Summary
Background
Few studies have investigated the relationship between the food and physical activity environment and odds of gestational diabetes mellitus (GDM). This study quantifies the association between densities of several types of food establishments and fitness centers with the odds of having GDM.
Methods
The density of supermarkets, fast-food restaurants, full-service restaurants, convenience stores and fitness centers at 500, 1000 and 1500 m (m) buffers was counted at residential addresses of 68,779 pregnant individuals from Eastern Massachusetts during 2000–2016. The ‘healthy food index’ assessed the relative availability of healthy (supermarkets) vs unhealthy (fast-food restaurants, convenience stores) food retailers. Multivariable logistic regression quantified the cross-sectional association between exposure variables and the odds of having GDM, adjusting for individual and area-level characteristics. Effect modification by area-level socioeconomic status (SES) was assessed.
Findings
In fully adjusted models, pregnant individuals living in the highest density tertile of fast-food restaurants had higher GDM odds compared to those living in the lowest density tertile (500 m: odds ratio (OR):1.17 95% CI: [1.04, 1.31]; 1000 m: 1.33 95% CI: [1.15, 1.53]); 1500 m: 1.18 95% CI: [1.01, 1.38]). Greater residential density of supermarkets was associated with lower odds of GDM (1000 m: 0.86 95% CI: [0.74, 0.99]; 1500 m: 0.86 95% CI: [0.72, 1.01]). Similarly, living in the highest fitness center density tertile was associated with decreased GDM odds (500 m:0.87 95% CI: [0.76, 0.99]; 1500 m: 0.89 95% CI: [0.79, 1.01]). There was no evidence of effect modification by SES and no association found between the healthy food index and GDM odds.
Interpretation
In Eastern Massachusetts, living near a greater density of fast-food establishments was associated with higher GDM odds. Greater residential access to supermarkets and fitness centers was associated with lower the odds of having GDM.
Funding
NIH.
Keywords: Food environment, Fast-food restaurant, Full-service restaurant, Supermarket, Fitness center, Gestational diabetes mellitus
Research in context.
Evidence before this study
We searched Google Scholar for epidemiological studies reporting on the association between the food environment and gestational diabetes mellitus. We used the following search terms: (“food environment” OR “supermarket” OR “fast-food” OR “convenience store” OR “restaurant” OR “fitness center”) AND (“gestational diabetes mellitus” OR “GDM” OR “maternal diabetes”). Our search was limited to studies published before October 1, 2023. Previous studies conducted in the US have had mixed findings regarding the association between less healthy food environments and odds of GDM. Existing studies typically have used only a single food environment indicator (e.g. grocery store density or fast-food restaurant density) and measured the density at a census tract or zip-code level. These single measures of grocery store or restaurant density do not adequately capture the complexity of the food environment, which contains a multitude of food establishment types. Additionally, no prior US studies have examined the association between fitness center density and the odds of having GDM.
Added value of this study
This analysis of approximately 70,000 pregnant individuals in Eastern Massachusetts is one of the first to examine multiple indicators of the food environment (density of supermarkets, fast-food restaurants, full-service restaurants and convenience stores) and physical activity environment (fitness center density) at a residential scale (500 m, 1000 m, 1500 m from an individual's household) to assess their associations with the odds of developing GDM. We demonstrate that a greater density of fast-food retailers is associated with increased odds of GDM after adjusting for relevant socioeconomic and individual factors. We detected associations between these exposures and GDM at all examined spatial scales. We also found that living in an area with a higher density of supermarkets and fitness centers was associated with a lower odds of GDM at multiple buffers.
Implications of all the available evidence
The study findings underscore the potential for a reduction in fast-food restaurant density and an increase in supermarket density to encourage more healthy dietary patterns and possibly reduce the odds of GDM in Eastern Massachusetts. Greater residential access to fitness centers may also protect against the odds of having GDM. Policymakers and city planners should consider zoning laws that lower the number of fast-food restaurants and replace with supermarkets or other affordable healthier food options to potentially help mitigate the burden of GDM. Expanding access to affordable indoor fitness centers may also help lower the prevalence of GDM in Eastern Massachusetts.
Introduction
Gestational diabetes mellitus (GDM), which is the onset or first recognition of glucose intolerance during pregnancy, affects an estimated 2–10% of pregnant individuals in the US.1 GDM can result in long-term metabolic risk to both the mother and child.2 While several unmodifiable odds factors have been identified for GDM, including advanced maternal age and family history of diabetes,3 diet and exercise are modifiable risk factors and key prevention and therapeutic strategies for GDM.4
In turn, dietary behavior can be affected by the availability, accessibility, and affordability of healthy food options.5 For example, the presence of a supermarket around an individual's residence may lead to increased consumption of fresh fruits and vegetables.6 Similarly, research has indicated that living in proximity to fitness centers increases exercise levels.7
Analyses have shown that the food and physical activity environment can affect dietary quality and exercise levels, respectively, during pregnancy.8,9 Studies conducted in Delaware,10 New York11 and Texas12 also have found a link between less healthy food environments and increased odds of GDM. However, these studies have focused on a single food environment indicator (e.g. grocery store density only) and measured the density at the census tract or zip-code level. Thus, these studies were unable to comprehensively assess the food environment and examine heterogeneity in access to healthy food and fitness centers at a more granular spatial scale. Understanding whether the density of healthy food options at small scales (e.g. 5-min walk) can reduce the odds of having GDM may help inform future urban planning policies (e.g. via zoning laws).13
To our knowledge, no studies have assessed the relationship between fitness center density and the odds of having GDM. Studies have typically investigated the relationship between urban greenspace as a proxy of access to recreational spaces for engaging in outdoor activities.14 However, some studies have not found associations between access to greenspace and physical activity level.15 Additionally, greenspace access may not be a suitable surrogate measure of overall physical activity during pregnancy in northern areas due to cold temperatures in winter months that may shift individuals’ exercise regimen predominantly indoors. Thus, fitness center density may be a more accurate measure of physical activity by incorporating indoor spaces.
Socioeconomic status (SES) may shape dietary and physical activity behaviors of individuals through the quantity and quality of food options available in their neighborhood,16 sensitivity to food prices,17 and the availability of transportation modes, which affects the accessibility of foods and physical activity spaces.18 For example, a study conducted in the UK uncovered that unhealthy food outlets were more likely to be associated with poorer dietary quality among mothers with lower educational attainment.19 Therefore, the association between the food and physical activity environment and the odds of having GDM may vary by SES.
This cross-sectional analysis (1) examines associations between densities of a wide range of food establishments and fitness centers with odds of having GDM in Eastern Massachusetts, USA and (2) assesses whether the associations differ by SES.
Methods
Study population
Prenatal and obstetric data was obtained for births that occurred at Beth Israel Deaconess Medical Center (BIDMC) from 2000 through 2016. BIDMC is a private, tertiary-care hospital in Boston, MA that serves Eastern Massachusetts. Data included maternal residential address; delivery characteristics; demographics; and medical and obstetric history, including diagnosis of type 2 diabetes or GDM. GDM was defined in the dataset based on International Classification of Diseases (ICD)-9 and ICD-10 codes (Supplementary Table S1).
Of the 69,815 identified pregnancies, those with pregestational diabetes (1.5%; n = 1036) were excluded since they would not meet the criteria for a GDM diagnosis, which is defined as onset or first recognition of glucose intolerance during pregnancy. The final analytic sample included 68,779 pregnant women.
Exposure variables
Density of food establishments and fitness centers across the contiguous US from every two-year period from 1998 to 2016 was obtained from the Infogroup US Historical Business Data.20 This database contains geocoded information and industry classifications as of the last day of the year. All establishments with ≥20 locations across the US were classified into the following categories: “fast-food restaurant”, “full-service restaurant”, “convenience store”, “supermarket or grocery store” and “fitness or recreational sport center”. Entities with >20 locations across the US were added to these categories based on the North American Industry Classification System 6-digit (NAICS6) codes. The NAICS6 codes are the standard used by Federal statistical agencies for classifying business establishments in the US census.
Limited-service restaurants and snack and non-alcoholic beverage bars identified from NAICS6 codes were included in the “fast-food restaurant” category. Supermarkets, grocery stores, warehouse clubs and supercenters were grouped into the “supermarket or grocery store” category.
Using Google Earth Engine and R,21 rasters of 100 square meter grid cells covering the contiguous US were developed every two years from 1998 to 2016. We counted all entities of each category (fast-food restaurants, full-service restaurants (restaurants), convenience stores, supermarkets, and fitness centers) in circular buffers of 500, 1000, and 1500 m around each grid cell. A 500 m radius represents around a 10-min walk, while a 1000–1500 m buffer is equivalent to a walking time of approximately 15–20 min.22 These buffer sizes likely capture a radius beyond which most individuals would not be willing to travel to food retailers23 and therefore probably represent most of their residential food consumption.
As the distribution of the exposure variables was skewed left due to a high percentage of residences having zero retailers within 500–1500 m, all food and physical activity density variables were grouped into tertiles such that approximately one-third of respondents fell into each category. The tertile cutoffs varied by buffer size. The tertile with the lowest density was used as the referent category. The exposure variables were linked to participants’ residential address on the date of delivery to conduct a cross-sectional analysis examining the density of food establishments and fitness centers during their pregnancy as the exposures of interest.
Healthy food index
The US Center for Disease Control (CDC) developed the Modified Retail Food Environment Index (mRFEI)24 to compare the number of healthy and less healthy food retailers within census tracts across the US:
mRFEI = number of healthy food retailers/(number of health food retailers + number of less healthy food retailers).
For the mRFEI definition, healthy food retailers include supermarkets, grocery stores, supercenters, and produce stores while less healthy food retailers include fast-food restaurants, small grocery stores, and convenience stores.
In line with the mRFEI, we created the “healthy food index”:
Healthy food index = number of supermarkets/(number of supermarkets + number of fast-food restaurants + number of convenience stores).
Covariates
Individual-level covariates abstracted from BIDMC medical records included marital status, maternal age, maternal education, insurance type (public/private), parity and fetal sex. Self-reported maternal race and ethnicity was also included as a covariate in the models as an indicator of differences in residential patterns that influence the local environment and a marker of structural racism that can influence pregnancy outcomes.25
Zip code-level median household income and population density obtained from the 2010 US census were additionally linked to the dataset. The tertiles for population density were 0–2685 people/mile2; 2686–10,000 people/mile2; >10,000 people/mile2. The Area Deprivation Index (ADI), which is a composite measure of 17 census variables designed to describe socioeconomic disadvantage across the entire US based on income, education, employment, and housing quality, was obtained through the Neighborhood Atlas.26 ADI was available at the census tract level.
Statistical analysis
Spearman correlation coefficients between all food and physical activity variables were calculated to assess for potential multicollinearity. If a particular food or physical activity environment variable was highly correlated (correlation coefficient ≥0.90) with other exposure variables at any buffer, that exposure variable was removed from final, adjusted models (at all buffers) to generate more precise effect estimates.
Logistic regression was used to assess the relationship between the food and physical activity environment and the odds of GDM. The lowest tertile of each exposure was compared to the middle and highest tertile when generating odds ratios. As a robustness check, we also modeled food and physical activity environment variables as dichotomous (above/below median density) exposures.
First, we built unadjusted logistic regression models containing only the food and physical activity environment variables. Then, we simultaneously added in potential confounding variables based on an a priori believed association with the exposure and outcome. All potential confounders were retained in the final model, regardless of their impact on model fit.
Models were built separately at each buffer (500 m, 1000 m, 1500 m) to assess consistency in the effect estimates as a robustness check. Within each buffer, two exposure models were built: (1) a model that included the density of each individual food retailer (supermarkets, fast-food restaurants, full-service restaurants, convenience stores) and fitness centers and (2) a model that included the healthy food index and fitness center density. Model (1) quantified the independent effect of each exposure variable, and model (2) assessed whether the ratio of healthy to unhealthy food establishments would produce a stronger association with GDM than the density of each individual food establishment. ADI was tested as an effect modifier using an interaction term in all models.
All analyses were performed in R (version 4.1.1).21 Ethical approval was obtained from the institutional review boards of Harvard T.H. Chan School of Public Health and Beth Israel Deaconess Medical Center. Informed consent was not needed as the data was previously collected from medical and administrative records.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
The prevalence of GDM among the 68,779 study participants was 4.5% (n = 3094). A greater proportion of White individuals were likely to live in areas with the lowest density of fast-food restaurants (n = 16,869; 69%) compared with medium (n = 11,809; 49%) or high density (8983; 45%) (Table 1). For all other races/ethnicities, a greater proportion lived in areas within the middle or highest tertile of fast-food restaurant density than the lowest tertile (Table 1). Population density was strongly correlated with fast-food restaurant and supermarket density; half of individuals in the lowest tertile of population density lived in areas with the lowest density of fast-food restaurant (Supplementary Table S2) and supermarket density (Supplementary Table S3).
Table 1.
Characteristics of study population (n = 68,779) by tertile of fast-food restaurant density at 1500 m buffer.
| Low (0–6) (N = 24,409) | Middle (7–16) (N = 24,317) | High (17+) (N = 20,064) | |
|---|---|---|---|
| Age (Mean (SD)) | 32.6 (4.8) | 31.2 (5.5) | 31.2 (5.2) |
| Race/ethnicity (N (%)) | |||
| White | 16,869 (69) | 11,809 (49) | 8983 (45) |
| Black | 1783 (7) | 4011 (16) | 2003 (10) |
| Hispanic | 603 (2) | 1658 (7) | 1429 (7) |
| Asian | 2089 (9) | 3472 (14) | 4162 (21) |
| Unspecified | 3065 (13) | 3367 (14) | 3487 (17) |
| Insurance (N (%)) | |||
| Public/uninsured | 1964 (8) | 4908 (20) | 4083 (20) |
| Private | 22,445 (92) | 19,409 (80) | 15,981 (80) |
| Maternal education (N (%)) | |||
| College or higher | 7312 (30) | 6645 (27) | 5364 (27) |
| Lower than college | 2844 (12) | 5085 (21) | 4096 (20) |
| Unspecified | 14,253 (58) | 12,587 (52) | 10,604 (53) |
| Parity (N (%)) | |||
| First born | 9857 (40) | 11,640 (48) | 11,193 (56) |
| Second or more | 14,552 (60) | 12,677 (52) | 8871 (44) |
| Population density (N (%)) | |||
| Low (0–2685 people/mile2) | 16,612 (68) | 5115 (21) | 631 (3) |
| Middle (2686–10,000 people/mile2) | 6334 (26) | 11,897 (49) | 4499 (22) |
| High (>10,000 people/mile2) | 1457 (6) | 7303 (30) | 14,931 (74) |
| Area deprivation index (Mean (SD)) | 13.36 (9.89) | 18.59 (11.78) | 15.33 (11.13) |
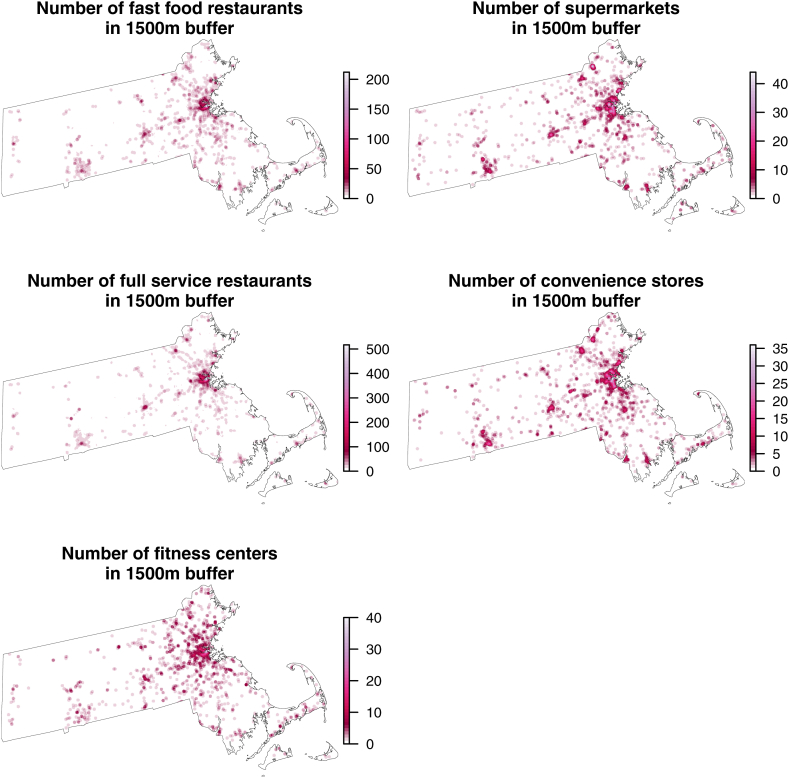
The density of the food and physical activity environmental variables at a 1500 m buffer was highest in more urban settings within Massachusetts (e.g. Boston metro area) (Fig. 1). The distribution of the exposure variables was similar at 500 m (Supplementary Figure S1) and 1000 m buffers (Supplementary Figure S2).
Fig. 1.
Map of food and physical activity environment (density at 1500 m) in Massachusetts.
The density of full-service restaurants was highly correlated (rSpearman ≥0.90) with the density of fast-food restaurants, supermarkets, and convenience stores at a 1500 m buffer (Supplementary Table S4). Due to multicollinearity, full-service restaurant density was removed from models assessing the association between each other exposure variable and the odds of having GDM.
Spearman correlations between fitness centers and each of the food environment variables were lower, ranging from 0.60 to 0.74 at 500-m and 1000-m buffers and 0.70–0.80 at a 1500-m buffer (Supplementary Tables S5 and S6).
There also was a high correlation between the density of each exposure variable at each buffer size, with Spearman correlation coefficients ranging from 0.70 to 0.90 (Supplementary Tables S7–S10). Correlations between the density of fitness centers at the three buffer sizes were slightly lower (rSpearman = 0.55–0.85) (Supplementary Table S11).
Multivariable modeling
While the number of food establishments and fitness centers included in each tertile varied by buffer size (Supplementary Table S12), living in the highest density tertile of supermarkets and fitness centers was associated with lower odds of having GDM in nearly all buffers in unadjusted models (Table 2). Conversely, an increasing density of fast-food restaurants, full-service restaurants and convenience stores were associated with greater GDM odds in unadjusted models.
Table 2.
The association between food and physical activity environment variables and the odds of having gestational diabetes mellitus (GDM) in Eastern Massachusetts (n = 68,779 pregnancies).
| Exposure | Buffer | Density tertile (# in buffer) (ref = lowest) | Unadjusted odds ratio (95% CI)a | Adjusted odds ratio (95% CI)b |
|---|---|---|---|---|
| Supermarkets | 500 m | 1–2 | 1.06 (0.97, 1.17) | 1.04 (0.94, 1.15) |
| 3+ | 1.01 (0.89, 1.14) | 1.02 (0.89, 1.17) | ||
| 1000 m | 1–4 | 0.94 (0.84, 1.05) | 0.90 (0.81, 1.00)d | |
| 5+ | 0.84 (0.73, 0.97)d | 0.86 (0.74, 0.99)d | ||
| 1500 m | 3–10 | 1.12 (0.99, 1.26) | 1.02 (0.90, 1.15) | |
| 11+ | 0.91 (0.78, 1.06) | 0.86 (0.72, 1.01) | ||
| Fast-food restaurants | 500 m | 1–2 | 1.08 (0.98, 1.19) | 1.08 (0.97, 1.19) |
| 3+ | 1.17 (1.05, 1.32)d | 1.19 (1.06, 1.33)d | ||
| 1000 m | 3–8 | 1.20 (1.07, 1.34)d | 1.17 (1.04, 1.31)d | |
| 9+ | 1.37 (1.19, 1.57)d | 1.33 (1.15, 1.53)d,e | ||
| 1500 m | 7–16 | 1.17 (1.04, 1.31)d | 1.11 (0.98, 1.24) | |
| 17+ | 1.26 (1.09, 1.47)d | 1.18 (1.01, 1.38)d | ||
| Full-service restaurantsc | 500 m | 1–6 | 1.34 (1.23, 1.46)d | 1.19 (1.06, 1.33)d |
| 7+ | 1.11 (1.01, 1.22)d | 0.99 (0.84, 1.16) | ||
| 1000 m | 6–22 | 1.18 (1.08, 1.28)d | 0.99 (0.86, 1.13) | |
| 23+ | 1.11 (1.02, 1.21)d | 0.93 (0.77, 1.12) | ||
| 1500 m | 16–50 | 1.22 (1.12, 1.33)d | 1.07 (0.92, 1.23) | |
| 51+ | 1.09 (1.00, 1.20) | 1.14 (0.92, 1.42) | ||
| Convenience stores | 500 m | 1 | 1.08 (0.98, 1.20) | 1.01 (0.91, 1.12) |
| 2+ | 1.09 (0.98, 1.21) | 1.01 (0.90, 1.13) | ||
| 1000 m | 2–5 | 1.08 (0.98, 1.20) | 0.96 (0.86, 1.07) | |
| 6+ | 1.13 (0.99, 1.30) | 0.95 (0.82, 1.10) | ||
| 1500 m | 2–7 | 1.04 (0.93, 1.17) | 0.92 (0.82, 1.03) | |
| 8+ | 1.24 (1.06, 1.46)d | 0.98 (0.83, 1.16) | ||
| Fitness centers | 500 m | 1 | 0.97 (0.88, 1.08) | 0.97 (0.87, 1.07) |
| 2+ | 0.78 (0.69, 0.89)d | 0.87 (0.76, 0.99)d | ||
| 1000 m | 1–2 | 1.08 (0.98, 1.19) | 1.08 (0.98, 1.20) | |
| 3+ | 0.90 (0.79, 1.01) | 1.00 (0.88, 1.13) | ||
| 1500 m | 3–5 | 0.94 (0.86, 1.04) | 0.96 (0.87, 1.06) | |
| 6+ | 0.77 (0.68, 0.87)d | 0.89 (0.79, 1.01) |
Unadjusted models include all food establishment (except full-service restaurants due to multicollinearity) and fitness center exposures simultaneously.
Adjusted models additionally control for maternal race/ethnicity, maternal age, maternal education, parity, type of insurance (public/private), zip code-level median household income, zip code-level population density and Area Deprivation Index.
Odds ratios for full-service restaurant density do not include any other food environment variables (only fitness center density) due to multicollinearity.
Significant at alpha = 0.05 level.
Significant at alpha = 0.0017 level (Bonferroni correction applied).
In the final models, excluding full-service restaurant density as a covariate due to multicollinearity generated slightly narrower confidence intervals (Supplementary Table S13).
After adjusting for individual and area-level confounding variables, the significant protective association between supermarket and fitness center density with GDM odds remained (Table 2). However, the density of fast-food restaurants was the only exposure that was significantly associated with increased odds of GDM at all buffer sizes in fully adjusted models (Table 2).
Individuals living in the tertile with the highest density of fast-food restaurants within 500 m, 1000 m and 1500 m had 1.19 (95% CI: 1.06, 1.33), 1.33 (95% CI: 1.15, 1.55) and 1.18 (95% CI: 1.01, 1.38) times the odds, respectively, of developing GDM as those living in the tertile with the lowest fast-food restaurant density. Living in the highest tertile of supermarket density was associated with lower odds of GDM at a 1000 m buffer (0.86 95% CI: 0.74, 0.99) and marginally associated with lower odds of having GDM at a 1500 m buffer (0.86 95% CI: 0.72, 1.01) in the final model. Living in the highest density tertile of fitness centers was associated with lower GDM odds at a 500 m buffer (0.87 95% CI: 0.76, 0.99) and marginally associated with lower odds at a 1500 m buffer (0.89 95% CI: 0.79, 1.01).
These associations generally remained when conducting a sensitivity analysis with the food and physical activity environment exposures re-defined as dichotomous (above vs below median density) variable (Supplementary Table S14). In another sensitivity analysis involving a Bonferroni correction to account for multiple hypothesis testing, the association between fast-food restaurant density and the odds of having GDM remained significant only at the 1000 m buffer (Table 2).
There was not a consistent association between the healthy food index and GDM odds at any buffer size (Table 3).
Table 3.
The association between the healthy food index and other food and physical activity environment variables and the odds of having gestational diabetes mellitus (GDM) in Eastern Massachusetts (n = 68,779 pregnancies).
| Exposure | Buffer | Density (# in buffer) (ref = lowest) |
Unadjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) |
|---|---|---|---|---|
| Healthy food index | 500 m | Medium | 1.16 (1.05,1.30)a | 1.13 (1.01,1.27)a |
| High | 1.00 (0.90, 1.12) | 1.00 (0.89, 1.13) | ||
| 1000 m | Medium | 1.04 (0.94,1.15) | 1.04 (0.94, 1.15) | |
| High | 0.96 (0.87, 1.06) | 0.93 (0.84, 1.03) | ||
| 1500 m | Medium | 1.04 (0.95, 1.14) | 0.98 (0.90, 1.08) | |
| High | 0.97 (0.88, 1.06) | 0.96 (0.87, 1.06) | ||
| Fitness centers | 500 m | 1 | 0.96 (0.86, 1.07) | 0.97 (0.87, 1.08) |
| 2+ | 0.78 (0.69,0.88)a | 0.88 (0.77,0.99a | ||
| 1000 m | 1–2 | 1.13 (1.03,1.25)a | 1.13 (1.02,1.13)a | |
| 3+ | 1.01 (0.91, 1.24) | 1.09 (0.97, 1.23) | ||
| 1500 m | 3–5 | 1.08 (0.98, 1.18) | 1.02 (0.93, 1.12) | |
| 6+ | 0.93 (0.85, 1.02) | 0.97 (0.86, 1.09) |
Unadjusted models include all food establishment and fitness center exposures simultaneously. Adjusted models additionally control for maternal race/ethnicity, maternal age, maternal education, parity, type of insurance (public/private), zip code-level median household income, zip code-level population density and Area Deprivation Index (ADI).
Effect modification by socioeconomic status
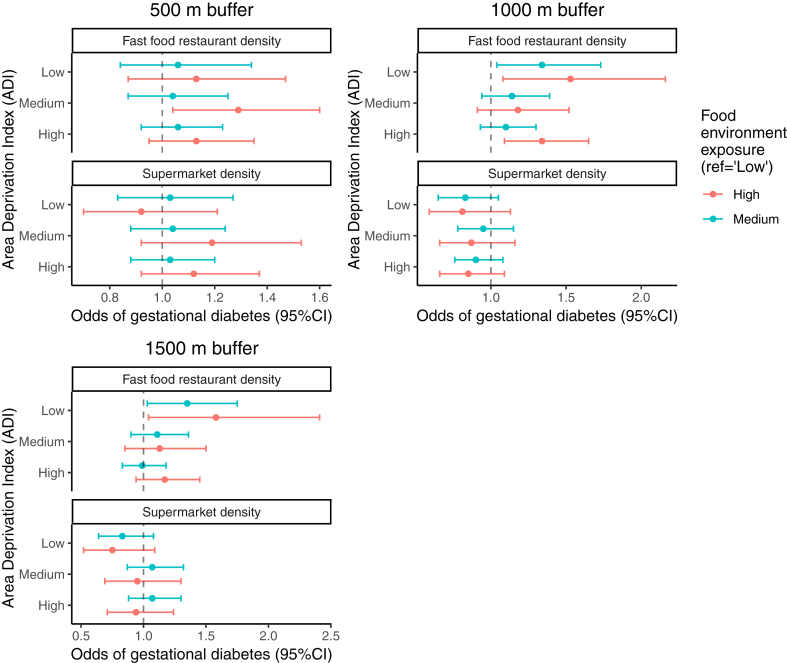
In models stratified by ADI, we did not find evidence of effect modification between fast-food restaurant density and the odds of having GDM (Fig. 2). However, the association appeared to be the most robust in low SES neighborhoods; in census tracts with the highest ADI, pregnant individuals living in the highest tertile of fast-food restaurant density had 1.13 (95% CI: [0.95, 1.35]), 1.34 (95% CI: [1.09, 1.65]) and 1.17 (95% CI: [0.94, 1.45]) times the odds of GDM as those living in the lowest tertile of fast-food restaurant density at 500, 1000 and 1500 m buffers, respectively (Supplementary Table S15). There was not significant effect modification by ADI in the association between supermarket density and the odds of having GDM (Fig. 2).
Fig. 2.
The association between density of fast-food restaurants and supermarkets stratified by Area Deprivation Index (ADI).
Discussion
This study of nearly 70,000 pregnant individuals examined the association between density of food establishments (e.g. supermarkets, convenience stores, fast-food restaurants, full-service restaurants) and fitness centers and GDM in Eastern Massachusetts. We firstly found that the density of fast-food restaurants was associated with higher odds of GDM (Table 2).
Two previous studies examining the association between fast-food restaurant density and the odds of having GDM have had mixed results.11,12 One study, which found no association between census tract-level density of fast-food restaurants and GDM odds in New York City, noted probable misclassification of the neighborhood food environment that likely biased the results toward the null. The other study, which was conducted in Houston, Texas and grouped fast-food restaurant density at a zip code-level into quartiles, found a significant association with the odds of having GDM that was similar in magnitude to those reported in this study (Table 3). While the Texas study found associations using density of fast-food restaurants at a zip code-level, we found a similar association between fast-food restaurant density and GDM odds at a residential level. Thus, the availability of fast-food restaurants in the immediate vicinity of residence may be important for shaping dietary behaviors during pregnancy.
There are several pathways that may explain why fast-food restaurant density was strongly associated with increased GDM odds. US studies have shown that those living closer to fast-food restaurants consume a less healthy diet,6 which contributes to weight gain and an elevated odds of GDM.27 Additionally, fast food in the US is typically high in saturated fat and added sugars; consuming these nutrients in high quantities can lead to insulin sensitivity28 and beta cell damage, which are precursors to GDM.29 Processed meats commonly consumed in fast-food restaurants contain certain compounds (e.g. nitrosamines) that can damage beta cells and cause oxidative stress.4 Moreover, fast food is low in fiber, which can protect against the development of GDM.30 Additionally, pregnancy-related fatigue may inhibit cooking and lead women to eat out more than they did pre-pregnancy.31
We additionally found that a greater density of supermarkets near participants' residences was associated with lower odds of GDM at multiple buffers (Table 2). Other studies have also found that greater access to supermarkets is associated with lower odds of having GDM.12,32,33 As studies have documented a link between supermarket proximity and greater dietary quality during pregnancy,8,11 increased consumption of healthier food at grocery stores can likely lower pregnant women's odds of obesity, which is a odds factor for GDM.34,35 Similarly, the association of increased density of fitness centers with lower GDM odds at multiple buffers is likely through the promotion of increased exercise before and/or during pregnancy, which many studies have shown reduces the odds of GDM.36
Socioeconomic status
We did not find evidence of effect modification by SES between the density of food retailers and odds of GDM (Fig. 2). However, other studies have reported that a lack of access to healthy foods can mediate the relationship between lower SES and higher body fat during pregnancy,37 and that lower neighborhood-level SES was associated with reduced vegetable consumption.38 Thus, research in other settings is warranted to determine if SES disparities exist in the relationship between the food environment the odds of having GDM among pregnant individuals.
Healthy food index
We did not find an association between a higher healthy food index and odds of GDM (Table 3). It is possible that the association was attenuated by the inclusion of convenience stores as an ‘unhealthy’ retailer when calculating the index since there was no association between residential density of convenience stores and GDM odds (Table 2). This lack of association may suggest that the food in convenience stores does not make up a substantial component of our study population's diet relative to the food available in supermarkets and at fast-food restaurants. This indicates the importance of prioritizing policies targeting specific food retailers (supermarkets, fast-food restaurants) when seeking to possibly help prevent GDM.
Strengths and limitations
A key strength of this study was the assessment of the food and physical activity environment at small spatial scales (500 m, 1000 m, 1500 m from residence), which more accurately represents individuals’ access to retail food establishments. We therefore increased the heterogeneity of our exposure profile from that of previous studies examining the food environment at a census tract or zip-code level.10,11 We adjusted for several individual and neighborhood-level SES indicators and included food and physical activity environment exposures in the same model to assess independent effects. However, we note that over half of participants did not specify their education level (Table 1), which may have led to slightly biased results. However, we believe our other variables of zip code-level median household income and ADI were able to capture potential confounding due to SES. The density of food establishments and fitness centers is not a perfect proxy of the actual frequency of visits to food outlets nor dietary or physical activity patterns, which could lead to residual bias. We do not expect exposure misclassification to vary by GDM status and therefore believe potential person-to-person variations in eating habits would likely be non-differential and bias towards a null finding.
The population of Eastern Massachusetts is generally of higher SES than the national US population; the median ADI in the US is 50, while the average ADI of our study population was approximately 16 (Table 1). Additionally, the prevalence of GDM in our study (4.5%) was slightly below that reported by other national studies, including the Nurses’ Health study (5–6%).39
Although our study population is racially and ethnically diverse, it is not necessarily representative of the Eastern Massachusetts population; patients of the Beth Israel Deaconess Medical Center are more highly educated and have higher enrollment in private health insurance plans than the general population. Thus, the generalizability of these findings may be limited to higher SES areas in Eastern Massachusetts.
Our food retailer and fitness center exposures were updated every two years to account for changes in establishments during the 15-year study period. We found that the median density of fast-food and full-service restaurants in Eastern Massachusetts roughly doubled across the study period (2000–2016) (Supplementary Table S16). Hence, our ability to use two-year windows to characterize the food environment represents another strength of this study. Other studies have used longer intervals (e.g. 5-years)10 when assessing the food environment, which are prone to greater exposure misclassification. Nonetheless, potential changes in the density of retailers over the course of participants’ pregnancy were not captured since the density of food establishments and fitness centers was only measured at the end of the calendar year. However, we expect that this will have had minimal effect on our results as the density of all food establishments and fitness centers did not typically increase by more than 1 vendor over a 2-year period (Supplementary Table S16).
We did not have information on whether our study participants were employed during their pregnancy; exposure misclassification will be present in our study if individuals travel to eateries or fitness centers beyond a 1500 m radius (e.g. near their office). We expect this misclassification to be non-differential and bias toward a null finding.
Despite nondifferential exposure misclassification due to possible variation in individuals’ eating habits within the same neighborhood (ecological fallacy), we detected robust associations at multiple buffers in our analysis. This highlights the potentially strong influence of the type of food establishments at a neighborhood-level on dietary behavior during pregnancy.
Conclusions
This study identifies the potential importance of reduced fast-food restaurant density in protecting against GDM. The influence of fast-food restaurant access on the odds of having GDM appears to be particularly important in lower income neighborhoods. Additionally, a greater density of supermarkets and fitness center may lower the burden of GDM. Hence, policymakers who wish to lower the burden of GDM in their communities should consider urban planning policies (e.g. zoning laws) that limit the number of fast-food establishments and promote the establishment of additional fitness facilities and supermarkets offering affordable, healthy food options.
Contributors
MS–conceptualisation, formal analysis, investigation, methodology, visualisation, writing–original draft. JOK–data curation, methodology, resources, writing–review & editing. ML–data curation, resources, writing–review & editing. JP–data curation, writing–review & editing. JPDC–data curation, writing–review & editing. AM–data curation, writing–review & editing. MH–data curation, writing–review & editing. HF–writing–review & editing. PJ–data curation, writing–review & editing. SHD–methodology, supervision, writing–review & editing. SP–conceptualisation, methodology, supervision, writing–review & editing. MS and JK accessed and verified the data. MS and SP were responsible for the decision to submit the manuscript.
Data sharing statement
The exposure data used in this study can be made available to researchers upon reasonable request directed to the corresponding author. The outcome data obtained from Beth Israel Deaconess Medical Center cannot be shared for confidentially purposes.
Editorial disclaimer
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
Jean-Philippe Drouin-Chartier received consulting fees from Dairy Farmers of Canada (unrelated to this manuscript).
Acknowledgements
Research reported in this publication was supported by the National Institute of Environmental Health Sciences of the National Institutes of Health (NIH) under Award Number R01ES034038. Dr. Matthew Shupler is funded by a T32 training grant (T32HD104612) awarded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the NIH.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2024.100775.
Appendix A. Supplementary data
References
- 1.National Institute of Diabetes and Digestive and Kidney Diseases Diabetes Statistics–NIDDK. www.cdc.gov/diabetes/basics/gestational.html
- 2.Saravanan P., Magee L.A., Banerjee A., et al. Gestational diabetes: opportunities for improving maternal and child health. Lancet Diabetes Endocrinol. 2020;8(9):793–800. doi: 10.1016/S2213-8587(20)30161-3. [DOI] [PubMed] [Google Scholar]
- 3.Solomon C.G., Willett W.C., Carey V.J., et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA. 1997;278(13):1078–1083. [PubMed] [Google Scholar]
- 4.Zhang C., Schulze M.B., Solomon C.G., et al. A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia. 2006;49(11):2604–2613. doi: 10.1007/s00125-006-0422-1. [DOI] [PubMed] [Google Scholar]
- 5.Morland K., Wing S., Diez Roux A., et al. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. doi: 10.1016/S0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 6.Morland K., Wing S., Roux A.D. The contextual effect of the local food environment on residents' diets: the atherosclerosis risk in communities study. Am J Publ Health. 2002;92(11):1761–1768. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordon-Larsen P., Nelson M.C., Page P., et al. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 8.Laraia B.A., Siega-Riz A.M., Kaufman J.S., et al. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Prev Med. 2004;39(5):869–875. doi: 10.1016/j.ypmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 9.Weir Z., Bush J., Robson S.C., et al. Physical activity in pregnancy: a qualitative study of the beliefs of overweight and obese pregnant women. BMC Pregnancy Childbirth. 2010;10(1):18. doi: 10.1186/1471-2393-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fonge Y.N., Jain V.D., Harrison C., et al. Examining the relationship between food environment and gestational diabetes. Am J Obstet Gynecol MFM. 2020;2(4) doi: 10.1016/j.ajogmf.2020.100204. [DOI] [PubMed] [Google Scholar]
- 11.Janevic T., Borrell L.N., Savitz D.A., et al. Neighbourhood food environment and gestational diabetes in New York City. Paediatr Perinat Epidemiol. 2010;24(3):249–254. doi: 10.1111/j.1365-3016.2010.01107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahr M.K., Suter M.A., Ballas J., et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am J Obstet Gynecol. 2016;214(1):110.e1–110.e9. doi: 10.1016/j.ajog.2015.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nixon L., Mejia P., Dorfman L., et al. Fast-food fights: news coverage of local efforts to improve food environments through land-use regulations, 2000–2013. Am J Public Health. 2015;105(3):490–496. doi: 10.2105/AJPH.2014.302368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liao J., Chen X., Xu S., et al. Effect of residential exposure to green space on maternal blood glucose levels, impaired glucose tolerance, and gestational diabetes mellitus. Environ Res. 2019;176 doi: 10.1016/j.envres.2019.108526. [DOI] [PubMed] [Google Scholar]
- 15.Yang B.-Y., Zhao T., Hu L.-X., et al. Greenspace and human health: an umbrella review. Innovation. 2021;2(4) doi: 10.1016/j.xinn.2021.100164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackenbach J.D., Nelissen K.G.M., Dijkstra S.C., et al. A systematic review on socioeconomic differences in the association between the food environment and dietary behaviors. Nutrients. 2019;11(9):2215. doi: 10.3390/nu11092215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bukman A.J., Teuscher D., Feskens E.J.M., et al. Perceptions on healthy eating, physical activity and lifestyle advice: opportunities for adapting lifestyle interventions to individuals with low socioeconomic status. BMC Publ Health. 2014;14(1):1036. doi: 10.1186/1471-2458-14-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.den Braver N.R., Lakerveld J., Rutters F., et al. Built environmental characteristics and diabetes: a systematic review and meta-analysis. BMC Med. 2018;16(1):12. doi: 10.1186/s12916-017-0997-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vogel C., Lewis D., Ntani G., et al. The relationship between dietary quality and the local food environment differs according to level of educational attainment: a cross-sectional study. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0183700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Infogroup . 2016. Infogroup US historical business data. [DOI] [Google Scholar]
- 21.R Core Team . 2017. R: a language and environment for statistical computing. [Google Scholar]
- 22.James P., Berrigan D., Hart J.E., et al. Effects of buffer size and shape on associations between the built environment and energy balance. Health Place. 2014;27:162–170. doi: 10.1016/j.healthplace.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caspi C.E., Kawachi I., Subramanian S.V., et al. The relationship between diet and perceived and objective access to supermarkets among low-income housing residents. Soc Sci Med. 2012;75(7):1254–1262. doi: 10.1016/j.socscimed.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Center for Disease Control Census tract level state maps of the modified retail food environment index (mRFEI) https://stacks.cdc.gov/view/cdc/61367
- 25.Gray S.C., Edwards S.E., Schultz B.D., et al. Assessing the impact of race, social factors and air pollution on birth outcomes: a population-based study. Environ Health. 2014;13(1):4. doi: 10.1186/1476-069X-13-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kind A.J.H., Buckingham W.R. Making neighborhood-disadvantage metrics accessible — the neighborhood Atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang C., Tobias D.K., Chavarro J.E., et al. Adherence to healthy lifestyle and risk of gestational diabetes mellitus: prospective cohort study. BMJ. 2014;349 doi: 10.1136/bmj.g5450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pereira M.A., Kartashov A.I., Ebbeling C.B., et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 29.Lopez S., Bermudez B., Ortega A., et al. Effects of meals rich in either monounsaturated or saturated fat on lipid concentrations and on insulin secretion and action in subjects with high fasting triglyceride concentrations. Am J Clin Nutr. 2011;93(3):494–499. doi: 10.3945/ajcn.110.003251. [DOI] [PubMed] [Google Scholar]
- 30.Zhang C., Liu S., Solomon C.G., et al. Dietary fiber intake, dietary glycemic load, and the risk for gestational diabetes mellitus. Diabetes Care. 2006;29(10):2223–2230. doi: 10.2337/dc06-0266. [DOI] [PubMed] [Google Scholar]
- 31.Reyes N.R., Klotz A.A., Herring S.J. A qualitative study of motivators and barriers to healthy eating in pregnancy for low-income, overweight, African-American mothers. J Acad Nutr Diet. 2013;113(9):1175–1181. doi: 10.1016/j.jand.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young C., Laurent O., Chung J.H., et al. Geographic distribution of healthy resources and adverse pregnancy outcomes. Matern Child Health J. 2016;20(8):1673–1679. doi: 10.1007/s10995-016-1966-4. [DOI] [PubMed] [Google Scholar]
- 33.Field C., Grobman W.A., Yee L.M., et al. Community-level social determinants of health and pregestational and gestational diabetes. Am J Obstet Gynecol MFM. 2023 doi: 10.1016/j.ajogmf.2023.101249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morland K., Diez Roux A.V., Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Hutchinson P.L., Nicholas Bodor J., Swalm C.M., et al. Neighbourhood food environments and obesity in southeast Louisiana. Health Place. 2012;18(4):854–860. doi: 10.1016/j.healthplace.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 36.Davenport M.H., Ruchat S.-M., Poitras V.J., et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1367–1375. doi: 10.1136/bjsports-2018-099355. [DOI] [PubMed] [Google Scholar]
- 37.Wood E.K., Stamos G., Mitchell A.J., et al. The association between food desert severity, socioeconomic status, and metabolic state during pregnancy in a prospective longitudinal cohort. Sci Rep. 2023;13(1):7197. doi: 10.1038/s41598-023-32783-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thornton L.E., Crawford D.A., Ball K. Neighbourhood-socioeconomic variation in women's diet: the role of nutrition environments. Eur J Clin Nutr. 2010;64(12):1423–1432. doi: 10.1038/ejcn.2010.174. [DOI] [PubMed] [Google Scholar]
- 39.Tobias D.K., Zhang C., Chavarro J., et al. Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes mellitus. Am J Clin Nutr. 2012;96(2):289–295. doi: 10.3945/ajcn.111.028266. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.