Abstract
Background
We recently sought to integrate our orthopaedic and plastic hand surgeons with the goal of improving education, patient care, and providing seamless, continuous coverage for our trauma center. Our hypothesis was that integration could serve both the orthopaedic and plastic surgery training programs well and provide more consistent care for the trauma patients.
Materials and Methods
Program director approval was granted for blinded analysis of case logs from plastic and orthopaedic surgery programs from 2012 through 2019. Data on mean and total number of hand cases were analyzed and compared for both specialties. Institutional Review Board approval was granted for a retrospective review of patient outcomes.
Results
For both orthopaedic and plastics resident trainees, the mean number of hand cases increased during this study period suggesting that the integration had a favorable impact on both programs. The mean number of hand cases for orthopaedic residents rose from 163 to 246. The mean number of hand cases for plastic surgery residents rose from 218 to 295. Patient outcomes as reflected in length of stay and time to consultation also improved.
Conclusion
To improve hand surgical training and patient care, an integrated orthoplastics approach to hand surgery was implemented at our institution. Plastic surgery trainees are completing more hand surgery cases in an integrated model (p < 0.001), including fracture care (p < 0.047). Orthopaedic surgery trainees have doubled the percentage of integumentary and microsurgery cases in the integrated model (p < 0.001). The educational and clinical changes affected in an integrated model have changed the paradigm for educating future hand surgeons at our institution.
Keywords: fellowship, training, hand, reconstructive, plastic and hand surgeon
Introduction
The popularity of the subspecialty of hand surgery is reflected in the increasing number of fellowship applicants and growth of the American Society for Surgery of the Hand (ASSH).1 With more than 80 Accreditation Council for Graduate Medical Education hand fellowship programs, it is time to reflect on variations in specialty-specific resident training. Plastic, orthopaedic, and general surgery curricula differ vastly, and this is reflected in the number of cases performed and type of cases completed.2, 3, 4
Despite completing significantly more cases in training than their orthopaedic colleagues, plastic surgery representation has diminished from 37% of the founding members of the ASSH in 1946 to 16% today.1,5, 6, 7 The upper extremity procedures to which plastic surgery trainees are exposed in their residency are bereft of uniformity, and this may be one modifiable factor contributing to the marginal presence of plastic surgeons in the ASSH.7, 8, 9, 10 To address this variability, experts have advocated for various interventions including extended training in an integrated hand surgery residency model or additional hand surgery fellowship years.6,11
We sought to compare the operative case logs of graduating plastic surgery trainees, as well as orthopaedic trainees, before and after the integration of the hand service at the authors’ institution. Furthermore, we analyzed patient outcome measures in hand pathology with treatment typically reserved for fellowship trained hand surgeons, focusing on scaphoid fractures, perilunate dislocations, and nerve injuries in the upper extremity. The aim of this study is to assess trainee hand exposure in an administratively supported integrated orthoplastic hand service at an academic level 1 trauma center. A secondary goal is to analyze patient outcome measures during this transition.
Materials and Methods
National ACGME surgical case log data available to our program directors were reviewed for plastic and orthopaedic surgery programs from 2012 through 2019. Data on mean and total number of hand cases were analyzed and compared for both specialties. Institutional Review Board approval was granted for a retrospective review of patient outcomes in length of stay (LOS), time from consultation to operation, and readmission for scaphoid fractures, perilunate dislocations, and upper extremity nerve injuries from 2012 through 2019.
Program director approval was granted for blinded analysis of case log data from our own institution for orthopaedic and plastic surgery trainee graduates.
The electronic medical record was queried from 2010 through 2019 for operative Current Procedural Terminology (CPT) codes related to scaphoid fracture, perilunate dislocations, and upper extremity nerve repairs. These injuries were chosen as representative pathologies treated exclusively by fellowship trained hand surgeons at our institution. The following CPT codes were included: 25680, 25685, 25320, 25440, 25622, 25624, 25628, 64831, 64834, 64835, 64836, 64856, and 64857.
Statistical Analysis
The Mann–Whitney’s U test was used to analyze LOS and time from consultation to operation. A chi-square test was used to assess readmission rates. The Cochran–Armitage’s test of trend was used to analyze total numbers of orthopaedic and plastic surgery cases as well as percentage of hand cases for each specialty. A chi-square test was used to compare specific hand cases including integumentary, fractures, nerve injuries, and microsurgery.
Results
Case Log Results
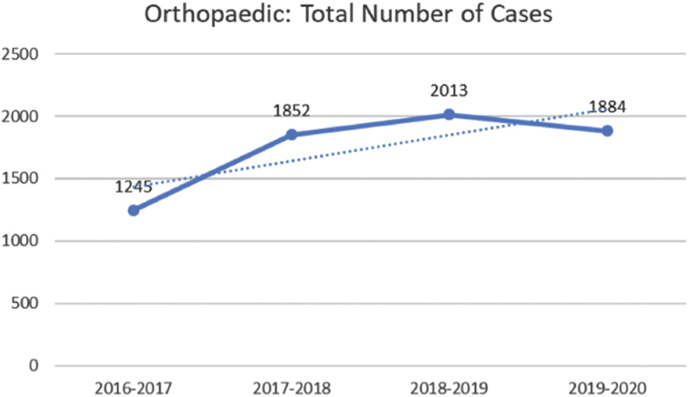
For both orthopaedic and plastics resident trainees, the mean number of hand cases increased during this study period suggesting that the integration had a favorable impact on both programs as measured by exposure to surgical cases. The mean number of hand cases for orthopaedic residents rose from 163 to 246. The mean number of hand cases for plastic surgery residents rose from 218 to 295. In both the orthopaedic and plastics training programs, the mean number of hand cases moved closer to the national means in the respective specialties. At the end of the study period, the orthopaedic mean was 246 compared with national mean of 271, and the plastics mean was 295 compared with national mean of 424. Both specialties have maintained pace with national trends, reflected in the increase in mean cases each year. The trend for total number of cases completed by orthopaedic surgery trainees (Fig. 1) has an upward trajectory (p < 0.048). The percentage of their total cases that are in the hand category for orthopaedic trainees has a downward trend (p < 0.001).
Fig. 1.
The trend of the number of orthopaedic cases per year has risen during the integration of the hand division.
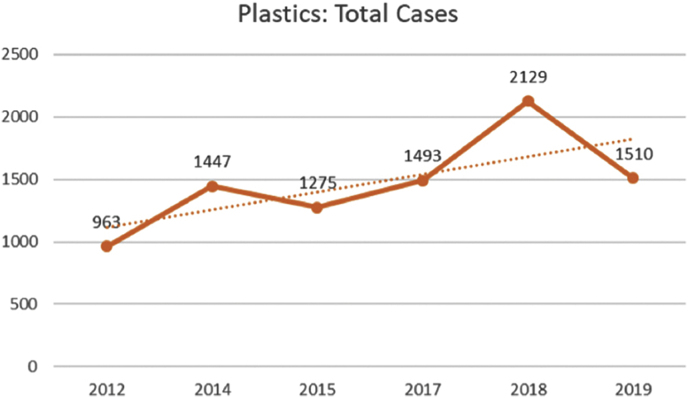
Plastic surgery trainees are also completing more cases on analysis of the trend of graduates from 2012 through 2019 (p < 0.002). Plastic surgery trainees have an increasing trend (Fig. 2), reflecting a bigger impact of hand surgery on their complete case log (p < 0.001). There is a marked increase in the total number of cases completed by plastic and orthopaedic surgery trainees in the second time interval (p < 0.001).
Fig. 2.
The trend of the number of plastic surgery cases per year has risen during the integration of the hand division.
Assessing specific types of cases by operative treatment yielded the following data. For fracture, dislocation, arthrodesis, and amputation cases, orthopaedic and plastic surgery percentages during the entire study period, there was no difference in the percentage of cases (p 0.590). For nerve injuries and nerve compressions, there were no differences in the percentage of cases (p 0.915 and 0.843, respectively). For integumentary cases, orthopaedic trainees are completing more as a percentage of their hand cases (p < 0.001). For microsurgical cases, plastic surgery graduates completed far more as a percentage of their hand cases (p < 0.001).
Data from preintegration and postintegration groups were analyzed for both orthopaedic and plastic surgeries. As a percentage of their hand cases, orthopaedic trainees completed 2.5 then 5.9% integumentary cases, showing an increase in the new model (p = 0.013). For fracture, dislocation, arthrodesis, and amputation cases before and after the change to the hand service remained stable with a small decrease from 5.2 to 4.8% (p = 0.439). Similarly, nerve injury was stable with a decrease from 1.2 to 1.1% (p = 0.706). For microsurgical cases, orthopaedic surgery had a stable and small increase from 0.3 to 0.6%, showing that they complete very few microsurgery cases (p = 0.105).
When comparing pre- and postintegration groups in plastic surgery, the following data were obtained. Integumentary case percentages increased from 2.8 to 3.8% (p = 0.013). Fracture case percentages increased from 4.6 to 5.6% (p = 0.047). Nerve injury also improved from 0.9 to 1.4% (p = 0.018). Microsurgery cases remained stable but increased from 6.1 to 7.0% (p = 0.088).
When comparing the percentage of hand cases for each program’s trainees in postintegration groups that were integumentary, fracture, nerve injury, and microsurgery, the following data were acquired. Orthopaedic trainees had a statistically significantly larger percentage of integumentary cases within their hand log at 5.9 compared with 3.8% (p < 0.001). Similarly, plastic surgery dominated microsurgery with 7.0 to 0.6% (p < 0.001). The insignificance of the p-values for fracture (p = 0.105) and nerve injury (p = 0.222) reflects a similar experience for both specialties for fracture and nerve cases.
Patient Outcome Results
One hundred and eleven patients were treated for scaphoid fractures, perilunate dislocations, and upper extremity nerve injuries from January 2012 through August 2016 (preintegration). In the subsequent time period ending December 2019 (postintegration), 209 patients were treated for the same pathologies. An absolute increase in patient volume by nearly 100% was noted with the increase in hand surgeons.
The median LOS in the preintegration group was postoperative day 1 discharge, whereas in the postintegration group, this decreased to same day discharge. Additionally, the 75th percentile for LOS decreased from 4 to 3 days. The p-value for these changes is 0.122, reflecting no statistical significance. Though, from a clinical and financial perspective, a full hospital day is important. Time from consultation to operation remained stable at 2 days for the median value. Readmission rates also remained stable with values of 12.1 and 13.9% for the pre- and postintegration groups, respectively.
Discussion
We believe that the cooperative model that we have developed echoes the original intent of integration to serve patients but also now can improve training for residents and fellows alike. It is also an example of how institutions can maximize the expertise of two specialties while preparing residents for fellowship or broad hand practice. The biggest benefit is noted in the improvement in education for plastic and orthopaedic surgery trainees.
Integrated Service Study Results
This study compares the operative exposure of both plastic and orthopaedic surgery trainees before and after integration of the hand service. The total number of cases for orthopaedic trainees increased in the postintegration group, but the percentage of hand cases decreased. At the same time, the total number of cases for plastic surgery trainees increased in the postintegration group, while the percentage of hand cases increased. This reflects a clear benefit for plastic surgery trainees. Orthopaedic trainees may be completing fewer hand cases as a percentage of their total cases, but they are far exceeding minimum requirements. A balance has resulted in the integrated orthoplastics model, whereas when two programs were present, plastic surgery trainees struggled to meet minimum requirements. The mean increase in both plastic and orthopaedic trainee case numbers confirms that orthopaedic trainees are not losing cases to plastic surgery trainees in the integrated model.
Orthopaedic trainees have benefited from this model. They are completing a statistically significant larger percentage of integumentary-based hand cases. This percentage is larger than plastic surgery trainees. At the same time, orthopaedic trainees have not had a statistically significant drop in fracture and nerve cases. Plastic surgery trainees have benefited with a statistically significant increase in the number of fracture and nerve injury cases. While their percentage of integumentary cases has decreased, the mean increase in the number of cases also shows no concern with losing a significant number of cases to orthopaedic trainees. One area for improvement is in microsurgery, where plastic surgery trainees still dwarf their orthopaedic colleagues in percentages. This is an important consideration in a replantation program.
The LOS for patients is clinically and financially significant as the median duration of stay decreased by a full day. The median LOS for many hand injuries being low, an important context to consider. The duration of time from consultation to operation remained stable. At baseline, the median time of 2 days is difficult to decrease as operating room access has not grown over the study period. Furthermore, the volume of patients has increased in the two time frames, reflecting more patients needing access to a stable number of operating rooms. Readmission rates remained stable, as one would expect given the predictable complication rates for the chosen hand pathologies.
Orthopaedic and Plastic Surgery Paradigms
There are inherent differences in trainees from plastic, orthopaedic, and general surgeries.10 There are 1.7- and 100-fold more hand operations performed by plastic surgery trainees compared with those from orthopaedic and general surgeries, respectively. While the authors of that study did not hypothesize on the reason for a smaller representation in the ASSH despite a higher overall case completion rate, valuable recommendations were provided. Optimization of prerequisite training, specialty track training modification, and a uniform ACGME supported hand case log are three suggestions provided. As part of this disparity, Higgins examined the “part-time hand surgeon” characterization of many plastic surgeons.5 One of the reasons is a higher rate of dependence on emergency rooms for referrals and practice patterns based on microsurgical and congenital training that necessitates the use of hospital operating rooms.
The current reality is that orthopaedic hand surgeons perform significantly more hand procedures than their plastic surgery counterparts.12 Despite performing more congenital hand and replantation cases, plastic surgeons are treating fewer operative distal radius fractures. When queried on their self-assessment of distal radius nonunion, distal radius and ulna open reduction and internal fixation, and intracarpal fusion, plastic surgeons report inadequate training.9 This further suggests that one of the points for intervention in increasing plastic surgery presence in the hand community is at the training level in both residency and fellowship.
Nonuniform operative experience has been previously studies between orthopaedic and general surgery trainees.13 This study revealed significant disparities in the operative experience relating to hand cases during training. Another study looking specifically at case logs from ASSH applicants demonstrated that the type of clinical practice and types of cases performed by hand surgeons differed based on their primary residency training.14 This study hypothesized that surgeon interest was another factor contributing to the specific pathologies in a hand surgeon’s practice. We believe that the seeds of a hand surgeon’s future practice are planted during residency and fellowship may be too late to alter the plastic surgery trained hand surgeon’s practice composition.
Integrated Paradigm
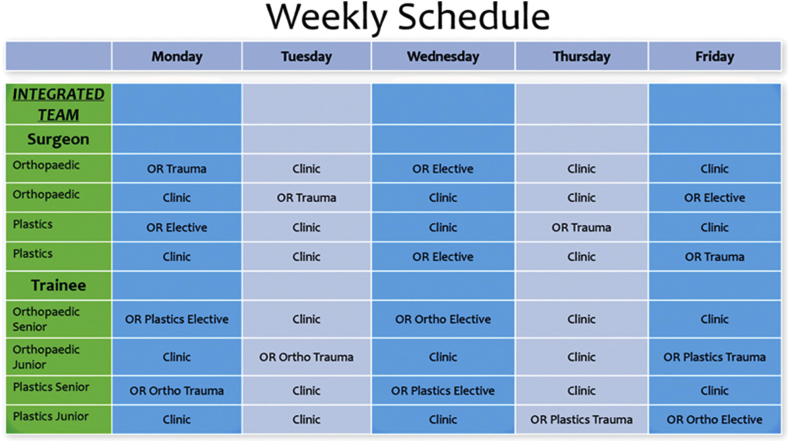
In our model, we have partial integration of services. The senior trainee on the service (from orthopaedic or plastic surgery) is responsible for organizing the case schedule (Fig. 3) for the two orthopaedic and two plastic surgery trained hand surgeon attendings. Thus, at times, one trainee from either specialty has oversight over junior trainees from both specialties and organizes operative schedules with hand surgeons from both specialties. This requires coordination with the other senior trainees, as the remainder of orthopaedic and plastic surgery trainees are scheduled to their respective field (orthopaedic oncology, cleft lip, and palate).
Fig. 3.
Integrated schedule alternates every other week, so there is a mixture of hand surgeons with trainees from each specialty in the operating room (OR) and clinic.
The success of the hand division has led to administrative support to integrate the spine surgery care between orthopaedic surgery and neurosurgery. This is a model that goes as far as there is cooperation among the trainees, surgeons, and administration. In addition to this integrated hand division, orthopaedic trainees spend dedicated time with general plastic surgery, while plastic surgery trainees rotate on orthopaedic trauma and oncology (rotation model). This results in trainees from both departments rotating with their own team, an integrated division, and the other specialty at different points in their training.
Each year, the senior plastic surgery trainee will spend 75% of their time solely within their specialty and the remainder of the time on the integrated hand team or as a rotator with another specialty. The priority remains to obtain board certification and meet training requirements within the respective specialty. Adding an integrated component to training gives each trainee a well-rounded foundation.
Applications of an Integrated Paradigm
We believe our study is important for developing countries and rural areas within the United States. While people in major cities around the world and United States may have access to many specialized hand surgeons, this is not the case in other areas. Training programs that adopt an integrated approach to hand surgery and other highly technical specialties will produce surgeons capable of managing both bony and soft tissue–based pathology. In this model, in a given week, trainees will operate with and attend clinic with hand surgeons trained in both plastic and orthopaedic surgeries. Senior plastic surgery residents will take junior orthopaedic trainees through microsurgical repair of blood vessels and nerves. In return, orthopaedic senior trainees will mentor junior plastic surgery trainees on osteosynthesis and fracture rehabilitation. Each specialty will contribute senior and junior trainees to the service. Trainees will take emergency call with attendings from both specialties. This allows the trainee to develop a composite cognitive approach and technical skillset week by week instead of fragmenting the training. Cooperation among trainees, department leadership, and administration is essential.
Our qualitative feedback is best seen in fellowship application trends. In the last 4 years, both plastic and orthopaedic trainees have matched into highly competitive hand surgery fellowship positions. There is currently a fifth trainee applying this year, with another planning to apply in the subsequent year. In the prior 5 years, no trainees applied to hand surgery.
In the United States, hand surgery originated as a specialty represented by multiple disciplines including neurosurgery, orthopaedic surgery, and plastic surgery. All of these fields included general surgical training. Over the past few decades, many institutions compartmentalized hand surgery into one specialty, most commonly orthopaedic surgery. Other institutions focused bony upper extremity care in orthopaedics and soft tissue, tendon, and nerve surgery in plastics. As a result, fewer “total upper extremity” surgeons are trained.
This study shows a model that may be gaining traction, an integrated hand service. In this model, a team of hand surgeons from many backgrounds have formed a division where trainees of all specialties work together with these attendings. Well-rounded trainees are graduating with experience in bone, tumor, nerve, tendon, soft tissue, and microsurgery. Future studies should prospectively evaluate this program’s case logs, fellowship placement, and career practice.
Limitations
This study is not without its limitations. The orthopaedic surgery and integrated plastic surgery training programs are new and contain small numbers of trainees. Furthermore, there is an obvious increase in absolute case numbers due to hiring more hand surgeons. The hand service integrated in 2016 with four attendings, previously being one attending. The impact of this training model evolved over the subsequent years. With small groups, subgroup analysis data are prone to error. Additionally, it is not possible to perfectly analyze the effect on each graduating class due to their differences in program duration and year of inception. Case log data are also subject to errors and rely on appropriate coding knowledge by trainees. Plastic surgery and orthopaedic case logs differ in reporting style. Another limitation is selecting three specific procedures for analysis. They were chosen as they represented cases only completed by a hand surgeon at the institution, whereas other such as distal radius fractures fell into the purview of orthopaedic trauma surgery. The retrospective nature of the patient outcomes limits the level of evidence of the data presented. A stronger study would be prospective in nature. Despite these limitations, an integrated model has benefited patients and trainees while providing a roadmap at an administrative level.
Conclusion
Plastic surgeons constitute a smaller percentage of ASSH membership relative to orthopaedic surgeons. The significant heterogeneity in residency experience is one area in which to affect change. After integration at our institution, marked education changes have occurred. Plastic surgery trainees are completing more hand surgery cases in an integrated model (p < 0.001), including fracture care (p < 0.047). Orthopaedic surgery trainees have doubled the percentage of integumentary and microsurgery cases in the integrated model (p < 0.001). These increases have both statistical and clinical significance, resulting in a more complete upper extremity surgeon in both departments. Additionally, the LOS for patients is clinically and financially significant as the median duration of stay decreased by a full day. The educational and clinical changes affected in an integrated model have changed the paradigm for educating future hand surgeons at our institution.
Acknowledgments
The authors of this study would like to acknowledge the contribution of Krystal Turner, biostatistician at Cooper University Hospital, for her assistance with statistical analysis. Her effort was instrumental in analyzing the data for this manuscript.
Funding
None.
Conflict of Interest
None declared.
References
- 1.Goldfarb CA, Lee WP, Briskey D, Higgins JP. An American Society for Surgery of the Hand (ASSH) task force report on hand surgery subspecialty certification and ASSH membership. J Hand Surg Am. 2014;39(2):330–334. doi: 10.1016/j.jhsa.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 2.Bell RH., Jr. Graduate education in general surgery and its related specialties and subspecialties in the United States. World J Surg. 2008;32(10):2178–2184. doi: 10.1007/s00268-008-9658-x. [DOI] [PubMed] [Google Scholar]
- 3.Bell RH. National curricula, certification and credentialing. Surgeon. 2011;9(Suppl 1) doi: 10.1016/j.surge.2010.11.007. S10–S11. [DOI] [PubMed] [Google Scholar]
- 4.Sachdeva AK, Bell RH, Jr., Britt LD, Tarpley JL, Blair PG, Tarpley MJ. National efforts to reform residency education in surgery. Acad Med. 2007;82(12):1200–1210. doi: 10.1097/ACM.0b013e318159e052. [DOI] [PubMed] [Google Scholar]
- 5.Higgins JP. The diminishing presence of plastic surgeons in hand surgery: a critical analysis. Plast Reconstr Surg. 2010;125(1):248–260. doi: 10.1097/PRS.0b013e3181c496a2c. [DOI] [PubMed] [Google Scholar]
- 6.Szabo RM. What is our identity? What is our destiny? J Hand Surg Am. 2010;35(12):1925–1937. doi: 10.1016/j.jhsa.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 7.Jones NF. 2016 ASSH presidential address: teaching hands-pass it on. J Hand Surg Am. 2018;43(7):591–605. doi: 10.1016/j.jhsa.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 8.Sears ED, Larson BP, Chung KC. Program director opinions of core competencies in hand surgery training: analysis of differences between plastic and orthopedic surgery accredited programs. Plast Reconstr Surg. 2013;131(3):582–590. doi: 10.1097/PRS.0b013e31827c6f54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aliu O, Chung KC. A role delineation study of hand surgery in the USA: assessing variations in fellowship training and clinical practice. Hand (N Y) 2014;9(1):58–66. doi: 10.1007/s11552-013-9592-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drinane JJ, Drolet B, Roth MZ, Eberlin KR. Preparation for hand surgery fellowship: a comparison of resident training pathways. Plast Reconstr Surg. 2021;147(4):887–893. doi: 10.1097/PRS.0000000000007722. [DOI] [PubMed] [Google Scholar]
- 11.Jupiter J. Hand surgery fellowships: time for reconsideration? Tech Hand Up Extrem Surg. 2011;15(4):197. doi: 10.1097/BTH.0b013e31823d23eb. [DOI] [PubMed] [Google Scholar]
- 12.Mehta K, Pierce P, Chiu DTW, Thanik V. The effect of residency and fellowship type on hand surgery clinical practice patterns. Plast Reconstr Surg. 2015;135(1):179–186. doi: 10.1097/PRS.0000000000000786. [DOI] [PubMed] [Google Scholar]
- 13.Silvestre J, Lin IC, Levin LS, Chang B. Variability in resident operative hand experience by specialty. Hand (N Y) 2018;13(1):103–107. doi: 10.1177/1558944716677537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reavey PL, Jones NF. Primary residency training and clinical practice profiles among board-certified hand surgeons. J Hand Surg Am. 2019;44(9) doi: 10.1016/j.jhsa.2018.10.026. 799.e1–799.e9. [DOI] [PubMed] [Google Scholar]