Abstract
BACKGROUND
Cardiac arrest (CA) induced by electric shock is a rare occurrence, particularly in cases of prolonged CA. Currently, there is limited literature on similar incidents, and we present a relevant case report.
CASE SUMMARY
A 27-year-old Asian male man, experiencing respiratory CA due to electric shock, was successfully restored to sinus rhythm after 50 min of cardiopulmonary resuscitation and 8 electrical defibrillation sessions. In the subsequent stages, the patient received multiple organ function protection measures, leading to a successful recovery and eventual discharge from the hospital.
CONCLUSION
Prolonging resuscitation time can enhance the chances of survival for patients, this study provide valuable insights into the management of electric shock-induced CA.
Keywords: Electric shock, Cardiac arrest, Prolonged cardiopulmonary resuscitation, Cerebral resuscitation, Case report
Core Tip: The successful management of a young patient experiencing respiratory cardiac arrest due to electrical injury was accomplished through prolonged cardiopulmonary resuscitation. This study emphasizes the significance of persisting in rescue efforts for individuals with cardiac and respiratory arrest, particularly among young patients without significant organ dysfunction. By extending the duration of resuscitation and implementing early measures for brain protection, not only can normal autonomic circulation be restored but also complete recovery of brain function can be achieved.
INTRODUCTION
Timely and proficient implementation of cardiopulmonary resuscitation (CPR) is crucial for the successful resuscitation of patients who undergo electric shock-induced cardiac arrest (CA), a critical and urgent condition in the emergency department. Prolonging the CPR duration as much as possible can potentially save more lives. Early hyperbaric oxygen intervention treatment plays a crucial role in protecting a patient's brain function and prognosis when vital signs are stable. Patients with respiratory CA secondary to electric shock were successfully treated with prolonged CPR, as illustrated by a case report. This aims to contribute valuable insights for fellow professionals in the field.
CASE PRESENTATION
Chief complaints
The electrical shock led to a 50-min respiratory CA.
History of present illness
A 27-year-old healthy young man suffered from respiratory and CA due to accidental electric shock (AC 380 V). The family members at the scene cut off power and began to implement CPR within 5 min. Paramedics arrived at the scene in 15 min and continued CPR, while transferring the patient to the emergency department of our hospital.
History of past illness
He used to be healthy.
Personal and family history
The parents are in good health and have no reported family history of genetic disease, infectious disease, or similar conditions.
Physical examination
Upon arrival at the emergency department, the patient displayed no spontaneous respiration or heartbeat. Immediate measures, including electrocardiography monitoring, tracheal intubation, continuous external chest compression, and intravenous administration of rapid fluid rehydration, adrenaline, and dopamine were implemented. Approximately 20 min later after receiving rescue medication, the patient regained a spontaneous heartbeat, only to suffer from repeated ventricular fibrillation. The patient achieved sinus rhythm after 8 electric defibrillation attempts, a 150 mg amiodarone intravenous push, and a 1 mg/min intravenous drip. However, the patient remained unconscious with frequent convulsions and was transferred to the emergency intensive care unit (EICU) for advanced life support. Physical examination within the EICU: The patient's temperature was 36.2 °C, heart rate was 99 beats/min, and ventilator-assisted breathing was provided (PS mode: PS 8 cm H2O, PEEP 4 cm H2O, FiO2 55%). Saturation of peripheral oxygen (SPO2) was 85%, blood pressure was 137/88 mmHg. The patient was in a coma state, with a Glasgow Coma Scale score of E1VTM1. No burns were detected on the entire skin surface. The pupils were equicircular, with a diameter of approximately 4 mm. The neck was soft, with no resistance observed. Corneal reflex was absent. The abdomen was soft, with bowel sounds occurring approximately once per minute, and abdominal wall reflex was not elicited. Both bilateral Babinsky signs and meningeal irritation signs were negative.
Laboratory examinations
The results of peripheral blood examination and arterial blood gas analysis are presented in Table 1.
Table 1.
Blood examination
|
Blood examination
|
WBC (× 109/L)
|
RBC (× 1012/L)
|
Hg (g/L)
|
PLT (× 109/L)
|
ALT (U/L)
|
AST (U/L)
|
TBIL (μmol/L)
|
Troponin (μg/L)
|
Myoglobin (μg/L)
|
CKMB (μg/L)
|
Arterial blood gas analysis
|
|||||
|
pH
|
PaO2 (mmHg)
|
PaCO2 (mmHg)
|
HCO3 (mmol/L)
|
Lac (mmol/L)
|
BE (mmol/L)
|
|||||||||||
| Day 1 | 21.1 | 6.12 | 166 | 397 | 163 | 290 | 11 | 15.4 | 3811 | 79.2 | 7.27 | 59.2 | 37.8 | 17 | 12.9 | -9.13 |
| Day 2 | 21 | 5.48 | 146 | 309 | 164 | 125 | 6.1 | 9.76 | 2028 | 50.2 | 7.361 | 189.5 | 40.4 | 26.5 | 1 | 0.48 |
| Reference value | 3.5-9.5 | 4.3-5.8 | 130-175 | 125-350 | 9-52 | 14-36 | 3-22 | 0.02-0.25 | 0-140 | 0-25 | 7.35-7.45 | 80-100 | 35-45 | 22-26 | 1.0-1.7 | -3.0 to 3.0 |
WBC: White blood cell; RBC: Red blood cell; Hg: Hemoglobin; PLT: Platelet; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; TBIL: Total bilirubin; CKMB: Creatine kinase-MB.
Imaging examinations
The aforementioned information is referenced in the section dedicated to treatment.
FINAL DIAGNOSIS
Electrical injury, respiratory and CA, and postcardiac arrest syndrome.
TREATMENT
The patient underwent a sequence of interventions, including administration of amiodarone to stabilize cardiac rhythm, rapid rehydration with succinyl gelatin, acid correction using sodium bicarbonate, sedation and muscle relaxation through midazolam and bensulfuron atracurium, cerebral protection via temperature control blanket, maintenance of blood pressure with norepinephrine, oxiracetam to safeguard the brain, mannitol for prevention and treatment of brain edema and pulmonary edema, coenzyme Q10 to protect the myocardium, omeprazole to preserve gastric mucosa, reduced glutathione to enhance liver function, ceftriaxone sodium to prevent infection, and other supportive treatments.
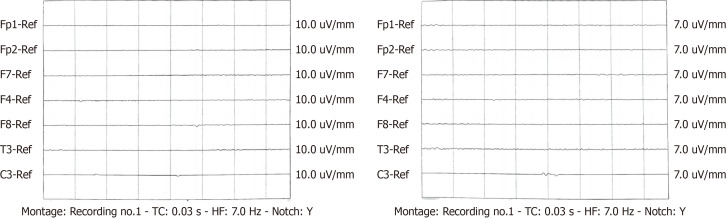
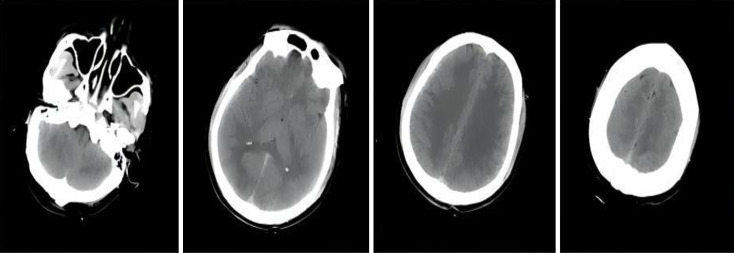
Two days post-admission, the patient underwent a repeated blood test (Table 1). The abdominal physical examination showed no positive signs, and bowel sounds were approximately 4 per minute. Enteral nutrition was administered, and ambulatory electroencephalography examination revealed severe abnormal brain waves (low voltage) (Figure 1). The computed tomography scan of the head, however, revealed no apparent abnormalities (Figure 2). Troxerutin brain protein was added to promote neurological function recovery following a neurology consultation.
Figure 1.
The ambulatory electroencephalography examination revealed pronounced abnormal brain waves characterized by low voltage.
Figure 2.
Computed tomography scan of the head showed no obvious abnormalities.
OUTCOME AND FOLLOW-UP
The patient's respiratory function improved 4 d post-admission, with Venturi oxygen used instead of mechanical ventilation, SPO2 was maintained at 96%. Seven days post-admission, the patient remained unconscious and was subjected to tracheotomy and hyperbaric oxygen therapy. By day 10, the patient could open his eyes, accompanied by significant agitation and coughing, and the sedation drugs were gradually tapered off while increasing the frequency of awakenings. By day 14, the patient could communicate simplistically, and his vital signs stabilized to facilitate a transfer to the general ward. By day 18, his condition notably improved, exhibiting autonomous eating, speaking after removal of the tracheal cannula, and mild physical activities. By day 20, the patient could communicate normally. Finally, by day 26 of admission, the patient's consciousness, activity, and speech returned to normal, resulting in discharge without lingering deficits in memory. The patient remained asymptomatic after a 6-month follow-up period post-discharge.
DISCUSSION
Electrical injury results in tissue damage and dysfunction upon entry of the current into the body, clinically manifesting as localized damage at the shock site, systemic injuries, particularly to the cardiovascular and nervous systems, and, in severe cases, respiratory and CA. The severity of electric injury is contingent on the intensity, type, voltage, contact resistance, duration, and pathway of the current within the body. Electric current typically follows the course of blood vessels and nerves, and when it traverses the heart, it can elicit respiratory depression or arrest, ventricular fibrillation, or CA[1]. In this case report, the patient promptly entered a coma subsequent to electric shock. Continuous CPR was immediately administered, which bought time for subsequent treatment. An decrease of 1 min in emergency response time could enhance patient survival rates by over 15%[2]. The essence of improving survival rates lies in promptly restoring heartbeat and respiration. The guidelines for CPR emphasize that the first 5 min post-CA constitute a golden window for CPR rescue. Beyond this critical period, the likelihood of resuscitation success precipitously declines, corresponding to a decrease in the CPR success rate for each additional minute[3,4]. Moreover, abbreviating emergency response time outside hospitals is a critical strategy for professional teams to optimize the CPR success rate in patients experiencing CA[5].
The probability of successful CPR for patients with CA decreases to less than 3% if spontaneous rhythm recovery is not achieved within 20 min, and clinical CPR may be terminated if there is still no detectable cardiac electrical activity after 30 min. However, given that most patients with electrical injuries are young adults with normal heart and lung function, medical professionals should embrace the concept of ultra-long CPR and endeavor to extend the CPR time in clinical practice, actively rescuing and saving lives[6].
Due to changes in societal roles, elderly individuals seldom encounter respiratory and CA caused by external or human factors, which sets them apart significantly from non-elderly adult patients. The primary etiologies of out-of-hospital CA (OHCA) among the elderly encompass cardiogenic and respiratory ailments as well as asphyxia. Owing to physiological deterioration, exacerbation of chronic underlying conditions, and diminished drug responsiveness following hypoxia, the success rate of resuscitation substantially diminishes with advancing age. Elderly individuals afflicted with cerebrovascular disease, dementia, cerebellar atrophy, and associated disorders frequently manifest a profound decline in swallowing function leading to an augmented risk of aspiration during meals. Furthermore, those suffering from multiple chronic diseases accompanied by respiratory tract infections may experience impaired cough reflexes and compromised airway protection functions that can further impede recovery from OHCA.
This case report presents a young male patient who underwent continuous CPR for 50 min, ultimately restoring autonomous rhythm and sinus rhythm after electrical defibrillation, providing compelling evidence for the effectiveness of long CPR.
Modern medical resuscitation strategies prioritize cardiopulmonary and cerebral resuscitation. Even during the resuscitation process, interventions such as hypothermia, dehydration, cranial pressure reduction, hyperbaric oxygen, and cerebral nerve protection should be implemented to ensure effective cerebral resuscitation. The timeliness and efficacy of cerebral resuscitation are crucial for patient recovery. Following successful CPR in this case, the patient received hypothermia, dehydration, brain tissue protection and early hyperbaric oxygen therapy. Hyperbaric oxygen therapy has been extensively used in cerebral resuscitation, and literature indicates that it can alleviate post-CPR organ ischemia and hypoxia, facilitating brain function recovery[7]. Therefore, it is recommended to administer hyperbaric oxygen therapy promptly.
In summary, the successful treatment in this case can be attributed to the following factors: (1) Implementation of effective rescue measures, including continuous and uninterrupted chest compressions, defibrillation, prompt establishment of an artificial airway with adequate ventilation, and appropriate administration of cardiovascular drugs, contributed significantly to the successful treatment in this case; (2) Despite the patient's heart stopping for over 50 min and complete loss of reflexes with no response to pain stimuli, medical staff and family members demonstrated unwavering persistence in resuscitation efforts without easily relinquishing treatment in what appeared to be a seemingly hopeless situation. This steadfast determination ultimately led to successful recovery; and (3) Continued preservation of organ function after resuscitation is crucial, particularly for vital organs such as the heart, brain, lungs, and kidneys. It is imperative to target control blood pressure levels, oxygen saturation levels, carbon dioxide partial pressure as well as body temperature. Early initiation of enteral nutrition can prevent dysbiosis-induced secondary infections. Additionally, the timely application of hyperbaric oxygen therapy following CPR greatly improves cerebral recovery outcomes, leading to enhanced prognosis through reduced disability rates or mortality risks and minimized occurrence of vegetative states. As a result, it contributes to an overall enhancement in patients' quality of life.
CONCLUSION
For patients experiencing sudden cardiac and respiratory arrest secondary to electrical injuries, particularly those aged between young and middle-aged without significant organ dysfunction, the pursuit of rescuing should not be relinquished lightly. Extending the duration of CPR, implementing early brain protection measures, and employing active and comprehensive treatments can result not only in the establishment of a normal autonomous circulation but also in the full restoration of brain function.
Footnotes
Informed consent statement: Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare no competing interests.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 11, 2023
First decision: February 8, 2024
Article in press: March 28, 2024
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mallet RT, United States S-Editor: Zheng XM L-Editor: A P-Editor: Xu ZH
Contributor Information
Jian Zhang, Department of General Surgery, Shengli Oilfield Central Hospital, Dongying 257000, Shandong Province, China.
Yan-Ru Qiao, Department of General Surgery, Shengli Oilfield Central Hospital, Dongying 257000, Shandong Province, China.
Ya-Dong Yang, Department of Emergency Medicine, Shengli Oilfield Central Hospital, Dongying 257000, Shandong Province, China.
Guo-Zheng Pan, Department of General Surgery, Shengli Oilfield Central Hospital, Dongying 257000, Shandong Province, China.
Chong-Qing Lv, Department of General Surgery, Shengli Oilfield Central Hospital, Dongying 257000, Shandong Province, China. lvchongqing2006@163.com.
References
- 1.Fish R. Electric shock, Part II: Nature and mechanisms of injury. J Emerg Med. 1993;11:457–462. doi: 10.1016/0736-4679(93)90250-b. [DOI] [PubMed] [Google Scholar]
- 2.Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61. doi: 10.1186/s13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merchant RM, Topjian AA, Panchal AR, Cheng A, Aziz K, Berg KM, Lavonas EJ, Magid DJ Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S337–S357. doi: 10.1161/CIR.0000000000000918. [DOI] [PubMed] [Google Scholar]
- 4.Bai Z, Wang L, Yu B, Xing D, Su J, Qin H. The success rate of cardiopulmonary resuscitation and its correlated factors in patients with emergency prehospital cardiac arrest. Biotechnol Genet Eng Rev. 2023:1–10. doi: 10.1080/02648725.2023.2202516. [DOI] [PubMed] [Google Scholar]
- 5.Sladjana A, Gordana P, Ana S. Emergency response time after out-of-hospital cardiac arrest. Eur J Intern Med. 2011;22:386–393. doi: 10.1016/j.ejim.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Liu W, Liu LN, Lin CW, Wang HY, Wang XD. Successful Recovery After Prolonged Cardiopulmonary Resuscitation and Rescue Thrombolytics in a Patient with Cardiac Arrest Secondary to Presumed Massive Pulmonary Embolism. Risk Manag Healthc Policy. 2021;14:4253–4256. doi: 10.2147/RMHP.S317205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmitz J, Liebold F, Hinkelbein J, Nöhl S, Thal SC, Sellmann T. Cardiopulmonary resuscitation during hyperbaric oxygen therapy: a comprehensive review and recommendations for practice. Scand J Trauma Resusc Emerg Med. 2023;31:57. doi: 10.1186/s13049-023-01103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]