Abstract
Importance
Large-scale estimates of bronchopulmonary dysplasia (BPD) are warranted for adequate prevention and treatment. However, systematic approaches to ascertain rates of BPD are lacking.
Objective
To conduct a systematic review and meta-analysis to assess the prevalence of BPD in very low birth weight (≤ 1,500 g) or very low gestational age (< 32 weeks) neonates.
Data sources
A search of MEDLINE from January 1990 until September 2019 using search terms related to BPD and prevalence was performed.
Study selection
Randomized controlled trials and observational studies evaluating rates of BPD in very low birth weight or very low gestational age infants were eligible. Included studies defined BPD as positive pressure ventilation or oxygen requirement at 28 days (BPD28) or at 36 weeks postmenstrual age (BPD36).
Data extraction and synthesis
Two reviewers independently conducted all stages of the review. Random-effects meta-analysis was used to calculate the pooled prevalence. Subgroup analyses included gestational age group, birth weight group, setting, study period, continent, and gross domestic product. Sensitivity analyses were performed to reduce study heterogeneity.
Main outcomes and measures
Prevalence of BPD defined as BPD28, BPD36, and by subgroups.
Results
A total of 105 articles or databases and 780,936 patients were included in this review. The pooled prevalence was 35% (95% CI, 28-42%) for BPD28 (n = 26 datasets, 132,247 neonates), and 21% (95% CI, 19-24%) for BPD36 (n = 70 studies, 672,769 neonates). In subgroup meta-analyses, birth weight category, gestational age category, and continent were strong drivers of the pooled prevalence of BPD.
Conclusions and relevance
This study provides a global estimation of BPD prevalence in very low birth weight/low gestation neonates.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12931-024-02850-x.
Keywords: Bronchopulmonary dysplasia, Chronic lung disease, Rates, Prevalence, Meta-analysis
Introduction
Bronchopulmonary dysplasia (BPD), characterized as an arrest of lung growth and development, is an important cause of morbidity and mortality in very preterm newborns [1]. While interventions in neonatal care have led to survival of smaller and younger neonates, therapies for BPD are still limited [2]. Therefore, there is an urgent need for early prediction of BPD and implementation of strategies and therapies that can attenuate disease progression. To accomplish such endeavors, we must first ascertain large-scale estimates of BPD and its global impact over time. In doing so, the effect of interventions and progress towards reducing rates of BPD can be more readily measured. Valid and consistent estimates of the prevalence of BPD around the globe are largely lacking.
A previous study estimated global rates of BPD; however, the definition of BPD was not determined a priori and the estimation was reported as a set of ranges per country as opposed to a pooled rate [3]. Challenges to estimating comprehensive rates of BPD include the varying definitions (e.g., 28 day versus 36 week assessment [4, 5]), as well as the heterogeneous inclusion criteria of preterm neonates in studies (e.g., gestational-based inclusion compared to birth weight-based parameters or a combination of both). To overcome these barriers, we sought to conduct a systematic review and meta-analysis that would: (i) estimate global trends in the prevalence of BPD, (ii) examine temporal changes in BPD rates, and (iii) stratify BPD rates according to definition, birth weight, gestational age, setting, continent, and gross domestic product (GDP).
Methods
We conducted a systematic review and meta-analysis according to recommendations from the Cochrane Handbook for Systematic Reviews of Interventions and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria [6]. A protocol of this review was not registered.
Search strategy
Two investigators (A.M. and M.N.) systematically searched MEDLINE from January 1990 to September 30th, 2019. Search terms included (bronchopulmonary dysplasia OR chronic lung disease) AND a list of each country. Articles were filtered to include children between the age range of birth and 1 month post-term, no limits were placed on language, and refined to remove review articles. Furthermore, review of references from included studies was performed to supplement our initial search. The full search strategy is presented in eMethods 1 in the Supplement. Lastly, we reviewed all the population-based articles from a systematic review by Siffel et al. [3] wherein they examined global rates of BPD. To enhance the comprehensiveness of our investigation, we integrated national registries from countries that were publicly available documenting outcomes related to BPD.
Study selection
Two groups of investigators (group 1: A.T. and M.N.; group 2: A.N. and A.M) independently reviewed the titles and abstracts of all citations to determine suitability for inclusion. This was followed by independent review of the full-text articles to confirm eligibility. A third author (S.Z.) resolved any disagreements. Studies were included if they were international or national level (e.g., population-based) studies reporting rates of BPD from 1990 to 2019. The search was initiated from 1990, as this marks the time when surfactant therapy became increasingly standard of care in neonatal centers [7]. The end date was chosen as 2019 to exclude publications using the newest definition for BPD [8]. We included data for all neonates at risk for BPD with confirmed diagnosis occurring in the hospital or prior to discharge. Studies with inclusion criteria of male and female neonates with a birth weight of less than or equal to 1,500 g or a gestational age of less than 32 weeks were included. Due to limited availability of granular patient-level data in the included studies, mortality rates for each study were collected. Case reports, editorials, and commentaries were excluded.
Data extraction
Two sets of authors (A.T. and M.N.; A.N. and A.M.) independently collected study details. Two authors (J.J. and S.Z.) independently verified the accuracy of collated information. Inconsistencies were discussed among a panel of at least four investigators. Study specifics included country, BPD definition, BPD rates, total number of neonates in the study, years of observation, inclusion criteria, and study design. Articles and standardized data collection sheets were maintained in Google Drive folders. GetData Graph Digitizer version 2.26.0.20 was used to collect values from figures when mortality data was not described in the article text.
Risk of bias
The risk of bias was judged in a binary fashion (e.g., yes = 1 or no = 0). We assessed the risk of bias for observational studies according to the Newcastle-Ottawa Quality Assessment Scale in three dimensions, selection, comparability, and outcome. The score for observational studies ranged from 0 to 8, representing bias risk for each article. Studies were defined as having a high risk of bias if the total score was five or lower, moderate risk of bias if the score was between five and six, and low bias if the total summed to greater than seven. We assessed the risk of bias for controlled studies according to the Cochrane Risk of Bias Tool using seven dimensions, selection bias (including random sequence generation and allocation concealment), reporting bias, other bias, performance bias, detection bias, and attrition bias. The score for randomized controlled studies ranged from 0 to 7, representing bias risk for each article.
Definitions and outcomes
A priori, BPD was defined by two categories: (i) BPD28- supplemental oxygen or positive pressure ventilation at 28 days of life, and (ii) BPD36- supplemental oxygen or positive pressure ventilation at 36 weeks postmenstrual age. The pooled prevalence of BPD is presented as forest plots for BPD28 and BPD36. If the study stratified patient numbers by both definitions, we included both to each pooled rate. When articles overlapped in time period for a particular country, the articles with more comprehensive data were selected for inclusion. Prespecified subgroup analyses included birth weight categories, gestational age, years, setting, continent, and gross domestic product (GDP). Precisely, gestational age was divided into extremely low gestational age (ELGA) (≤ 28 weeks) vs. very low gestational age (VLGA) (< 32 weeks), while study setting was stratified into international or national. Study years were binned into three decades: 1990–1999, 2000–2009, 2010–2019. This approach was used to explore temporal changes in BPD. The year 1990 was used as the time of inception as the late 1980s and early 1990s is when clinical trials for surfactant use demonstrated efficacy in the care of preterm neonates with respiratory distress syndrome. Birth weight was sorted into extremely low birth weight (ELBW) (≤ 1,000 g), very low birth weight (VLBW) (≤ 1,500 g), and modifications of these terms (e.g., 501–750 g, 751–1000 g, 1001–1250 g, and 1251–1500 g). To clarify, the subgroup analysis by birth weight of 1000 g was conducted by categorizing studies based on the specified birth weight ranges. Specifically, studies were included in this subgroup analysis if they reported data on all infants falling within the designated birth weight range of interest and not average birthweight reported for a cohort.
Statistical analysis
The primary outcome was expressed using direct proportions (PR) with a 95% confidence interval (CI) following Freeman-Tukey double arc-sine transformation of the raw data [9]. Expecting high heterogeneity, defined as an I2#x2009;> 50%, all analyses used a DerSimonian–Laird estimate with a random-effects meta-analysis model. The presence of publication bias was evaluated qualitatively using funnel plots and quantitatively conducing Egger’s linear regression test. At least ten studies were needed to perform subgroup analyses. All statistical analyses were performed using R version 4.1.0.
Results
Identification of Eligible studies
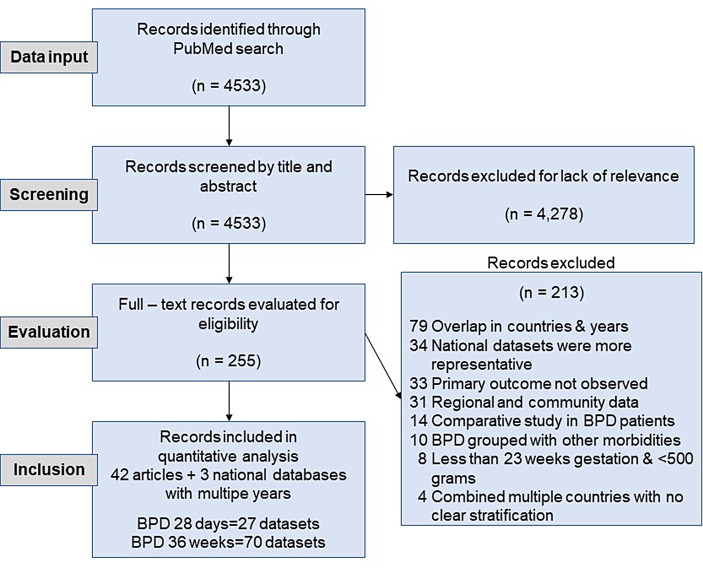
Our search yielded 4582 records, of which 2318 were reviewed in full. After applying the eligibility criteria, a total of 42 were included in this review. We also identified three publicly available national datasets: Australian and New Zealand Neonatal Network, Canadian Neonatal Network, and Neonatal Research Network of Japan Database. Meta-analyses were performed on all studies and databases, moving forward now referred to as datasets. In sum, a combination of 74 datasets comprised the analysis for BPD28 and BPD26 as well as their subgroup analyses. The flow diagram of selected articles is shown in Fig. 1.
Fig. 1.
Life satisfaction scores at age 30. 12 = highest possible score. 3 = Lowest possible score
Figure 1 PRISMA flowchart of literature identification and study selection.
Study characteristics
Table 1 provides detailed characteristics of the included articles. All the chosen articles were based on cohort investigations and on the two predetermined BPD definitions: BPD28 and BPD36. The most commonly used definition for BPD was BPD36. Thirty countries were represented in the studies, and the countries that produced the most data were Australia and New Zealand (n = 24/70 datasets, 34.3%). A total of 672,769 patients were included in this review. Twenty-six out of the 70 datasets (37.1%) in BPD36 were published from 2010 onwards.
Table 1.
Study characteristics of included articles
| Article No. | Author | Country | Data years | Number of BPD patients | Number of patients | Definition of BPD | Type of representativeness |
|---|---|---|---|---|---|---|---|
| 1 | Álvarez-Fuente | Spain | 2013 | 917 | 2628 | O2 at 28 days | National |
| 2 | Ancel | France | 2011 | 251 | 4308 | O2 at 36 weeks | National |
| 3 | Bevilacqua | Italy | 1996 | 47 | 268 | O2 at 28 days | National |
| 4 | Bonamy | Belgium, Denmark, Estonia, France, Germany, Italy, Netherlands, Poland, Portugal, UK, Sweden | 2011–2012 | 94 | 1951 | O2 at 36 weeks | Multinational |
| 5 | Chen | Switzerland | 2000–2012 | 840 | 8899 | O2 at 36 weeks | National |
| 6 | Choi | Korea | 2007–2008 | 1191; 685 | 3841 | O2 at 28 days and 36 weeks | National |
| 7 | Fanaroff | United States | 1991–1992 | 1284; 771 | 4279 | O2 at 28 days and 36 weeks | National |
| 8 | Fanaroff | United States | 1997–2002 | 5151; 4224 | 18,153 | O2 at 28 days and 36 weeks | National |
| 9 | Fortmann | Germany | 2009–2015 | 2118 | 13,343 | O2 at 36 weeks | National |
| 10 | Gortner | Belgium, Denmark, France, Germany, Italy, Poland, Portugal, UK | 2003 | 285 | 1603 | O2 at 36 weeks | Multinational |
| 11 | Grandi | Argentina, Brazil, Chile, Paraguay, Peru, Uruguay | 2001–2010 | 2768; 1861 | 11,332 | O2 at 28 days and 36 weeks | Multinational |
| 12 | Grisaru-Granovsky | Israel | 1995–2007 | 1152 | 7913 | O2 at 28 days | National |
| 13 | Guimarães | Portugal | 2004–2006 | 33 | 256 | O2 at 36 weeks | National |
| 14 | Guinsberg | Brazil | 2012–2013 | 497 | 2646 | O2 at 36 weeks | National |
| 15 | Hentschel | Switzerland | 1996&2000 | 184 | 1236 | O2 at 36 weeks | National |
| 16 | Horbar | United States | 2005–2014 | 95,260 | 327,840 | O2 at 36 weeks | National |
| 17 | Kamper | Denmark | 1994–1995 | 43 | 269 | O2 at 36 weeks | National |
| 18 | Koc | Turkey | 2016–2017 | 800 | 3381 | O2 at 36 weeks | National |
| 19 | Kong | China | 2013–2014 | 200 | 1749 | O2 at 28 days | National |
| 20 | Kusuda | Japan | 2003 | 601 | 2145 | O2 at 36 weeks | National |
| 21 | Lee | Canada | 1996–1997 | 1011 | 3494 | O2 at 36 weeks | National |
| 22 | Lee | South Korea | 2013–2016 | 2440 | 7441 | O2 at 36 weeks | National |
| 23 | Lemons | United States | 1995–1996 | 1598; 1021 | 4438 | O2 at 28 days and 36 weeks | National |
| 24 | Marret | France | 1997–2002 | 89 | 1638 | O2 at 28 days | National |
| 25 | Murphy | Ireland | 2004–2007 | 529 | 2889 | O2 at 36 weeks | Multinational |
| 26 | Persson | Canada, Finland, Israel, Italy, Japan, Sweden, UK | 2007–2015 | 19,155 | 76,360 | O2 at 36 weeks | Multinational |
| 27 | Qiu | Canada | 2005 | 717 | 3242 | O2 at 36 weeks | National |
| 28 | Rodrigo | Spain | 2002–2006; 2007–2011 | 369 | 2485 | O2 at 36 weeks | National |
| 29 | Rutkowska | Poland | 2014–2015 | 319 | 707 | O2 at 36 weeks | National |
| 30 | Sasaki | Japan | 2003–2008 | 5354 | 15,765 | O2 at 28 days | National |
| 31 | Skromme | Norway | 1999–2000 | 165 | 372 | O2 at 36 weeks | National |
| 32 | Stensvold | Norway | 2013–2014 | 78 | 185 | O2 at 36 weeks | National |
| 33 | Stevenson | United States | 1993–1994 | 1424; 260 | 4593; 999 | O2 at 28 days and 36 weeks | National |
| 34 | Su | Taiwan | 1997–2011 | 3193 | 10,479 | O2 at 36 weeks | National |
| 35 | Toome | Estonia | 2002–2003; 2007–2008 | 115 | 601 | O2 at 36 weeks | National |
| 36 | Tsou | Taiwan | 1997–2011 | 113 | 485 | O2 at 28 days | National |
| 37 | Tyson | United States | 1996–1997 | 534 | 807 | O2 at 2836 weeks | National |
| 38 | Vanhaesebrouck | Belgium | 1999–2000 | 143; 78 | 175 | O2 at 28 days and 36 weeks | National |
| 39 | Waal | Netherlands | 2007 | 35 | 144 | O2 at 36 weeks | National |
| 40 | Walsh | United States and Canada | 2001&2003 | 21,739 | 75,974 | O2 at 36 weeks | Multinational |
| 41 | Watson | England | 2009–2011 | 6551 | 20,554 | O2 at 28 days | National |
| 42 | Weber | Austria | 1999–2001 | 95 | 321 | O2 at 36 weeks | National |
| 43 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 1995 | 512 | 2863 | O2 at 36 weeks | Multinational |
| 44 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 1996 | 501 | 2964 | O2 at 36 weeks | Multinational |
| 45 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 1997 | 549 | 2979 | O2 at 36 weeks | Multinational |
| 46 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 1998 | 577 | 3084 | O2 at 36 weeks | Multinational |
| 47 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 1999 | 643 | 2883 | O2 at 36 weeks | Multinational |
| 48 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2000 | 752 | 2972 | O2 at 36 weeks | Multinational |
| 49 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2001 | 740 | 2924 | O2 at 36 weeks | Multinational |
| 50 | Report of the Au3349stralian and New Zealand Neonatal Network | Australia and New Zealand | 2002 | 692 | 2944 | O2 at 36 weeks | Multinational |
| 51 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2003 | 621 | 2607 | O2 at 36 weeks | Multinational |
| 52 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2004 | 673 | 3204 | O2 at 36 weeks | Multinational |
| 53 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2005 | 623 | 3349 | O2 at 36 weeks | Multinational |
| 54 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2006 | 476 | 3084 | O2 at 36 weeks | Multinational |
| 55 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2007 | 585 | 3439 | O2 at 36 weeks | Multinational |
| 56 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2008 | 624 | 3666 | O2 at 36 weeks | Multinational |
| 57 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2009 | 634 | 3552 | O2 at 36 weeks | Multinational |
| 58 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2010 | 720 | 3273 | O2 at 36 weeks | Multinational |
| 59 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2011 | 1574;747 | 3536;3736 | O2 at 28 days and 36 weeks | Multinational |
| 60 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2012 | 1067;782 | 3348;3520 | O2 at 28 days and 36 weeks | Multinational |
| 61 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2013 | 1218;792 | 2985;3501 | O2 at 28 days and 36 weeks | Multinational |
| 62 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2014 | 1261;871 | 3058;3615 | O2 at 28 days and 36 weeks | Multinational |
| 63 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2015 | 885 | 3449 | O2 at 36 weeks | Multinational |
| 64 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2016 | 1698;1028 | 3385;3610 | O2 at 28 days and 36 weeks | Multinational |
| 65 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2017 | 1728;988 | 3263;3262 | O2 at 28 days and 36 weeks | Multinational |
| 66 | Report of the Australian and New Zealand Neonatal Network | Australia and New Zealand | 2018 | 1721;984 | 3211;3417 | O2 at 28 days and 36 weeks | Multinational |
| 67 | Canadian Neonatal Network | Canada | 2004 | 175 | 687 | O2 at 36 weeks | National |
| 68 | Canadian Neonatal Network | Canada | 2006 | 298 | 958 | O2 at 36 weeks | National |
| 69 | Canadian Neonatal Network | Canada | 2016 | 811 | 1954 | O2 at 36 weeks | National |
| 70 | Canadian Neonatal Network | Canada | 2017 | 812 | 1963 | O2 at 36 weeks | National |
| 71 | Canadian Neonatal Network | Canada | 2018 | 1223 | 4023 | O2 at 36 weeks | National |
| 72 | Neonatal Research Network of Japan Database | Japan | 2016 | 1473;727 | 3982;3030 | O2 at 28 days and 36 weeks | National |
| 73 | Neonatal Research Network of Japan Database | Japan | 2017 | 1174;718 | 3354;3262 | O2 at 28 days and 36 weeks | National |
| 74 | Neonatal Research Network of Japan Database | Japan | 2018 | 1438;873 | 3507;3010 | O2 at 28 days and 36 weeks | National |
Pooled and stratified prevalence of BPD
The pooled prevalence for BPD28 calculated from 27 datasets and 132,424 neonates was 35% (95% CI, 0.28–0.42) using random effects meta-analysis (Fig. 2). For BPD36 (n = 70 studies, 672,769 neonates), the pooled prevalence was 21% (95% CI, 0.19–0.24) (Fig. 3). Table 2 depicts the prevalence of BPD28 and BPD36 according to gestational age, birth weight, study period, continent, setting, and GDP (subgroup analysis).
Table 2.
Rates of BPD28 and BPD36 using subgroup meta-analysis
| Variable | No. of Datasets |
No. of Cases | No. of Participants | Prevalence (95% CI) |
I^2 | p value |
|---|---|---|---|---|---|---|
| Global analysis for BPD | ||||||
| BPD 28 day | 26 | 42,868 | 132,247 | 0.35 (0.28–0.42) | 0.99 | < 0.01 |
| BPD 36 weeks | 70 | 178,044 | 672,769 | 0.21 (0.19–0.24) | 0.99 | < 0.01 |
| Subgroup analysis for BPD 28 day | ||||||
| Birthweight | ||||||
| <500 g | 6 | 129 | 131 | 0.99 (0.97, 1.00) | 0.0 | 0.51 |
| 501–750 g | 11 | 6,593 | 9,263 | 0.87 (0.75–0.96) | 1.00 | < 0.01 |
| 751–1000 g | 11 | 7,210 | 12,005 | 0.74 (0.62–0.84) | 1.00 | < 0.01 |
| 1001–1250 g | 11 | 4,434 | 13,454 | 0.41 (0.31–0.52) | 1.00 | < 0.01 |
| 1251–1500 g | 11 | 2,187 | 16,367 | 0.16 (0.11–0.22) | 0.99 | < 0.01 |
| <=1000 g | 1 | 534 | 807 | 0.66 (0.63–0.69) | -- | -- |
| <=1500 g | 7 | 14,144 | 47,355 | 0.32 (0.25–0.41) | 1.00 | < 0.01 |
| Overall | 58 | 35,231 | 99,382 | 0.61 (0.58–0.63) | 1.00 | < 0.01 |
| Gestational age | ||||||
| ELGA | 9 | 7,119 | 8,161 | 0.90 (0.84–0.95) | 0.99 | < 0.01 |
| VLGA | 17 | 21,237 | 70,759 | 0.29 (0.22–0.38) | 1.00 | < 0.001 |
| Overall | 26 | 28,356 | 78,920 | 0.62 (0.56–0.68) | 1.00 | < 0.001 |
| Year | ||||||
| 1990–1999 | 5 | 4,887 | 14,385 | 0.36 (0.21–0.52) | 0.99 | < 0.01 |
| 2000–2009 | 2 | 6,545 | 19,606 | 0.33 (0.30–0.35) | 0.92 | < 0.01 |
| 2010–2019 | 12 | 15,469 | 38,006 | 0.39 (0.32–0.46) | 0.99 | < 0.001 |
| Overall | 19 | 26,902 | 71,997 | 0.34 (0.31–0.36) | 0.99 | 0.22 |
| Setting | ||||||
| National | 18 | 29,833 | 98,129 | 0.42 (0.35–0.50) | 1.00 | < 0.001 |
| Multinational | 8 | 13,035 | 34,118 | 0.32 (0.23–0.41) | 0.99 | < 0.001 |
| Overall | 26 | 42,868 | 132,247 | 0.38 (0.33–0.44) | 1.00 | 0.07 |
| Continent | ||||||
| Asia | 7 | 10,943 | 32,683 | 0.30 (0.22–0.38) | 1.00 | < 0.001 |
| Europe | 6 | 8,899 | 33,176 | 0.29 (0.10–0.53) | 1.00 | < 0.001 |
| North America | 5 | 9,991 | 32,270 | 0.38 (0.25–0.52) | 0.99 | < 0.01 |
| Oceania | 7 | 10,267 | 22,786 | 0.45 (0.39–0.51) | 0.99 | < 0.01 |
| South America | 1 | 2,768 | 11,332 | 0.24 (0.24–0.25) | -- | -- |
| Overall | 26 | 42,868 | 132,247 | 0.25 (0.24–0.26) | 1.00 | < 0.01 |
| GDP | ||||||
| 1st quartile (lowest) | 3 | 1,408 | 8,573 | 0.39 (0.05–0.81) | 0.99 | < 0.01 |
| 2nd quartile | 3 | 3,682 | 10,005 | 0.37 (0.29–0.45) | 0.99 | < 0.01 |
| 3rd quartile | 3 | 6,687 | 22,460 | 0.17 (0.05–0.35) | 1.00 | < 0.01 |
| 4th quartile (highest) | 3 | 2,957 | 10,010 | 0.25 (0.11–0.42) | 1.00 | < 0.001 |
| Overall | 12 | 14,734 | 51,048 | 0.33 (0.26–0.39) | 1.00 | 0.17 |
| Subgroup analysis for BPD 36 weeks | ||||||
| Birthweight | ||||||
| <500 g | 8 | 285 | 391 | 0.71 (0.51–0.87) | 0.91 | < 0.01 |
| 501–750 g | 15 | 3,877 | 7,330 | 0.60 (0.51–0.68) | 0.99 | < 0.01 |
| 751–1000 g | 15 | 4,400 | 10,585 | 0.43 (0.38–0.49) | 0.97 | < 0.01 |
| 1001–1250 g | 15 | 2,411 | 11,803 | 0.22 (0.18–0.26) | 0.95 | < 0.01 |
| 1251–1500 g | 15 | 1,291 | 14,293 | 0.10 (0.07–0.13) | 0.94 | < 0.01 |
| <=1000 g | 1 | 165 | 372 | 0.44 (0.39–0.49) | -- | -- |
| <=1500 g | 13 | 148,254 | 534,587 | 0.24 (0.20–0.27) | 1.00 | < 0.01 |
| Overall | 82 | 160,683 | 579,361 | 0.28 (0.26–0.30) | 0.99 | < 0.01 |
| Gestational age | ||||||
| ELGA | 29 | 110,462 | 358,636 | 0.43 (0.39–0.48) | 1.00 | < 0.001 |
| VLGA | 42 | 25,199 | 126,368 | 0.12 (0.10–0.14) | 0.99 | < 0.001 |
| Overall | 71 | 135,661 | 485,004 | 0.21 (0.19–0.23) | 1.00 | < 0.01 |
| Year | ||||||
| 1990–1999 | 10 | 5,888 | 28,252 | 0.21 (0.18–0.23) | 0.96 | < 0.01 |
| 2000–2009 | 23 | 9,893 | 48,359 | 0.20 (0.18–0.22) | 0.95 | < 0.01 |
| 2010–2019 | 26 | 17,440 | 69,244 | 0.22 (0.16–0.27) | 0.99 | < 0.001 |
| Overall | 59 | 33,221 | 145,855 | 0.20 (0.19–0.22) | 0.99 | 0.85 |
| Setting | ||||||
| National | 33 | 117,903 | 425,177 | 0.26 (0.23–0.30) | 1.00 | < 0.001 |
| Multinational | 37 | 60,662 | 247,592 | 0.18 (0.16–0.21) | 0.99 | < 0.001 |
| Overall | 70 | 178,565 | 672,769 | 0.21 (0.19–0.23) | 0.99 | < 0.01 |
| Continent | ||||||
| Asia | 8 | 10,037 | 36,589 | 0.26 (0.22–0.29) | 0.98 | < 0.01 |
| Europe | 21 | 5,638 | 37,787 | 0.16 (0.11–0.22) | 0.99 | < 0.001 |
| North America | 12 | 124,098 | 429,851 | 0.29 (0.25–0.33) | 0.99 | < 0.01 |
| North America, Europe, Asia | 1 | 19,155 | 76,360 | 0.25 (0.25–0.25) | -- | -- |
| Oceania | 24 | 16,999 | 77,897 | 0.22 (0.20–0.23) | 0.97 | < 0.01 |
| South America | 2 | 2,358 | 13,312 | 0.18 (0.17–0.19) | 0.61 | 0.11 |
| Overall | 68 | 178,285 | 671,796 | 0.25 (0.24–0.25) | 0.99 | < 0.01 |
| GDP | ||||||
| 1st quartile (lowest) | 6 | 734 | 4,867 | 0.11 (0.05–0.20) | 0.98 | < 0.01 |
| 2nd quartile | 5 | 5,001 | 23,367 | 0.19 (0.06–0.38) | 1.00 | < 0.01 |
| 3rd quartile | 5 | 2,558 | 12,162 | 0.18 (0.16–0.19) | 0.99 | < 0.01 |
| 4th quartile (highest) | 5 | 4,752 | 27,569 | 0.18 (0.10–0.28) | 1.00 | < 0.01 |
| Overall | 21 | 13,045 | 67,965 | 0.17 (0.12–0.21) | 0.99 | 0.61 |
Figure 2 Pooled prevalence for BPD28. Forest plot demonstrating pooled prevalence for BPD28 and 95% CI with a random-effects meta-analysis model.
Figure 3 Pooled prevalence for BPD36. Forest plot demonstrating pooled prevalence for BPD36 and 95% CI with a random-effects meta-analysis model.
Subgroup analysis for BPD28
When stratified by birth weight, the highest rates of BPD28 were found in infants with lower birth weights: <1000 g (ELBW). For instance, infants in the lowest birth weight stratum (< 500 g) had a BPD28 prevalence of 99% (95% CI, 0.97-1.00), while those in the second-lowest birth weight stratum (501–750 g) had a BPD28 prevalence of 87% (95% CI, 0.75–0.96). The BPD28 prevalence was lowest (16%; 95% CI, 0.11–0.22) in infants with the highest birth weights (1251–1500 g). The prevalence of BPD28 was higher in ELGA versus VLGA neonates (90% vs. 29%). The subgroup analysis of BPD28 by setting showed a higher rate in the national compared to multinational studies, as well as Oceania compared to other continents. Overall, no differences were observed in BPD28 prevalence when stratified by year or GDP.
Subgroup analysis for BPD36
The subgroup analysis for prevalence of BPD36 stratified by birth weight was very similar to the BPD28 analysis, in which an upward trend in the prevalence of BPD36 was associated with lower birth weights. For example, the highest prevalence of BPD36 was noted in neonates with a birth weight of less than 1000 g (ELBW). Further stratification of the ELBW neonates revealed BPD36 prevalence rates of 71% (95% CI, 0.51–0.87) and 60% (95% CI, 0.51–0.68) in neonates with birth weights of < 500 g and 501–750 g, respectively. Again, the lowest prevalence of BPD36, 10% (95% CI, 0.07–0.13), was seen in the highest (1251–1500 g) birth weight stratum.
Similar to the findings using the BPD28 definition, prevalence of BPD36 was higher in ELGA neonates (43% n = 358,636, versus 12% n = 126,368). Prevalence of BPD36 was also higher in national studies. Lastly, BPD36 prevalence again differed when stratified by continent. The highest prevalence was seen in North America at 329% (95% CI, 0.25–0.33). Rates of BPD36 were similar across GDP strata and year.
Sensitivity analysis and mortality rate
We conducted sensitivity analysis on the prevalence of BPD28 and BPD36 to reduce heterogeneity, defined as an I2 ≥ 50%. After keeping only 4 studies, the prevalence of BPD28 was 32% (95% CI, 0.31–0.32; I2 = 0%, eResults 1). For BPD36, 10 studies remained after filtering for high heterogeneity. The resulting rate of BPD36 was 25% (95% CI, 0.25–0.26; I2 = 49%, eResults 2). The table in eResults 3 shows the varying range of mortality rates for each of the studies (range of 0–23.9% with an average rate of 8.1%).
Risk of bias and publication bias
Forty-two studies were evaluated by the Newcastle-Ottawa Quality Assessment Scale and one study by the Cochrane Risk of Bias Tool. Thirty (74%) of the observational studies had a moderate bias (total score ranging from 5 to 6) (eTable 1). The domain that had the most bias pertained to questions regarding follow-up outcomes. Nine studies (21%) had low risk of bias (total score between 7 and 8). The single randomized controlled trial had a risk of bias score of five out of seven. Publication bias was low for BPD28 and BPD36. Plots can be viewed in eFigures 1, 2.
Discussion
Bronchopulmonary dysplasia remains the most common morbidity of prematurity and carries a significant disease burden [10]. Throughout the published literature, BPD displays itself as a disease with significant heterogeneity [11–14]. This is found not only within different “types” of BPD but also within the definition itself; as published data defines it as oxygen at 28 days, 36 weeks or other combinations of factors [15]. Therefore, it is essential to have accurate information for prediction, analysis and treatment. We performed this systematic review and meta-analysis to determine large-scale rates of bronchopulmonary dysplasia, with a subgroup analysis according to two major definitions. To our knowledge this is the largest and most comprehensive study describing BPD prevalence to date.
Our study expands on the 2019 study by Siffel et al. [3] to provide a more complete review of available data. We discovered, reviewed and analyzed data over a 41-year period (versus 11 years), with inclusion of a higher number of studies across more regions. As an additional contrast, we defined BPD (oxygen at 28 days or 36 weeks) and manually extracted data for combined analysis. This allowed us to use pooled data to compare subgroups and pursue further statistical analyses. We were therefore able to provide a more accurate prevalence for each provided outcome, rather than reporting outcomes as a set of ranges from individual studies.
As anticipated, the foremost risk factor for developing BPD was found to be low birth weight, particularly with a weight below 750 g. This trend was evident across both individual subgroup analyses and combined evaluations. Additionally, our observations revealed discrepancies in BPD rates among different gestational age groups, notably between ELGA and VLGA infants. These findings align with existing literature that underscores an inverse association between BPD rates and gestational age/birthweight, further affirming the current understanding in the field [8, 16].
We also compared BPD rates across three decades (1990–1999, 2000–2010 and 2010–2020), which showed no difference between the groups across the definitions of BPD. This is found throughout the literature and highlights the difficulty in preventing and treating this disease. Medical advancements in the care of preterm neonates have led to higher survival, especially in the most industrialized nations [17, 18]. This coincides with the survival of more infants with BPD and accounts for much of the similarity of the prevalence across decades. While our study focuses on reporting BPD rates in decade cohorts, it’s essential to acknowledge the limitations inherent in utilizing these broader definitions of BPD. We recognize that the clinical landscape of BPD management may have evolved over the past 30 years, potentially leading to improvements not fully captured by the BPD28 and BPD36 definitions. Our exclusion of studies using the newer BPD definition by Jensen et al. was indeed mentioned in the methods section, but we acknowledge the importance of reiterating this point here for clarity.
While the incidence of BPD exhibits considerable variation among different countries, current evidence indicates minimal disparities in its prevalence across major continents. Numerous studies have explored BPD incidence and associated risk factors in various regions spanning North America, Europe, Asia, and Australia, generally yielding comparable rates. For instance, research by Jain et al. found no significant divergence in BPD incidence among preterm infants across North America, Europe, and Australia [19]. In contrast, our investigation suggests notable differences in BPD rates among regions or continents, particularly with lower rates observed in Europe and South America. However, it’s noteworthy that South America’s data pool was limited to just 1–2 studies. These findings imply that the risk factors and underlying pathophysiology of BPD may not uniformly align across geographical regions, underscoring the imperative for further investigation to elucidate these distinctions. This prompts consideration as to whether disparities in clinical practices might potentially justify these findings.
The Neonatal Research Network (NRN) in the United States has compiled large retrospective analyses of care practice and patient outcomes among extremely premature infants. They have demonstrated that rates of antenatal steroids and surfactant administration have increased, delivery room intubation has decreased [7]. However, the rates of bronchopulmonary dysplasia (BPD36) in their study ranged from 32 to 45%, which is notably higher than the 21% observed in this study. This difference could be attributed to the varying gestational ages included in the studies, as the NRN’s research comprised newborns between 22 and 28 weeks. In comparison, the Chinese Neonatal Network’s cohort of 8,148 preterm neonates had a BPD36 rate of 29.2%, which is higher than our study’s results, again differences most likely due to their inclusion of neonates 31 weeks and younger whereas our study included neonates of ≤ 32 weeks [20].
The prevalence of BPD varied depending on the study setting, with national cohorts demonstrating the highest rates for both definitions of BPD. These estimates may be more reliable, as they offer a broader representation across multiple institutions, reducing the impact of outliers and the unique management practices of individual hospitals on the results. Furthermore, many of these national studies employed inclusion criteria that targeted younger gestational ages, further enhancing their robustness. Despite the thought that GDP may have an impact on BPD rates, subgroup analyses based on quartiles of a nation’s GDP showed no differences. One possible explanation for this finding is that other factors beyond GDP, such as access to healthcare and neonatal resources, may play a more significant role.
Limitations
Despite conducting an extensive data search employing multiple reviewers and diverse search methods, there remains a possibility that certain available studies may have been overlooked. Our findings reveal considerable heterogeneity across all examined outcomes, with many I2 values approaching 1. Despite efforts to minimize this through meticulous data extraction and analysis, the persistence of heterogeneity underscores the importance of cautiously applying the results to specific disease populations. For example, Bonamy et al. reported low BPD rates as it exclusively classified the condition in individuals with the severe form of the disease. In an attempt to mitigate the observed heterogeneity, we conducted a sensitivity analysis, which yielded rates comparable to those obtained in the initial analysis characterized by high heterogeneity.
Another constraint stems from the limited granularity of the original datasets, owing to the diverse definitions of BPD and the myriad ways in which data can be presented. This limitation restricts our ability to conduct more sophisticated statistical analyses and may lead to unequal weighting of studies where data accessibility varies. Additionally, there is a notable disparity in the amount of data available for some regions, notably North America, Oceania, and Europe, compared to other global populations. It would have been ideal to gather data as comprehensive as that publicly available from Australia and New Zealand, Canada, and Japan. Moreover, handling mortality data was a significant challenge in our analysis. We encountered variations among studies, where some solely included survivors while others reported mortality rates without adjusting them in their BPD rates. Some observed rates may have been exceptionally low, especially if their mortality rates were high. We were unable to solely include survivors due to variations in study methodologies, with some studies including only survivors while others encompassed all patients in their denominator for BPD, regardless of neonatal mortality. Adapting our analysis to account for this disparity without access to patient-level data limited our analyses. To address this limitation, we included mortality rates in the supplementary materials. This allows for transparency regarding the impact of mortality on our findings and provides additional context for interpreting the results. While we hypothesized differences in pathophysiology as a possible cause for national differences, it is essential to acknowledge other potential factors that may influence BPD rates, such as variations in reporting practices, gestational age and birth weight distributions, and early mortality rates. These factors could contribute to the observed regional differences in BPD rates and warrant further investigation. Also, differences in the sophistication of medical treatment across regions impacts survival and eventual diagnosis of BPD, all of which affect overall outcomes and generalizability.
Conclusions
To conclude, this large systematic review and meta-analysis shows that despite advancements, the prevalence of bronchopulmonary dysplasia has remained consistent through decades and is a significant burden across populations. The data generated from this study could serve as baseline rates for future research and could help guide the development of bundled care strategies aimed at decreasing BPD rates [21]. Ultimately, a greater understanding of modifiable factors that contribute to BPD development is critical to improving outcomes and reducing the burden of this disease.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- BPD
bronchopulmonary dysplasia
- GDP
gross domestic product
- ELGA
extremely low gestational age
- VLGA
very low gestational age
- ELBW
extremely low birth weight
- VLBW
very low birth weight
- CI
confidence interval
- NRN
Neonatal Research Network
Author contributions
AM collected data and was a major contributor in writing the manuscript, assessed risk of bias, and statistical analysis. MN collected data, assessed risk of bias and was a major contributor in writing the manuscript. JJ collected data and was a major contributor in writing the manuscript. NB was a major contributor in writing the manuscript. AT collected data and assessed risk of bias. AN collected data and assessed risk of bias. SZ verified all data collection. MJ collected data. AM collected data.TV reviewed and critiqued manuscript writing. JB reviewed and critiqued manuscript writing. CW was a major contributor in writing the manuscript and reviewed and critiqued manuscript writing. MP collected data and critiqued manuscript writing. ID reviewed and critiqued manuscript writing. MB verified risk of bias and reviewed and critiqued manuscript writing. SA oversaw the project and reviewed and critiqued manuscript writing. All authors approved final version of manuscript.
Funding
AM reports a grant from the Parker B. Francis Foundation, National Institutes of Health (NIH) Eunice Kennedy Shriver National Institute of Child Health and Human Development K23HD101701 and a research grant from NIH National Heart, Lung, and Blood Institute 2R25-HL126140, outside the submitted work. All other authors declare no competing interests.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Role of Sponsor
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Originality of content
All information and materials in the manuscript are original.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Michelle Noronha and Jooby Joy co-1st authors.
References
- 1.Jobe AH. The new bronchopulmonary dysplasia. Curr Opin Pediatr. 2011 doi: 10.1097/MOP.0b013e3283423e6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doyle LW, Carse E, Adams A-M, Ranganathan S, Opie G, Cheong JLY. Ventilation in extremely Preterm infants and respiratory function at 8 years. N Engl J Med. 2017;377(4):329–37. doi: 10.1056/nejmoa1700827. [DOI] [PubMed] [Google Scholar]
- 3.Siffel C, Kistler KD, Lewis JFM, Sarda SP. Global prevalence of bronchopulmonary dysplasia among extremely preterm infants: a systematic literature review. J Matern Neonatal Med. 2021;34(11):1721–31. doi: 10.1080/14767058.2019.1646240. [DOI] [PubMed] [Google Scholar]
- 4.Jobe AH, Bancalari E. NICHD / NHLBI / ORD workshop Summary. Am J Respir Crit Care Med. 2001;163:1723–9. doi: 10.1164/ajrccm.163.7.2011060. [DOI] [PubMed] [Google Scholar]
- 5.Higgins RD, Jobe AH, Koso-Thomas M, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8. doi: 10.1016/j.jpeds.2018.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moher D, Liberati A, Tetzlaff J, Altman DG. Academia and Clinic annals of Internal Medicine Preferred reporting items for systematic reviews and Meta-analyses. Ann Intern Med. 2009;151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 7.Stoll BJ, Hansen NI, Bell EF, et al. Trends in Care practices, Morbidity, and mortality of extremely Preterm neonates, 1993–2012. JAMA. 2015;314(10):1039–51. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bancalari E, Jain D. Bronchopulmonary dysplasia: 50 years after the original description. Neonatology. 2019;115(4):384–91. doi: 10.1159/000497422. [DOI] [PubMed] [Google Scholar]
- 9.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence p = Ì ^ i) E- -. 2013;67(11):974–8. [DOI] [PubMed]
- 10.Thébaud B, Goss KN, Laughon M, et al. Bronchopulmonary dysplasia. Nat Rev Dis Prim. 2019;5(1). 10.1038/s41572-019-0127-7. [DOI] [PMC free article] [PubMed]
- 11.Gibbs K, Jensen EA, Alexiou S, Munson D, Zhang H. Ventilation strategies in severe bronchopulmonary dysplasia. Neoreviews. 2020;21(4):e226–37. doi: 10.1542/NEO.21-4-E226. [DOI] [PubMed] [Google Scholar]
- 12.Cochrane database Syst Rev. 2021;10(10):CD001146. doi:10.1002/14651858.CD001146.pub6. [DOI] [PMC free article] [PubMed]
- 13.Wu KY, Jensen EA, White AM, et al. Characterization of Disease phenotype in very preterm infants with severe bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2020;201(11):1398–406. doi: 10.1164/RCCM.201907-1342OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bamat NA, Zhang H, McKenna KJ, Morris H, Stoller JZ, Gibbs K. The clinical evaluation of severe bronchopulmonary dysplasia. Neoreviews. 2020;21(7):e442–53. doi: 10.1542/NEO.21-7-E442. [DOI] [PubMed] [Google Scholar]
- 15.Ibrahim J, Bhandari V. The definition of bronchopulmonary dysplasia: an evolving dilemma. Pediatr Res. 2018;84(5):586–8. doi: 10.1038/s41390-018-0167-9. [DOI] [PubMed] [Google Scholar]
- 16.Jensen EA, Schmidt B. Epidemiology of bronchopulmonary dysplasia. Birth Defects Res Part Clin Mol Teratol. 2014;100(3):145–57. doi: 10.1002/BDRA.23235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bell EF, Hintz SR, Hansen NI, et al. Mortality, In-Hospital morbidity, Care practices, and 2-Year outcomes for extremely Preterm infants in the US, 2013–2018. JAMA. 2022;327(3):248–63. doi: 10.1001/jama.2021.23580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Twilhaar ES, Wade RM, De Kieviet JF, Van Goudoever JB, Van Elburg RM, Oosterlaan J. Cognitive outcomes of children born extremely or very Preterm since the 1990s and Associated Risk factors: a Meta-analysis and Meta-regression. JAMA Pediatr. 2018;172(4):361–7. doi: 10.1001/JAMAPEDIATRICS.2017.5323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jain D, Bancalari E. Bronchopulmonary dysplasia: clinical perspective. Birth Defects Res Clin Mol Teratol. 2014;100(3):134–44. doi: 10.1002/bdra.23229. [DOI] [PubMed] [Google Scholar]
- 20.Cao Y, Jiang S, Sun J, et al. Assessment of neonatal Intensive Care Unit practices, Morbidity, and Mortality among very Preterm infants in China. JAMA Netw Open. 2021;4(8):e2118904. doi: 10.1001/jamanetworkopen.2021.18904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villosis MFB, Barseghyan K, Ambat MT, Rezaie KK, Braun D. Rates of Bronchopulmonary Dysplasia following implementation of a Novel Prevention Bundle. JAMA Netw Open. 2021;4(6):e2114140. doi: 10.1001/jamanetworkopen.2021.14140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information.