Abstract
Objectives
This study aimed to compare the clinical outcomes of patients with lateral epicondylitis (LE) treated with local massage, corticosteroid (CS) injection, and extracorporeal shock wave therapy (ESWT).
Patients and methods
This randomized prospective study included 52 patients. Patients treated with local massage in Group 1 (n=17; 9 males, 8 females; mean age: 46.1±10.9 years; range, 27 to 64 years), CS injection in Group 2 (n=17; 7 males, 10 females; mean age: 46.0±8.8 years; range, 28 to 63 years), and ESWT in Group 3 (n=18; 12 males, 6 females; mean age: 46.7±11.3 years; range, 28 to 68 years) for LE were evaluated between March 2021 and June 2022. Clinical outcomes were assessed using the Visual Analog Scale (VAS), Disabilities of the Arm, Shoulder, and Hand (DASH), and DASH-Work Model (DASH-WM) scoring systems at the initial examination at the beginning of the study and at two-week, three-month, and six-month follow-up controls.
Results
Similar results were observed between VAS, DASH, and DASH-WM scores measured during LE diagnosis. In the first two weeks of follow-up, statistically significant decreases were observed in VAS, DASH, and DASH-WM scores in all three groups. Compared to baseline values, Group 1 and 2 had significant difference in VAS and DASH scores at three months. Group 3 had a significant difference in all clinical evaluation scores. At six months, no significant difference was observed in Groups 1 and 2 in any of the scoring systems, while Group 3 showed significant improvements in all scoring systems.
Conclusion
Treatment with ESWT was superior to other treatments throughout the study and at the final follow-up. In patients receiving CS injections, the clinical outcomes worsened with time, evidenced by the six-month follow-up. Further studies on combined treatment modalities are needed on this subject.
Keywords: Extracorporeal shock wave therapy, lateral epicondylitis, local massage, corticosteroids.
Introduction
The lateral epicondyle is the starting point of the extensor muscles of the wrist. Damage to this structure results in fibroblastic proliferation, hyaline degeneration, vascular proliferation, and calcific deposits.[1] This change causes severe elbow pain that increases with repetitive supination and dorsiflexion movements of the hand, wrist, and forearm.[2] In 1873, Runge and Zur[3] described this disease as “lawn tennis arm.” The etiology of the condition is poorly understood.[4] Lateral epicondylitis (LE) was previously thought to be an inflammatory process resulting from the overuse of the tendon.[5] By examining the histological structure of the affected tissue, Regan et al.[1] demonstrated that the disease is a degenerative process rather than an inflammatory process. In addition, Kraushaar and Nirschl[6] provided a good description with several histological stages. Although an acute inflammatory response occurs in the initial stage of LE, repeated microtrauma in the later stage leads to microtears. Microtear formation results in angiofibroblastic hyperplasia, vascular hyperplasia, and the appearance of irregular collagen. Because this degeneration process is the most common stage at which patients present to their physicians, inflammatory cells such as neutrophils and macrophages are histologically rare at the time of LE diagnosis.[5] Although the origin of pain is not fully understood, the literature suggests granulation tissue around the lateral epicondyle, increased substance P receptors, aponeurosis of free nerve endings, and increased levels of the excitatory neurotransmitter glutamate.[5] The poor understanding of the specific pathoanatomic origin of pain has led to a variety of treatment approaches for LE.[7] There is evidence in the literature supporting physical therapy protocols that focus on strengthening and stretching the affected muscles.[8]
Although the exact action mechanisms of local massage are unknown, has been suggested that this procedure causes mechanothermal changes in the affected tissue, and the resulting temperature increase may help to reduce joint stiffness and increase muscle elasticity. Mechanical impact can help dissolve granulation deposits within the muscle, which are byproducts of tendon injury.[9] Kohia et al.[8] showed in their study that local massage relieves pain. Another very common treatment approach for LE is the injection of a preparation of corticosteroid (CS) and a local anesthetic into the area. Such injections usually help relieve pain by blocking nociceptive transmission, simultaneously suppressing inflammatory responses and promoting joint mobility.[10] The effect is transient after two months[10] and has the potential to cause complications, such as subcutaneous fat atrophy, skin depigmentation, muscle loss, and tendon rupture.[11] Despite this, many physicians administer CS injections periodically.[12] Extracorporeal shock wave therapy (ESWT) has recently been used for various musculoskeletal disorders. It involves stimulating the skin in the affected area with sound waves of specific frequencies.[13] Although the mechanism of action of ESWT is not fully known, it is similar to that of local massage. Sound and vibration pulses generated in the affected tissue are thought to help reduce joint stiffness and increase muscle elasticity.[14] ESWT reduces elbow pain.[15] This effect is due to the stimulation of tendon healing by promoting neovascularization, accompanied by hyperstimulation analgesia.[16] In the present study, we aimed to compare the healing process and clinical outcomes of patients with LE treated with local massage, CS injection, and ESWT.
Patients and Methods
A total of 52 patients who were admitted to the Harran University Faculty of Medicine, Department of Orthopedics and Traumatology and diagnosed with LE via physical examination and magnetic resonance imaging between March 2021 and June 2022 were evaluated in the randomized prospective study. Patients aged >18 years with symptoms persisting for more than six weeks and diagnosed with LE were included in the study.
Patients who had not received any treatment for LE in the last six months were considered for inclusion. The follow-up and treatment of the patients were performed by the same two physicians to ensure objectivity and accuracy of the scoring. The patients were divided into groups to receive local massage, CS injection, and ESWT treatments in the order they presented to the hospital.
Group 1 (n=17; 9 males, 8 females; mean age: 46.1±10.9 years; range, 27 to 64 years) received deep skin massage on the lateral epicondyle for 5 min once a day, three times a week for two weeks. Local massage consisted of transverse movements with the fingertips and skin as a single unit over the area of maximum tenderness. Firm pressure was applied to compress the roots of the extensor carpi radialis brevis tendons at their origin and the underlying bone. Group 2 (n=17; 7 males, 10 females; mean age: 46.0±8.8 years; range, 28 to 63 years) received a single injection of 1 mL of 40 mg methylprednisolone acetate and 2 mL of 2% prilocaine hydrochloride. The injection was administered with the patient's arm in abduction on a hard surface and the elbow in 90° flexion. After the skin was cleaned, a local anesthetic was injected deep into the subcutaneous tissues and muscles. Then, the points with maximum tenderness in the lateral epicondyle region were determined, and a CS injection was administered by touching the needle tip to the bone. Group 3 (n=18; 12 males, 6 females; mean age: 46.7±11.3 years; range, 28 to 68 years) received ESWT consisting of 1500 shock waves at an intensity of 2.0 bar and a frequency of 8 Hz for four sessions, two sessions per week for two weeks. During the treatment, patients were seated with their shoulder in 30° abduction, their elbow in 90° flexion, and their forearm, wrist, and hand on the table. The point of maximum tenderness was marked with a pencil before treatment to ensure correct shock wave delivery. Local anesthesia was not performed. Ultrasound coupling gel was used. Each treatment session lasted 20 to 30 min. All patients in the three groups received standard treatment, including nonsteroidal anti-inflammatory drugs, splinting, exercise, and rest.
All patients in the three groups were clinically evaluated using the Visual Analog Scale (VAS), Disabilities of the Arm, Shoulder, and Hand (DASH), and DASH-Work Model (DASH-WM) scores at the initial examination at the beginning of the study and at two-week, three-month, and six-month follow-up controls.
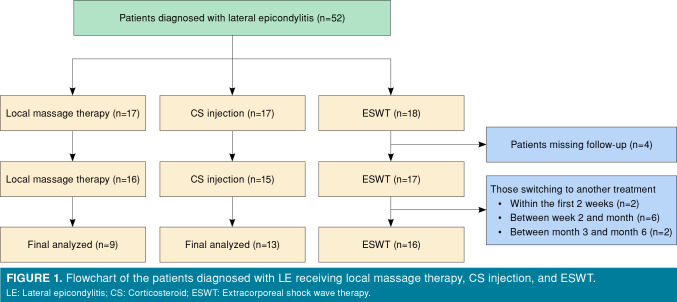
In the second week, patients who did not come to the control examinations (n=4) or received additional treatment (n=2), were not evaluated. Thus, a total of 46 patients (local massage 14; CS inj. 15; ESWT: 17) were evaluated in the second week. In the third month, six patients receiving additional therapy were not included in the evaluation and a total of 40 patients (local massage 10; CS inj. 14; ESWT: 16) were evaluated. In the sixth month, two patients who received additional treatment were excluded from evaluation. As a result, 38 patients (local massage 9; CS inj. 13; ESWT: 16) were evaluated at the final follow-up at the end of the sixth month (Figure 1). The follow-up of 10 patients who needed additional treatment during the study and who were not evaluated at checkpoints in the main study group, continued as a subgroup.
Figure 1. Flowchart of the patients diagnosed with LE receiving local massage therapy, CS injection, and ESWT. LE: Lateral epicondylitis; CS: Corticosteroid; ESWT: Extracorporeal shock wave therapy.
Statistical analysis
Statistical analyses were performed using IBM SPSS version 25.0 version (IBM Corp., Armonk, NY, USA). The Shapiro-Wilk test was used to evaluate whether the data conformed to a normal distribution. Normally distributed numerical variables were expressed as mean ± standard deviation (SD), and nonnormally distributed data were expressed as median (range of quartiles). Categorical variables were presented as numbers (n) and percentages (%). One-way analysis of variance (ANOVA) was used to evaluate normally distributed data, and the Tukey's honest significant difference test was used for post hoc pairwise comparisons within groups. The Mann-Whitney U test, Wilcoxon signed-rank test, repeated measures ANOVA, and Kruskal-Wallis test were used for nonnormally distributed data, and Bonferroni correction was used for post hoc pairwise comparisons. The Pearson chi-square test was used to compare categorical variables. The confidence interval was set at 95%, and a p-value <0.05 was considered statistically significant in all analyses. A power analysis was performed using G*Power version 3.1.9.7 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). Based on the local massage DASH-WM values, post hoc power analysis for 52 patients was calculated as 0.99 of 0.05 error margin and 0.719 effect.
Results
The three groups were similar in terms of age, sex, dominant hand, and affected side (p>0.05). The right elbow was affected in 65% of patients, the right hand was dominant in 90% of the patients, and the dominant elbow was affected in 67% of the patients. The demographic data of the participants are presented in Table I.
Table 1. Demographic data of the patients.
| Group 1 (n=17) | Group 2 (n=17) | Group 3 (n=18) | p | |||||||
| n | % | Mean±SD | n | % | Mean±SD | n | % | Mean±SD | ||
| Age (year) | 46.1±10.9 | 46.0±8.8 | 46.7±11.3 | 0.940 NS | ||||||
| Sex | 0.318 NS | |||||||||
| Female | 8 | 47.06 | 10 | 58.52 | 6 | 33.33 | ||||
| Male | 9 | 52.94 | 7 | 41.18 | 12 | 66.67 | ||||
| Side (Dom/Aff) | 0.268 NS | |||||||||
| Right/Right | 12 | 70.58 | 9 | 52.94 | 11 | 61.11 | ||||
| Right/Left | 4 | 23.52 | 4 | 23.52 | 7 | 38.88 | ||||
| Left/Right | 0 | 0 | 2 | 11.76 | 0 | 0 | ||||
| Left/Left | 1 | 5.88 | 2 | 11.76 | 0 | 0 | ||||
| SD: Standard deviation; Dom: Dominant; Aff: Affected; NS: Nonsignificant. | ||||||||||
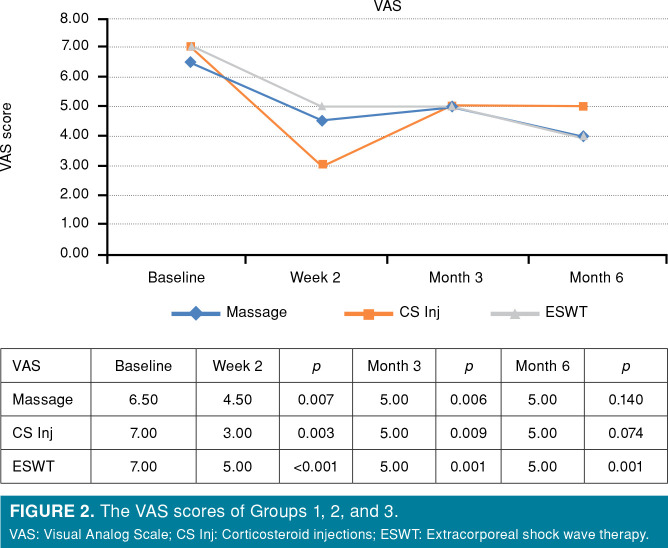
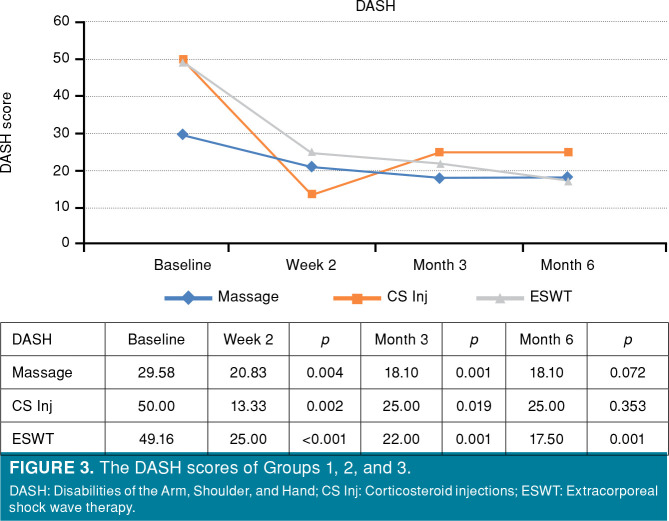
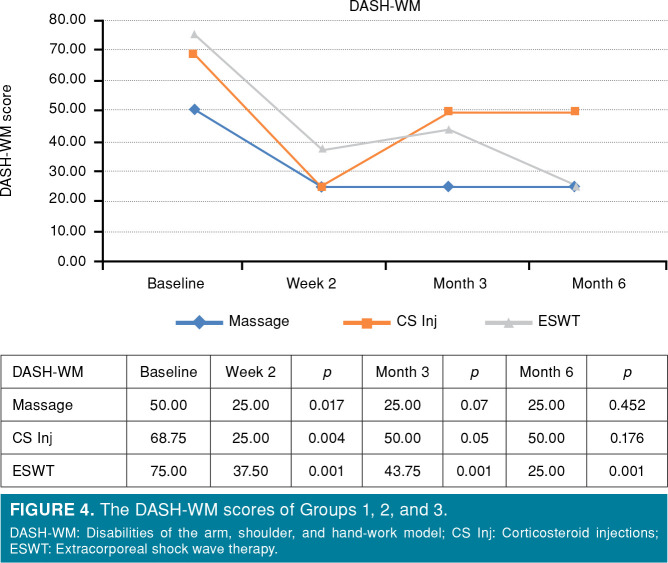
Similar results were observed between VAS, DASH, and DASH-WM scores measured during LE diagnosis (p=0.069, p=0.059, and p=0.086). In the first two weeks of follow-up, VAS scores decreased from 6.5 to 4.5 in Group 1 (p=0.007), from 7.0 to 3.0 in Group 2 (p=0.03), and from 7.0 to 5.0 in Group 3 (p<0.001). The DASH scores decreased from 29.58 to 20.83 in Group 1 (p=0.04), from 50.0 to 13.33 in Group 2 (p=0.02), and from 49.16 to 25.0 in Group 3 (p<0.001). The DASH-WM scores decreased from 50.0 to 25.0 in Group 1 (p=0.017), from 68.75 to 25.0 in Group 2 (p=0.04), and from 75.0 to 37.50 in Group 3 (p=0.001). At the two-week follow-up, statistically significant decreases were observed in VAS, DASH, and DASH-WM scores in all three groups (Table II).
Table 2. Clinical scores of the patient groups.
| Measurement values | Compared to baseline | ||||||||||
| Baseline | 2nd | Week | 3rd Month | 6th Month | 2nd Week | 3rd Month | 6th Month | ||||
| VAS | Median | IQR | Median | IQR | Median | IQR | Median | IQR | p value | p value | p value |
| Massage | 6.50 | 1.50 | 4.50 | 3.25 | 5.00 | 1.50 | 5.00 | 3.00 | 0.007* | 0.006* | 0.140 |
| CS Inj | 7.00 | 3.00 | 3.00 | 1.00 | 5.00 | 3.25 | 5.00 | 3.50 | 0.003* | 0.009* | 0.074 |
| ESWT | 7.00 | 1.00 | 5.00 | 2.50 | 5.00 | 2.75 | 4.00 | 3.50 | <0.001* | 0.001* | 0.001* |
| DASH | |||||||||||
| Massage | 29.58 | 12.92 | 20.83 | 23.13 | 18.10 | 14.58 | 18.10 | 10.95 | 0.004* | 0.001* | 0.072 |
| CS Inj | 50.00 | 25.83 | 13.33 | 18.70 | 25.00 | 18.00 | 25.00 | 20.45 | 0.002* | 0.019* | 0.353 |
| ESWT | 49.16 | 9.40 | 25.00 | 25.25 | 22.00 | 39.37 | 17.50 | 39.63 | <0.001* | 0.001* | 0.001* |
| DASH-WM | |||||||||||
| Massage | 50.00 | 50.00 | 25.00 | 34.38 | 25.00 | 25.25 | 25.00 | 31.25 | 0.017* | 0.07 | 0.452 |
| CS Inj | 68.75 | 31.25 | 25.00 | 25.00 | 50.00 | 25.00 | 50.00 | 25.00 | 0.004* | 0.05 | 0.176 |
| ESWT | 75.00 | 25.00 | 37.50 | 25.00 | 43.75 | 43.45 | 25.00 | 56.25 | 0.001* | 0.001* | 0.001* |
| VAS: Visual Analog Scale; IQR: Inter quartile range; CS Inj: Corticosteroid injections; ESWT: Extracorporeal shock wave therapy; DASH: Disabilities of the Arm, Shoulder, and Hand; WM: Work model; * Significant at p<0.05. | |||||||||||
At the three-month follow-up, the patients were reevaluated, and the scores were compared with those of the two-week follow-up. When we analyzed the VAS scores (Figure 2), an 11% increase was observed in Group 1 (from 4.5 to 5.0), while no change was found in Group 3. However, a dramatic increase of 66% was observed in Group 2 (from 3.0 to 5.0). When DASH scores were evaluated, a decrease was observed in Groups 1 and 3 (from 20.83 to 18.10 and from 25.00 to 22.00, respectively), whereas a significant increase of 87% was observed in Group 2 (from 13.33 to 25.00; Figure 3). There was no change in DASH-WM scores in Group 1, whereas an increase of 14% was observed in Group 3 (from 35.50 to 43.75). In Group 2, a considerable increase of 50% was observed (Figure 4).
Figure 2. The VAS scores of Groups 1, 2, and 3. VAS: Visual Analog Scale; CS Inj: Corticosteroid injections; ESWT: Extracorporeal shock wave therapy.
Figure 3. The DASH scores of Groups 1, 2, and 3. DASH: Disabilities of the Arm, Shoulder, and Hand; CS Inj: Corticosteroid injections; ESWT: Extracorporeal shock wave therapy.
Figure 4. The DASH-WM scores of Groups 1, 2, and 3. DASH-WM: Disabilities of the arm, shoulder, and hand-work model; CS Inj: Corticosteroid injections; ESWT: Extracorporeal shock wave therapy.
When the three-month follow-up values were compared with the baseline values, a decrease in VAS scores was observed in all three groups. The decrease in DASH scores was statistically significant in all three groups (p<0.05). While a decrease in DASH-WM scores was observed in all three groups, this decrease was statistically significant only in Group 3 (p=0.001). At the three month follow-up Group 1 and Group 2 showed a significant difference both VAS and DASH scores. Group 3 had a significant difference in all clinical evaluation scores.
When the scores measured at the three-month follow-up were compared with the scores measured at the six-month follow-up, there was no change in VAS scores in Groups 1 and 2, whereas the decrease in VAS scores continued in Group 3. The DASH and DASH-WM scores were unchanged in Groups 1 and 2 but continued to decrease in Group 3.
When the six-month follow-up values were compared with the baseline values, although the VAS scores were lower in all three groups, only the decrease in VAS scores in Group 3 was statistically significant (p=0.001). The DASH and DASH-WM scores decreased in all three groups, but only the decrease in Group 3 was statistically significant (p=0.001). At the six-month follow-up, no significant difference was observed in Groups 1 and 2 in any of the scoring systems, while Group 3 showed significant improvements in all scoring systems.
In Group 1, all three scores decreased significantly in the first two weeks, but no significant difference was observed in any of the scores at the six-month follow-up. This showed th at local massage therapy was most effective in the first two weeks. Group 2 showed a significant decrease in all scores at two weeks, whereas no statistically significant decrease was observed in any of the scores at six months. However, a significant decrease was observed in VAS and DASH scores at three months. In addition, all measurements at the three-month follow-up were higher than those at two weeks but lower than the baseline values. Group 3 showed statistically significant decreases in all scores throughout the follow-up period.
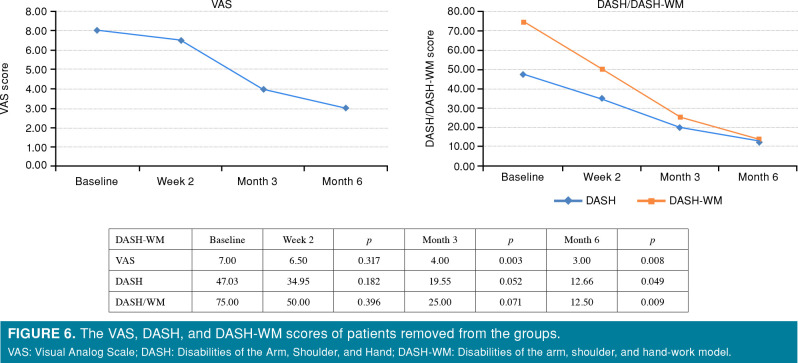
Subgroup patients who need additional treatment (n=10), seven patients were in the local massage group, two in the CS injection group, and one in the ESWT group. Two patients were excluded from the study after the first week, six patients after the second week, and two patients after the third month. Of the three patients who received CS injection as the final treatment, two started treatment with local massage therapy and one with ESWT. Among the seven patients who underwent ESWT as the final treatment, one patient started treatment with local massage, two patients started treatment with CS injection, and four patients first received local massage therapy, followed by CS injection due to no improvement and then ESWT treatment for the same reason (Figure 5). Although subgroup patients who need additional treatment, their outcomes were followed, and all patients showed significant improvement in all three scores at the end of six months (p<0.05, Figure 6). Thus, two patients who received local massage and CS injection, one patient who received local massage + ESWT, three patients who received CS injection + ESWT, and four patients who received local massage + CS injection + ESWT were followed and evaluated for six months.
Figure 5. Patients switching treatment. ESWT: Extracorporeal shock wave therapy; CS: Corticosteroid.
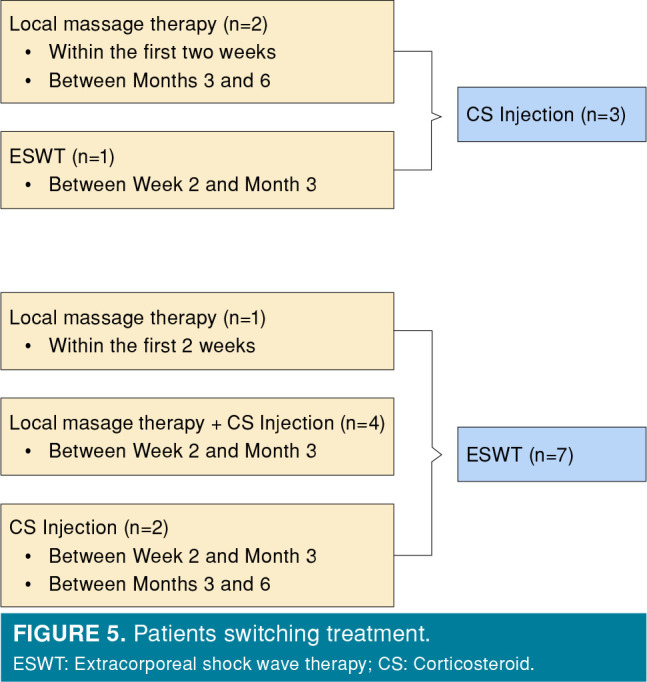
Figure 6. The VAS, DASH, and DASH-WM scores of patients removed from the groups. VAS: Visual Analog Scale; DASH: Disabilities of the Arm, Shoulder, and Hand; DASH-WM: Disabilities of the arm, shoulder, and hand-work model.
Discussion
Although there are many treatment methods used for LE, there is still no consensus on a standard, effective method. Moreover, there are relatively few studies that show the superiority of these treatments over one another. In the present study, we investigated the effect of local massage, CS injection, and ESWT treatment on LE. We also analyzed the relationships between these treatments. According to the results of the present study, improvement in clinical scores was observed in all three groups at the six-month follow-up, while significant results were recorded only in the ESWT group. On the contrary, significant clinical improvement was observed in all three groups in the short term.
Numerous studies have evaluated massage therapy for LE in the literature. Yi et al.[17] reported significant results obtained with massage therapy at the six-month follow-up. Our results are not consistent with the findings of these study. We did not detect a significant improvement with local massage therapy between diagnosis and six months of follow-up. Conversely, Eapen et al.[18] reported positive results from local massage therapy in the short term. In the present study, local massage therapy also showed improvement in the short term. According to Waters-Banker et al.,[19] local massage is effective in the short term because it alleviates the inflammatory process, facilitates early healing, and relieves pain in muscle injuries. They described this effect as an immunomodulatory response to the biochemical and cellular changes induced by massage.
In 1983, Cyriax and Cyriax[20] suggested that local massage increased the circulation and recycling of fluids by vasodilatation. In addition, Stasinopoulos and Johnson[21] reported that local massage produces a rapid analgesic effect in the affected area. In 1984, Bruijn[22] suggested that the analgesic effect was due to local anesthesia resulting from the release of endogenous opiates or the release of inhibitory neurotransmitters that reduce pain intensity. These data suggest that local massage is a method of analgesia rather than treatment. Although VAS and DASH scores of the patients in the local massage group improved in the two-week and three-month controls, DASH-WM scores did not improve. Although patients were able to perform simple daily activities, significant improvements and full recovery can only be achieved when they return to work. Therefore, we believe that local massage therapy does not provide full recovery, even in the short term.
Some studies have shown that CS injection yields significant results in the short term but not in the long term.[23,24] The results obtained in the present study were consistent with those in the literature. The use of CS in combination with local anesthetics provides short-term improvement for patients due to their anti-inflammatory and analgesic effects. However, clinical evaluations at three months in our study showed worse results compared to the two-week follow-up. The results did not change between three and six months. Nevertheless, we achieved good results at six months compared to baseline, albeit not significant. Corticosteroid injection led to some improvement in the long term. The high recurrence rates and some side effects of CS should be considered by the physician and patient.[23] The superior short-term effectiveness of CS injection and the loss of long-term effectiveness could be attributed to the use of short- or long-acting CS, but in studies using long-acting steroids, the steroid was not as effective in the long term as it was in the short term.[25] Patients may benefit more if the injection is administered in combination with another longacting treatment (for example, ESWT).[26]
Extracorporeal shock wave therapy is a treatment method used in diseases such as fasciitis, tendonitis, and epicondylitis. It involves the application of sound waves to the affected area.[13] Some studies reported significant improvements with the ESWT application in the treatment of LE.[27] However, other studies reported that ESWT had no effect.[28] To the best of our knowledge, there are no studies in the literature where all three treatments (local massage, CS injection, and ESWT) were applied and the treatment process was analyzed.[29] According to the results of the present study, improvement in clinical scores was observed in all three groups at the six-month follow-up, while significant results were recorded only in the ESWT group (p=0.001).[29] More studies should be conducted to establish a consensus on ESWT treatment regarding the specific frequency, specific number of sessions, specific treatment interval, specific pressure level, total treatment time, and specific number of pulses. Thus, as long as ESWT is applied correctly in LE treatment, a protocol can be established. The results obtained in the present study could have been even more promising if such a protocol had been followed.
Yalvaç et al.[30] compared CS injection and ESWT in their study and reported that both treatments provided equal improvement in the short term, but ESWT yielded better results in the following three months.
In the present study, patients who had to receive additional treatment and were continued to be followed as a subgroup were also evaluated. According to our analyses, the clinical outcomes of patients whose pain did not improve and who switched to another treatment were much better than those of patients who benefited from the first treatment and continued with one treatment. Based on this finding, if the response of patients with LE to initial treatment is not satisfactory or if there is an increase in complaints, instead of continuing with the same treatment, treatment can be changed, or a combined treatment can be tried. However, since there were no patients in the present study who received local massage as a subsequent treatment, it is not possible to recommend local massage as a subsequent treatment at this time. More comprehensive studies are needed for combined therapies for patients with LE.
The fact that patients whose pain persisted and who received additional treatment were followed up on in subsequent controls can be considered a strength of the study in terms of transparency. On the other hand, the small number of patients who received combined treatment may be considered a limitation of the study.
In conclusion, ESWT was superior to both local massage and CS injection treatments throughout the study and at final follow-up on LE. Local massage therapy did not provide complete recovery, even in the short term. In patients receiving CS injections, as the treatment process gets longer the clinical outcomes get worsen. Patients who were excluded from the groups and received double and triple combination therapy had good clinical outcomes at the final follow-ups. Further studies on combined treatment modalities are needed on this subject.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: Design, data collection and processing, analysis and interpretation, literature review, writing, critical review, references and fundings: B.V.Ç.; Data collection and processing, materials: Ö.S., M.D.; Analysis and interpretation, literature review, writing: İ.Y.; Analysis and interpretation: A.Y.K., Ö.O.; Conception, design, control/ supervision: M.A.A.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
Data Sharing Statement: The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Regan W, Wold LE, Coonrad R, Morrey BF. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med. 1992;20:746–749. doi: 10.1177/036354659202000618. [DOI] [PubMed] [Google Scholar]
- 2.Yaka H, Başbuğ V, Tekin AA, Özer M. Evaluation of the relationship between lateral epicondylitis and vitamin D. Jt Dis Relat Surg. 2022;33:414–418. doi: 10.52312/jdrs.2022.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Runge F. Zur RF. Genese und behandlung des schreibekramfes. Berlin: Klin Wochenschr. 1873;10:245–248. [Google Scholar]
- 4.Rio E, Moseley L, Purdam C, Samiric T, Kidgell D, Pearce AJ, et al. The pain of tendinopathy: Physiological or pathophysiological. Sports Med. 2014;44:9–23. doi: 10.1007/s40279-013-0096-z. [DOI] [PubMed] [Google Scholar]
- 5.Alfredson H, Ljung BO, Thorsen K, Lorentzon R. In vivo investigation of ECRB tendons with microdialysis technique--no signs of inflammation but high amounts of glutamate in tennis elbow. Acta Orthop Scand. 2000;71:475–479. doi: 10.1080/000164700317381162. [DOI] [PubMed] [Google Scholar]
- 6.Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg [Am] 1999;81:259–278. [PubMed] [Google Scholar]
- 7.Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis. A systematic review. Clin Rehabil. 2014;28:3–19. doi: 10.1177/0269215513491974. [DOI] [PubMed] [Google Scholar]
- 8.Kohia M, Brackle J, Byrd K, Jennings A, Murray W, Wilfong E. Effectiveness of physical therapy treatments on lateral epicondylitis. J Sport Rehabil. 2008;17:119–136. doi: 10.1123/jsr.17.2.119. [DOI] [PubMed] [Google Scholar]
- 9.Viola L. A critical review of the current conservative therapies for tennis elbow (lateral epicondylitis) Australas Chiropr Osteopathy. 1998;7:53–67. [PMC free article] [PubMed] [Google Scholar]
- 10.Olaussen M, Holmedal O, Lindbaek M, Brage S, Solvang H. Treating lateral epicondylitis with corticosteroid injections or non-electrotherapeutical physiotherapy: A systematic review. e003564BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Price R, Sinclair H, Heinrich I, Gibson T. Local injection treatment of tennis elbow--hydrocortisone, triamcinolone and lignocaine compared. Br J Rheumatol. 1991;30:39–44. doi: 10.1093/rheumatology/30.1.39. [DOI] [PubMed] [Google Scholar]
- 12.Hanna M, Trinh K, Degregoris G, Ferriter P, Steven M. Differential diagnosis of isolated elbow pain and treatment in patients with medial or lateral epicondylitis. Part 2. Pract Neurol. 2014:37–40. [Google Scholar]
- 13.Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N. Lateral epicondylitis: A review of pathology and management. Bone Joint J. 2013;95- B:1158–1164. doi: 10.1302/0301-620X.95B9.29285. [DOI] [PubMed] [Google Scholar]
- 14.Arnett JJ, Mandel S, Aydin SM, Brigham CR. A review of the evaluation, treatment, and rating of lateral epicondylitis. Guides Newsletter. 2016;21:10–13. doi: 10.1001/amaguidesnewsletters.2016.JanFeb02. [DOI] [Google Scholar]
- 15.Pettrone FA, McCall BR. Extracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitis. J Bone Joint Surg [Am] 2005;87:1297–1304. doi: 10.2106/JBJS.C.01356. [DOI] [PubMed] [Google Scholar]
- 16.Trentini R, Mangano T, Repetto I, Cerruti P, Kuqi E, Trompetto C, et al. Short- to mid-term follow-up effectiveness of US-guided focal extracorporeal shock wave therapy in the treatment of elbow lateral epicondylitis. S91-7Musculoskelet Surg. 2015;99 Suppl 1 doi: 10.1007/s12306-015-0361-4. [DOI] [PubMed] [Google Scholar]
- 17.Yi R, Bratchenko WW, Tan V. Deep friction massage versus steroid injection in the treatment of lateral epicondylitis. Hand (N Y) 2018;13:56–59. doi: 10.1177/1558944717692088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eapen C, Rosita R, Sohani MS, Patel VD. A systematic review of the effectiveness of wrist manipulative therapy in patients with lateral epicondylitis. J Hand Ther. 2023;36:528–535. doi: 10.1016/j.jht.2022.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Waters-Banker C, Dupont-Versteegden EE, Kitzman PH, Butterfield TA. Investigating the mechanisms of massage efficacy: The role of mechanical immunomodulation. J Athl Train. 2014;49:266–273. doi: 10.4085/1062-6050-49.2.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cyriax HJ, Cyriax JP. Cyriax's illustrated orthopedic medical manual. Boston: Butterworth-Heinemann; 1983. [Google Scholar]
- 21.Stasinopoulos D, Johnson MI. Cyriax physiotherapy for tennis elbow/lateral epicondylitis. Br J Sports Med. 2004;38:675–677. doi: 10.1136/bjsm.2004.013573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Bruijn R. Deep transverse friction: Its analgesic effect. Int J Sports Med. 1984;5:35–36. doi: 10.1055/s-2008-1025944. [DOI] [Google Scholar]
- 23.Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: Randomised trial. BMJ. 2006;333:939–939. doi: 10.1136/bmj.38961.584653.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smidt N, van der Windt DA, Assendelft WJ, Devillé WL, Korthals-de Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: A randomised controlled trial. Lancet. 2002;359:657–662. doi: 10.1016/S0140-6736(02)07811-X. [DOI] [PubMed] [Google Scholar]
- 25.Lindenhovius A, Henket M, Gilligan BP, Lozano-Calderon S, Jupiter JB, Ring D. Injection of dexamethasone versus placebo for lateral elbow pain: A prospective, double-blind, randomized clinical trial. J Hand Surg Am. 2008;33:909–919. doi: 10.1016/j.jhsa.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Tonks JH, Pai SK, Murali SR. Steroid injection therapy is the best conservative treatment for lateral epicondylitis: A prospective randomised controlled trial. Int J Clin Pract. 2007;61:240–246. doi: 10.1111/j.1742-1241.2006.01140.x. [DOI] [PubMed] [Google Scholar]
- 27.Maffulli G, Iuliano E, Padulo J, Furia J, Rompe J, Maffulli N. Extracorporeal shock wave therapy in the treatment of tennis elbow the ASSERT database. Muscles Ligaments Tendons J. 2018;8:437–443. doi: 10.11138/mltj/2018.8.3.423. [DOI] [Google Scholar]
- 28.Buchbinder R, Green SE, Youd JM, Assendelft WJ, Barnsley L, Smidt N. Shock wave therapy for lateral elbow pain. CD003524Cochrane Database Syst Rev. 2005;2005 doi: 10.1002/14651858.CD003524.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atik OŞ. Writing for Joint Diseases and Related Surgery (JDRS): There is something new and interesting in this article! Jt Dis Relat Surg. 2023;34:533–533. doi: 10.52312/jdrs.2023.57916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yalvaç B, Mesci N, Geler Külcü D, Yurdakul OV. Comparison of ultrasound and extracorporeal shock wave therapy in lateral epicondylosis. Acta Orthop Traumatol Turc. 2018;52:357–362. doi: 10.1016/j.aott.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]