (burn-treated 3% nutmeg cream), B+SSD (burn-treated SSD), and B+N+SSD (burn-treated 3% nutmeg cream + SSD in a 1:1 ratio). The number of rats and repetitions in each group were determined using the degrees of freedom (DF) for the analysis of variance (ANOVA) formula [11], which yielded a minimum sample size of four rats for each group.
Plant material and extraction
One kilogram of nutmeg was obtained from South Aceh, Indonesia, for essential oil extraction involving steam distillation. Semiquantitative analysis of the nutmeg essential oil was conducted using gas chromatography and mass spectroscopy (GC-MS). The nutmeg essential oil was also made into a 3% cream which was tested in this study.
Gas chromatography and mass spectroscopy (GC-MS)
The phytochemical analysis of nutmeg essential oils by GC-MS was performed using the Shimadzu - QP2010 Ultra (Shimadzu Corporation, Kyoto, Japan). Details of the GC-MS method used in this study were available elsewhere [12].
Animal housing and husbandry
This study used healthy, male, Wistar strain white rats, aged between 12−16 weeks, with a weight of 200±20 grams. Rats were obtained from an animal supplier under the supervision of the Faculty of Veterinary Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia. They were housed in standard conditions, maintaining a constant room temperature and humidity at 25±1°C, with a 12-hour light-dark cycle. Rats had ad libitum access to food and water, and all procedures were conducted under veterinary supervision.
Base cream and nutmeg cream formulation
The base cream formulation included separating the oil phase (stearic acid, cetyl alcohol, and vaseline) and the water phase (distilled water, glycerin, and triethanolamine). Nutmeg cream formulation was then created using the oil-in-water process, incorporating essential oil in a concentration of 3%, resulting in a 3% nutmeg cream. The compositional details of the cream formulation, amounting to 100 grams, are presented in Table 1.
Table 1.
Cream formulations of 3% nutmeg cream and base cream used in the study
| Composition | Amount (g) | |
|---|---|---|
| 3% nutmeg cream | Base cream | |
| Stearic acid | 6 | 6 |
| Alcohol cetyl | 6 | 6 |
| Vaseline | 39 | 39 |
| Aquadest | 63.5 | 66.5 |
| Glycerin | 15 | 15 |
| Triethanolamine | 3 | 3 |
| Phenoxyethanol | 0.5 | 0.5 |
| Nutmeg essential oil | 3 | 0 |
Burn induction and body weight measurement
After the 7-day acclimatization period, the body weight of the rats was measured. Intramuscular ketamine (50 mg/kg) and xylazine (10 mg/kg) were administered for anesthesia. Subsequently, the back fur was shaved and cleaned with 70% ethanol swabs. A second-degree burn was induced by applying a heated circular iron metal (2 cm diameter) at 100°C on the back of rats for five seconds without pressure. The body weight of each rat was measured every 3 days starting from days 0, 3, 6, 9, 12, 15, and 18.
Nutmeg cream application
The tested substances (base cream, 3% nutmeg cream, SSD, and a combination of 3% nutmeg cream and SSD) were topically applied five minutes after the burn induction at a dose of 0.1 mg/mm burn diameter. The application was conducted twice daily (8 a.m. and 5 p.m.) for 18 days covering all burn areas.
Burn diameter measurement and burn wound healing percentage calculation
The assessment of burn diameter commenced on day 0, precisely five minutes after induction using calipers (in centimeters). Then burn diameter measurement was conducted every three days for a total of 18 days, in the morning prior to the application of the cream. Furthermore, the diameter was calculated in four quadrants (Figure 1) using the Morton method:
Figure 1.
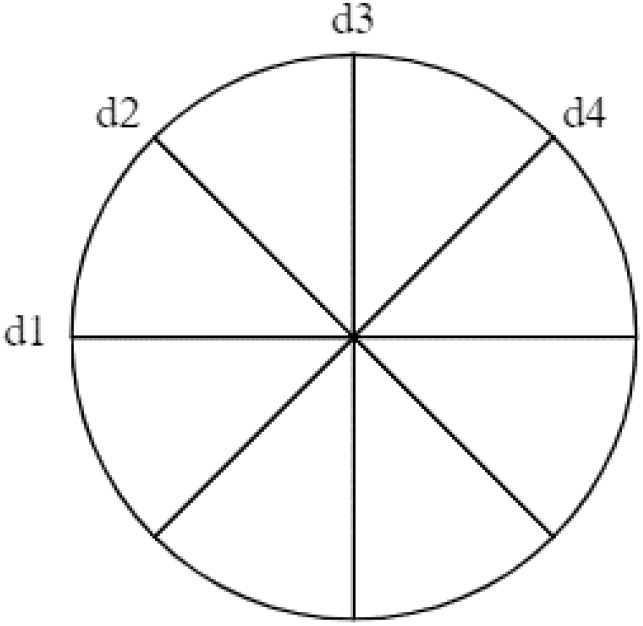
Method for measuring burn diameter with quadrants.
The burn wound healing percentage was calculated from the burn diameter on days 3 and 18 using formula:
Observation of macroscopic description
A macroscopic description of burns was observed on the rats for signs of inflammation, such as erythema, edema, presence of pus, and the formation of new skin tissue, on days 0, 3, and 18.
Statistical analysis
The data were analyzed using one-way ANOVA followed by post hoc analysis using the least significant difference (LSD) to determine the effects of 3% nutmeg cream. A p-value of <0.05 was considered statistically significant. All analysis was performed using the SPSS version 20.o (SPSS Inc., Chicago, USA).
Results
Gas chromatography-mass spectroscopy (GC-MS) of nutmeg essential oil
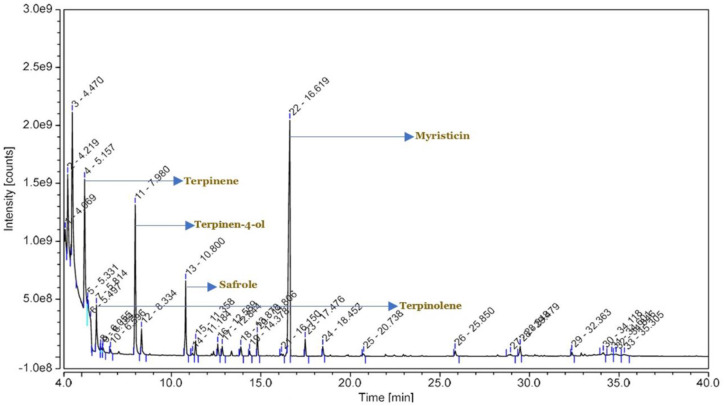
The semiquantitative analysis by GC-MS showed that nutmeg essential oils contained 18 putative compounds: terpinene, terpinolene, terpineol, terpinene-4-ol, iso-β-terpineol, safrole, eugenol, copaene, methyl eugenol, trans-isoeugenol, ß-bisabolene, myristicin, isoelemicin, methoxy eugenol, naphthalene, n-hexadecanoic acid, 13-octadecenoic acid, and heptadecadienyl furan (Figure 2 and Table 2). The most abundant putative compounds were myristicin (21.30%), terpinene-4-ol (13.57%), terpinene (12.13%), safrole (6.77%), and terpinolene (4.23%). It also contains eugenol compounds in the form of eugenol, methyl eugenol, trans isoeugenol, and methoxy eugenol, as much as 3.22% (Figure 2 and Table 2).
Figure 2.
Gas chromatography-mass spectroscopy (GC-MS) spectral of chemical compounds from nutmeg essential oil.
Table 2.
The compounds of nutmeg essential oil based on gas chromatography-mass spectroscopy (GC-MS)
| Retention time (minute) | Relative height (%) | Putative compound |
|---|---|---|
| 5.16 | 12.13 | Terpinene |
| 5.81 | 4.23 | Terpinolene |
| 6.60 | 0.40 | Terpineol |
| 7.98 | 13.57 | Terpinen-4-ol |
| 8.33 | 2.30 | iso-β-terpineol |
| 10.80 | 6.77 | Safrole |
| 12.59 | 1.07 | Eugenol |
| 12.84 | 0.89 | Copaene |
| 13.88 | 0.83 | Methyleugenol |
| 14.81 | 0.46 | trans-Isoeugenol |
| 16.15 | 0.22 | ß-Bisabolene |
| 16.62 | 21.30 | Myristicin |
| 17.48 | 1.56 | Isoelemicin |
| 18.45 | 0.86 | Methoxyeugenol |
| 20.74 | 0.27 | Naphthalene |
| 25.85 | 0.51 | n-Hexadecanoic acid |
| 28.95 | 0.20 | 13-Octadecenoic acid |
| 29.48 | 0.85 | Heptadecadienyl furan |
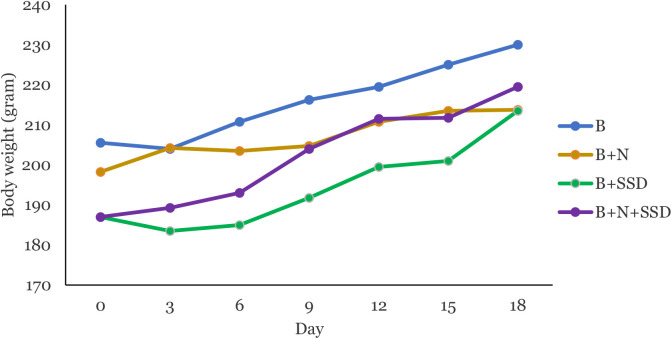
Body weight measurement
The body weight of each rat every three days is presented in Figure 3. No significant difference was observed in the rat’s body weight (p=0.158) on day 0, indicating a uniform body weight across all groups. By day 18, there was an increase in body weight with no significant difference (p=0.803) among the treatment groups (Figure 3).
Figure 3.
Comparison of body weight of rats between groups. B (burn group treated with base cream only); B+N (burn-treated with 3% nutmeg cream); B+SSD (burn-treated with silver sulfadiazine (SSD); and B+N+SSD (burn-treated with 3% nutmeg cream and SSD in a 1:1 ratio).
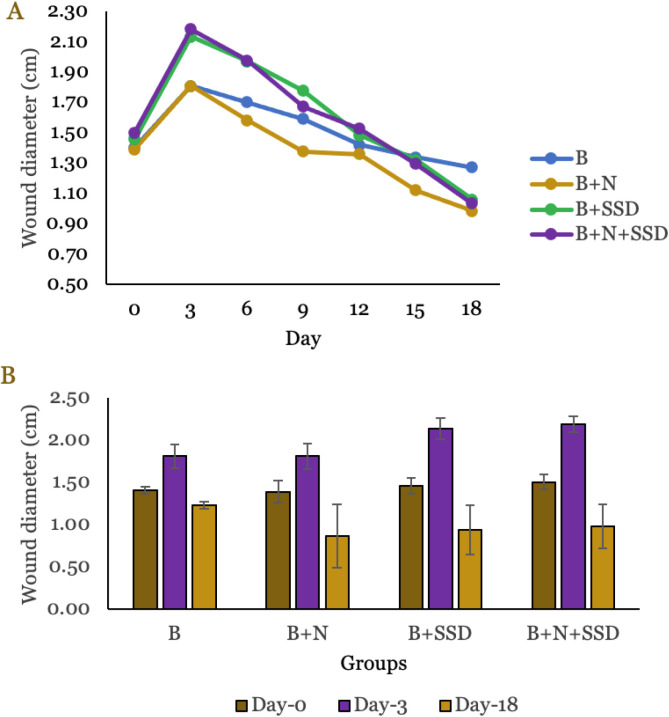
Effect of nutmeg cream on burn diameter
Across all treatment groups, there was a significant increase in diameter on day 3, followed by a gradual decrease until day 18. The largest increase in diameter observed on day 3 was the B+N+SSD group (2.18±0.09 cm). Meanwhile, the base cream and 3% nutmeg cream group had the smallest increase on day 3, measured at 1.81±0.14 cm and 1.81±0.15 cm, respectively. The largest diameter found on day 18 was in the base cream group (1.23±0.04 cm), while the other groups exhibited substantially lower diameters. The smallest diameters were observed in the 3% nutmeg cream group, which showed a decrease from 1.81±0.15 cm to 0.86±0.37 cm. Despite the decrease in all groups, there were no significant differences on day 18 (p=0.359). Figure 4A shows the change in burn wound diameter every three days. The specific data for days 0, 3, and 18 are visually presented in Figure 4B.
Figure 4.
Diameter of burn wound between groups. (A) Measured every 3 days, (B) Measured on day 0, 3, and 18. B (burn group treated with base cream only); B+N (burn-treated with 3% nutmeg cream); B+SSD (burn-treated with silver sulfadiazine (SSD); and B+N+SSD (burn-treated with 3% nutmeg cream and SSD in a 1:1 ratio).
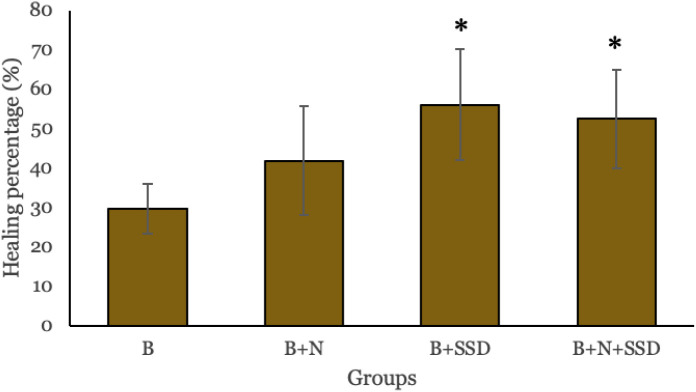
Effect of nutmeg cream on burn wound healing percentage
The highest healing percentage occurred in the B+SSD group (56%), which showed a significant difference compared to the base cream group (p=0.029). The B+N+SSD group demonstrated a healing percentage of 52%. The healing percentage of B+N group (41%) was not significantly different from B+SSD (p=0.312) (Figure 5).
Figure 5.
Healing percentage on day-18 between groups. Group with * indicates statistically significant at p<0.05 compared to B group. B (burn group treated with base cream only); B+N (burn-treated with 3% nutmeg cream); B+SSD (burn-treated with silver sulfadiazine (SSD); and B+N+SSD (burn-treated with 3% nutmeg cream and SSD in a 1:1 ratio).
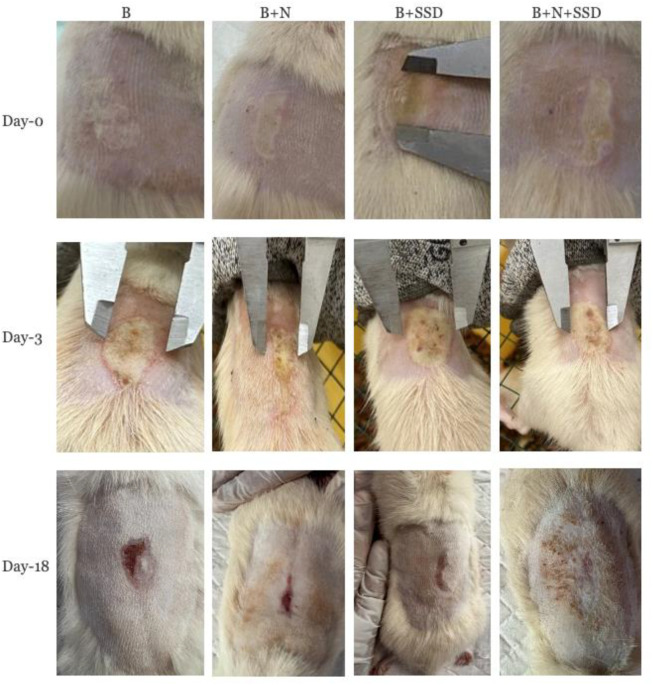
Macroscopic observation
On day 0, the burn manifested as a dense white area with a hard texture due to epidermal damage. Hyperemia was evident in the affected tissue area without the presence of bullae. By day 3, it increased along with an enlargement of the burn diameter. On day 18, a reduction in diameter was observed, accompanied by the emergence of new skin tissue. Healing conditions for each group on days 0, 3, and 18 were presented in Figure 6.
Figure 6.
Macroscopic observation of burn wound healing between groups. B (burn group treated with base cream only); B+N (burn-treated with 3% nutmeg cream); B+SSD (burn-treated with silver sulfadiazine (SSD); and B+N+SSD (burn-treated with 3% nutmeg cream and SSD in a 1:1 ratio).
Discussion
This study found that nutmeg essential oils contained several secondary metabolites, consisting of myristicin, safrole, terpinene, terpinen-4-ol, and terpinolene. Several studies have shown that the main compounds found in nutmeg essential oils are monoterpene compounds, constituting approximately 80% [8]. Other compounds identified in nutmeg essential oils are sabinene, pinene, limonene, linalool, phellandrene, safrole, thujene, and methyl eugenol [13,14]. Myristicin, identified prominently in nutmeg, exhibits anti-inflammatory properties through various pathways, including the inhibition of cytokines and mediators such as tumor necrosis factor-α (TNF-a) and nitric oxide, consequently suppressing the migration and proliferation of neutrophils and macrophages [15]. Terpenes, another compound investigated in nutmeg seed essential oil, have reported antimicrobial activities, primarily attributed to their disruption of bacterial cell membranes, protein synthesis, DNA replication, biofilm formation, and modulation of bacterial enzymes [16]. Furthermore, safrole has been associated with cytotoxic, analgesic, and antimicrobial properties in several studies [17]. Additionally, terpinen-4-ol has bactericidal effects against Staphylococcus aureus and Candida albicans, while terpineol has been recognized for its antioxidative properties [8-10].
Several wound models, such as incision, laser, dermatome, biopsies, and burn, were used to evaluate wound healing compounds [18,19]. This study adopted a previous study method to induce second-degree burns through the attachment of a round hot iron at 100°C for 5 seconds [20]. Rattus norvegicus, employed in this study’s animal model, was ideal for burn induction due to their physiological and pathological similarities to humans [21]. Although rats possess the main skin layers to humans, their skin exhibits higher elasticity and stronger adhesion due to underlying structures. This characteristic makes it challenging to distinguish between second-degree burns type A and B [18].
This study reported that SSD cream reduced the diameter of burn wound significantly compared to other groups. SSD is considered as the gold standard therapy for burns. SSD consists of silver nitrate and sodium sulfadiazine, acting as antimicrobial agents to inhibit bacterial growth and aid in the healing process, such as facilitating exudate absorption in burnt skin. Additionally, silver enhances the efficacy of sulfadiazine in suppressing the proliferation or colonization of diverse bacteria, fungi, and viruses. Sulfadiazine functions by inhibiting the synthesis of folic acid, thereby inhibiting enzymes crucial for cellular function and bacterial DNA denaturation [22].
The groups in this study had healing patterns consistent with the phases reported in previous studies [23]. Examination of the burn wound diameter on day 3 revealed an increase in diameter in all groups, suggesting the crucial role of the inflammatory phase in the initial stages of wound healing. Several studies have shown that nutmeg has antibacterial properties against Staphylococcus aureus and Escherichia coli, inhibiting bacterial growth during the inflammation phase [13,24]. This mechanism works by inhibiting the permeability of bacterial cell membranes and disrupting energy transduction towards the cytoplasmic membrane, thereby hindering bacterial motility and accelerating the resolution of the inflammation phase [25,26]. Therefore, the nutmeg cream was able to suppress the burn wound diameter on day 3. On day 18, the burn wound diameter in all groups decreased significantly with the formation of new skin tissues, demonstrating the onset of the proliferation and early remodeling phase. At this stage, antioxidant properties might modulate wound contraction and enhance the speed of epithelialization [27,28]. Nutmeg essential oils have reported to possess antioxidant properties, inhibit lipid peroxidation, and reduce metal ions [29].
Conclusion
The essential oil derived from nutmeg contains a variety of compounds, including myristicin, safrole, terpinene, terpinen-4-ol, and terpinolene. The application of nutmeg cream resulted in a reduction of burn wound diameter and promoted burn wound healing in the rats induced with second-degree burns. Further study with extended duration should be conducted to comprehensively assess all stages of wound healing, including inflammation, proliferation, and remodeling. Skin histopathological analyses can be carried out at various stages to provide valuable insights into the dynamics of wound healing.
Acknowledgments
The authors express their gratitude to the Directorate of Research and Community Services at Universitas Syiah Kuala, Indonesia, for their generous financial support.
Ethics approval
This study was approved by the Ethical Committee of the Faculty of Veterinary Medicine, Syiah Kuala University No. 25/KEPH/5/2023 on May 4, 2023.
Competing interests
All the authors declare that there are no conflicts of interest.
Funding
This research received a grant from the Directorate of Research and Community Services at Universitas Syiah Kuala, Indonesia, through the Penelitian Tesis Magister grant (Grant No. 454/ UN11.2.1/ PT.01.03/PNBP).
Underlying data
Derived data supporting the findings of this study are available from the corresponding author on request.
How to cite
Angilia C, Sary NL, Indah R, et al. Wound healing effect of nutmeg (Myristica fragrans) cream on second-degree burn in animal model. Narra J 2024; 4 (1): e621 - http://doi.org/10.52225/narra.v4i1.621.
References
- 1.Jeschke MG, van Baar ME, Choudhry MA, et al. Burn injury. Nat Rev Dis Primers 2020;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evers LH, Bhavsar D, Mailänder P.. The biology of burn injury. Exp Dermatol 2010;19:777–783. [DOI] [PubMed] [Google Scholar]
- 3.Markiewicz-Gospodarek A, Kozioł M, Tobiasz M, et al. Burn wound healing: Clinical complications, medical care, treatment, and dressing types: The current state of knowledge for clinical practice. Int J Environ Res Public Health 2022;19:1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yakupu A, Zhang J, Dong W, et al. The epidemiological characteristic and trends of burns globally. BMC Public Health 2022;22:1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ertaş B, Okuyan B, şen A, et al. The effect of Cotinus coggygria L. ethanol extract in the treatment of burn wounds. J Res Pharm 2022;26:554–564. [Google Scholar]
- 6.Vitale S, Colanero S, Placidi M, et al. Phytochemistry and biological activity of medicinal plants in wound healing: An overview of current research. Molecules 2022;27:3566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abourashed EA, El-Alfy AT. Chemical diversity and pharmacological significance of the secondary metabolites of nutmeg (Myristica fragrans Houtt.). Phytochem Rev 2016;15:1035–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ashokkumar K, Simal-Gandara J, Murugan M, et al. Nutmeg (Myristica fragrans Houtt.) essential oil: A review on its composition, biological, and pharmacological activities. Phytother Res 2022;36:2839–2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barman R, Bora PK, Saikia J, et al. Nutmegs and wild nutmegs: An update on ethnomedicines, phytochemicals, pharmacology, and toxicity of the Myristicaceae species. Phytother Res 2021;35:4632–4659. [DOI] [PubMed] [Google Scholar]
- 10.Ha MT, Vu NK, Tran TH, et al. Phytochemical and pharmacological properties of Myristica fragrans Houtt.: An updated review. Arch Pharm Res 2020;43:1067–92. [DOI] [PubMed] [Google Scholar]
- 11.Serdar CC, Cihan M, Yücel D, et al. Sample size, power and effect size revisited: Simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem Med (Zagreb) 2021;31:27–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qarani W, Husna F, Yulia W, et al. Antioxidant and antiaging activity of Cinnamomum burmannii and Michelia champaca extract and combinations. Narra J 2023;3:e111.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lemnaru (Popa) GM, Motelica L, Trusca RD, et al. Antimicrobial wound dressings based on bacterial cellulose and independently loaded with nutmeg and fir needle essential oils. Polymers (Basel: ) 2023;15:3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mickus R, Jančiukė G, Raškevičius V, et al. The effect of nutmeg essential oil constituents on Novikoff hepatoma cell viability and communication through Cx43 gap junctions. Biomed Pharmacother 2021;135:111229. [DOI] [PubMed] [Google Scholar]
- 15.Ramírez-Alarcón K, Martorell M, Gürer ES, et al. Myristicin: From its biological effects in traditional medicine in plants to preclinical studies and use as ecological remedy in plant protection. eFood 2023;4:e90. [Google Scholar]
- 16.Masyita A, Mustika Sari R, Dwi Astuti A, et al. Terpenes and terpenoids as main bioactive compounds of essential oils, their roles in human health and potential application as natural food preservatives. Food Chem X 2022;13:100217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eid AM, Hawash M.. Biological evaluation of Safrole oil and Safrole oil Nanoemulgel as antioxidant, antidiabetic, antibacterial, antifungal and anticancer. BMC Complement Med Ther 2021;21:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dorsett-Martin WA. Rat models of skin wound healing: A review. Wound Repair Regen 2004;12:591–599. [DOI] [PubMed] [Google Scholar]
- 19.Masson-Meyers DS, Andrade TAM, Caetano GF, et al. Experimental models and methods for cutaneous wound healing assessment. Int J Exp Pathol 2020;101:21–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khorasani G, Hosseinimehr SJ, Zamani P, et al. The effect of saffron (Crocus Sativus) extract for healing of second-degree burn wounds in rats. Keio J Med 2008;57:190–5. [DOI] [PubMed] [Google Scholar]
- 21.Abdullahi A, Amini-Nik S, Jeschke MG. Animal models in burn research. Cell Mol Life Sci 2014;71:3241–3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heyneman A, Hoeksema H, Vandekerckhove D, et al. The role of silver sulphadiazine in the conservative treatment of partial thickness burn wounds: A systematic review. Burns 2016;42:1377–1386. [DOI] [PubMed] [Google Scholar]
- 23.Rahman MS, Islam R, Rana MM, et al. Characterization of burn wound healing gel prepared from human amniotic membrane and Aloe vera extract. BMC Complement Altern Med 2019;19:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Członka S, Strąkowska A, Kairytė A, et al. Nutmeg filler as a natural compound for the production of polyurethane composite foams with antibacterial and anti-aging properties. Polym Test 2020;86:106479. [Google Scholar]
- 25.Ustuner O, Anlas C, Bakirel T, et al. In vitro evaluation of antioxidant, anti-inflammatory, antimicrobial and wound healing potential of Thymus sipyleus Boiss. subsp. Rosulans (Borbas) Jalas. Molecules 2019;24:3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaniad P, Tewtrakul S, Sudsai T, et al. Anti-inflammatory, wound healing and antioxidant potential of compounds from Dioscorea bulbifera L. bulbils. PLoS One 2020;15:e0243632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ullah S, Mansoor S, Ayub A, et al. An update on stem cells applications in burn wound healing. Tissue Cell 2021;72:101527. [DOI] [PubMed] [Google Scholar]
- 28.Shahouzehi B, Sepehri G, Sadeghiyan S, et al. Effect of Pistacia atlantica resin oil on anti-oxidant, hydroxyprolin and VEGF changes in experimentally-induced skin burn in rat. World J Plast Surg 2018;7:357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Šojić B, Tomović V, Kocić-Tanackov S, et al. Effect of nutmeg (Myristica fragrans) essential oil on the oxidative and microbial stability of cooked sausage during refrigerated storage. Food Control 2015;54:282–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Derived data supporting the findings of this study are available from the corresponding author on request.