Abstract
Background Distal radius fractures are commonly seen among the elderly, though studies examining their long-term outcomes are limited.
Purpose The aim of this study was to describe the 5-year trajectory of recovery of distal radius fractures treated with open reduction and internal fixation (ORIF).
Methods Patients with distal radius fractures (AO/OTA 23.A-C) treated by ORIF were prospectively studied. Patient-Rated Wrist Evaluation (PRWE) score was measured at baseline (preinjury recall) and postoperatively at 6 months, 1 year, and 5 years. Clinically relevant change in PRWE score was assessed using the minimal clinically important difference (MCID).
Results A total of 390 patients were included, of which 75% completed 5-year follow-up. Mean baseline PRWE score was 1.25 (standard deviation, SD: 2.9). At 6 months, mean PRWE score was at its highest up to 20.2 (SD: 18.4; p < 0.01). A significant improvement in mean PRWE score was observed at 1 year down to 15.2 (SD: 17.6; p < 0.01); 44% of patients were still one MCID outside of their baseline PRWE score at 1 year. Further significant improvement in mean PRWE score occurred at 5 years down to 9.4 (SD: 13.4; p < 0.01); 29% of patients remained one MCID outside of their baseline PRWE score at 5 years.
Conclusion Recovery after ORIF for distal radius fractures showed significant worsening after surgery, followed by significant improvements up to 1 year and between years 1 and 5, albeit to a lesser extent. Statistically and clinically relevant wrist pain and disability persisted at 5 years. Future research should examine different treatment modalities and include a nonoperative treatment arm for comparison.
Level of Evidence Prognostic level II.
Keywords: radius, fracture, wrist, PRWE, MCID, patient-reported outcome measure, trajectory, disability, ORIF, trauma
Distal radius fractures are common injuries. 1 They present as a bimodal distribution, with a first peak in the pediatric population (10–14 years of age) and a second peak in the elderly (>65 years of age). 1 Treatment in the pediatric population commonly involves closed reduction and casting, while treatment in the adult and elderly population is more controversial. Improved understanding of disabilities associated with these injuries, and their trajectory of recovery, is vital to fracture management and studies aimed at decreasing overall burden. 2
Previous research has focused on outcomes of different treatment regimens for distal radius fractures, albeit with measurements at varied time points. 3 4 5 6 7 8 9 Limited studies have observed the trajectory of recovery after distal radius fracture using responsive measures. Modarresi et al 7 reported recovery trajectory for a range of treatments in 318 patients and found a significant improvement in Patient-Rated Wrist Evaluation (PRWE) score by 3 to 6 months postfacture. However, their lack of preinjury measurement precluded comparison to baseline and their follow-up ending at 1 year limited commentary on further progression. Thorninger et al 10 reported Disability of the Arm, Shoulder and Hand (DASH) scores for 50 patients treated nonoperatively and found that their patients returned to a preinjury DASH score by 1 year postinjury. Rozental et al 11 examined 45 distal radius fracture patients who underwent closed reduction and pin fixation or open reduction and internal fixation (ORIF) with a volar plate, and showed the latter had superior DASH scores at 6-, 9-, and 12-week follow-up, while DASH scores improved significantly at 1-year follow-up regardless of technique. Ingall et al 12 reported 96% of the 80 patients who completed final follow-up achieved one QuickDASH minimal clinically important difference (MCID) by 1 year, while over 80% of total expected functional improvement was achieved by 3 to 6 months after surgery. These three studies did not report beyond 1 year, and the DASH measurement tool has been shown to be less responsive than the PRWE in this injury population. 13
The aim of our study was to characterize the trajectory of recovery of patients after distal radius fracture treated with an ORIF. To better illustrate patient recovery, this study includes a baseline preinjury recall score as well as follow-up out to 5 years after surgery.
Patients and Methods
Patients
Patients over 16 years of age with a distal radius fracture (AO-Muller/Orthopaedic Trauma Association [AO/OTA] 23.A-C) treated with ORIF were approached for enrolment into a prospective database study at a single level 1 trauma center between 2005 and 2013. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and received ethics approval from the clinical research ethics board at our institution. Necessary and appropriate informed consent was obtained from all patients before enrollment. We adhered to Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
The decision to treat the distal radius fracture with ORIF was made by one of six fellowship trained orthopaedic trauma surgeons at the time of injury based on the following criteria: level of patient functional demand and number of comorbidities, fracture pattern (e.g., depressed articular fracture, fracture dislocation of the radiocarpal joint), fracture displacement, and alignment following closed reduction (e.g., >5-mm shortening of the radial height, >2-mm articular step off, volar angulation, or increased dorsal angulation more than 20 degrees of the contralateral side). Demographics, medical comorbidities, injury severity score (ISS), age, and sex were recorded at the time of injury.
Functional Outcomes
Patient-reported outcome measures (PROMs) were collected at baseline using preinjury recall (up to 2 weeks after their index visit) and then again after surgery at 6-month, 1-year, and 5-year follow-up (until 2018) using the PRWE questionnaire. 14 Previous studies have shown the ability for patients to accurately recall their preoperative function 2 weeks after elective knee arthroscopy, as well as up to 6 weeks after hip arthroplasty surgery. 15 16 The PRWE is a validated questionnaire that provides a score specific to wrist pathology to assess pain and function. PRWE scores add up to a maximum of 100 points, with 0 being no disability and 100 representing worst disability. The PRWE is a superior measure of functional change over time compared with other PROMs, especially with regard to floor and ceiling effects, which occur when substantial proportions of individuals obtain either minimum or maximum scores, thus skewing the distribution of scores, and the true extent of their abilities cannot be determined (i.e., floor effect: 1% at baseline, 9% at 6 months, 6% at 1 year; ceiling effect: 75% at baseline, 8% at 6 months, 17% at 1 year). 17
Statistics
The mean difference in PRWE scores between each time point was calculated with a repeated-measures analysis of variance with a post hoc t -test corrected with Bonferroni. The use of MCID, defined as the minimal improvement in an outcome score for patient-perceived clinical improvement, 18 provides a patient-focused clinical relevance that can highlight the real impact of specific treatments on functionality and quality of life. 17 19 20 21 Previous studies have reported MCID for PRWE scores between 9 and 17 points, depending on injuries and pathologies. 22 23 Walenkamp et al, 22 who determined MCID for PRWE scores in patients with distal radius fractures using an anchor-based questionnaire approach, defined MCID as a difference of 11.5. This MCID point differential has not been widely cited nor utilized by other authors—potentially because of methodological differences, specifically that the weeks from trauma to the second PRWE measurement in this study was a median of 16 weeks, but with an interquartile range of 13 to 52 weeks. 22 Another way to define MCID, specific to a pathology and a population, has been described by Norman et al 24 wherein they defined half the standard deviation (SD) as a threshold that corresponds to the MCID for any health-related quality of life questionnaire. As there is no widely accepted MCID for PRWE scores, we employed the method proposed by Norman et al 24 for our MCID calculation as we felt it more appropriate to utilize our own patient data for the calculation. Consequently, we used one-half of the SD at 6-month follow-up to calculate our MCID, as the 6-month time point was when our patients were maximally affected by this injury in their recovery journey (as opposed to 1-year or 5-year follow-up). The MCID in PRWE scores we calculated was 9.2 points. We used a chi-squared test to evaluate the improvement in individual patients and compare the proportion of patients achieving MCID at each time point.
Results
A total of 447 eligible patients were enrolled. Of these, 57 were excluded because of an incomplete dataset (i.e., missing data from ≥2 of the following time points: baseline [preinjury recall], 6 months, or 1 year). Therefore, 390 patients were included in this study; overall, 367 patients (94%) completed baseline (preinjury recall); 380 patients (97%) completed 6-month follow-up; 319 patients (82%) completed 1-year follow-up; and 294 patients (75%) completed 5-year follow-up. Results at the overall group level compiled from the PROMs completed at each respective time point—which is a common technique to counteract the problematic lost-to-follow-up rates seen in orthopaedic trauma research—are discussed and presented in Table 1 and Fig. 1 . Results calculated at the individual patient level—where it matters most in relation to the proportion of patients meeting MCID—are discussed and presented in Table 2 .
Table 1. Patients demographics.
| Demographic | N | Value |
|---|---|---|
| Sex | ||
| Male | 125 | 32.0% |
| Female | 265 | 68.0% |
| Age (y) | 51 | Range: 17–93 |
| Injury severity score | ||
| 9 | 378 | 97.0% |
| > 9 | 12 | 3.0% |
| Multiple medical comorbidities (≥3) | 35 | 9.0% |
| History of mental illness | 18 | 4.6% |
| Secondary surgical procedure | 41 | 10.4% |
| Revision ORIF/acute failure | 5 | 1.3% |
| Planned staged procedure (i.e., removal of bridge or dorsal plates) | 7 | 1.8% |
| Elective or delayed hardware removal | 29 | 7.4% |
Abbreviation: ORIF, open reduction and internal fixation.
Fig. 1.
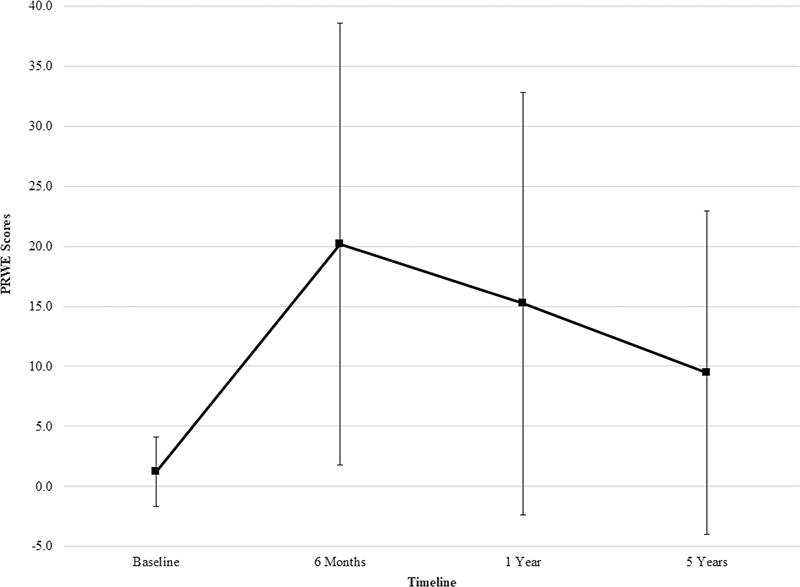
Trajectory of recovery according to Patient-Rated Wrist Evaluation (PRWE) scores. Error bars represent the standard deviation (SD) in mean PRWE scores at each time point.
Table 2. Breakdown of minimal clinically important difference (MCID) trajectory for Patient-Rated Wrist Evaluation (PRWE) scores.
| Time point | 6 mo | 1 y | 5 y |
|---|---|---|---|
| Proportion of patients improving at least one MCID in PRWE score from their last time point | Reference | 29% | 22% |
| Proportion of patients remaining one MCID outside of their baseline PRWE score | 62% | 44% | 29% |
Abbreviation: MCID, minimal clinically important difference; PRWE, Patient-Rated Wrist Evaluation.
Patient demographics are shown in Table 1 . Mean age was 51 years old. One-third of patients (32%) were male. Most patients (97%) had an ISS score of 9 (i.e., isolated injuries), while 35 (9%) patients had multiple comorbidities (>3). The 41 patients (9%) who had a secondary surgical procedure on average 404 days (SD: 351 days; range: 4–1,777 days) after their initial ORIF at our center can be categorized as follows: complication from initial surgery and thus required an unplanned remedial operation, or underwent a planned staged procedure (median: 45 days; range 4–226 days); or needed an elective or delayed instrumentation extraction (median: 384 days; range: 55–1,777).
The mean baseline preinjury recall PRWE score was 1.25 (SD: 2.9). The trajectory of recovery indicated an increase (i.e., worsening) in PRWE scores at 6 months after surgery, such that mean PRWE scores were at their highest levels of disability (mean: 20.2; SD: 18.4), after which they began to improve at 1 year (mean: 15.2; SD: 17.6). PRWE scores improved again—as shown by the continuing downward trajectory slope—at 5-year follow-up (mean: 9.4; SD: 13.4) ( Fig. 1 ). The difference in PRWE scores between each time point was statistically significant ( p < 0.05).
With respect to MCID in PRWE scores, at 6 months 62% of patients were more than one MCID away from baseline preinjury recall scores. Between 6 months and 1 year, 29% of patients improved their PRWE score by at least one MCID. However, at 1 year 44% of patients were still more than one MCID from baseline preinjury recall scores. Between 1 year and 5 years, 22% of patients improved their PRWE score by at least one MCID. At 5 years, 29% of patients were not back within one MCID from their baseline level of functionality ( Table 2 ).
Discussion
Our study of the trajectory of recovery for distal radius fractures treated with ORIF illustrates that these injuries have a long-lasting impact on patient function. We showed a decrease in function postsurgery with disability still present at 6 months, followed thereafter by significant improvements up to 1 year postsurgery. However, even 5 years postsurgery, almost a third of patients (29%) still had clinically relevant disability compared with their baseline preinjury levels of function.
A previous trajectory study looking at the 1-year recovery of distal radius fractures treated nonoperatively showed that in 50 patients aged 65 years and older, most were back to a preinjury DASH score at 1 year. 10 Another study looking at the trajectory of recovery in 318 patients aged 20 to 87 years reported a significant decrease in the PRWE score from postinjury to 1 year. 7 Our findings add to the literature by incorporating baseline preinjury recall, as well as a long-term follow-up out to 5 years. It is worth noting that our mean PRWE scores were similar to those reported by Modarresi et al 7 at 6-month and 1-year follow-up.
A strength of our study is the use of MCID to evaluate and better characterize the evolution of PRWE scores over time. Previous trajectory recovery studies evaluating a different pathology have used MCID to good effect to evaluate the impact of treatment on their patients. 17 19 20 21 Our results showed that at 6 months, almost two-thirds of the patients were still more than one MCID away from their baseline preinjury recall level, close to 50% of patients were not back within one MCID of their baseline preinjury recall levels at 1 year, and almost 30% of patients were similarly deficient still at 5 years. To our knowledge, we are the first to use MCID to analyze return to baseline preinjury recall function in examining distal radius fractures, and that may account for the differences in our findings. A previous study by Ingall et al 12 showed MCID improvement in 96% of their patients from the postinjury DASH score to the 1-year follow-up. However, only 45% of their patients completed the 1-year questionnaire, and they did not record a baseline preinjury score. A similar study by Thorninger et al 10 reported no statistical differences in DASH scores at 1-year follow-up compared with baseline preinjury recall. However, they did not report the percentage of patients achieving MCID in relation to their baseline preinjury score. Therefore, it is possible that the true impact of distal radius fractures on long-term recovery may have been underestimated in these two previous studies.
The main limitation of our study is that 41% of patients were missing one of their PRWE scores at either 6-month, 1-year, or 5-year follow-up (i.e., only 229 patients [59%] had a complete PROMs dataset inclusive from every time point). High rates of lost-to-follow-up are a known drawback of research dealing with high-energy trauma patients referred from a wide catchment area to a level 1 trauma center. 25 26 However, the overall PROMs completion rates we observed at the overall group level at each respective time point accumulatively were very high for our patient sample (75–97%), so we feel confident with the trajectory data presented herein. Most importantly, we focused on individual patient-level data to calculate the proportional changes in MCID between time points, thus showcasing clinically relevant change in PRWE score. Unfortunately, our capture of secondary surgical procedures was limited by the data availability from a single-center cohort. Another limitation was the lack of a nonoperative conservative treatment group to act as a comparison, as well as the fact that we did not evaluate each patient's dominant handedness. We also did not consider any differences between patients still working versus retired, nor did we account for patients' rehabilitation programs and how consistently they were undertaken, and we did not record any other conditions (e.g., trauma, disease) the patient may have developed from year 1 to year 5 that could have affected their trajectory of the recovery. Nonetheless, we feel that the design of our study and the heterogenous patient cohort lend itself to increasing the overall generalizability of the results. It is worth noting that our patients' mean baseline preinjury recall PRWE score of 1.25 (SD: 2.9) differs from a population-based normative PRWE score of 7.7 (SD: 15.0) identified by Mulders et al 27 in their study of 1,042 individuals from the normal population. Thus, it is possible that our patients overestimated their preinjury functional levels. Finally, the lack of an interim time point between baseline preinjury recall and 6-month follow-up could be perceived as a limitation if most of the recovery occurs within the first 6 months after surgery. However, many trajectory studies have been published using 6-month follow-up as the first questionnaire data point, 17 19 20 21 and the focus of our study is to assess residual disability by following up patients out to 5 years postsurgery.
Conclusion
In conclusion, we report the longer term trajectory of recovery of patients with distal radius fractures treated with ORIF. The trajectory of recovery showed worsening of PRWE scores after injury with substantial disability at 6 months. PRWE scores significantly improved between 6 months and 1 year, and continued to improve, albeit to a lesser extent, up to 5 years after surgery. Statistically and clinically relevant wrist disability persisted at 5 years postinjury. Future research should focus on the long-term trajectory of recovery of different treatment modalities for distal radius fractures and include a nonoperative treatment arm for comparison.
Acknowledgment
None.
Funding Statement
Funding/Sponsorship This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest None declared.
Informed Consent
Necessary and appropriate informed consent was obtained from all patients before enrollment.
Institutional Ethical Committee Approval (for All Human Studies)
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and received ethics approval from the clinical research ethics board at our institution.
References
- 1.Azad A, Kang H P, Alluri R K, Vakhshori V, Kay H F, Ghiassi A. Epidemiological and treatment trends of distal radius fractures across multiple age groups. J Wrist Surg. 2019;8(04):305–311. doi: 10.1055/s-0039-1685205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shauver M J, Yin H, Banerjee M, Chung K C. Current and future national costs to medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36(08):1282–1287. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 3.Fogel N, Mertz K, Shapiro L M, Roe A, Denduluri S, Kamal R N.Outcome metrics in the treatment of distal radius fractures in patients aged above 50 years: a systematic review Hand (N Y) 202217(1_suppl):43S–49S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anzarut A, Johnson J A, Rowe B H, Lambert R GW, Blitz S, Majumdar S R. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29(06):1121–1127. doi: 10.1016/j.jhsa.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23(04):237–242. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 6.Grewal R, MacDermid J C, Pope J, Chesworth B M. Baseline predictors of pain and disability one year following extra-articular distal radius fractures. Hand (N Y) 2007;2(03):104–111. doi: 10.1007/s11552-007-9030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Modarresi S, Suh N, Walton D M, MacDermid J C. Depression affects the recovery trajectories of patients with distal radius fractures: a latent growth curve analysis. Musculoskelet Sci Pract. 2019;43:96–102. doi: 10.1016/j.msksp.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Brogren E, Hofer M, Petranek M, Dahlin L B, Atroshi I. Fractures of the distal radius in women aged 50 to 75 years: natural course of patient-reported outcome, wrist motion and grip strength between 1 year and 2-4 years after fracture. J Hand Surg Eur Vol. 2011;36(07):568–576. doi: 10.1177/1753193411409317. [DOI] [PubMed] [Google Scholar]
- 9.Lalone E, MacDermid J, Grewal R, King G. Patient reported pain and disability following a distal radius fracture: a prospective study. Open Orthop J. 2017;11:589–599. doi: 10.2174/1874325001711010589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thorninger R, Wæver D, Pedersen J et al. Objective outcome measures continue to improve from 6 to 12 months after conservatively treated distal radius fractures in the elderly-a prospective evaluation of 50 patients. J Clin Med. 2021;10(09):1831. doi: 10.3390/jcm10091831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rozental T D, Blazar P E, Franko O I, Chacko A T, Earp B E, Day C S. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 2009;91(08):1837–1846. doi: 10.2106/JBJS.H.01478. [DOI] [PubMed] [Google Scholar]
- 12.Ingall E M, Bernstein D N, Shoji M M, Merchan N, Harper C M, Rozental T D. Using the QuickDASH to model clinical recovery trajectory after operative management of distal radius fracture. J Hand Surg Glob Online. 2020;3(01):1–6. doi: 10.1016/j.jhsg.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheema A S, O'Brien P J, Broekhuyse H M, Lefaivre K A. Measuring outcomes over time in distal radius fractures: a comparison of generic, upper extremity-specific and wrist-specific outcome measures. J Hand Surg Glob Online. 2020;2(05):272–276. doi: 10.1016/j.jhsg.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacDermid J C. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9(02):178–183. doi: 10.1016/s0894-1130(96)80076-7. [DOI] [PubMed] [Google Scholar]
- 15.Marsh J, Bryant D, MacDonald S J. Older patients can accurately recall their preoperative health status six weeks following total hip arthroplasty. J Bone Joint Surg Am. 2009;91(12):2827–2837. doi: 10.2106/JBJS.H.01415. [DOI] [PubMed] [Google Scholar]
- 16.Bryant D, Norman G, Stratford P, Marx R G, Walter S D, Guyatt G. Patients undergoing knee surgery provided accurate ratings of preoperative quality of life and function 2 weeks after surgery. J Clin Epidemiol. 2006;59(09):984–993. doi: 10.1016/j.jclinepi.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 17.Ramoutar D N, Lefaivre K, Broekhuyse H, Guy P, O'Brien P. Mapping recovery in simple and complex tibial plateau fracture fixation. Bone Joint J. 2019;101-B(08):1009–1014. doi: 10.1302/0301-620X.101B8.BJJ-2018-1288.R1. [DOI] [PubMed] [Google Scholar]
- 18.Jaeschke R, Singer J, Guyatt G H. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(04):407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 19.Neufeld M E, Broekhuyse H M, OʼBrien P J, Guy P, Lefaivre K A. The longitudinal short-, medium-, and long-term functional recovery after unstable pelvic ring injuries. J Orthop Trauma. 2019;33(12):608–613. doi: 10.1097/BOT.0000000000001588. [DOI] [PubMed] [Google Scholar]
- 20.Ko S J, OʼBrien P J, Guy P, Broekhuyse H M, Blachut P A, Lefaivre K A. Trajectory of short- and long-term recovery of tibial shaft fractures after intramedullary nail fixation. J Orthop Trauma. 2017;31(10):559–563. doi: 10.1097/BOT.0000000000000886. [DOI] [PubMed] [Google Scholar]
- 21.Middleton S D, Guy P, Roffey D M, Broekhuyse H M, O'Brien P J, Lefaivre K A. Long term trajectory of recovery following pilon fracture fixation. J Orthop Trauma. 2022;36(06):e250–e254. doi: 10.1097/BOT.0000000000002312. [DOI] [PubMed] [Google Scholar]
- 22.Walenkamp M MJ, de Muinck Keizer R-J, Goslings J C, Vos L M, Rosenwasser M P, Schep N WL. The minimum clinically important difference of the patient-rated wrist evaluation score for patients with distal radius fractures. Clin Orthop Relat Res. 2015;473(10):3235–3241. doi: 10.1007/s11999-015-4376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmitt J S, Di Fabio R P. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol. 2004;57(10):1008–1018. doi: 10.1016/j.jclinepi.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Norman G R, Sloan J A, Wyrwich K W. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(05):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 25.Sleat G KJ, Lefaivre K A, Broekhuyse H M, O'Brien P J. Predicting completion of follow-up in prospective orthopaedic trauma research. OTA Int. 2019;2(04):e047. doi: 10.1097/OI9.0000000000000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zelle B A, Buttacavoli F A, Shroff J B, Stirton J B. Loss of follow-up in orthopaedic trauma: who is getting lost to follow-up? J Orthop Trauma. 2015;29(11):510–515. doi: 10.1097/BOT.0000000000000346. [DOI] [PubMed] [Google Scholar]
- 27.Mulders M AM, Kleipool S C, Dingemans S A et al. Normative data for the Patient-Rated Wrist Evaluation questionnaire. J Hand Ther. 2018;31(03):287–294. doi: 10.1016/j.jht.2017.10.007. [DOI] [PubMed] [Google Scholar]


