Abstract
Background
The study determined the pattern and distribution of gynaecological cancer cases seen at a university teaching hospital in southwest Nigeria over a 5-year period.
Methodology
It was a 5-year retrospective review of all gynaecological cancer cases seen and managed at the hospital from 1 September 2013 to 31 August 2018.
Results
A total of 6247 gynaecological admissions and 902 gynaecological cancers were seen in the hospital during the study period accounting for a proportion of 14.4%. Of these 902 cases, 835 (92.6%) women had their detailed records available for data extraction and analyses. Cervical cancer was the most commonly seen malignancy (61.7%). The mean age of the patients was 52.5 ± 12.4 years with the largest proportion of the women being in the age group of 50–59 years (26.9%). A large proportion (35.6%) of the patients had a parity of 5 or more with an overall median parity of 4 (IQR, 1–5) while the largest proportion (59.1%) were postmenopausal women. The highest mean age was seen in women with vulvar cancer (67.2 ± 0.6 years) while the lowest was in those with sarcoma botryoides (12.3±1.01 years).
Conclusion
There was a steady annual increase in the number of gynaecological cancer cases at the hospital during the period under review. The most common cancers seen in this study are associated with advanced age, increased parity and postmenopausal status. There is a need for improved public enlightenment on the importance of routine screening and for consistent government policy on the institution of an effective organised screening programme for cervical cancer.
Keywords: Cervical Cancer, Gynecological Cancer, Nigeria, Sarcoma Botryoides, Vulvar Cancer
Introduction
Cancer is expected to rank as the leading cause of death and the single most important contributor to reduced life expectancy in every country of the world in the 21st century.[1]Cancer incidence and mortality are rapidly growing worldwide,[1,2]and the reasons for these are complex but reflect both increased ageing and growth of the population, as well as changes in the prevalence and distribution of the main risk factors for cancer occurrences. Several of these are associated with socioeconomic development and the westernisation of diets. [1-3] Cancer transitions are most striking in emerging economies, where an increasing magnitude of the disease is paralleled by a changing profile of common cancer types. [1-3]
Gynaecological malignancies are cancers of the female genital tract which include those of the vulva, vagina, cervix, uterus, fallopian tube, ovary, and gestational trophoblastic tumours. The pattern of gynaecological malignancies varies among nations and even among health institutions in the same country,[4] and these variations are mainly due to different genetic patterns, lifestyles, environmental, socio-cultural and economic factors.[4,5] It is noteworthy that high-quality cancer registry data, the basis for the planning and implementation of evidence-based cancer control programmes, are not available in most low- and middle-income countries (LMIC). [1,2] With the rapid growth and ageing of the population in many countries of the world, the rising prominence of cancer as a leading cause of death now partly reflects the marked declines in mortality from cardiovascular diseases such as stroke and coronary artery disease, relative to cancer.[1,4]The extent to which cancer is positioned as a cause of premature death is a reflection of the national levels of social and economic development.[1,2]
Worldwide, breast cancer is the most commonly diagnosed cancer in females and the leading cause of cancer death, followed by colorectal and lung cancer.[1] Cervical cancer, with an estimated 570,000 cases and 311,000 deaths in 2018 worldwide, ranks as the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women.[1-3,5] It only ranks second in incidence and mortality behind breast cancer in most low-income settings[1,3] with the highest regional incidence and mortality rates seen in sub-Saharan Africa.[1] The incidence of cervical cancer in most western countries has declined since the early 1980s when effective cervical cancer screening became the standard of care, unlike what is obtainable in developing countries where opportunistic screening is the norm.[5] Approximately 80% of cervical cancer cases are reported in developing countries.[5-7] The disparity in incidence between the developing and developed world can also be attributed to a lack of awareness of cervical cancer, poverty, poor access to medical care and the focus on other competing national health priorities such as HIV/AIDS, tuberculosis and malaria.[5,6] Globally, ovarian cancer is the leading cause of gynaecological cancer death and this is mostly due to its late-stage diagnosis.[5,6] Endometrial cancer is more common in developed countries such as the United States, Northern Europe, Eastern Europe and North America.[1,7]Despite the high incidence and mortality of some of these genital tract cancers in our environment, there is a dearth of reliable facility- or population-based cancer registries, which in turn leads to poor or inadequate government planning in the care of cancer patients in the country. This study was, therefore, aimed to determine the pattern and distribution of gynaecological cancer cases seen at a university teaching hospital in southwest Nigeria over 5-years (from September 2013 to August 2018).
Materials and Methods
Study design and setting.
The study was a retrospective review of all gynaecological cancer cases seen at a university teaching hospital in southwest Nigeria between September 2013 and August 2018. The hospital is one of the largest tertiary health institutions in Nigeria. It has an 800-bed capacity, and it is a referral centre for a wide range of specialist consultations, particularly for patients in the southwest region and Nigeria in general. The hospital has a gynaecological oncology unit in its Department of Obstetrics and Gynecology. This unit provides specialized multidisciplinary oncology care in conjunction with clinicians in the Departments of Radiotherapy, Radiodiagnosis, Anatomic and Molecular Pathology, General Surgery, and Urology. The unit also oversees weekly outpatient and cytology clinics and a daily Colposcopy clinic where patients with preinvasive diseases of the cervix are diagnosed, evaluated, and offered the appropriate treatment.
Data collection
The names and hospital numbers of patients with gynaecological cancers managed in the hospital during the period under review were retrieved from the gynaecological, radiotherapy and paediatric ward and clinic registers, and the operating theatre record books. The total number of gynaecological malignancies seen in the hospital during the review period was then extracted. The patients' case notes were retrieved from the medical records department and information on the women's age, parity, menstrual status, and histopathological diagnoses were extracted with the use of a standardized study proforma. Most of the patients had a histological diagnosis of gynaecological cancers while all cases of choriocarcinoma were diagnosed based on their clinical features supported by biochemical testing.
Data analyses
The data were collated and analysed using the SPSS version 23.0 Statistical Package for Windows (IBM Corp, Armonk, NY, United States). Descriptive statistics were computed for all data, and the results were presented with a simple table and charts.
Ethical considerations
Ethical approval for the study was obtained from the hospital's Health Research Ethics Committee (HREC Approval number – ADM/DCST/HREC/APP/2619) before the retrieval of the patients' data. De-identifying codes were assigned to the patients' information for confidentiality.
Results
There was a total of 6247 gynaecological admissions in the hospital during the study period with 902 of these diagnosed and managed for various types of gynaecological cancers. This constitutes a proportion of 14.4% of all gynaecological cases seen. However, only 835 (92.6%) of these women diagnosed with cancers had their detailed records available for analysis. Of these, cervical cancer accounted for the largest proportion of cases seen (61.7%) while the least common was vaginal cancer (0.1%) [Figure 1].
Figure 1:

Distribution of gynaecological cancer cases
Table 1 shows that the overall mean age of the patients was 52.5 ± 12.4 years with the largest proportions of them being in the age group of 50–59 years (26.9%). A large proportion (35.6%) of the patients had a parity of 5 or more with an overall median parity of 4 (IQR, 1 – 5) while the largest proportion (59.1%) were postmenopausal. As shown in Table 2, the highest mean age was seen in women with vulvar cancer (67.2 ± 0.6 years) while the lowest was seen in those with sarcoma botryoides (12.3±1.01 years). Figure 2 showed a steady annual increase in the number of gynaecological cancer cases in the hospital from 101 in 2013 to 245 in 2018, signifying a percentage increase of 142.6% during the period under review.
Table 1:
Sociodemographic/obstetric characteristics of women with gynaecological cancers (n=835)
| Characteristics | Frequency, n (%) |
|---|---|
| Age group (in years) | |
| 4(0.5) | |
| 20-29 | 10 (1.2) |
| 30-39 | 117(14.0) |
| 40-49 | 218(26.1) |
| 50-59 | 225 (26.9) |
| 60-69 | 188(22.5) |
| ≥70 | 73 (8.7) |
| __ | 52.5 ± 12.4 years |
| Parity | |
| 0 | 82 (9.8) |
| 1-2 | 203 (24.3) |
| 3-4 | 253 (30.3) |
| ≥5 | 297 (35.6) |
| Median parity (IQR) | |
| Menstrual status | |
| Premenarcheal | 2 (0.2) |
| Premenopausal | 340 (40.7) |
| Menopausal | 493 (59.1) |
* Abbreviations: SD, standard deviation; IQR, interquartile range
Table 2:
Mean age distribution of the various gynaecological cancers
| Cancer type | Mean age ± SD (in years) |
|---|---|
| Cervical cancer | 54.7 ±13.3 |
| Choriocarcinoma | 29.3 ±2.1 |
| Endometrial cancer | 58.1 ±3.4 |
| Uterine leiomyosarcoma | 66.4 ±1.6 |
| Ovarian cancer | 56.6 ±4.0 |
| Sarcoma Botryoides | 12.3 ±1.0 |
| Vaginal cancer | 46.2 ±3.7 |
| Vulvar cancer | 67.2 ±0.6 |
* Abbreviations: SD, standard deviation
Figure 2:
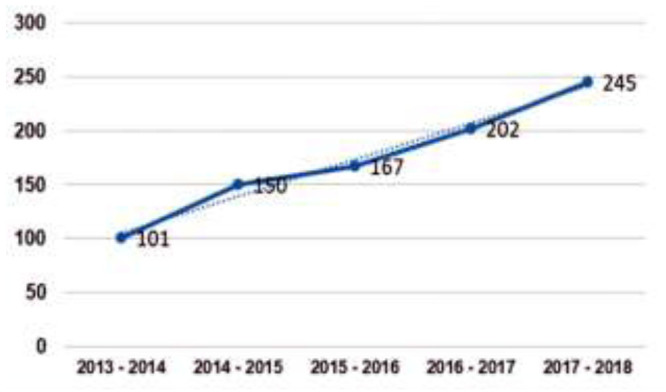
Yearly trend of gynaecological cancers
Discussion
In this study, gynaecological malignancies account for 14.4%of all gynaecological cases managed in the hospital during the period under review and this is much higher than 4.6% reported in Ilorin,[8] 5.4% in Jos[9]and 8.4% in Abakaliki[10] but almost comparable to the rates of 11.5% reported in Kano[5] and 12.8% in Calabar.[11] The rate is also similar to the reported finding of 12.5% reported by Manzoor et al[12] from the Western region of Pakistan but much higher than the 2.8% reported by Nkyekyer from Ghana.[13] This may be explained by the relatively large number of cases seen at our gynaecological oncology unit which is the largest referral center for patients in Lagos and most parts of Ogun State in South-west Nigeria.
Cervical cancer is the commonest gynaecological malignancy seen in this study (61.7%). It is also the commonest cancer reported from previous studies conducted in different parts of Nigeria[8-11]and other sub-Saharan African(SSA) countries.[13] This similarity is attributed primarily to the current poor access to cervical screening with a subsequent increase in the number of cervical cancer cases due to the absence of a national health programme that should make screening and vaccination available, accessible and affordable. The sub-Saharan African region which carries the greatest burden of cervical cancer has the least resources to tackle this problem.[14] Although the proportion of 61.7% of cervical cancer reported in this study is quite high it is still relatively lower than the 70.5% reported by Kyari et al in Maiduguri[15] and 78% reported by Ugwu et al in Enugu.[16] This may be attributed to the improved efforts of cervical cancer prevention through opportunistic screenings introduced in the last 2 decades in our hospital which have led to a slight reduction in the proportion of cervical cancer cases seen.
Ovarian cancer is the second commonest gynaecological malignancy in our study (25.1%). This is comparable to the findings from similar studies conducted in Nigeria [5,9-11,15,17,18]and Ghana[13]but a study conducted in Pakistan by Jamal et al[19] reported that ovarian cancer, with a proportion of 42.4%,was the most frequently encountered gynaecological malignancy followed by cervical cancer. This is in sharp contrast to the findings from most developing countries where cervical cancer is the most commonly seen. This suggests that countries with better organised and efficient cervical cancer screening programmes now have a smaller number of cervical cancer relative to the ovarian cancer cases which conversely has no recommended screening strategies for the low-risk population of women at the moment.
In this study, endometrial carcinoma accounts for 9.5% of cases seen and thus ranked as the third commonest gynaecological cancer reported during the review period. This is consistent with the findings in other studies from SSA[5,9,10,13,20] but different from the findings by Ibrahim et al in Ilorin[8] and Sanni et al in Jos[9] where the proportion of choriocarcinoma seems to be slightly higher than that of endometrial cancer. This may be attributed to the metropolitan nature of Lagos and some other urban cities in Nigeria that are now characterised by increased intake of westernised diet and its consequent tendencies for obesity,[20] one of the major risk factors for endometrial cancer, among the populace. As expected, other gynaecological malignancies such as vaginal and vulvar carcinomas, uterine leiomyosarcoma and sarcoma botryoides are generally rarely seen as reported in this study and various other studies conducted within and outside Nigeria. [9-13]
The mean age of patients with cervical cancer in the study was 52.5±12.4 years and this is comparable to the 50 to 52years reported in similar studies conducted in Ghana [13]and Nigeria [11]but much higher than the 43.1±7.5years reported by Okunade et al in Lagos[21] and Yakasai et al in Kano[5]respectively. The mean age of 56.6±4.0 years reported in patients with ovarian cancer in this study is higher than that of patients with cervical cancer and this is consistent with reports from previous studies[15,22] but lower than the 45.7 years reported by Okunade et al in a retrospective review conducted in the same setting in 2016.[23]The mean age of patients with endometrial cancer in this study (58.1±3.4 years) is also at par with that of cervical and ovarian cancers but only slightly lower than the 62.2 years reported by Okunowo et al in the same setting.[20]The reason for this is that cervical, ovarian and endometrial cancers are diseases most commonly found in women of older age group and the increased life expectancy among women in most countries may probably account for the increasing number of women having these conditions at predominantly more advanced age group. Conversely, as expected choriocarcinoma and sarcoma botryoides with mean ages of 29.3±2.1 years and 12.3±1.0 years respectively are seen mostly in younger women and girls as the case may be. The poor medical record-keeping system currently being used in our hospital contributed to the high number of missed data in this study with a significant impact on the accuracy of the data collected for analyses.
Conclusions
The number of patients with gynaecological cancers presenting to this hospital is on a steady increase. Cervical cancer is the most common female genital tract malignancy in our study, followed by ovarian and endometrial cancers in that order. These commonly encountered cancers are associated with advanced age, increased parity, and postmenopausal status. Improved health education and public enlightenment on the importance of routine screening and the need for a consistent government policy on the institution of an effective organised screening programme for cervical cancer. In addition, the identification and screening of women at risk of ovarian and endometrial cancers will lead to early diagnosis and treatment which will, in turn, reduce the morbidity and mortality from these much-dreaded diseases.
Acknowledgments
The authors appreciate the assistance given by the medical record staff of the teaching hospital and the resident doctors of the department of obstetrics and gynaecology. This work was partly supported by the Fogarty International Center of the National Institutes of Health under Award Numbers D43TW010134, D43TW010543 and D43TW010934. The views expressed by the authors are theirs alone and do not reflect the official views of the National Institutes of Health.
Conflicts of interest
The authors report no conflicts of interest.
References
- 1.Bray F, Jacques FM, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68: 394-424. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Health Observatory. Geneva: World Health Organization; 2018. who.int/gho/database/en/. Accessed October 5, 2018. [Google Scholar]
- 3.Bray F. Transitions in human development and the global cancer burden. In: Stewart BW, Wild CP, eds. World Cancer Report 2014. Lyon: IARC Press; 2014: 42-55. [Google Scholar]
- 4.Nnadi DC, Singh S, Ahmed Y, Siddique S, Bilal S. Histopathological features of genital tract malignancies as seen in a tertiary health centre in North-western Nigeria: A 10-year review. Annals of Medical and Health Sciences Research; 2014: 213-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yakasai IA, Ugwa EA, Otubu J. Gynecological malignancies in Aminu Kano Teaching Hospital Kano: A 3-year review. Nigerian Journal of Clinical Practice; 2013: 63-66. [DOI] [PubMed] [Google Scholar]
- 6.Balogun MR, Odukoya OO, Oyediran MA, Ujomu PI. Cervical Cancer Awareness and Preventive Practices: A Challenge for Female Urban Slum Dwellers in Lagos, Niger Afr J Reprod Health 2012; 16:75-82. [PubMed] [Google Scholar]
- 7.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012; 62:10-15. [DOI] [PubMed] [Google Scholar]
- 8.Ibrahim HM, Ijaiya MA. Pattern of gynaecological malignancies at the University of Ilorin Teaching Hospital, Ilorin, Nigeria. Journal of Obstetrics and Gynaecology; 2013: 194–19 [DOI] [PubMed] [Google Scholar]
- 9.Sanni WO, Ocheke AN, Oyebode T, Musa J, Nyango DD, Silas OA, Sagay AS. Pattern of gynaecological malignancies in Jos. Trop J Obstet Gynaecol; 2013: 97-102. [Google Scholar]
- 10.Agboeze J, Ezeonu PO, Onoh RC, Nwali MI, Agwu MR, Egbuji CC. Frequency and Pattern of Gynecological Cancers in Federal Teaching Hospital, Abakaliki, Nigeria. Journal of Basic and Clinical Reproductive Sciences; 2015: 54-57. [Google Scholar]
- 11.Omotoso J, Odusolu P, Ekpe EL, Okon U. Oshatuyi O. Gynaecological Malignancies in Calabar, Nigeria: A Tertiary Hospital-Based Study. ARJGO; 2018: 1-9. [Google Scholar]
- 12.Manzoor H, Naheed H, Ahmad K, Iftikhar S, Asif M, Shuja J, Sultan N, Ali I, Inayatullah S, Khan YH. Pattern of gynaecological malignancies in Southwestern region of Pakistan: An overview of 12 years. Biomedical Reports. 2017; 7: 487-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nkyekyer K. Pattern of gynaecological cancers in Ghana. East African Medical Journal; 2000: 534-538. [DOI] [PubMed] [Google Scholar]
- 14.Toye MA, Okunade KS, Roberts AA, Salako O, Oridota ES, Onajole AT. Knowledge, perceptions, and practice of cervical cancer prevention among female public secondary school teachers in Mushin Local government area of Lagos State, Nigeria. The Pan African Medical Journal. 2017; 28: 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kyari O, Nggada H, Mairiga A. Malignant tumors of female genital tract in North-Eastern Nigeria. East AfriMed J. 2004; 81:142-5. [DOI] [PubMed] [Google Scholar]
- 16.Ugwu EO, Iferikigwe ES, Okeke TC, Ugwu AO, Okezie OA, Agu PU. Pattern of gynecological cancers in University of Nigeria Teaching Hospital, Enugu, Southeastern Nigeria. Niger J Med. 2011; 20:266-9. [PubMed] [Google Scholar]
- 17.Emembolu JO, Ekwempu CC. Carcinoma of the cervix uteri in Zaria: Etiological factors. Int J gynecol Obstet. 1988; 26:265-9. [DOI] [PubMed] [Google Scholar]
- 18.Briggs ND, Katchy KC. Pattern of primary gynecological malignancies as seen in a tertiary hospital situated in the Rivers State of Nigeria. Int J Gynecol Obstet. 1990; 31:157-61. [DOI] [PubMed] [Google Scholar]
- 19.Jamal S, Mamoon N, Mushtaq S, Luqman M, Moghal S. The pattern of gynecological malignancies in 968 cases from Pakistan. Ann Saudi Med. 2006; 26:382-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okunowo AA, Alakaloko MA, Ohazurike EO, Okunade KS, Anorlu RI. Trend and characteristics of endometrial cancer in Lagos, Nigeria. Gulf J Oncolog. 2019; 1: 52-59. [PubMed] [Google Scholar]
- 21.Okunade KS, Dawodu OO, Salako O, Osanyin GE, Okunowo AA, Anorlu RI. Comparative analysis of serum trace element levels in women with invasive cervical cancer in Lagos, Nigeria. The Pan African Medical Journal. 2018; 31:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Armon PJ, Missaleh W. Carcinoma of the cervix in Tanzania. East Afr Med J. 1978; 55:534-7. [PubMed] [Google Scholar]
- 23.Okunade KS, Okunola H, Okunowo AA, Anorlu RI. A five-year review of ovarian cancer at a tertiary institution in Lagos, Southwest, Nigeria. Niger J Gen Pract. 2016; 14: 23-7. [Google Scholar]


