Abstract
Introduction
An infected popliteal pseudoaneurysm has never been described in the pediatric population. Physicians need to be aware of its presentation and management, in order to diagnose and treat this medical condition adequately.
Methods
We describe the case of a 14-year-old boy who developed myositis and cellulitis centered at the popliteal fossa after playing basketball. A treatment of intravenous cefazolin was started. 5 days later, he experienced a knee pain flare-up, which turned out to be a popliteal pyomyositis with a pseudoaneurysm of the popliteal artery. A saphenous vein graft bypass of the popliteal artery and an excision of the popliteal pseudoaneurysm were performed. Intravenous cefazolin was continued for 6 weeks and prophylactic acetylsalicylic acid for 6 months.
Results and conclusion
This case highlighted the importance of repeating radiologic investigations if a patient suffering from soft tissue infection has persistent pain after several days of appropriate antibiotics. A popliteal pseudoaneurysm can be diagnosed with ultrasound imaging and treated with a popliteal-popliteal bypass. Our patient needed a catheter-guided dilation of the anastomosis at the vein graft 6 months post-surgery, and then evolved favorably and went back to playing basketball 6 months post-dilation.
Keywords: Pseudoaneurysm, popliteal, infected, bypass, graft, angioplasty
A 14-year-old boy with no particular medical history presented with acute knee pain, inability to bear weight, chills, sweat, and decreased appetite, but no documented fever. He played basketball right before the onset of symptoms, but could not recall any major trauma.
Clinical findings
On arrival at our center, the patient had an erythematous, edematous, hot and painful right distal posterior thigh and knee. He was still afebrile. The pulmonary exam was normal, but a heart murmur was heard. He did not have any skin lesions. The blood test showed a white blood cell (WBC) count of 6000 cells/mL, a C-reactive protein (CRP) of 81.4 mg/L and creatine kinase at 265 UI/L (normal range being 30–150 UI/L for males of 11–14 years old). The two initial blood cultures were positive for multi-sensible Staphylococcus aureus, and the culture of the right knee joint aspiration (done before initiating antibiotics) came back negative. Intravenous Cefazolin was initiated to treat what seemed to be a soft tissue infection. A magnetic resonance imaging (MRI) revealed myositis and cellulitis centered at the popliteal fossa, but no signs of osteomyelitis, nor any collection or abscess. A heart ultrasound ruled out endocarditis.
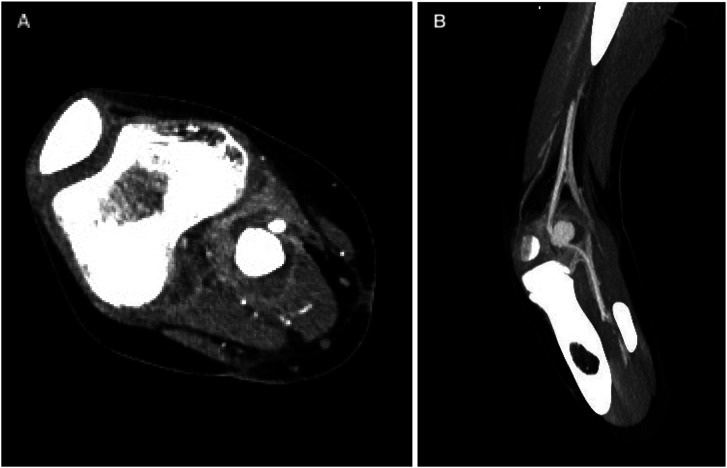
Initially, a good clinical and biological response to intravenous Cefazolin was observed, with an absence of fever, a decreased soft tissue swollenness and pain, as well as a lower CRP (14 mg/L) and CK (62 UI/L). Five days following the admission, an ultrasound of the right knee was ordered because of a knee pain flare-up, particularly in the popliteal fossa. It revealed a popliteal pyomyositis with a pseudoaneurysm of the popliteal artery, which was partially thrombosed. Then, a computed-tomography (CT) angiography of the right leg identified a pyomyositis and an aneurysm of the popliteal artery surrounded by an abscessed cavity in the proximal medial gastrocnemius (Figure 1). Transient synovitis of the knee was also suspected because of synovial knee enhancement, but no sign of osteomyelitis was found.
Figure 1.
(a) Transverse and (b) sagittal computed-tomography angiography images of the right knee showing a pyomyositis and a popliteal artery pseudoaneurysm of 2.2 × 2 × 1.6 cm surrounded by an abscessed cavity of 3.7 × 3.4 × 2.9 cm in the proximal medial gastrocnemius.
Therapeutic intervention
The patient was brought to the operating room to perform a saphenous vein graft bypass of the popliteal artery and an excision of the diseased artery and pseudoaneurysm.
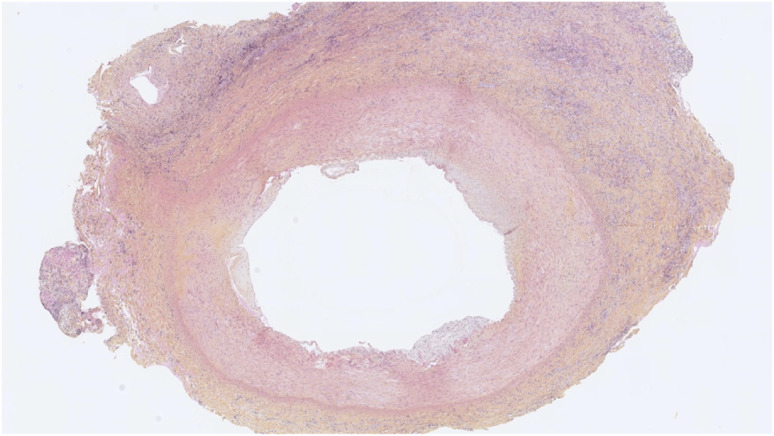
The perioperative cultures (popliteal cavity and popliteal artery) were both positive for multi-sensible Staphylococcus aureus. The strains were negative for Panton-Valentine leucocidin toxins. The resected popliteal artery was consistent with an infectious vasculitis with a zone of fibrinoid necrosis, loss of the vascular wall and a pseudoaneurysm secondarily associated (Figure 2).
Figure 2.
Histological image with hematoxylin-eosin saffron staining showing an inflamed popliteal artery surrounded with fibrinoid necrosis and pseudoaneurysm.
Follow-up and outcomes
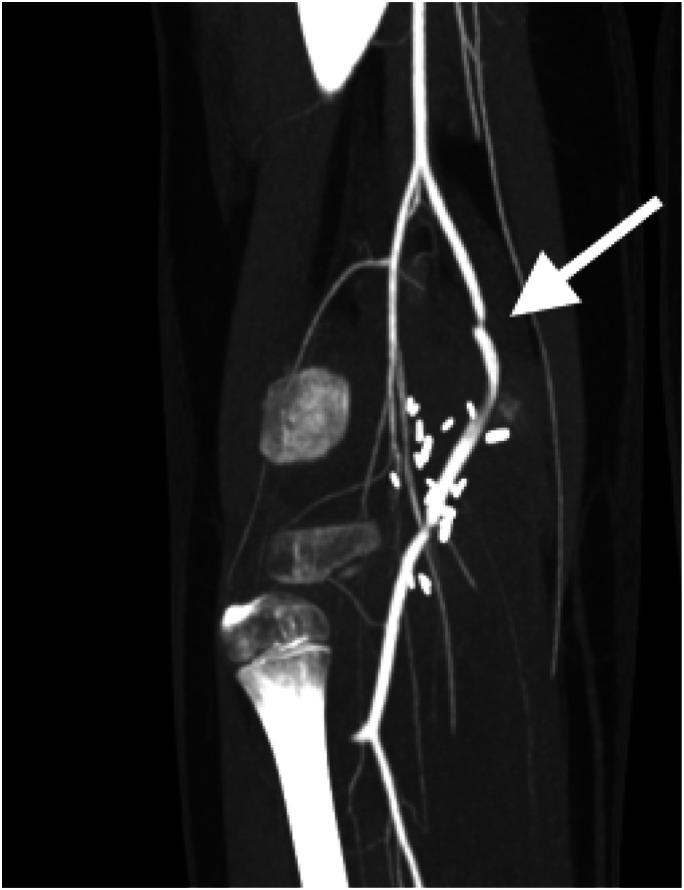
A CT angiography on postoperative day 5 showed complete disappearance of the abscess, a slight inflammatory reaction and a permeable bypass (Figure 3). The patient was discharged on postoperative day 10 with intravenous Cefazolin administered with a peripherally inserted central catheter (PICC line) for 6 weeks, and prophylactic acetylsalicylic acid for 6 months.
Figure 3.
Computed-tomography angiography image at 5 days postoperatively showing permeability of the popliteal artery bypass.
Antibiotics were discontinued 6 weeks after surgery since the patient had no clinical signs of infection anymore. The CRP was within the normal range (0.5 mg/L). A controlled CT angiography confirmed the bypass was still permeable, but there was focal anastomotic stenosis of 60% of the vessel caliber (Figure 4). No pseudoaneurysm nor any collection were visible, but there was a residual inflammatory reaction at the popliteal fossa. The graft partial stenosis was still present on the following Doppler ultrasound done at 9 weeks post-surgery, respectively.
Figure 4.
Computed-tomography angiography image at 6 weeks postoperatively showing the 60% focal stenosis (arrow) of the graft.
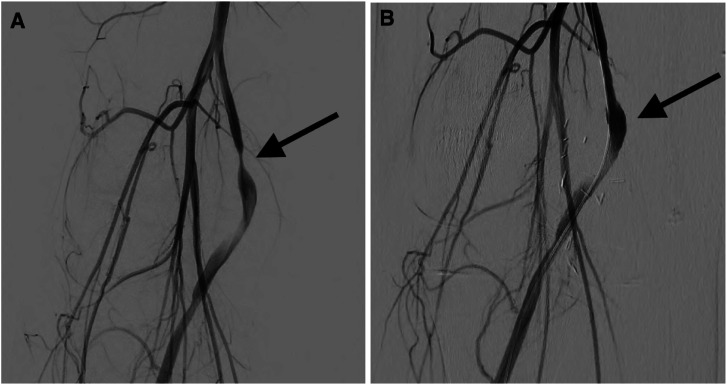
Six months after surgery, the anastomotic stenosis was still present, and the patient had intermittent claudication and limb weakness (Figure 5(a)). A catheter-guided dilation of the anastomosis was successfully performed (Figure 5(b)), and then, 3 months post-dilation, the patient was asymptomatic and had no sign of abnormal blood flow on subsequent ultrasound. At 6 months post-dilation (1-year post-popliteal artery bypass), the patient started playing basketball again and was pain-free.
Figure 5.
Angiogram images at 6 months postoperatively showing (a) the pre-angioplasty focal stenosis of the graft (arrow) and (b) the catheter-guided balloon angioplasty (arrow).
Discussion
In the pediatric population, vascular aneurysms are rare entities, even more so for infected aneurysms, which account for 15% of all pediatric aneurysms. 1 To our knowledge, this is the first pediatric case of an infected popliteal artery pseudoaneurysm reported in the literature. This condition is often referred to as mycotic pseudoaneurysm, but it is a misnomer considering that the pathogen is more often bacterial than fungal. 2 A pseudoaneurysm is caused by an arterial wall injury such as an infection, which can thicken that vessel wall. 3
Four pathophysiological mechanisms of infected pseudoaneurysms have been described: bacteremia seeding a pre-existing arterial wall injury, septic thromboembolism from endocarditis, direct bacterial inoculation during an arterial trauma, and bacterial propagation from an adjacent infected tissue. 4
In our case, the bacterial propagation from the adjacent infected structures seems more likely as the patient had pyomyositis right next to the popliteal artery, in the proximal medial head of the gastrocnemius. The histopathologic examination confirmed that there was a destruction of the blood vessel high likely due to the bacteria propagation. Also, the knee MRI completed at arrival (before the bacterial propagation) did not show any abnormalities of the popliteal artery, suggesting that there was no aneurysm initially.
Even if the blood cultures were initially positive, it would be unlikely that a bacteremic seeding is the cause of our patient’s infected aneurysm, since it takes an arterial injury to the blood vessel to be at risk of infection. Indeed, this teenager did not have any sign of blunt or penetrating trauma when examined at arrival, and he did not have risk factors of aneurysms and atherosclerosis, such as smoking, hypertension, and family history of aneurysms, as usually found among adults with infected popliteal pseudoaneurysm.4,5
A septic embolism is not likely to be the cause of our patient’s aneurysm either. First, he had no clinical signs of pulmonary or skin emboli or any neurological complaints. Second, a heart ultrasound performed shortly after his arrival ruled out endocarditis, which could have been the origin of an infected embolism. 3
The pain relapse in the popliteal area, despite appropriate antimicrobial therapy, was a signal of an unexpected complication. Most often, in this context, an infectious complication such as an abscess, a collection, a phlegmon, or less frequently, a thrombosis, necrosis or myofasciitis can be found. In our case, the finding of an infected pseudoaneurysm originating from an adjacent focus of infection was unexpected.
There are currently no guidelines for the treatment of pediatric infected pseudoaneurysms. Our patient was treated as an endovasculitis, with a 6-week intravenous antibiotic course that started from the moment the pseudoaneurysm was resected. A long course of antibiotics was needed following the bypass surgery considering the procedure was performed on an active infection site. There are no guidelines either on the use of anticoagulation or antiplatelet therapy following lower-extremity bypass surgery in the pediatric population. The use of acetylsalicylic acid for 6 months was based on experts’ opinions.
Five cases of children affected by infected pseudoaneurysms have been reported, but none from the popliteal artery. One case was a vertebral artery-infected pseudoaneurysm preceded by a lower tract respiratory infection. 1 That patient was also diagnosed with a chronic granulomatous disease, which could have caused vascular dilatation and bacteremic seeding according to the authors. That pseudoaneurysm was treated with endovascular coiling, considering the high risk of performing a surgical treatment in that anatomic location.
Furthermore, a case series described four post-liver transplantation hepatic artery fungal pseudoaneurysms in immunosuppressed children, 2 which were also caused by a bacteremic seeding into an abnormal vessel wall at the anastomosis site. They were treated with surgical reintervention on the hepatic artery and antifungal therapy.
In the adult population, two case reports have described infected pseudoaneurysms of the popliteal artery.4,5 The case presented by Nakagawa et al. 4 had cellulitis and a pre-existing popliteal aneurysm, and the one by Killeen et al. 5 had endocarditis with septic thromboembolism from vegetation that infected the previously normal popliteal artery according to the authors. These two cases were both treated successfully with surgical excision of the pseudoaneurysm and a below-knee bypass using a saphenous vein graft, followed by a 6-week antibiotic treatment. None of them had recurrent infections at follow-ups.
The long-term prognosis of arterial graft at the popliteal fossa in the context of an infected pseudoaneurysm is unknown. None of the two authors above described the permeability of the popliteal bypass in the months following the popliteal infected pseudoaneurysm surgical treatment. In our case, anastomotic stenosis occurred 3 months post-surgery and responded well to endovascular dilation. Those procedures allowed the patient to go back to playing basketball a year after the bypass surgery without ischemic symptoms.
Conclusion
To our knowledge, this is the first case of a pediatric infected pseudoaneurysm of the popliteal artery, which is a rare complication of soft tissue infection. This case highlighted the importance to repeat radiologic investigations if a child suffering from deep soft tissue infection has persistent pain after several days of appropriate antibiotics and the importance of serial post-revascularisation CT angiography and Doppler ultrasound to assess the vessel graft permeability and prevent complete thrombosis.
As for adults, children with an infected popliteal artery pseudoaneurysm seem to respond well to a pseudoaneurysm resection and revascularisation surgery, associated with a 6-week course of intravenous antibiotics.
Acknowledgements
The research team wants to thank Dr Victor Kokta for providing the histological image.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent for publication: Informed consent was obtained from the legally authorized representatives and assent was obtained from minor child whose images and case are included in this publication.
ORCID iD
Alexandre Lavigne https://orcid.org/0000-0003-4668-4543
References
- 1.Nadarajah J, Sebastian L, Jain N, et al. Endovascular management of a rare case of pediatric vertebral artery mycotic aneurysm: a case report. Pediatr Neurosurg 2018; 53(5): 346–350. [DOI] [PubMed] [Google Scholar]
- 2.Camagni S, Stroppa P, Tebaldi A, et al. Mycotic aneurysm of the hepatic artery in pediatric liver transplantation: A case series and literature review. Transpl Infect Dis 2018; 20(3): e12861. [DOI] [PubMed] [Google Scholar]
- 3.Krings T, Geibprasert S, terBrugge KG. Pathomechanisms and treatment of pediatric aneurysms. Childs Nerv Syst 2010; 26(10): 1309–1318. [DOI] [PubMed] [Google Scholar]
- 4.Nakagawa T, Shibuya T, Oono M, et al. An infected popliteal aneurysm simultaneously treated with resection and revascularization. Ann Vasc Dis 2019; 12(4): 541–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Killeen SD, O'Brien N, O'Sullivan MJ, et al. Mycotic aneurysm of the popliteal artery secondary to Streptococus pneumoniae: a case report and review of the literature. J Med Case Rep 2009; 3: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]