Abstract
Objective
To develop an approach for identifying, investigating, and initially managing common causes of chronic wrist pain seen by primary care practitioners.
Sources of information
Relevant clinical evidence and literature were identified using the PubMed database.
Main message
Chronic wrist pain is a common presentation in the primary care setting. The complex anatomy of the wrist leads to a broad differential diagnosis. Elements of history, findings of physical examinations and investigations, and management relevant to the following pathologies are discussed, including scaphoid fracture nonunion, thumb carpometacarpal joint osteoarthritis, scapholunate ligament instability, triangular fibrocartilage complex injuries, de Quervain tenosynovitis, extensor carpi ulnaris tendinopathy, carpal tunnel syndrome, and ganglion cysts. When evaluating chronic wrist pain, diagnostic imaging with x-ray scans can serve as an important ancillary investigation tool but should not override clinical suspicion. Advanced imaging (computed tomography or magnetic resonance imaging) is generally best ordered by a hand surgeon when it will help clarify a diagnosis and guide treatment.
Conclusion
Chronic wrist pain is a functionally limiting problem best managed with timely diagnosis and treatment. A thorough history and physical examination are the cornerstones of an effective evaluation. When diagnosis is delayed, some wrist pathologies can lead to relatively poor outcomes, such as a scaphoid fracture nonunion resulting in diffuse wrist osteoarthritis.
Case presentation
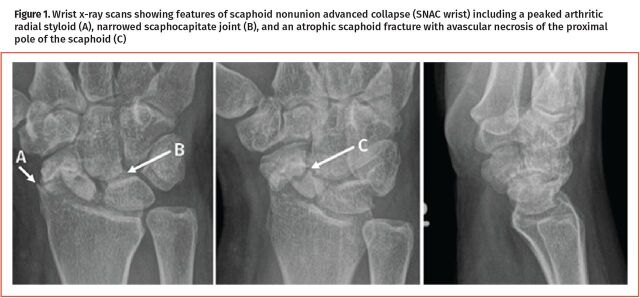
A 40-year-old woman presents with a progressive 5-year history of dorsoradial wrist pain that worsens with activity, especially loaded wrist extension. She has noted increased soft tissue edema over the dorsoradial wrist and loss of wrist range of motion, particularly in extension. Her wrist is tender on palpation of the radial styloid process, anatomic snuffbox (scaphoid), and radioscaphoid joint. She recalls falling on her wrist in her 20s while playing volleyball and being diagnosed with a “sprain.” No x-ray scans were taken at that time. Her most recent x-ray scan findings reveal a pointed and arthritic radial styloid process, a narrowed joint space between the distal scaphoid and capitate, and a collapsed scaphoid with sclerosis and proximal pole avascular necrosis (Figure 1).
Figure 1.
Wrist x-ray scans showing features of scaphoid nonunion advanced collapse (SNAC wrist) including a peaked arthritic radial styloid (A), narrowed scaphocapitate joint (B), and an atrophic scaphoid fracture with avascular necrosis of the proximal pole of the scaphoid (C)
Sources of information
The PubMed electronic database was searched for articles discussing the pathogenesis, evaluation, and management of important osseous, tendinous, ligamentous, or neuropathic pathologies that can cause chronic wrist pain. Articles were reviewed for relevance, assessed for quality of evidence, and categorized as level 1, 2, or 3 evidence. When there was an absence of high-level evidence, expert opinion and key review papers were referenced.1-4
Main message
Clinical evaluation. Standard history taking is important. All patients are asked about hand dominance, occupation and hobbies, and prior hand history of trauma, masses, and surgery. In addition to a pain history, patients are asked about other symptoms including wrist edema, catching, popping, clicking, stiffness, and instability. These features can suggest intra-articular loose bodies, subluxation of a tendon, midcarpal instability, structural compromise of a tendon and ligament, or arthritic changes. A review of systems can help identify associated systemic features, which can increase suspicion of rheumatic pathologies such as rheumatoid arthritis, psoriasis, or CREST (calcinosis, Raynaud phenomenon, esophageal motility disorder, sclerodactyly, and telangiectasia) syndrome affecting the wrists. These features can include fatigue, weight loss, myalgias, polyarticular swelling and stiffness, morning stiffness, nodules on extensor surfaces, skin changes, and ocular impairment.
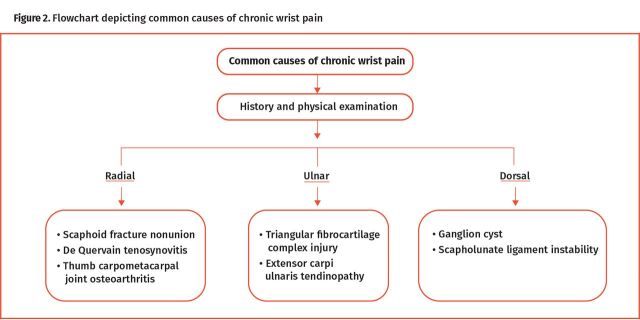
The goal of the physical examination is to pinpoint the location of the pain, as this can simplify the differential diagnosis (Figure 2). After inspection for signs of trauma, edema, scars, masses, and muscle atrophy, systematically palpate each anatomic structure (ie, the 8 carpal bones, multiple intercarpal ligaments, flexor and extensor tendons, surrounding soft tissues) for tenderness (Figure 3). Passive, active, and resisted range of motion with wrist flexion, extension, and radial and ulnar deviation are compared with the contralateral limb. Localizing tenderness to the radial, central, or ulnar aspect of the wrist will assist clinicians in narrowing the differential diagnosis and identifying appropriate special tests or investigations to confirm or rule out specific pathologies. A video overview is available (https://youtu.be/J5EbzrK5ttI).5
Figure 2.
Flowchart depicting common causes of chronic wrist pain
Figure 3.
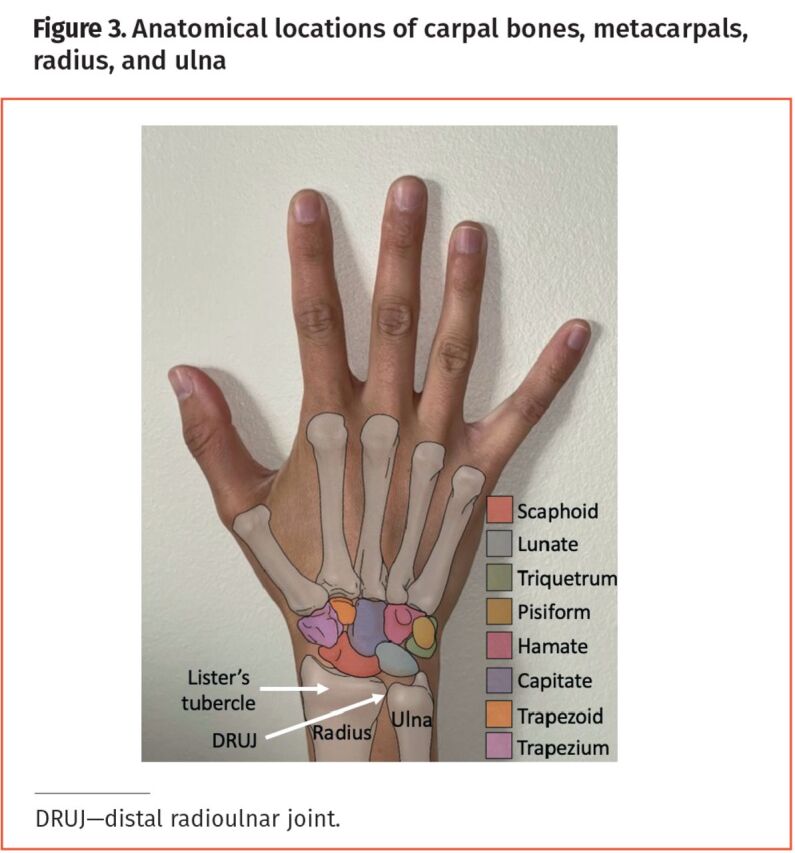
Anatomical locations of carpal bones, metacarpals, radius, and ulna
Common causes of chronic wrist pain
Scaphoid fracture nonunion: If missed or inadequately immobilized, fractures of the scaphoid can result in nonunion, presenting with radial-sided wrist pain and loss of wrist range of motion. Suspicion of scaphoid nonunion should be investigated with plain x-ray scans with 4 views: posteroanterior (PA) with the wrist in neutral position, PA with the wrist in ulnar deviation to improve visualization of the scaphoid (“scaphoid view”), oblique, and lateral; these are commonly ordered as “x-ray 3 views of the wrist plus a scaphoid view.” The unhealed fracture will be seen and, depending on the chronicity of the nonunion, additional findings around the fracture may include bone resorption, cyst formation, and sclerosis (Figure 1). Referral to a hand surgeon permits surgical treatment, which is typically open reduction internal fixation with a screw and bone grafting, ideally before patient progression to scaphoid nonunion advanced collapse (SNAC) wrist osteoarthritis. In SNAC, the surrounding carpal bones undergo a predictable pattern of degenerative wrist osteoarthritis changes caused by abnormal scaphoid anatomy when not united. Once SNAC has developed, open reduction internal fixation of the scaphoid alone is no longer an option and extensive surgery is often required to address the arthritic changes if symptomatic.
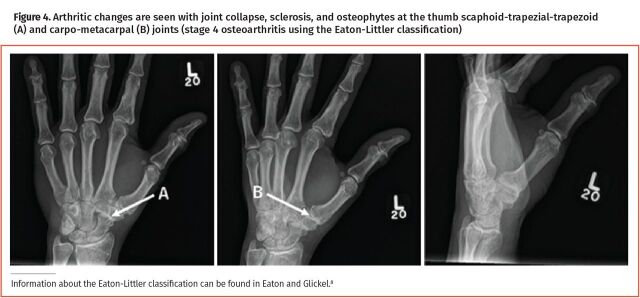
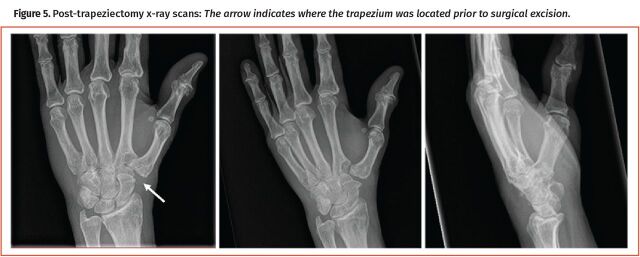
Thumb carpometacarpal (CMC) joint osteoarthritis: Osteoarthritis of the thumb CMC joint is a degenerative condition common in postmenopausal women.6 In addition to a dull aching pain at rest, patients may report weakness in their grip strength and ability to pinch, which can manifest as pain when opening a jar or twisting a key. Physical examination can reveal tenderness and crepitus at the thumb CMC joint. The “grind test” is a valuable diagnostic maneuver (sensitivity 41%; specificity 100%) where pain when the CMC joint is loaded axially and the thumb is simultaneously rotated indicates a positive test result.7 As a complement, the “lever test” is a more sensitive maneuver that has a positive test result if there is pain when the first metacarpal is rocked back and forth radially and ulnarly on the trapezium (sensitivity 82%; specificity 81%).7 X-ray scans of the hand (ordered as “x-ray 3 views of the hand” or “3 views of the thumb”; an additional true anteroposterior view ordered as “x-ray Robert’s view of the thumb” helps to see the thumb CMC joint) can help visualize the radiographic severity of arthritic changes, although this does not always correlate to clinical findings (Figure 4).8 Therefore, treatment is guided by patient symptoms, especially pain with activity. First-line treatment includes splinting, activity modification, and nonsteroidal antiinflammatory drugs (NSAIDs).9 Steroid injections can provide short-term pain relief but have less effect with repeated use and limited value in moderate- to late-stage arthritis (level 1 evidence).10 Ultimately, patients whose symptoms do not respond to non-operative management, with daily painful symptoms limiting function, should be referred to a hand surgeon for consideration of surgery, which would most commonly be a trapeziectomy (removal of the trapezium to relieve the arthritic contact between the thumb metacarpal base and the distal trapezium) (Figure 5).
Figure 4.
Arthritic changes are seen with joint collapse, sclerosis, and osteophytes at the thumb scaphoid-trapezial-trapezoid (A) and carpo-metacarpal (B) joints (stage 4 osteoarthritis using the Eaton-Littler classification)
Figure 5.
Post-trapeziectomy x-ray scans: The arrow indicates where the trapezium was located prior to surgical excision.
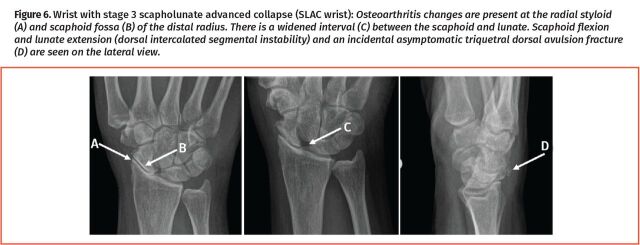
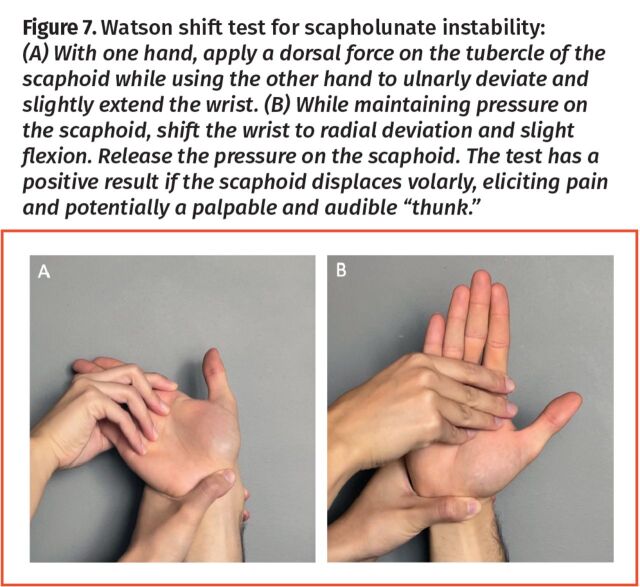
Scapholunate (SL) ligament instability: The SL ligament is an intrinsic (intrinsic—connecting the carpal bones, as opposed to extrinsic—connecting a carpal bone to a noncarpal bone) wrist ligament between the scaphoid and lunate bones that provides stability to the wrist. When torn, usually during a fall, the interval between the scaphoid and lunate bones can widen. This can be seen on a PA x-ray scan when this deformity is static or on a PA provocative x-ray scan of a clenched fist when the deformity is dynamic (Figure 6). With SL ligament injuries, the scaphoid can flex and the lunate can extend (known as dorsal intercalated segmental instability pattern, best seen on lateral x-ray scans) (Figure 6). Patients with untreated SL ligament injury report central dorsal wrist pain and decreased grip strength. Palpation over the dorsal wrist reveals tenderness over the SL interval, located a finger’s width distal to the dorsal tubercle of the radius (palpable as a bony prominence on the dorsal distal radius). The Watson shift test can elicit SL ligament pain or instability, with a sensitivity of 69% and specificity of 66% (Figure 7).11 Bilateral x-ray scans to compare the symptomatic and asymptomatic wrists (ordered as “x-ray 3 views of the bilateral wrists plus a bilateral clenched fist view x-ray”) are helpful. The clenched-fist view x-ray scan can suggest an SL ligament injury when the symptomatic wrist’s SL interval is wide compared with the contralateral side in dynamic SL ligament injuries. Uncommonly, if the x-ray scan findings are normal but there is high suspicion of an SL ligament injury based on the history and physical examination findings, a hand surgeon may order magnetic resonance imaging (MRI) with intra-articular gadolinium contrast, typically before considering wrist arthroscopy for further information. A chronic untreated injury of the SL ligament can lead to SL advanced collapse, where the surrounding carpal bones undergo degenerative osteoarthritis change because of the loss of SL ligament stability (Figure 6). Multiple surgical options exist for SL ligament reconstruction, but outcomes are often poor. In SL advanced collapse, such as in SNAC, “reconstruction” is often no longer possible due to osteoarthritis and different surgeries are offered to symptomatic patients to alleviate pain.
Figure 6.
Wrist with stage 3 scapholunate advanced collapse (SLAC wrist): Osteoarthritis changes are present at the radial styloid (A) and scaphoid fossa (B) of the distal radius. There is a widened interval (C) between the scaphoid and lunate. Scaphoid flexion and lunate extension (dorsal intercalated segmental instability) and an incidental asymptomatic triquetral dorsal avulsion fracture (D) are seen on the lateral view.
Figure 7.
Watson shift test for scapholunate instability: (A) With one hand, apply a dorsal force on the tubercle of the scaphoid while using the other hand to ulnarly deviate and slightly extend the wrist. (B) While maintaining pressure on the scaphoid, shift the wrist to radial deviation and slight flexion. Release the pressure on the scaphoid. The test has a positive result if the scaphoid displaces volarly, eliciting pain and potentially a palpable and audible “thunk.”
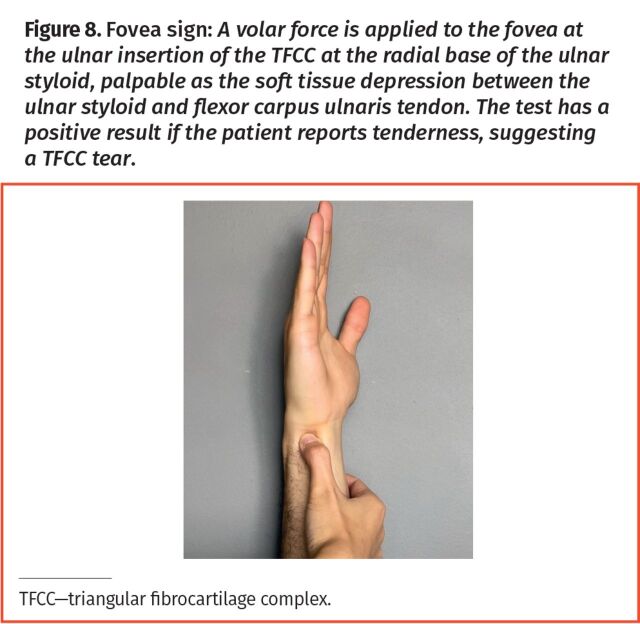
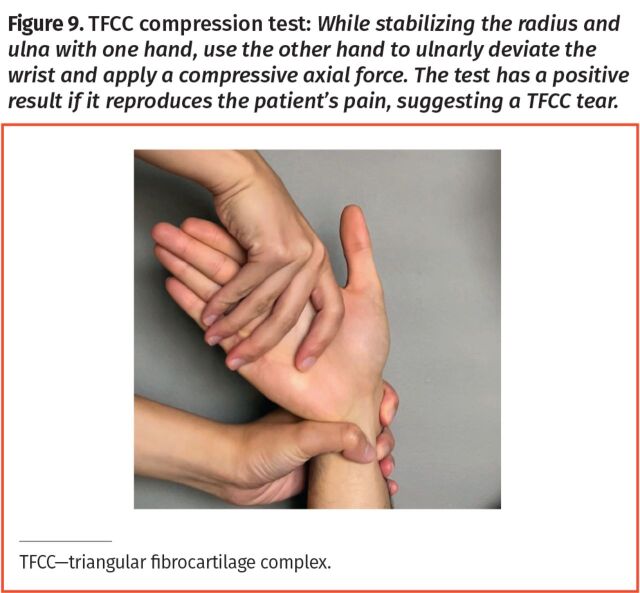
Triangular fibrocartilage complex (TFCC): Serving as the primary stabilizer of the distal radioulnar joint (DRUJ), the TFCC also functions to distribute forces from the carpal bones to the ulna. The TFCC is susceptible to damage from chronic wear or from falling on an extended, pronated, ulnarly deviated wrist, which patients may recall as a prior wrist sprain.12 Patients report ulnar-sided pain aggravated by activities requiring pronation and supination.2 Physical examination findings demonstrate tenderness at the fovea—the soft tissue depression at the volar ulnar wrist between the ulnar styloid and flexor carpi ulnaris tendon (Figure 8). The TFCC compression test reproduces the patient’s pain with axial compression on the TFCC while the wrist is ulnarly deviated (Figure 9); it has a sensitivity of 59% and specificity of 91%.13,14 To assess for instability of the DRUJ, employ the ballottement test, which has a sensitivity of 59% and specificity of 96%. This test involves stabilizing the patient’s radiocarpal joint in a neutral position with one hand while the other hand grasps the distal ulna to apply alternating dorsal and palmar force to check for laxity or a firm end point. This should be compared with the contralateral wrist. Note that DRUJ instability may also occur with malunion of a prior distal radius fracture, which can develop in up to 24% in those treated with cast immobilization.15-17 Distal radioulnar joint instability can lead to osteoarthritis due to altered wrist biomechanics.
Figure 8.
Fovea sign: A volar force is applied to the fovea at the ulnar insertion of the TFCC at the radial base of the ulnar styloid, palpable as the soft tissue depression between the ulnar styloid and flexor carpus ulnaris tendon. The test has a positive result if the patient reports tenderness, suggesting a TFCC tear.
Figure 9.
TFCC compression test: While stabilizing the radius and ulna with one hand, use the other hand to ulnarly deviate the wrist and apply a compressive axial force. The test has a positive result if it reproduces the patient’s pain, suggesting a TFCC tear.
There is no consensus on the specifics of short-term conservative treatment of TFCC tears, as some recommend above-elbow casting, which limits forearm pronosupination if there is a tear with no DRUJ instability, while others recommend a volar wrist splint for 4 weeks (level 2 evidence).18 If there is instability or persistent symptoms, a referral to a hand surgeon is recommended to guide immobilization, followed by a return to activity and surgical intervention when indicated. Typically, wrist arthroscopy is used to fully visualize, probe, and repair the tear. Wrist x-ray scans are helpful in assessing ulnar variance (the length of the distal ulna compared with the distal radius). Patients with an ulna longer than the radius are often offered an ulnar-shortening osteotomy to offload the painful TFCC and to tighten the TFCC and adjacent ulnocarpal ligaments.
De Quervain tenosynovitis: De Quervain tenosynovitis results from inflammation and thickening of the first extensor compartment sheath from repeated use and presents with painful thumb extension and abduction and radial-sided wrist pain. It is 10 times more common in women compared with men, which is believed to be due to underlying anatomic and hormonal differences.19-21 A positive Finkelstein test result, executed by passively flexing the thumb while ulnarly deviating the wrist to tighten the first extensor compartment and reproduce the patient’s pain, is pathognomonic for this condition.22 Palpation over the first extensor compartment tendons, the adductor pollicis longus and extensor pollicis brevis, is painful in this condition. Management initially includes thumb spica splinting, compression, activity modification, NSAIDs, or steroid injections, which can result in 82% of patients being symptom free at 6 weeks and 52% at both 6 and 12 months (level 1 evidence).23-25 Steroid injections should ideally be performed under ultrasound guidance to improve injection accuracy, leading to better outcomes.24 Ultrasound guidance is particularly important if there is an intracompartmental septum separating the adductor pollicis longus and extensor pollicis brevis, which would necessitate injection into both “sub-tunnels” within the first extensor compartment. If there are symptoms despite non-surgical management, referral to a hand surgeon can be made for consideration of surgical decompression of the first extensor compartment.22,24 This condition is often self-limiting in pregnancy and non-surgical measures with observation are typically sufficient.
Extensor carpi ulnaris (ECU) tendinopathy: Common in tennis and golf players, distal tendinopathy of the ECU can lead to ulnar-sided wrist pain and weakness with wrist extension and ulnar deviation. The ECU synergy test can reproduce the patient’s pain through isometric contraction of the ECU muscle: While flexing the patient’s elbow at 90°, supinating the forearm, and grasping the patient’s thumb and long digit, the patient radially abducts the thumb against resistance.26 Subluxation of the ECU can also cause dorsal ulnar wrist pain. It can be reproduced by moving the patient’s wrist from supination and extension to flexion and ulnar deviation; in a positive test result, pain is noted when the ECU tendon subluxes from its dorsal location on the ulnar head to a volar-ulnar location relative to the ulnar head (sensitivity 74%; specificity 86%). Bracing or surgery can be considered to reconstruct the ECU tendon sheath to stabilize the tendon.27,28 In the setting of chronic ECU tendinopathy without subluxation, initial management consists of NSAIDs with isometric and eccentric strengthening of the ECU (level 3 evidence).29
Carpal tunnel syndrome (CTS): As the most common nerve entrapment syndrome, CTS affects 3.1% to 4.6% of the population.30 Clinically, patients describe the pain affecting the hand more than the wrist. Patients usually report tingling or numbness in the median nerve distribution, affecting the thumb, index finger, middle finger, and ulnar half of the ring finger. The Phalen test (sensitivity 70%; specificity 84%) and Tinel test (sensitivity 56%; specificity 80%) can provoke these symptoms by maximally flexing the wrists while placing the dorsa of the hands together in the former and percussing over the carpal tunnel in the latter.31 The carpal compression test, which involves compressing the carpal ligament, carries the highest diagnostic value (sensitivity 87%; specificity 90%).31 Weakness with thumb abduction and opposition is seen in advanced neuropathy, along with thenar muscle atrophy on inspection. Carpal tunnel syndrome is often a clinical diagnosis, but nerve conduction studies and electromyography can provide further information on severity and can be helpful when there is additional pathology (eg, cervical spine disease) or atypical symptoms. Initial management consists of minimizing activities with excessive wrist flexion to decrease compression of the carpal tunnel and night-time neutral wrist splinting, which has been shown to improve symptoms in the short term (level 1 evidence).32 Steroid injections can be considered for short-term relief; however, long-term outcomes are variable, with 1 study reporting a single steroid injection achieving symptom relief in 79% of patients at 6 weeks, 53% at 6 months, and 31% at 12 months.25,33 If symptoms persist, a referral for surgical decompression is recommended.
Ganglion cyst: Ganglion cysts, also referred to as synovial cysts, are benign fluid-filled masses commonly found on the dorsal radial wrist arising from the SL ligament. If the cysts are asymptomatic, education, reassurance, and observation are recommended. If the cysts are symptomatic, with substantial pain impairing daily function, consider aspiration or referral for surgical excision; recurrence rates after aspiration and surgery are 21% and 59%, respectively (level 1 evidence).34 However, education regarding recurrence rates is key; patients should understand that the associated wrist pain does not always resolve. Substantial pain may suggest further underlying pathology, such as an SL ligament injury, and advanced imaging with MRI or wrist arthroscopy may be indicated. For superficial soft tissue masses like ganglion cysts, ultrasound has excellent sensitivity (94.1%) and specificity (99.7%)35 although it is rarely indicated; clinical diagnosis is the mainstay.
Imaging recommendations. First-line imaging for ligamentous injuries of the wrist consists of plain x-ray scans (Table 1). Widening of ligamentous intervals, when compared with the contralateral limb, and compensatory changes of surrounding carpal bones can be seen. In other cases, x-ray scan findings can be normal, prompting further assessment by a physician with added competencies in musculoskeletal conditions, guided by the patient’s history, physical examination, and MRI findings. Ultrasound scans have a low sensitivity in identifying ligamentous injuries (sensitivity 46.2%; specificity 100%), so MRI is recommended in the context of negative x-ray scan findings and persistent symptoms.36,37 Although MRI is 97% accurate in detecting central and radial-side ligament tears, it does not offer the same accuracy in detecting ulnar-sided ligamentous injuries. Magnetic resonance arthrography (sensitivity 85%; specificity 76%) is helpful in the diagnosis of ulnar-sided ligamentous pathology.38
Table 1.
First-line investigations for common causes of chronic wrist pain
| PATHOLOGY | FIRST-LINE INVESTIGATION | VIEWS |
|---|---|---|
| Scaphoid fracture nonunion | X-ray scan | 3 views of the wrist plus a scaphoid view |
| Thumb CMC joint osteoarthritis | X-ray scan | 3 views of the hand and thumb; true AP view of the thumb |
| Scapholunate instability | X-ray scan | 3 views of the bilateral wrists plus a bilateral clenched-fist view |
| TFCC injury | X-ray scan | 3 views of the wrist |
| De Quervain tenosynovitis | Ultrasound scan | Views of the first extensor compartment |
| ECU tendinopathy | Ultrasound scan | Views of the sixth extensor compartment |
| Carpal tunnel syndrome | Nerve conduction study or electromyography | NA |
| Ganglion cyst | Ultrasound scan | Views of the mass |
AP—anteroposterior, CMC—carpometacarpal, ECU—extensor carpi ulnaris, NA—not applicable, TFCC—triangular fibrocartilage complex.
For tendinopathies, the diagnosis is based on history and clinical examination findings. Imaging is indicated if the patient does not respond to conservative management to look for alternative diagnoses or if the diagnosis is initially unclear.26 For tendon pathologies, regular ultrasound scans can visualize tears or inflammation (Table 1). Additionally, dynamic evaluation can aid visualization of subluxation.39
Case resolution
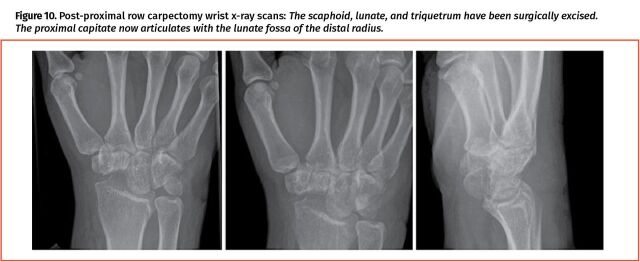
The patient has a distal scaphoid nonunion with associated SNAC arthritic changes that have developed over years. Despite non-operative interventions including splinting, topical and oral NSAIDs, steroid injections, and activity modification, the patient continued to have daily, worsening wrist pain, and opted for surgical treatment. Due to the extent of the scaphoid collapse, avascular necrosis, and associated osteoarthritis, the scaphoid and associated changes were deemed nonreconstructable. The patient was offered “salvage” options and elected for a proximal row carpectomy (removal of the proximal carpal row bones: scaphoid, lunate, and triquetrum) instead of a partial wrist fusion to maintain greater wrist range of motion and to avoid hardware complications and the risk of malunion or nonunion (Figure 10). The patient’s pain was much improved after surgery.
Figure 10.
Post-proximal row carpectomy wrist x-ray scans: The scaphoid, lunate, and triquetrum have been surgically excised. The proximal capitate now articulates with the lunate fossa of the distal radius.
Conclusion
Chronic wrist pain is a common presentation with a broad differential diagnosis that includes masses and pathologies spanning bony, tendinous, ligamentous, and neuropathic causes. We have discussed the approach to identifying, diagnosing, and initially managing common causes of chronic wrist pain. In most cases, a thorough history and clinical examination considerably narrow the differential diagnosis. With the increased reliance on imaging and with rising health care costs, judicious use of diagnostic imaging is also important. If imaging is indicated, radiography and ultrasound are often appropriate, but advanced imaging may be indicated in specific clinical scenarios.
Editor’s key points
▸ Chronic wrist pain is a common presentation with a broad differential diagnosis that includes masses and pathologies spanning bony, tendinous, ligamentous, and neuropathic causes. A thorough history and clinical examination considerably narrow the differential diagnosis. With the increased reliance on imaging and rising health care costs, judicious use of diagnostic imaging is important. If imaging is indicated, radiography and ultrasound scans are often appropriate, but advanced imaging may be indicated in specific clinical scenarios.
▸ Standard history taking is important. All patients are asked about hand dominance, occupation and hobbies, and prior hand history of trauma, masses, and surgery. Patients are also asked about other symptoms including wrist edema, catching, popping, clicking, stiffness, and instability. These features can suggest intraarticular loose bodies, subluxation of a tendon, midcarpal instability, structural compromise of a tendon or ligament, or arthritic changes.
▸ The goal of the physical examination is to pinpoint the location of the pain. Passive, active, and resisted range of motion with wrist flexion, extension, and radial and ulnar deviation are compared with the contralateral limb. Localizing tenderness to the radial, central, or ulnar aspect of the wrist will assist clinicians in narrowing the differential diagnosis and identifying appropriate tests or investigations to confirm or rule out specific pathologies.
Footnotes
Contributors
All authors collectively conceived of the presented idea for the report. Shayan Hemmati, Dr Brett Ponich, Dr Ann-Sophie Lafreniere, Dr Olivia Genereux, and Dr Brian Rankin worked together to acquire and interpret current literature and to write the manuscript. Dr Kate Elzinga guided and assisted in manuscript preparation and writing by providing expert opinion on the topics discussed. All authors revised the manuscript critically and approved the final version.
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to https://www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à https://www.cfp.ca dans la table des matières du numéro de janvier 2024 à la page e1 .
References
- 1.DaSilva MF, Goodman AD, Gil JA, Akelman E.. Evaluation of ulnar-sided wrist pain. J Am Acad Orthop Surg 2017;25(8):e150-6. [DOI] [PubMed] [Google Scholar]
- 2.Pang EQ, Yao J.. Ulnar-sided wrist pain in the athlete (TFCC/DRUJ/ECU). Curr Rev Musculoskelet Med 2017;10(1):53-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyd B, Adams J.. Distal radioulnar joint instability. Hand Clin 2021;37(4):563-73. [DOI] [PubMed] [Google Scholar]
- 4.Kuo CE, Wolfe SW.. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am 2008;33(6):998-1013. [DOI] [PubMed] [Google Scholar]
- 5.Shayan K. Chronic wrist pain: physical exam overview [video]. San Bruno, CA: YouTube; 2023. Available from: https://youtu.be/J5EbzrK5ttI. Accessed 2023 Nov 29. [Google Scholar]
- 6.Bakri K, Moran SL.. Thumb carpometacarpal arthritis. Plast Reconstr Surg 2015;135(2):508-20. [DOI] [PubMed] [Google Scholar]
- 7.Model Z, Liu AY, Kang L, Wolfe SW, Burket JC, Lee SK.. Evaluation of physical examination tests for thumb basal joint osteoarthritis. Hand (N Y) 2016;11(1):108-12. Epub 2016 Jan 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eaton RG, Glickel SZ.. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin 1987;3(4):455-71. [PubMed] [Google Scholar]
- 9.Pickrell BB, Eberlin KR.. Thumb basal joint arthritis. Clin Plast Surg 2019;46(3):407-13. [DOI] [PubMed] [Google Scholar]
- 10.Meenagh GK, Patton J, Kynes C, Wright GD.. A randomised controlled trial of intraarticular corticosteroid injection of the carpometacarpal joint of the thumb in osteoarthritis. Ann Rheum Dis 2004;63(10):1260-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LaStayo P, Howell J.. Clinical provocative tests used in evaluating wrist pain: a descriptive study. J Hand Ther 1995;8(1):10-7. [DOI] [PubMed] [Google Scholar]
- 12.Henry MH. Management of acute triangular fibrocartilage complex injury of the wrist. J Am Acad Orthop Surg 2008;16(6):320-9. [DOI] [PubMed] [Google Scholar]
- 13.Lindau T, Adlercreutz C, Aspenberg P.. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am 2000;25(3):464-8. [DOI] [PubMed] [Google Scholar]
- 14.Ahn AK, Chang D, Plate AM.. Triangular fibrocartilage complex tears: a review. Bull NYU Hosp Jt Dis 2006;64(3-4):114-8. [PubMed] [Google Scholar]
- 15.Katt B, Seigerman D, Lutsky K, Beredjiklian P.. Distal radius malunion. J Hand Surg Am 2020;45(5):433-42. Epub 2020 Mar 24. [DOI] [PubMed] [Google Scholar]
- 16.Cooney WP, Linscheid RL, Dobyns JH, editors. The wrist: diagnosis and operative treatment, volume 1. St Louis, MO: Mosby; 1998. p. 365-84. [Google Scholar]
- 17.Sharma H, Khare GN, Singh S, Ramaswamy AG, Kumaraswamy V, Singh AK.. Outcomes and complications of fractures of distal radius (AO type B and C): volar plating versus nonoperative treatment. J Orthop Sci 2014;19(4):537-44. Epub 2014 Mar 26. Erratum in: J Orthop Sci 2014;19(4): 545. [DOI] [PubMed] [Google Scholar]
- 18.Park MJ, Jagadish A, Yao J.. The rate of triangular fibrocartilage injuries requiring surgical intervention. Orthopedics 2010;33(11):806. [DOI] [PubMed] [Google Scholar]
- 19.Kahn SB, Xu RY, editors. Musculoskeletal sports and spine disorders: a comprehensive guide. Cham, Switz: Springer International; 2018. [Google Scholar]
- 20.Ramchandani J, Thakker A, Tharmaraja T.. Time to reconsider occupation induced de Quervain’s tenosynovitis: an updated review of risk factors. Orthop Rev (Pavia) 2022;14(4):36911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shen PC, Wang PH, Wu PT, Wu KC, Hsieh JL, Jou IM.. The estrogen receptor-β expression in de Quervain’s disease. Int J Mol Sci 2015;16(11):26452-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ilyas AM, Ast M, Schaffer AA, Thoder J.. De Quervain tenosynovitis of the wrist. J Am Acad Orthop Surg 2007;15(12):757-64. Erratum in: J Am Acad Orthop Surg 2008;16(2): 35A. [DOI] [PubMed] [Google Scholar]
- 23.Ashraf MO, Devadoss VG.. Systematic review and meta-analysis on steroid injection therapy for de Quervain’s tenosynovitis in adults. Eur J Orthop Surg Traumatol 2014;24(2):149-57. Epub 2013 Jan 22. [DOI] [PubMed] [Google Scholar]
- 24.Abi-Rafeh J, Kazan R, Safran T, Thibaudeau S.. Conservative management of de Quervain stenosing tenosynovitis: review and presentation of treatment algorithm. Plast Reconstr Surg 2020;146(1):105-26. [DOI] [PubMed] [Google Scholar]
- 25.Blazar PE, Floyd WE 4th, Han CH, Rozental TD, Earp BE.. Prognostic indicators for recurrent symptoms after a single corticosteroid injection for carpal tunnel syndrome. J Bone Joint Surg Am 2015;97(19):1563-70. [DOI] [PubMed] [Google Scholar]
- 26.Patrick NC, Hammert WC.. Hand and wrist tendinopathies. Clin Sports Med 2020;39(2):247-58. [DOI] [PubMed] [Google Scholar]
- 27.Sato J, Ishii Y, Noguchi H.. Diagnostic performance of the extensor carpi ulnaris (ECU) synergy test to detect sonographic ECU abnormalities in chronic dorsal ulnar-sided wrist pain. J Ultrasound Med 2016;35(1):7-14. Epub 2015 Nov 20. [DOI] [PubMed] [Google Scholar]
- 28.Wagner ER, Gottschalk MB.. Tendinopathies of the forearm, wrist, and hand. Clin Plast Surg 2019;46(3):317-27. Epub 2019 Apr 12. [DOI] [PubMed] [Google Scholar]
- 29.Campbell D, Campbell R, O’Connor P, Hawkes R.. Sports-related extensor carpi ulnaris pathology: a review of functional anatomy, sports injury and management. Br J Sports Med 2013;47(17):1105-11. Epub 2013 Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I.. Prevalence of carpal tunnel syndrome in a general population. JAMA 1999;282(2):153-8. [DOI] [PubMed] [Google Scholar]
- 31.Durkan JA. A new diagnostic test for carpal tunnel syndrome. J Bone Joint Surg Am 1991;73(4):535-8. Erratum in: J Bone Joint Surg Am 1992;74(2): 311. [PubMed] [Google Scholar]
- 32.Page MJ, Massy-Westropp N, O’Connor D, Pitt V.. Splinting for carpal tunnel syndrome. Cochrane Database Syst Rev 2012;(7):CD010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Calandruccio JH, Thompson NB.. Carpal tunnel syndrome: making evidence-based treatment decisions. Orthop Clin North Am 2018;49(2):223-9. Epub 2018 Feb 1. [DOI] [PubMed] [Google Scholar]
- 34.Head L, Gencarelli JR, Allen M, Boyd KU.. Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am 2015;40(3):546-53.e8. [DOI] [PubMed] [Google Scholar]
- 35.Hung EHY, Griffith JF, Ng AWH, Lee RKL, Lau DTY, Leung JCS.. Ultrasound of musculoskeletal soft-tissue tumors superficial to the investing fascia. AJR Am J Roentgenol 2014;202(6):W532-40. [DOI] [PubMed] [Google Scholar]
- 36.Expert Panel on Musculoskeletal Imaging; Torabi M, Lenchik L, Beaman FD, Wessell DE, Bussell JK, et al. . ACR Appropriateness Criteria® acute hand and wrist trauma. J Am Coll Radiol 2019;16(5S):S7-17. [DOI] [PubMed] [Google Scholar]
- 37.Dao KD, Solomon DJ, Shin AY, Puckett ML.. The efficacy of ultrasound in the evaluation of dynamic scapholunate ligamentous instability. J Bone Joint Surg Am 2004;86(7):1473-8. [DOI] [PubMed] [Google Scholar]
- 38.Rüegger C, Schmid MR, Pfirrmann CWA, Nagy L, Gilula LA, Zanetti M.. Peripheral tear of the triangular fibrocartilage: depiction with MR arthrography of the distal radioulnar joint. AJR Am J Roentgenol 2007;188(1):187-92. [DOI] [PubMed] [Google Scholar]
- 39.Starr HM Jr, Sedgley MD, Means KR Jr, Murphy MS.. Ultrasonography for hand and wrist conditions. J Am Acad Orthop Surg 2016;24(8):544-54. [DOI] [PubMed] [Google Scholar]