Before measles vaccine was introduced, around 5.7 million people worldwide died each year of measles; by 1995 this total had fallen by 88%.1 In Latin America, measles incidence and mortality fell by 99% after vaccination was introduced. As a result, an international meeting in July 1996 recommended a global programme of measles eradication by a target date between 2005 and 2010.2 We discuss whether such a goal is feasible and appropriate.
Case for eradicating measles
Reducing mortality due to measles is a public health priority in developing countries. Measles eradication—defined as the interruption in the transmission of measles globally so that vaccination can be stopped—is possible theoretically because no animal reservoir is known to exist and measles vaccine is highly effective.2,3 Eradication of the measles virus would obviate the need for the continuous monitoring of changes in measles epidemiology (and responses to this) induced by measles vaccination.4,5 These epidemiological changes include a shift in the age distribution of measles towards older children and adults6,7; the occurrence of “post honeymoon” outbreaks, when numbers of susceptible people grow over years of moderate vaccination coverage until their total surpasses the epidemic threshold5,6,8; and the fact that babies born to mothers whose immunity is not natural but induced by vaccine have a shorter period of passive protection.5,9
Do we need to know more?
The World Health Organisation recommends that countries aiming to eliminate measles adopt the strategy used in Latin America of an initial catch-up campaign, with high coverage of routine infant vaccination, intensive surveillance, and periodic follow up campaigns.2,10 However, questions remain on which age range to vaccinate in campaigns, maintaining safe injection practices, and the feasibility and cost of achieving high enough coverage in the poorest countries. Cost-benefit analyses need to compare programmes that aim to eradicate measles and those whose aim is control. Furthermore, the effects on social development in poor countries of diverting resources to a measles eradication programme must be assessed.
Summary points
Dramatic progress in reducing measles incidence and mortality in many parts of the world has recently led to calls for a global programme of eradication in the next 10 to 15 years
Mass catch-up campaigns are being conducted—in some countries the aim is to interrupt measles transmission and in others to increase immunisation coverage rapidly
Questions remain on the age range that should be included in catch-up campaigns, maintaining safe injection practices, and the feasibility and costs of achieving high enough coverage in poor countries
Cost-benefit analyses of programmes to eradicate and to control measles are needed
Effects on social development of diverting funds into programmes to eradicate measles must be assessed in poorer countries
The international health and development community must address these issues and set priorities before declaring goals and time limits for global eradication of measles
Age range
What age range should be included in catch-up campaigns? In Latin America, the age group 1-14 years was selected because catch-up campaigns were being carried out about 15 years after large scale vaccination programmes had begun, and disease surveillance showed few cases of measles in older people.10 In many countries, measles surveillance is not good enough to inform decisions on which age group to vaccinate. In countries where vaccination coverage is low and the incidence of measles is high, school children are likely to have natural immunity, and targeting an age range narrower than 1-15 years might be as effective and less costly. Conversely, in sparsely populated areas such as the Sahel in west Africa, many adults may be susceptible, and vaccinating a wider age range may be appropriate.11 Without adequate geographical data on trends in susceptibility to measles, predicting the cost effectiveness of simply adopting the age range used in Latin America is difficult.
Safe injection practices
Can safe injection practices be guaranteed if widespread campaigns are conducted now? In 1994, the WHO reported that up to a third of immunisation injections in four of its six regions were unsterile, carrying the risk of iatrogenic infections, including fatal septicaemia, and transmission of bloodborne pathogens.12 Technological developments, such as autodestruct syringes, that make injections safer are costly, and proper collection and destruction of used needles is difficult.13 Alternative methods of vaccine administration, including improved jet injectors and delivery via aerosol or intranasal routes, are under development and evaluation but do not offer a solution in the short term.14,15
Vaccination coverage in poor countries
What degree of coverage is feasible in the poorest countries? For the incidence of measles to fall towards zero, it is estimated that more than 90% (and possibly more than 95%) of the population must be immune.16 In Latin America, coverage greater than 90% was achieved in campaigns.10 In the polio eradication programme, poor countries are achieving coverage of over 80% for oral polio vaccine on national immunisation days (Children’s Vaccination Initiative, unpublished data, 1996). Measles campaigns are more challenging, however, because the target population is three or four times larger (polio campaigns target children less than 5 years of age since older children have natural immunity), and trained health workers are needed as the vaccine is given by injection.
In 1995, 32 countries reported measles vaccine coverage levels below 60% (WHO; unpublished data, 1996). A short but intensive effort to eradicate measles might be more feasible, therefore, than achieving and sustaining the high coverage needed for measles control. In Haiti, for example, reported coverage of routine infant immunisation is only 23%, but 94% of children aged 1-14 years were immunised in the 1994 campaign.10 In countries where the coverage of routine vaccination is low, however, follow up campaigns might need to be repeated every year or two to prevent the resurgence of measles. Whether the poorest countries can achieve sufficiently high coverage in successive campaigns is unknown.
Reducing measles mortality in Africa—areas requiring simultaneous investment
Infrastructure for routine health services in the poorest countries must be strengthened
Research is needed to develop better ways of delivering vaccine and field laboratory assays to improve surveillance
Basic research should be conducted to further our understanding of the long term effects of measles infection and vaccination in these countries
Cost-benefit analysis
What is the marginal cost-benefit of measles eradication compared with measles control? Measles control by immunisation has a high benefit-cost ratio in industrialised countries.17 In developing countries, where measles case fatality ratios are up to 100-fold higher, mortality can be reduced to very low levels by control programmes that sustain high immunisation coverage of infants.6,18 The measles case fatality ratio also falls as the socioeconomic status of a population increases.19 Assessing the marginal benefits and costs of measles eradication compared with measles control in different settings is important.
The major additional benefits from measles eradication are predicted to be further savings on treatment of patients with measles and savings achieved by stopping measles surveillance and vaccination.3 However, the appropriateness of stopping measles vaccination after eradication has been questioned. Aaby et al report that measles immunisation reduces overall child mortality through non-specific beneficial effects of the vaccine over and above the avoidance of measles or its complications. They suggest, therefore, that measles vaccination should be continued even if measles is eradicated.20
The marginal costs of eradication include the costs of public health campaigns, the additional vaccine and syringe costs, and any potential increase in health risks associated with the injection. The costs of the intensive surveillance, case investigation, and outbreak response components of eradication strategies will probably be high in countries with a poor health service infrastructure. The opportunity costs of investing in the extra activities required for measles eradication should also be reviewed in the context of competing health priorities such as introducing hepatitis B and other new vaccines.
Effects on social development
Would an eradication programme have effects on social development in poor countries? Official development assistance worldwide is at its lowest level in real terms for 25 years.21 Knowing whether eradication programmes stimulate increased assistance for social development or compete for scarce resources is essential. An exciting eradication programme might attract new funds that would not otherwise be available. External donors supplied more than $25 million for Africa’s national immunisation days in 1996, and a consortium of vaccine manufacturers will donate 100 million doses of polio vaccine plus $1 million to support polio surveillance in the region (Children’s Vaccine Initiative, unpublished data, 1996). Systems must be established to show whether funds generated for eradication programmes are additional or are diverted from other programmes and to monitor the effect of specifically targeted expenditure on the overall development of health and social services.22
What should be done now?
Measles is currently estimated to cause almost 800 000 deaths a year, 500 000 of which occur in Africa.1 Average reported coverage of measles vaccine in 1995 was only 53% in western Africa and 38% in central Africa.23 Reducing measles mortality in these regions is a priority. Ideally, resources should be invested simultaneously in several areas of endeavour (box).
The feasibility and cost of developing safe methods of delivering measles vaccine in global campaigns—and a realistic schedule—need to be determined in consultation with the private sector. The coverage that can be achieved safely and effectively in campaigns should be determined in the most difficult settings. The marginal costs and benefits of measles eradication should be estimated, and it also makes sense to include an analysis of a potential combined programme against measles, mumps, and rubella. Consensus should be sought from immunologists and virologists on the long term effects of measles vaccines and the implications of stopping vaccination should measles be eradicated. Lastly, coordinated processes of funding and accountability should be developed to monitor not only the investment in disease eradication programmes but also the effect of such programmes on social development in the poorest countries. We need answers to these questions before the declaration of an eradication goal sets severe time constraints on the search for informed solutions.
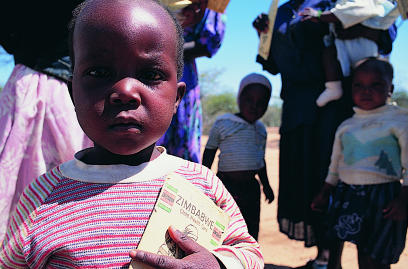
Figure.
Measles causes 800 000 deaths each year worldwide—500 000 of them are in Africa
Acknowledgments
We thank Professor Paul Fine, London School of Hygiene and Tropical Medicine, and Dr Ron Waldman, BASICS, for helpful comments on earlier drafts of this paper.
References
- 1.Global Programme for Vaccines and Immunisation. Progress of vaccine research and development and plan of activities—1996. Geneva: WHO, 1996.
- 2.Expanded Programme on Immunisation. Meeting on advances in measles elimination: conclusions and recommendations. Weekly Epidemiol Rec 1996;71:305-12. [PubMed]
- 3.Hopkins DR, Hinman AR, Koplan JP, Lane JM. The case for global measles eradication. Lancet. 1982;i:1396–1398. doi: 10.1016/s0140-6736(82)92510-7. [DOI] [PubMed] [Google Scholar]
- 4.Cutts FT, Markowitz LE. Successes and failures in measles control. J Infect Dis. 1994;170:S1–10. doi: 10.1093/infdis/170.supplement_1.s32. [DOI] [PubMed] [Google Scholar]
- 5.McLean AR. After the honeymoon in measles control. Lancet. 1995;345:272. doi: 10.1016/s0140-6736(95)90272-4. [DOI] [PubMed] [Google Scholar]
- 6.Cutts FT, Henderson RH, Clements CJ, Chen RT, Patriarca PA. Principles of measles control. Bull WHO. 1991;69:1–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Gay NJ, Hesketh LM, Morgan-Capner P, Miller E. Interpretation of sero-logical surveillance data for measles using mathematical models: implications for vaccine strategy. Epidemiol Infect. 1995;115:139–156. doi: 10.1017/s0950268800058209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McLean AR, Anderson RM. Measles in developing countries. Part II. The predicted impact of mass vaccination. Epidemiol Infect. 1987;100:419–441. doi: 10.1017/s0950268800067170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulholland K. Measles and pertussis in developing countries with good vaccine coverage. Lancet. 1995;345:305–307. doi: 10.1016/s0140-6736(95)90282-1. [DOI] [PubMed] [Google Scholar]
- 10.De Quadros CA, Olivé JM, Hersh BS, Strassburg MA, Henderson DA, Brandling-Bennett D, et al. Measles elimination in the Americas. Evolving strategies. JAMA. 1996;275:224–229. doi: 10.1001/jama.275.3.224. [DOI] [PubMed] [Google Scholar]
- 11.Loutan L, Paillard S. Measles in a west African nomadic community. Bull WHO. 1992;70:741–744. [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organisation, UNICEF. State of the world’s vaccines and immunisation. Geneva: WHO, 1996: 1-161.
- 13.Steinglass R, Boyd D, Grabowsky M, Laghari AG, Khan MA, Qavi A, et al. Safety, effectiveness and ease of use of a non-reusable syringe in a developing country immunisation programme. Bull WHO. 1995;73:57–63. [PMC free article] [PubMed] [Google Scholar]
- 14.Aylward B, Lloyd J, Zaffran M, McNair-Scott R, Evans P. Reducing the risk of unsafe injections in immunisation programmes: financial and operational implications of various injection technologies. Bull WHO. 1995;73:531–540. [PMC free article] [PubMed] [Google Scholar]
- 15.Cutts FT, Clements CJ, Bennett JV. Alternative routes of measles immunisation: a review. Biologicals. 1997;25:323–338. doi: 10.1006/biol.1997.0103. [DOI] [PubMed] [Google Scholar]
- 16.Fine PEM. Herd immunity: history, theory, practice. Epidemiol Rev. 1993;15:265–302. doi: 10.1093/oxfordjournals.epirev.a036121. [DOI] [PubMed] [Google Scholar]
- 17.White CC, Koplan JP, Orenstein WA. Benefits, risks and costs of immunisation for measles, mumps and rubella. Am J Public Health. 1985;75:739–744. doi: 10.2105/ajph.75.7.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cutts FT, Monteiro O, Tabard P, Cliff J. Measles control in Maputo, Mozambique, using a single dose of Schwarz vaccine at age 9 months. Bull WHO. 1994;72:227–231. [PMC free article] [PubMed] [Google Scholar]
- 19.Aaby P, Bukh J, Lisse IM, Smits AJ. Severe measles in Sunderland, 1885: a European-African comparison of causes of severe infection. Int J Epidemiol. 1986;15:101–107. doi: 10.1093/ije/15.1.101. [DOI] [PubMed] [Google Scholar]
- 20.Aaby P, Samb B, Simondon F, Seck AMC, Knudsen K, Whittle H. Non-specific beneficial effect of measles immunisation: analysis of mortality studies from developing countries. BMJ. 1995;311:481–485. doi: 10.1136/bmj.311.7003.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nelson EAS, Yu LM. Poverty focused assistance: new category of development aid. Lancet. 1996;348:1642–1643. doi: 10.1016/s0140-6736(96)06389-1. [DOI] [PubMed] [Google Scholar]
- 22.Taylor C, Cutts F, Taylor M. Ethical dilemmas in current planning for polio eradication. Am J Public Health. 1997;87:922–925. doi: 10.2105/ajph.87.6.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Expanded Programme on Immunisation. Measles control in the WHO African Region. Weekly Epidemiol Rec 1996;26:201-3. [PubMed]