Abstract
Background
Since the mid‐1970s, short‐term psychodynamic psychotherapies (STPP) for a broad range of psychological and somatic disorders have been developed and studied. Early published meta‐analyses of STPP, using different methods and samples, have yielded conflicting results, although some meta‐analyses have consistently supported an empirical basis for STPP. This is an update of a review that was last updated in 2006.
Objectives
To evaluate the efficacy of STPP for adults with common mental disorders compared with wait‐list controls, treatments as usual and minimal contact controls in randomised controlled trials (RCTs). To specify the differential effects of STPP for people with different disorders (e.g. depressive disorders, anxiety disorders, somatoform disorders, mixed disorders and personality disorder) and treatment characteristics (e.g. manualised versus non‐manualised therapies).
Search methods
The Cochrane Depression, Anxiety and Neurosis Group's Specialised Register (CCDANCTR) was searched to February 2014, this register includes relevant randomised controlled trials from The Cochrane Library (all years), EMBASE (1974‐), MEDLINE (1950‐) and PsycINFO (1967‐). We also conducted searches on CENTRAL, MEDLINE, EMBASE, CINAHL, PsycINFO, DARE and Biological Abstracts (all years to July 2012) and all relevant studies (identified to 2012) were fully incorporated in this review update. We checked references from papers retrieved. We contacted a large group of psychodynamic researchers in an attempt to find new studies.
Selection criteria
We included all RCTs of adults with common mental disorders, in which a brief psychodynamic therapy lasting 40 or fewer hours in total was provided in individual format.
Data collection and analysis
Eight review authors working in pairs evaluated studies. We selected studies only if pairs of review authors agreed that the studies met inclusion criteria. We consulted a third review author if two review authors could not reach consensus. Two review authors collected data and entered it into Review Manager software. Two review authors assessed and scored risk of bias. We assessed publication bias using a funnel plot. Two review authors conducted and reviewed subgroup analyses.
Main results
We included 33 studies of STPP involving 2173 randomised participants with common mental disorders. Studies were of diverse conditions in which problems with emotional regulation were purported to play a causative role albeit through a range of symptom presentations. These studies evaluated STPP for this review's primary outcomes (general, somatic, anxiety and depressive symptom reduction), as well as interpersonal problems and social adjustment. Except for somatic measures in the short‐term, all outcome categories suggested significantly greater improvement in the treatment versus the control groups in the short‐term and medium‐term. Effect sizes increased in long‐term follow‐up, but some of these effects did not reach statistical significance. A relatively small number of studies (N < 20) contributed data for the outcome categories. There was also significant heterogeneity between studies in most categories, possibly due to observed differences between manualised versus non‐manualised treatments, short versus longer treatments, studies with observer‐rated versus self report outcomes, and studies employing different treatment models.
Authors' conclusions
There has been further study of STPP and it continues to show promise, with modest to large gains for a wide variety of people. However, given the limited data, loss of significance in some measures at long‐term follow‐up and heterogeneity between studies, these findings should be interpreted with caution. Furthermore, variability in treatment delivery and treatment quality may limit the reliability of estimates of effect for STPP. Larger studies of higher quality and with specific diagnoses are warranted.
Keywords: Adult; Humans; Mental Disorders; Mental Disorders/therapy; Psychotherapy, Brief; Psychotherapy, Brief/methods; Psychotherapy, Psychodynamic; Psychotherapy, Psychodynamic/methods; Randomized Controlled Trials as Topic; Somatoform Disorders; Somatoform Disorders/therapy
Plain language summary
Short‐term psychodynamic psychotherapies for common mental disorders
Background
Common mental disorders include anxiety disorders, depressive disorders, stress‐related physical conditions, certain behaviour disorders and personality disorders. People with these disorders tend to have problems handling difficult emotions and often respond with physical and psychic symptoms or avoidant behavioural patterns. Such patterns and emotional responses are theoretically treatable by short‐term psychodynamic psychotherapies (STPP) because these therapies aim to improve long‐ and short‐term problems with emotion processing, behaviour and communication/relationships with others. STPP is thought to work by making people aware of emotions, thoughts and problems with communication/relationships that are related to past and recent trauma. This in turn helps to correct problems with emotions and relationships with others.
This review sought to find out whether STPP is more effective than wait‐list control (where people receive therapy after a delay during which people in the 'active' group receive the therapy), treatment as usual and minimal treatment (partial treatments not expected to provide a robust effect).
Study characteristics
We searched scientific databases to find all published and unpublished studies of STPP compared with wait‐list control, treatment as usual or minimal treatment up to July 2012. We searched for studies in adults over 17 years of age with common mental disorders being treated in an outpatient setting. We excluded people with psychotic disorders.
Key results
We included 33 studies involving 2173 people. When the results of the studies were combined and analysed, we found that there was a significantly greater improvement in the groups of people who received STPP versus the control groups, both in the short‐term (less than three months after treatment) and medium‐term (three to six months after treatment). These benefits generally appeared to increase in the long‐term. However, some results did not remain statistically significant in the long‐term and, in addition, the studies varied in terms of their design, meaning that these conclusions are tentative and need confirmation with further research. The finding that a short‐term psychological therapy treatment may be broadly applicable and effective is of importance in the atmosphere of current global healthcare and economic restrictions.
Quality of the evidence
The studies were of variable quality.
Background
Description of the condition
Common mental disorders (CMD) are the range of non‐psychotic symptom and behaviour disorders frequently seen in primary care and psychiatry services. They include depressive disorders, anxiety disorders, somatoform disorders and other conditions often mixed with interpersonal or personality disorders. These are extremely common conditions, with 12‐month prevalences of 6.9% for depression, 14.0% for anxiety disorders and 6.3% for somatoform disorders in one European review (Wittchen 2011). Collectively, they produce great expense to society and personal suffering for those people afflicted (Lazar 2010). Treatment guidelines for these conditions commonly cite the use of psychological therapy alongside medication as front‐line treatment options. Psychotherapies have established effectiveness in some of these conditions. Medications such as antidepressants are frequently used and, although there is some controversy about the magnitude of their effectiveness in real world samples, these appear to be marginally superior to (non‐active) placebo controls in short‐term randomised controlled trials (RCTs) for many of these conditions.
People with such a broad range of CMDs present to physicians, hospitals and mental health services. Common treatment options in these settings include psychotherapy (e.g. psychodynamic psychotherapy, cognitive behavioural therapies), medications and, in certain situations such as severe depression, procedures such as electroconvulsive therapy.
Description of the intervention
Short‐term psychodynamic psychotherapy (STPP) has been developed since the mid‐1970s by a number of proponents including James Mann (Mann 1973), David Malan (Malan 1979), Habib Davanloo (Davanloo 2000), Peter Sifneos (Sifneos 1972), Hans Strupp and Jeffrey Binder (Strupp 1984), and Lester Luborsky (Luborsky 1984), as brief alternatives to the prior long‐term psychodynamic therapy models. These treatments are brief talking therapies developed to work with unconscious impulses, feelings and processes that can underpin or perpetuate CMDs. Such unconscious impulses, feelings and processes often relate to losses or traumatising events in the past. Such adverse events are known risk factors for self destructive behaviours, multiple CMDs and multiple somatic disorders (Felitti 1998). Thus, psychodynamic psychotherapy, with its focus on resolving old trauma and its damaging effects on relationships, is used to treat multiple conditions including CMD (Leichsenring 2014; Shedler 2010).
Psychodynamic psychotherapy has common factors outlined by Blagys and Hilsenroth including: focus on affect and expression of emotion, exploration of attempts to avoid distressing thoughts and feelings, identification of recurring themes and patterns, discussion of past experience, focus on interpersonal relations, focus on the therapy relationship and exploration of wishes and fantasies (Blagys 2000). These features can reliably distinguish psychodynamic therapy from other models such as cognitive therapy (Blagys 2000).
In addition to these factors, elements that distinguish STPP from long‐term psychodynamic treatments include the use of selection criteria, time restriction, selection of and adherence to a therapeutic focus, efforts to prevent regression, high degrees of therapist activity and active focus on the transference (therapeutic) relationship as a template to learn about and activate emotional‐relational processes. Some models use a strict time limited format (e.g. Mann 1973), while others do not (Davanloo 2000), but the within‐study mean number of sessions is typically 12 to 24 with a range of four to 40 weekly sessions. The sessions are face‐to‐face and generally 45 to 60 minutes weekly. Many STPP methods use the triangle of conflict (the link between feelings, anxiety and defence) and the triangle of person (the link between past, therapist and current people) as key linkages to examine in the therapeutic process (Davanloo 1980;Malan 1979).
STPP treatment efforts include interventions falling along a continuum between 'supportive' (such as reassurance and encouragement) and 'expressive' elements (such as challenge to defences and elicitation of emotions) (Luborsky 1984). They may also be more or less focused on emotional mobilisation and experiencing versus insight into processes. Some models include a process to build anxiety tolerance through graded exposure to unconscious anxiety, feelings and impulses (Davanloo 2000). Hence, models of STPP can be used with people who may otherwise be unable to tolerate an emotion‐focused treatment. This includes people with active major depression or somatisation and people who use projective defences and dissociation. Hence, these models (e.g. Davanloo 2000; Luborsky 1984; McCullough 2003) can be used with a broad range of people with personality disorder including borderline personality disorder (Town 2011), and a range of depressive (Abbass 2010; Driessen 2010), and somatic disorders (Abbass 2009).
In the early phase of STPP development, case‐based research showed that a range of people could be successfully treated by these brief therapies, and that the gains were maintained at follow‐up (Davanloo 1980; Malan 1979; Mann 1973; Sifneos 1972). Since the 1980s, other STPP models have, and continue to be, developed. Some are more focused on various aspects of these above‐noted common processes. For example, one well‐studied model, psychodynamic interpersonal therapy (PIT), which was developed based on the Hobson model (Hobson 1985), emphasises interpersonal problems and the use of the therapy relationship as a means of understanding and changing these problematic patterns. A second model, intensive short‐term dynamic psychotherapy, is an emotion‐focused model developed by Davanloo (Davanloo 2000) and Malan (Malan 1986) with the expressed purpose of treating complex and resistant populations. Twenty‐one studies of this model were reviewed revealing large within‐ and between‐group (cases versus controls) effects across a broad range of populations (Abbass 2012) and specifically for personality and somatic disorders (Town 2013). Luborsky's technique (Luborsky 1984), supportive‐expressive therapy, operationalises and focuses on conflict through the examination of core conflictual relationship themes. Affect phobia therapy (McCullough 2003), influenced by Davanloo's model, focuses on exposure to feared affect warded off by defence mechanisms that are associated with symptoms and personality disorder (Svartberg 2004). Milrod and colleagues have developed and studied panic‐focused psychodynamic psychotherapy (Milrod 2007), and Monsen 2000 developed psychodynamic body therapy. Other new STPP models include dynamic interpersonal therapy (Lemma 2010), a time‐limited treatment for anxiety and depression.
How the intervention might work
STPP is a form of psychodynamic therapy and, thus, its mechanisms of action parallel that of psychodynamic therapy overall (Blagys 2000; Shedler 2010). These mechanisms include facilitation of a therapeutic alliance, building emotional capacities, building self awareness, emotional work to heal past wounds and an interpersonally corrective experience.
In terms of key processes, STPP is purported to work by engaging the person to recognise and relinquish intrapsychic and interpersonal patterns that interrupt the processing and working through of anxiety‐laden past and current experiences. The therapy relationship is used as vehicle to promote change. It is seen to provide both a window to access unprocessed emotions related to past relationships, and as an in vivo interpersonal context in which to learn how to respond adaptively to these unprocessed emotions (Shedler 2010). Helping a person see the connections between past/current and therapeutic relationships plus feelings/impulses/anxiety and defences brings insight on how emotions activate unconscious reactions and how the past and present are intertwined in the unconscious mind. Healing may take place through the emergence of new understanding about the impact of these often previously implicit processes associated with emotional trauma. The extent to which this involves emotional as well as intellectual neural structures may point to the nature and relative degree of therapeutic change (Diener 2007; Ulvenes 2012). Long‐lasting and sustained improvement in quality of life and interpersonal relationships, as well as symptom reduction, are presumed to be associated with the healthy adaptation of previously negative internal representations of the self and other. Common results from this work include improved awareness of emotions, awareness of and changes in interpersonal patterns, and improved capacity to tolerate both interactions and emotions. So overall, combinations of building insight, interpersonal corrective experiences with the therapist and emotional processing appear key treatment factors.
The STPP therapist uses a range of interventions to facilitate the therapeutic alliance. In STPP, the therapeutic alliance is mobilised through, in addition to other elements, efforts to help the person face difficult emotions, clarification of observed repeated defensive patterns and challenge to emotional avoidance in the therapeutic relationship (Davanloo 1980; Luborsky 1984). These efforts activate conscious and unconscious drives in the person to be aware of and address hitherto avoided emotions: these healing forces are what comprise the therapeutic alliance contributions of the person. Recapitulation and interpretation of what is discovered is employed to help cement learning and foster a stronger therapeutic alliance (Davanloo 2000; Messer 1995). This alliance appears to be a strong contributor to outcomes across many forms of psychotherapy.
Some STPP models are more supportive than confrontative of defences. Some are more reliant on developing insight into repeated patterns (Luborsky 1984), while others rely more on defence handling and emotional mobilisation (e.g. Davanloo 2000; McCullough 2003). Most models and therapists are likely to use combinations of supportive/confrontative techniques and interpretation/emotion mobilisation in line with patient in‐session response and presentation (Luborsky 1984; Messer 1995).
As noted, the treatment course is relatively brief averaging 12 to 24 sessions, although some treatment courses will extend up to 40 sessions when working with people with more severe emotional dysregulation, limited anxiety tolerance and depression. Working through of emotions and conflict takes place over a series of sessions followed by a phase of termination. At termination, emotions related to past losses are generally activated and worked through (Mann 1973; Messer 1995).
STPP may be provided in combination with medication such as antidepressants, especially where first‐line psychotherapy or medication alone were not adequately effective (Malhi 2009). Some reviews have suggested that combination treatments are more effective than either medication or psychotherapy alone, for example in the treatment of chronic depression (Malhi 2009).
Why it is important to do this review
When we published this original review (Abbass 2006), we estimated that there were over 50 studies of STPP published in the English language literature and that the mix of results from early meta‐analyses made a call for a formal review of this evidence base using Cochrane methodology. Since then, many more studies have been published along with a series of meta‐analyses (e.g. Abbass 2009; Abbass 2010; Abbass 2011; Driessen 2010; Town 2011; Town 2012). Conservatively, there are now over 100 published trials of STPP reviewed in over 12 meta‐analyses. These individual studies are of a broad range of psychological and medical conditions and with a range of controls and research methodologies. Furthermore, recent research shows that psychodynamic therapy is frequently used in clinical practice (Cook 2010; Norcross 2013). Hence, it is important to update this Cochrane review to clarify the current state of evidence of STPP for CMDs.
While early meta‐analyses have yielded differing results due to differences in methodology (Anderson 1995; Crits‐Christoph 1992;Svartberg 1991), more recent reviews have generally reported large effects sustained or increasing over time within group while studying RCTs and non‐RCTs. Heterogeneity has been high in many studies and not all results were maintained in subgroup analyses suggesting a cautious interpretation is required. None of these reviews employed a methodology similar to ours including the entire cluster of CMDs versus all non‐formal psychotherapy or wait‐list controls.
Thus, we present this updated Cochrane review of these treatment approaches compared with non‐treatment and minimal treatment controls for people with CMDs.
Objectives
To evaluate the efficacy of STPP for adults with CMDs compared with wait‐list controls, treatments as usual and minimal contact controls in RCTs. To specify the differential effects of STPP for people with different disorders (e.g. depressive disorders, anxiety disorders, somatoform disorders, mixed disorders and personality disorder) and treatment characteristics (e.g. manualised versus non‐manualised therapies).
Methods
Criteria for considering studies for this review
Types of studies
RCTs of STPP treatments. Cluster randomised trials and cross‐over randomised trials were eligible.
Types of participants
Participant characteristics
Adults (i.e. over 17 years old).
Diagnosis
We reviewed the following CMDs (among others), anxiety disorders, depressive disorders, somatoform disorders, certain behaviour disorders (such as eating disorder, self injurious behaviour) and interpersonal or personality problems mixed with symptom disorders.
Co‐morbidities
We accepted studies with medical or psychiatric co‐morbidity, including personality disorder.
We excluded studies of people with psychotic disorders.
Setting
We limited the population to outpatients.
Types of interventions
Experimental intervention
We defined STPP as:
at least one treatment group as psychodynamic in nature and treatment lasted 40 weeks or less on average.
treatment was 40 or fewer sessions, as this is the definition used in previous meta‐analyses;
the treatment technique was derived from the work of one or more developers of STPPs such as Malan (Malan 1979), Davanloo (Davanloo 1980), or Luborsky (Luborsky 1984), or was specifically developed and described for a brief psychodynamic approach;
the treatment under investigation was given in an individual format; and
the treatment had standard length sessions of 45 to 60 minutes.
Control interventions
We included studies in which controls were those conditions other than robust, bona fide psychological therapy treatments for the condition studied. These included:
wait‐list controls;
minimal treatment controls that had been designed as psychological 'placebo treatments'. For example these may have included short supportive conversations each month, the provision of psycho‐education, or partial treatments not expected to provide a robust psychotherapy effect;
treatments as usual including, for example, medical treatment as usual and psychiatric care as usual; and
studies in which non‐psychotherapeutic treatments (such as medications or medical care as usual) were provided equally in both arms.
Types of outcome measures
Primary outcomes
1. General symptoms as defined by standardised psychiatric instruments or criteria (e.g. Symptom Checklist 90; Derogatis 1994).
2. Somatic symptoms (e.g. McGill Pain Questionnaire; Melzack 1975).
3. Anxiety (e.g. Hamilton Anxiety Rating Scale; Hamilton 1959).
4. Depression (e.g. Beck Depression Inventory (BDI); Beck 1961).
Secondary outcomes
5. Social adjustment (e.g. the Social Adjustment Scale; Weissman 1978).
6. Quality of life (e.g. EuroQol; EuroQol 1990).
7. Behavioural measures (e.g. attempts at self harm).
8. Interpersonal problem measures (e.g. Inventory of Interpersonal Problems; Horowitz 1988).
9. Patient satisfaction as measured by standardised instruments.
10. Health service use (e.g. hospital admission, outpatient contacts, visits to primary care).
11. Cost measures (e.g. medication cost changes).
12. Death.
13. Dropout rates.
14. Occupational functioning.
Hierarchy of outcome measures
When more than one scale was used to measure similar elements or the same element (e.g. depression), we used the following approach:
blind observer rated measures were used over self reported measures;
well‐known, validated measures were used ahead of lesser known, not well‐validated measures;
measures covering the scope of a condition were used ahead of measures covering only part of a condition (e.g. BDI versus Beck Hopelessness Scale: hopelessness is only one part of depression and is covered in the BDI so the BDI is used);
the measure designated as the a priori primary outcome measure was used over what was an a priori designated secondary outcome measure.
We solved cases of any disagreement between evaluators through consensus or eliciting the opinion of a third rater.
Timing of outcome assessment
Where sufficient data were available, we studied treatment outcomes in three time frames:
short‐term: less than three months after treatment was concluded;
medium‐term: three to nine months after treatment was concluded;
long‐term: nine or more months after treatment is completed.
When there were multiple measurement points inside one time frame, we used data from the longest follow‐up assessment.
Search methods for identification of studies
The Cochrane, Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK, a references register and a studies based register. The CCDANCTR‐References Register contains over 34,000 reports of randomized controlled trials in depression, anxiety and neurosis. Approximately 60% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Coordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950‐), EMBASE (1974‐) and PsycINFO (1967‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the World Health Organisation’s trials portal (ICTRP), ClinicalTrials.gov, drug companies, the hand‐searching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies can be found on the Group‘s website.
Electronic searches
1. The Cochrane, Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR)
The CCDANCTR was searched by the Group's Trials Search Co‐ordinator (TSC) to February 2010 using a sensitive list of terms for psychodynamic psychotherapies (intervention only). An update search was conducted in February 2014 using a more precision maximazing search strategy (intervention + comparator). A companion search of PsycINFO was also conducted at this time.
CCDANCTR (Studies and References Register, update search 2014‐02‐21): #1 (psychoanalytic or psychodynamic* or psycho‐dynamic* or (*dynamic* and (brief or *psycho* or *therap*)) or "time limited psychotherap*" or mann's or davanloo* or hobson* or STPP or ISTDP):ti,ab,kw,ky,emt,mh,mc #2 ("treatment as usual" or tau:ab or "usual care" or "care as usual" or waitlist* or "wait* list*" or wait‐list* or "minim* contact*") #3 (enhanced or routine or standard or traditional or usual) NEAR2 (*care or treatment or *therap*) #4 (delay* or “no treatment” or “no *therap*”) NEAR (control or group or treatment*) #5 (peer or “self help*” or “mutual help*” or (support* NEAR2 (“help” or group or *therap* or listening)) or relaxation) #6 (“combined modality” or (combin* NEAR2 (therapy or treatment))) #7 (#1 and (#2 or #3 or #4 or #5 or #6))
OVID PsycINFO (update search 2014‐02‐21): 1. PSYCHODYNAMICS/ 2. PSYCHODYNAMIC PSYCHOTHERAPY/ 3. (psychodynamic* and (therapy or psychotherapy)).ti,ab. 4. ((brief adj3 dynamic) and (therapy or psychotherapy)).ti,ab. 5. (dynamic* adj3 (therapy or psychotherapy)).ti,ab. 6. or/1‐5 7. (randomized or randomised).ti,ab,sh. 8. (random* adj3 (administ* or allocat* or assign* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab. 9. or/7‐8 10. 6 and 9 PsycINFO records were screened and added to the CCDANCTR as appropriate.
CCDANCTR (Studies and References Register, initial search, all years to 2010‐02‐03): Studies Register: Intervention = (Psychodynamic or Dynamic or Psychoanalytic or Analytic) and Age Group = (Adult or Aged) References Register: Free‐Text = Psychodynamic or Dynamic or Psychoanalytic or Analytic
2.Other electronic searches To ensure all eligible studies and review articles were identified, we conducted our own searches on the following electronic databases (2012‐07‐23): The Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE (1966‐); EMBASE (1980‐), CINAHL (1982‐), PsycINFO (1887‐ ), the Database of Abstracts of Reviews of Effectiveness (DARE) and Biological Abstracts (January 1980‐). The search strategy included terms for common mental health disorders and brief/time limited psychodynamic psychotherapies, see CENTRAL search (Appendix 1).
For MEDLINE, we expanded the search to include ANALYTIC, PSYCHOANALYTIC, DYNAMIC or PSYCHODYNAMIC, as the National Library of Medicine has defined brief psychotherapy as being not more than 20 sessions for indexing purposes since 1973. This ensured we did not miss therapies of up to 40 sessions.
No restrictions on date, language or publication status were applied to the searches. All relevant foreign language papers were translated.
Searching other resources
Reference lists
We checked the reference lists of all retrieved and potentially relevant papers, as well as relevant systematic reviews and literature reviews to identify other potentially relevant articles. We retrieved and assessed these articles for possible inclusion in the review.
Personal communications
We wrote to the lead author of relevant studies to ascertain if they knew of any additional related published or unpublished data that may have been relevant to the review. We contacted two list serves containing psychodynamic researchers to ask about recent studies.
Handsearching
We scrutinised abstracts from national and international psychiatry and psychology conferences to identify unpublished studies. These included meetings organised by national and international medical colleges, speciality societies and professional organisations. We contacted the authors of these studies to obtain further details about the studies and to enquire if they knew of any other unpublished or published relevant work.
Data collection and analysis
Selection of studies
Pairs of review authors independently selected suitable studies for inclusion in this review as detailed below. Where the two review authors disagreed about the inclusion of a study, we resolved disagreements by consensus, and consulted a third author if they could not reach consensus. Where resolution was not possible, we contacted the investigator to obtain more information and clarification.
We assessed the titles and abstracts of studies identified by searching electronic databases to determine whether each article met the eligibility criteria. In order to limit bias, we printed out a list of all titles and abstracts excluding the investigators' names, institutions and journal title. If the title and abstract contained sufficient information to determine that an article did not meet the inclusion criteria, we rejected that article. We documented all rejected papers and the reasons for rejection.
We retrieved the full papers of all remaining titles and abstracts deemed relevant. In addition, we reviewed all other potentially relevant articles identified by the various search strategies (reference checking, personal communications, etc.). We translated all papers in languages other than English or someone competent in that language reviewed them.
Data extraction and management
Two review authors independently reviewed all articles, each of whom completed a form for each study and made a judgement on the quality using the 'Risk of bias' tools defined below. We documented the reasons for exclusion. Where the same study had more than one article written about the outcomes, we treated all articles as one study and presented the results only once.
Data extraction
We extracted data from the papers and recorded them on forms to elicit the following information:
general (published/unpublished, title, authors, source, contact address, country, language of publication, year of publication, duplicate publications);
interventions (frequency, timing, individual versus group, up to 20 sessions versus 20 to 40 sessions, manual driven versus non‐manualised therapies), comparison interventions, concurrent medications;
participant characteristics ‐ sampling, exclusion criteria, number of participants, age, sex, ethnicity, marital status, educational status, duration of symptoms, number of complications, similarity of groups at baseline (including any co‐morbidity), withdrawals/losses to follow‐up (reasons/descriptions);
primary diagnosis (e.g. depression, anxiety or somatoform disorders). These were determined based on the reported diagnoses being treated in the paper independent of which diagnostic criteria were being used (e.g. Feighner Criteria or Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM‐IV) for major depression were both considered as depression);
type of medical co‐morbidity if present;
type of psychiatric co‐morbidity ‐ clinical diagnosis or symptomatology assessed by questionnaire;
type of outcome ‐ self report or observer‐rated;
type of assessment tool used to assess psychiatric co‐morbidity (e.g. BDI, Zung Depression Scale, Hospital Anxiety and Depression Scale, Structured interview, DSM‐IV criteria;
cut‐off used on psychiatric scale, percentage of people defined as psychiatric cases on this basis; mean (standard deviation (SD)) symptom score;
timing of follow‐up: short‐term (less than three months), medium‐term (three to nine months) and long‐term (more than nine months);
assessment of different domains of bias according to the 'Risk of bias' tool defined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008b).
We reported a summary of data extracted from included studies.
Main planned comparisons
STPP versus wait‐list/treatment as usual/minimal treatment.
Assessment of risk of bias in included studies
For the current update of this review, we have updated the methods to include assessment for 'Risk of bias' based on the revised version of the Cochrane Handbook for Systematic Reviews of Interventions (Section 8.5.1; Higgins 2008b). For each included study, two review authors assessed the degree to which:
the allocation sequence was adequately generated (random sequence generation);
the allocation was adequately concealed (allocation concealment);
knowledge of the allocated interventions was adequately prevented during the study (blinding);
incomplete outcome data were adequately addressed;
reports of the study were free of suggestion of selective outcome reporting; and
the study was apparently free of other problems that could put it at high risk of bias.
We allocated each domain one of three possible categories for each of the included studies: low risk of bias, high risk of bias and unclear risk of bias (where the risk of bias was uncertain or unknown).
We resolved any disagreements by discussion or by involving a third review author.
In future reviews, we will adapt the 'Risk of bias' tool to incorporate features such as the use of adherence ratings, the use of manuals, therapist experience, handling of participants lost to follow‐up and researcher allegiance to enable measurement of psychotherapy quality.
Measures of treatment effect
Many rating scales are available to measure outcomes in psychological trials. These scales vary in the quality of their validation and reliability. Therefore, if a rating scale's validation had not been published in a peer‐reviewed journal, then the data were not included in this review. In addition, the rating scale should have been either self report or completed by an independent observer or relative. Trials that used the same instrument to measure specific outcomes were used in direct comparisons where possible. We reported the mean and SD. Where SDs were not reported in the paper, we attempted to obtain them from the authors or to calculate them using others measures of variation that were reported, such as the confidence intervals (CI). Where possible, we meta‐analysed data from different scales, rating the same effect using the standardised mean difference (SMD). We considered SMDs of 0.2 as small, 0.5 as moderate and 0.8 and greater as large (Cohen 1988).
Unit of analysis issues
Cross‐over trials
Due to the risk of carry‐over effects in cross‐over trials, we used only data from the first phase of the study.
Cluster‐randomised trials
Should any cluster randomised trials be identified in future updates of this review, we will include them as long as proper adjustment for the intra‐cluster correlation can be undertaken as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2009).
Studies with multiple treatment groups
Where studies had additional treatment arms that were not relevant to this review, we did not consider those additional data. If a study had more than two treatment arms that met the inclusion criteria (e.g. two brief psychodynamic psychotherapy models and a psychological placebo arm), then the data from the psychological placebo arm were split equally between to produce two (or more) pair wise comparisons.
Dealing with missing data
Where it was not possible to analyse data quantitatively as reported in published studies, we contacted the first author to obtain the additional data required. We used data from intention‐to‐treat (ITT) analyses where possible. We listed issues of attrition bias in the 'Risk of Bias' tables.
Assessment of heterogeneity
We assessed heterogeneity on the basis of the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (I2 values of 0% to 40%: might not be important; 30% to 60%: may represent moderate heterogeneity; 50% to 90%: may represent substantial heterogeneity; 75% to 100%: considerable heterogeneity). In addition to the I2 value (Higgins 2003), we presented the Chi2 and its P value and considered the direction and magnitude of the treatment effects. In a meta‐analysis with few studies, the Chi2 test is underpowered to detect heterogeneity should it exist, thus, we used a P value of 0.10 as a threshold of statistical significance. Hence, we consider P value < 0.10 and I2 of 50% or more to reflect significant heterogeneity.
Assessment of reporting biases
We used data from all identified and selected trials to draw a funnel plot (size of study versus effect size) (Egger 1997), to attempt to detect the possibility of publication bias. However, it should be noted that there may be other reasons for asymmetry in funnel plots, such as heterogeneity and small‐study effects.
Data synthesis
If studies were available that were sufficiently similar and of sufficient quality, we pooled those that could be grouped together and used the statistical techniques of meta‐analysis using Review Manager 5 software (RevMan 2012). We used a fixed‐effect model when there was little statistical heterogeneity (both P value > 0.10 and I2 of 50% or greater). In cases where there was significant heterogeneity (both P value < 0.10 and I2 of 50% or greater), we used a random‐effects model. Thus, we relied on the results of these two measures to decide which model to report. The rationale for this decision was that, even though there were expectations of variation between studies (due to samples, treatment approaches and controls), within each subgroup (e.g. social adjustment, short‐term follow‐up) there was a possibility of low heterogeneity due to the measures, timing and groups using those measures (e.g. mostly studies of people with depression measuring depression). In cases where these measures of heterogeneity were not significant and we used a fixed‐effect model, we also examined the effects using a random‐effects model to determine if this decision had any bearing on outcomes.
Subgroup analysis and investigation of heterogeneity
In order to investigate sources of heterogeneity, we performed subgroup analyses as follows:
studies using minimal treatment or wait‐list controls as opposed to treatment as usual as a comparator;
studies of therapy of up to 20 sessions versus over 20 sessions in duration;
studies of specific STPP methods when there were adequate numbers (five or more) of such studies; and
studies of different diagnostic groups including depressive disorders, anxiety disorders, somatoform disorders, mixed disorders and personality disorder.
Sensitivity analysis
We performed sensitivity analyses examining treatment effects of the following groups of studies in comparison with those of the entire group of studies:
manualised therapies only;
studies giving observer‐rated outcome;
studies with medications provided on both study arms.
Results
Description of studies
Results of the search
We carried out update searches to 23 July 2012. These broad searches identified more than 6800 references. It is likely many of these overlapped with the large set of studies reviewed for this original review (Abbass 2006). We excluded all but 18 from assessment of title and abstract. Fifteen remained after de‐duplication. We retrieved full papers for these 15 records. After inspection of the full‐text papers, we excluded five records. The remaining 10 references were added to those from the earlier version of this review and they contributed to the analysis (Characteristics of included studies).
In this updated version of the review, Dare 2001 was moved from the excluded studies to the included studies, in accordance with Cochrane's MECIR standards (Chandler 2013), which states that eligible studies be included irrespective of whether measured outcome data has been reported in a 'useable' way.
The study selection process is also detailed in the PRISMA flow diagram (Figure 1).
1.
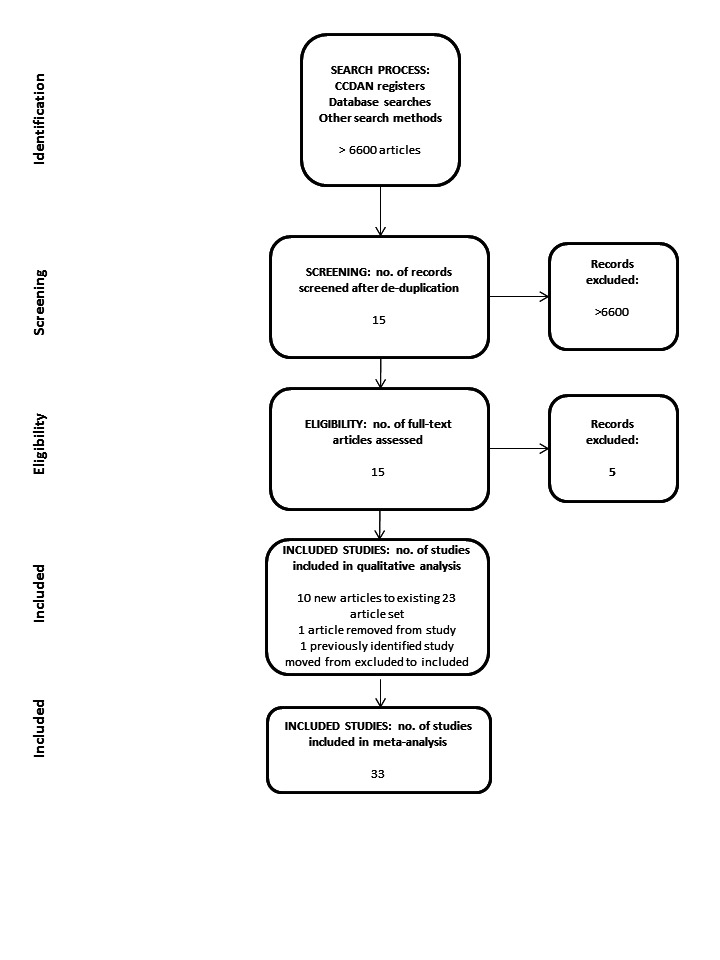
PRISMA flow diagram.
A late‐stage literature search was conducted by the Cochrane, Depression, Anxiety and Neurosis Group (February 2014) and publications to be considered for inclusion in the next update of this review are listed (for the reader's benefits) in the Characteristics of studies awaiting classification .
Included studies
See Characteristics of included studies table.
Design
All 33 studies included were RCTs. We found several cross‐over trials but no cluster randomised trials.
Sample sizes
The mean number of randomised participants was 65.3 with nearly all samples containing between 30 and 80 participants.
Setting
All studies were conducted in outpatient settings. Studies were conducted in several countries primarily in Europe and North America.
Participants
All studies were of adult samples. Six studies included only female participants (Alstrom 1984b; Baldoni 1995; Carrington 1979; Cooper 2003; Marmar 1988; Vitriol 2009), and almost all of the studies had a majority of females. Primary problems were diverse and included somatoform disorders (eight studies), mixed conditions (eight studies), anxiety disorders (seven studies), depressive disorders (five studies), personality disorders (three studies), self induced poisoning (one study) and eating disorders (one study). The somatoform disorders included multisomatoform disorder, irritable bowel syndrome (three studies), chronic pain, urethral syndrome, pelvic pain, chronic dyspepsia and atopic dermatitis. Anxiety disorders included obsessive‐compulsive disorder, generalised anxiety disorder, hypochondriasis, agoraphobia, social phobia, panic disorder and post‐traumatic stress disorder.
Over one‐third of these studies included challenging‐to‐treat populations. Three studies included people with co‐morbid personality disorders among their samples or as the main study sample (Abbass 2008; Emmelkamp 2006;Winston 1994). One study included people with deliberate self poisoning (Guthrie 2001). Several studies were of 'treatment resistant' (Guthrie 1993), 'high utilizers' (Guthrie 1999), 'chronic' (Hamilton 2000), or 'severe' (Creed 2003; Sattel 2012; Vitriol 2009) populations, while two included participants who were not candidates for a traditional psychoanalytic treatment (Alstrom 1984a;Alstrom 1984b).
Interventions
A range of brief psychodynamic‐based psychotherapy methods were represented in these studies. Eleven cited Davanloo/Malan's model (Davanloo 1980;Malan 1979), while six cited PIT derived from Hobson 1985. These courses of therapy averaged 15.0 psychodynamic therapy sessions (SD 8.9, range 4 to 40). They were described as employing common factors of brief dynamic therapies such as focus on unconscious operations and emotions, and their link to symptoms or behavioural problems. All but one study described the use of some brief therapy framework, while two studies had a general psychoanalytic model of short duration (Cooper 2003; Sloane 1975). Fourteen of these studies described using experienced therapists, but it was often unclear whether the therapists were experienced in the specific brief therapy approach versus other psychotherapy models. Fifteen studies referred to specific manuals while others referenced models including those of Davanloo 1980; Malan 1979;Mann 1973; and Strupp 1984. Because we did not exclude studies with medication use on both treatment arms, we included five such studies (Burnand 2002;de Jonghe 2001;Maina 2010;Vitriol 2009; Wiborg 1996). These five studies included people with depression, panic disorder and mixed disorders: participants were provided medications including clomipramine (two studies), other antidepressants (two studies) and psychotropic agents (one study) according to an algorithm from antidepressants to antipsychotics.
A range of controls was employed in these studies. Eighteen studies had treatment as usual, which included medications, medical management and, in some cases, psychotherapeutic support that did not constitute a robust treatment effort. Ten studies had wait‐list controls, often with cross‐over designs where participants received STPP after the wait list. Five studies had minimal psychological interventions used as controls. Overall, treatment as usual control situations provided less face‐to‐face therapist contact time than the STPP groups, although these were considered standard treatment approaches with presumed effectiveness. Fewer treatment benefits, due in part to less intense therapeutic exposures, would be expected in the wait list and minimal treatment controls versus controls with more robust treatments as usual including medication in many cases: for this reason, we conducted a sensitivity analysis excluding studies with treatment as usual controls.
Outcomes
Nineteen studies reported on general psychiatric symptoms, 18 studies used measures of depression, 18 studies used measures of anxiety, eight studies used somatic symptom measures, six studies used interpersonal problem measures and nine studies used measures of social adjustment. Other measures were used only a few times or were not comparable enough to combine in this review.
Follow‐up periods varied from immediately post treatment up to four years (Baldoni 1995).
Excluded studies
We listed 22 studies in the Characteristics of excluded studies table. Most studies examined in detail and ultimately excluded were studies that had other formal treatment controls. We excluded a study of ulcers that was included in the previous version of this review as it was conducted prior to the discovery of Helicobacter pylori and specific treatment of this (Sjodin 1986): thus, the care of ulcer disease has undergone major changes since this discovery. Other studies were not randomised trials.
Studies awaiting classification
There are 11 studies awaiting classification (see Characteristics of studies awaiting classification table). Three of these studies are of depression, three studies are of somatic symptom disorders and two studies are of anxiety disorders. Four of the studies are large with over 150 participants. Due to these large numbers and sets of studies inside of specific diagnostic categories, it is possible these studies may influence meta‐analytic outcomes.
New studies found at this update
We included 10 new trials in this update (Bressi 2010; Burnand 2002; Carrington 1979; Emmelkamp 2006; Levy Berg 2009; Maina 2010; Milrod 2007; Sattel 2012; Sørensen 2010; Vitriol 2009). Dare 2001 was moved from the excluded studies to the included studies, in accordance with The Cochrane Collaboration's methodological stipulation that studies that meet the inclusion criteria should be included in the review irrespective of whether they reported data in a useable way (Chandler 2013).
Ongoing studies
We have identified three ongoing studies (see Characteristics of ongoing studies). One of these is an RCT of intensive short‐term dynamic psychotherapy versus medical care as usual for treatment‐refractory depression (NCT01141426). One is an RCT of intensive short‐term dynamic psychotherapy versus care as usual for medically unexplained symptoms in the emergency department (NCT02076867). One is an RCT of dynamic interpersonal therapy versus an enhanced wait list condition for major depression (ISRCTN38209986).
Risk of bias in included studies
For details of the risk of bias judgements for each study, see Characteristics of included studies. Graphical representations of the overall risk of bias in included studies are presented in Figure 2 and Figure 3.
2.
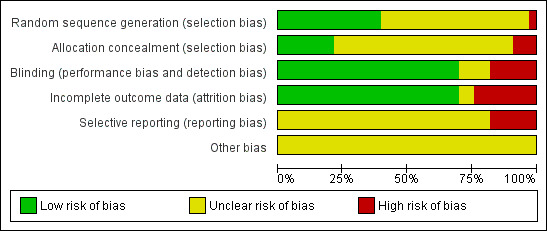
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We judged only three of the 33 included studies to be at high risk of selection bias. However, for the majority of studies (19 out of 33 for selection bias (random sequence generation) and 23 out of 33 for selection bias (allocation concealment)), there was inadequate information to make a satisfactory risk of bias judgement.
Blinding
With self reported measures, blinding of the observer was less important. We judged the majority of studies (24 out of 33) to be of low risk of bias. For observer‐rated measures, we reported six studies as being at high risk of detection bias because raters were not blinded to treatment allocation group.
Incomplete outcome data
For the majority of studies (23 out of 33), we judged attrition bias to be at low risk of bias. We judged eight studies to be at high risk of bias and there was insufficient information to make an assessment for two studies. Studies classified as at high risk of attrition bias did not account for evident attrition in analyses.
To limit the influences of attrition bias, we only included studies with less than 20% drop‐outs but in the next iteration of this review, this will not be the case. Examination of the effects of the methods of handling of lost cases will be performed through risk of bias assessment and subgroup analyses.
Selective reporting
In six studies, we deemed there to be high risk of reporting bias. Without details of the study protocol, we deemed there to be insufficient information regarding reporting bias and therefore, we judged assessment of reporting bias to be unclear for the remaining studies.
Other potential sources of bias
For all studies, we judged risk of other sources of bias to be unclear due to insufficient information. One study employed a restricted STPP model where some key treatment ingredients were withheld for purposes of the study (Sørensen 2010).
Effects of interventions
We were able to combine results from studies for general psychiatric symptoms as well as anxiety disorders, depressive disorders and somatic symptoms. In each case, we have grouped findings under the following diagnostic groups: depression, anxiety, somatoform and mixed disorders. We highlighted any differences between groups in the section on subgroup analyses.
A few studies (e.g. Baldoni 1995;Creed 2003;Wiborg 1996 in general outcome measures) provided data at long‐term follow‐up but not at short‐term follow‐up in some outcome categories. Attrition data was lacking from or varied in definition in most papers so we reported only papers with self described dropout rates where they did statistical analyses and reported on it: we are considering a plan to extract/seek this data formally and report it in the next review.
Comparison 1. Short‐term psychodynamic psychotherapy versus wait‐list/treatment as usual/minimal treatment
Primary outcomes
There was significant heterogeneity (P values < 0.10, I2 = 50% or greater) in 10 of the 16 analyses. Therefore, we reported results derived from the random‐effects model for these comparisons. We reported results derived from the fixed‐effect model for the remaining analyses where measures of heterogeneity were not significant. These are illustrated in the Data and analyses table and figures. Given the frequency of significant heterogeneity in these analyses, in each study where a fixed‐effect model was reported, we also examined results using a random‐effects model: in each of the six cases, the differences were nil to negligible and there were no changes in statistical significance.
1.1 General symptoms as defined by standardised psychiatric instruments or criteria
We were able to incorporate 19 studies that reported measures of general psychiatric symptoms. We used the random‐effects model for short‐ and long‐term follow‐up, as there was significant heterogeneity and used the fixed‐effect model for medium‐term comparisons. These measures showed small to large differences in favour of STPP treatment.
The differences reached significance in the short‐term (SMD ‐0.71, 95% CI ‐1.00 to ‐0.41; 19 studies, 1424 participants) (Analysis 1.1) and medium‐term (SMD ‐0.27, 95% CI ‐0.46 to ‐0.08; 5 studies, 437 participants) (Analysis 1.2). In the case of long‐term follow‐up, the effect sizes increased but marginally did not reach significance (SMD ‐1.51, 95% CI ‐3.14 to 0.12, P value = 0.07; 4 studies, 344 participants) (Analysis 1.3).
1.1. Analysis.
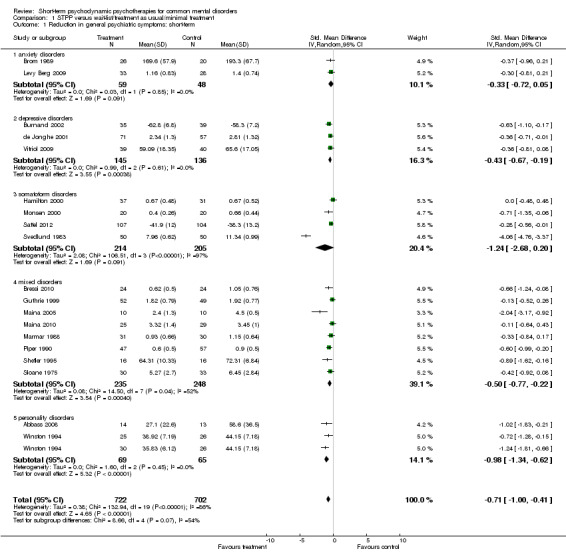
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 1 Reduction in general psychiatric symptoms: short‐term.
1.2. Analysis.

Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 2 Reduction in general psychiatric symptoms: medium‐term.
1.3. Analysis.

Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 3 Reduction in general psychiatric symptoms: long‐term.
1.2 Somatic symptoms
We were able to incorporate eight studies that reported measures of somatic symptoms. We used the random‐effects model for short‐, medium‐ and long‐term follow‐up, as there was significant heterogeneity. These measures showed moderate to large differences in favour of STPP treatment.
The difference between treatment and control groups marginally did not reach statistical significance in the short‐term (SMD ‐0.63, 95% CI ‐1.29 to 0.04, P value = 0.07; 8 studies, 744 participants) (Analysis 1.4). The effects were significant in the medium‐term (SMD ‐1.39, 95% CI ‐2.75 to ‐0.02; 4 studies, 359 participants) (Analysis 1.5) but did not reach significance in long‐term follow‐up (SMD ‐2.21, 95% CI ‐5.49 to 1.07; 3 studies, 280 participants) (Analysis 1.6).
1.4. Analysis.
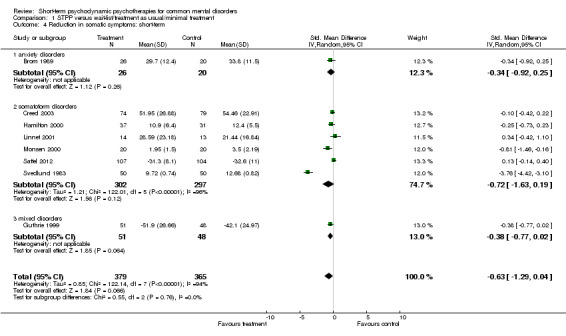
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 4 Reduction in somatic symptoms: short‐term.
1.5. Analysis.

Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 5 Reduction in somatic symptoms: medium‐term.
1.6. Analysis.

Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 6 Reduction in somatic symptoms: long‐term.
1.3 Anxiety
We were able to incorporate 18 studies that reported measures of anxiety symptoms. We used the random‐effects model for short‐, medium‐ and long‐term follow‐up, as there was significant heterogeneity. These measures showed modest to large differences in favour of STPP treatment.
The differences were statistically significant in the short‐term (SMD ‐0.64, 95% CI ‐1.02 to ‐0.26; 18 studies, 1102 participants) (Analysis 1.7) and medium‐term (SMD ‐0.46, 95% CI ‐0.77 to ‐0.16; 7 studies, 506 participants) (Analysis 1.8). In the long‐term follow‐up, these effects increased but marginally did not reach significance (SMD ‐1.10, 95% CI ‐2.24 to 0.04, P value = 0.06; 5 studies, 293 participants) (Analysis 1.9).
1.7. Analysis.
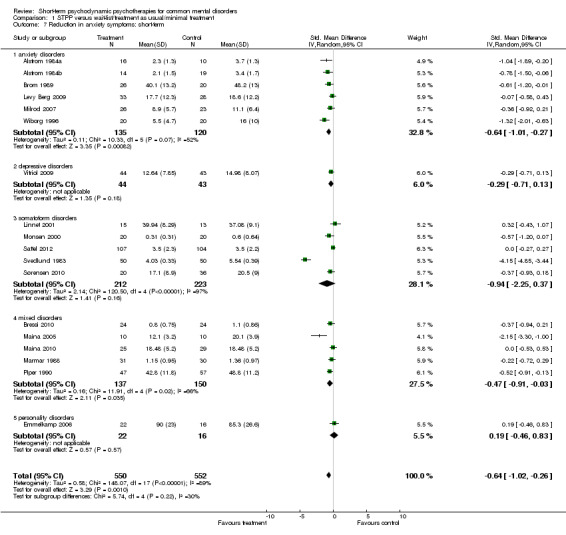
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 7 Reduction in anxiety symptoms: short‐term.
1.8. Analysis.
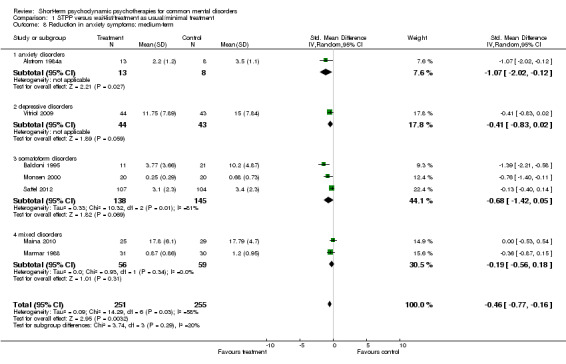
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 8 Reduction in anxiety symptoms: medium‐term.
1.9. Analysis.
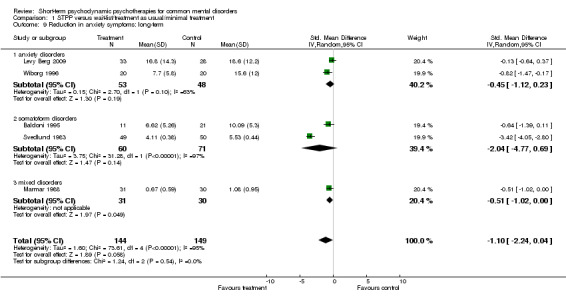
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 9 Reduction in anxiety symptoms: long‐term.
1.4 Depression
We were able to incorporate 18 studies that reported measures of depression symptoms. We used the random‐effects model for medium‐ and long‐term follow‐up, as there was significant heterogeneity and used the fixed‐effect model for short‐term comparisons.
Measures of depression showed small to medium and significant treatment effects relative to controls in the short‐term (SMD ‐0.50, 95% CI ‐0.61 to ‐0.39; 18 studies, 1415 participants) (Analysis 1.10) and the medium‐term (SMD ‐0.34, 95% CI ‐0.60 to ‐0.09; 7 studies, 601 participants) (Analysis 1.11). The effects increased but did not reach significance in long‐term follow‐up (SMD ‐1.00, 95% CI ‐2.22 to 0.21; 5 studies, 321 participants) (Analysis 1.12).
1.10. Analysis.
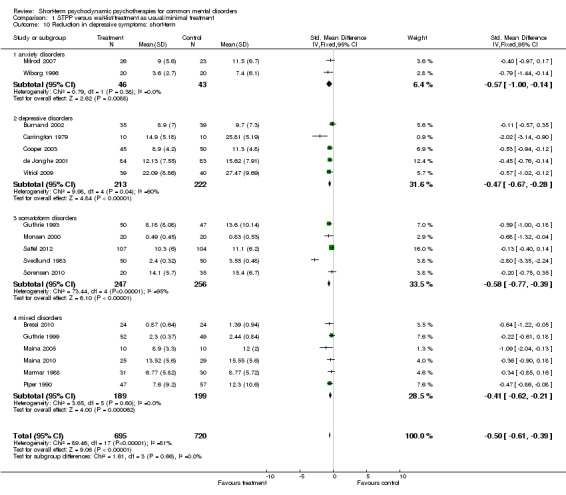
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 10 Reduction in depressive symptoms: short‐term.
1.11. Analysis.
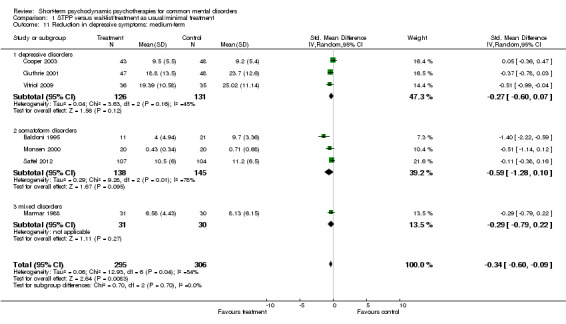
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 11 Reduction in depressive symptoms: medium‐term.
1.12. Analysis.

Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 12 Reduction in depressive symptoms: long‐term.
Secondary outcomes
In our protocol, we stated that we would consider secondary outcome measures including social adjustment, quality of life, behavioural measures, interpersonal problem measures and participant satisfaction as measured by standardised instruments. However, studies reported very different measures in insufficient detail for quantitative integration of data in most cases. In all cases, we used the fixed‐effect model, as tests for heterogeneity were non‐significant.
1.5 Social adjustment
Ten studies reported on social adjustment and showed significant and moderate effects in short‐term follow‐up using the fixed‐effect model (SMD ‐0.51, 95% CI ‐0.66 to ‐0.36; 9 studies, 720 participants) (Analysis 1.13), which increased in long‐term follow‐up (SMD ‐0.58, 95% CI ‐0.86 to ‐0.29; 3 studies, 199 participants) (Analysis 1.14).
1.13. Analysis.
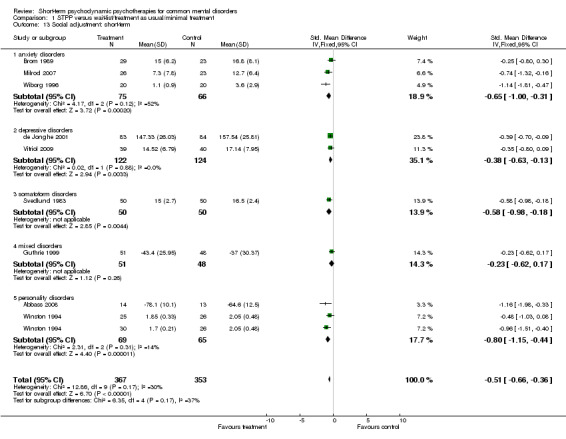
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 13 Social adjustment: short‐term.
1.14. Analysis.
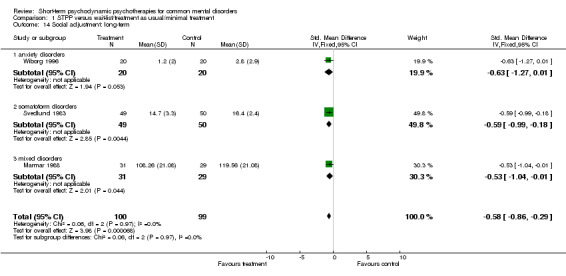
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 14 Social adjustment: long‐term.
1.6 Quality of life
Guthrie 1999, using the EuroQol 5D, did not find significant differences at termination but did find significantly higher quality of life ratings in the STPP group in follow‐up. Creed 2003 found significant and persistent improvements on the 36‐item Short Form (SF‐36) physical scores relative to controls, but found significant superiority of STPP only in the short‐term on mental symptom subscales relative to controls. Levy Berg 2009 found greater improvement on the World Health Organization (WHO) Well Being Index in people receiving STPP with generalised anxiety disorder. de Jonghe 2001 reported greater gains on a measure of depression‐related quality of life in people who received combined STPP plus antidepressants versus antidepressant medication alone in the ITT sample.
1.7 Behavioural measures
In a unique and high‐quality study, Guthrie 2001 found treated participants had a reduction in suicidal ideation and self harm episodes relative to treatment as usual in people who had self induced poisoning. Dare 2001 found STPP to produce superior weight gains and recovery rates compared with controls in a group of adults with anorexia nervosa.
1.8 Interpersonal problem measures
Six studies reported outcomes on measures of interpersonal problems. Using the fixed‐effect model, significant effects were seen in the short‐term follow‐up (SMD ‐0.42, 95% CI ‐0.67 to ‐0.17; 6 studies, 265 participants) (Analysis 1.15), which increased in the long‐term follow‐up (SMD ‐0.49, 95% CI ‐0.92 to ‐0.05; 3 studies, 85 participants) (Analysis 1.16).
1.15. Analysis.

Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 15 Interpersonal problems: short‐term.
1.16. Analysis.
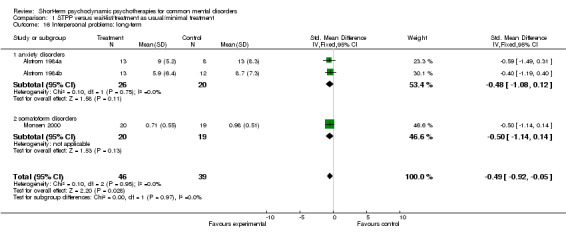
Comparison 1 STPP versus wait‐list/treatment as usual/minimal treatment, Outcome 16 Interpersonal problems: long‐term.
1.9 Participant satisfaction
Guthrie 2001 reported positive participant satisfaction measures after the six‐session treatment for deliberate self poisoning.
1.10 Health service use
Hamilton 2000 reported within‐group reduction in hospital, medication and service use but no differences between treatment and control groups. Burnand 2002 reported significantly fewer hospital admissions and days in people with depression provided STPP versus the treatment as usual control. Vitriol 2009 reported that severely depressed women with trauma histories treated with STPP had fewer hospital days (6 versus 21.3) but did not note if this was statistically different. Psychiatry use was greater in the STPP group (7 versus 2.5) as was psychologist use (5.7 versus 4.5 visits) in six‐month follow‐up. Guthrie 2001 reported no differences in healthcare use versus controls in follow‐up except treated participants with deliberate self poisoning saw psychiatric nurses more often. Sattel 2012 reported significantly less medication and psychotherapy use versus controls in follow‐up after STPP versus enhanced medical care for people with multisomatoform disorder: there were no differences in medical visits between the groups at any time point.
1.11 Cost measures
Creed 2003 found STPP was more cost effective than treatment as usual over the first year of treatment in people with irritable bowel syndrome, while paroxetine was not significantly more cost effective than control. Guthrie 1999 found STPP to reduce several cost measures significantly compared with treatment as usual in a mixed sample of high service‐utilising participants. Hamilton 2000 did not find significant cost savings relative to the control treatment but did note significant cost savings compared with the period before treatment. Burnand 2002 found significant cost savings beyond treatment costs of USD 2311 due to reduced hospital and disability costs: this is greater than controls but statistical analysis of the difference was not provided.
1.12 Mortality
No data were available for mortality.
1.13 Dropout rates
Two studies reported statistical analysis of differential dropout rates. de Jonghe 2001 specifically compared dropout rates between STPP added to treatment with medications versus medications alone. They found a 10% dropout rate using STPP plus medication versus 40% for medication alone. Milrod 2007 reported 7% drop‐out in the STPP group compared with 34% in treatment as usual, which was significantly different.
1.14 Occupational functioning
Monsen 2000 found those treated with STPP had significantly more job advancements and Creed 2003 found STPP‐treated participants had significantly less work disability compared with the paroxetine‐treated group. Abbass 2008 reported significantly more works hours and higher employment rates after STPP treatment versus the control condition in people with anxiety disorders. Alstrom found significantly superior improvement in work capacity relative to controls in the agoraphobic group (Alstrom 1984b), but not in the socially phobic group (Alstrom 1984a). Burnand 2002 reported significantly improved occupational functioning with fewer lost days due to disability.
Heterogeneity analysis
Tests for heterogeneity were statistically significant at the P value 0.10 or less and an I2 statistic of 50% or greater in 10 of the 16 cases. Heterogeneity was not significant for some subgroup analyses of the symptom most specific to the condition under consideration (e.g. medium‐term comparisons of depressive symptoms in depressive disorders). It was not significant in measures of social adjustment and interpersonal problems.
Sensitivity and subgroup analyses
Because of the small number of trials in each analysis, these results are limited and should be interpreted with caution. Given the degree of heterogeneity expected in these analyses, we only present results using the random‐effects model. See Table 1 and Table 2.
1. Properties of studies.
| Study | Diagnosis | Manualised |
Observer rated |
Medication on both arms |
Wait‐list/ minimal treatment control |
20 or fewer sessions |
Malan/ Davanloo |
Hobson/ PIT |
| Abbass 2008 | Mixed: personality disorders | Yes | Yes | No | Yes | No | Yes | No |
| Alstrom 1984a | Anxiety: social phobia | No | No | No | Yes | Yes | No | No |
| Alstrom 1984b | Anxiety: agoraphobia | No | No | No | Yes | Yes | No | No |
| Baldoni 1995 | Somatic/medical: urethral syndrome | No | No | No | No | Yes | Yes | No |
| Bressi 2010 | Mixed: depressive and anxiety disorders | Yes | Yes | No | No | No | Yes | No |
| Brom 1989 | Anxiety: PTSD | No | No | No | Yes | Yes | No | No |
| Burnand 2002 | Depression: major depression | No | Yes | Yes | No | Yes | No | No |
| Carrington 1979 | Depression: Feighner Criteria | Yes | No | No | Yes | Yes | No | No |
| Cooper 2003 | Depression: postpartum depression | Yes | No | No | No | Yes | No | No |
| Creed 2003 | Somatic/medical: IBS | Yes | No | No | No | Yes | No | No |
| Dare 2001 | Anorexia nervosa | No | No | No | Yes | Yes/No | Yes | No |
| de Jonghe 2001 | Depression: major depression | Yes | Yes | Yes | No | Yes | No | No |
| Emmelkamp 2006 | Mixed: personality disorders | No | No | No | Yes | Yes | Yes | No |
| Guthrie 1993 | Somatic/medical: IBS | No | Yes | No | No | Yes | No | Yes |
| Guthrie 1999 | Mixed diagnoses: general outpatient referrals | Yes | No | No | No | Yes | No | Yes |
| Guthrie 2001 | Mixed diagnoses: self poisoning presenting to emergency | Yes | No | No | No | Yes | No | Yes |
| Hamilton 2000 | Somatic/medical: functional dyspepsia | Yes | Yes | No | No | Yes | No | Yes |
| Levy Berg 2009 | Anxiety: generalised anxiety disorder | Yes | No | No | Yes | No | No | No |
| Linnet 2001 | Somatic/medical: atopic dermatitis | No | Yes | No | No | Yes | Yes | No |
| Maina 2005 | Mixed: mood and anxiety disorders | Yes | Yes | No | Yes | Yes | Yes | No |
| Maina 2010 | Mixed: OCD and depression | Yes | Yes | Yes | No | Yes | Yes | No |
| Marmar 1988 | Mixed: major depression, PTSD, adjustment disorders | No | Yes | No | Yes | Yes | No | No |
| Milrod 2007 | Anxiety: panic disorder | Yes | Yes | No | Yes | No | No | No |
| Monsen 2000 | Somatic/medical: pain syndromes | No | No | No | No | No | No | No |
| Piper 1990 | Mixed: mood, anxiety, adjustment, axis II | Yes | Yes | No | Yes | Yes | Yes | No |
| Sattel 2012 | Somatic/medical: multisomatoform disorders | Yes | No | No | No | Yes | No | Yes |
| Shefler 1995 | Mixed: anxiety, depression, adjustment disorders | No | Yes | No | Yes | Yes | No | No |
| Sloane 1975 | Mixed: 'psychoneuroses' and axis II | No | No | No | Yes | Yes | No | No |
| Sørensen 2010 | Anxiety: hypochondriasis | No | Yes | No | Yes | Yes | No | No |
| Svedlund 1983 | Somatic/medical: IBS | No | Yes | No | No | Yes | Yes | No |
| Vitriol 2009 | Depression: severe major depression | No | Yes | Yes | No | Yes | No | No |
| Wiborg 1996 | Anxiety: panic disorder | Yes | Yes | Yes | No | Yes | Yes | No |
| Winston 1994 | Mixed: personality disorders | Yes | No | No | Yes | No | Yes | No |
OCD: obsessive‐compulsive disorder; IBS: irritable bowel syndrome; PIT: psychodynamic interpersonal therapy; PTSD: post‐traumatic stress disorder.
2. Subgroup analyses.
| Outcome or subgroup |
Manualised (SMD (95% CI) |
Observer‐rated outcomes (SMD (95% CI) |
Medications on both arms (SMD (95% CI) |
Wait‐list or minimal treatment controls (SMD (95% CI) |
20 or fewer sessions (SMD (95% CI) |
Malan/ Davanloo (SMD (95% CI) |
Hobson/ PIT (SMD (95% CI) |
| 1.1 Reduction in general psychiatric symptoms: short‐term | ‐0.49 (‐0.72 to ‐0.27) | ‐0.87 (‐1.37 to ‐0.37) | ‐0.38 (‐0.59 to ‐0.16) | ‐0.67 (‐0.92 to ‐0.43) | ‐0.69 (‐1.08 to ‐0.30) | ‐1.28 (‐2.06 to ‐0.49) | ‐0.19 (‐0.39 to 0.01) |
| 1.2 Reduction in general psychiatric symptoms: medium‐term | ‐0.09 (‐0.34 to 0.15) | ‐0.37 (‐0.66 to ‐0.08) | ‐0.31 (‐0.66 to 0.04) | ‐0.50 (‐1.01 to 0.01) | ‐0.23 (‐0.44 to ‐0.02) | ‐0.11 (‐0.64 to 0.43) | ‐0.09 (‐0.36 to 0.18) |
| 1.3 Reduction in general psychiatric symptoms: long‐term | ‐0.44 (‐1.26 to 0.39) | ‐2.01 (‐4.29 to 0.27) | ‐0.91 (‐1.56 to ‐0.26) | ‐0.60 (‐1.11 to ‐0.08) | ‐1.51 (‐3.14 to 0.12) | ‐2.73 (‐6.30 to 0.84) | ‐0.06 (‐0.39 to 0.26) |
| 1.4 Reduction in somatic symptoms: short‐term | ‐0.11 (‐0.33 to 0.12) | ‐1.22 (‐3.62 to 1.17) | Not estimable | ‐0.34 (‐0.92 to 0.25) | ‐0.60 (‐1.34 to 0.13) | ‐1.71 (‐5.73 to 2.30) | ‐0.11 (‐0.33 to 0.12) |
| 1.5 Reduction in somatic symptoms: medium‐term | ‐1.91 (‐5.18 to 1.35) | Not estimable | Not estimable | Not estimable | ‐1.58 (‐3.56 to 0.39) | ‐0.94 (‐1.71 to ‐0.17) | ‐1.91 (‐5.18 to 1.35) |
| 1.6 Reduction in somatic symptoms: long‐term | 0.05 (‐0.27 to 0.37) | ‐6.61 (‐7.62 to ‐5.59) | Not estimable | Not estimable | ‐2.21 (‐5.49 to 1.07) | ‐3.38 (‐9.68 to 2.91) | 0.05 (‐0.27 to 0.37) |
| 1.7 Reduction in anxiety symptoms: short‐term | ‐0.45 (‐0.80 to ‐0.10) | ‐0.82 (‐1.43 to ‐0.21) | ‐0.50 (‐1.16 to 0.17) | ‐0.47 (‐0.74 to ‐0.20) | ‐0.74 (‐1.23 to ‐0.25) | ‐0.97 (‐1.90 to ‐0.05) | 0.00 (‐0.27 to 0.27) |
| 1.8 Reduction in anxiety symptoms: medium‐term | ‐0.10 (‐0.34 to 0.14) | ‐0.28 (‐0.56 to ‐0.01) | ‐0.24 (‐0.64 to 0.16) | ‐0.60 (‐1.26 to 0.06) | ‐0.57 (‐1.05 to ‐0.08) | ‐0.83 (‐2.45 to 0.79) | ‐0.13 (‐0.40 to 0.14) |
| 1.9 Reduction in anxiety symptoms: long‐term | ‐0.45 (‐1.12 to 0.23) | ‐1.58 (‐3.37 to 0.21) | ‐0.82 (‐1.47 to ‐0.17) | ‐0.32 (‐0.69 to 0.05) | ‐1.35 (‐2.73 to 0.03) | ‐1.64 (‐3.45 to 0.18) | Not estimable |
| 1.10 Reduction in depressive symptoms: short‐term | ‐0.56 (‐0.81 to ‐0.31) | ‐0.66 (‐0.99 to ‐0.32) | ‐0.43 (‐0.63 to ‐0.23) | ‐0.71 (‐1.20 to ‐0.22) | ‐0.68 (‐0.99 to ‐0.36) | ‐0.93 (‐1.16 to ‐0.70) | ‐0.26 (‐0.45 to ‐0.06) |
| 1.11 Reduction in depressive symptoms: medium‐term | ‐0.14 (‐0.34 to 0.07) | ‐0.57 (‐1.00 to ‐0.14) | ‐0.51 (‐0.99 to ‐0.04) | ‐0.29 (‐0.79 to 0.22) | ‐0.33 (‐0.61 to ‐0.05) | ‐1.40 (‐2.22 to ‐0.59) | ‐0.20 (‐0.44 to 0.04) |
| 1.12 Reduction in depressive symptoms: long‐term | ‐0.26 (‐0.93 to 0.41) | ‐0.41 (‐0.75 to ‐0.06) | ‐0.65 (‐1.29 to ‐0.01) | ‐0.35 (‐0.86 to 0.16) | ‐1.00 (‐2.22 to 0.21) | ‐1.59 (‐3.61 to 0.44) | Not estimable |
CI: confidence interval; PIT: psychodynamic interpersonal therapy; SMD: standardised mean difference.
Sensitivity analyses
a) Manualised therapies
When restricting analyses to studies using manualised treatments, there were smaller effects in most outcome categories compared with studies of the overall set of studies.
b) Studies that gave observer‐rated outcomes
The effect sizes were larger compared with those of the overall review studies in most outcome categories when analyses were restricted to studies that included observer ratings.
c) Studies that used medications on both treatment arms
When analyses were restricted to studies with medication on both treatment arms, effect sizes were generally smaller than the effects of the overall set of studies.
Subgroup analyses
a) Therapy of up to 20 sessions
When analyses were restricted to studies that averaged 20 or fewer sessions, measures of general symptoms in medium‐term, social adjustment and interpersonal problems were smaller compared with studies where treatment was over 20 sessions.
b) Studies that used minimal treatment or wait‐list controls as opposed to treatment as usual controls
Anxiety effect sizes were smaller when analyses were restricted to studies with minimal contact or wait‐list controls. Otherwise, there were no differences in degrees of significance or effect sizes compared with studies using treatment as usual controls.
c) Effects of short‐term psychodynamic psychotherapy treatment models
As a post hoc analysis, we examined outcomes by STPP treatment approach where five or more studies were available.
When analyses were restricted to models derived from Hobson or PIT (six studies), effects across all outcomes were smaller than studies using the Malan/Davanloo short‐term dynamic psychotherapy model (11 studies) with the exceptions of general symptoms at medium‐term and somatic symptom at medium‐term follow‐up. The effects of Hobson/PIT studies were negligible to small in all the other categories. In contrast, the effects of analyses restricted to Malan/Davanlo studies were large in all but general symptoms at medium‐term follow‐up.
d) Differences in outcomes between different diagnostic groups
People diagnosed with somatoform disorders had the greatest effects sizes in most outcome categories except general symptoms at medium‐term and somatic symptoms at medium‐term follow‐up. People diagnosed with depression tended to have the lowest effects on measures of anxiety and depression. See Data and analyses.
Assessing publication bias: funnel plot analysis
We explored funnel plots as an indication of publications bias. The largest number of studies available was in each of the short‐term outcome measures. Each of these had funnel plots that had some features of an inverted funnel (somatic) or had studies with similar standard errors (anxiety, depression), leaving a flat but dispersed distribution. Other categories had too few studies to allow an interpretation. Thus, we could not draw definitive conclusions about publication bias using this method.
Discussion
Summary of main results
This meta‐analysis of 33 RCTs of STPP comprised of 2173 participants found it to have modest to large effects relative to controls across a broad range of CMDs. With the exception of somatic measures in the short‐term, these effects were also statistically significant in short‐ and medium‐term follow‐ups while not reaching significance in long‐term follow‐up in some outcome categories. Benefits were observed across a broad range of outcome measures including general measures and somatic symptoms, as well as depression, anxiety, interpersonal and social adjustment. Individual studies also reported reduced self injury and weight gain in anorexia nervosa, suggesting behavioural as well as symptomatic gains. Studies also reported occupational gains and cost benefits. Combined, these findings provide converging evidence of treatment benefits. In each of somatic symptoms, depressive symptoms, anxiety, general symptoms, social adjustment and interpersonal problems, the treatment effect sizes were greater in long‐term follow‐up than in short‐term follow‐up suggesting accrued gains over time though some of this effect may have been from different studies reporting at different time intervals (i.e. short‐ versus long‐term follow‐up periods).
Study quality was variable in these studies, which spanned 1975 to 2012. Although STPP method (e.g. Hobson versus Malan/Davanloo) appeared to impact outcomes, it is yet to be determined if these effects are better accounted for by common (e.g. therapist training, adherence, allegiance effects) or specific (e.g. emotional experiencing, intellectual insight) factors. Heterogeneity and loss of significance of some measures in follow‐up suggest these results be interpreted with caution.
Overall completeness and applicability of evidence
This review found preliminary evidence that STPP may be effective for a broad range of CMDs as are seen in mental health and medical clinics. Common specific psychiatric conditions including major depression, somatic symptom disorders, eating disorders, anxiety disorders and personality disorders were treated in these studies.
Several studies included treatment resistant, severe and character‐disordered participants, which are challenging‐to‐treat patient groups. Treatment effects in these groups may be lower than what may be expected in samples without such resistance or complexity. Thus, these studies may underestimate the effects of this brief treatment. This is an important finding since these patient groups are common in clinical populations where half or more do not reach remission with first‐line psychotropic medication or talking therapies. These problems are costly to the system as they induce prolonged disability from work and excess hospital and medical service use, so, brief and relatively low‐cost treatment options are necessary and welcome.
The number of studies in many analyses was relatively small making comparisons across diagnostic groups and other subgroup analyses difficult. The diversity of the samples and treatment methods likely contributed to heterogeneity, which influences our ability to interpret these groups of studies. However, this diversity is also a strength of this literature implying the range of methods in STPP may be broadly applied in clinical populations.
Quality of the evidence
Study quality
The studies were of variable quality. Manuals and adherence measures were not employed in each study calling into question the quality of psychotherapy provided. Therapist experience was in question in many studies, raising the chance that the therapy was not provided in an optimal fashion. It was apparent in one study that the STPP provided was restricted to withhold key interventions likely weakening its effects and underestimating its benefits.
As noted, some studies had high internal risk of bias in the categories described and many had insufficient information to rate using The Cochrane Collaboration's 'Risk of bias' tool. In future reviews, we will adapt the 'Risk of bias' tool to incorporate features such as the use of adherence ratings, the use of observer ratings, the use of manuals, therapist experience and researcher allegiance to enable measurement of psychotherapy quality. In this study, subgroup analyses pointed towards reduced effects when restricting to studies using manuals and increased effects in studies using observer ratings.
Diagnostic criteria
The lack of specific diagnostic criteria in a few studies and the use of mixed samples may limit the clinician's ability to determine suitability of STPP for individual patients in his or her practice. This is less of an issue in studies performed in the past 20 years versus before.
Treatment methods
Although common psychotherapy factors are the core of the treatment (Blagys 2000), many therapy directions are possible. In subgroup analyses, we saw a signal of differential effects between two commonly used models. The methods were both STPP models but one (Malan/Davanloo) was primarily focused on emotional experiencing, a factor that relates to outcome in some STPP meta‐analyses (Abbass 2009; Diener 2007). However, such differences may be from many causes, such as variation in levels of therapist experience, participant samples and research methods rather than from methods inherent in the models.
A further issue is that the quality of the STPP provided (e.g. therapist experience, use of manual, use of adherence ratings) varied between studies raising the probability that STPP may have been provided suboptimally in some of the included studies. Therefore, the efficacy of STPP may have been underestimated in this meta‐analysis. Indeed, Leichsenring 2004 found greater effect sizes with his sample of STPP studies that were selected for quality of, and validation of, treatment provided. However, given the option of excluding studies of questionable therapy technique, we decided to include all studies meeting our basic criteria. Our decision was to be cautious to avoid a possible selection bias where information was lacking or vague regarding these parameters.
Study heterogeneity
The significant heterogeneity in 10 of the 16 analyses was a concern and suggests our findings must be treated with caution in these cases. Because of this, we have reported results of the random‐effects model in these cases and verified the effects using the random‐effects model in other cases. The above‐noted methodological and treatment variability account for some of the observed heterogeneity of outcomes. Differences in the control conditions (i.e. treatment as usual versus wait list versus minimal treatment) may have brought more or less treatment effects in these studies leading to inter‐study variability as illustrated by our subgroup analyses. Another factor that probably contributed was the collection of diverse patient populations with a broad range of physical and psychological symptoms including depression, anxiety, personality problems and diverse somatic conditions.
Arguably, studies included in this review should include people with clear and specific diagnoses while excluding other confounding diagnoses. However, these studies reflect the heterogeneity and complexity of people with multiple problems including symptom, somatic and personality disorders who present to all healthcare settings. Thus, this body of studies may tell us more about the real‐world utility of STPP, than would a highly selected sample of participants who often do not exist in public and private psychotherapy clinics.
Potential biases in the review process
We have performed this review in ways to reduce the chances of bias where possible. First, if anything, we have leaned towards being over‐inclusive of studies so as not to exclude any RCT study of any STPP model. This led us to include STPP studies with medications on both arms, studies of ill‐defined STPP models, studies of poor quality and older studies when the method was not well developed. Thus, one possible source of bias was possible over‐inclusiveness due to the breadth of our inclusion criteria. Second, we collectively, in pairs, selected studies. Third, we extended the team to include expert review authors with no affiliation to any variety of psychotherapy, and colleagues who research in long‐term dynamic psychotherapy. Finally, analyses were performed or verified by a review author with no affiliation to psychotherapy.
As noted, we have reported results of the random‐effects model in cases with significant heterogeneity and verified the effects using the random‐effects model when we did not find statistical heterogeneity. As noted, there are several likely sources of heterogeneity, and this will not be likely to change between now and the next time we update this review. Hence, we are going to reconsider an approach to best examine these studies before the next update.
Other possible sources of bias include the inclusion of studies with medication on both arms, which may have lowered the effects of STPP relative to those studies without medication on both arms (Table 2). This and other subgroup analyses showing outcome differences highlight hypothetical outcome factors that can be tested in future research. A few studies (e.g. Baldoni 1995; Creed 2003; Wiborg 1996) in general outcome measures provided data at long‐term follow‐up but not at short‐term follow‐up in some outcome categories: this could increase or decrease relative long‐term outcome effects versus short‐term outcome effects. As a result of this and limited numbers of medium‐term follow‐up data, we are considering collapsing short and medium term into one group when we next update this review.
The original protocol called for exclusion of studies with over 20% attrition, introducing a possible bias. In the next update of the review, this criteria will no longer be in effect; rather we will rate techniques of handling attrition and evaluate the effects of this using the 'Risk of bias' tool.
Agreements and disagreements with other studies or reviews
Comparison to other meta‐analyses
Overall, this review is in line with other meta‐analyses and reviews of STPP since 2007 that have reported moderate to large and sustained or increased gains across diverse clinical populations. These reviews tended to focus on specific diagnostic groups. Some included non‐randomised controlled trials and some provided combined pre‐versus‐post analyses, post‐versus‐post analyses and subgroup analyses including only RCTs. Overall these studies, with various limitations, found moderate to large and sustained effects within categories of depression (Driessen 2010), somatic disorders (Abbass 2009), personality disorders (Town 2011), and combined personality disorder‐depression (Abbass 2011). The common limitations were heterogeneity, small samples in some subgroup analyses and wide ranges of study quality. In 2012, the largest published psychodynamic psychotherapy meta‐analysis to date likewise found significantly increased gains in follow‐up compared with immediately post treatment in a group of 46 studies of psychodynamic therapies, most all of which were STPP models (Town 2012). Our findings also parallel the most recent review of psychodynamic therapies in specific disorders (Leichsenring 2014).
Lazar and colleagues published a review of all psychological therapy cost‐effectiveness studies in a 2010 book and noted growing evidence for cost effectiveness of the treatment overall (Lazar 2010). The results of our review support the concept of an inexpensive talking approach that could potentially provide cost reduction in diverse populations.
Authors' conclusions
Implications for practice.
We have attempted to draw modest conclusions, based on the available evidence and to highlight areas requiring further study rather than draw conclusions that may not be based on evidence of high quality. Short‐term psychodynamic psychotherapies (STPP) may be effective for a very broad range of common mental disorders (CMD), with evidence of modest to large treatment effect sizes that increase in long‐term follow‐up. This finding supports STPP as a candidate treatment for the majority of non‐psychotic and non‐organic psychotherapeutic presentations. However, given the limited data, loss of significance in some measures at long‐term follow‐up and heterogeneity between studies, these findings should be interpreted with caution.
Although cost comparisons were not made in this review, it should be noted that these therapies are relatively short and much less expensive than long‐term psychotherapy models. The observed reduction in symptoms may contribute to observed reductions in healthcare use, costs and improved occupational functioning noted in individual studies. STPP may represent an economical approach to problems as complex as chronic pain, personality disorder, panic disorder, self induced poisoning and other challenging‐to‐treat conditions. They are also less expensive than even one year of some psychotropic medications, depending on who is delivering the therapy and the setting (public versus private pay). While all people with CMD do not respond to STPP or any other short therapy, it is prudent to consider such relatively low‐risk talking approaches before medications, treatment combinations or more invasive procedures such as electroconvulsive therapy are employed (e.g. Malhi 2009).
Implications for research.
Future research in these approaches should aim to improve study quality using specific treatment manuals, videotaped adherence rating (as in Abbass 2008;Milrod 2007; and Winston 1994), cost‐benefit measures and treatment‐specific, experienced therapists. More studies would also tend to reduce the heterogeneity observed here. More future studies should also focus on specific diagnostic categories to allow clinicians evidence with which to consider these treatments for specific populations. Studies should also examine specific treatment factors, such as emotional focus, and their contributions to outcomes across therapy models. There are signs of more studies in this since 2006 and overall study quality and diagnostic specificity appear to have improved.
What's new
| Date | Event | Description |
|---|---|---|
| 4 April 2014 | New citation required but conclusions have not changed | Review updated |
| 4 April 2014 | New search has been performed | Review updated with newer methodology and new studies incorporated |
History
Protocol first published: Issue 2, 2004 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 6 November 2008 | Amended | Converted to new review format. |
| 21 August 2006 | New citation required and conclusions have changed | Substantive amendment |
| 9 November 2005 | Amended | A minor update was submitted for publication in November 2005 |
Acknowledgements
This review team acknowledges the support of the Nova Scotia Department of Health and the Dalhousie University Department of Psychiatry. The original review was supported by a grant from Cochrane, Canada.
Appendices
Appendix 1. Other electronic searches: CENTRAL
#1 ANXIETY #2 DEPRESSION #3 (PANIC next DISORDER) #4 (DEPRESSIVE next DISORDER) #5 (DEPRESSIVE next SYMPTOMS) #6 (ANXIOUS next SYMPTOMS) # 7 (SOMATIZATION next SYMPTOMS) # 8 (SOMATIZATION next SYMPTOMS) #9 (SOMATIZATION next DISORDER) #10 (SOMATIZATION next DISORDER) #11 (SOMATOFORM next SYMPTOMS) #12 (SOMATOFORM next SYMPTOMS) #13 (((((#1 or #2) or #3) or #4) or #5) or #6) or #7) or #8) or #9) or #10) or #11) or #12) #14 (BRIEF next PSYCHODYNAMIC) #15 (BRIEF next DYNAMIC) #16 (TIME‐LIMITED next PSYCHODYNAMIC) #17 (TIME‐LIMITED next DYNAMIC) #18 (BRIEF next PSYCHOANALYTIC) #19 (BRIEF next ANALYTIC) #20 (TIME‐LIMITED next PSYCHOANALYTIC) #21 (TIME‐LIMITED next ANALYTIC) #22 (((((((#14 or #15) or #16) or #17) or #18) or #19) or #20) or #21)#19 (#13 and #22)
Data and analyses
Comparison 1. STPP versus wait‐list/treatment as usual/minimal treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reduction in general psychiatric symptoms: short‐term | 19 | 1424 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.00, ‐0.41] |
| 1.1 anxiety disorders | 2 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.72, 0.05] |
| 1.2 depressive disorders | 3 | 281 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.67, ‐0.19] |
| 1.3 somatoform disorders | 4 | 419 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.24 [‐2.68, 0.20] |
| 1.4 mixed disorders | 8 | 483 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.77, ‐0.22] |
| 1.5 personality disorders | 2 | 134 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.98 [‐1.34, ‐0.62] |
| 2 Reduction in general psychiatric symptoms: medium‐term | 5 | 437 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.46, ‐0.08] |
| 2.1 depressive disorders | 1 | 71 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐0.94, 0.00] |
| 2.2 somatoform disorders | 2 | 251 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.45, 0.05] |
| 2.3 mixed disorders | 2 | 115 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.68, 0.06] |
| 3 Reduction in general psychiatric symptoms: long‐term | 4 | 344 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.51 [‐3.14, 0.12] |
| 3.1 anxiety disorders | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.56, ‐0.26] |
| 3.2 somatoform disorders | 2 | 243 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐6.69, 2.11] |
| 3.3 mixed disorders | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.11, ‐0.08] |
| 4 Reduction in somatic symptoms: short‐term | 8 | 744 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.29, 0.04] |
| 4.1 anxiety disorders | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.92, 0.25] |
| 4.2 somatoform disorders | 6 | 599 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.63, 0.19] |
| 4.3 mixed disorders | 1 | 99 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.77, 0.02] |
| 5 Reduction in somatic symptoms: medium‐term | 4 | 359 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.39 [‐2.75, ‐0.02] |
| 5.1 somatoform disorders | 3 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.04, ‐0.11] |
| 5.2 mixed disorders | 1 | 76 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.60 [‐4.34, ‐2.86] |
| 6 Reduction in somatic symptoms: long‐term | 3 | 280 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐5.49, 1.07] |
| 6.1 somatoform disorders | 3 | 280 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐5.49, 1.07] |
| 7 Reduction in anxiety symptoms: short‐term | 18 | 1102 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.02, ‐0.26] |
| 7.1 anxiety disorders | 6 | 255 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.01, ‐0.27] |
| 7.2 depressive disorders | 1 | 87 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.71, 0.13] |
| 7.3 somatoform disorders | 5 | 435 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐2.25, 0.37] |
| 7.4 mixed disorders | 5 | 287 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.91, ‐0.03] |
| 7.5 personality disorders | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.46, 0.83] |
| 8 Reduction in anxiety symptoms: medium‐term | 7 | 506 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.77, ‐0.16] |
| 8.1 anxiety disorders | 1 | 21 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐2.02, ‐0.12] |
| 8.2 depressive disorders | 1 | 87 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.83, 0.02] |
| 8.3 somatoform disorders | 3 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.42, 0.05] |
| 8.4 mixed disorders | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.56, 0.18] |
| 9 Reduction in anxiety symptoms: long‐term | 5 | 293 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐2.24, 0.04] |
| 9.1 anxiety disorders | 2 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.12, 0.23] |
| 9.2 somatoform disorders | 2 | 131 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.04 [‐4.77, 0.69] |
| 9.3 mixed disorders | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.02, ‐0.00] |
| 10 Reduction in depressive symptoms: short‐term | 18 | 1415 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐0.61, ‐0.39] |
| 10.1 anxiety disorders | 2 | 89 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.57 [1.00, ‐0.14] |
| 10.2 depressive disorders | 5 | 435 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐0.67, ‐0.28] |
| 10.3 somatoform disorders | 5 | 503 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.58 [‐0.77, ‐0.39] |
| 10.4 mixed disorders | 6 | 388 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.41 [‐0.62, ‐0.21] |
| 11 Reduction in depressive symptoms: medium‐term | 7 | 601 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.60, ‐0.09] |
| 11.1 depressive disorders | 3 | 257 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.60, 0.07] |
| 11.2 somatoform disorders | 3 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.28, 0.10] |
| 11.3 mixed disorders | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.79, 0.22] |
| 12 Reduction in depressive symptoms: long‐term | 5 | 321 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐2.22, 0.21] |
| 12.1 anxiety disorders | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.29, ‐0.01] |
| 12.2 depressive disorders | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.38, 0.46] |
| 12.3 somatoform disorders | 2 | 131 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.06 [‐5.12, 1.01] |
| 12.4 mixed disorders | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.86, 0.16] |
| 13 Social adjustment: short‐term | 9 | 720 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.51 [‐0.66, ‐0.36] |
| 13.1 anxiety disorders | 3 | 141 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [1.00, ‐0.31] |
| 13.2 depressive disorders | 2 | 246 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.38 [‐0.63, ‐0.13] |
| 13.3 somatoform disorders | 1 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.58 [‐0.98, ‐0.18] |
| 13.4 mixed disorders | 1 | 99 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐0.62, 0.17] |
| 13.5 personality disorders | 2 | 134 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐1.15, ‐0.44] |
| 14 Social adjustment: long‐term | 3 | 199 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.58 [‐0.86, ‐0.29] |
| 14.1 anxiety disorders | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.27, 0.01] |
| 14.2 somatoform disorders | 1 | 99 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐0.99, ‐0.18] |
| 14.3 mixed disorders | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.53 [‐1.04, ‐0.01] |
| 15 Interpersonal problems: short‐term | 6 | 265 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐0.67, ‐0.17] |
| 15.1 anxiety disorders | 2 | 59 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.56, 0.49] |
| 15.2 depressive disorders | 1 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐0.81, 0.08] |
| 15.3 somatoform disorders | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.93, 0.31] |
| 15.4 mixed disorders | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.85 [‐1.38, ‐0.32] |
| 15.5 personality disorders | 1 | 27 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.47, 0.09] |
| 16 Interpersonal problems: long‐term | 3 | 85 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.49 [‐0.92, ‐0.05] |
| 16.1 anxiety disorders | 2 | 46 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.48 [‐1.08, 0.12] |
| 16.2 somatoform disorders | 1 | 39 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐1.14, 0.14] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abbass 2008.
| Methods | Multicentre RCT of 2 parallel conditions | |
| Participants | 27 participants referred from physicians or mental health professionals Inclusion criteria: aged 18‐70 years, ≥ 1 DSM IV Personality Disorder. People with co‐morbid non‐psychotic symptom disorders were acceptable Exclusion criteria: psychosis, organic brain syndrome, mental retardation, current substance dependence, acute suicidal behaviour, violent behaviour, no new psychotropic medication in the previous 3 months |
|
| Interventions | Intervention: intensive STDP, manualised, based on Davanloo 2000 Control: minimal contact wait‐list (mean duration 14.8 weeks) 5 therapists with over 5 years training and experience in ISTDP. Mean number of sessions 27.7. All sessions videotaped, adherence rated through sampling of videotapes using adherence rating scale | |
| Outcomes | BSI, IIP, GAF Symptoms and Social Occupational, medication use and cost, work hours and function, all measured at pre therapy, post therapy, and at 1 and 2 year follow‐up | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomized and stratified by age and sex...randomised cards were used so the screener was blind to the allocation before selection of a card" Comment: randomised cards |
| Allocation concealment (selection bias) | Low risk | Comment: additional information provided by lead author indicating the use of randomised cards in sealed envelopes thus minimising risk of bias |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: no psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible Primary measures: self reports (BSI, IIP): low risk Insufficient information on blinding of clinician ratings of GAF‐S, therefore overall bias considered unclear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 1 drop‐out only and ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Alstrom 1984a.
| Methods | Single‐centre RCT, between 1973 and 1979, parallel design with 4 arms | |
| Participants | Inclusion criteria: 18‐60 years old, sought help for social phobia at outpatient services Exclusion criteria: any form of continuous treatment for the previous 6 months; drug abuse; dementia; neurological signs of brain damage; symptoms of endogenous depression, schizophrenia, obsessive‐compulsive neurosis or mental retardation; poor knowledge of Swedish language. Study included 42 social phobic men and women. They were all assessed as not suitable for insight‐oriented psychotherapy |
|
| Interventions | Common to each group ‐ psychoeducation, information on prolonged exposure in vivo, encouragement to participate in anxiety‐provoking situations. Participants could continue to take medications
Control: basal therapy ‐ included the above, and meetings once a month for 20‐30 min Intervention 1: behavioural therapy (prolonged exposure in vivo) Intervention 2: relaxation therapy Intervention 3: psychodynamically oriented supportive therapy, based on Dewald 1964, 30‐min appointments once/week for 3 months (˜ 12 appointments). No mention of manual for therapy, measures of therapist adherence |
|
| Outcomes | Measured pre‐treatment, end (post‐) treatment, and 9 months follow‐up Measures were scales constructed by the study authors to measure indirect manifestations of anxiety (target phobia, other phobias, OCD symptom), direct manifestations of anxiety, ego‐restriction and social functions, and a global rating. In addition, intellectual ability was measured with the Synonyms Reasoning Block test, personality with the Eysenck Personality Inventory, and the Cesarec‐Marke Personality Schedule. Therapist rated measures | |
| Notes | Free anxiety measures and global symptom data used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: inadequate description |
| Allocation concealment (selection bias) | Unclear risk | Comment: inadequate description |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: therapists outcome ratings (free anxiety and global symptoms) were unblinded thus considered a high risk of detection bias Blinding participants to treatment group not possible No psychotherapist was blinded to the treatment delivered |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: all participants completed treatment but only 8/10 in the control group provided follow‐up data |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Alstrom 1984b.
| Methods | Single‐centre RCT, between 1973 and 1979, parallel design with 4 arms | |
| Participants | Inclusion criteria: 18‐60 years old, sought help for agoraphobic syndromes at outpatient services Exclusion criteria: any form of continuous treatment for the previous 6 months; drug abuse; dementia; neurological signs of brain damage; symptoms of endogenous depression, schizophrenia, obsessive‐compulsive neurosis or mental retardation; poor knowledge of Swedish language. Study included 73 agoraphobic women. They were all assessed as not suitable for insight‐oriented psychotherapy |
|
| Interventions | Common to each group ‐ psychoeducation, information on prolonged exposure in vivo, encouragement to participate in anxiety‐provoking situations. Participants could continue to take medications
Control: basal therapy ‐ included the above, and meetings once a month for 20‐30 min Intervention 1: behavioural therapy (prolonged exposure in vivo) Intervention 2: relaxation therapy Intervention 3: psychodynamically oriented supportive therapy, based on Dewald 1964, 30‐min appointments once/week for 3 months (˜ 12 appointments). No mention of manual for therapy, measures of therapist adherence |
|
| Outcomes | Measured pre‐treatment, end (post‐) treatment, and 9 months follow‐up Measures were scales constructed by the authors to measure indirect manifestations of anxiety (target phobia, other phobias, OCD symptom), interpersonal relations, direct manifestations of anxiety, ego‐restriction and social functions, and a global rating. In addition, intellectual ability was measured with the Synonyms Reasoning Block test, personality with the Eysenck Personality Inventory, and the Cesarec‐Marke Personality Schedule. Therapist rated measures. Global scale and free anxiety measures were used in this review | |
| Notes | Both Alstrom 1984a and Alstrom 1984b in this review used the same methods Free anxiety measures, interpersonal relations and global symptom data used. Could not use 9‐month follow‐up data as more than 20% of sample lost to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: inadequate description |
| Allocation concealment (selection bias) | Unclear risk | Comment: inadequate description |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: therapists were raters of some cases and may have been unblinded: high risk Blinding participants to treatment group not possible No psychotherapist was blinded to the treatment delivered |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: significant dropout rate (12/73 participants) but how handled was not described |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Baldoni 1995.
| Methods | Single‐centre RCT, 2‐year study, parallel design | |
| Participants | 36 women with urethral syndrome (urinary symptoms and pain without organic lesions) aged 18‐63 years (mean 40). All complained of urgency, dysuria and tenesmus at the first evaluation | |
| Interventions | Intervention: STDP (Davanloo 1980; Malan 1979). The psychotherapy consisted of 12‐16 weekly sessions lasting 1 hr conducted by a single psychotherapist Control: "traditional urological treatment", which included medical therapy (anticholinergic and alpha‐adrenoceptor antagonist drugs) and urethral dilation Both groups had 3‐4 months of therapy for a mean of 14 weeks |
|
| Outcomes | Pre‐, 6 months post‐, 4 years post‐treatment. Presence and nature of urinary disorders such as urgency, dysuria, tenesmus; number of day and night micturitions; pain in the pelvic area and its features; the Symptom Questionnaire, which can discriminate between psychiatric patients and others and between various psychological discomfort levels by assessing anxiety, depression, somatic symptoms and hostility. Continuous data from Symptom Questionnaire used as obtained from authors | |
| Notes | 4 participants allocated to STDP group were given antidepressant pharmacotherapy (a combination of amitriptyline and mianserin) but 2 stopped treatment before completion and are not considered in the results Data obtained from authors in form of means, standard deviations for outcomes of interest: anxiety, depression and somatic symptoms of Symptom Questionnaire | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "randomly selected on the basis of the psychotherapist's schedule. i.e. when a treatment could be started, the urologists were asked to send the first patient" Comment: sequence generated by a non‐random approach |
| Allocation concealment (selection bias) | High risk | Comment: not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report questionnaires only: low risk Blinding participants to treatment group not possible No psychotherapist was blinded to the treatment delivered |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: did not include drop‐outs in analysis but reported on clinical status |
| Selective reporting (reporting bias) | High risk | Comment: did not include complete outcome data on all measures for entry in a meta‐analysis |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Bressi 2010.
| Methods | Single‐centre RCT, 1‐year study, parallel design | |
| Participants | 30 participants were each randomised to receive STPP or TAU Inclusion criteria: 18‐60 years old with a main diagnosis of an anxiety disorder or depressive disorder; participants were not to have been on psychotropic medication for a period of at least 2 weeks (4 weeks for monoamine oxidase inhibitors). Exclusion criteria: mental retardation; history of organic mental disorders, schizophrenia, bipolar disorders or substance use; severe axis II personality disorder; currently undergoing treatment. An independent interview confirmed DSM IV ‐ TR diagnoses using the SCID |
|
| Interventions | Intervention: STPP derived from Malan 1976 and Malan 1992 based on a 40‐session treatment plan. Therapists were 4 psychiatrists with experience (12.3 mean years) in STPP. Therapists received weekly individual and group supervision and were given verbatim transcripts of sessions. Adherence was rated and additional supervision provided when STPP techniques were not being applied. Treatment sessions were audio‐recorded. Concomitant psychotropic medication was only allowed for the first 3 weeks of the study Control: TAU consisted of routine psychiatric treatment: drug treatment (selective serotonin reuptake inhibitors/serotonin noradrenaline (norepinephrine) reuptake inhibitors) and ongoing clinical interviews with a minimum of 1 session per month of and a maximum of 4 sessions a month for 40 weeks. Interviews monitored drug treatment (compliance, side effects, dose adjustment) and general clinical state |
|
| Outcomes | Primary outcome measures included the Clinical Global Impression Scale, the SCL‐90‐R, and the SCL‐90‐GSI. The IIP was included as a measure of interpersonal functioning. Measures were completed at recruitment and 12‐months post admission | |
| Notes | IIP, SCL‐90‐GSI, anxiety and depression subscales used in analyses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "block randomization...then randomly allocated using computer generated random number" Comment: selection bias unlikely |
| Allocation concealment (selection bias) | Unclear risk | Quote: "block randomization...then randomly allocated using computer generated random number" Comment: no further details; therefore, insufficient information to conclude on concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report data (IIP, SCL‐90‐GSI and anxiety and depression subscales) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "intention‐to‐treat analysis was performed...observation carried forward for participants who did not complete the trial" Comment: ITT controlled for incomplete data. 80% completed the trial, with equal non‐completers across groups |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Brom 1989.
| Methods | RCT with 4 parallel conditions | |
| Participants | 112 participants diagnosed with PTSD with DSM‐III criteria, with the condition that not more than 5 years had elapsed since the incurring event. Recruited through a general assessment with 1 of the study authors, and a further interview to ensure the participant could cope with a confronting therapy. Aged 18‐73 years (mean 42.0), 79% were women, 21% were men | |
| Interventions | Intervention 1: trauma desensitisation (mean length of treatment 15.0 sessions) Intervention 2: hypnotherapy (mean 14.4 sessions) Intervention 3: brief psychodynamic therapy (mean length 18.8 sessions) based on Horowitz 1976 Control: wait‐list group (4 months long) |
|
| Outcomes | Pre‐, post‐ and 3 months post‐treatment. SCL‐90, with 5 subscales; STAI; State‐Trait Anger Inventory; Dutch Personality Questionnaire; Introversion‐Extroversion scale of the Amsterdam Biographical Questionnaire; scale for internal vs. external control | |
| Notes | SCL‐90 total score and STAI data used in the review Unable to use personality data as it was reported only into subscales | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self reports used (SCL90, STAI, Stait Trait Anger Inventory): low risk No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: even distribution of drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Burnand 2002.
| Methods | 10‐week, single‐centre RCT, with 2 parallel arms | |
| Participants | From 110 eligible participants, 95 were randomised to either the experimental or control group. Consecutively referred from acute outpatient clinic, aged 20‐65 years Inclusion criteria: diagnosis of MMD confirmed using the SCID, with HDRS score > 20 Exclusion criteria: bipolar disorder, psychotic symptoms, severe substance dependence, organic disorder, intolerance to clomipramine |
|
| Interventions | Intervention: Intensive nursing care plus 10 sessions of STPP provided by experienced nurses. Control: Intensive nursing plus clomipramine plus supportive care including individual sessions aimed at providing empathic listening, guidance, support, and facilitation of an alliance by one carefully designated caregiver. |
|
| Outcomes | Depression severity was measured at intake and termination using the SCID, HRSD and the Health Sickness Rating Scale. Outcome data were also collected on the GAS and hospital days and sick days were independently recorded | |
| Notes | GAS total score and HAM‐D rating used in this review. GAS scores required reversing for analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no reference to sequence generation method: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Quote: "random assignment process included stratification by presence of personality disorders..." Comment: no further details therefore insufficient details |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "All raters were independent...[however]...individuals who rated the presence and severity of major depression and HSRS score at 10 weeks were not blinded to treatment assignment" Comment: high risk of detection bias due to raters not being blinded to treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 22% excluded from analyses because they did not begin treatment, mostly due to exclusion characteristics. This was similar across group, and ITT analyses were conducted |
| Selective reporting (reporting bias) | High risk | Comment: ≥ 1 outcomes of interest were reported incompletely so that they cannot be entered in a meta‐analysis (e.g., HAM‐D not provided at discharge) |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Carrington 1979.
| Methods | RCT of STPP (Mann 1973) versus cognitive therapy and wait‐list controls | |
| Participants | Inclusion criteria: African‐American women with depression (Feighner Criteria), BDI of 20‐40, aged 20‐50 years Exclusion criteria: hallucinations or delusions, substance addiction and antisocial personality |
|
| Interventions | Intervention: STPP 12 x 50‐min sessions according to Mann's time‐limited model (Mann 1973) Control: wait‐list Psychotherapy provided by doctoral level graduate psychology students with variable but relatively little experience Supervision was provided in groups Treatment adherence rated from audiotapes |
|
| Outcomes | Self report ratings were used including the BDI, Beck Hopelessness Scale. VAS | |
| Notes | BDI used as primary depression measure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report only. Low risk No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes. ≥ 1 outcomes of interest reported incompletely; however, additional data obtained from study authors |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Cooper 2003.
| Methods | Single‐centre RCT | |
| Participants | Large consecutive series of 3222 primiparous women identified through birth records of Addenbrooke's Hospital, Cambridge, UK, screened between January 1990 and August 1992 for mood disturbance in the early post‐partum period, using postal administration of EPDS. EPDS score of ≥ 12 assessed; women with PPD invited to take part Inclusion criteria: 15‐mile radius to hospital, English as first language Exclusion: delivered prematurely, if infant had any gross congenital abnormality, if they did not have a singleton birth or were intending to move out of the area during the study period 206 women identified; 193 agreed to take part |
|
| Interventions | Women assigned to 1 of 4 conditions Intervention 1: CBT Intervention 2: psychodynamic therapy (as described by Cramer 1990; Stern 1995) Intervention 3: non‐directive counselling Control: "routine primary care" Therapy was conducted in women's homes on a weekly basis from 8 to 18 weeks post‐partum There were 6 study therapists: specialist in each of the 3 research treatments and 3 non‐specialists A Therapist Rating Scale was administered to participant to measure adherence to treatment |
|
| Outcomes | Follow‐up at 4.5, 9 and 18 months. 5‐year follow‐up for women who had completed therapy Symptoms of depression, as measured using the EPDS. Also, measures of infant‐mother attachment and behaviour | |
| Notes | Primary care condition used as minimal treatment control EPDS data used in depression outcome of review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "allocated randomly to a treatment group by the study recruiter, who drew one of four coloured balls from a bag" |
| Allocation concealment (selection bias) | High risk | Quote: "...the assignment of each therapy to a different coloured ball having been defined at the start of the study and maintained until the end" Comment: concealment not blinded; therefore, high risk of bias |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report data (EPDS) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: incomplete data (> 20%) at 5‐year follow‐up; however, comparison between completer only analyses versus ITT aimed to address attrition bias in respect to drop‐out |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Creed 2003.
| Methods | Multicentre RCT with 3 parallel conditions. Participants were stratified by hospital and severity | |
| Participants | 257 adults with severe IBS recruited from gastroenterology clinics Inclusion criteria: Rome I criteria for IBS satisfied, IBS symptoms > 6 months, failure to respond to usual medical treatment for ≥ 3 months, severe abdominal pain, no contraindications to psychotherapy or paroxetine, ability to complete questionnaires, aged 18‐65 years |
|
| Interventions | Intervention 1: PIT based on Hobson 1985, manualised, for 1 long, 2‐hr session, and 7, 45‐min sessions over 3 months Intervention 2: paroxetine 20 mg orally each day for 3 months Control: 'TAU', continuing to see gastroenterologist or GP for duration of study For the psychotherapy or paroxetine groups, after 3 months they returned to GP to decide on further management |
|
| Outcomes | Trial entry, 3 months, 1‐year post‐treatment. IBS symptoms ‐ VAS of severity of abdominal pain, record of days of pain, change in symptoms. SF‐36 (health related quality of life), GSI of SCL‐90, healthcare costs, utilisation | |
| Notes | VAS scale data for abdominal pain used for somatic symptoms SCL‐90 score data used for general psychiatric symptom measures in long‐term follow‐up comparison; 20% of sample lost in the 3‐month follow‐up assessment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Stratified". "Randomization was performed in blocks of 12 subjects using randomization lists supplied by the trial statistician drawn from a computer generated series of random numbers" |
| Allocation concealment (selection bias) | Low risk | Comment: an independent trial administrator co‐ordinated the allocation process and clinicians and researchers were blinded to allocation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report data (SCL‐90, SF‐36, VAS) considered low risk of detection bias No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all participants followed and measured and ITT analyses used |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Dare 2001.
| Methods | RCT of 3 forms of therapy vs. routine care for anorexia nervosa | |
| Participants | 84 participants with DSM‐IV anorexia nervosa Exclusion criteria: people with severe low weight, severe health consequences or suicidality |
|
| Interventions | Intervention 1: 1 year of focal analytic therapy (derived from Malan 1976) (mean 24.9 sessions) Intervention 2: 7 months of cognitive analytic therapy (mean 12.9 sessions) Intervention 3: 1 year of family therapy Control: routine care |
|
| Outcomes | Primary outcome measure was body weight measured as body mass index. Morgan‐Russell Assessment Schedule for anorexia nervosa | |
| Notes | Both individual psychotherapies were methods of STPP | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stratified randomisation method called the 'minimisation method' was used. Method of sequence generation was unclear |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used |
| Blinding (performance bias and detection bias) All outcomes | High risk | Some ratings were done by unblinded clinicians No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analyses were performed. None of the differences between treatments in the rates of engagement was statistically significant |
| Selective reporting (reporting bias) | Unclear risk | Some measures of the Morgan Russell Schedule were not reported by therapy group, rather for the whole group only. The stated reason for this was that there were no intra‐group differences |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
de Jonghe 2001.
| Methods | Single‐centre RCT with 2 parallel arms | |
| Participants | Consecutive newly registered psychiatric clinic outpatients Inclusion criteria: aged 18‐60 years, DSM‐III‐R major depression, HDRS baseline score of at least 14 points and informed consent Exclusion criteria: presence of psycho‐organic disorder, drug abuse, psychotic disorder, with or without dissociative disorder; communication barrier; participant was not considered 'reliable' enough to participate; participation was physically impossible; contraindication for 1 of the antidepressants in the trial; adequate pharmacotherapy treatment for the current major depressive episode; pregnancy 167 people were randomised to each arm, but 38 refused after randomisation. 129 participants started the trial |
|
| Interventions | Intervention: combined treatment arm with psychotherapy and pharmacotherapy for 24 weeks. Psychotherapy was SPSP, based on Werman 1984 or de Jonghe 1994; 18 sessions of 45 min, the first 8 weekly and the last 8 biweekly, performed by 6 psychotherapists who were not the psychiatrists providing medication; all psychotherapists had at least 5 years of experience in psychoanalytic supportive therapy. The therapy was manualised (by the study authors) and there were weekly sessions to assess adherence to therapy. The pharmacotherapy was a stepwise approach in which participants where in the case of intolerance or inefficacy the treatment was changed from fluoxetine, to amitriptyline, then moclobemide Control: pharmacotherapy alone for 24 weeks |
|
| Outcomes | Measures were the HDRS, the SCL‐90 Depression scale, the CGI Improvement and Severity scales, and the QLDS. These were measured at pre‐ and post‐treatment. Remission rates were also measured at 8, 16 and 24 weeks. The study used ITT data (including participants who refused treatment after randomisation), completers only data, and a per‐protocol set (all participants who started with the treatment to which they were allocated) | |
| Notes | HDRS Depression score and QLDS data used in short‐term measures of ITT sample. CGI‐Severity data only available for per‐protocol sample and risk of attrition bias noted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "Patients and treating physicians were not masked to randomisation, the raters were not informed about the treatment condition and were instructed to restrict themselves to discussion of the HRSD items" Comment: the use of independent raters to rate depression (HSRD) minimises a risk of detection bias ‐ low risk. However, physician rated psychiatric symptoms (CGI‐S) scores bring a high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analyses conducted and ITT data used in analyses of depression and social adjustment, thus minimising the risk of attrition bias. Per‐protocol data used for examining CGI, therefore, high risk of bias |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Emmelkamp 2006.
| Methods | Single‐centre RCT with 2 parallel conditions and a wait‐list control | |
| Participants | 62 participants with a avoidant personality disorder, aged 23‐65 years Exclusion criteria: avoidant personality disorder not the primary diagnosis, history of psychotic disorder, high risk of suicide, undergoing psychotherapy treatment or in receipt of therapy in previous 3 years, unable to complete questionnaires |
|
| Interventions | Intervention: treatment involved 20 scheduled sessions over a 6‐month period. Both active therapies were manual guided, treatment adherence was monitored and rated using audiotapes. BDT directed at defence and affect restructuring using interventions based on Malan 1976; Malan 1979; and in some cases incorporating supportive interventions informed by Luborsky 1984 and others Control: wait‐list control group received no treatment between pre‐assessment and follow‐up 20 weeks later |
|
| Outcomes | Assessment measures conducted pre‐treatment, immediately post‐treatment and 6 months' follow‐up. This involved an independent evaluation of personality disorder diagnosis and participant self report measures tapping personality disordered beliefs, avoidant personality traits, anxiety symptoms, social phobia and avoidant behaviours | |
| Notes | LWASQ used for measure of anxiety | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomly assigned" Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report data (LWASQ) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Six patients in total withdrew before the post treatment assessment...forty‐six (46/62) cases for follow‐up analyses" Comment: ITT not reported. Follow‐up data likely to be effected by missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Guthrie 1993.
| Methods | 12‐week, single‐centre RCT with 2 parallel conditions | |
| Participants | 102 participants who had been diagnosed with IBS and had been experiencing symptoms for > 1 year, and who had been treated for a minimum of 6 months with no improvement on bulking agents, antispasmodic therapy, or both | |
| Interventions | Intervention: dynamic psychotherapy based on the conversational model of Hobson 1985 consisting of 1 long 2‐hr session, and 6 follow‐up sessions or a control group at attended on 3 occasions (2, 4 and 8 weeks) to discuss their daily bowel habits Control: standard care All participants continued standard medical treatment in the gastroenterology clinic |
|
| Outcomes | Pre‐, post‐ 12‐week trial. BDI, Symptoms Rating Test, PAS (a modified PSE) | |
| Notes | Same trial as Guthrie (1991) but further data analysis and later follow‐up BDI score used at end‐treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report measures (BDI) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "data for drop‐outs have been included in the results that indicate the overall efficacy of treatments" Comment: similar drop‐outs between groups, data collected for all but 2 of dropouts and included in analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient Information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Guthrie 1999.
| Methods | 2 year, multicentre RCT with 2 parallel conditions | |
| Participants | 110 participants referred from consultant psychiatrists who had received treatment for > 6 months Inclusion criteria: aged 18‐65 years with no improvement in psychological symptoms while in psychiatric treatment Exclusion criteria: schizophrenia, dementia, brain damage, learning difficulties and limited command of English 69 were female and the mean age was 41.4 years |
|
| Interventions | Intervention: psychodynamic‐interpersonal therapy, manualised, based on Hobson 1985 for 8 sessions Control: 'TAU' under the care of their consultant psychiatrist Adherence was checked through supervision, audiotapes and used of the SPRS |
|
| Outcomes | Pre‐, post‐ and 6 months follow‐up GSI of SCL‐90‐R, SF‐36 (health status), Euro‐Qol5D (quality of life), all self rated. Direct treatment costs, non‐treatment costs, indirect costs | |
| Notes | SCL‐90‐GSI and Depression subscale data used; could not use 6‐month follow‐up data as dropout rate was > 20%
SF‐36 only presented as subscales, no overall measures to use; however, Social Functioning and Pain scale included; Euro‐QoL5D data not presented in a form to be useable in review SF‐36 data required reversing for analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was carried out using a computer generated series of random numbers provided by the trial statistician" Comment: low risk of selection bias |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation of patients to trial groups was carried out by a trial secretary who was not involved in the assessment of patients" Comment: method deemed to minimise risk of selection bias |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report measures (SCL‐90‐GSI and Depression subscale, SF‐36 social functioning scale and pain scale) considered low risk of detection bias No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: data analysed using ITT and adequate description of number and reason for drop‐outs |
| Selective reporting (reporting bias) | High risk | Comment: ≥ 1 outcomes are reported incompletely so that they cannot be entered in a meta‐analysis |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Guthrie 2001.
| Methods | RCT with 2 parallel treatment conditions | |
| Participants | 119 participants presenting to the emergency department with an episode of deliberate self poisoning, aged 18‐65 years, able to read and write English, live within the catchment area of the hospital, registered with a GP, not need inpatient psychiatric treatment | |
| Interventions | Intervention: PIT, manualised, based on Hobson 1985, 4 sessions within 1 week of presentation, 50‐min long, in the participant's home Control: 'TAU' ‐ often consists of assessment by emergency department doctor or junior psychiatrist, one‐third referred for outpatient psychiatric treatment, some to addiction services, the remainder to GPs Adherence to treatment through weekly supervision, audiotaping, rating by SPRS |
|
| Outcomes | Entry, 1 month, 6 months. Beck Scale for Suicidal Ideation, detailed description of episodes of self harm, healthcare utilisation | |
| Notes | BDI data at 6‐month follow‐up used; > 20% loss to follow‐up in data at end of treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were assigned using...randomization lists provided by statistician" Comment: low risk of bias |
| Allocation concealment (selection bias) | High risk | Comment: high risk of bias due to open random allocation schedule based on "random list of numbers" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report ratings (BDI) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "psychological assessments were completed in 74.8% patients at the end of treatment, and 78.9% at follow‐up" Comment: significant attrition reported. No ITT described and insufficient information provided about reasons for incomplete information suggest risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Hamilton 2000.
| Methods | RCT with 2 parallel treatment conditions | |
| Participants | 71 participants fulfilling criteria for functional dyspepsia, having continuous symptoms for 6 months, had been unresponsive to at least 2 medical treatments | |
| Interventions | Intervention: psychodynamic‐interpersonal therapy, based on Hobson 1985, manualised, 1 x 3‐hr session and 6 x 50‐min sessions Control: supportive therapy, with session length and number identical to psychodynamic‐interpersonal therapy Adherence to therapy by therapists was measured through SPRS rating of audiotapes |
|
| Outcomes | Entry, end of 12‐week intervention, 12‐month follow‐up. Self rating of dyspeptic symptoms, gastroenterological rating of dyspeptic symptoms, SCL‐90‐R and GSI, healthcare use (gastroenterology clinic visits, medications, inpatient stays, procedures) | |
| Notes | Participants with reflux were included in the study, but a subanalysis was performed excluding them Data used for somatic symptoms and SCL‐90 scores at end of treatment. More than 20% of participants were lost to follow‐up, so 1‐year follow‐up data were not used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed using a computer‐generated series of random numbers supplied by the trial statistician" |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "The gastroenterologists remained blind to the treatment groups" Comment: physician were blinded to treatment, therefore, scores on somatic symptoms at termination: low risk of bias Participants could not be blinded to treatment allocation Self report data on the SCL‐90: low risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: at end of treatment, 37/37 in the experimental group completed outcome data and 31/36 in the control group. Treatment drop‐out was similar across groups but none of the participants in the control group provided outcome data: this would suggest attrition bias. At follow‐up, these figures were 31/37 in the experimental group and 27/36 in the control group. In total, data were available for 79.5% of participants at 1‐year follow‐up. ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information provided to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Levy Berg 2009.
| Methods | RCT with 2 parallel conditions | |
| Participants | Consecutively recruited participants from Swedish outpatient clinics meeting DSM‐IV diagnostic criteria for generalised anxiety disorder Exclusion criteria: participants with major depression excluded Total participant group was 61, 80% with at least 1 personality disorder |
|
| Interventions | Intervention: affect‐focused body psychotherapy: manualised treatment (Monsen 2000) provided once weekly for 1 year. Described as an integration of bodily techniques and the exploration of affects within a psychodynamic frame of reference. Treatment quality and adherence monitored through regular supervision. 7/38 participants treated continued in therapy after 1 year. 11/28 received psychotherapy, 6 of whom continued in treatment after 1 year Control: TAU: at the discretion of the treating psychiatric clinic |
|
| Outcomes | Outcome measures collected at baseline and about 1 and 2 years after the beginning of treatment. Outcome measures used included SCL‐90, BAI, WHO Well‐being Index, SCID screen questionnaire | |
| Notes | Data from BAI and SCL‐90‐GSI score ‐ anxiety items used in the review 7 participants in the STPP group received further treatment a year after the start of therapy, therefore measures at two years after start of therapy not used. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "we assigned patients to either of the two treatment groups using a random number table" |
| Allocation concealment (selection bias) | Unclear risk | Comment: unclear whether the allocation used an open random number table |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants could not be blinded to treatment group. Risk of detection bias considered low based on use of participant self report measures. No psychotherapist was blinded to the treatment delivered |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: at a year after start of therapy, 28% in the TAU did not complete outcome assessments, otherwise missing data was minimal and comparable between groups. ITT controlled for incomplete data |
| Selective reporting (reporting bias) | Unclear risk | Comment: incomplete information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Linnet 2001.
| Methods | Single‐centre RCT with 2 parallel conditions | |
| Participants | 32 adults (23 women, 9 men) with atopic dermatitis. Aged 18‐60 years (mean 28.3), diagnosed with mild to moderate atopic dermatitis by a dermatologist, with no other somatic or psychiatric disease | |
| Interventions | Intervention: psychodynamic psychotherapy, based on Malan 1979, for 11‐18 sessions (mean 15.5) over 6 months Control: no treatment Both groups were instructed to continue their dermatological treatment and keep it as stable as possible |
|
| Outcomes | STAI, SCORAD at entry, 6 months (end‐treatment), 12 months (6 months post‐treatment) | |
| Notes | SCORAD and STAI data scores used in review Loss of > 20% at 12‐month follow‐up, so these data were not used in the review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: inadequate description |
| Allocation concealment (selection bias) | Unclear risk | Comment; Inadequate description |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: self reported anxiety symptoms (low risk) plus blind rating but unclear how blinded rater was using the SCORAD (unclear risk). No psychotherapist was blinded to the treatment delivered. Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: the study authors found and reported evidence of attrition bias in anxiety levels in the control group without statistically controlling for bias |
| Selective reporting (reporting bias) | High risk | Comment: ≥ 1 outcomes are reported incompletely so that they could not be entered in a meta‐analysis |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Maina 2005.
| Methods | Single‐centre RCT with 3 parallel arms | |
| Participants | 30 participants recruited from the wait‐list for BDT at the Mood and Anxiety Disorders unit, Department of Neuroscience of the University of Turin, Italy. Inclusion criteria: BDT wait‐list: participant request for psychotherapeutic approach; presence of a focal problem, a recent precipitant life event or both; aged 18‐60 years Exclusion criteria: evidence of mental retardation, organic mental disorders, psychotic disorders, bipolar disorders, substance abuse, severe axis II pathology Inclusion for study: dysthymic disorder, minor depressive disorder or adjustment disorder with depressed mood; CGI‐S score > 2 Exclusion: current suicidal ideation, current pharmacological treatment, evidence of severe or unstable or active neurological or physical diseases, and on the wait‐list for > 1 month |
|
| Interventions | Intervention 1: STPP based on Malan 1976, 15‐30 sessions (mean 19.6) for 45 min, provided by psychiatrists with personal training in psychodynamic psychotherapy. Case notes reviewed by experienced BDT therapist for supervised treatment adherence Intervention 2: brief supportive therapy Control: wait‐list where they were contacted weekly by telephone |
|
| Outcomes | HAM‐D, HAM‐A, CGI‐I, CGI‐S. Intake, post‐treatment, 6‐month follow‐up, 12‐mo follow‐up for both treatment conditions. Wait‐list controls were only measured at intake and post‐treatment | |
| Notes | Data from HAM‐D, HAM‐A and CGI‐S at post‐treatment used in the review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised into 3 different blocks of 10 subjects, then randomly assigned to ..." Comment: not enough information on procedure |
| Allocation concealment (selection bias) | Unclear risk | Comment: not enough information on procedure |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: Blinded outcome rater HAM‐D, HAM‐A, CGI: low risk No psychotherapist was blinded to the treatment he or she delivered by definition Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Maina 2010.
| Methods | RCT of STPP | |
| Participants | 57 adult outpatients who met the DSM‐IV [21] criteria for a primary diagnosis of OCD with concurrent MDD Inclusion criteria: obsessive‐compulsive symptoms had to have been present for at least 1 year prior to the study entry; Y‐BOCS [23, 24] total score of 6 16 had to be reached, 17‐item HAM‐D [25] score of 6 15 at the baseline evaluation Exclusion criteria: lifetime diagnosis of bipolar disorder, schizophrenia, other psychotic disorders, mental retardation or drug abuse; organic brain syndrome or medical illness that would contraindicate the use of fluvoxamine or sertraline; severe axis II psychopathology (cluster A personality disorder, antisocial personality disorder and borderline personality disorder according to the DSM‐IV) that would contraindicate the treatment with BDT; pregnant or nursing women and women of childbearing potential not using adequate contraceptive measures; ongoing psychological treatment |
|
| Interventions | Intervention: STPP derived from Malan 1976 10 up to 16 sessions. Treatment was interpretive and used clarification. "Manuals" were noted but not described or referenced. Therapist experience was unclear as they were only noted to be trained in psychodynamic psychotherapy. STPP was combined with antidepressant medications Control: antidepressant medications |
|
| Outcomes | Primary outcomes: Y‐BOCS and 17‐item HAM‐D Secondary efficacy measures: included the CGI‐S, CGI‐I and GAF |
|
| Notes | CGI‐S as general measure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: random selection of balls |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: raters were blinded and not therapists or treaters in study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: ITT analysis and low dropout rate |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Marmar 1988.
| Methods | RCT with 2 parallel conditions | |
| Participants | 61 women who sought treatment following the death of their husbands. DSM‐III axis I diagnoses were 29 cases of adjustment disorder, 17 cases of PTSD, 10 cases of major depressive episode, and 5 cases of major depressive episode and PTSD Exclusion criteria: past or present psychotic illness, previous psychiatric hospitalisation, history of drug or alcohol abuse, concurrent psychological treatment, pending litigation, or widowhood < 4 months' or > 3 years' duration |
|
| Interventions | Intervention: BDT (Horowitz 1984) for 12 weekly sessions conducted by 11 faculty therapists with a mean 9.3 years of experience Control: Mutual‐help group treatment led by women who had experienced the deaths of their own husbands |
|
| Outcomes | Pre‐, 4 months post‐treatment, 1‐year follow‐up Stress measures: Impact Event Scale (self report), Stress Response Rating Scale (clinician report). SCL‐90, short BDI, clinician report Brief Psychiatric Rating Scale. SAS, GAS | |
| Notes | SCL‐90, BDI, SAS and SCL‐90 subscale data used in review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: inadequate description |
| Allocation concealment (selection bias) | Unclear risk | Comment: inadequate description |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "In every case the independent evaluator (who) was not the same person as the treating clinician" Self reports (BDI, SCL90, SAS): low risk Blinding participants to treatment group not possible No psychotherapist was blinded to the treatment delivered |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: missing data imputed using last values carried forward procedure |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Milrod 2007.
| Methods | Randomised controlled design with 2 parallel arms | |
| Participants | Inclusion criteria: participants were required to have a primary diagnosis of DSM‐IV panic disorder, a minimum severity score on the DSM‐IV Anxiety Disorder Interview Schedule, and a minimum of 1 weekly panic attack. Participants with co‐morbid depression, personality disorders and severe agoraphobia Exclusion criteria: psychosis, bipolar disorder, active substance abuse and participants were required to discontinue existing psychotherapy treatments |
|
| Interventions | Intervention: Panic‐focused brief psychodynamic psychotherapy (Milrod 1997) was provided by 8 therapists trained in the model, each with a minimum of 2 years' experience using psychodynamic psychotherapy for this client group. Control: Applied relaxation provided by 6 trained and experienced therapists. |
|
| Outcomes | Outcome was examined at baseline, termination, and at 2, 4, 6 and 12 months post treatment termination. Severity of panic disorder, HAM‐A, HAM‐D and the Sheehan Disability Scale were all rated by independent raters, blinded to treatment group. Clinician administered instruments measures frequency of panic attacks and other anxiety‐related symptom data | |
| Notes | HAM‐A and HAM‐D data used. Sheehan Disability Scale provided data on social adjustment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "subjects were randomly assigned using a computer generated treatment assignment list" Comment: unlikely to produce bias |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: Use of self report ratings (Sheehan Disability Scale) and blinded observer raters for depression and anxiety ratings deemed low risk of detection bias No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "rates of dropout [between groups]... differed significantly....The analysis adhered to intention to the treat principle" Comment: attrition 7% in psychodynamic group compared with 34% in applied relaxation training group. ITT analyses controlled for outcome attrition |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Monsen 2000.
| Methods | RCT of matched pairs of participants in 2 parallel conditions | |
| Participants | 40 participants (35 women), all employees of a large Norwegian office company, self referred to company's health service because of pain problems Inclusion criteria: diagnosis of pain disorder associated with psychological factors according to the DSM‐IV Exclusion criteria: pain associated with other medical conditions, such as spine prolapse, neuralgia or chronic disorders manifested in organ systems other than the musculoskeletal system (such as irritable colon) |
|
| Interventions | Intervention: PBT: a variant of the affect‐consciousness treatment model, based on Monsen 1999. The PBT group received a mean of 33 individual, 1‐hr sessions during a period of 9 months (ranging from 15 to 41 sessions). Psychotherapy was performed by the project leader who was a well‐qualified clinical psychologist and physiotherapist Control: received TAU: 3 participants received traditional physiotherapy, 5 participants received both traditional physiotherapy and pain‐reducing medication, 3 participants received pain‐reducing medication and 1 participant received psychological counselling. 8 participants in the control group received no treatment during the intervention period. The treatment was performed by the project leader who was a well‐qualified clinical psychologist and physiotherapist |
|
| Outcomes | Measured at pre‐treatment, post, and 1 year follow‐up. Measures were VAS Pain scale, SCL‐90‐R, IIP‐C, Minnesota Multiphase Personality Inventory, Affect‐Consciousness Scales and job advancement | |
| Notes | Data used from SCL‐90 scores, IIP and VAS for pain | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomised in two groups of twenty patients each" Comment: randomised but not clearly described how |
| Allocation concealment (selection bias) | Unclear risk | Comment: not clearly described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: mainly self report measures used (SCL, VAS, IIP): low risk Blind ratings of Affect Consciousness Scales: low risk No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "all patients participated in the assessments at T1 [pre‐treatment], T2 [post‐treatment] and T3 [1‐year follow‐up], except one person in the control group absent at T3 due to complications after child birth" Comment: proportion of missing data not likely to have relevant impact |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Piper 1990.
| Methods | RCT (participants matched in pairs by QOR, sex and age, then assigned to 1 condition or another) with cross‐over design. Wait‐list controls were used here for comparison | |
| Participants | 105 psychiatric outpatients referred from a walk‐in clinic. Axis I DSM‐III diagnoses were affective (31%), adjustment (23%), anxiety (7%) and impulse control (8%). 32% of participants had axis II diagnoses. Mean age 31 years, 65% female | |
| Interventions | Intervention: short‐term individual psychotherapy, manualised, based on Malan 1976 and Strupp 1984, for a maximum of 20 weekly 50‐min sessions (actual mean 18.6) Control: wait‐list subsequently received STI therapy. Sessions were audio‐recorded, rated by Therapist Intervention Rating System. 8 therapists, mean experience 11.5 years (range 4‐35) |
|
| Outcomes | QOR, SAS, Interpersonal Dependency Scale (2 subscales used), Interpersonal Behaviour Scale, GSI of SCL‐90, BDI, Trait Anxiety Scale, Rosenberg's Pre‐(therapy, wait‐list), post (therapy, wait), follow‐up/post‐therapy, then overall follow‐up ‐ 5‐month intervals. Self‐Esteem Scale, Insight Scale, life satisfaction by 7‐point Likert scale | |
| Notes | Only immediately post‐treatment data used for SCL‐90, BDI and Trait Anxiety Scale Unable to use SAS data as not presented with means and standard deviations | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The research coordinator matched patients in pairs...and randomly assigned one member to the immediate therapy condition and the other member to the delayed therapy control condition" Comment: insufficient information about the sequence generation process |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report data (SCL‐90, BDI, STAI) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: it was reported that 11 in the immediate therapy condition and 9 in the delayed therapy condition dropped out, and 67/86 provided follow‐up data. Insufficient information was provided on reasons for missing data to determine judgement of bias |
| Selective reporting (reporting bias) | High risk | Comment: ≥ 1 outcomes are reported incompletely so they could not be entered in a meta‐analysis |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Sattel 2012.
| Methods | RCT of STPP for people with multisomatoform disorders | |
| Participants | 211 participants with multisomatoform disorders Exclusion criteria: people SF‐36 < 40, hypochondriasis, cognitive impairment, severe somatic illness, serious mental illness 67/107 were females, mean age 47.9 years |
|
| Interventions | Intervention: 12 weekly sessions of modified PIT specifically adapted to the needs of participants in bodily distress, manual authored by Henningsen 2011. Treatment was 3 phases focusing on building therapeutic relationships, working on emotions about the bodily symptoms and termination future planning Control: enhanced TAU: this included "education and counselling regarding the therapeutic alternatives based on the evidence‐based guidelines for the treatment of somatoform disorders/functional somatic syndromes in primary and somatic specialist care" |
|
| Outcomes | SF‐36 (Physician and Patient forms), PHQ somatisation, HQ Depression, Health Anxiety/Whiteley Index; healthcare utilisation: visit counts, medication use | |
| Notes | Primary general measure SF‐36 MCS. Somatic measure used was SF‐36 PCS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: a computer program generated a blocked randomisation list |
| Allocation concealment (selection bias) | Low risk | Quote: "After receiving informed consent, we submitted a randomisation request and the centre returned the result for the patient in question within 24 h. The patients completed the baseline assessment independently immediately after providing informed consent and delivered the assessment to the study therapist in person or by post. Thereafter, the therapist disclosed the group assignment to the patient and treatment began" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report measures were used. Healthcare use was recorded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses...were based on the intent to‐treat method for all participants and confirmed that the missing data for the primary and secondary outcomes were missing at random... Multiple imputations were used to replace missing data, which consisted mainly of patients who were lost to follow‐up (n = 26). We performed sensitivity analyses to estimate the potential differences in the imputed outcomes v. those derived from incomplete data" |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Shefler 1995.
| Methods | Single‐centre RCT with cross‐over design | |
| Participants | 33 participants referred from a walk‐in psychiatric clinic, 9 men, 24 women, aged 23‐42 years Exclusion criteria: schizophrenia and any subtypes, bipolar disorder, schizoid characters, obsessional characters with major defences of isolation and intellectualisation, borderline conditions and psychosomatic disorders; also, further suitability for therapy Only 45 of 404 participants from the clinic were deemed suitable for TLP. This was attributed to only 15% of participants being suitable for psychodynamic therapy due to higher percentages of participants with psychoses, and severe social and personality disorders in the centre's catchment area. DSM‐III‐R diagnoses were performed Axis I: 9 participants received no diagnosis, 7 participants had anxiety disorders, 6 participants had depressive disorders, 10 participants had adjustment disorders and 1 participant had a life‐phase problem Axis II: 5 participants had diagnoses (not given) | |
| Interventions | TLP, based on Mann 1973, 12 weekly 50‐min sessions, or wait‐list control, then cross‐over into other condition. All 9 therapists were graduates in TLP courses | |
| Outcomes | Assessments done at pre‐treatment, mid (end TLP or wait), end TLP and wait, follow‐up 6 months, follow‐up 12 months Target Complaints Scale, SCT, BSI‐53 (brief revision of SCL‐90), HSRS, GAS | |
| Notes | BSI‐53 data used for general psychiatric symptoms measure comparison | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report data (BSI) considered low risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "the numbers represent the number of patients who had complete ratings on all three occasions" Comment: completer only analyses presented and no data on participant drop‐out |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Sloane 1975.
| Methods | RCT with 3 conditions. Participants matched within conditions by sex and severity of neurosis as measured by Eysenck Personality Inventory | |
| Participants | 94 adults who had applied for treatment at a university psychiatric outpatient clinic, aged 18‐45 years, not too mildly ill or too disturbed to risk waiting for 4 months Exclusion criteria: psychotic, mentally retarded, organic brain damage, or primarily in need of drug therapy. Participants were mostly in early 20s, 60% female |
|
| Interventions | Intervention 1: psychoanalytically oriented therapy (no manual or reference provided) Intervention 2: behaviour therapy Control: wait‐list control Therapies were 4 months of weekly sessions, 14.2 for psychoanalytic therapy, mean 13.2 sessions for behaviour therapy. 3 therapists per therapy condition, range of experience 6‐20 years. External rating used for adherence |
|
| Outcomes | Measured at pre‐treatment, post‐treatment, 1‐year follow‐up 3 target symptoms rated, SSIAM | |
| Notes | Most frequent symptoms were, in decreasing order, generalised anxiety, interpersonal difficulties, low self esteem, generalised worry and bodily complaints. One‐third of participants had personality disorders Data for Target symptoms used at post‐treatment. Unable to use data at other follow‐up times as some of the sample went on to continue or have treatment. SSIAM data not presented in parameters that could be combined with other continuous data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After interviewing and testing, the patients were randomly assigned...Within this random assignment, patients were matched within the three groups in terms of sex and severity of neurosis" Comment: insufficient information to determine possible selection bias |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information to determine possible selection bias |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "assessors were blind as to type of therapy in most cases, but a few patients inadvertently gave clues to their therapist’s identity...A comparison of outcome ratings did not reveal any bias toward any group" Comment: method for observer ratings on patient Target complaint ratings and SSIAM indicate an unclear risk of possible bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: at termination (4 months), attrition across groups was small: intervention 0/30, control 3/33. At follow‐up, although a large percentage of participants received additional treatment, data for these participants versus those who did not require additional therapy suggested total sample data remained valid |
| Selective reporting (reporting bias) | High risk | Comment: ≥ 1 outcomes of interest are reported incompletely so that they cannot be entered in a meta‐analysis |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Svedlund 1983.
| Methods | RCT with 2 parallel conditions | |
| Participants | 102 participants with IBS, aged 16‐60 years (mean 24), 70 females Exclusion criteria: other somatic or mental disorders requiring treatment, had previous abdominal surgery affecting the gastrointestinal tract, were on a disability pension or were not fluent in Swedish |
|
| Interventions | Intervention: brief dynamic psychotherapy, based on Malan 1979, for 10 x 1‐hr long sessions over 3 months (mean 7.4 sessions), with medical TAU Control: TAU ‐ bulk‐forming agents and, when appropriate, anticholinergic drugs, antacids and minor tranquillisers |
|
| Outcomes | Pre, post and 15 months (after start of psychotherapy) Mental symptoms by CPRS and somatic symptoms, all rated by psychiatrist. On follow‐up, participant rating. In addition, SSIAM | |
| Notes | Additional data provided by study author used for psychiatric symptoms, anxiety symptoms, depression symptoms and somatic symptoms. SSIAM data used for social adjustment measure Data used for somatic symptoms, and anxiety, depression and general symptoms. SSIAM for social adjustment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: stratified by gender and randomised. Details of method not provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: inadequate description |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: therapists were raters of some cases and may have been unblinded (CPRS, SSIAM): high risk Self reports (social adjustment): low risk No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "dropouts can be ruled out as contributing to different outcomes" Comment: only 1 drop‐out from each group |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes. Additional information was obtained from the authors to be entered in a meta‐analysis |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Sørensen 2010.
| Methods | RCT with 3 parallel conditions | |
| Participants | Participants were required to meet ICD‐10 criteria for hypochondriasis and experience significant levels of health anxiety, as indicated by a score of > 17 on the HAI. Having received previous adequate cognitive behavioural or psychodynamic treatment was an exclusion criteria | |
| Interventions | Intervention 1: STPP was a 16‐session, 50‐min weekly treatment. Treatment was not manualised and described as a "relational approach" using common dynamic interventions Intervention 2: CBT involved 8 individual sessions, followed by 8 group sessions that included mindfulness training. Treatment was manualised and supervision was provided by the inventor of the model Control: wait‐list control lasted 6‐months. Participants were asked to keep in touch with their GP but no further contact was pre‐arranged All therapy sessions were audiotaped and 12 sessions from each treatment arm were randomly selected and independently rated to evaluate therapist adherence to specific and non‐specific components of psychotherapy |
|
| Outcomes | The HAI and HAM‐A were described a primary outcome measures and secondary outcome measures included the HAM‐D and BAI. Independent trained raters, blinded to treatment group, provided observer ratings using the HAM‐D and HAM‐A. Outcome data were collected prior to treatment onset and 1 year after the end of treatment | |
| Notes | Data from HAM‐D and HAM‐A used in review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomised allocation was computer generated in permuted blocks of eight. The block sizes were concealed until the end of the trial" Comment: low risk of selection bias |
| Allocation concealment (selection bias) | Low risk | Quote: "Concealment of allocation from the initial assessor was ensured by a procedure involving centralized telephone randomisation" Comment: low risk of selection bias |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "It was not possible to blind the patients and therapists to the group allocation, but the raters assessing outcome were blinded with respect to group assignment. The blinding was evaluated" Comments: self report data (Health Anxiety Inventory, BAI) considered low risk of detection bias. Objective ratings (HAMA, HAMD) considered low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "we used a modified ITT analysis" and "missing data were imputed using the last observation carried forward procedure" |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Model of STPP is restricted from using core psychodynamic techniques and questionable as to whether or not it is a bona fide versus a "built to under perform" control model of STPP |
Vitriol 2009.
| Methods | RCT with 2 parallel conditions | |
| Participants | Consecutive women, aged > 20 years, diagnosed with severe depression in primary care clinics were referred for evaluation. Participants meeting ICD‐10 criteria for severe depression, HAM‐D score > 20 and reporting past traumatic life experiences were included in the trial | |
| Interventions | Intervention: participants were randomised to receive either standard treatment, described as supportive psychotherapy provided by a psychologist. The 3‐month brief psychodynamic intervention treatment was non‐manualised weekly psychotherapy focused on, "developing a cognitive understanding of personal characteristics and behaviours that allowed the repetition of traumatic experiences past and present. Behavioural changes that would alter the relationship between the victim and aggressor were addressed." An initial assessment session with a multidisciplinary team was described as using a psychodynamic orientation Control: standard treatment Participants in both groups received pharmacological treatment as appropriate |
|
| Outcomes | Outcome data was collected pre‐treatment, at 3 months (or on treatment completion) and at 6 months. An external rater administered the HAM‐D, and a different external rater administered the OQ‐45.2 and PTO | |
| Notes | Subscale data from the OQ‐45 used in review for measurement of general psychiatric symptoms, interpersonal problems and social adjustment. HAM‐D ratings were used for depression and the PTO for a measure of anxiety symptoms | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: observer‐rated outcome ratings (HAM‐D) and participant self report ratings (OQ‐45, PTO) considered a low risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: a similar level of attrition was present in the intervention group (9/45) compared with standard treatment (11/46) but there may have been differences in the reasons for drop‐out between groups: 4 in the intervention group "got better". However, outcome data were available for 91% of participants at 3 months and 81% at 6 months and ITT analyses were conducted thus minimising possible effects of missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Wiborg 1996.
| Methods | RCT with 2 parallel conditions | |
| Participants | 40 participants (23 women, 17 men) with panic disorder, with or without agoraphobia Inclusion criteria: at least 1 panic attack per week in the 3‐week period prior to inclusion into the study. There was co‐morbidity: 3 participants had GAD, 3 had participants social phobia, 3 participants had hypochondriasis, 14 participants had simple phobia, 2 participants had secondary major depressive episode, 2 participants had secondary OCD |
|
| Interventions | Intervention: clomipramine with brief dynamic psychotherapy (manualised, based on Davanloo 1980;Malan 1976;Strupp 1984) Control: clomipramine alone Clomipramine was administered with a flexible step‐up procedure (during which time benzodiazepines were allowed), until a dosage of 150 mg/day, for 36 weeks BDP was administered by 1 therapist with experience (years not given), 1 weekly visit for 15 weeks, with 3 sessions given before the start of pharmacotherapy | |
| Outcomes | Pre‐, during (weekly), post‐, 18 months follow‐up. Overall: SCL‐90, STAI, GAS, CGI. Panic attack diary, PAAS, HAM‐A, Sheehan Disability Scale, Phobia Scale, HRSD, Medical Events Checklist (register adverse effects of clomipramine) | |
| Notes | SCL‐90, HAM‐D, and HAM‐A, Sheehan Disability Scale ‐ Social Functioning data used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomised using computerized random number generator and sealed envelopes" |
| Allocation concealment (selection bias) | Low risk | Quote: "sealed envelopes" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: self report outcome data (SCL‐90) considered low risk of detection bias. Insufficient information on blinding of observer‐rated measures (HAM‐D, HAM‐A, Sheehan Disability Scale); therefore, bias considered unclear No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all evaluated at all points |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
Winston 1994.
| Methods | RCT with 3 parallel conditions | |
| Participants | 93 psychiatric outpatients Inclusion criteria: aged 18‐60 years; evidence of at least 1 close personal relationship; no evidence of psychosis, organic brain syndrome, or mental retardation; no active DSM‐III‐R axis III medical diagnosis; no evidence of current substance abuse; no acute suicidal behaviour; no history of violent behaviour or destructive impulse control problems; and no use of psychotropic medications, such as lithium, neuroleptics or antidepressants in the past year Exclusion criteria: axis II diagnoses of schizoid, paranoid, schizotypal, narcissistic and borderline personality disorders |
|
| Interventions | Intervention 1: STDP, manualised, based on Davanloo 1980 Intervention 2: BAP based on Pollack 1991 Control: waiting list (mean wait‐list time 14.9 weeks) 24 therapists (13 for STDP, 11 for BAP), mean experience 11.6 years, mean number of sessions, both techniques combined, 40.3 All sessions videotaped, adherence rated through systematic scales | |
| Outcomes | Assessed at pre‐treatment and 1 month post‐treatment: GSI of SCL‐90‐R, SAS, target complaints rating 6 months post: target complaints | |
| Notes | SCL‐90 and SAS data used in review STDP and BAP entered separately as contrasting forms of STPP models |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: self report ratings (SCL‐90, SAS) considered low risk of bias No psychotherapist was blinded to the treatment delivered Blinding participants to treatment group not possible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "the patients who dropped out of the study were similar to the treated patients in both demographic characteristics and diagnosis, although no formal analyses were conducted because of the small number of dropouts" Comment: 6/31 participants in STDP dropped out vs. 2/32 in BAP: this is considered significant enough to warrant analysis to rule out attrition bias |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement. No published report on pre‐specified outcomes |
| Other bias | Unclear risk | Comment: insufficient information to permit judgement |
BAI: Beck Anxiety Inventory; BAP: brief adaptive psychotherapy; BDI: Beck Depression Inventory; BDT: brief dynamic therapy; BSI: Brief Symptom Inventory; CBT: cognitive behavioural therapy; CGI: Clinical Global Impressions; CGI‐I: Clinical Global Impression ‐ Improvement scale; CGI‐S: Clinical Global Impression ‐ Severity scale; CPRS: complex regional pain syndrome; DSM‐III: Diagnostic and Statistical Manual of Mental Disorders ‐ third edition; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders ‐ fourth edition; EPDS: Edinburgh Postnatal Depression Scale; GAF: Global Assessment of Functioning; GAS: Global Assessment Scale; GP: general practitioner; GSI: Global Severity Index; HAI: Health Anxiety Inventory; HAM‐A: Hamilton Anxiety Rating Scale; HAM‐D: Hamilton Depression Rating Scale; HDRS: Hamilton Depression Rating Scale; HQ: Health Questionnaire; hr: hour; IBS: irritable bowel syndrome; ICD‐10: International Statistical Classification of Diseases and Health Related Problems 10th Revision; IIP: Inventory of Interpersonal Problems; ISTDP: intensive short‐term dynamic psychotherapy; ITT: intention to treat; LWASQ: Lehrer Woolfolk Anxiety Symptom Questionnaire; MDD: major depressive disorder; min: minute; OCD: obsessive‐compulsive disorder; OQ: Outcome Questionnaire; PAAS: Panic Attack and Anxiety Scale; PBT: psychodynamic body therapy; PHQ: Patient Health Questionnaire; PIT: psychodynamic interpersonal therapy; PPD: postpartum depression; PTO: Post‐traumatic Stress Treatment Outcome scale; PTSD: post‐traumatic stress disorder; QLDS: Quality of Life Depression Scale; QOR Quality of Object Relations; RCT: randomised controlled trial; SAS: Social Adjustment Scale; SCID: Structured Clinical Interview for DSM‐IV Disorders; SCL‐90: Symptom Checklist‐90; SCL‐90‐GSI: Symptom Checklist‐90 Global Severity Index; SCL‐90‐R: Symptom Checklist‐90 ‐ Revised; SCORAD: Scoring of Atopic Dermatitis Index; SF‐36 MCS: 36‐item Short Form ‐ Mental Component Summary; SF‐36 PCS: 36‐item Short Form ‐ Physical Component Summary; SF‐36: 36‐item Short Form; SPRS: Sydney Psychosocial Reintegration Scale; SPSP: short psychodynamic supportive psychotherapy; SSIAM: Structured and Scaled Interview to Assess Maladjustment; STAI: State‐trait Anxiety Inventory; STDP: short‐term dynamic psychotherapy; STPP: short‐term psychodynamic psychotherapy; TAU: treatment as usual; TLP: time‐limited psychotherapy; VAS: visual analogue scale; WHO: World Health Organization; Y‐BOCS: Yale‐Brown Obsessive Compulsive Scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Brodaty 1983 | Length of sessions only 30 min |
| Budman 1988 | Compared individual STPP to an active treatment: group STPP |
| Fairburn 1986 | Short‐form focal therapy compared with an active treatment: cognitive behavioural approach |
| Gallagher 1982 | Compared STPP with 2 active treatments: behavioural therapy and cognitive therapy |
| Gallagher‐Thompson 1994 | Brief psychodynamic therapy compared with an active treatment, cognitive‐behavioural therapy, for clinically depressed family carers |
| Gilbert 1982 | Group therapy |
| Hall 1987 | Randomised controlled trial of 30 females with anorexia nervosa. Excluded because the treatment group was a combined individual psychodynamic psychotherapy and family therapy approach |
| Hardy 1995 | Psychodynamic‐interpersonal therapy was compared with an active control: cognitive behavioural therapy |
| Hellerstein 1998 | STDP was compared with an active treatment control |
| Knekt 2004 | Compared STPP with active comparators |
| Maina 2009 | Participants included in this long‐term follow‐up study only include remitters who were not a randomised sample of original participants |
| McLean 1979 | Short‐term psychotherapy was compared with active controls in people with depression |
| Morris 1975 | Group therapy |
| Nanzer 2012 | Not a randomised controlled trial |
| Piper 1998 | A randomised controlled trial comparing 2 active forms of therapy, interpretive and supportive forms of short‐term individual psychotherapy, in adult outpatients with a variety of axis I and II diagnoses |
| Shapiro 1987 | Exploratory (relationship‐oriented) therapy, a "nonspecific dynamic therapy" was compared was an active control |
| Shapiro 1995 | Psychodynamic‐interpersonal therapy was compared with an active control, cognitive behavioural therapy |
| Simpson 2003 | Use of a brief therapy by general practitioners in people with chronic depression. Method of psychotherapy used was "Freudian psychoanalysis", which is not a standard STPP |
| Sjodin 1986 | Short‐term psychotherapy in combination with medical treatment was compared with medical treatment only in people with chronic peptic ulcer disease. This was a study from 20 years ago before the introduction of triple therapy for the eradication of Helicobacter pylori |
| Svartberg 2004 | STDP was compared with cognitive therapy, an active treatment control |
| Thompson 1987 | STDP was compared with 2 active treatments and a delayed treatment condition. Data for the wait‐list could not be compared with the treatment as it was a partially case‐controlled study, with the participants in the wait‐list groups ultimately being incorporated into the treatment conditions |
| Vinnars 2005 | Control group was an active psychotherapy |
min: minutes; STDP: short‐term dynamic psychotherapy; STPP: short‐term psychodynamic psychotherapy.
Characteristics of studies awaiting assessment [ordered by study ID]
Barber 2012.
| Methods | RCT of STPP versus placebo and versus medication management |
| Participants | 156 adults with major depression |
| Interventions | STPP 16 weeks' time limited. Luborsky 1984 |
| Outcomes | HAM‐D, remission and response |
| Notes | NCT00043550 |
Beutel 2014.
| Methods | RCT of STPP vs. care as usual |
| Participants | 157 women with major depression and breast cancer |
| Interventions | STPP 20 sessions maximum Luborsky 1984 |
| Outcomes | Hospital Anxiety and Depression Scale |
| Notes | ISRCTN96793588 |
Bressi 2011.
| Methods | RCT of STPP vs. CBT vs. routine care |
| Participants | 35 adults with panic disorder |
| Interventions | STPP Malan 1976 vs. CBT |
| Outcomes | HAM‐D, HAM‐A, PAAAS, TAS‐20 |
| Notes |
Faramarzi 2013.
| Methods | RCT of STPP vs. medical management |
| Participants | 49 participants with functional dyspepsia |
| Interventions | STPP Luborsky 1984 vs. medical management |
| Outcomes | PAGI‐SYM: measure of gastrointestinal symptoms; DSQ 40; TAS‐20 |
| Notes | IRCT201102285931N1 |
Gibbons 2012.
| Methods | RCT of STPP |
| Participants | 40 adults with major depression |
| Interventions | STPP 12 session limited time, Luborsky 1984. Treatment as usual |
| Outcomes | Basis 24, HAM‐D |
| Notes |
Kompoliti 2014.
| Methods | RCT of STPP. Cross‐over after wait‐list |
| Participants | 15 with functional movement disorders |
| Interventions | STPP Davanloo 1980. 12 sessions time limited |
| Outcomes | CGI, HAM‐D, Beck Anxiety Inventory |
| Notes |
Leichsenring 2013.
| Methods | RCT of STPP vs. CBT vs. wait‐list |
| Participants | 495 adults with social anxiety disorder |
| Interventions | STPP Luborsky 1984 up to 25 sessions |
| Outcomes | Liebowitz Social Anxiety Scale, Social Phobia and Anxiety Inventory, Beck Depression Inventory, Inventory of Interpersonal Problems |
| Notes | ISRCTN53517394 |
Reneses 2013.
| Methods | RCT of STPP vs. psychiatric treatment as usual |
| Participants | 44 with borderline personality disorder |
| Interventions | 20 sessions of psychic representation focused psychotherapy |
| Outcomes | Severity global index of SCL‐90‐R, Barratt Impulsivity Scale scores, Social Adaptation Self‐Evaluation Scale |
| Notes |
Scheidt 2013.
| Methods | RCT of STPP vs. treatment as usual for fibromyalgia plus anxiety or depression |
| Participants | 46 females with fibromyalgia and an International Classification of Diseases, 10th Revision diagnosis of a co‐morbid depression or anxiety disorder |
| Interventions | Participants were randomised to receive either an adapted version of STPP (25 sessions, 1 session/week) or treatment as usual (4 consultations/6 months) |
| Outcomes | Fibromyalgia Impact Questionnaire, Hospital Anxiety and Depression Scale, Pain Disability Index, Symptom Checklist 27 and health‐related quality of life |
| Notes |
Shaw 2001.
| Methods | RCT of STPP versus wait‐list control. Cross‐over design |
| Participants | 54 adults with mixed common mental disorders |
| Interventions | 12 weeks of STPP (psychodynamic interpersonal therapy, Hobson 1985) delivered by psychiatry trainees |
| Outcomes | SCL‐90‐R and Inventory of Interpersonal Problems |
| Notes |
Zipfel 2014.
| Methods | Multicentre, randomised controlled efficacy trial in adults with anorexia nervosa of STPP vs. enhanced CBT vs. optimised treatment as usual |
| Participants | 242 participants with anorexia nervosa |
| Interventions | 10 months of focal psychodynamic therapy, enhanced CBT or optimised treatment as usual |
| Outcomes | Weight gain (body mass index), rate of weight gain. Hence, does not include outcomes measures of interest in this review |
| Notes | ISRCTN72809357 |
CBT: cognitive behavioural therapy; CGI: Clinical Global Impression; DSQ: Defense Style Questionnaire; HAM‐A: Hamilton Anxiety Rating Scale; HAM‐D: Hamilton Depression Rating Scale; PAAS: Panic and Anticipatory Anxiety Scale; PAGI‐SYM: Patient Assessment of Upper Gastrointestinal Symptoms; RCT: randomised controlled trial; SCL‐90‐R: Symptom Checklist‐90 ‐ Revised; STPP: short‐term psychodynamic psychotherapy; TAS‐20: 20‐item Toronto Alexithymia Scale.
Characteristics of ongoing studies [ordered by study ID]
ISRCTN38209986.
| Trial name or title | Improving Psychodynamic Psychotherapy in Primary Care: Randomised Evaluation of Dynamic Interpersonal Therapy (DIT) |
| Methods | Single‐blind, multi‐site RCT |
| Participants | 1. Aged over 18 years, male or female 2. Current diagnosis of Major depressive disorder (MDD) with or without dysthymic disorder according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM‐IV) criteria 3. Hamilton Depression Rating Scale score above 14 4. Patient Health Questionnaire (PHQ) score above 10 5. Confirmed need for high‐intensity treatment either at triage, following referral, or by low‐intensity worker and supervisor |
| Interventions | Dynamic Interpersonal Therapy vs Enhanced Wait List, Enhanced Wait list condition involving low‐level routine clinical care with elements of low‐intensity treatment. |
| Outcomes | Primary outcome measure: Hamilton Depression Rating Scale (HDRS‐17) Secondary outcome measures: Beck Depression Inventory (BDI‐II); Brief Symptom Inventory (BSI); EuroQOL (EQ‐5D); MINI+ (Mini‐International MINI international neuropsychiatric interview); Reflective Function Questionnaire (RFQ‐54); Revised Social Adjustment Scale (SAS‐r) |
| Starting date | 20/06/2012 |
| Contact information | Ms Tara McFarquhar, email: tara.mcfarquhar@annafreud.org |
| Notes |
NCT01141426.
| Trial name or title | Halifax Treatment Refractory Depression Trial |
| Methods | RCT of STPP (Davanloo) vs. community treatment as usual |
| Participants | Treatment‐resistant depression |
| Interventions | Davanloo's model of STPP |
| Outcomes | Primary outcome measures: Hamilton Rating Scale for Depression Secondary outcome measures: GAD‐7, Inventory of Interpersonal Problems, 32‐item Toronto Alexithymia Scale, SF‐12, CORE‐OM, Trimbos and Institute of Medical Technology Assessment Cost Questionnaire for Psychiatry, PHQ‐9, Patient Health Questionnaire ‐ somatic symptom scale |
| Starting date | 2012 |
| Contact information | Joel Town DClinPsy, telephone: 1‐902‐473‐2543, email: joel.town@dal.ca |
| Notes |
NCT02076867.
| Trial name or title | Halifax Somatic Symptom Disorder Trial: A Randomized Parallel Group Cross‐Over Study of Intensive Short‐Term Dynamic Psychotherapy Compared to Medical Treatment as Usual for Somatic Symptoms in the Emergency Department |
| Methods | Randomized Parallel Group Cross‐Over Study |
| Participants | Men and women aged 18‐65 years with somatic symptom and related disorders (as assessed by the Structured Clinical Interview for DSM Disorders 5th Edition Research Version (SCID‐5‐RV)) |
| Interventions | Intervention: Intensive Short‐Term Dynamic Psychotherapy Control: Medical Care As Usual (MCAU) |
| Outcomes | Primary outcome measure: Change in Somatic Symptom Severity score using the SOMS‐7 Secondary outcome measures: Patient Health Questionnaire‐depression scale (PHQ‐9); Whiteley Index for Health Anxiety; Short Form Health Survey (SF‐12); Inventory of Interpersonal Problems (IIP‐32); Presence of somatic symptom and related disorder diagnosis using the Structured Clinical Interview for DSM Disorders Version 5 |
| Starting date | March 2014 |
| Contact information | Joel Town DClinPsy, telephone: 1‐902‐473‐2543, email: joel.town@dal.ca |
| Notes |
CORE‐OM: Clinical Outcomes in Routine Evaluation Outcome Measure; GAD‐7: 7‐item Generalized Anxiety Disorder Scale; PHQ‐9: 9‐item Patient Health Questionnaire; RCT: randomised controlled trial; SF‐12: 12‐item Short‐Form Health Survey; STPP: short‐term psychodynamic psychotherapy.
Differences between protocol and review
As the protocol was written in 2004, the methods have been updated to those of the Cochrane Handbook for Systematic Reviews of Interventions of 2008 (Higgins 2008a). We added several new international researchers from Germany, the Netherlands, Australia and the USA strengthening the team of this review. We have also included 'occupational function' as a relevant cost‐related issue in common mental disorders outcome.
In following phrase was deleted from the methods: "Where no further usable data was provided, studies were not included in the meta‐analysis, and were listed as excluded due to missing data." This is in accordance with Cochrane's methodological stipulation that studies that meet the inclusion criteria should be included in the review irrespective of whether measured they report data in a useable way (Chandler 2013).
Contributions of authors
Abbass is the guarantor of this review. Abbass originally conceived the review. Abbass, Kisely and Hancock designed the review. Rusalovska collected data for the review. Kisely and Hancock developed the search strategy. Rusalovska and Abbass undertook searches. All review authors screened and retrieved papers against inclusion criteria. Abbass and Town appraised quality of papers. Town and Abbass abstracted data from papers. Abbass and Rusalovska wrote to authors of papers for additional information. Kisely, Town and Abbass entered data into Review Manager 5. Kisely, Town and Abbass analysed and interpreted data. All review authors provided a methodological perspective. Abbass, Leichsenring and Town provided a clinical perspective. All review authors contributed towards writing the review.
Sources of support
Internal sources
Department of Psychiatry, Dalhousie University, Canada.
Nova Scotia Department of Health, Canada.
External sources
Cochrane Canada, Canada.
Declarations of interest
Allan A Abbass: academic focus on a variant of short‐term psychodynamic psychotherapies (STPP), and was the lead author on one of the included studies. He acknowledges a psychotherapeutic bias in his clinical work and teaching in favour of some of these methods. However, he is aware of the need to review the literature, and improve upon the research done in this field. To balance this view, colleagues without such a bias participated in this review.
Elizabeth Crowe: none known.
Saskia De Maat: works and teaches in a psychoanalytical oriented workplace (doing therapies) and teaches on the subject of psychoanalysis and psychoanalytic psychotherapy.
Jack Dekker: none known.
Ellen Driessen: none known.
Andrew Gerber: none known.
Steve R Kisely: none known.
Falk Leichsenring: none known.
Sven Rabung: none known.
Svitlana Rusalovska: none known.
Joel M Town: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Abbass 2008 {published data only}
- Abbass A, Sheldon A, Gyra J, Kalpin A. Intensive short‐term dynamic psychotherapy of patients with DSM IV personality disorders: a randomized controlled trial. Journal of Nervous and Mental Disease 2008;196(3):211‐6. [DOI] [PubMed] [Google Scholar]
Alstrom 1984a {published data only}
- Alstrom JE, Nordlund CL, Persson G, Harding M, Ljungqvist C. Effects of four treatment methods on social phobic patients not suitable for insight‐oriented psychotherapy. Acta Psychiatrica Scandinavica 1984;70:97‐110. [DOI] [PubMed] [Google Scholar]
Alstrom 1984b {published data only}
- Alstrom JE, Nordlund, G, Persson G, Harding M, Lundquist C. Effects of four treatment methods on agoraphobic women not suitable for insight‐oriented psychotherapy. Acta Psychiatrica Scandinavica 1984;70:1‐17. [DOI] [PubMed] [Google Scholar]
Baldoni 1995 {published and unpublished data}
- Baldoni F, Baldaro G, Trombin G. Psychotherapeutic perspectives in urethral syndrome. Stress Medicine 1995;11:79‐84. [Google Scholar]
Bressi 2010 {published data only}
- Bressi C, Porcellana M, Marinaccio PM, Nocito EP, Magri L. Short‐term psychodynamic psychotherapy versus treatment as usual for depressive and anxiety disorders. A randomized clinical trial of efficacy. Journal of Nervous Mental Disease 2010;198(9):647‐52. [DOI] [PubMed] [Google Scholar]
Brom 1989 {published data only}
- Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. Journal of Consulting and Clinical Psychology 1989;57(5):607‐12. [DOI] [PubMed] [Google Scholar]
Burnand 2002 {published data only}
- Burnand Y, Andreoli A, Kolatte E, Venturini A, Rosset N. Psychodynamic psychotherapy and clomipramine in the treatment of major depression. Psychiatric Services 2002;53(5):585‐90. [DOI] [PubMed] [Google Scholar]
- Cailhol L, Rodgers R, Burnand Y, Brunet A, Damsa C, Andreoli A. Therapeutic alliance in short‐term supportive and psychodynamic psychotherapies: a necessary but not sufficient condition for outcome?. Psychiatry Research 2009;170(2‐3):229‐33. [DOI] [PubMed] [Google Scholar]
Carrington 1979 {published data only}
- Carrington CH. A comparison of cognitive and analytically oriented brief treatment approaches to depression in black women. Dissertation Abstracts International 1979;40(6B):UMI No. 7926513. [Google Scholar]
Cooper 2003 {published data only}
- Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression: 1. Impact on maternal mood. British Journal of Psychiatry 2003;182:412‐9. [PubMed] [Google Scholar]
- Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression: 2. Impact on the mother‐child relationship and child outcome. British Journal of Psychiatry 2003;182:420‐7. [PubMed] [Google Scholar]
Creed 2003 {published and unpublished data}
- Creed F, Fernandes L, Guthrie E, Palmer S, Ratcliffed J, Read N, et al. The cost‐effectiveness of psychotherapy and paroxetine for severe irritable bowel syndrome. Gastroenterology 2003;124:303‐17. [DOI] [PubMed] [Google Scholar]
- Hyphantis T, Guthrie E, Tomenson B, Creed F. Psychodynamic interpersonal therapy and improvement in interpersonal difficulties in people with severe irritable bowel syndrome. Pain 2009;145(1‐2):196‐203. [DOI] [PubMed] [Google Scholar]
Dare 2001 {published data only}
- Dare C, Eisler I, Russell G, Treasure J, Dodge L. Psychological therapies for adults with anorexia nervosa: randomised controlled trial of out‐patient treatments. British Journal of Psychiatry 2001;178:216‐21. [DOI] [PubMed] [Google Scholar]
de Jonghe 2001 {published data only}
- Gijsbers Van Wijk CMT, Dekker J, Peen J, Jonghe F. Depression in men and women: sex differences in treatment outcomes of pharmacotherapy and combined therapy. Tijdschrift Voor Psychiatrie 2002;44(5):301‐11. [Google Scholar]
- Henricus L, Schoevers RA, Kool S, Hendriksen M, Peen J, Dekker J. Does early response predict outcome in psychotherapy and combined therapy for major depression?. Journal of Affective Disorders 2008;105(1‐3):261‐5. [DOI] [PubMed] [Google Scholar]
- Jonghe F, Kool S, Aalst J, Dekker J, Peen J. Combining psychotherapy and antidepressants in the treatment of depression. Journal of Affective Disorders 2001;64:217‐29. [Molenaar PJ, Dekker J, Van R, Hendriksen M, Vink A, Schoevers RA. Does adding psychotherapy to pharmacotherapy improve social functioning in the treatment of outpatient depression? Depression and Anxiety 2007;24:553‐62.] [Google Scholar]
Emmelkamp 2006 {published data only}
- Emmelkamp P, Benner A, Kuipers A, Feiertag G, Koster H, Apeldoorn F. Comparison of brief dynamic and cognitive‐behavioural therapies in avoidant personality disorder. British Journal of Psychiatry 2006;189:60‐4. [DOI] [PubMed] [Google Scholar]
Guthrie 1993 {published and unpublished data}
- Guthrie E, Creed F, Dawson D, Tomenson B. A controlled trial of psychological treatment for the irritable bowel syndrome. Gastroenterology 1991;100:450‐7. [DOI] [PubMed] [Google Scholar]
- Guthrie E, Creed F, Dawson D, Tomenson B. A randomised controlled trial of psychotherapy in patients with refractory irritable bowel syndrome. British Journal of Psychiatry 1993;163:315‐21. [DOI] [PubMed] [Google Scholar]
Guthrie 1999 {published data only}
- Guthrie E, Moorey J, Margison F, Barker H, Palmer S, McGrath G, et al. Cost‐effectiveness of brief psychodynamic‐interpersonal therapy in high utilizers of psychiatric services. Archives of General Psychiatry 1999;56:519‐26. [DOI] [PubMed] [Google Scholar]
Guthrie 2001 {published data only}
- Guthrie E, Kapur N, Mackway‐Jones K, Chew‐Graham C, Moorey J, Mendel E, et al. Predictors of outcome following brief psychodynamic‐interpersonal therapy for deliberate self‐poisoning. Australian and New Zealand Journal of Psychiatry 2003;37:532‐6. [DOI] [PubMed] [Google Scholar]
- Guthrie E, Kapur N, Mackway‐Jones K, Chew‐Graham C, Moorey J, Mendel E, et al. Randomised controlled trial of brief psychological intervention after deliberate self poisoning. BMJ 2001;323(7305):135‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 2000 {published data only}
- Hamilton J, Guthrie E, Creed F, Thompson D, Tomenson B, Bennett R, et al. A randomized controlled trial of psychotherapy in patients with chronic functional dyspepsia. Gastroenterology 2000;119:661‐9. [DOI] [PubMed] [Google Scholar]
Levy Berg 2009 {published data only}
- Levy Berg A, Sandell R, Sandahl C. Affect‐focused body psychotherapy in patients with generalized anxiety disorder: evaluation of an integrative method. Journal of Psychotherapy Integration 2009;19(1):67‐85. [Google Scholar]
Linnet 2001 {published and unpublished data}
- Linnet J, Jemec GB. Anxiety level and severity of skin condition predicts outcome of psychotherapy in atopic dermatitis patients. International Journal of Dermatology 2001;40:632‐6. [DOI] [PubMed] [Google Scholar]
Maina 2005 {published data only}
- Maina G, Forner F, Bogetto F. Randomized controlled trial comparing brief dynamic and supportive therapy with waiting list condition in minor depressive disorders. Psychotherapy and Psychosomatics 2005;74:43‐50. [DOI] [PubMed] [Google Scholar]
Maina 2010 {published data only}
- Maina G, Rosso G, Bogetto F. Brief Dynamic Therapy Combined With Pharmacotherapy in the Treatment of Major Depressive Disorder: Long‐Term Results. Journal of Affective Disorders 2009;114(1‐3):200‐7. [DOI] [PubMed] [Google Scholar]
- Maina G, Rosso G, Rigardetto S, Chiadò Piat S, Bogetto F. No effect of adding brief dynamic therapy to pharmacotherapy in the treatment of obsessive‐compulsive disorder with concurrent major depression. Psychotherapy and Psychosomatics 2010;79(5):295‐302. [DOI] [PubMed] [Google Scholar]
Marmar 1988 {published data only}
- Marmar CR, Horowitz MJ, Weiss DS, Wilner NR, Kaltreider NB. A controlled trial of brief psychotherapy and mutual‐help group treatment of conjugal bereavement. American Journal of Psychiatry 1988;145(2):203‐9. [DOI] [PubMed] [Google Scholar]
Milrod 2007 {published data only}
- Busch FN, Milrod BL, Sandberg LS. A study demonstrating efficacy of a psychoanalytic psychotherapy for panic disorder: implications for psychoanalytic research, theory, and practice. Journal of the American Psychoanalytic Association 2009;57(1):131‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graf EP. The relationship of reflective functioning and severity of agoraphobia in the outcome of a psychoanalytic psychotherapy for panic disorder. Dissertation Abstracts International: Section B: the Sciences and Engineering Dissertation Abstracts International 2010; Vol. 70, issue 10‐B:6550.
- Klass ET, Milrod BL, Leon AC, Kay SJ, Schwalberg M, Li C, et al. Does interpersonal loss preceding panic disorder onset moderate response to psychotherapy? An exploratory study. Journal of Clinical Psychiatry Diseases of the Nervous System 2009;70(3):406‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Busch F, Rudden M, Schwalberg M, Clarkin J, Aronson A, et al. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder: erratum. American Journal of Psychiatry 2007;164(7):1123. [DOI] [PubMed] [Google Scholar]
- Milrod B, Leon AC, Busch F, Rudden M, Schwalberg M, Clarkin J, et al. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. American Journal of Psychiatry 2007;164(2):265‐72. [DOI] [PubMed] [Google Scholar]
Monsen 2000 {published data only}
- Monsen K, Monsen JT. Chronic pain and psychodynamic body therapy: a controlled outcome study. Psychotherapy: Theory, Research, Practice, Training 2000;37(3):257‐69. [Google Scholar]
Piper 1990 {published and unpublished data}
- Piper WE, Azim HF, McCallum M, Joyce AS. Patient suitability and outcome in short‐term individual psychotherapy. Journal of Consulting and Clinical Psychology 1990;58(4):475‐81. [DOI] [PubMed] [Google Scholar]
Sattel 2012 {published data only}
- Sattel H, Lahmann C, Gundel H, Guthrie E, Kruse J, Noll‐Hussong M, et al. Brief psychodynamic interpersonal psychotherapy for patients with multisomatoform disorder: randomised controlled trial. British Journal of Psychiatry 2012;100:60‐7. [DOI] [PubMed] [Google Scholar]
Shefler 1995 {published data only}
- Shefler G, Dasberg H, Ben‐Shakhar G. A randomized controlled outcome and follow‐up study of Mann's time‐limited psychotherapy. Journal of Consulting and Clinical Psychology 1995;63(4):585‐93. [DOI] [PubMed] [Google Scholar]
Sloane 1975 {published data only}
- Sloane RB, Staples FR, Cristol AH, Yorkston NJ, Whipple K. Short‐term analytically oriented psychotherapy versus behavior therapy. American Journal of Psychiatry 1975;132(4):373‐7. [DOI] [PubMed] [Google Scholar]
Svedlund 1983 {published and unpublished data}
- Svedlund J, Sjodin I, Ottoson JO, Dotevall G. Controlled study of psychotherapy in irritable bowel syndrome. Lancet 1983;2(8350):589‐92. [DOI] [PubMed] [Google Scholar]
Sørensen 2010 {published data only}
- Sørensen P, Birket‐Smith M, Wattar U, Buemann I, Salkovskis P. A randomised controlled study of cognitive behavioural therapy for hypochondriasis. Proceedings of the 32nd Congress of the British Association for Behavioural and Cognitive Psychotherapies (jointly with the European Association of Behavioural and Cognitive Therapies); 2004 Sept 8‐11; Manchester, UK. 2004.
- Sørensen P, Birket‐Smith M, Wattar U, Buemann I, Salkovskis P. A randomized clinical trial of cognitive behavioural therapy versus short‐term psychodynamic psychotherapy versus no intervention for patients with hypochondriasis. Psychological Medicine 2010;41(2):431‐41. [DOI] [PubMed] [Google Scholar]
Vitriol 2009 {published data only}
- Vitriol VG, Ballesteros ST, Florenzano RU, Weil KP, Benadof DF. Evaluation of an outpatient intervention for women with severe depression and a history of childhood trauma. Psychiatric Services 2009;60(7):936‐42. [DOI] [PubMed] [Google Scholar]
Wiborg 1996 {published data only}
- Wiborg IM, Dahl AA. Does brief dynamic psychotherapy reduce the relapse rate of panic disorder?. Archives of General Psychiatry 1996;53:689‐94. [DOI] [PubMed] [Google Scholar]
Winston 1994 {published data only}
- Winston A, Laikin M, Pollack J, Samstag LW, McCullough L, Muran JC. Short‐term psychotherapy of personality disorders. American Journal of Psychiatry 1994;151(2):190‐4. [DOI] [PubMed] [Google Scholar]
- Winston A, Pollack J, McCullough L, Flegenheimer W, Kestenbaum E, Trujillo M. Brief psychotherapy of personality disorders. Journal of Nervous and Mental Disorders 1991;179:188‐93. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Brodaty 1983 {published data only}
- Brodaty H, Andrews G. Brief psychotherapy in family practice. British Journal of Psychiatry 1983;143:11‐9. [DOI] [PubMed] [Google Scholar]
Budman 1988 {published data only}
- Budman SH, Demby A, Redondo JP, Hannan M, Feldstein M, Ring J, et al. Comparative outcome in time‐limited individual and group psychotherapy. International Journal of Group Psychotherapy 1988;38(1):63‐86. [DOI] [PubMed] [Google Scholar]
Fairburn 1986 {published data only}
- Fairburn CG, Kirk J, O'Connor M, Cooper PJ. A comparison of two psychological treatments for bulimia nervosa. Behavioral Research and Therapy 1986;24(6):629‐43. [DOI] [PubMed] [Google Scholar]
Gallagher 1982 {published data only}
- Gallagher DE, Thompson LW. Treatment of major depressive disorder in older adult outpatients with brief psychotherapies. Psychotherapy: Theory, Research and Practice 1982;19(4):482‐90. [Google Scholar]
Gallagher‐Thompson 1994 {published data only}
- Gallagher‐Thompson D, Steffen A. Comparative effects of cognitive‐behavioral and brief psychodynamic psychotherapies for depressed family caregivers. Journal of Consulting and Clinical Psychology 1994;62(3):543‐9. [DOI] [PubMed] [Google Scholar]
Gilbert 1982 {published data only}
- Gilbert AR. Psychotherapy and clinical depression: an evaluation of cognitive‐behavioral and psychoanalytic modes of therapeutic intervention. Dissertation Abstracts International 1982;43(4B):UMI No. 8220795. [Google Scholar]
Hall 1987 {published data only}
- Hall A, Crisp AH. Brief psychotherapy in the treatment of anorexia nervosa: outcome at one year. British Journal of Psychiatry 1987;151:185‐91. [DOI] [PubMed] [Google Scholar]
Hardy 1995 {published data only}
- Hardy GE, Barkham M, Shapiro DA, Stiles WB, Rees A, Reynolds S. Impact of cluster C personality disorders on outcomes of contrasting brief psychotherapies for depression. Journal of Consulting and Clinical Psychology 1995;63(6):997‐1004. [DOI] [PubMed] [Google Scholar]
Hellerstein 1998 {published data only}
- Hellerstein DJ, Rosenthal RN, Pinsker H, Wallner Samstag L, Muran JC, Winston A. A randomized prospective study comparing supportive and dynamic therapies. Journal of Psychotherapy Practice and Research 1998;7:261‐71. [PMC free article] [PubMed] [Google Scholar]
Knekt 2004 {published data only}
- Knekt P, Lindfors O. A randomized trial of the effect of four forms of psychotherapy on depressive and anxiety disorders. Design, methods, and results on the effectiveness of short‐term psychodynamic psychotherapy and solution‐focused therapy during a one‐year follow‐up [Sataunnaistettu kiininen koe neljan psykoterapiamuodon vaikuttavuudesta masennustiloihin ja ahdistuneisuushairioihin]. Studies in Social Security and Health 2004; Vol. 77, issue 112.
Maina 2009 {published data only}
- Maina G, Rosso G, Bogetto F. Brief dynamic therapy combined with pharmacotherapy in the treatment of major depressive disorder: long‐term results. Journal of Affective Disorders 2009;114:200‐7. [DOI] [PubMed] [Google Scholar]
McLean 1979 {published data only}
- McLean PD, Hakstian AR. Clinical depression: comparative efficacy of outpatient treatments. Journal of Consulting and Clinical Psychology 1979;47(5):818‐36. [DOI] [PubMed] [Google Scholar]
Morris 1975 {published data only}
- Morris NE. A Group Self‐Instruction Method for the Treatment of Depressed Outpatients [doctoral thesis]. Toronto, Canada: University of Toronto, 1975. [Google Scholar]
Nanzer 2012 {published data only}
- Nanzer N, Rossignol AS, Righetti‐Veltema M, Knauer D, Manzano J, Espasa FP. Effects of a brief psychoanalytic intervention for perinatal depression. Archives of Women's Mental Health 2012;15(4):259‐68. [DOI] [PubMed] [Google Scholar]
Piper 1998 {published data only}
- Piper WE, Joyce AS, McCallum M, Azim HF. Interpretive and supportive forms of psychotherapy and patient personality variables. Journal of Consulting and Clinical Psychology 1998;66(3):558‐67. [DOI] [PubMed] [Google Scholar]
Shapiro 1987 {published data only}
- Shapiro DA, Firth J. Prescriptive v. exploratory psychotherapy: outcomes of the Sheffield Psychotherapy Project. British Journal of Psychiatry 1987;151:790‐9. [DOI] [PubMed] [Google Scholar]
Shapiro 1995 {published data only}
- Shapiro DA, Rees A, Barkham M, Hardy G. Effects of treatment duration and severity of depression on the maintenance of gains after cognitive‐behavioral and psychodynamic‐interpersonal psychotherapy. Journal of Counselling and Clinical Psychology 1995;63(3):378‐87. [DOI] [PubMed] [Google Scholar]
Simpson 2003 {published data only}
- Simpson S, Corney R, Fitzgerald P, Beecham J. A randomized controlled trial to evaluate the effectiveness and cost‐effectiveness of psychodynamic counselling for general practice patients with chronic depression. Psychological Medicine 2003;33:229‐39. [DOI] [PubMed] [Google Scholar]
Sjodin 1986 {published and unpublished data}
- Sjodin I, Svedlund J, Ottoson JO, Dotevall G. Controlled study of psychotherapy in chronic peptic ulcer disease. Psychosomatics 1986;27(3):187‐200. [DOI] [PubMed] [Google Scholar]
Svartberg 2004 {published data only}
- Svartberg M, Stiles TC, Seltzer MH. Randomized, controlled trial of the effectiveness of short‐term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. American Journal of Psychiatry 2004;161(5):810‐7. [DOI] [PubMed] [Google Scholar]
Thompson 1987 {published data only}
- Thompson LW, Gallagher D, Breckenridge JS. Comparative effectiveness of psychotherapies for depressed elders. Journal of Consulting and Clinical Psychology 1987;55(3):385‐90. [DOI] [PubMed] [Google Scholar]
Vinnars 2005 {published data only}
- Vinnars B, Barber J, Noren K, Gallop R, Weinryb R. Manualized supportive‐expressive therapy versus nonmanualized community‐delivered psychodynamic therapy for patients with personality disorders: bridging efficacy and effectiveness. American Journal of Psychiatry 2005;162(10):1933‐40. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Barber 2012 {published data only}
- Barber JP, Barrett MS, Gallop R, Rynn MA, Rickels K. Short‐term dynamic psychotherapy versus pharmacotherapy for major depressive disorder: a randomized, placebo‐controlled trial. Journal of Clinical Psychiatry 2012;73(1):66‐73. [DOI] [PubMed] [Google Scholar]
Beutel 2014 {published data only}
- Beutel ME, Weißflog G, Leuteritz K, Wiltink J, Haselbacher A, Ruckes C, et al. Efficacy of short‐term psychodynamic psychotherapy (STPP) with depressed breast cancer patients: results of a randomized controlled multicenter trial. Annals of Oncology 2014;25(2):378‐84. [DOI] [PubMed] [Google Scholar]
- Haselbacher A, Barthel Y, Brahler E, Imruck B, Kuhnt S, Zwerenz R, et al. Psychodynamic short‐term therapy for cancer patients suffering from depression A treatment manual on the basis of Luborsky's supportive‐expressive therapy. Psychotherapeut Praxis der Psychotherapie Und Psychosomatik 2010;55(4):321‐8. [Google Scholar]
- Leuteritz K, Brahler E, Weisflog G, Barthel Y, Kuhnt S, Zwerenz R, et al. Efficacy and predictors of outcome of short‐term psychodynamic psychotherapy (STPP) in depressed breast cancer patients: A randomised controlled trial. Journal of Psychosomatic Research 2013;74(6):552. [Google Scholar]
Bressi 2011 {published data only}
- Bressi C, Ciabatti M, Nocito EP, Catenacci E, Porcellana M, Invernizzi G, et al. A preliminary longitudinal study on the importance of early intervention in panic disorder. Journal of Psychosomatic Research 2010;68(6):610. [Google Scholar]
Faramarzi 2013 {published data only}
- Faramarzi M, Azadfallah P, Book HE, Tabatabaei KR, Taheri H, Shokri‐shirvani J. A randomized controlled trial of brief psychoanalytic psychotherapy in patients with functional dyspepsia. Asian Journal of Psychiatry 2013;6(3):228‐34. [DOI] [PubMed] [Google Scholar]
Gibbons 2012 {published data only}
- Gibbons MB, Thompson SM, Scott K, Schauble LA, Mooney T, Thompson D, et al. Supportive‐expressive dynamic psychotherapy in the community mental health system: a pilot effectiveness trial for the treatment of depression. Psychotherapy (Chicago, Ill.) 2012;49(3):303‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kompoliti 2014 {published data only}
- Kompoliti K, Wilson B, Stebbins G, Bernard B, Hinson V. Immediate vs. delayed treatment of psychogenic movement disorders with short term psychodynamic psychotherapy: randomized clinical trial. Parkinsonism and Related Disorders 2014;20(1):60‐3. [DOI] [PubMed] [Google Scholar]
Leichsenring 2013 {published data only}
- Leichsenring F, Hoyer J, Beutel M, Herpertz S, Hiller W, Irle E, et al. The social phobia psychotherapy research network ‐ The first multicenter randomized controlled trial of psychotherapy for social phobia: Rationale, methods and patient characteristics. Psychotherapy and Psychosomatics Acta Psychotherapeutica 2009;78(1):35‐41. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Salzer S, Beutel ME, Herpertz S, Hiller W, Hoyer J, et al. Long‐term outcome of psychodynamic therapy and cognitive‐behavioral therapy in social anxiety disorder. American Journal of Psychiatry (In press). [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Salzer S, Beutel ME, Herpertz S, Hiller W, Hoyer J, et al. Psychodynamic therapy and cognitive‐behavioral therapy in social anxiety disorder: a multicenter randomized controlled trial [SOPHO‐NET]. American Journal of Psychiatry 2013;170(7):759‐67. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Salzer S, Beutel ME, Consbruch K, Herpertz S, Hiller W, et al. SOPHO‐NET ‐‐ A research network on psychotherapy for social phobia. Psychotherapie, Psychosomatik, Medizinische Psychologie 2009;59(3‐4):117‐23. [DOI] [PubMed] [Google Scholar]
- Ritter V, Leichsenring F, Strauss BM, Stangier U. Changes in implicit and explicit self‐esteem following cognitive and psychodynamic therapy in social anxiety disorder. Psychotherapy Research 2013;23(5):547‐58. [DOI] [PubMed] [Google Scholar]
Reneses 2013 {published data only}
- Reneses B, Galin M, Serrano R, Figuera D, Salcedo G, Moral AF, et al. A new time limited psychotherapy for BPD: preliminary results of a randomized and controlled trial [Una nueva psicoterapia breve para trastornoslímite de la personalidad. Resultados preliminaresde un ensayo controlado y aleatorizado]. Actas Españolas de Psiquiatría 2013;41(3):139‐48. [PubMed] [Google Scholar]
Scheidt 2013 {published data only}
- Scheidt CE, Waller E, Endorf K, Schmidt S, Konig R, Zeeck A, et al. Is brief psychodynamic psychotherapy in primary fibromyalgia syndrome with concurrent depression an effective treatment? A randomized controlled trial. General Hospital Psychiatry 2013;35(2):160‐7. [DOI] [PubMed] [Google Scholar]
Shaw 2001 {published data only}
- Shaw CM, Margison FR, Guthrie EA, Tomenson B. Psychodynamic interpersonal therapy by inexperienced therapists in a naturalistic setting: a pilot study. European Journal of Psychotherapy, Counselling and Health European Journal of Psychotherapy and Counselling 2001;4(1):87‐101. [Google Scholar]
Zipfel 2014 {published data only}
- Wild B, Friederich H‐C, Gross G, Teufel M, Herzog W, Giel KE, et al. The ANTOP study: focal psychodynamic psychotherapy, cognitive‐behavioural therapy, and treatment‐as‐usual in outpatients with anorexia nervosa ‐ a randomized controlled trial. Trials 2009;10:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zipfel S, Wild B, Groß G, Friederich HC, Teufel M, Schellberg D, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet 2014;383(9912):127‐37. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN38209986 {published data only}
- ISRCTN38209986. Psychodynamic Psychotherapy in Primary Care: A Randomised Study to evaluate the effectiveness of Dynamic Interpersonal Therapy (DIT). http://www.controlled‐trials.com/ISRCTN38209986 (accessed 15 May 2014).
NCT01141426 {published data only}
- NCT01141426. Halifax Treatment Refractory Depression Trial: A Randomized Controlled Trial of Intensive Short‐Term Dynamic Psychotherapy (ISTDP) Compared to Secondary Care Treatment as Usual. clinicaltrials.gov/ct2/show/NCT01141426 (accessed 6 May 2014).
NCT02076867 {published data only}
- NCT02076867. Halifax Somatic Symptom Disorder Trial: A Randomized Parallel Group Cross‐Over Study of Intensive Short‐Term Dynamic Psychotherapy Compared to Medical Treatment as Usual for Somatic Symptoms in the Emergency Department. http://clinicaltrials.gov/ct2/show/NCT02076867 (accessed 15 May 2014).
Additional references
Abbass 2006
- Abbass AA, Henderson J, Kisely S, Hancock JT. Short‐term psychodynamic psychotherapies for common mental disorders. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD004687.pub3] [DOI] [PubMed] [Google Scholar]
Abbass 2009
- Abbass A, Kisely S, Kroenke K. Short‐term psychodynamic psychotherapy for somatic symptom disorders: a systematic review and meta‐analysis. Psychotherapy and Psychosomatics 2009;78:265‐74. [DOI] [PubMed] [Google Scholar]
Abbass 2010
- Abbass A, Driessen E. The efficacy of short‐term psychodynamic psychotherapy for depression: a summary of recent findings. Acta Psychiatrica Scandinavica 2010;121:398‐9. [DOI] [PubMed] [Google Scholar]
Abbass 2011
- Abbass A, Driessen E, Town J. The efficacy of short‐term psychodynamic psychotherapy for depressive disorders with comorbid personality disorder. Psychiatry 2011;74:58‐71. [DOI] [PubMed] [Google Scholar]
Abbass 2012
- Abbass A, Town J, Driessen E. Intensive short‐term dynamic psychotherapy: a systematic review and meta‐analysis of outcome research. Harvard Review of Psychiatry 2012;20:97‐108. [DOI] [PubMed] [Google Scholar]
Anderson 1995
- Anderson E, Lambert M. Short‐term dynamically oriented psychotherapy: a review and meta‐analysis. Clinical Psychology Review 1995;15(6):503‐14. [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4(6):561‐71. [DOI] [PubMed] [Google Scholar]
Blagys 2000
- Blagys MD, Hilsenroth MJ. Distinctive activities of short‐term psychodynamic‐interpersonal psychotherapy: a review of the comparative psychotherapy process literature. Clinical Psychology: Science and Practice 2000;7:167‐88. [Google Scholar]
Chandler 2013
- Chandler J, Churchill R, Higgins J, Lasserson T, Tovey D. Methodological standards for the conduct of new Cochrane intervention reviews, 2013. www.editorial‐unit.cochrane.org/sites/editorial‐unit.cochrane.org/files/uploads/MECIR_conduct_standards%202.3%2002122013.pdf (accessed 6 May 2014).
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition. Hillsdale, NJ: Lawrence Erlbaum, 1988. [Google Scholar]
Cook 2010
- Cook JM, Biyanova T, Elhai J, Schnurr PP, Coyne JC. What do psychotherapists really do in practice? An internet study of over 2000 practitioners. Psychotherapy: Theory, Research, Practice,Training 47:260‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cramer 1990
- Cramer B, Robert‐Tissot C, Stern D, Serpa‐Rusconi S, Muralt M, Besson G, et al. Outcome evaluation in brief mother‐infant psychotherapy. Infant Mental Health Journal 1990;11:278‐300. [Google Scholar]
Crits‐Christoph 1992
- Crits‐Christoph P. The efficacy of brief dynamic psychotherapy: a meta‐analysis. American Journal of Psychiatry 1992;149(2):151‐8. [DOI] [PubMed] [Google Scholar]
Davanloo 1980
- Davanloo H. Short‐Term Dynamic Psychotherapy. New York, NY: Jason Aronson, 1980. [Google Scholar]
Davanloo 2000
- Davanloo H. Intensive Short‐term Dynamic Psychotherapy. Chichester, UK: John Wiley & Sons, 2000. [Google Scholar]
de Jonghe 1994
- Jonghe F, Rijnierse P, Janssen R. Psychoanalytic supportive psychotherapy. Journal of American Psychoanalytic Association 1994;42:421‐46. [DOI] [PubMed] [Google Scholar]
Derogatis 1994
- Derogatis LR. Symptom Checklist‐90 ‐ Revised: Administration, Scoring, and Procedures Manual. 3rd Edition. Minneapolis, MN: National Computers Systems, 1994. [Google Scholar]
Dewald 1964
- Dewald PA. A Dynamic Approach. Oxford: Blackwell Scientific Publications, 1964. [Google Scholar]
Diener 2007
- Diener M, Hilsenroth M, Weinberger J. Therapist affect focus and patient outcomes in psychodynamic psychotherapy: a meta‐analysis. American Journal of Psychiatry 2007;164:936‐41. [DOI] [PubMed] [Google Scholar]
Driessen 2010
- Driessen E, Cuijpers P, Maat S, Abbass A, Jonghe F, Dekker J. The efficacy of short‐term psychodynamic psychotherapy for depression: a meta‐analysis. Clinical Psychology Review 2010;30:25‐36. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder CE. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
EuroQol 1990
- EuroQol. EuroQol ‐ a new facility for the measurement of health related quality of life. Health Policy 1990;16:199‐208. [DOI] [PubMed] [Google Scholar]
Felitti 1998
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine 1998;14(4):245‐58. [DOI] [PubMed] [Google Scholar]
Hamilton 1959
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology 1959;32:50‐5. [DOI] [PubMed] [Google Scholar]
Henningsen 2011
- Henningsen P. Psychodynamic interpersonal therapy for somatoform disorders ‐ a manualized short‐term psychotherapy. In: Beutel M, Doering S, Leichsenring F, Reich G editor(s). In Practice of Psychodynamic Psychotherapy. Oxford: Hogrefe, 2011. [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008a
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Higgins 2008b
- Higgins JPT, Altman DG, editors. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Hobson 1985
- Hobson RF. Forms of Feeling: the Heart of Psychotherapy. London: Tavistock Publications, 1985. [Google Scholar]
Horowitz 1976
- Horowitz MJ. Stress Response Syndromes. New York: Aronson, 1976. [Google Scholar]
Horowitz 1984
- Horowitz M, Marmar C, Krupnick J, Wilner N, Kaltreider N, Wallerstein R. Personality Styles and Brief Psychotherapy. New York: Basic Books, 1984. [Google Scholar]
Horowitz 1988
- Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of interpersonal problems: psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology 1988;56:885‐92. [DOI] [PubMed] [Google Scholar]
Lazar 2010
- Lazar SG. Psychotherapy is Worth it: a Comprehensive Review of its Cost‐effectiveness. Arlington, VA: American Psychiatric Publishing, 2010. [Google Scholar]
Leichsenring 2004
- Leichsenring F, Rabung S, Leibing E. The efficacy of short‐term psychodynamic psychotherapies in specific psychiatric disorders. Archive of General Psychiatry 2004;61:1208‐16. [DOI] [PubMed] [Google Scholar]
Leichsenring 2014
- Leichsenring F, Klein S. Evidence for psychodynamic psychotherapy in specific mental disorders: a systematic review. Psychoanalytic Psychotherapy 2014;28(1):4‐32. [Google Scholar]
Lemma 2010
- Lemma A, Target M, Fonagy P. The development of a brief psychodynamic protocol for depression: dynamic interpersonal therapy (DIT). Psychoanalytic Psychotherapy 2010;24:4:329‐46. [Google Scholar]
Luborsky 1984
- Luborsky L. Principles of Psychoanalytic Psychotherapy: a Manual for Supportive‐Expressive Treatment. New York: Basic Books, 1984. [Google Scholar]
Malan 1976
- Malan D. The Frontier of Brief Psychotherapy. New York: Plenum, 1976. [Google Scholar]
Malan 1979
- Malan D. Individual Psychotherapy and the Science of Psychodynamics. London: Butterworth, 1979. [Google Scholar]
Malan 1986
- Malan D. Beyond interpretation: initial evaluation and technique in short‐term dynamic psychotherapy. International Journal of Intensive Short‐Term Dynamic Psychotherapy 1986;1:59‐82. [Google Scholar]
Malan 1992
- Malan D, Osimo F. Psychodynamics, Training, and Outcome in Brief Psychotherapy. Oxford: Butterworth‐Heinemann, 1992. [Google Scholar]
Malhi 2009
- Malhi GS, Adams D, Porter R, Wignall A, Lampe L, O'Connor N, et al. Clinical practice recommendations for depression. Acta Psychiatrica Scandinavica 2009;119:8‐26. [DOI] [PubMed] [Google Scholar]
Mann 1973
- Mann J. Time Limited Psychotherapy. Cambridge: Harvard University Press, 1973. [Google Scholar]
McCullough 2003
- McCullough L, Kuhn N, Andrews S, Kaplan A, Wolf J, Hurley CL. Treating Affect Phobia. A Manual for Short‐Term Dynamic Psychotherapy. New York: Guilford Press, 2003. [Google Scholar]
Melzack 1975
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975;1:277‐99. [DOI] [PubMed] [Google Scholar]
Messer 1995
- Messer SB, Warren CS. Models of Brief Psychodynamic Therapy: a Comparative Approach. New York: Guilford, 1995. [Google Scholar]
Milrod 1997
- Milrod B, Busch F, Cooper A, Shapiro T. Manual of Panic Focused Psychodynamic Psychotherapy. Arlington: American Psychiatric Publishing, 1997. [Google Scholar]
Monsen 1999
- Monsen JT, Monsen K. Affects and affect consciousness ‐ a psychotherapy model integrating Silvan Tomkins' affect and script theory within the framework of self‐psychology. Progress in Self‐Psychology 1999;15:287‐306. [Google Scholar]
Norcross 2013
- Norcross JC, Rogan JD. Psychologists conducting Psychotherapy in 2012: current practices and historical trends among Division 29 members. Psychotherapy (Chic) 2012;50(4):490‐5. [DOI] [PubMed] [Google Scholar]
Pollack 1991
- Pollack J, Flegenheimer W, Winston A. Brief adaptive psychotherapy. In: Crits‐Christoph P, Barber J editor(s). Handbook of Short‐Term Dynamic Psychotherapy. New York: Basic Books, 1991:199‐219. [Google Scholar]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Shedler 2010
- Shedler J. The efficacy of psychodynamic psychotherapy. American Psychologist 2010;February‐March:98‐109. [DOI] [PubMed] [Google Scholar]
Sifneos 1972
- Sifneos P. Short‐Term Psychotherapy and Emotional Crisis. Cambridge: Harvard University Press, 1972. [Google Scholar]
Stern 1995
- Stern D. The Motherhood Constellation. New York: Basic Books, 1995. [Google Scholar]
Strupp 1984
- Strupp HH, Binder JL. Psychotherapy in a New Key: a Guide to Time Limited Dynamic Psychotherapy. New York: Basic, 1984. [Google Scholar]
Svartberg 1991
- Svartberg M, Stiles T. Comparative effects of short‐term psychodynamic psychotherapy: a meta‐analysis. Journal of Consulting and Clinical Psychology 1991;59(5):704‐14. [DOI] [PubMed] [Google Scholar]
Town 2011
- Town J, Abbass A, Hardy G. Short‐term psychodynamic psychotherapy for personality disorders: a critical review of randomised controlled trials. Journal of Personality Disorders 2011;26(6):723‐40. [DOI] [PubMed] [Google Scholar]
Town 2012
- Town JM, Diener MJ, Abbass A, Leichsenring F, Driessen E, Rabung S. A meta‐analysis of psychodynamic psychotherapy outcomes: evaluating the effects of research‐specific procedures. Psychotherapy 2012;49(3):276‐90. [DOI] [PubMed] [Google Scholar]
Town 2013
- Town JM, Driessen E. Emerging evidence for intensive short‐term dynamic psychotherapy with personality disorders and somatic disorders. Psychiatric Annals 2013;43(11):502‐7. [Google Scholar]
Ulvenes 2012
- Ulvenes PG, Berggraf L, Hoffart A, Stiles TC, Svartberg M, McCullough L, et al. Different processes for different therapies: therapist actions, therapeutic bond, and outcome. Psychotherapy 2012;49:291‐302. [DOI] [PubMed] [Google Scholar]
Weissman 1978
- Weissman MM, Prusoff BA, Thompson DW, Harding PS, Myers JK. Social adjustment by self‐report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease 1978;166:317‐26. [DOI] [PubMed] [Google Scholar]
Werman 1984
- Werman DS. The Practice of Supportive Psychotherapy. New York: Brunner/Mazel, 1984. [Google Scholar]
Wittchen 2011
- Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology 2011;21:655‐79. [DOI] [PubMed] [Google Scholar]


