The Clinical Standards Advisory Group has expressed concern over the lack of clear criteria with which to accord priority to patients awaiting coronary artery bypass surgery.1 Until recently, the most notable research on what determines “urgency” was to be found in reports from Ontario which point to variations between doctors and institutions in the criteria they use to place patients in a queue.2–4 Earlier this year the New Zealand National Advisory Committee on Health published its findings on the impact that some social factors, such as the threat to independence, the care of dependants, or the patient’s ability to work, might have on decisions related to priority.5
The influence of demographic or lifestyle factors, such as age or smoking habit, on waiting list priority has been debated prominently in the United Kingdom.6,7 Doctors may take an individual view of the probable effectiveness of revascularisation in some patients (for example, smokers compared with non-smokers). However, neither the perceived efficacy of the procedure nor the distinction between “urgency” (the speed required to intervene to obtain a desired clinical outcome) and “priority” (the relative position on a surgical waiting list) has yet been investigated. Doctors might agree that a patient who smokes needs urgent intervention but disagree over the priority this patient should be accorded on a waiting list for surgery.
In response to the Clinical Standards Advisory Group report, a regional workshop sponsored by the Northern Ireland Clinical Resource Efficiency Support Team was convened in the spring of 1996 to address these issues. Two main research questions were:
• • Do clinicians pay attention to demographic and lifestyle factors when making urgency and priority judgments?
• • Do disagreements between clinicians arise out of differences in how they attend to clinical and demographic factors in arriving at these judgments?
Summary points
Scoring systems developed to allocate priority for coronary bypass surgery may have potentially competing objectives, such as ensuring that the most urgent cases are treated first or that added life years gained or the quality adjusted life years are maximised in those waiting
The scoring systems so far devised have not made their specific objectives clear and have not distinguished between “urgency” and “priority”
Judgments about urgency and priority can produce different weighting for demographic and lifestyle factors such as age and smoking habit
Lifestyle characteristics often influence doctors’ judgments on priority independently of their beliefs about the probable effectiveness of surgery
Methods
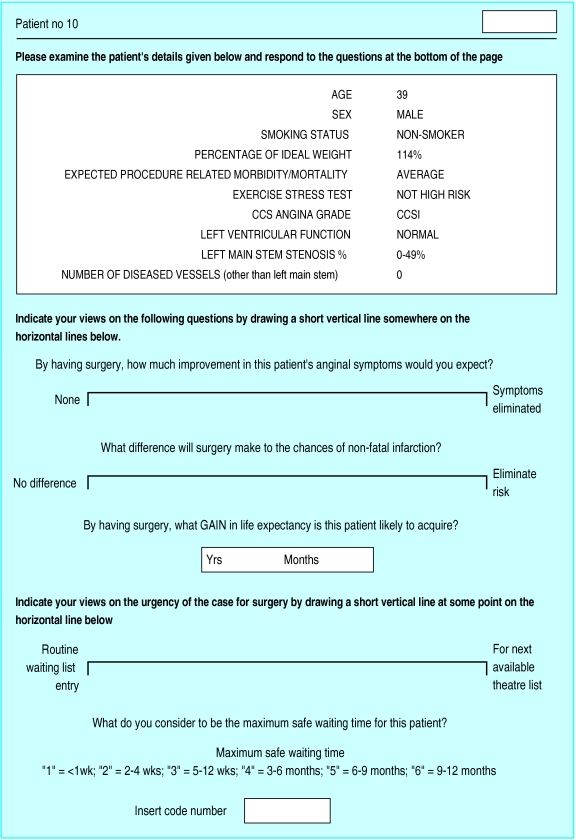
The key task which participants (“judges”) undertook before the workshop was an appraisal of “paper patients” (as in Ontario and New Zealand). In fact, the cases were based on a random sample of real patients who had undergone bypass surgery in Northern Ireland in 1991.8 Each patient was described by 10 clinical “cues.” A sample case is shown in figure 1, while table 1 summarises the patients’ characteristics. Each participating doctor was given a folder of details of 60 patients, of which 10 were duplicated cases, to assess.
Figure 1.
Case appraisal form
Table 1.
Characteristics of the “paper patients”
| Clinical characteristic | No (%)* |
|---|---|
| Median (range) age (years) | 57.5 (39 to 71) |
| Median (range) % of ideal weight | 125.5 (103 to 158) |
| Sex: | |
| Male | 39 (78) |
| Female | 11 (22) |
| Smoking status: | |
| Non-smoker | 36 (72) |
| Smoker | 14 (28) |
| Expected morbidity/mortality related to procedure: | |
| Average | 40 (80) |
| Higher than average | 10 (20) |
| Exercise stress test: | |
| High risk | 40 (80) |
| Not high risk | 10 (20) |
| CCS angina grade: | |
| I | 5 (10) |
| II | 17 (34) |
| III | 14 (28) |
| IVa | 5 (10) |
| IVb | 5 (10) |
| IVc | 4 (8) |
| Left ventricular function: | |
| Normal | 32 (64) |
| Abnormal | 18 (36) |
| Left main stem stenosis: | |
| 0-49% | 43 (86) |
| 50-74% | 2 (4) |
| ⩾75% | 5 (10) |
| Severely diseased vessels: | |
| 0 | 4 (8) |
| 1 | 10 (20) |
| 2 | 15 (30) |
| 3 | 18 (36) |
| 4 | 3 (6) |
Except where stated otherwise. CCS=Canadian Cardiovascular Society.
Urgency
The exercise was carried out in two stages. Firstly, the doctor had to consider each case independently, and, using a visual analogue scale, indicate his or her views on the urgency of the case for surgery (fig 1). Doctors also indicated their views on the probable effectiveness of coronary bypass surgery in improving symptoms, reducing the risk of infarction, and extending the patient’s life.
Priority
When this work had been completed, the folder was returned to the authors. The cases, which had originally been in random order, were then reordered in the folder according to the urgency scores of the particular “judge” in question. At this stage, the 10 duplicate cases were removed. The judges were then asked to rearrange the cases, in any way they saw fit, to reach a final priority order for surgery (1-50).
Statistical methods
Multiple regression analysis was used to express the relation between judgments of urgency or priority for surgery and the demographic and clinical cues. Stepwise (backwards) elimination of variables was used to select these for the model. To minimise the risk of rejecting cues inappropriately, a relatively conservative P value of 0.10 was set.
The contribution of each cue to the model is represented by its contribution to r2, which was assessed by dropping each variable in turn from the model (the change in the type II sum of squares, cr2). We also compared equations from different judges in terms of the cr2 relative to that of all the other cues in the equation (rcr2)—a method that standardises for variation in the models’ explanatory power.9 Though neither method overcomes entirely the problem of collinearity, the rank order of importance of the cues in the decision models was not changed. (Data in table 2 relate to the first method.)
Table 2.
“Urgency” and “priority” decision models of three sample judges
| Judge | Age | Sex | Smoking | Body mass index | Expected morbidity related to procedure | Exercise stress test | CCS angina class | Left ventricular function | Left main stem stenosis | No of vessels affected | r2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urgency score | ||||||||||||
| 1 | Contribution to decision model (%) | — | — | 3 | — | — | 3 | 28 | — | 6 | 3 | 0.80 |
| Unstandardised β coefficient (95% CI) | — | — | −11.5 | — | — | 12.8 | 38.8 | — | 38.0 | 18.0 | ||
| (−21.2 to −1.72) | (0.63 to 25.1) | (24.7 to 53.1) | (5.0 to 71.0) | (1.7 to 34.3) | ||||||||
| 2 | Contribution to decision model (%) | — | — | — | — | — | — | 15 | — | 3 | — | 0.92 |
| Unstandardised β coefficient (95% CI) | — | — | — | — | — | — | 54.4 | — | 38.2 | — | ||
| (42.1 to 66.7) | (18.2 to 58.2) | |||||||||||
| 3 | Contribution to decision model (%) | — | — | — | — | 3 | — | 76 | — | 12 | — | 0.78 |
| Unstandardised β coefficient (95% CI) | — | — | — | — | 12.1 | — | 74.5 | — | 38.1 | — | ||
| (−0.2 to 24.4) | (60.2 to 88.8) | (20.3 to 55.9) | ||||||||||
| Priority ranks | ||||||||||||
| 1 | Contribution to decision model (%) | — | — | 2 | 2 | — | — | 38 | 2 | 8 | 4 | 0.88 |
| Unstandardised β coefficient (95% CI) | — | — | 4.2 | 0.1 | — | — | −24.4 | −5.1 | −24.3 | −10.3 | ||
| (0.6 to 7.8) | (0.04 to 0.3) | (−29.4 to −19.4) | (−9.2 to −1.0) | (−38.8 to −9.8) | (−16.6 to −4.0) | |||||||
| 2 | Contribution to decision model (%) | — | — | — | — | — | — | 9 | — | 1 | — | 0.93 |
| Unstandardised β coefficient (95% CI) | — | — | — | — | — | — | −14.3 | — | −9.8 | — | ||
| (−18.9 to −9.8) | (−17.2 to −2.4) | |||||||||||
| 3 | Contribution to decision model (%) | — | 3 | — | 2 | — | 5 | 51 | — | 4 | — | 0.88 |
| Unstandardised β coefficient (95% CI) | — | 6.0 | — | −0.2 | — | −8.6 | −31.8 | — | −10.4 | — | ||
| (2.0 to 10.1) | (−0.3 to −0.05) | (−13.0 to −4.1) | (−36.9 to −26.7 ) | (−16.5 to −4.3) | ||||||||
The regression coefficients represent the strength of effect on the dependent variable. Categorical variables (with n categories) were fitted when appropriate, using n-1 dummy variables.
Results
Sixteen cardiologists, four general practitioners, four cardiac surgeons, and nine consultant physicians with an interest in cardiology participated. There was a high intraclass correlation between urgency scores for the 10 duplicate cases (mean:median, 0.79:0.88).10
Determinants of variability in responses
Before determining the urgency and priority policy models of each judge, we assessed which case characteristics were associated with greater or lesser dispersion in responses between doctors. More severe angina class and left main stem stenosis were associated with less dispersion in responses for urgency scores (t=4.7, P=0.0001; and t=5.2, P=0.0001 respectively). Smoking habit was the major determinant of the scatter of priority ranks, as greater variation was seen in priority ranks for smoking than non-smoking patients (t=2.4; P=0.02).
Initial decision models
Once it had been determined that some case characteristics affected the variability in responses between doctors, a decision model was derived for each of the 33 judges. Table 2 illustrates the results for three judges. As well as giving the regression coefficients (expressing the change in urgency score, or priority rank, for a unit change in the value of the cue), table 2 shows the relative contribution of each cue to the final decision model (calculated as described in the methods section). The models generally had high explanatory power—the mean r2 was 73% for urgency judgments and 82% for priority judgments. (Details are available from us.)
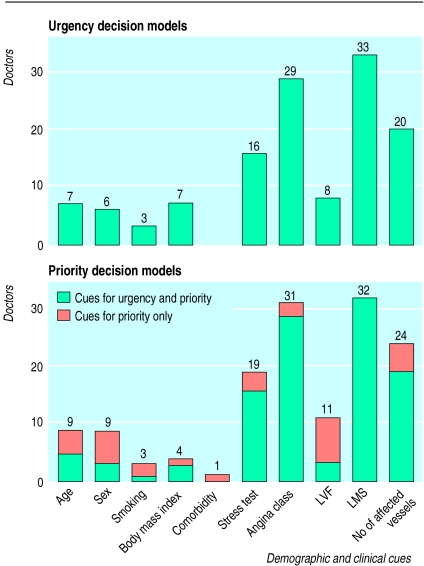
Figure 2 shows the frequency of demographic and clinical clues in the doctors’ decision models. Consensus is evident on the inclusion of major clinical variables such as angina class, left main stem disease, and the extent of disease (the number of vessels affected). However, even with allowance for a 1 in 10 chance of a type I error (that is, including a variable with no explanatory power in reality), the urgency judgments of a few doctors were affected by the demographic cues of age, sex, smoking habit, and body mass index (weight(kg)/(height(m)2). Figure 2 also shows that for some doctors the demographic variables affected priority judgments independently of their influence on perceived urgency.
Figure 2.
Frequency of demographic and clinical cues in decision models of urgency and priority. LVF=left ventricular function, LMS = left main stem stenosis
Models including perceptions of efficacy
Perceptions of urgency and priority may be influenced not only by the weighting given to particular clinical cues but also by the doctors’ perceptions of the probable efficacy of surgery in particular patients. We derived further policy models, after introducing into the equation the judge’s views about the capacity of the operation to relieve symptoms, to reduce the risk of infarction, and to prolong the patient’s life. The rationale behind this was that if a variable—for example, smoking—were an arbiter of priority judgments, its effects might logically be mediated by its influence on the perceived capacity to benefit. A modest improvement in the fit of the models resulted. The mean r2 for all doctors increased from 73% to 80% for judgments on urgency and from 82% to 86% for those on priority.
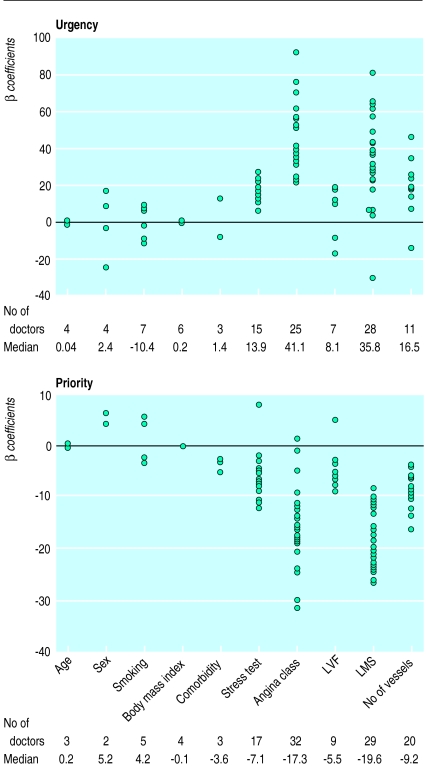
Although a few models were influenced by the demographic cues, the magnitude of this effect (reflected by the β or regression coefficient, which expresses the change in priority rating that accrues from each unit change in the clinical variables) was generally much smaller than that of the major clinical cues such as the severity of angina or left main stem stenosis (fig 3).11
Figure 3.
β Coefficients (unstandardised) for clinical cues in decision models of urgency and priority. Age=per decade, sex=men v women, smoking=smokers v non-smokers, body mass index=per additional 10% above ideal, stress test=high risk v not high risk, angina class=stable angina (grade IVb/c v Canadian Cardiovascular Society grade I/II, LVF=abnormal v normal left ventricular function, LMS=left main stem stenosis >75% v <50%, no of affected vessels=⩾3 affected v 0 or 1
Discussion
What do we think scoring systems will achieve?
Our approach differs from that of the Ontario group. Firstly, by using data from real patients we hoped to avoid the potential for unrealistic combinations of clinical cues. Secondly, we derived decision policy models for each judge, whereas Naylor et al produced a composite regression model after averaging the ratings of their panellists.3 The validity of such an approach has been seriously questioned.11 Thirdly, we addressed the influence of demographic and lifestyle factors and the judges’ beliefs about the probable efficacy of surgery.
We differed from the New Zealand group, too, in that we distinguished between urgency and priority, and we showed that this can affect the weight given to some factors.5 However, the wording in the New Zealand study is noteworthy: “Physicians were asked to consider what a reasonable waiting time would be for each patient, considering an adequately, not infinitely funded service.... Reasonable waiting time was considered indicative of likely benefit and used as the outcome variable in our analyses.”5 Note the tautology in their approach. Weights (supposedly reflecting the capacity for surgery to affect life expectancy or quality of life) were first gleaned from published reports and then “adjusted” after observing their correspondence with the regression weights, which were derived under an assumption of adequate funding. It can only be assumed that adequate funding implies that those with a material capacity to benefit would have surgery provided.
Somewhat perversely, a few of the weights, such as that applicable to age, were imposed on or adjusted externally to the scoring system. In addition, the dataset was pruned to exclude non-elective cases, so there was a preconceived notion of capacity to benefit that was not subject to investigation.5 Debate about what constitutes a non-elective case is bound to be vigorous—the urgency and magnitude of any benefits of surgery in patients with unstable angina are different, but they have been overestimated by many doctors.
What do we think surgery will achieve?
The apparent consensus over including clinical variables such as the angina class or extent of disease in the urgency and priority policy models in our study was not surprising. Meta-analyses have already shown how these variables may affect the outcome of revascularisation.12,13 For groups devising urgency scoring systems based on these variables, however, a few caveats exist. Firstly, we cannot assume that cardiologists are always able to assess objectively the relation between the patient’s clinical history and the state of his or her coronary anatomy.14 Some may systematically overestimate the degree of luminal stenosis before treatment and underestimate the residual stenosis, which might give a biased view of treatment success.15
Secondly, clinicians seem to weight reduction in the risk of death more than improvement in symptoms.16 This would seem reasonable, if doctors did not tend to overestimate risk17 and to believe that most patients who die while waiting for revascularisation would have been saved by surgery.18 Even in our fairly expert group the average perceived gain in life expectancy from surgery for the 29 patients who had neither left main stem disease nor triple vessel disease was 2.5 years.19 Finally, although the state of the coronary anatomy and angina class were included in most final decision models, our preliminary analysis clearly indicated that these factors were important determinants of the variation in the judgments made by these doctors.
Are we driven by the evidence or by our values?
Demographic variables have been the focus of more contentious debate. While little evidence exists that the relative efficacy of surgery (that is, compared with continued medical treatment) is any different for smokers than for non-smokers,20 or for fat patients than for lean ones,21 or, within bounds, for young than for old people, we surmised that a clinician who would give priority to one group or another would do so from such a belief.
Before perceptions of surgical efficacy were included in decision models for priority, the numbers of doctors influenced appreciably by demographic and lifestyle variables were: three for smoking habit, four for body mass index, and nine for age. When doctors’ perceptions of the effectiveness of revascularisation were included in the models, only one of the three doctors eliminated smoking habit and two of the four eliminated body mass index as important determinants. However, age was eliminated in all nine instances. The overall numbers of doctors for whom smoking habit, body mass index, or age were significant determinants (either with or without accounting for their views on efficacy) were six, seven, and 11 respectively. Our conclusion, for the lifestyle characteristics at least, is that when these variables were deemed important in decisions about priority for surgery, their influence was usually independent of effects they were perceived to have on surgical efficacy.
Consensus on allocating priority was difficult to achieve because original clinical trials were not designed to determine the risks of delay. Judgments about the appropriateness of care may nevertheless be affected by how the outcomes and the risks are perceived. Indeed, sometimes “we may enter a debate with an established prior belief, bias or prejudice ... and seek to maintain established medical or scientific paradigms by selecting evidence that supports those beliefs.”22 By sharing their decision models in discussion groups, our doctors made the impact of prior beliefs more evident. Only a few were influenced noticeably by demographic variables in their decisions about urgency or priority. In fact, the size of the effect of these variables was far outweighed by the clinical cues. There are thus important lessons for those taking forward the recommendations of the Clinical Standards Advisory Group.
Firstly, health authorities who adopt the Ontario or New Zealand scoring systems must note that these do not take account of the distinction between urgency and priority—a distinction we find many clinicians seem to make. Secondly, the relative weight that doctors give to clinical and demographic or lifestyle factors is different for urgency and priority judgments. As Hughes and Griffiths point out: “The overlap between a technical discourse dealing with risk and a moral discourse dealing with character opens the way for unacknowledged shifts between the two. There is space for doctors to act according to their perceptions of deservingness, while accounting for their actions in terms of medical benefit.”23
Footnotes
Funding: British Heart Foundation.
Conflict of interest: None.
References
- 1.Clinical Standards Advisory Group. Coronary artery bypass grafting and coronary angioplasty. Access to and availability of specialist services. London: HMSO; 1993. [Google Scholar]
- 2.Naylor CD, Basinski A, Baigrie R, Goldman B, Lomas J. Placing patients in the queue for coronary revascularisation: evidence for practice variations from an expert panel process. Am J Public Health. 1990;80:1246–1252. doi: 10.2105/ajph.80.10.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naylor CD, Baigrie R, Goldman B, Basinski A. Assessment of priority for coronary revascularisation procedures. Lancet. 1990;335:1070–1073. doi: 10.1016/0140-6736(90)92640-4. [DOI] [PubMed] [Google Scholar]
- 4.Naylor CD, Levinton C, Baigrie RS. Adapting to waiting lists for coronary revascularisation. Do Canadian specialists agree on which patients come first? Chest. 1992;101:715–722. doi: 10.1378/chest.101.3.715. [DOI] [PubMed] [Google Scholar]
- 5.Hadorn DC, Holmes AC. The New Zealand priority criteria project. Part 2. Coronary artery bypass graft surgery. BMJ. 1997;314:135–138. doi: 10.1136/bmj.314.7074.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Underwood MJ, Bailey JS. Coronary bypass surgery should not be offered to smokers. BMJ. 1993;306:1047–1048. doi: 10.1136/bmj.306.6884.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zolese G. Each patient is a special case. BMJ. 1993;306:1408. doi: 10.1136/bmj.306.6889.1408-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kee F, Gaffney B. Priority for coronary artery bypass surgery: who gets by-passed when demand outstrips capacity? Q J Med. 1995;88:15–22. [PubMed] [Google Scholar]
- 9.Darlington RB. Multiple regression in psychological research. Psychol Bull. 1968;3:161–182. doi: 10.1037/h0025471. [DOI] [PubMed] [Google Scholar]
- 10.Fleiss JL. The design and analysis of clinical experiments. New York: Wiley; 1986. [Google Scholar]
- 11.Brehmer B, Joyce CRB, editors. Human judgement: the social judgement theory view. Amsterdam: Elsevier; 1988. [Google Scholar]
- 12.Nwasokwa O, Koss J, Friedman G, Grunwald A, Bodenheimer M. Bypass surgery for chronic stable angina: predictors of survival benefit and strategy for patient selection. Ann Intern Med. 1991;114:1035–1049. doi: 10.7326/0003-4819-114-12-1035. [DOI] [PubMed] [Google Scholar]
- 13.Wong J, Sonnenber F, Salem D, Pauker S. Myocardial revascularisation for chronic stable angina. Analysis of the role of percutaneous transluminal coronary angioplasty based on data available in 1989. Ann Intern Med. 1990;113:852–871. doi: 10.7326/0003-4819-113-11-852. [DOI] [PubMed] [Google Scholar]
- 14.Klein L, Liebson P. Coronary angiography in patients with established coronary artery disease. How much does the angiogram help in assessing changes in symptoms? Cathet Cardiovasc Diagn. 1994;32:330–331. doi: 10.1002/ccd.1810320408. [DOI] [PubMed] [Google Scholar]
- 15.Kimball B, Bui S, Cohen E, Cheung P, Lima V. Systematic bias in the reporting of angioplasty outcomes: accuracy of visual estimates of absolute lumen diameters. Can J Cardiol. 1994;10:815–820. [PubMed] [Google Scholar]
- 16.Li TCM, Sherman H, Cook EF, Mudge GH, Mitchell N, Flatley M, et al. The selective impact of a cardiology data bank on physicians therapeutic recommendations. Med Decis Making. 1984;4:165–176. doi: 10.1177/0272989X8400400205. [DOI] [PubMed] [Google Scholar]
- 17.Rover S, Lowensteyn I, Esrey K, Steinert Y, Joseph L, Abrahamowicz M. Do doctors accurately assess coronary risk in their patients ? Preliminary results of the coronary health assessment study. BMJ. 1995;310:975–978. doi: 10.1136/bmj.310.6985.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kee F, Gaffney B, Canavan C, Little J, McConnell W, Telford AM, et al. Expanding access to coronary artery bypass surgery: who stands to gain? Br Heart J. 1995;73:129–133. doi: 10.1136/hrt.73.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kee F, McDonald P, Kirwan J, Patterson CC, Love AHG. What is a safe waiting time for coronary artery bypass surgery? Q J Med. 1997;90:669–676. doi: 10.1093/qjmed/90.11.669. [DOI] [PubMed] [Google Scholar]
- 20.Julian D. Smoking and coronary heart disease. Br Heart J. 1994;72:9–11. doi: 10.1136/hrt.72.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prasad US, Walker WS, Sang CT, Campanella C, Cameron EW. Influence of obesity on the early and long term results of surgery for coronary artery disease. Eur J Cardiothoracic Surg. 1991;5:65–73. doi: 10.1016/1010-7940(91)90003-3. [DOI] [PubMed] [Google Scholar]
- 22.West R. Assessment of evidence versus consensus or prejudice. J Epidemiol Community Health. 1992;46:321–322. doi: 10.1136/jech.46.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes D, Griffiths L. “But if you look at the coronary anatomy ...”: risk and rationing in cardiac surgery. Sociology of Health and Illness. 1996;18:172–197. doi: 10.1111/1467-9566.ep10934703. [DOI] [PubMed] [Google Scholar]