Abstract
COVID-19 breakthrough infection (BTI) can occur despite vaccination. Using a multi-centre, prospective, observational Canadian cohort of people with HIV (PWH) receiving ≥2 COVID-19 vaccines, we compared the SARS-CoV-2 spike (S) and receptor-binding domain (RBD)-specific IgG levels 3 and 6 months post second dose, as well as 1 month post third dose, in PWH with and without BTI. BTI was defined as positivity based on self-report measures (data up to last study visit) or IgG data (up to 1 month post dose 3). The self-report measures were based on their symptoms and either a positive PCR or rapid antigen test. The analysis was restricted to persons without previous COVID-19 infection. Persons without BTI remained COVID-19-naïve until ≥3 months following the third dose. Of 289 participants, 92 developed BTI (31.5 infections per 100 person-years). The median days between last vaccination and BTI was 128 (IQR 67, 176), with the most cases occurring between the third and fourth dose (n = 59), corresponding to the Omicron wave. In analyses adjusted for age, sex, race, multimorbidity, hypertension, chronic kidney disease, diabetes and obesity, a lower IgG S/RBD (log10 BAU/mL) at 1 month post dose 3 was significantly associated with BTI, suggesting that a lower IgG level at this time point may predict BTI in this cohort of PWH.
Keywords: COVID-19 vaccination, SARS-CoV-2, HIV, breakthrough infection, immunogenicity, humoral immunity, immunosuppressed hosts
1. Introduction
HIV infection induces both humoral and cell-mediated immune defects, impacting the severity of respiratory infections, as well as vaccine-induced immune responses [1]. During the COVID-19 pandemic, people with HIV (PWH) had twice the risk of hospitalization compared to HIV-negative individuals [2], and large studies showed up to a threefold increased risk of COVID-19-related mortality in PWH [3,4,5,6,7]. The vulnerability of PWH to severe COVID-19 outcomes stems from a combination of risk factors including high rates of smoking, multimorbidity [8] and social determinants of health [9,10]. Importantly, the suboptimal immunogenicity to many common vaccines in PWH is well recognized and may be attributed, in part, to ongoing B cell dysfunction and ongoing immune activation, resulting in inappropriate responses to stimuli [11,12,13]. HIV infection, especially in the context of low CD4 T cell counts (<200 cells/mm3) and unsuppressed viral loads [14,15], may cause predisposition to poor immunogenicity to various vaccines such as influenza [16], pneumococcal [17,18], meningococcal [19] and hepatitis A [20,21,22] and B vaccines [23,24]. Additional vulnerabilities increase the risk of SARS-CoV-2 acquisition and symptomatic/severe COVID-19 in PWH, including multimorbidity and membership in socioeconomic or racialized groups disproportionately affected by COVID-19 [25]. As the majority of PWH enrolled in COVID-19 vaccine trials have had normal CD4 T cell counts (>500 cells/mm3) and few comorbidities [26,27], these immunogenicity results may not be generalizable to the wide spectrum of PWH who are followed in Canadian centres.
Despite advances in understanding the immunogenicity outcomes in PWH, there remains a paucity of data regarding COVID-19 breakthrough infection (BTI) in PWH. The objective of the current study was to compare the socioeconomic, clinical and vaccine immune response correlates of BTI following two and three doses of COVID-19 vaccines in a prospective Canadian cohort of PWH enrolled in a vaccine immunogenicity study (CTN 328). This knowledge could help to identify persons at risk for BTI and inform us on whether different vaccine strategies, such as additional vaccine boosters for certain individuals, may portend benefit.
2. Materials and Methods
The CTN 328 study was designed and implemented in 2020 to address the knowledge gaps regarding the COVID-19 vaccine responses in diverse PWH and HIV-negative participants over long time periods, when little information was available on the responses to third or booster vaccinations in PWH. It was also designed to describe the safety and tolerability of COVID-19 vaccines in PWH [28]. An exploratory objective was to determine whether subpopulations of PWH respond differently to COVID-19 vaccination [28]. The CTN 328 was a multi-centre, prospective, observational cohort study of PWH recruited from sites in Montreal, QC, Toronto, ON, Ottawa ON, and Vancouver, BC with the aim of comparing their COVID-19 vaccine-induced immune response with that of HIV-negative controls. The CTN 328 protocol was previously published [28] and later amended to accommodate third and fourth doses/boosters. Enrolment occurred from April to June 2021 in Vancouver and from June 2021 to January 2022 for the remaining sites [29,30]. The participants attended visits prior to and following the vaccine dosing for phlebotomy and questionnaire completion [29,30].
2.1. Ethics Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the McGill University Health Centre Research Ethics Board (REB) under protocol 2022-7857, the Ottawa Health Science Network REB under protocol 20210361-01H, the University Health Network REB under protocol 21-5504 and the University of British Columbia Providence Health Care and Simon Fraser University REBs under protocols #H21-01515 and #H21-00742. Written informed consent was obtained from all the participants.
2.2. Human Participants
The inclusion criteria for participation in the CTN 328 study were (must meet all criteria) (1) age ≥16 years; (2) living with HIV (for the PWH group); (3) planning on receiving a COVID-19 vaccine or has received no more than 2 doses at enrolment; (4) able to provide signed, informed consent; (5) able to attend study visits. The exclusion criteria included signs or symptoms of active COVID-19 at enrolment [28].
Subpopulations of PWH were prioritized for the study enrolment: (1) Older age (≥55 years) given its association with immunosenescence, comorbidities and reduced vaccine efficacy [31,32]; (2) Immune non-responders (CD4 T cell count < 350 cells/mm3, CD4/CD8 < 0.75 with an undetectable viral load for at least 6 months). Immune non-responders may be at risk of more adverse COVID-19-related outcomes than HIV immune responders [7,33]; (3) Multimorbidity (defined as having ≥2 comorbidities) given the association with worse COVID-19 outcomes with COVID-19 [34]; (4) An HIV-positive ‘stable’ or ‘reference’ group (undetectable HIV viral load for at least 6 months, CD4 T cell counts ≥ 350 cells/mm3 and a maximum of one comorbidity). The sites were encouraged to enrol PWH at risk of worse outcomes due to COVID-19 infection, such as the subpopulations described above [28,29], because at-risk participants had been excluded from many of the vaccine trials that had been reported. The current analysis was restricted to persons who received 2 or more vaccine doses
2.3. Study Visits
For the present analysis, we evaluated samples collected between 11 August 2021 and 20 April 2022 at 3 and 6 months after the 2nd dose and 1 month after the 3rd dose. Moderately to severely immunocompromised individuals in some provinces were given a 3rd dose [35] as part of the primary series. Of note, in the 3 provinces enrolling participants, PWH were not included in this group. In accordance with the Public Health Agency of Canada guidelines, the 3rd doses of the mRNA-1273 vaccine were 50 µg (vs. 100 µg 1st and 2nd doses) for those under 65 years [36,37], whereas the 3rd doses of the BNT162b2 vaccine were the same as for the 1st and 2nd doses (30 µg).
2.4. Sociodemographic Health and Clinical History
Sociodemographic and general health information were captured via participant self-reporting. The data were gathered from interviews and clinic chart reviews following written informed consent and included comorbidities, medications, body mass index and history and date of COVID-19 infection. COVID-19 infection was based on a positive PCR test and/or self-report with a rapid antigen test (RAT). With regards to HIV history, we extracted year of HIV diagnosis, nadir and most recent CD4 T cell counts and ART regimen [28,29]. We also collected contextual information related to risk factors, including working in an environment in close proximity to others, working in a hospital or healthcare facility, the number of individuals living in the participant’s household and the number of bedrooms and bathrooms in the household.
2.5. Definition of BTI and Clinical Evaluation for COVID-19 Infection
BTI was defined as positivity based on the self-reporting (data up to the last study visit) or IgG data (only available up to 1 month post dose 3). Thus, all the BTI after 1 month post dose 3 was based on self/site reporting. The self-reporting was based on symptoms and either a positive PCR or rapid antigen test. All participants who developed symptoms consistent with COVID-19 throughout the study were asked to go to their nearest testing centre for testing. Participants were asked to notify the study staff by telephone of the test result so that this could be recorded.
COVID-19-like symptoms were defined as a temperature >38.0 °C associated with any one or more of the following clinical symptoms: feverishness/chills; cough; tachypnea/dyspnea; wheezing/stridor; rhinorrhea; sore throat; myalgias; loss of smell or taste; diarrhea. Participants were asked to record the signs and symptoms of COVID-19-like illness daily until resolution. These signs and symptoms are outlined in Appendix A. Hospitalizations, as disclosed by the participant or clinic records, were recorded.
2.6. Sample Collection
At each visit, blood was collected to isolate serum and plasma [28,29].
2.7. Humoral Immunity (SARS-CoV-2 Binding Antibodies)
The levels of IgG targeting the SARS-CoV-2 spike trimer (S) protein, spike receptor-binding domain (RBD) and nucleocapsid (N) protein were measured using an automated high-throughput chemiluminescent ELISA [38,39]. Vaccine-induced immunity was distinguished by co-positivity with the S and RBD protein and infection-induced immunity by co-positivity with the S and N protein (signal-to-cutoff ratio ≥ 1.0) [38] This assay was selected since it has been used in other Canadian studies [40,41,42], enabling future comparison of the results across cohorts.
If someone was anti-N-seropositive but an infection was not self/site-reported, they were still included in the BTI group. However, the timing of infection was uncertain in this case, so the sample date for anti-N seropositivity was used as the infection date.
For those with anti-N seropositivity after dose 2 (without self-reported infection), they were only counted as having a BTI if they had a negative anti-N result after dose 2 prior to anti-N seropositivity. This way, we could be sure that the infection occurred after dose 2. We excluded cases that did not satisfy this criterion. The IgG antibody titres (binding antibody units (BAU)/mL) were generated using a conversion model (4-parameter log-logistic curve based on measurements from the WHO International Standard) [43].
2.8. Statistical Analysis
All the analyses were performed using Statistical Analysis System (SAS) software version 9.4 (SAS Institute, Cary, NC, USA). We examined the differences in the proportions of participants with BTI vs. without BTI between a stratified sub-population of interest (persons ≥ 55 years old, immune non-responders (CD4 < 350 cells/mm3, CD4/CD8 ratio < 0.75, UD VL) and the HIV reference population (CD4 ≥ 350 cells/mm3, UD VL and ≤1 comorbidity). We also examined the differences in the proportions of PWH developing BTI based on having received the ChAdOx1 vaccine as at least one of the first two vaccine doses and those who received mRNA vaccines for both doses. These comparisons were based on the Chi-square test or Fisher’s exact test as appropriate. Other continuous variables, such as age and CD4 count, were compared between groups using the Wilcoxon rank sum test. Descriptive statistics were used to determine number of days between the last vaccine dose and BTI. We also examined the difference in the IgG spike/RBD (log10 BAU/mL) levels at 3 and 6 months post dose 2 (±2 months) and 1 month post dose 3 (±2 weeks) in participants with vs. without BTI after these time points using the Wilcoxon rank sum test. Only IgG data prior to breakthrough infection were included. We further conducted logistic regression adjusted for age, sex, multimorbidity, hypertension, chronic kidney disease, diabetes and obesity to examine the effect of IgG spike/RBD on the odds of BTI. We did not adjust for vaccine type since it was believed that vaccine type would be too highly collinear with IgG to be included as an adjustment variable. No adjustment for multiple comparisons was made given the exploratory nature of the study. p values < 0.05 were considered statistically significant.
2.9. Data Availability
The data presented in this study may be made available upon written request to the corresponding author.
3. Results
3.1. Participant Characteristics Stratified by BTI
A total of 375 PWH were enrolled in the CTN 328 study, of whom 289 (77.1%) individuals were included in the current analysis. Thus, all BTI 1 month post dose 3 was based on self/site reporting. The self-reporting was based on symptoms and either a positive PCR or rapid antigen test. Of 289 participants, 92 (31.8%) developed BTI, equating to 31.5 infections per 100 person-years. Individuals were excluded if they had COVID-19-like symptoms and PCR-confirmed COVID-19 infection prior to their second vaccine dose (n = 44/375, 11.7%); if the timing of COVID-19 infection was unconfirmed (n = 25/375, 6.7%); if these infections were identified only using IgG data and it could not be confirmed that the infection occurred after dose 2; if they did not receive dose 2 or if they were lost to follow-up following dose 2 (n = 17/375, 4.5%). The median number (IQR) of days between last vaccination and BTI was 128 (67, 176), with most of the cases occurring after the third dose and before the fourth dose (n = 59).
The baseline characteristics for PWH with (n = 92) and without (n = 197) BTI are presented in Table 1 and Supplementary Table S1.
Table 1.
Participant characteristics stratified based on COVID-19 BTI.
| Variable | Participants without COVID-19 BTI (n = 197) | Participants with COVID-19 BTI (n = 92) | p |
|---|---|---|---|
| Age | 0.098 | ||
| Median (IQR) | 54.8 (45.1, 62.8) | 53.6 (39.7, 61.7) | |
| Range | (19.7, 81.6) | (24.3, 83.5) | |
| # Missing | 1 (0.5%) | 0 (0%) | |
| Sex, n (%) | 0.786 | ||
| Male | 150 (76.1) | 73 (79.3) | |
| Female | 45 (22.8) | 19 (20.7) | |
| Prefer to self-describe | 2 (1.0) | 0 (0.0) | |
| Self-declared race or ethnicity 1, n (%) | 0.125 | ||
| White | 118 (60.2) | 60 (65.9) | |
| Black | 38 (19.4) | 9 (9.9) | |
| Other | 40 (20.4) | 22 (24.2) | |
| Unknown | 1 | 1 | |
| Sub-population, n (%) | |||
| Age ≥ 55 years | 97/196 (49.5) | 39/92 (42.4) | 0.261 |
| Multimorbidity (≥2 comorbidities) | 56/191 (29.3) | 23/92 (25.0) | 0.448 |
| Immune non-responder 2 | 18/187 (9.6) | 7/85 (8.2) | 0.713 |
| HIV + stable/reference (CD4 ≥ 350, suppressed VL and ≤1 comorbidity) |
96/183 (52.5) | 48/85 (56.5) | 0.54 |
| Duration of HIV infection, years | 0.778 | ||
| Median (IQR) | 17.0 (8.0, 25.0) | 16.0 (7.0, 26.0) | |
| Range | (0.0, 38.0) | (0.0, 39.0) | |
| Missing/unknown | 19 (9.6%) | 3 (3.2%) | |
| Duration of HIV infection, years, n (%) | 0.963 | ||
| Unknown | 19 | 3 | |
| <10 | 50 (28.1) | 26 (29.2) | |
| 10–19 | 57 (32.0) | 29 (32.6) | |
| 20+ | 71 (39.9) | 34 (38.2) | |
| CD4 nadir (cells/mm3) | 0.161 | ||
| Median (IQR) | 220.0 (120.0, 400.0) | 293.0 (146.5, 427.0) | |
| Range | (1.0, 900.0) | (10.0, 900.0) | |
| Unknown | 72 (36.5%) | 32 (34.8%) | |
| CD4 nadir (cells/mm3), n (%) | 0.334 | ||
| <100 | 27 (21.6) | 7 (11.7) | |
| 100–199 | 25 (20.0) | 12 (20.0) | |
| 200–299 | 27 (21.6) | 12 (20.0) | |
| 300–399 | 14 (11.2) | 12 (20.0) | |
| ≥400 | 32 (25.6) | 17 (28.3) | |
| Unknown | 72 | 32 | |
| CD4 count (cells/mm3) | 0.409 | ||
| Median | 620.0 (422.0, 855.0) | 667.0 (446.0, 865.0) | |
| Range | (9.0, 1800.0) | (84.0, 1180.0) | |
| Missing | 11 (5.6%) | 9 (9.8%) | |
| CD4 count (cells/mm3), n (%) | 0.763 | ||
| <250 | 12 (6.5) | 6 (7.2) | |
| 250–349 | 15(8.1) | 3 (3.6) | |
| 350–499 | 38(20.4) | 18 (21.7) | |
| 500–999 | 100 (53.8) | 46 (55.4) | |
| ≥1000 | 21(11.3) | 10 (12.0) | |
| Unknown | 11 | 9 | |
| CD4/CD8 ratio | 0.048 | ||
| Median (IQR) | 0.80 (0.51, 1.15) | 0.90 (0.60, 1.33) | |
| Range | (0.00, 2.50) | (0.15, 2.40) | |
| Missing | 21 (10.7%) | 12 (13.0%) | |
| CD4/CD8 ratio ≥ 0.75, n (%) | 93/176 (52.8) | 51/80 (63.8) | 0.103 |
| Undetectable viral load for at least 6 months, n (%) | 177/195 (90.8) | 77/89 (86.5) | 0.279 |
| ART regimen, n (%) | 0.052 | ||
| NRTI-based regimen | 2 (1.0) | 1 (1.1) | |
| NNRTI-based regimen | 21 (10.7) | 3 (3.3) | |
| PI-based regimen | 6 (3.0) | 2 (2.2) | |
| INSTI-based regimen | 144 (73.1) | 68 (73.9) | |
| Other 3 | 20 (10.2) | 18 (19.6) | |
| None | 4 (2.0) | 0 (0.0) | |
| Paid or unpaid work in an environment where you work in close proximity to other people, n (%) | 59/193 (30.6) | 32/90 (35.6) | 0.403 |
| Working in hospital or healthcare facility, n (%) | 9/193 (4.7) | 3/90 (3.3) | 0.605 |
| Number of individuals (including participant) living in household, n (%) | 0.268 | ||
| 1 | 98 (51.9) | 39 (43.3) | |
| 2 | 68 (36.0) | 36 (40.0) | |
| 3 | 17 (9.0) | 8 (8.9) | |
| 4 or more | 6 (3.2) | 7 (7.8) | |
| Unknown | 8 | 2 | |
| Number of bedrooms in household per person, mean (SD) | 1.3 (0.7) | 1.1 (0.6) | 0.124 |
| Number of bathrooms in household per person, mean (SD) | 1.0 (0.5) | 1.0 (0.5) | 0.788 |
1 Multiple could be selected. 2 (CD4 < 350, CD4/CD8 < 0.75, suppressed VL). 3 Regimens containing combinations of the above and/or other drug classes (i.e., cell entry inhibitor). Comparisons were based on Chi-square test or Fisher’s exact test as appropriate. Other continuous variables, such as age and CD4 count, were compared between groups using Wilcoxon rank sum test.
An undetectable HIV viral load 6 months preceding enrolment was observed in PWH without vs. with BTI (91% vs. 87%, p = 0.279), respectively. Of the individuals with BTI, 4 individuals (2%) were not on ART, whereas all the individuals without BTI were on ART. In both groups, greater than two-thirds of the PWH were on integrase strand inhibitor regimens (73.1 vs. 73.9%), and the ART regimen did not significantly differ between groups (p = 0.052).
The most frequent comorbidities included obesity (20.4% vs. 20.7% without vs. with BTI, respectively, p = 0.961), dyslipidemia (15.5% vs. 12% without vs. with BTI, respectively, p = 0.420) and hypertension (16.1% vs. 8.7% without vs. with BTI, respectively, p = 0.091), but these did not differ significantly between those without and those with BTI (Supplementary Table S1). The participants with vs. without BTI did not differ in terms of their age, sex, ethnicity, duration of HIV, CD4 or nadir CD4 count or comorbidities. There were no significant differences in the proportions of participants with BTI vs. without BTI who were persons ≥ 55 years old, immune non-responders (CD4 < 350 cells/mm3, CD4/CD8 ratio < 0.75, UD VL) or in the HIV reference population (CD4 ≥ 350 cells/mm3, UD VL and ≤1 comorbidity).
3.2. Numbers and Types of Vaccines Received Stratified by BTI
The vast majority of the participants had received mRNA vaccines. In the current analysis, performed in September 2023, 83% of PWH without BTI and 89% with BTI had received at least two mRNA vaccines (either BNT162b2 and/or mRNA-1273). The types of vaccines received and the time interval between vaccine doses are shown in Table 2. More individuals with BTI had received ChAdOx1 vaccines, as one or both of the first two doses, than individuals who had received mRNA vaccines for both doses (p = 0.004).
Table 2.
Types of vaccines received and time interval between doses in PWH without vs. with BTI.
| Breakthrough Infection No |
Breakthrough Infection Yes |
p | |
|---|---|---|---|
| Types of COVID-19 vaccines received, doses 1 and 2, n (%) | 0.004 | ||
| mRNA–mRNA | 182 (89.7) | 71 (76.3) | |
| ChAdOx1–mRNA | 13 (6.4) | 9 (9.7) | |
| ChAdOx1–ChAdOx1 | 7 (3.4) | 12 (12.9) | |
| Janssen/Novavax | 1 (0.5) | 1 (1.1) | |
| Types of COVID-19 vaccines received, dose 3, n (%) | 0.929 | ||
| Unknown/received only 2 doses | 34 | 13 | |
| BNT162b2 | 67 (67/163, 41.1) | 32 (32/79, 40.5) | |
| mRNA-1273 | 96 (96/163, 58.9) | 47 (47/79, 59.5) | |
| Number of vaccine doses received at the time of BTI, n (%) | - | ||
| 2 | - | 25 (26.9) | |
| 3 | - | 59 (63.4) | |
| 4 | - | 9 (9.7) | |
| Number of days since last vaccine dose (IQR) | - | 127.5 (67, 176) | - |
| Number of days since second dose (for persons who develop BTI between second and third doses) (n = 25) | 168 (135, 182) | ||
| Number of days since third dose (for persons who develop BTI between third and fourth doses) (n = 59) | 108 (55, 167) | ||
| Follow-up time from dose 2 to study end or BTI, months (median, IQR) | 14.0 (11.5, 17.3) | 8.8 (6.1, 10.9) | <0.001 |
| Follow-up time from third dose (for those who did not have BTI prior to third dose) | 8.8 (6.1, 12.4) | 3.9 (1.9, 5.7) | <0.001 |
| Follow-up time from fourth dose (for those who did not have BTI prior to fourth dose) | 1.6 (1.0, 3.3) | 0.6 (0.3, 1.4) | 0.017 |
Comparisons were based on Chi-square test or Fisher’s exact test as appropriate. Other continuous variables, were compared between groups using Wilcoxon rank sum test.
3.3. SARS-CoV-2 Antibody Concentrations Stratified by BTI
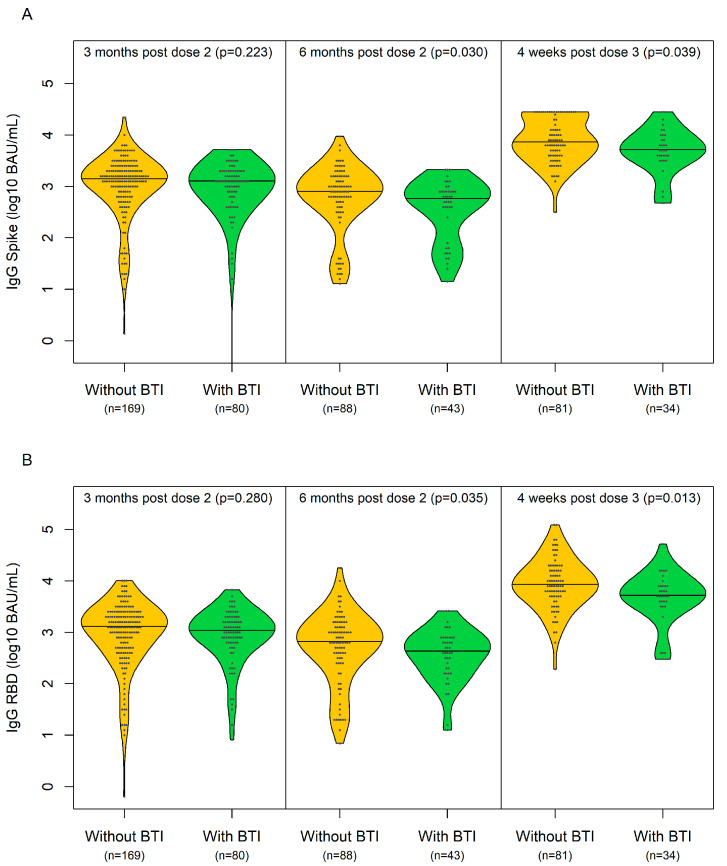
The median titres of IgG spike/RBD (log10 BAU/mL) at 3 months post dose 2 (±1 month), months post dose 2 (±2 months) and 1 month post dose 3 (±2 weeks) are depicted in Figure 1 and Table 3. Only serology data prior to breakthrough infection were included. In the analyses adjusted for age, sex, race, multimorbidity, hypertension, chronic kidney disease, diabetes and obesity, a lower IgG spike/RBD value (log10 BAU/mL) at 1 month post dose 3 was significantly associated with BTI in PWH.
Figure 1.
Median (IQR) IgG spike/RBD (log10 BAU/mL) at 3 months post dose 2 (±1 month), 6 months post dose 2 (±2 months) and 1 month post dose 3 (±2 weeks) in participants without (yellow) and with (green) breakthrough infection. (A) Median (IQR) IgG spike (log10 BAU/mL); (B) median (IQR) IgG RBD (log10 BAU/mL).
Table 3.
Adjusted odds ratio of breakthrough infection per log10 BAU/mL decrease in IgG.
| Time Point 1 | aOR (95% CI) 2 | Padj 3 | |
|---|---|---|---|
| 3 months post dose 2 (±1 month) | IgG spike | 1.21 (0.73, 1.99) | 0.464 |
| IgG RBD | 1.19 (0.74, 1.91) | 0.381 | |
| 6 months post dose 2 (±2 months) | IgG spike | 1.74 (0.95, 3.16) | 0.071 |
| IgG RBD | 1.71 (0.92, 3.19) | 0.092 | |
| 1 month post dose 3 (±2 weeks) | IgG spike | 2.83 (1.02, 7.87) | 0.046 |
| IgG RBD | 2.84 (1.13, 7.15) | 0.027 |
1 Only data prior to breakthrough infection were included. Participants who developed BTI prior to any of these time points were excluded from these time points. 2 Adjusted odds ratio of breakthrough infection per log10 BAU/mL decrease in IgG. 3 Logistic regression adjusted for age, sex, multimorbidity, hypertension, chronic kidney disease, diabetes and obesity was used to examine the effect of IgG spike/RBD on the odds of BTI.
3.4. Clinical Presentation of Participants with BTI
Most of the participants with BTI had mild symptoms (Table S2), encompassing fever, cough, sore throat, malaise, headache, muscle pain, nausea, vomiting, diarrhea and/or loss of taste/smell [44]. Shortness of breath was seen in 12 individuals (17.4%) with BTI for whom their symptoms were captured, suggesting that a nearly a fifth of individuals had moderate infection [44]. We did not capture data on abnormal chest imaging, which is also suggestive of moderate infection. Three participants were hospitalized (Table S3). We did not capture information that enabled us to differentiate between severe illness (SpO2 < 94% on room air, ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) < 300 mm Hg, a respiratory rate > 30 breaths/min or lung infiltrates > 50%) and critical illness (respiratory failure, septic shock and/or multiple organ dysfunction) [44]. None of the participants died.
4. Discussion
In this study, we examined BTI arising in a large cohort of PWH in Canada enrolled in a prospective observational study on COVID-19 vaccine immunogenicity. BTI occurred at a rate of 31.5 infections per 100 person-years in the PWH. Whereas other studies examining BTI in PWH have been conducted over the course of the pandemic, most of these studies have examined BTI based on HIV status (i.e., HIV-positive vs. HIV-negative). These studies yielded variable results. Furthermore, some studies have found that the severity of COVID-19 illness was similar between PWH and HIV-negative individuals [45,46,47,48], whereas other studies have found increased severity amongst PWH compared to HIV-negative persons [49,50,51,52,53]. One study which examined the risk of COVID-19 hospitalization in the pre-Omicron era found that PWH had about a two times greater risk of COVID-19 hospitalization than HIV-negative individuals in crude analyses, which was attenuated in propensity-score-weighted models [2]. This study found the risk differential could be explained by sociodemographic factors and history of comorbidity, underscoring the need to address the social and comorbid vulnerabilities (e.g., injecting drugs) that are more prominent among PWH [2]. The discrepancies across studies have been attributed to small sample sizes, a lack of HIV-negative control groups, the confounding inherent in observational studies or them having been conducted prior to the COVID-19 vaccine rollout. Moreover, finding an ideal control group remains a challenge for HIV studies since this group would, in theory, be individuals identical to the HIV-seropositive group in all aspects except for HIV status [54].
A study conducted by Coburn et al. combined electronic-health-record-based cohort data from integrated health systems and academic centres to examine PWH fully vaccinated prior to 30 June 2021 and HIV-negative individuals matched by date of full vaccination, age, race and ethnicity and sex. Among 113,994 patients (33,029 PWH and 80,965 HIV-negative controls) followed until 31 December 2021 [55], the risk of severe illness (defined as hospitalization within 28 days following SARS-CoV-2 BTI, with a primary or secondary COVID-19 discharge diagnosis) was low for both groups (6.8% of 3649 vaccinated PWH and HIV-negative individuals) and did not differ by HIV status overall [55]. BTI was 28% higher in the PWH than the HIV-negative persons (adjusted hazard ratio, 1.28 [95% CI, 1.19–1.37]) [55]. Most of the people with BTI were aged 55 or older (60%) and male (89%) [55]. In another study by Sun et al., cohort study data from the National COVID Cohort Collaborative (N3C), using a centralized electronic-medical-record-based repository of COVID-19 clinical data from academic medical centres across the US, were analyzed [56]. Amongst persons with HIV who had received a full vaccination series between December 2020 and September 2021, the IR of breakthrough infection was 7.1 (95% CI, 7.1–7.2) per 1000 person-months for people without immune dysfunction vs. 9.1 (95% CI, 8.8–9.4) per 1000 person-months for person with HIV infection [56]. Furthermore, HIV infection was independently associated with an increased BTI rate compared to persons without HIV or another form of immune compromise [56]. Importantly, the associations were independent of demographic characteristics, geographic region and comorbidity burden.
We found that the PWH who developed BTI were similar to the PWH who did not develop BTI with regards to age, sex, ethnicity, HIV duration, CD4 count and comorbidities. Although our study did not examine the severity of BTI, Coburn et al. found that severe breakthrough infection was 59% higher in the PWH with CD4 counts less than 350 cells/mm3 compared to the HIV-negative controls (aHR, 1.59; 95% CI, 0.99 to 2.46; p = 0.049) [55]. Furthermore, in multivariable analyses among PWH, Coburn et al. found that being female and older was associated with an increased risk of BTI. Other possible reasons for the differences between our study and the previously published study may relate to the types of individuals included in these studies and economic disparities. As regards vaccine type, we observed that the PWH who received ChAdOx1 vaccines as either one or two of their first two doses had significantly more BTIs than those who received mRNA vaccines for both doses. This finding has been observed in other studies [57]. mRNA vaccines are recognized for their ability to elicit strong immune responses compared to non-mRNA vaccines [58].
A very small number of participants in our study who developed BTI were hospitalized, and nobody died. These findings suggest that vaccination appeared to attenuate the disease severity in those acquiring infection. In the study by Coburn et al., mechanical ventilation and death were rare among PWH with BTI. When mechanical ventilation and death did occur, it was more likely in persons over 55 years of age with one or more comorbidity [55]. Although our study was not designed to assess the severity of COVID-19 infection amongst persons with BTI, these findings are nonetheless reassuring.
Interestingly, we found that PWH with BTI had a significantly lower median IgG spike/RBD level at 1 month post dose 3 than the participants without BTI. This observation suggests that lower IgG may predict BTI at this time point in this cohort. Although studies in both PWH and HIV-negative populations have tried to identify the protective antibody level against BTI, few have identified a specific cutoff [59].
In a systematic review of COVID-19 vaccine antibody responses in PWH which included studies from 1 January 2020 to 31 March 2022, Chun et al. reviewed 28 studies from 12 countries. Twenty-two (73%) studies reported high COVID-19 vaccine seroconversion rates in PWH, although PWH with lower baseline CD4 counts and CD4/CD8 ratios and higher baseline viral loads had lower seroconversion rates and antibody titres [60,61]. To date, there is still no consensus on what constitutes the best correlate of immune protection, and there are no disease-specific correlates of immune protection. In a large prospective longitudinal population-based study of COVID-19 in the general population, Vivaldi et al. observed correlations between vaccine-induced anti-spike antibody titres and protection against severe BTI [57]. Several studies have demonstrated that higher levels of neutralizing antibodies are associated with immune protection from symptomatic BTI infection following vaccination [62,63,64,65,66].
As IgG is involved in binding viruses, it makes intuitive sense there may be an association between lower IgG levels preceding BTI, although neutralizing antibody titres during the first months after vaccination may be better correlated with vaccine effectiveness [62,66] and have been predictive of the risk of BTI [62,65,67]. However, no specific antibody or neutralizing threshold titre has yet been identified that can predict the degree of protection, as it changes over time with waning or boosting. Moreover, it is worth underscoring that rates of BTI are a consequence of an individual’s level of immunity at a particular moment in time, the variant to which a person is exposed and the severity of the illnesses [67] BTI is influenced by, including their timing, frequency, severity and degree of infectiousness. BTI is important, as it is informative regarding the duration of restrictions in order to limit transmission and the need for additional booster doses or changes to dosing intervals [67].
SARS-CoV-2 vaccines have been designed to elicit immune responses—including the formation of antibodies against the outer spike protein of the Ancestral strain. However, SARS-CoV-2 variants, including Omicron, harbour mutations in the spike protein. Omicron harbours greater than 30 mutations in its virus’ spike protein, which attaches to cells, thereby increasing the chance of infection [68]. Moreover, Omicron and other variants are more transmissible than the Ancestral strain and are more able to evade antibody response, resulting in more BTIs [69]. Antibody waning, along with antigenic drift, limits the ability of long-term immunity to prevent reinfection. Furthermore, while earlier variants had a few mutation amino acids in their RBDs, Omicron harbours 15 RBD mutations—many in key antibody sites—preventing antibody binding. In addition, while earlier variants required both ACE2 and TMPRSS2 proteins to inject their genomes into a cell, Omicron bound only to ACE2. As many cells do not have TMPRSS2 on their exterior, if the virus does not need the surface protein, it has a wider number of potential target cells. Furthermore, unlike Delta, which had a subdued interferon response, Omicron activated interferon signaling [70]. Omicron infections tended to be less severe, but they were also associated with rises in cases and significant increases in hospitalizations and deaths. Therefore, Omicron and its subvariants quickly became dominant starting in late 2021, as they were more transmissible and also evaded antibodies more than prior variants. Consequently, there was an increase in BTIs [70,71,72].
Although this is not included in the current manuscript, more research needs to be dedicated to understanding the role of cell-mediated immunity and mucosal immunity in the nasal, oropharyngeal and pulmonary tissues in relation to protection against SARS-CoV-2 and other emerging viral infections [69,73,74,75,76]. In vaccinated HIV-negative individuals infected with SARS-CoV-2 during the Omicron wave, there were increased spike-specific responses during the infection of vaccinated compared to unvaccinated individuals [73]. Spike-specific clusters of CD4 T cells and plasmablasts expanded, and CD8 T cells were potently activated during the first week. In contrast, memory B cell activation, neutralizing antibody production and the primary responses to non-spike antigens occurred during the second week.
Given the importance of different arms of the immune system working synergistically, it is likely that the best correlate of protection will be a combination of measures. HIV induces a wide spectrum of immune abnormalities and is characterized by chronic low-grade inflammation despite ART Cell-mediated immunity [61,74,75,76,77,78,79] and antibody-dependent cell cytotoxicity merit examination, especially given the underlying propensity of HIV to infect and target CD4 T cells, which play a role in establishing vaccine memory, and to induce dysfunction in cytotoxic CD8 T cell response [80].
Measures of mucosal immunity should also be given greater attention given that this is the first site of immune defense. In HIV-negative individuals, it has been demonstrated that a local secretory component-associated IgA response is induced by COVID-19 mRNA vaccination that persists in some, but not all, individuals. The serum and saliva IgA responses were modestly correlated at 2–4 weeks post dose 2. Interestingly, the levels of anti-spike serum IgA (but not IgG) at this time point were lower in the participants who subsequently become infected with SARS-CoV-2 [81].
Our study has several limitations. An important limitation is the risk of misclassification bias. During many time periods during the pandemic, PCR tests were reserved for healthcare workers, hospitalized persons and residents in long-term care facilities. During other time periods, rapid antigen tests were in short supply in some regions. Therefore, participants may have had symptoms, but diagnostic testing may not have been easily accessible. Ascertainment of BTI was based on patient-initiated healthcare seeking, as opposed to being systematic. Thus, there may have been cases of asymptomatic BTI that were not captured. We acknowledge that relying on self-report and IgG data may introduce bias, as BTI in those vaccinated or who have had a prior infection may result in mild symptoms or even a lack of symptoms. Self-reporting can also impact representativeness and accuracy due to self-selection and recall biases. Moreover, there was a considerable overlap in the antibody levels between both those with and without BTI such that one cannot identify a threshold level of antibody that predicts protection. We did not determine the duration of BTI, nor the duration of post COVID chronic symptomatology. Furthermore, we did not report on the neutralization efficiency, as neutralization assays are still in progress at this time. The relative lack of information on disease severity is another limitation. This study was conducted in Canada, which has a well-developed healthcare system, and therefore its findings may not be generalizable to PWH in other countries. Even within Canada, the recruitment sites were large urban tertiary care clinics, and the participants may not necessarily be representative of other PWH in rural regions who differ in their access to healthcare, adherence to preventative behaviours and social determinants of health. Furthermore, our findings may not be generalizable to all the SARS-CoV-2 variants in circulation given that our study was conducted when the Alpha, Delta and Omicron variants were circulating. Given the timing of most of the BTIs in our study (between the third and fourth vaccine doses), most of the BTIs occurred when Omicron was circulating.
5. Conclusions
In summary, BTIs were more common in participants who received ChAdOx1 vaccines as the primary series. BTI was not associated with age or HIV-related factors. PWH with BTI following COVID-19 vaccination had lower median IgG Spike/RBD antibody levels 1 month post dose 3 than those who did not develop BTI at this point, suggesting that antibody levels at this time point may be a predictor of BTI in this cohort. However, given the large overlap in the IgG spike/RBD antibody levels between groups, this statement requires some caution in its interpretation. Ongoing evaluation is needed to determine the optimal correlates of immune protection and the durability of immune response in order to further inform vaccine guidelines and policies.
Acknowledgments
The authors thank the CTN staff who were involved in the planning and preparation of this study, in addition to the CTN Scientific Review Committee and the Community Advisory Board for their expedited review and helpful comments. They also thank all of the participants for their time and commitment. In addition, the authors thank the study coordinators and study nurses Florian Bobeuf, Claude Vertzagias, Lina Del Balso, Nathalie Paisible, Guillaume Theriault, Hansi Peiris, Lianne Thai, Rosemarie Clarke, Erin Collins, Nadia Ohene-Adu, Aron Dyks and Jill Jackson; the data manager Elisa Lau; the laboratory staff Tara Mabanga, Yulia Alexandrova, Ralph-Sydney Mboumba Bouassa, Erik Pavey and Stephanie Burke-Schinkel and the members of the University of Ottawa Serology and Diagnostics High-Throughput Facility, including Danielle Dewar-Darch, Justino Hernandez Soto, Abishek Xavier, Nicholas Bradette, Klaudia Baumann, Gwendoline Ward and Yuchu Dou. The authors also thank the physicians who assisted with recruitment. The COVID-19 antigens as well as the anti-hIgG#5-HRP fusion antibody were generously provided by Yves Durocher, the National Research Council of Canada (NRC), Montreal. C.T.C. is supported by a Fonds de recherche du Québec-Santé (FRQS) Junior 2 career award. A.B. holds a Canada Research Chair Tier 2 Canada Research Chair (CRC) position in sexually transmitted infection (STI) prevention. MAL holds a CRC position, Tier 2, in human immunovirology. M.A.J. holds a CRC position, Tier 2, in human immunovirology. S.W. is supported by a Research Chair position in HIV Clinical Care and Aging with the Ontario HIV Treatment Network. D.T. is supported by a Tier 2 CRC position in HIV Prevention and STI Research. M.A.B. holds a Canada Research Chair position, Tier 2, in viral pathogenesis and immunity. Z.L.B. holds a Scholar Award from Michael Smith Health Research BC. BL is supported by a career award LE 250 from the Quebec Ministry of Health for researchers in family medicine and an FRQS Junior 2 career award and holds a Canadian Institutes of Health Research Strategy for Patient-Oriented Research (SPOR) Mentoring Chair position in Innovative Clinical Trials. J.P.R. holds a Lowenstein Chair role in Hematology. Y.G. is supported by a Charles Best and Frederick Banting (CGS Doctoral) award from the CIHR (476885).
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/vaccines12050447/s1, Table S1: Participant characteristics stratified based on COVID-19 BTI; Table S2: COVID-19 symptoms based on presence or absence of BTI for participants self-reporting BTI; Table S3: Characteristics of the three participants with BTI who were hospitalized due to COVID-19.
Appendix A
Table A1.
Study period COVID-19 symptom questionnaire. Have you experienced any of the following COVID-19 signs or symptoms?
| Sign | Yes | No | If Yes, Provide Date/Time |
|---|---|---|---|
| Fever, chills | |||
| Cough | |||
| Shortness of breath | |||
| Acute loss of smell or taste | |||
| Fatigue | |||
| Headache | |||
| Muscle aches | |||
| Nausea/vomiting/diarrhea | |||
| General weakness | |||
| Nasal congestion | |||
| Sore throat |
Author Contributions
Conceptualization, C.T.C., C.L.C. and A.H.A.; data curation: T.L., J.S., Y.G. and C.A.; formal analysis: T.L., J.S., Y.G., C.A. and M.-A.J.; funding acquisition: C.T.C., J.S., M.-A.L., J.N., A.N.B., H.S., C.C., S.W., M.O. and A.H.A.; investigation: C.T.C., T.L., J.S., Y.G., C.A., M.-A.J., J.N., M.-A.J., A.N.B., H.S., C.C., S.W., M.O., C.K., D.H.S.T. and C.L.C.; methodology: C.T.C., J.S., T.L., Y.G., C.A., M.-A.L., J.N., M.-A.J., M.A.B., H.S., C.C., S.W., M.O., C.K., D.H.S.T., M.H. (Marianne Harris), M.H. (Mark Hull), Z.L.B., H.R.L., M.A.B., S.M., E.M., S.S., B.L., J.B.A., J.-P.R., C.L.C. and A.H.A.; project administration: C.T.C., Y.G., C.A., J.N., M.-A.J., A.N.B., H.S., S.W., M.O., C.K., D.H.S.T., M.H. (Marianne Harris), M.H. (Mark Hull), Z.L.B., H.R.L., M.A.B., S.M., E.M., S.S., J.B.A., J.-P.R., C.L.C. and A.H.A.; resources: M.-A.L., M.-A.J., Z.L.B. and A.H.A.; software: T.L.; supervision: C.T.C., J.S., T.L., C.A., M.-A.L., J.N., M.-A.J., M.A.B., H.S., S.W., M.H. (Marianne Harris), M.H. (Mark Hull), Z.L.B., H.R.L., M.A.B.,S.S., J.B.A., C.L.C. and A.H.A.; validation: T.L., Y.G. and C.A.; visualization: C.T.C., T.L., J.S., Y.G., C.A., M.-A.L., J.N., A.N.B. and H.S.; writing—original: C.T.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the McGill University Health Centre Research Ethics Board (REB) (#2022-7857), Ottawa Health Science Network REB (#20210361-01H), University Health Network REB (#21-5504) and the University of British Columbia Providence Health Care and Simon Fraser University REB s(#H21-01515, #H21-00742)).
Informed Consent Statement
Informed consent was obtained from all the participants of the study.
Data Availability Statement
The data presented in this study may be made available upon written request to the corresponding author. Researchers wishing to access the CITF core data elements can submit an application to the CITF Data Access Committee.
Conflicts of Interest
The authors declare no conflicts of interest. The CITF had no role in the design of the study; in the collection, analyses or interpretation of the data; in the writing of the manuscript or in the decision to publish the results.
Funding Statement
This research was supported by funding from the Public Health Agency of Canada, through the Vaccine Surveillance Reference group and the COVID-19 Immunity Task Force (grant number: 2122-HQ-000075) and the CTN (grant number: N/A). The production of the COVID-19 reagents was financially supported by NRC’s Pandemic Response Challenge Program.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Beck J.M., Rosen M.J., Peavy H.H. Pulmonary complications of HIV infection. Report of the Fourth NHLBI Workshop. Am. J. Respir. Crit. Care Med. 2001;164:2120–2126. doi: 10.1164/ajrccm.164.11.2102047. [DOI] [PubMed] [Google Scholar]
- 2.Puyat J.H., Fowokan A., Wilton J., Janjua N.Z., Wong J., Grennan T., Chambers C., Kroch A., Costiniuk C.T., Cooper C.L., et al. Risk of COVID-19 hospitalization in people living with HIV and HIV-negative individuals and the role of COVID-19 vaccination: A retrospective cohort study. Int. J. Infect. Dis. 2023;135:49–56. doi: 10.1016/j.ijid.2023.06.026. [DOI] [PubMed] [Google Scholar]
- 3.Davies M.A. HIV and risk of COVID-19 death: A population cohort study from the Western Cape Province, South Africa. medRxiv. 2020 doi: 10.1101/2020.07.02.20145185. [DOI] [Google Scholar]
- 4.Geretti A.M., Stockdale A.J., Kelly S.H., Cevik M., Collins S., Waters L., Villa G., Docherty A., Harrison E.M., Turtle L., et al. Outcomes of COVID-19 related hospitalization among people with HIV in the ISARIC WHO Clinical Characterization Protocol (UK): A prospective observational study. Clin. Infect. Dis. 2020;73:e2095–e2106. doi: 10.1093/cid/ciaa1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D., Inglesby P., et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vizcarra P., Perez-Elias M.J., Quereda C., Moreno A., Vivancos M.J., Dronda F., Casado J.L., Team C.-I. Description of COVID-19 in HIV-infected individuals: A single-centre, prospective cohort. Lancet HIV. 2020;7:e554–e564. doi: 10.1016/S2352-3018(20)30164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Augello M., Bono V., Rovito R., Tincati C., Marchetti G. Immunologic Interplay Between HIV/AIDS and COVID-19: Adding Fuel to the Flames? Curr. HIV/AIDS Rep. 2023;20:51–75. doi: 10.1007/s11904-023-00647-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong C., Gange S.J., Moore R.D., Justice A.C., Buchacz K., Abraham A.G., Rebeiro P.F., Koethe J.R., Martin J.N., Horberg M.A., et al. Multimorbidity Among Persons Living with Human Immunodeficiency Virus in the United States. Clin. Infect. Dis. 2018;66:1230–1238. doi: 10.1093/cid/cix998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fehr D., Lebouche B., Ruppenthal L., Brownc M., Obasc N., Bourbonniere E., Girouard J., Massicotte A., Jenabian M.A., Almomen A.A., et al. Characterization of people living with HIV in a Montreal-based tertiary care center with COVID-19 during the first wave of the pandemic. AIDS Care. 2022;34:663–669. doi: 10.1080/09540121.2021.1904500. [DOI] [PubMed] [Google Scholar]
- 10.Almomen A., Cox J., Lebouche B., Cheng M.P., Frenette C., Routy J.P., Costiniuk C.T. Short Communication: Ongoing Impact of the Social Determinants of Health During the Second and Third Waves of the COVID-19 Pandemic in People Living with HIV Receiving Care in a Montreal-Based Tertiary Care Center. AIDS Res. Hum. Retroviruses. 2022;38:359–362. doi: 10.1089/aid.2021.0186. [DOI] [PubMed] [Google Scholar]
- 11.Lane H.C., Masur H., Edgar L.C., Whalen G., Rook A.H., Fauci A.S. Abnormalities of B-cell activation and immunoregulation in patients with the acquired immunodeficiency syndrome. N. Engl. J. Med. 1983;309:453–458. doi: 10.1056/NEJM198308253090803. [DOI] [PubMed] [Google Scholar]
- 12.Cobos Jimenez V., Wit F.W., Joerink M., Maurer I., Harskamp A.M., Schouten J., Prins M., van Leeuwen E.M., Booiman T., Deeks S.G., et al. T-Cell Activation Independently Associates with Immune Senescence in HIV-Infected Recipients of Long-term Antiretroviral Treatment. J. Infect. Dis. 2016;214:216–225. doi: 10.1093/infdis/jiw146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Austin J.W., Buckner C.M., Kardava L., Wang W., Zhang X., Melson V.A., Swanson R.G., Martins A.J., Zhou J.Q., Hoehn K.B., et al. Overexpression of T-bet in HIV infection is associated with accumulation of B cells outside germinal centers and poor affinity maturation. Sci. Transl. Med. 2019;11:eaax0904. doi: 10.1126/scitranslmed.aax0904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amoah S., Mishina M., Praphasiri P., Cao W., Kim J.H., Liepkalns J.S., Guo Z., Carney P.J., Chang J.C., Fernandez S., et al. Standard-Dose Intradermal Influenza Vaccine Elicits Cellular Immune Responses Similar to Those of Intramuscular Vaccine in Men with and Those without HIV Infection. J. Infect. Dis. 2019;220:743–751. doi: 10.1093/infdis/jiz205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kroon F.P., van Dissel J.T., de Jong J.C., Zwinderman K., van Furth R. Antibody response after influenza vaccination in HIV-infected individuals: A consecutive 3-year study. Vaccine. 2000;18:3040–3049. doi: 10.1016/S0264-410X(00)00079-7. [DOI] [PubMed] [Google Scholar]
- 16.Klein M.B., Lu Y., DelBalso L., Cote S., Boivin G. Influenzavirus infection is a primary cause of febrile respiratory illness in HIV-infected adults, despite vaccination. Clin. Infect. Dis. 2007;45:234–240. doi: 10.1086/518986. [DOI] [PubMed] [Google Scholar]
- 17.French N., Gordon S.B., Mwalukomo T., White S.A., Mwafulirwa G., Longwe H., Mwaiponya M., Zijlstra E.E., Molyneux M.E., Gilks C.F. A trial of a 7-valent pneumococcal conjugate vaccine in HIV-infected adults. N. Engl. J. Med. 2010;362:812–822. doi: 10.1056/NEJMoa0903029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glaser J.B., Volpe S., Aguirre A., Simpkins H., Schiffman G. Zidovudine improves response to pneumococcal vaccine among persons with AIDS and AIDS-related complex. J. Infect. Dis. 1991;164:761–764. doi: 10.1093/infdis/164.4.761. [DOI] [PubMed] [Google Scholar]
- 19.MacNeil J.R., Rubin L.G., Patton M., Ortega-Sanchez I.R., Martin S.W. Recommendations for Use of Meningococcal Conjugate Vaccines in HIV-Infected Persons—Advisory Committee on Immunization Practices, 2016. MMWR Morb. Mortal. Wkly. Rep. 2016;65:1189–1194. doi: 10.15585/mmwr.mm6543a3. [DOI] [PubMed] [Google Scholar]
- 20.Wallace M.R., Brandt C.J., Earhart K.C., Kuter B.J., Grosso A.D., Lakkis H., Tasker S.A. Safety and immunogenicity of an inactivated hepatitis A vaccine among HIV-infected subjects. Clin. Infect. Dis. 2004;39:1207–1213. doi: 10.1086/424666. [DOI] [PubMed] [Google Scholar]
- 21.Crum-Cianflone N.F., Wilkins K., Lee A.W., Grosso A., Landrum M.L., Weintrob A., Ganesan A., Maguire J., Klopfer S., Brandt C., et al. Long-term durability of immune responses after hepatitis A vaccination among HIV-infected adults. J. Infect. Dis. 2011;203:1815–1823. doi: 10.1093/infdis/jir180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kemper C.A., Haubrich R., Frank I., Dubin G., Buscarino C., McCutchan J.A., Deresinski S.C., California Collaborative Treatment G. Safety and immunogenicity of hepatitis A vaccine in human immunodeficiency virus-infected patients: A double-blind, randomized, placebo-controlled trial. J. Infect. Dis. 2003;187:1327–1331. doi: 10.1086/374562. [DOI] [PubMed] [Google Scholar]
- 23.Overton E.T., Sungkanuparph S., Powderly W.G., Seyfried W., Groger R.K., Aberg J.A. Undetectable plasma HIV RNA load predicts success after hepatitis B vaccination in HIV-infected persons. Clin. Infect. Dis. 2005;41:1045–1048. doi: 10.1086/433180. [DOI] [PubMed] [Google Scholar]
- 24.El Chaer F., El Sahly H.M. Vaccination in the Adult Patient Infected with HIV: A Review of Vaccine Efficacy and Immunogenicity. Am. J. Med. 2019;132:437–446. doi: 10.1016/j.amjmed.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 25.Weiser J.K., Tie Y., Beer L., Neblett Fanfair R., Shouse R.L. Racial/Ethnic and Income Disparities in the Prevalence of Comorbidities that Are Associated with Risk for Severe COVID-19 Among Adults Receiving HIV Care, United States, 2014-2019. J. Acquir. Immune Defic. Syndr. 2021;86:297–304. doi: 10.1097/QAI.0000000000002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramasamy M.N., Minassian A.M., Ewer K.J., Flaxman A.L., Folegatti P.M., Owens D.R., Voysey M., Aley P.K., Angus B., Babbage G., et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): A single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396:1979–1993. doi: 10.1016/S0140-6736(20)32466-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.COVID-19 Vaccine (ChAdOx1 nCoV-19) Trial in South African Adults with and without HIV-Infection. [(accessed on 6 May 2021)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04444674?cond=HIV+and+COVID&draw=4.
- 28.Costiniuk C.T., Singer J., Langlois M.A., Kulic I., Needham J., Burchell A., Jenabian M.A., Walmsley S., Ostrowski M., Kovacs C., et al. CTN 328: Immunogenicity outcomes in people living with HIV in Canada following vaccination for COVID-19 (HIV-COV): Protocol for an observational cohort study. BMJ Open. 2021;11:e054208. doi: 10.1136/bmjopen-2021-054208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costiniuk C.T., Singer J., Lee T., Langlois M.A., Arnold C., Galipeau Y., Needham J., Kulic I., Jenabian M.A., Burchell A.N., et al. COVID-19 vaccine immunogenicity in people with HIV. AIDS. 2023;37:F1–F10. doi: 10.1097/QAD.0000000000003429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Costiniuk C.T., Singer J., Lee T., Galipeau Y., McCluskie P.S., Arnold C., Langlois M.A., Needham J., Jenabian M.A., Burchell A.N., et al. Antibody neutralization capacity after coronavirus disease 2019 vaccination in people with HIV in Canada. AIDS. 2023;37:F25–F35. doi: 10.1097/QAD.0000000000003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pereira B., Xu X.N., Akbar A.N. Targeting Inflammation and Immunosenescence to Improve Vaccine Responses in the Elderly. Front. Immunol. 2020;11:583019. doi: 10.3389/fimmu.2020.583019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wagner A., Garner-Spitzer E., Jasinska J., Kollaritsch H., Stiasny K., Kundi M., Wiedermann U. Age-related differences in humoral and cellular immune responses after primary immunisation: Indications for stratified vaccination schedules. Sci. Rep. 2018;8:9825. doi: 10.1038/s41598-018-28111-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Braunstein S.L., Wahnich A., Lazar R. COVID-19 Outcomes Among People with HIV and COVID-19 in New York City. J. Infect. Dis. 2023;228:1571–1582. doi: 10.1093/infdis/jiad311. [DOI] [PubMed] [Google Scholar]
- 34.Gallant J., Hsue P.Y., Shreay S., Meyer N. Comorbidities Among US Patients with Prevalent HIV Infection-A Trend Analysis. J. Infect. Dis. 2017;216:1525–1533. doi: 10.1093/infdis/jix518. [DOI] [PubMed] [Google Scholar]
- 35.Public Health Agency of Canada 2022. [(accessed on 31 May 2022)]. Available online: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-26-covid-19-vaccine.html.
- 36.Public Health Agency of Canada. [(accessed on 15 February 2022)]. Available online: https://www.canada.ca/en/health-canada/news/2021/11/health-canada-authorizes-the-use-of-the-moderna-spikevax-covid-19-vaccine-as-a-booster-shot.html.
- 37.Ministry of Health COVID-19 Vaccine Booster Recommendation. [(accessed on 22 July 2022)]; Available online: https://www.ontario.ca/page/covid-19-vaccines#:~:text=If%20you%20are%20at%20increased,available%20closer%20to%20fall%202024.
- 38.Cholette F., Fabia R., Harris A., Ellis H., Cachero K., Schroeder L., Mesa C., Lacap P., Arnold C., Galipeau Y., et al. Comparative performance data for multiplex SARS-CoV-2 serological assays from a large panel of dried blood spot specimens. Heliyon. 2022;8:e10270. doi: 10.1016/j.heliyon.2022.e10270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colwill K., Galipeau Y., Stuible M., Gervais C., Arnold C., Rathod B., Abe K.T., Wang J.H., Pasculescu A., Maltseva M., et al. A scalable serology solution for profiling humoral immune responses to SARS-CoV-2 infection and vaccination. Clin. Transl. Immunol. 2022;11:e1380. doi: 10.1002/cti2.1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Collins E., Galipeau Y., Arnold C., Bosveld C., Heiskanen A., Keeshan A., Nakka K., Shir-Mohammadi K., St-Denis-Bissonnette F., Tamblyn L., et al. Cohort profile: Stop the Spread Ottawa (SSO)—A community-based prospective cohort study on antibody responses, antibody neutralisation efficiency and cellular immunity to SARS-CoV-2 infection and vaccination. BMJ Open. 2022;22:e062187. doi: 10.1136/bmjopen-2022-062187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vinh D.C., Gouin J.P., Cruz-Santiago D., Canac-Marquis M., Bernier S., Bobeuf F., Sengupta A., Brassard J.P., Guerra A., Dziarmaga R., et al. Real-world serological responses to extended-interval and heterologous COVID-19 mRNA vaccination in frail, older people (UNCoVER): An interim report from a prospective observational cohort study. Lancet Healthy Longev. 2022;3:e166–e175. doi: 10.1016/S2666-7568(22)00012-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fakhraei R., Erwin E., Alibhai K.M., Murphy M.S.Q., Dingwall-Harvey A.L.J., White R.R., Dimanlig-Cruz S., LaRose R., Grattan K., Jia J.J., et al. Prevalence of SARS-CoV-2 infection among obstetric patients in Ottawa, Canada: A descriptive study. CMAJ Open. 2022;10:E643–E651. doi: 10.9778/cmajo.20210228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.4-Parameter Log-Logistic Curve Based on Measurements from the World Health Organization International Standard. WHO; Geneva, Switzerland: 2022. [Google Scholar]
- 44.National Institutes of Health Clinical Spectrum of SARS-CoV-2 Infection NIH COVID-19 Treatment Guidelines. [(accessed on 6 March 2023)]; Available online: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/
- 45.Collins L.F., Moran C.A., Oliver N.T., Moanna A., Lahiri C.D., Colasanti J.A., Kelley C.F., Nguyen M.L., Marconi V.C., Armstrong W.S., et al. Clinical characteristics, comorbidities and outcomes among persons with HIV hospitalized with coronavirus disease 2019 in Atlanta, Georgia. AIDS. 2020;34:1789–1794. doi: 10.1097/QAD.0000000000002632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shalev N., Scherer M., LaSota E.D., Antoniou P., Yin M.T., Zucker J., Sobieszczyk M.E. Clinical Characteristics and Outcomes in People Living with Human Immunodeficiency Virus Hospitalized for Coronavirus Disease 2019. Clin. Infect. Dis. 2020;71:2294–2297. doi: 10.1093/cid/ciaa635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ceballos M.E., Ross P., Lasso M., Dominguez I., Puente M., Valenzuela P., Enberg M., Serri M., Munoz R., Pinos Y., et al. Clinical characteristics and outcomes of people living with HIV hospitalized with COVID-19: A nationwide experience. Int. J. STD AIDS. 2021;32:435–443. doi: 10.1177/0956462420973106. [DOI] [PubMed] [Google Scholar]
- 48.Durstenfeld M.S., Sun K., Ma Y., Rodriguez F., Secemsky E.A., Parikh R.V., Hsue P.Y. Association of HIV infection with outcomes among adults hospitalized with COVID-19. AIDS. 2022;36:391–398. doi: 10.1097/QAD.0000000000003129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bhaskaran K., Rentsch C.T., MacKenna B., Schultze A., Mehrkar A., Bates C.J., Eggo R.M., Morton C.E., Bacon S.C.J., Inglesby P., et al. HIV infection and COVID-19 death: A population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV. 2021;8:e24–e32. doi: 10.1016/S2352-3018(20)30305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tesoriero J.M., Swain C.E., Pierce J.L., Zamboni L., Wu M., Holtgrave D.R., Gonzalez C.J., Udo T., Morne J.E., Hart-Malloy R., et al. COVID-19 Outcomes Among Persons Living with or without Diagnosed HIV Infection in New York State. JAMA Netw. Open. 2021;4:e2037069. doi: 10.1001/jamanetworkopen.2020.37069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yang X., Sun J., Patel R.C., Zhang J., Guo S., Zheng Q., Olex A.L., Olatosi B., Weissman S.B., Islam J.Y., et al. Associations between HIV infection and clinical spectrum of COVID-19: A population level analysis based on US National COVID Cohort Collaborative (N3C) data. Lancet HIV. 2021;8:e690–e700. doi: 10.1016/S2352-3018(21)00239-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dong Y., Li Z., Ding S., Liu S., Tang Z., Jia L., Liu J., Liu Y. HIV infection and risk of COVID-19 mortality: A meta-analysis. Medicine. 2021;100:e26573. doi: 10.1097/MD.0000000000026573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dandachi D., Geiger G., Montgomery M.W., Karmen-Tuohy S., Golzy M., Antar A.A.R., Llibre J.M., Camazine M., Diaz-De Santiago A., Carlucci P.M., et al. Characteristics, Comorbidities, and Outcomes in a Multicenter Registry of Patients with Human Immunodeficiency Virus and Coronavirus Disease 2019. Clin. Infect. Dis. 2021;73:e1964–e1972. doi: 10.1093/cid/ciaa1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wong C., Althoff K., Gange S.J. Identifying the appropriate comparison group for HIV-infected individuals. Curr. Opin. HIV AIDS. 2014;9:379–385. doi: 10.1097/COH.0000000000000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coburn S.B., Humes E., Lang R., Stewart C., Hogan B.C., Gebo K.A., Napravnik S., Edwards J.K., Browne L.E., Park L.S., et al. Analysis of Postvaccination Breakthrough COVID-19 Infections Among Adults with HIV in the United States. JAMA Netw. Open. 2022;5:e2215934. doi: 10.1001/jamanetworkopen.2022.15934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sun J., Zheng Q., Madhira V., Olex A.L., Anzalone A.J., Vinson A., Singh J.A., French E., Abraham A.G., Mathew J., et al. Association Between Immune Dysfunction and COVID-19 Breakthrough Infection After SARS-CoV-2 Vaccination in the US. JAMA Intern. Med. 2022;182:153–162. doi: 10.1001/jamainternmed.2021.7024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vivaldi G., Jolliffe D.A., Holt H., Tydeman F., Talaei M., Davies G.A., Lyons R.A., Griffiths C.J., Kee F., Sheikh A., et al. Risk factors for SARS-CoV-2 infection after primary vaccination with ChAdOx1 nCoV-19 or BNT162b2 and after booster vaccination with BNT162b2 or mRNA-1273: A population-based cohort study (COVIDENCE UK) Lancet Reg. Health Eur. 2022;22:100501. doi: 10.1016/j.lanepe.2022.100501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee J., Woodruff M.C., Kim E.H., Nam J.H. Knife’s edge: Balancing immunogenicity and reactogenicity in mRNA vaccines. Exp. Mol. Med. 2023;55:1305–1313. doi: 10.1038/s12276-023-00999-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walmsley S., Ravindran R., Clarke R., Wouters B., Silva A., Gingras A.C., Szadkowski L. COVID-19 breakthrough infections in vaccinated participants of the Safety and Efficacy of Preventative COVID Vaccines sub-study. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2022;7:333–342. doi: 10.3138/jammi-2022-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chun H.M., Milligan K., Agyemang E., Ford N., Rangaraj A., Desai S., Wilder-Smith A., Vitoria M., Zulu I. A Systematic Review of COVID-19 Vaccine Antibody Responses in People with HIV. Open Forum Infect. Dis. 2022;9:ofac579. doi: 10.1093/ofid/ofac579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Augello M., Bono V., Rovito R., Tincati C., Bianchi S., Taramasso L., Di Biagio A., Callegaro A., Maggiolo F., Borghi E., et al. Association between SARS-CoV-2 RNAemia, skewed T cell responses, inflammation, and severity in hospitalized COVID-19 people living with HIV. iScience. 2024;27:108673. doi: 10.1016/j.isci.2023.108673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khoury D.S., Cromer D., Reynaldi A., Schlub T.E., Wheatley A.K., Juno J.A., Subbarao K., Kent S.J., Triccas J.A., Davenport M.P. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 2021;27:1205–1211. doi: 10.1038/s41591-021-01377-8. [DOI] [PubMed] [Google Scholar]
- 63.Feng S., Phillips D.J., White T., Sayal H., Aley P.K., Bibi S., Dold C., Fuskova M., Gilbert S.C., Hirsch I., et al. Correlates of protection against symptomatic and asymptomatic SARS-CoV-2 infection. Nat. Med. 2021;27:2032–2040. doi: 10.1038/s41591-021-01540-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gilbert P.B., Montefiori D.C., McDermott A.B., Fong Y., Benkeser D., Deng W., Zhou H., Houchens C.R., Martins K., Jayashankar L., et al. Immune correlates analysis of the mRNA-1273 COVID-19 vaccine efficacy clinical trial. Science. 2022;375:43–50. doi: 10.1126/science.abm3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bergwerk M., Gonen T., Lustig Y., Amit S., Lipsitch M., Cohen C., Mandelboim M., Levin E.G., Rubin C., Indenbaum V., et al. Covid-19 Breakthrough Infections in Vaccinated Health Care Workers. N. Engl. J. Med. 2021;385:1474–1484. doi: 10.1056/NEJMoa2109072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Earle K.A., Ambrosino D.M., Fiore-Gartland A., Goldblatt D., Gilbert P.B., Siber G.R., Dull P., Plotkin S.A. Evidence for antibody as a protective correlate for COVID-19 vaccines. Vaccine. 2021;39:4423–4428. doi: 10.1016/j.vaccine.2021.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lipsitch M., Krammer F., Regev-Yochay G., Lustig Y., Balicer R.D. SARS-CoV-2 breakthrough infections in vaccinated individuals: Measurement, causes and impact. Nat. Rev. Immunol. 2022;22:57–65. doi: 10.1038/s41577-021-00662-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Martin D.P., Lytras S., Lucaci A.G., Maier W., Gruning B., Shank S.D., Weaver S., MacLean O.A., Orton R.J., Lemey P., et al. Selection Analysis Identifies Clusters of Unusual Mutational Changes in Omicron Lineage BA.1 That Likely Impact Spike Function. Mol. Biol. Evol. 2022;39:msac061. doi: 10.1093/molbev/msac061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hoffmann M., Kruger N., Schulz S., Cossmann A., Rocha C., Kempf A., Nehlmeier I., Graichen L., Moldenhauer A.S., Winkler M.S., et al. The Omicron variant is highly resistant against antibody-mediated neutralization: Implications for control of the COVID-19 pandemic. Cell. 2022;185:447–456 e411. doi: 10.1016/j.cell.2021.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kumar S., Thambiraja T.S., Karuppanan K., Subramaniam G. Omicron and Delta variant of SARS-CoV-2: A comparative computational study of spike protein. J. Med. Virol. 2022;94:1641–1649. doi: 10.1002/jmv.27526. [DOI] [PubMed] [Google Scholar]
- 71.Chatterjee S., Bhattacharya M., Nag S., Dhama K., Chakraborty C. A Detailed Overview of SARS-CoV-2 Omicron: Its Sub-Variants, Mutations and Pathophysiology, Clinical Characteristics, Immunological Landscape, Immune Escape, and Therapies. Viruses. 2023;15:167. doi: 10.3390/v15010167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Menni C., Valdes A.M., Polidori L., Antonelli M., Penamakuri S., Nogal A., Louca P., May A., Figueiredo J.C., Hu C., et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: A prospective observational study from the ZOE COVID Study. Lancet. 2022;399:1618–1624. doi: 10.1016/S0140-6736(22)00327-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Keeton R., Tincho M.B., Ngomti A., Baguma R., Benede N., Suzuki A., Khan K., Cele S., Bernstein M., Karim F., et al. T cell responses to SARS-CoV-2 spike cross-recognize Omicron. Nature. 2022;603:488–492. doi: 10.1038/s41586-022-04460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Grifoni A., Weiskopf D., Ramirez S.I., Mateus J., Dan J.M., Moderbacher C.R., Rawlings S.A., Sutherland A., Premkumar L., Jadi R.S., et al. Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell. 2020;181:1489–1501.e1415. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Braun J., Loyal L., Frentsch M., Wendisch D., Georg P., Kurth F., Hippenstiel S., Dingeldey M., Kruse B., Fauchere F., et al. SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19. Nature. 2020;587:270–274. doi: 10.1038/s41586-020-2598-9. [DOI] [PubMed] [Google Scholar]
- 76.Yang Y., Miller H., Byazrova M.G., Cndotti F., Benlagha K., Camara N.O.S., Shi J., Forsman H., Lee P., Yang L., et al. The characterization of CD8(+) T-cell responses in COVID-19. Emerg. Microbes Infect. 2024;13:2287118. doi: 10.1080/22221751.2023.2287118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Deeks S.G., Tracy R., Douek D.C. Systemic effects of inflammation on health during chronic HIV infection. Immunity. 2013;39:633–645. doi: 10.1016/j.immuni.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hoffmann C., Casado J.L., Harter G., Vizcarra P., Moreno A., Cattaneo D., Meraviglia P., Spinner C.D., Schabaz F., Grunwald S., et al. Immune deficiency is a risk factor for severe COVID-19 in people living with HIV. HIV Med. 2021;22:372–378. doi: 10.1111/hiv.13037. [DOI] [PubMed] [Google Scholar]
- 79.Marchitto L., Chatterjee D., Ding S., Gendron-Lepage G., Tauzin A., Boutin M., Benlarbi M., Medjahed H., Sylla M., Lanctot H., et al. Humoral Responses Elicited by SARS-CoV-2 mRNA Vaccine in People Living with HIV. Viruses. 2023;15:2004. doi: 10.3390/v15102004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bhattacharyya S., Crain C.R., Goldberg B., Gaiha G.D. Features of functional and dysfunctional CD8+ T cells to guide HIV vaccine development. Curr. Opin. HIV AIDS. 2023;18:257–263. doi: 10.1097/COH.0000000000000812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sheikh-Mohamed S., Isho B., Chao G.Y.C., Zuo M., Cohen C., Lustig Y., Nahass G.R., Salomon-Shulman R.E., Blacker G., Fazel-Zarandi M., et al. Systemic and mucosal IgA responses are variably induced in response to SARS-CoV-2 mRNA vaccination and are associated with protection against subsequent infection. Mucosal Immunol. 2022;15:799–808. doi: 10.1038/s41385-022-00511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study may be made available upon written request to the corresponding author. Researchers wishing to access the CITF core data elements can submit an application to the CITF Data Access Committee.