The practice of avoiding exposure to allergens (allergen avoidance) for allergic diseases such as asthma is not a new idea. In the 16th century the Archbishop of St Andrews had a miraculous remission of his intractable asthma by getting rid of his feather bedding, and in 1927 Storm van Leeuwen created a “climate chamber” in Holland in an attempt to recreate the beneficial environment of high altitude sanatoriums. This article focuses on how to avoid indoor allergens in homes in temperate climates and the potential benefits for sensitised patients with atopic disorders.
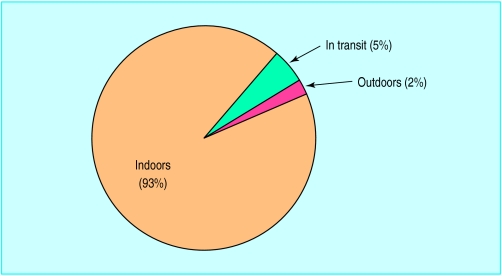
Nowadays most people spend more than 90% of their lives indoors. Over the past 30 years, the home environment has changed enormously with the introduction of soft furnishings, fitted carpets, and central heating. Indoor ventilation has decreased—the rate at which indoor air is exchanged for fresh air is now 10 times lower than it was 30 years ago, with a considerable increase both in humidity and in concentrations of indoor pollutants and airborne allergens. As exposure to allergens is an important cause of symptoms in sensitised patients, reducing exposure should improve disease control. In spite of this, few patients in Britain with asthma, eczema, or perennial rhinitis, or any combination of these, are skin tested.
Few patients in Britain with asthma, eczema, or perennial rhinitis receive advice on appropriate avoidance measures
Characteristics of indoor allergens
The predominant indoor allergens in Britain are from mites, cats, and dogs, and they have dramatically different aerodynamic characteristics. Mite allergens are present on large particles in beds, soft furnishings, and carpets, which become airborne only after vigorous disturbance and settle quickly. In contrast, about 25% of cat and dog allergens are associated with small particles <5 μm in diameter, which after disturbance remain airborne for prolonged periods. This in part explains the difference in clinical presentation between asthmatic people who are sensitive to mites and those sensitive to their pets. Patients allergic to dust mite may be unaware of the relation between asthma and exposure to mites, as this is a predominantly low grade chronic exposure occurring overnight in bed. Patients allergic to cats or dogs may develop symptoms within minutes of entering a home with these animals or simply by stroking an animal, as a result of inhaling large amounts of easily respirable cat and dog allergen.
Concentrations of indoor allergens
The highest concentration of mite allergens is found in beds; patients spend 6-8 hours every night in close contact with their mattress, pillow, and bedding, so the reduction of exposure in the bedroom is critical
Most exposure to pet allergens probably occurs in living areas other than the bedroom, and this must be taken into account when planning avoidance strategies
In public areas—for example, cinemas and public transport—mite allergen levels are low, but exposure to airborne pet allergens can be substantial even in hospital outpatient areas
Exposure to cockroach allergens may be important in schools and some high rise blocks of flats
For symptoms to occur, atopic patients need to be exposed to allergens to which they are sensitised. Allergen avoidance should be recommended only to those symptomatic individuals who are sensitised on the basis of skin tests or specific serum IgE concentration.
Mites
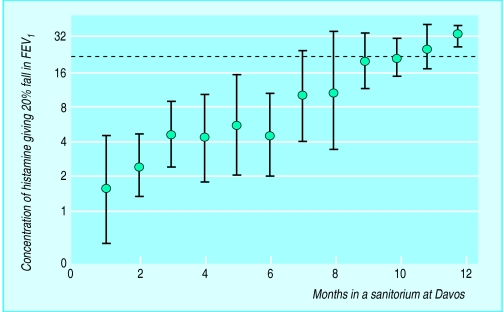
Lessons from high altitude
At high altitude, low levels of humidity mean that mites cannot survive, and so mite allergen concentrations are low. Asthma control in mite sensitive patients moving to high altitude improves, although full improvement may take 6-12 months to achieve. The real challenge facing physicians in Britain is to create a low allergen environment in patients’ homes that is sufficiently flexible to suit individual needs and at the same time not prohibitively expensive. Many avoidance measures have been tested, but only a few have been subjected to randomised controlled trials.
Controlling concentrations of mite allergens
Bedrooms
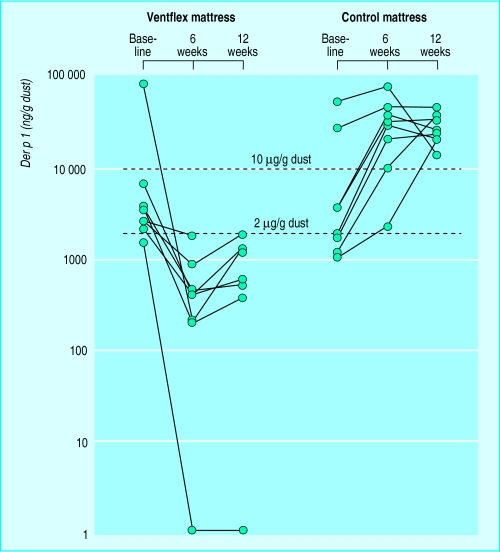
The single most effective measure is to cover the mattress, pillows, and duvet with covers that are impermeable to mite allergens. These covers used to be made of plastic and were uncomfortable to sleep on. Now fabrics permeable to water vapour (either microporous or polyurethane coated) but also both impermeable to mite allergens and comfortable to sleep on are available. Allergen concentrations decrease by up to 100-fold after such covers are introduced.
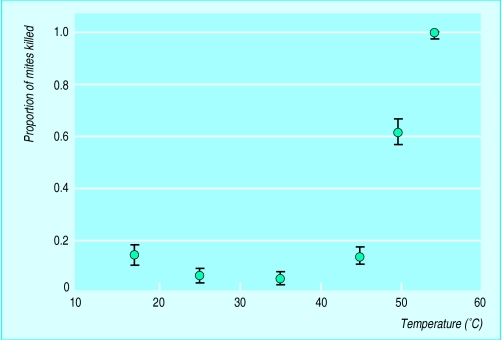
All exposed bedding should be washed at 55°C. This kills mites and removes allergen; although the “cold” cycle (30°C) of laundry washing dramatically reduces allergen concentrations, most mites survive it. The covers should be wiped down at each change of bedding.
Buying a new mattress produces only a temporary benefit as reinfestation may occur within a few months from other reservoirs, such as carpets. Ideally, bedroom carpets should be replaced with sealed wooden or vinyl flooring, and the curtains should be hot washed regularly or replaced with wipeable blinds. In this way exposure to mite allergens in the bedroom at night can be virtually abolished. Substantial clinical benefit of effective mite avoidance has been shown in mite sensitised asthmatic patients and in patients with eczema or perennial rhinitis.
Rest of the house
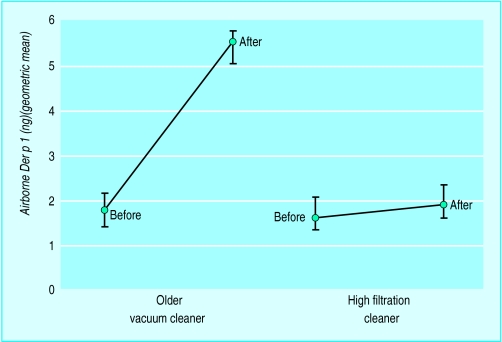
Intensive vacuum cleaning with high filtration cleaners reduces the size of the allergen reservoir, but no benefit has been established in a clinical trial. Older vacuum cleaners with inadequate exhaust filtration should be avoided as they provide one of the few ways to get large amounts of mite allergen airborne. Sensitised asthmatic patients who have to use a vacuum cleaner should use one with a built-in high efficiency particulate air filter and also use double thickness bags.
Actions for avoiding exposure to mite allergens in relation to asthma in Britain
| Do help | Do not help |
| Special bed covers (with or without cleaning) | Acaricides |
| Removal of habitat (eg, carpet) | Air filters or ionisers |
| Moving to Switzerland | Ventilation systems |
Killing mites with chemicals (acaricides) is feasible in the laboratory, but convincing evidence of clinical benefit is lacking. Mites can be killed in carpets either with steam or by freezing with liquid nitrogen, but both techniques are unlikely to produce sufficient benefits to warrant the huge effort required (in addition, regular treatment is necessary). Air filters and ionisers are of no clinical benefit as mite allergen does not stay airborne.
A final alternative might be to reduce humidity to suppress the growth of mites. This has been attempted by the use of mechanical ventilation and with portable dehumidifiers. Neither of these techniques reduces humidity levels in typical British houses sufficiently to suppress mite growth, and allergen concentrations have not been shown to be reduced.
Pet allergens
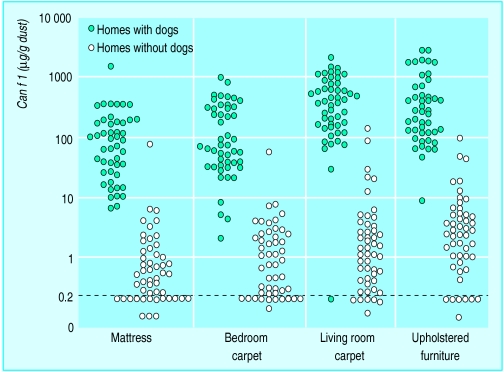
Pet allergens are present in huge concentrations in houses with cats and dogs, but they are also transferred on clothing, so concentrations are detectable in homes without pets and in public buildings and transport.
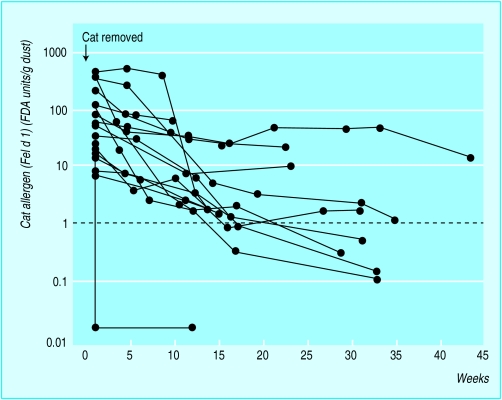
For an asthmatic patient who owns a pet and is sensitised to the animal, the best way to reduce exposure is to get rid of the pet, but this is rarely feasible as owners are usually very attached to their pets. Even after permanent removal of a cat or dog from the home, it may take many months before the reservoir allergen concentration returns to normal. So if patients do get rid of their pets they should not expect their symptoms to improve immediately—it may take 6-12 months for full benefit.
If the pet remains in the home, advice can be given about methods that are known to reduce airborne pet allergens. The pet should be kept out of the bedroom and preferably outdoors or in a well ventilated area—for example, a kitchen. In homes with a pet, the concentration of airborne pet allergens will be considerable higher when the pet is actually in a room than when it is elsewhere in the house.
Ideally, carpets should be removed, as the concentration of pet allergens can be as much as 100 times higher in carpets than in polished floors. If carpets remain then regular cleaning with a high filtration cleaner is advised. Washing the animal thoroughly and as often as possible, combined with the use of a high efficiency particulate air cleaner, is the best way to reduce allergens, but whether these practices are clinically effective is as yet unproved.
Avoiding cat and dog allergens
| Reduce airborn allergen | Gives clinical benefit | |
| Removal of pet | ✓ | ✓ |
| Pet in situ: | ||
| ✓ | ? | |
| Wash pet | ✓ | ? |
| ✓ | ? | |
| Remove carpets | ✓ | ? |
| High efficiency particulate air filter | ||
| Castrate male or get a female (cat) |
Allergen avoidance in primary prevention of atopic diseases
Sensitisation to allergens seems to be related to exposure to allergens in early life. The key question is whether early allergen avoidance can prevent allergic disease developing in the first place.
The innovative Isle of Wight study has examined the effect of avoiding mite allergens and certain foods from birth onwards on the development of atopy and asthma. This study used acaricides, and hence the reduction in the concentration of mite allergens was relatively modest. Even these minor reductions, however, were associated with a reduction in eczema and episodic wheezing.
First steps in treating atopic diseases
Diagnose disease by taking a history and by either performing skin testing or measuring specific serum IgE concentrations
Minimise the impact of identified environmental risk factors such as mites, cats, and dogs
Regard allergen avoidance as an integral part of the overall management of sensitised asthmatic patients
Several prospective cohorts of babies at high risk of atopy or asthma have been randomised to more effective protocols for avoiding exposure to mite allergens and are currently being studied. Population based studies are also being planned.
The future
Exposure to indoor allergens may have contributed to the observed increase in asthma prevalence. The important issue is whether asthma can be prevented by allergen avoidance in early life. Primary allergen avoidance is premature outside the context of a clinical trial but may be an important aspect of preventive therapy by the end of this century. Major changes in the domestic environment are likely over the next decade, with the removal of dust mite habitats—that is, a return to hard flooring—a reduction in indoor humidity, and the encasing of all bed and bedding with mite proof covers.
Further reading
Platts Mills TAE, Vervloet D, Thomas WR, Aalberse RC, Chapman MD. Indoor allergens and asthma: report of the third international workshop. J Allergy Clin Immunol 1997;100(6):S1-24
Custovic A, Simpson A, Chapman MD, Woodcock A. Allergen avoidance in the treatment of asthma and atopic disorders. Thorax 1998;53:63-72
Collof MJ, Ayres J, Carswell F, Howarth PH, Merrett TG, Mitchell EB, et al. The control of allergens of dust mites and domestic pets: a position paper. Clin Exp Allergy 1992;22(suppl 2):1-28
Pope AM, Patterson R, Burge H, eds. Indoor allergens—assessing and controlling adverse health effects. Washington, DC: National Academy Press, 1993
Figure.
Amount of time that most Americans spend indoors, outdoors, and in transit
Figure.
Progressive reduction in non-specific bronchial hyperreactivity (histamine) in 10 asthmatic children allergic to mites who moved from home to a mite free environment (a sanatorium in Davos, Switzerland)
Figure.
Approximate 100-fold reduction in concentrations of house dust mite allergen (Der p 1) on mattresses after introduction of covers that are impermeable to mite allergens (Ventflex covers)
Figure.
Proportion of mites killed at different washing temperatures
Figure.
Comparison of older vacuum cleaner (with inadequate exhaust filtration) with high filtration cleaner, showing significantly increased concentrations of airborne house dust mite allergen (Der p 1) in older cleaners before and after vacuuming
Figure.
Distribution of dog allergen (Can f 1) in settled dust from four sampling sites in 100 homes in Manchester (50 with a dog, 50 without). Can f 1 was readily detectable in homes without dogs, but the levels were between 10-fold and 100-fold lower than in houses with dogs
Figure.
Milo: could you get rid of her?
Figure.
Effect on allergen concentrations of removing a cat from a home
Acknowledgments
The following illustrations are reproduced or adapted with the permission of the publishers: the pie chart (Pope et al (Indoor Allergens, National Academy Press, 1993)); and the graphs showing results in children in Davos (Plant Mills et al (J Allergy Clin Immunol 1987;80:755-75)); allergen concentrations on mattresses (Owen S, et al (Lancet 1990;335:396-7)); mites killed during washing (McDonald et al (J Allergy Clin Immunol 1992;90:599-608)); concentrations of airborne house dust mite allergen in vacuum cleaners (Kalra S, et al (Lancet 1990;336:449)); distribution of dog allergen (Custovic A, et al (Am J Respir Crit Care Med—1997;155:94-8)); and effect on allergen concentrations by cat removal (Wood RA, et al (J Allergy Clin Immunol 1989;83:730-4)).
Footnotes
Ashley Woodcock is a consultant respiratory physician and Adnan Custovic is a specialist registrar in allergy at the North West Lung Centre, Wythenshawe Hospital, Manchester.
The ABC of allergies is edited by Stephen Durham, honorary consultant physician in respiratory medicine at the Royal Brompton Hospital, London. It will be published as a book later in the year. BMJ 1998;316:0000-0