Abstract
Background
Tuberculosis (TB) remains a global health concern, particularly in India, which carries a significant portion of the global burden. The role of sex as a determinant of health is increasingly recognized, impacting various aspects of TB, including treatment compliance and outcomes. This study aimed to determine the mediating role of treatment compliance in the relationship between sex and sputum conversion in newly diagnosed pulmonary TB patients in Chennai, South India.
Methods
We conducted a retrospective cohort study among patients newly diagnosed for TB at ESIC Medical College & PGIMSR between April 2020 and April 2022. A causal mediation analysis was performed to identify the direct and indirect effects of sex on sputum conversion via the mediator, treatment compliance. We employed logistic regression models and the “paramed” package for the analysis, with bootstrapping technique for examining the significance of indirect and direct effects.
Results
The Marginal Total Effect (MTE) suggested that females were more likely to have sputum positivity compared to males (OR: 6.77; p = 0.003). Direct effect of being female increased the odds of sputum positivity at the end of the intensive phase (OR: 3.42; p = 0.03). The indirect effect of being female via treatment compliance significantly increased the odds of sputum positivity at the end of the intensive phase (OR: 1.98; p = 0.03).
Conclusion
The study provides evidence that treatment compliance significantly mediates the relationship between sex and sputum conversion in TB patients, highlighting the necessity to consider gendered dimensions of health in TB control strategies.
Keywords: Mediation analysis, Medication adherence, Sputum positivity, Tuberculosis, Compliance
1. Introduction
Tuberculosis (TB) remains a significant global public health concern, despite considerable advancements in disease control and prevention strategies [1]. Global TB report 2022 has reported that around 1.6 million deaths have occurred due to TB, an increase from 1.5 million in 2020 and 1.4 million in 2019 (taking it back to the 2017 levels) [2]. This has happened despite the reduction in the incidence of TB from 7.1 million in 2019 to 5.8 million in 2020 [3]. This indicates that the number of individuals with undetected and untreated TB has expanded, leading initially to a rise in TB-related fatalities and heightened transmission of the infection within communities [4].
India, as a major contributor to the global TB burden, has been striving to improve prevention, diagnosis, and treatment services through the Revised National Tuberculosis Control Program (RNTCP) and the National TB Elimination Programme (NTEP) [5]. However, numerous challenges persist, including inadequate funding, limited access to health resources, stigmatization, poverty, and non-compliance [6]. The initiation and completion of anti-TB treatment is crucial in controlling the spread of the disease and enhancing patient survival. However, non-compliance to TB treatment poses a significant challenge to these goals [7]. Treatment non-compliance can lead to the perpetuation of disease transmission, extended illness, increased mortality, and the emergence of drug-resistant TB strains [8]. Therefore, understanding the variables influencing treatment compliance is paramount to effectively combat TB.
Sex, as a biological and social determinant of health, has been increasingly recognized as influencing various aspects of TB, including vulnerability to infection, disease progression, and treatment outcomes [9,10]. While biological differences between sexes may account for some disparities, social factors, often intertwined with gender roles and expectations, also play a significant role. These may manifest as differential access to health services, health-seeking behaviours, social stigma, and financial independence, among others [11]. The impact of sex on treatment compliance, and in turn, on sputum conversion—a key indicator of treatment success—is complex and multi-faceted.
Under NTEP, all new cases of drug-sensitive tuberculosis are treated with daily fixed-dose combinations of first-line antituberculosis drugs in appropriate weight bands. The intensive phase consists of eight weeks of Isoniazid, Rifampicin, Ethambutol and Pyrazinamide. In the continuation phase, Isoniazid, Rifampicin and Ethambutol are continued for another 16 weeks. Sputum smear microscopy and/or culture is done at the end of the intensive phase and continuation phase to assess the prognosis of the disease [12].
Sputum conversion, the transition from a positive to a negative sputum smear or culture, is a critical milestone in TB treatment. It typically indicates a reduction in infectivity and a positive response to therapy. Non-compliance to treatment, however, could disrupt this process, prolonging the infectious period and jeopardizing the treatment's success [13]. Hence, exploring this relationship could offer valuable insights to inform TB control strategies that consider the gendered dimensions of health.
Causal mediation analysis, a powerful statistical tool, enables us to dissect the direct and indirect effects of an exposure (in this case, sex) on an outcome (sputum conversion), via a mediator (treatment compliance) [14]. This approach facilitates a deeper understanding of the relationships between these variables and helps uncover potential intervention points.
This study, therefore, contributes to the burgeoning literature on the interplay between sex, treatment compliance, and sputum conversion in TB patients. It emphasizes the need to recognize and address the diverse needs and experiences of males and females in TB care and control. By exploring these complex relationships in the specific context of Chennai, this study also adds to the evidence base required to design and implement more tailored and effective TB interventions in India and other similar settings. Hence, this study was done to determine the mediating role of treatment compliance in the relationship between sex and sputum conversion at the end of the intensive phase in newly diagnosed pulmonary TB patients in Chennai, South India.
2. Methods
2.1. Study setting and participants
This study was conducted as a part of a large-scale retrospective cohort study amongst patients newly diagnosed with TB at ESIC Medical College & PGIMSR between April 1, 2020 and April 2022 were enrolled. Patients aged 6 years and above with newly diagnosed pulmonary TB were included. Patients with previous history of TB or drug-resistant TB were excluded.
2.2. Study procedure
Ethical approval was obtained from the Institutional Ethics Committee (IEC) of ESIC Medical College, Chennai. Tuberculosis treatment details namely sociodemographic details, co-morbidities, addiction history, diagnosis, treatment and follow-up history were retrieved from NIKSHAY portal. NIKSHAY, India's web-based tuberculosis (TB) surveillance system, serves as a comprehensive platform for the electronic management of TB patients, enabling real-time case notification, treatment monitoring, and outcome tracking. Additionally, a pretested semi-structured questionnaire was utilized to collect any missing information from participants via phone interviews. Informed consent was obtained from adult participants (≥18 years) or parents of children (6–17 years). Data collection occurred during May and June 2023.
A total of 531 TB patients (231 females, 43.7 %) were newly diagnosed at ESIC Medical College & PGIMSR between April 1, 2020, and April 2022. Of the 531, 237 (68 females, 28.7 %) were identified as pulmonary TB cases. All these patients were diagnosed with tuberculosis by sputum acid-fast bacilli smear and 236 patients (except one female) were initiated on anti-tuberculosis treatment at ESIC Medical College and Hospital. Incomplete information and missing entries in the NIKSHAY portal were collected from the patients through phone interviews. After excluding those with missing contact details or who did not respond, 213 patients (57 females, 26.8 %) were enrolled in our study.
2.3. Operational definitions
New case: A TB patient who has never had treatment for TB or has taken anti-TB drugs for less than a month.
2.4. Treatment compliance
The data used in this study was gathered from the patients' treatment cards available on NIKSHAY portal upon the completion of the intensive phase. It displays the information about daily intake of anti-tuberculosis medications through dots-99 technology in the form of colour coded bands. Green indicates consumption of medicine and red indicates skipping of medication. This information was noted down from the portal by research assistants. Patients who consistently took their medication (>80 % of the days) throughout the entire intensive phase were deemed to have demonstrated good compliance to the tuberculosis treatment regimen.
2.5. Sputum conversion
Sputum conversion is the achievement of a negative result, indicating the absence of Mycobacterium tuberculosis, in sputum smear examination using acid-fast bacilli (AFB) staining or culture following tuberculosis treatment initiation. Information about treatment compliance and sputum conversion was obtained from NIKSHAY portal and from phone call interviews.
2.6. Sputum positivity
Sputum Positivity is the presence of Mycobacterium tuberculosis in the sputum sample of the patient demonstrated by sputum AFB staining or culture after TB treatment initiation.
2.7. Statistical analysis
We have performed a mediation analysis in STATA v14.0 using the logistic regression (to account for binary mediator and outcome variables) models that take mediator into account when estimating controlled direct (CDE), natural direct (NDE) and indirect effect (NIE). The NDE reports the exposure-outcome link without the inclusion of a mediator variable, while the NIE reflects the portion of the exposure-outcome relationship that includes mediator.
The equations fitted with the logistic regression (binary mediator and dependent variable) are as follows [15]:
| Y = i1 + cX … | (1) |
| M = i2 + aX …. | (2) |
| Y = i3 + c′X + bM … | (3) |
In Equation (1), ‘Y' denotes the dependent variable (sputum positivity), while ‘c' symbolizes the gradient of the independent variable (sex). In Equation (2), ‘M' stands for mediator variable (compliance to treatment), and ‘a' indicates gradient of the independent variable (sex). In Equation (3), ‘Y' stands for dependent variable (sputum positivity), ‘c' signifies the gradient of the independent variable (sex), and ‘b' designates the gradient of the mediator variable (compliance to treatment). In all these equations, ‘i' is representative of intercept.
The odds ratio (OR) for the NIE and NDE are calculated using Equation (4) &(5)14:
| (4) |
| (5) |
In this context, ‘i2′ denotes intercept derived from equation two, ‘b' signifies the coefficient ‘b' from equation three, ‘a' designates a coefficient from equation two, and ‘c′' stands for the coefficient ‘c’ derived from equation three.
We determined the relative scale of mediated effect using two metrics: the proportion mediated (PM) and the mediated to non-mediated ratio. The formula for calculation ar given in (6), (7) [16]:
| (6) |
| (7) |
To ensure compatibility with the odds ratios calculated for the direct and indirect effects, we transformed these effects to their natural logarithms prior to the calculation of the PM effect and the ratio of mediated to non-mediated effect. The logarithm transformation was implemented because the odds ratios, which are a measure of effect size in our logistic regression analysis, are multiplicative. By taking natural logarithms, we are able to convert these multiplicative odds ratios into additive log-odds units, making it possible to meaningfully add and subtract these quantities for the purpose of our calculations. The formula are given in (8), (9) as follows:
| (8) |
| (9) |
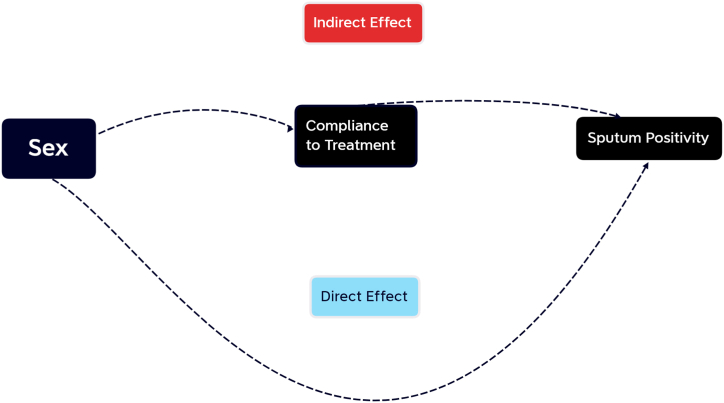
Fig. 1 illustrates the assumed relationship among the variables. The arrow's orientation signifies the impact direction. We proposed that the sex exerts both direct and indirect influences (through treatment compliance) on sputum positivity at completion of intensive phase.
Fig. 1.
Mediation pathway between Sex and sputum positivity via compliance to treatment
To evaluate the association between exposure variable (sex) and mediator variable (treatment compliance), between the mediator (treatment compliance) and outcome variable (sputum positivity), and between the exposure (sex) and outcome variable (sputum positivity), we utilized the Baron and Kenny method with logistic regression models [17].
After ensuring the primary assumptions were met, we conducted a mediation analysis using the “paramed” package [18]. To assess the significance of the indirect and direct impacts, we implemented a bootstrapping method (with 500 iterations) coupled with the bootstrapped bias-corrected Confidence Intervals.
3. Results
Of the total 213 participants, 9 (4.2) died and 11 (5.16) were lost to follow up. Characteristics of the participants are given in Table-1. Among females, 2 (3.50) died and 4 (7.01) were lost to follow-up. In terms of sputum conversion at the end of the intensive phase, among the 213 pulmonary TB patients, 44 (20.7 %) remained positive for Mycobacterium tuberculosis, indicating unsuccessful sputum conversion and ongoing infection. Sputum positivity at the end of the Intensive phase was 15.4 % among males and 35.1 % among females (p = 0.002). Of the 44 sputum-positive cases, 19 (43.2) achieved sputum conversion at the end of the continuation phase, 4 (9.1) died, 7 (15.9) were lost to follow-up and 10 (22.7) were labelled as emerging resistance. Among females 9 (45.0) achieved sputum conversion at the end of the continuation phase, 2 (10.0) died, 5 (25.0) were lost to follow-up and 3 (15.0) were labelled as emerging resistance.
Table 1.
Characteristics of study participants (N = 213).
| Sl no. | Characteristics | Male (156) | Female (57) | Frequency n (%) | P value |
|---|---|---|---|---|---|
| 1 | Age Categories, in years | ||||
| <60 | 123 (78.9) | 40 (70.2) | 163 (76.5) | ||
| ≥60 | 33 (21.1) | 17 (29.8) | 50 (23.5) | 0.186 | |
| 2 | Marital status | ||||
| Currently married | 144 (92.3) | 51 (89.5) | 195 (91.6) | ||
| Never married | 12 (7.7) | 6 (10.5) | 18 (8.4) | 0.510 | |
| 4 | Smoking statusa | ||||
| Non-Smoker | 89 (57.1) | 57 (100) | 146 (68.5) | ||
| Smoker | 66 (42.3) | 0 | 66 (31.0) | ||
| No information | 1 (0.6) | 0 | 1 (0.5) | <0.001 | |
| 5 | Alcohol usea | ||||
| Alcohol user | 63 (40.4) | 0 | 63 (29.6) | ||
| Non-drinker | 92 (59.0) | 57 (100) | 149 (69.9) | ||
| No information | 1 (0.6) | 0 | 1 (0.5) | <0.001 | |
| 6 | Diabetes Mellitus status | ||||
| Present | 59 (37.9) | 30 (53.6) | 89 (41.8) | ||
| Absent | 96 (61.5) | 26 (44.2) | 122 (57.3) | ||
| No information | 1 (0.6) | 1 (1.8) | 2 (0.9) | 0.044 | |
| 7 | Hypertension | ||||
| Present | 21 (13.5) | 7 (12.5) | 28 (13.2) | ||
| Absent | 134 (85.9) | 49 (85.7) | 183 (85.9) | ||
| No information | 1 (0.6) | 1 (1.8) | 2 (0.9) | 0.843 | |
| 8 | Other comorbidities | ||||
| Chronic heart disease | 6 (3.84) | 0 | 6 (2.8) | 0.135 | |
| Chronic obstructive pulmonary disease | 5 (3.2) | 1 (1.8) | 6 (2.8) | 0.578 | |
| Asthma | 5 (3.2) | 1 (1.8) | 6 (2.8) | 0.578 | |
| Hypothyroidism | 2 (1.3) | 2 (3.5) | 4 (1.9) | 0.283 | |
| Cancer | 0 | 2 (3.5) | 2 (0.9) | 0.18 | |
| Stroke | 1 (0.6) | 0 | 1 (0.5) | 0.547 | |
| Chronic kidney disease | 1 (0.6) | 0 | 1 (0.5) | 0.547 | |
| 9 | Symptom history | ||||
| Cough | 129 (82.7) | 46 (80.7) | 175 (82.2) | 0.737 | |
| Fever | 21 (13.5) | 7 (12.3) | 28 (13.2) | 0.821 | |
| Loss of weight | 5 (3.2) | 2 (3.5) | 7 (3.3) | 0.912 |
Self-reported by participants.
Non-compliance to Tb treatment was found to be higher among females (14, 24.6 %) compared to males (19, 12.2 %) with an odds ratio of OR: 2.35; 95 % CI: 1.09–5.08 (p = 0.03). Sputum positivity was found to be higher among treatment-non-compliant (31, 93.9 %) compared to treatment-compliant patients (13, 7.2 %) with an odds ratio of 199.11; 95 % CI: 42.80–926.24 (p < 0.001). Since both the basic assumptions were satisfied, mediation analysis was performed to study the direct and indirect effects of sex on sputum positivity (Table-2).
Table 2.
Relationship between sex, treatment compliance and sputum positivity.
| Treatment compliance |
||||
|---|---|---|---|---|
| S.No | Yes | No | Odds ratio | |
| 1. | Sex | |||
| Male | 137 (87.8) | 19 (12.2) | ||
| Female | 43 (75.4) | 14 (24.6) | 2.348 (1.086–5.073) | |
| 2. | Sputum positivity | |||
| Treatment compliance | Yes | No | ||
| Compliance | 13 (7.2) | 167 (92.8) | ||
| Noncompliance | 31 (93.9) | 2 (6.1) | 199.115 (42.804–926.244) | |
Table 3 provides the results of causal mediation analysis with non-compliance to TB treatment compliance as mediator between sex and sputum conversion in the cohort of newly diagnosed pulmonary TB patients. Marginal Total Effect MTE indicated that females were significantly more likely to have sputum positivity at the end of the intensive phase compared to males (OR: 6.77; 95 % CI: 1.93–23.73; p = 0.003). The analysis found that the direct effect of being female not mediated by treatment compliance increased the odds of sputum positivity at the end of the intensive phase (OR: 3.42; 95 % CI: 1.15–10.22; p = 0.03). The indirect effect of being female via treatment non-compliance significantly increased the odds of sputum positivity at the end of the intensive phase (OR: 1.98; 95 % CI: 1.08–3.62; p = 0.03).
Table 3.
Results of Causal Mediation Analysis with Non-compliance to TB treatment Compliance as Mediator between Sex and Sputum Conversion in the Cohort of Newly Diagnosed Pulmonary TB patients at Chennai, South India.
| Effect | Exposure | Odds Ratio (95 % CI)* | P-value | Bias-corrected CIs |
|---|---|---|---|---|
| Marginal Total Effect (MTE) of Sex on Sputum positivity at the end of intensive phase | Females | 6.77 (1.93–23.73) | 0.003 | 1.83–29.00 |
| Males | Ref | – | – | |
| Direct Effect of Sex on Sputum positivity at the end of intensive phase | Females | 3.42 (1.15–10.22) | 0.03 | 1.33–12.48 |
| Males | Ref | – | – | |
| Indirect Effect of Sex on Sputum positivity via treatment compliance during intensive phase | Females | 1.98 (1.08–3.62) | 0.03 | 1.06–3.44 |
| Males | Ref | – | – | |
| Effect of Sex on Non-compliance to TB treatment during the intensive phase | Females | 2.35 (1.09–5.08) | 0.03 | [Not Applicable] |
| Males | Ref | – | ||
| Effect of Treatment compliance on Sputum positivity at the end of intensive phase | Non-compliant | 199.11 (42.80–926.24) | <0.001 | |
| Compliant | Ref | – |
Our analysis involved the application of natural logarithms (ln) to convert the Odds Ratios (OR) of the Direct and Indirect Effects into a more suitable format for our computations. Specifically, the OR for the Direct Effect (3.42) was transformed to a ln value of 1.23, while the OR for the Indirect Effect (1.98) corresponded to a ln value of 0.68.
Following these transformations, we calculated the Proportional Mediated (PM) effect, which represented the portion of the total effect of sex on sputum positivity mediated by non-compliance to TB treatment. The PM was found to be 0.36, implying that approximately 36 % influence of sex on sputum positivity was mediated by variations in treatment compliance between males and females. We also calculated the ratio of the mediated (Indirect) effect to the non-mediated (Direct) effect. This ratio yielded a value of 0.55. This indicates that for every unit increase in the non-mediated effect of being female on sputum positivity, there is a 0.55-fold increase in the mediated effect through non-compliance to TB treatment.
4. Discussion
Our study revealed a significant disparity in the sex ratio among notified pulmonary TB cases, with the gap gradually narrowing across all forms of tuberculosis. This observation aligns with existing literature suggesting gender-specific variations in TB presentation and diagnosis. Studies have consistently shown a higher prevalence of microbiologically confirmed pulmonary TB among men, while women are more prone to clinically diagnosed pulmonary TB and extrapulmonary TB forms [[19], [20], [21], [22], [23]]. Women may present with nonspecific symptoms, potentially contributing to delays in diagnosis [19,23,24]. Additionally, in Asia, younger women are disproportionately affected by extrapulmonary TB and female genital TB, further underscoring the importance of considering gender in TB surveillance and management [19,25]. The convergence of our findings with established patterns in TB epidemiology enhances the accuracy and generalizability of our data.
The causal mediation analysis presented in this study reveals profound insights into the multifaceted interplay between sex, treatment compliance, and sputum positivity among newly diagnosed pulmonary tuberculosis (TB) patients in Chennai, South India. Through careful examination of both direct and indirect effects, the findings spotlight the intersectionality of sex and treatment compliance in shaping interim TB outcomes.
Firstly, the marginal total effect indicates that females were significantly more likely to have sputum positivity at the end of the intensive treatment phase when compared to males. This finding aligns with existing literature which has underscored sex-based disparities in interim TB treatment outcomes [[26], [27], [28]]. The reasons for such disparities are possibly multifactorial in nature, shaped by a combination of biological, social, and health system-related determinants. Biologically, sex-related differences in immune responses could influence susceptibility to TB infection, disease progression, and response to therapy [11]. From a socio-cultural perspective, females may face unique challenges such as gender-related stigma, socio-economic constraints, limited decision-making power, and healthcare access barriers that can affect their health-seeking behaviors and treatment compliance [11]. Additionally, health systems may not be adequately gender-responsive, potentially leading to the provision of suboptimal care for female patients [29].
Upon disentangling the total effect, the study identifies significant direct and indirect effects of sex on sputum positivity. The direct effect highlights an intrinsic link between sex and sputum positivity, independent of treatment compliance. This suggests that being female alone increases the odds of sputum positivity at the end of the intensive phase, hinting at the other social factors like difference in addiction rates between sexes, biological and genetic factors that may affect interim treatment outcomes. Although the mechanisms behind this are not fully understood, possibilities could include influence of sex hormones on the immune responses or pharmacokinetics of the anti-tubercular drugs necessitating further research to corroborate these hypotheses [30].
Simultaneously, the indirect effect identifies the influence of sex on sputum positivity mediated by treatment compliance. Females were found to be significantly more likely to be non-compliant with TB treatment, which, in turn, increased their likelihood of sputum positivity at the end of the intensive phase. This finding underscores the salient role of treatment compliance in determining TB treatment outcomes and throws light on the need to address gender-based barriers to medication compliance.
Treatment non-compliance is a well-known barrier to TB control, with far-reaching consequences such as prolonged disease transmission, increased disease severity, and the emergence of drug-resistant TB [7,8]. For females, treatment non-compliance could be driven by various factors, such as limited access to healthcare services, economic constraints, social stigma associated with TB, lack of autonomy, fear of discrimination, inadequate knowledge about the disease, and side effects of the medication [31].
Contrary to conventional understanding, which attributed poor Tb treatment outcomes among women to barriers in access and social factors, our study uncovered a different reality. While acknowledging the impact of such barriers, we found that treatment compliance emerged as a pivotal factor influencing TB outcomes, particularly among women. Moreover, our findings suggest that addressing compliance issues, in addition to improving access may have a more pronounced impact on improving TB outcomes among women than mitigating other social determinants. Sensitizing the health care providers and TB treatment supporters such as DOTS providers and Senior Treatment supervisors on gender-responsive TB care would improve treatment compliance and treatment outcomes [19].
Moreover, this also confirms the substantial relationship between treatment compliance and sputum positivity, where non-compliant patients had significantly higher odds of having sputum positivity [32,33]. This association reinforces the global emphasis on ensuring treatment compliance for successful TB control and validates the myriad interventions aimed at promoting compliance, such as patient-centred care, DOTS-99, treatment literacy, and social support [34].
This study has the following set of limitations. Firstly, as the study was conducted in Chennai, South India, the findings might not be generalizable to other regions with differing socio-cultural contexts or health system characteristics. Secondly, there may be potential unmeasured confounding variables such as socio-economic status, educational level, or genetic factors that were not accounted for in the analysis, which could influence both treatment compliance and interim TB outcomes. Finally, while this study examined the mediating role of treatment compliance in the relationship between sex and sputum positivity, it did not explore other potential mediators such as access to healthcare, stigma, or gender norms. This multi-dimensional aspect necessitates further investigation to provide a comprehensive understanding of the observed disparities.
This study has important implications for public health policy. This study contributes significantly to the growing body of evidence demonstrating sex-based disparities in TB outcomes. Identifying the pathways through which sex influences sputum conversion, mediated by treatment compliance, offers valuable insights to guide gender-responsive TB control strategies. It underscores the necessity of tackling the complex barriers to treatment compliance, particularly among females, to improve TB outcomes. Addressing these challenges will require concerted, multi-sectoral efforts that engage not only health systems but also communities and individuals to foster an enabling environment that promotes treatment compliance and ultimately, successful TB control.
However, the study also serves as a reminder that our understanding of the intricate interplay between sex, treatment compliance, and sputum positivity remains incomplete. More comprehensive research is needed to fully understand the underlying mechanisms and to tailor interventions effectively. As the world strives towards the goal of ending TB, we must recognize and address these gender-based disparities to ensure that no one is left behind in the fight against this devastating disease.
5. Conclusion
Overall, the study findings provide evidence that treatment compliance partially mediates the relationship between sex and sputum positivity at the end of the intensive phase. While females have a direct higher risk of sputum positivity, part of their increased risk is also explained by lower treatment compliance. Interventions targeting treatment compliance, particularly among female patients, may help to reduce sputum positivity and improve overall TB treatment outcomes.
Ethical approval
This study was approved by Institutional Ethics Committee of ESIC Medical College & Hospital (IEC number: IEC/2022/2/50)
Funding
The work was supported by grant from Tuberculosis Association of India (TAI) under short term research projects financial assistance scheme (2022–23). The grant was awarded to Dr. Yuvaraj Krishnamoorthy.
Data availability statement
Data will be made available upon reasonable request.
CRediT authorship contribution statement
Yuvaraj Krishnamoorthy: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Selvaraja C: Writing – review & editing, Validation, Supervision, Project administration, Methodology, Investigation, Data curation. Dhanajayan Govindan: Writing – review & editing, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: First Author Yuvaraj Krishnamoorthy is Associate Editor for Heliyon Journal.
Acknowledgement
Nil.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e31185.
Contributor Information
Yuvaraj Krishnamoorthy, Email: yuvi.1130@gmail.com, yuvaraj@propulevidence.org.
Selvaraja C, Email: ljcljcljc17@gmail.com.
Dhanajayan Govindan, Email: gdhanajayanj@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Bloom B.R., Atun R., Cohen T., Dye C., Fraser H., Gomez G.B., et al. In: Major Infectious Diseases. third ed. Holmes K.K., Bertozzi S., Bloom B.R., Jha P., editors. The International Bank for Reconstruction and Development/The World Bank; Washington (DC): 2017. Tuberculosis. [PubMed] [Google Scholar]
- 2.Bagcchi S. WHO's global tuberculosis report 2022. Lancet Microbe. 2023;4(1) doi: 10.1016/S2666-5247(22)00359-7. [DOI] [PubMed] [Google Scholar]
- 3.Chakaya J., Petersen E., Nantanda R., Mungai B.N., Migliori G.B., Amanullah F., et al. The WHO Global Tuberculosis 2021 Report - not so good news and turning the tide back to End TB. Int. J. Infect. Dis. 2022;124:S26–S29. doi: 10.1016/j.ijid.2022.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chakaya J., Khan M., Ntoumi F., Aklillu E., Fatima R., Mwaba P., et al. Global tuberculosis report 2020 - Reflections on the global TB burden, treatment and prevention efforts. Int. J. Infect. Dis. 2021;113:S7–S12. doi: 10.1016/j.ijid.2021.02.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khanna A., Saha R., Ahmad N. National TB elimination programme - what has changed. Indian J. Med. Microbiol. 2023;42:103–107. doi: 10.1016/j.ijmmb.2022.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thakur G., Thakur S., Thakur H. Status and challenges for tuberculosis control in India - Stakeholders' perspective. Indian J. Tubercul. 2021;68(3):334–339. doi: 10.1016/j.ijtb.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waitt C.J., Squire S.B. A systematic review of risk factors for death in adults during and after tuberculosis treatment. Int. J. Tubercul. Lung Dis. 2011;15:871–885. doi: 10.5588/ijtld.10.0352. [DOI] [PubMed] [Google Scholar]
- 8.Tesfahuneygn G., Medhin G., Legesse M. Adherence to Anti-tuberculosis treatment and treatment outcomes among tuberculosis patients in Alamata District, northeast Ethiopia. BMC Res. Notes. 2015;8:503. doi: 10.1186/s13104-015-1452-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Central TB Division. Ministry of Health and Family Welfare . 2023. National Framework for a Gender-Responsive Approach to TB in India.https://tbcindia.gov.in/WriteReadData/l892s/388838054811%20NTEP%20Gender%20Responsive%20Framework_311219.pdf Available from: [Google Scholar]
- 10.Krishnamoorthy Y., Ezhumalai K., Murali S., Rajaa S., Majella M.G., Sarkar S., et al. Development of prognostic scoring system for predicting 1-year mortality among pulmonary tuberculosis patients in South India. J. Public Health. 2023;45(2):e184–e195. doi: 10.1093/pubmed/fdac087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Onifade D.A., Bayer A.M., Montoya R., et al. Gender-related factors influencing tuberculosis control in shantytowns: a qualitative study. BMC Publ. Health. 2010;10:381. doi: 10.1186/1471-2458-10-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.TOG-Chapter 4-Treatment of TB Part 1 Ministry of health and family welfare. 2023. https://tbcindia.gov.in/showfile.php?lid=3219 Oct 13]. Available from:
- 13.Kayigamba F.R., Bakker M.I., Mugisha V., De Naeyer L., Gasana M., Cobelens F., et al. Adherence to tuberculosis treatment, sputum smear conversion and mortality: a retrospective cohort study in 48 Rwandan clinics. PLoS One. 2013;8(9) doi: 10.1371/journal.pone.0073501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.VanderWeele T.J. Mediation analysis: a practitioner's guide. Annu. Rev. Publ. Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- 15.Rijnhart J.J.M., Twisk J.W.R., Eekhout I., Heymans M.W. Comparison of logistic-regression based methods for simple mediation analysis with a dichotomous outcome variable. BMC Med. Res. Methodol. 2019;19(1):19. doi: 10.1186/s12874-018-0654-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Introduction to statistical mediation analysis [internet]. Routledge & CRC press. 2023. https://www.routledge.com/Introduction-to-Statistical-Mediation-Analysis/MacKinnon/p/book/9780805864298 Oct 13]. Available from:
- 17.Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 18.PARAMED: Stata module to perform causal mediation analysis using parametric regression models. In [https://ideas.repec.org/c/boc/bocode/s457581.html].
- 19.Central Tuberculosis Division . Ministry of Health with Family Welfare; 2019. New Delhi: National Framework for a Gender-Responsive Approach to TB in India.https://tbcindia.gov.in/index1.php?page=2&ipp=10&lang=1&level=1&sublinkid=4571&lid=3176 [updated 2024 March 20; cited 2024 April 13] Available from: [Google Scholar]
- 20.Balasubramanian R., Garg R., Santha T., Gopi P.G., Subramani R., Chandrasekaran V., Thomas A., Rajeswari R., Anandakrishnan S., Perumal M., Niruparani C., Sudha G., Jaggarajamma K., Frieden T.R., Narayanan P.R. Gender disparities in tuberculosis: report from a rural DOTS programme in south India. Int. J. Tubercul. Lung Dis. 2004;8(3):323–332. [PubMed] [Google Scholar]
- 21.Dandona R., Dandona L., Mishra A., Dhingra S., Venkatagopalakrishna K., Chauhan L.S. Utilization of and barriers to public sector tuberculosis services in India. Natl. Med. J. India. 2004;17(6):292–299. [PubMed] [Google Scholar]
- 22.Mukherjee A., Saha I., Sarkar A., Chowdhury R. Gender differences in notification rates, clinical forms and treatment outcome of tuberculosis patients under the RNTCP. Lung India. 2012;29(2):120. doi: 10.4103/0970-2113.95302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weiss M, Christian Auer DS, Abdallah Abouihia JK, M Shaheed Jawahar FK, N L Arias. Gender and tuberculosis: cross-site analysis and implications of a multi-country study in Bangladesh, India, Malawi, and Colombia [Internet]. WHOI. Available from: http://www.who.int/tdr/publications/tdr-researchpublications/gender-tb-multicountry-study/en/(accessed 2.22.18).
- 24.Long N.H., Diwan V.K., Winkvist A. Difference in symptoms suggesting pulmonary tuberculosis among men and women. J. Clin. Epidemiol. 2002;55(2):115–120. doi: 10.1016/s0895-4356(01)00455-3. [DOI] [PubMed] [Google Scholar]
- 25.Sharma J.B., Sharma E., Sharma S., Dharmendra S. Female genital tuberculosis: revisited. Indian J. Med. Res. 2018;148:71. doi: 10.4103/ijmr.IJMR_648_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stanikzai M.H., Bairwa M., Wasiq A.W., Gupta S.D., Akbari K. Factors influencing sputum smear conversion among smear positive pulmonary tuberculosis patients in kandahar City, Afghanistan. J. Clin. Diagn. Res. 2019;13(10):18–21. [Google Scholar]
- 27.Holtz T.H., Sternberg M., Kammerer S., Laserson K.F., Riekstina V., Zarovska E., et al. Time to sputum culture conversion in multidrug-resistant tuberculosis: predictors and relationship to treatment outcome. Ann. Intern. Med. 2006;144(9):650–659. doi: 10.7326/0003-4819-144-9-200605020-00008. PMID: 16670134. [DOI] [PubMed] [Google Scholar]
- 28.Iqbal Z., Khan M.A., Aziz A., Nasir S.M. Time for culture conversion and its associated factors in multidrug-resistant tuberculosis patients at a tertiary level hospital in Peshawar, Pakistan. Pakistan J. Med. Sci. 2022;38(4Part-II):1009–1015. doi: 10.12669/pjms.38.4.5058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hay K., McDougal L., Percival V., Henry S., Klugman J., Wurie H., et al. Disrupting gender norms in health systems: making the case for change. Lancet. 2019 Jun 22;393(10190):2535–2549. doi: 10.1016/S0140-6736(19)30648-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taneja V. Sex hormones determine immune response. Front. Immunol. 2018;9:1931. doi: 10.3389/fimmu.2018.01931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nezenega Z.S., Perimal-Lewis L., Maeder A.J. Factors influencing patient adherence to tuberculosis treatment in Ethiopia: a literature review. Int. J. Environ. Res. Publ. Health. 2020;17(15):5626. doi: 10.3390/ijerph17155626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Izudi J., Tamwesigire I.K., Bajunirwe F. Sputum smear non-conversion among adult persons with bacteriologically confirmed pulmonary tuberculosis in rural eastern Uganda. J Clin Tuberc Other Mycobact Dis. 2020;20 doi: 10.1016/j.jctube.2020.100168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hermosilla S., You P., Aifah A., Abildayev T., Akilzhanova A., Kozhamkulov U., et al. Identifying risk factors associated with smear positivity of pulmonary tuberculosis in Kazakhstan. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0172942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Companion Handbook to the WHO Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis. World Health Organization; Geneva: 2014. https://www.ncbi.nlm.nih.gov/books/NBK247419/ Available from: [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available upon reasonable request.