Evidence based medicine is founded upon an ideal—that decisions about the care of individual patients should involve the “conscientious, explicit and judicious use of current best evidence.”1 Several publications are dedicated to evidence based medicine, and, at an international level, the Cochrane Collaboration has been formed to gather, analyse, and disseminate evidence derived from published research.2 Several practical approaches to evidence based medicine in clinical decision making have also been described.3,4
Evidence based medicine, it is claimed, leads to improvements in clinicians’ knowledge, reading habits, and computer literacy; provides a framework for teaching; enables junior team members to contribute to decisions; and allows better communication with patients and more effective use of resources.5 From an ethical perspective, the strongest arguments in support of evidence based medicine are that it allows the best evaluated methods of health care (and useless or harmful methods) to be identified and enables patients and doctors to make better informed decisions.5,6
However, the presence of reliable evidence does not ensure that better decisions will be made. Claims that evidence based medicine offers an improved method of decision making are difficult to evaluate because current practice is so poorly defined. Medical decision making draws upon a broad spectrum of knowledge—including scientific evidence, personal experience, personal biases and values, economic and political considerations, and philosophical principles (such as concern for justice). It is not always clear how practitioners integrate these factors into a final decision, but it seems unlikely that medicine can ever be entirely free of value judgments.
Summary points
Evidence based medicine is based on a strong ethical and clinical ideal—that it allows the best evaluated methods of health care to be identified and enables patients and doctors to make better informed decisions
Evidence based medicine is unable to resolve competing claims of different interest groups
Collecting sufficient satisfactory evidence raises problems—randomised controlled trials are only possible where there is genuine “therapeutic equipoise”
Crude application of results of clinical trials to individual care may disadvantage some patients
Allocating resources on the basis of evidence involves implicit value judgments and could imply that lack of evidence means lack of value
We review ethical concerns associated with evidence based medicine—in particular that it invites a simplistic approach to the role of evidence in medicine, which can be misinterpreted and may not allow for the complexity of clinical decision making.
The philosophical basis
Evidence based medicine represents a practical example of consequentialism—the proposition that the worth of an action can be assessed by the measurement of its consequences. Criticisms of consequentialist philosophies may be considered under three main headings. Firstly, many important outcomes cannot be adequately measured or defined. Secondly, it is often unclear whose interests should be considered in determining outcomes. Thirdly, consequentialism may lead to conclusions that are thought to be unethical from other points of view. These criticisms may equally apply to evidence based medicine.
Immeasurable outcomes
The first philosophical criticism of evidence based medicine is that many important outcomes of treatment cannot be measured. This arises from the fact that evidence based medicine claims to provide a simple, logical process for reasoning and decision making—look at the evidence and decide accordingly. But to make balanced decisions, all the relevant consequences of an action must be considered. Unfortunately, current measures of some outcomes of medical treatment (such as pain) are inadequate; some (such as justice) may not be measurable; and other complex outcomes (such as quality of life) may not even be adequately definable.7,8 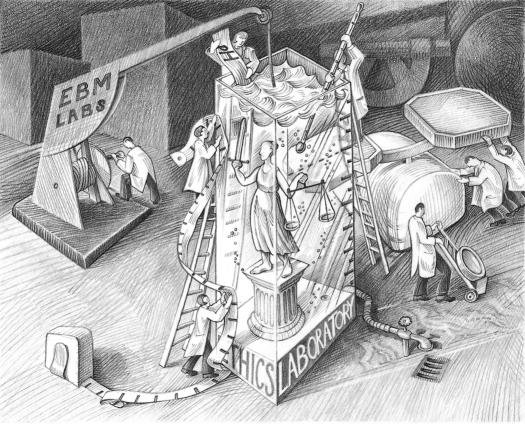
The philosopher Bernard Williams notes that values which may be easily quantified in economic terms often require comparison with values which are not quantifiable. “Again and again defenders of such values are faced with the dilemma of either refusing to quantify the value in question, in which case it disappears from the sum altogether, or else of trying to attach some quantity to it, in which case they misrepresent what they are about and also usually lose the argument, since the quantified value is not enough to tip the scale.”9 This is particularly the case in medicine, where intangible values such as justice or quality of life are frequently balanced against easily quantified values such as cost or mortality.
Deciding between competing claims
The second philosophical criticism, that it may be impossible to decide between competing claims of different stakeholders, is emphasised by the manner in which patients continue to have little influence over the priorities of research. Evidence based medicine claims to reject the power of expert opinion but it is still mostly doctors who determine research objectives, who interpret research data, and who implement research findings. A number of commentators have called for greater involvement by consumer groups in setting research agendas, but how conflicts between the agendas of the different stakeholders are to be resolved remains unclear.10,11 Evidence based medicine is unable to address political concerns because the values of different stakeholders, and hence the way in which they interpret evidence, cannot always be made congruent with each other.
At odds with common morality
The third philosophical criticism, that evidence based medicine may lead to activities that seem at odds with common morality, arises from the fact that evidence based medicine assesses interventions solely in terms of evidence of efficacy. An example of the difficulties that may arise from this approach occurs in the field of meta-analysis. Researchers performing meta-analyses are generally urged to search as widely as possible for data and to use unpublished studies if they are methodologically sound. However, valuable research findings may arise from unethically conducted research and data from unpublished studies may not meet the ethical safeguards that are demanded by publishers. In such cases it may be unclear whether results should be used or discarded.
Most of the discussion of this topic has focused on Nazi experimentation,12 but there are many more recent examples of unethical research.13 The New England Journal of Medicine has stated that it will not publish results of unethical research, regardless of scientific merit; but what these standards mean in practice is not entirely clear.13–15 For example, the Gruppo Italianao per lo Studio della Sopravivenza nell Infarto Micardio (GISSI-2) trial, published in the Lancet in 1990, did not require the informed consent of trial subjects.16 Although few present day ethics committees would accept this standard, this study has been widely quoted and included in many meta-analyses. Ethically it seems clear that both researchers and publishers should consider the ethical basis of studies that are included in meta-analysis, but the extent of this obligation remains uncertain.
Collecting evidence
Randomised controlled trials
Proponents of evidence based medicine emphasise the value of some forms of evidence over others, placing particular emphasis upon the results of randomised controlled trials.17 For example, the United States Preventive Services Taskforce rates the value of evidence from randomised controlled trials as “grade I,” evidence from non-randomised trials as “grade II,” and evidence from the opinions of respected authorities as “grade III.”18
Ethical concerns
Randomised controlled trials have the potential to prevent the propagation of worthless treatments and confirm the value of effective treatments. They raise a number of issues that cause ethical concern, including: the selection of subjects, consent, randomisation, the manner in which trials are stopped, and the continuing care of subjects once the trials are complete.
“Therapeutic equipoise”
The administration of randomised controlled trials requires doctors and patients to balance the requirements of several distinct roles—doctors may act simultaneously as physicians and research scientists, and patients as invalids and research subjects. It has been suggested that physicians’ moral responsibilities towards their patients are inconsistent with any recommendation that the patients should participate in randomised controlled trials because of this conflict of interest.19,20 However, it is held that doctors may recommend that their patients participate if they are in a state of “therapeutic equipoise”—that is, there is genuine doubt about the value of different interventions.21
Equipoise is not generally a problem in large clinical trials designed to investigate treatments with only moderate effect sizes. Indeed, a major value of randomised controlled trials is that they allow identification of moderate benefits that would otherwise be obscured by bias and random effects.22 However, equipoise may not be achievable when interventions have very great benefits, or major risks. These interventions need to be investigated in other ways, such as by reporting clinical observations or through the use of historical controls. Researcher’s choice of experimental protocols may therefore be limited by ethical concerns and the gathering of “grade I” or “grade II” evidence may be prohibited by ethical requirements.
Using evidence
Individual care and resource allocation
Clinical trials seem the best basis for clinical decision making. However, compared with other topics in evidence based medicine, the techniques for accurate application of trial results have received scant attention. There is a widely held view that the correct approach is through a comparison of the trial subjects and the population to which the results are to be applied.23 This is not necessarily so, as the overall results of a trial represent an average effect, and even within the trial population some will experience a greater than average improvement in outcomes, while others may suffer harm.24,25 Consequently, although crude applications of trial results may on average do more good than harm, they may none the less disadvantage some patients.
Systematic bias
Governments and health funds find the notion of allocating health resources on the basis of evidence attractive.26 Eddy has suggested that healthcare funds should be required to cover interventions only if there is sufficient evidence that they can be expected to produce their intended effects.27 The Australian health minister, Dr Michael Wooldridge, who is a strong supporter of evidence based medicine, has adopted a similar position, stating “[we will] pay only for those operations, drugs and treatments that according to available evidence are proved to work.”26
Given the complexities of the issues surrounding resource allocation, the drive to seek certainty and simplicity at the policy level is understandable. However, the large quantities of trial data required to meet the standards of evidence based medicine are available for relatively few interventions. Evidence based medicine may therefore introduce a systematic bias, resulting in allocation of resources to those treatments for which there is rigorous evidence of effectiveness, or towards those for which there are funds available to show effectiveness (such as new pharmaceutical agents). This may be at the expense of other areas where rigorous evidence does not currently exist or is not attainable (such as palliative care services). Allocating resources on the basis of evidence may therefore involve implicit value judgments, and it may only be a short step from the notion that a therapy is “without substantial evidence” to it being thought to be “without substantial value.”8
Individual versus population health
Evidence based medicine, as described above, concentrates upon the efficacy of individual treatments. Physicians must not only address the needs of individual patients, but should also be concerned with issues of efficiency and population health.28 Proponents of evidence based medicine argue that these issues can be resolved by the use of “evidence based purchasing.” However, decisions reached rationally at the population level will at times conflict with those made in the interests of the individual. Evidence based medicine does not provide a means to settle such conflicts. Even attempts to replace evidence based medicine with other quantitative methods such as “decision-analysis based medical decision-making” seem unlikely to remove from medicine the need for reasoning that is based on value.29
Simplistic solutions
According to Williams, “there is great pressure for research into techniques to make larger ranges of social value commensurable. Some of the effort should rather be devoted to learning—or learning again—how to think intelligently about conflicts of values which are incommensurable.”9 This is particularly the case where it comes to making decisions about allocation of health resources. Those charged with making these decisions are seeking simplistic solutions to inherently complex problems—the danger is that through evidence based medicine we will supply them.
Footnotes
Funding: No additional funding.
Conflict of interest: None.
References
- 1.Sackett DL, Rosenberg WMC, Gray JAM, Harnes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chalmers I, Dickersin K, Chalmers TC. Getting to grips with Archie Cochrane’s agenda. BMJ. 1992;305:786–788. doi: 10.1136/bmj.305.6857.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem-solving. BMJ. 1995;312:1122–1126. doi: 10.1136/bmj.310.6987.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henry D. Economic analysis as an aid to subsidisation decisions. The development of Australian guidelines for pharmaceuticals. PharmacoEconomics. 1992;1:54–67. doi: 10.2165/00019053-199201010-00010. [DOI] [PubMed] [Google Scholar]
- 5.Bastian H. The power of sharing knowledge. Consumer participation in the Cochrane Collaboration. Oxford: UK Cochrane Centre; 1994. [Google Scholar]
- 6.Hope T. Evidence-based medicine and ethics. J Med Ethics. 1995;21:259–260. doi: 10.1136/jme.21.5.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyatt GH, Sackett DL Cook DJ for the Evidence-Based Medicine Working Group. Users’ guides to the medical literatures. JAMA. 1994;271:59–63. doi: 10.1001/jama.271.1.59. [DOI] [PubMed] [Google Scholar]
- 8.Evidence-Based Care Resource Group. Evidence-based care. 1. Setting priorities: how important is this problem? Can Med Assoc J. 1994;150:1249–1254. [PMC free article] [PubMed] [Google Scholar]
- 9.Williams B. Morality. Cambridge: Cambridge University Press; 1972. [Google Scholar]
- 10.Chalmers I. What do I want from health researchers when I am a patient? BMJ. 1995;310:1315–1318. doi: 10.1136/bmj.310.6990.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliver SR. How can health service users contribute to the NHS R and D program? BMJ. 1995;310:1318–1320. doi: 10.1136/bmj.310.6990.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berger RL. Nazi science—the Dachau hypothermia experiments. N Engl J Med. 1990;322:1435–1440. doi: 10.1056/NEJM199005173222006. [DOI] [PubMed] [Google Scholar]
- 13.Samei E, Kearfott KJ. A limited bibliography of the federal government-funded human radiation experiments. Health Physics. 1995;69:885–891. doi: 10.1097/00004032-199512000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Angel M. The Nazi hypothermia experiments and unethical research today. N Engl J Med. 1990;322:1462–1464. doi: 10.1056/NEJM199005173222011. [DOI] [PubMed] [Google Scholar]
- 15.Smith R. Informed consent: the intricacies. BMJ. 1997;314:1059–1060. doi: 10.1136/bmj.314.7087.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gruppo Ialiano per lo Studio della Sopravvivenza nell Infarto Miocardio. GISSI-2: a factorial randomised trial of alteplase versus streptokinase and heparin versus no heparin among 12,490 patients with acute myocardial infarction. Lancet. 1990;336:65–71. [PubMed] [Google Scholar]
- 17.Mulrow CD. Rationale for systematic reviews. BMJ. 1994;309:597–599. doi: 10.1136/bmj.309.6954.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Preventive Services Taskforce. Guide to clinical preventive services. 2nd ed. Baltimore: Williams and Wilkins; 1995. p. 862. [Google Scholar]
- 19.Hellman S, Hellman DS. Of mice but not men. Problems of the randomised clinical trial. N Engl J Med. 1991;324:1585–1589. doi: 10.1056/NEJM199105303242208. [DOI] [PubMed] [Google Scholar]
- 20.Howson C, Urbach P. Scientific reasoning—a Bayesian approach. 2nd ed. Chicago: Open Court; 1993. [Google Scholar]
- 21.Shimm DS, Spece RG. Ethical issues and clinical trials. Drugs. 1993;46:579–584. doi: 10.2165/00003495-199346040-00001. [DOI] [PubMed] [Google Scholar]
- 22.Yusof S, Collins R, Peto R. Why do we need some large, simple randomised trials? Stat Med. 1984;3:409–420. doi: 10.1002/sim.4780030421. [DOI] [PubMed] [Google Scholar]
- 23.Walsh JT, Gray D, Keating NA, Cowley AJ, Hampton JR. ACE for whom? Implications for clinical practice of post-infarct trials. Br Heart J. 1995;73:470–474. doi: 10.1136/hrt.73.5.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hlakty MA, Califf RM, Harrell FE, Jr, Lee KL, Mark DB, Muhlbaier LH, et al. Clinical judgement and therapeutic decision making. J Am Coll Cardiol. 1990;15:1–14. doi: 10.1016/0735-1097(90)90167-n. [DOI] [PubMed] [Google Scholar]
- 25.Glasziou PP, Irwig LM. An evidence based approach to individualising treatment. BMJ. 1995;311:1356–1359. doi: 10.1136/bmj.311.7016.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Downey M. Trust me I’m a doctor. Sydney Morning Herald. 10 May 1997:1.
- 27.Eddy DK. Benefit language; criteria that will improve quality while reducing costs. JAMA. 1996;275:650–657. doi: 10.1001/jama.275.8.650. [DOI] [PubMed] [Google Scholar]
- 28.Maynard A. Evidence-based medicine: an incomplete method for informing treatment choices. Lancet. 1997;349:126–128. doi: 10.1016/S0140-6736(96)05153-7. [DOI] [PubMed] [Google Scholar]
- 29.Dowie J. “Evidence-based”, “cost-effective”, and “preference-driven” medicine: decision analysis based medical decision making is the pre-requisite. J Health Serv Res Policy. 1996;1:104–113. doi: 10.1177/135581969600100208. [DOI] [PubMed] [Google Scholar]


