Abstract
Background Posttraumatic extensor carpi ulnaris (ECU) instability is an increasingly recognized cause of ulnar-sided wrist pain that occurs when the ECU subsheath is disrupted.
Purpose The purpose of this systematic review was to assess outcomes of operatively treated posttraumatic ECU instability.
Methods A systematic search of Medline, Embase, Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature) databases was performed using “extensor carpi ulnaris” as the keyword. Studies were systematically screened and data extracted independently by two reviewers.
Results Eight retrospective studies met the inclusion criteria with a total of 97 wrists. The mean age was 32 years (13–61). Patients underwent either primary repair (40%) using sutures and anchors, or reconstruction (60%) using extensor retinaculum flaps. One study performed deepening of the osseous ulnar groove. Two studies compared preoperative and postoperative values. They both reported a significant improvement in pain scores, functional scoring instruments, satisfaction, and grip strength. The rest of the studies reported similarly favorable outcomes across the same outcomes. Concomitant pathologies were identified in 66% of the study population. Complications occurred in 9% of the sample size, including ECU tendinitis, ulnar sensory nerve irritation, and reintervention for concomitant pathology. None of the studies reported recurrence or reruptures. However, five patients (6.7%) did not return to their previous activity level.
Conclusion Patients can expect favorable outcomes with a potentially low complication rate. Nevertheless, the heterogeneity of the sample population, operative techniques, and outcome measures warrant further standardized studies.
Level of Evidence IV.
Keywords: extensor carpi ulnaris, instability, subluxation, dislocation, operative treatment, outcomes, repair, reconstruction
Among the various causes of ulnar-sided wrist pain, extensor carpi ulnaris (ECU) instability is a challenging entity to diagnose and manage. Stability of the ECU is dependent on the integrity of the tendon, the extensor tendon retinaculum, and the ECU subsheath, which forms part of the triangular fibrocartilage complex (TFCC) that keeps the tendon within the ulnar head osseous groove. 1 2 3 Various definitions of ECU instability have been proposed, unified by the presence of an unconstrained tendinopathy resulting in recurrent tendon subluxation or dislocation secondary to extensor subsheath damage as initially described by Spinner and Kaplan in 1970. 2 Etiologies include degenerative conditions such as rheumatoid disorders that can destroy the tendon subsheath, and posttraumatic instability among other causes. Posttraumatic ECU injuries are often a consequence of repetitive or excessively forceful wrist movements that stress the tendon, such as supination, flexion, and ulnar deviation of the wrist. Thus, this injury has been frequently reported in sports where these wrist-specific movements are more common including tennis, golf, and rugby. Further, while there is an increasing amount of surfacing evidence, there have been no previous systematic reviews to evaluate outcomes in this injury.
The scarcity of evidence on the management options reflects the relatively rare occurrence of ECU instability, the exact incidence of which remains unknown. 4 Although it is believed to be an uncommon injury, the prevalence is likely underestimated particularly in patients engaged activities such as racquet sports. A recent analysis of 50 professional tennis players over a 10-year period showed that 24% of these patients had been diagnosed with symptomatic traumatic ECU instability. 5 6 7 Difficulties may also arise in differentiating this condition from other, occasionally concomitant causes of ulnar-sided wrist pain, such as: (1) TFCC injuries; (2) ECU tendinopathies and tendon ruptures; and (3) distal radioulnar joint injuries among others. In 2001, Inoue and Tamura described an intraoperative classification of subsheath damage depending on the location of the sheath injury; radial rupture, ulnar rupture, and detachment of the periosteum. 8 This classification has frequently been utilized in recent literature despite reports of some unclassifiable injuries. 9
Management of this injury can be challenging given the demanded functionality of the injured wrist among the young and highly active affected population. Several questions arise from the surgical management options, such as whether to perform an ECU subsheath repair versus a reconstruction, the role of wrist arthroscopy in the diagnosis and treatment of associated injuries. Further, the clinical outcomes, return-to-sport rates, and the rate of complications and revision surgery have not been systematically studied.
Despite a lack of consensus on the optimal treatment of ECU instability, the management of this injury has been primarily surgical, with some emerging evidence of cases successfully managed nonoperatively. 5 However, given the lack of clear evidence supporting the various operative techniques, their outcomes, and safety profile, we aimed to conduct a systematic review of the literature to assess the clinical outcomes and complications of surgically treated patients with posttraumatic ECU instability.
Materials and Methods
The search and selection process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and was prospectively registered with PROSPERO (International Prospective Register of Systematic Reviews) (ID: CRD42022327483). 10
Search Strategy
A systematic search of Medline, Embase, Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature) databases was performed using “extensor carpi ulnaris” as the only keyword. Given the rarity of the condition and the heterogeneity of the available literature, this encompassing approach was utilized to identify all articles possibly pertinent to the topic and minimize the effect of variation in definitions and terminology attributed to ECU instability. The search was limited to articles published on or before the 20th of May, 2022. A review of the reference lists of relevant articles was performed to identify any additional articles that were potentially unidentified in the initial database search.
Eligibility Criteria
Studies that met the following inclusion criteria were reviewed: (1) clinical studies reporting outcomes of operatively treated posttraumatic ECU instability, (2) case series reporting outcomes of at least 5 patients, and (3) studies with a study population ≥ 18 years. All levels of evidence were included and there were no language restrictions.
Studies were excluded if they met any of the following criteria: (1) cadaveric studies, (2) biomechanical analysis, (3) ECU pathology secondary to nontraumatic origin, (4) studies assessing nonoperative treatment, and (5) review articles.
Data Collection/Extraction
Study Screening
Titles and abstracts were independently screened for relevance by two reviewers (A.L., W.B.) using Covidence (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia; www.covidence.org ). Potentially relevant articles underwent full-text screening, with any conflicts between the reviewers resolved by discussion and consensus with the senior author (C.P.).
Quality Assessment
Study quality assessment was conducted using the methodological index for non-randomized studies (MINORS) tool. 11 A score of 0, 1, or 2 is given for each of the 12 items on the MINORS checklist with a score of up to 16 for noncomparative studies and 24 for comparative studies. Methodological quality was categorized prior as follows: a score of 0 to 8 or 0 to 12 was considered poor quality, 9 to 12 or 13 to 18 was considered fair quality, and 13 to 16 or 19 to 24 was considered excellent quality, for noncomparative and comparative studies, respectively.
Data Extraction
Two reviewers (A.L., W.B.) independently extracted relevant data from the included articles and to a dedicated Microsoft Excel spreadsheet (Microsoft, Redmond, WA). The retrieved data included general article information (title, author, date of publication, journal, originating country, and contact information), sample data and methodological information (study design, sample size, inclusion/exclusion criteria), patient demographic and surgical procedure details (age, gender, diagnoses, method of operative interventions), and outcome measures (follow-up period, patient-reported outcome scores, complications, satisfaction, pain score, and return to previous level of activity).
Data Analysis
Descriptive statistics including the mean, range, and measures of variance (e.g., standard deviations, 95% confidence intervals) were utilized where applicable. Data were synthesized where possible into pooled demographics, treatment, and outcome measures. Due to the heterogeneity of the included outcome measures, subgroup analysis was not possible.
Results
After the removal of duplicates from the initial search, a total of 1,959 results were generated for title and abstract screening ( Fig. 1 ). A total of 1,872 were excluded after the initial title/abstract review. Next, 87 studies underwent full-text review. Finally, a total of 8 studies were included in the final analysis.
Fig. 1.
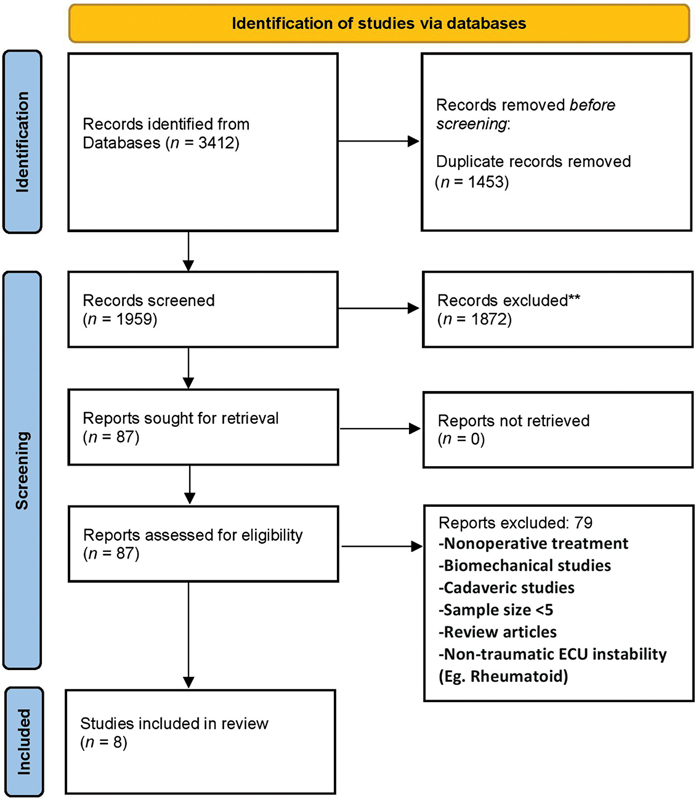
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram summarizing the study selection process.
Study Designs and Patient Demographics
The study designs and demographics are depicted in Table 1 . All studies included were either retrospective case series ( n = 5) or retrospective cohort studies ( n = 3). The total number of patients and wrists included were 96 and 97, respectively. There was a male preponderance in the sample group ( n = 56, 58%) with a mean age of 32 years (range 13–61). All studies included some form of nonstandardized immobilization for 2 to 8 weeks along with nonsteroidal anti-inflammatory medication. Corticosteroid injections were used in two studies (25%). The average time between the onset of symptoms and operative treatment averaged 8.6 months (range 1.5–17 months).
Table 1. Study designs and sample population demographics.
| Study | Study type | MINORS score | Sample size Wrists |
Sex ( N /%) Female |
Age Mean (range) |
Follow-up (mean -mo) | Nonoperative management | Time from symptoms to surgery Mean (range in mo) | Diagnostic modality |
|---|---|---|---|---|---|---|---|---|---|
| Inoue and Tamura 1998 |
Case series | 4 | 5 | None (0) | 38 (34–40) |
22 | NR | 15 (3–60) |
Clinical/intraoperative |
| Inoue and Tamura 2001 |
Case series | 6 | 12 | 4 (33) | NR (19–40) |
20 | NR | 17 (0.3 to 84 mo) |
Clinical/intraoperative |
| Allende 2005 21 | Retrospective cohort | 8 | 9 | 5 (55) | 34 (includes other ECU pathology) |
23 | NR | 11 (4–58) |
Radiographs/CT/MRI/Arthrogram |
| Maclennan et al, 2008 | Case series | 9 | 21 | 7 (33) | 27 (14–44) |
31 | 2–6 weeks of immobilization and analgesia | 1.5 | Dynamic ultrasound |
| Fram et al, 2018 |
Retrospective cohort | 10 | 12 (11 patients) |
3 (27) | 25 (13–52) |
39 | (5) bracing (5) casting |
Median 3.5 (1–24) |
Radiographs + MRI |
| Oh et al, 2018 |
Case series | 9 | 11 | 2 (18) | 25 (19–49) |
11 | Nonspecific immobilization for 2–4 months |
6 | MRI and US in all patients |
| Peter et al 2019 |
Retrospective cohort | 9 | 12 | 10 (83) | 35.3 (19–53) |
44 | Nonspecific immobilization | NR | MRI |
| Verhiel et al, 2020 | Case series | 7 | 15 | 9 (60) | 43.5 (29–61) |
9.5 | Immobilization (10) Corticosteroid injections (6) |
1.5 | MRI |
| Mean a | 97 | 40 (42) | 32 (13–61) |
25 | 8 |
Abbreviations: CT, computed tomography; ECU, extensor carpi ulnaris; MINORS, methodological index for non-randomized studies; MRI, magnetic resonance imaging; NR, not reported; US, ultrasound.
Row reporting mean values.
Diagnostic Modalities
The most common diagnostic modalities included were magnetic resonance imaging (MRI) and dynamic ultrasound (US). MRI was utilized in 5 (63%) of the included studies and US in 2 studies (25%). Concomitant injuries were reported in 4 out of 8 studies (50%) with a mean of 66.5%. The most common associated pathologies included TFCC injuries ( n = 10), ECU tendinopathy ( n = 10), ECU tenosynovitis ( n = 10), and ECU split tears ( n = 4). There were 4 studies that utilized both MRI and arthroscopy. These studies detected concomitant pathology in more than 50% of the sample group. Further, most studies reported utilizing Inoue's classification to guide management. 8 12
Interventions
The interventions performed and concomitant pathologies reported are displayed in Table 2 . A total of 39 patients (40%) underwent primary repair with either direct suturing of a ruptured subsheath or anchoring of an elevated fibro-osseous sheath (mean time from injury to 12 months). The rest of the sample group ( N = 79) underwent any of several different reconstruction techniques. The extensor retinaculum flap was the most common utilized tissue to reconstruct a sheath in 5 (63%) of the included studies. An extensor retinaculum sling reconstruction and dorsal transposition of the ECU was utilized by Fram et al and Verhiel et al. 13 14 Maclennan et al reported a shallow groove and a detached periosteal sheath in all 21 patients. 15
Table 2. Interventions and concomitant pathology reported in the sample population.
| Study | Repair N (%) |
Reconstruction N (%) |
Arthroscopy | Concomitant pathology, N (%) | Type of concomitant pathology | Postoperative protocol |
|---|---|---|---|---|---|---|
| Inoue and Tamura 1998 |
2 (40) | 3 (60) Extensor retinaculum flap | N | NR | NR | |
| Inoue and Tamura 2001 |
7 (58) | 5 (42) Extensor retinaculum flap | N | NR | NR | |
| Allende 2005 21 | 4 (44) | 5 (56) Extensor retinaculum flap (+1 patient with deepened groove) |
N | N (100) | ECU Tenosynovitis/tendinopathy (12) | Long arm cast elbow in 90 for 4 weeks |
| Maclennan et al, 2008 |
21 (100) Subsheath repair with anchors + groove deepening | 0 | N | NR | NR | Long arm splint in 90 for 6 weeks |
| Fram et al, 2018 |
None | 12 (100) (Retinacular sling + dorsal transposition) | Y | Excluded major wrist pathology | Wrist synovitis in 4 patients | Long arm splint in pronation 8 weeks |
| Oh et al, 2018 |
5 (45) (Anchors) |
6 (55) Extensor retinaculum flap | Y | 63 | •TFCC (5) •Ulnar nerve entrapment (2) •DRUJ (2) •Nonunion styloid (2) •ECU split tear (3) |
Long arm splint for 6 weeks |
| Peter et al 2019 |
None | 12 (100) Extensor retinaculum flap | Y | 50 | •TFCC (3) •Carpal instability (2) •Ulnocarpal impingement (1) •Distal radius fracture (2) |
Long arm splint for 6 weeks |
| Verhiel et al, 2020 |
None | 15 (100) Extensor retinaculum sling | Y | 53 | •TFCC (2) •ECU tendinopathy (4) •ECU Split tear (1) •Ganglion excision (1) |
Long arm splint for 6 weeks |
Abbreviations: DRUJ, distal radioulnar joint; ECU, extensor carpi ulnaris; N, no; NR, not reported; TFCC, triangular fibrocartilage complex; Y, yes.
Outcome Measures
Outcome measures utilized in the included studies are displayed in Table 3 . Five out of eight studies (63%) used at least one limb-specific outcome scoring instrument. Outcome measures used included the Disabilities of Arm, Shoulder and Hand (DASH), Quick - DASH (Q-DASH), Patient-Reported Outcomes Measurement Information System Upper Extremity, Mayo Wrist Score, and the Visual Analogue Scale (VAS).
Table 3. Outcome measured reported in the included studies.
| Study | DASH Mean (SD) |
Q-DASH Mean (SD) |
PROMIS-UE Mean (SD) |
Mayo Wrist Score Mean (SD) |
VAS Mean (SD) |
Satisfaction Mean (SD) |
Grip strength |
|---|---|---|---|---|---|---|---|
| Inoue and Tamura 1998 |
NR | NR | NR | NR | 0 | NR | NR |
| Inoue and Tamura 2001 |
NR | NR | NR | NR | 0 | NR | NR |
| Allende 2005 21 | NR | NR | NR | NR | NR | NR | (4) > 70% compared with CLS (5) “normal” compared with CLS |
| Maclennan et al, 2008 |
Preop: 97 (19) Postop: 58 (14) p < 0.001 |
NR | NR | NR |
a
Preop: 6 (2) Postop: 0.5 (1) p < 0.001 |
b
Preop: 3 (1) Postop: 5 (1) p < 0.001 |
Mean kg (SD) Preop: 34 (10) Postop: 36 (10) p < 0.001 |
| Fram et al, 2018 |
NR | Postop: 1.8 (SD 3.5) |
Postop: 56 (SD 6.3) |
NR |
a
Preop: 6.5 Postop: 0.2 |
a
Preop: NR Postop: 9.8 |
NR |
| Oh et al, 2018 |
NR | Preop: 41 Postop: 12.4 p = 0.004 |
NR | Preop: 76 Postop: 86 p = 0.004 |
a
Preop: 6 Postop: 1.1 p = 0.004 |
NR | Preop: 78.3% of CLS Postop: 88% of CLS p = 0.004 |
| Peter et al 2019 |
-Postop 24.2 (SD 25.1) |
NR | NR | NR | 0 (painless) |
a
Postop 7.8 (SD 2.5) |
Postop: 30.5 (kg) (SD 8.9) Mean: 92% of CLS (SD 22.7%) |
| Verhiel et al, 2020 |
NR | NR | Postop Median 56 (IQR: 41–56) |
NR |
a
Postop Median 0.5 (IQR: 0–2) |
a
Postop Median 9.5 (range 6–10) |
NR |
Abbreviations: CLS, contralateral side; DASH, Disabilities of Arm, Shoulder and Hand; IQR, interquartile range; NR, not reported; Postop, postoperative; Preop, preoperative; PROMIS-UE, Patient-Reported Outcomes Measurement Information System Upper Extremity ; Q-DASH, Quick - Disabilities of Arm, Shoulder and Hand; SD, standard deviation; VAS, Visual Analogue Scale.
Scale out of 10.
Scale out of 5.
Two studies (25%) compared preoperative and postoperative outcome measures, reporting improvements in all included parameters. 9 15 Maclennan et al reported a statistically significant improvement of the mean preoperative DASH score ( p < 0.001). 15 Oh et al reported a mean preoperative Q-DASH score of 41, improving to 12.4 ( p = 0.004) following surgery. 9 Satisfaction was measured on rating scales in 4 studies (50%) of the included studies ( Table 3 ). In the absence of complications, significant improvement in satisfaction scores were reported in all of the included studies. 15 16
Pain was measured by the VAS instrument in 5 studies (63%) ( Table 3 ). All studies reported good pain scores that normally ranged from 0 to 3. Three studies by Fram et al, Verhiel et al, and Maclennan et al measured preoperative pain values and reported a significant improvement in pain scores postoperatively. Grip strength was measured in 4 studies (50%). Overall, all studies reported improvements in grip strength postoperatively when compared with the contralateral side. Oh et al measured strength compared with the contralateral side (78.3% preop to 88.2% postop) ( p = 0.004).
Complications and Revision Surgery
The complications reported are summarized in Table 4 . Complications occurred in 9 patients (9.2%) of the overall sample group. In a series of 15 operatively treated wrists, Verhiel et al reported 5 complications (33%). Of these, two patients developed postoperative ECU tendinitis managed with corticosteroid injections. One patient improved, while the second reported continuous symptoms. Another patient underwent neurolysis of the dorsal cutaneous branch of the ulnar nerve twice. According to the author, neuropathy was likely due to damage to the nerve. This patient continued to have pain and stiffness postoperatively. Finally, among all studies, there were no reports of reruptures postoperatively.
Table 4. Complications, reinterventions, and return to sports reported in the included studies.
| Study | ROM Mean (SD) |
Complications N (%) |
Complications details | Reoperations | Restriction of ADLs | Restriction of sport activity |
|---|---|---|---|---|---|---|
| Inoue and Tamura 1998 |
Normal – No details reported | 0 | – | – | No restriction | No restriction |
| Inoue and Tamura 2001 |
Normal – No details reported | 0 | – | – | No restriction | No restriction |
| Allende 2005 21 | NR | 3 complications in entire group | CRPS (1) Tenolysis and synovectomy (2) |
– | No restriction | No restriction |
| Maclennan et al, 2008 |
Pre/Postop (°) Flexion/Extension 125 (11)/129 (8) Radioulnar deviation 51 (7)/54 (8) Pro-supination 160 (14)/163 (14) p < 0.05 |
1 / 4.7% | Anchor loosening | None needed | No Restriction | (1) Restricted - Did not return to previous activity (mean return of 8 months) |
| Fram et al, 2018 |
NR | 2 / 16.6% | -Sensory branch of ulnar nerve irritation (resolved spontaneously) (1) -Persistent clicking (1) |
Scar excision for persistent clicking (1) | No restriction | No restrictions (mean return of 2.6 months) |
| Oh et al, 2018 |
a
Preop: 84.6%
Postop: 92.4% p = 0.032 |
0 | None | None | NR | NR |
| Peter et al 2019 |
a
Extension 95.0%/Flexion 89.7%
Pronation 94.0%/Supination 96.9% Radial deviation 72.8%/Ulnar deviation 87.4% |
1 | CRPS – Persistent pain and reduced ROM | None | NR | NR |
| Verhiel et al, 2020 |
NR | 5 / 33% | Postoperative tendinitis (2) - Corticosteroid injections |
Stitch irritation (1) TFCC debridement (1) Neurolysis and ulnar osteotomy (1) |
(1) Restricted ADL | (4) Restricted tennis (2)/Pushups (1)/Yoga/Pilates (1) |
Abbreviations: ADL, activities of daily living; CLS, contralateral side; CRPS, complex regional pain syndrome; NR, not reported; ROM, range of motion; SD, standard deviation; TFCC, triangular fibrocartilage complex.
Compared with CLS.
Return to Sports or Previous Activity
Six out of eight studies (75%) ( n = 74 patients) reported return to previous sports/activity as an outcome measure. Across the 6 studies, only one patient reported restriction in activities of daily living (1.3%). However, 5 patients reported restriction to return to sports and previous hobbies (6.7%). The time to return to sports was reported in two studies (25%), ranging from 2.6 to 8 months. 13 15 Fram et al reported that all patients ( n = 10) returned to their previous or higher level of sporting (all professional athletes) after a mean of 2.6 months. These sports included golf, baseball, hockey, and diving.
Discussion
Overall, the operative management of patients with posttraumatic ECU instability yielded favorable outcomes. This systematic review's main finding is that most patients report satisfactory outcomes with low complication rates. However, discrepancies in the time to operative management, the different surgical techniques used, and the low quality of the included studies make it challenging to draw firm conclusions. Nevertheless, this review has highlighted areas in need of further investigation.
Two main general approaches have been utilized to manage posttraumatic ECU instability. In our series, some patients underwent a direct repair of the subsheath that encapsulates the tendon with the use of sutures when the sheath sustained reparable acute damage, or bone anchors in the case of fibrous subsheath detachment to try to recreate the native anatomy. On the other hand, some authors performed some type of tendon sling reconstruction, often using an extensor retinaculum flap to stabilize the tendon in position. Unfortunately, comparisons on superiority cannot be made using the current evidence. Another unanswered question is how much time surgeons have to attempt a subsheath repair successfully without compromising the clinical outcomes or needing to reconstruct using retinacular flaps. Maclennan et al reported good outcomes by deepening the osseous ECU groove and using bone anchors to reattach the fibrous subsheath after noting shallow grooves in the entirety of their sample group. 15 However, the degree of osseous depth was not clearly defined, thus being potentially subjective to determine.
Recent studies have displayed a trend toward performing some sort of subsheath reconstruction, yielding favorable results. One potential reason to explain the more frequent favorable reconstructive approach may be the common delay in the diagnosis associated with this injury, which may raise concerns over the viability of the tendon subsheath and its ability to be repaired. Currently, there are no clear guidelines or cutoff time to decide between any of the two options. However, the two main methods appeared to be comparable with regards to safety and benefit. In addition, while the treatment remains largely operative, nonoperative management has been reported to yield promising results with prolonged immobilization. 5
The high-demand population of patients who suffer this injury seek an asymptomatic return to their previous levels of activity as the primary goal of management. Surgical management has demonstrated marked pain relief and improved satisfaction rates in studies that compared these parameters with preoperative values. 9 13 15 However, specific scales assessing the ability of these patients to fully return to their preinjury level are lacking. Although, the vast majority of included patients returned to their previous activities, the majority of studies did not specify the level and type. This is especially important to ascertain whether elite athletes return to their preinjury levels and allow surgeons to guide the preoperative discussion and expectation management when dealing with these patients. Verhiel et al reported that 4 patients (27%) exhibited some degree of restriction in sports activity and one patient with restriction in activities of daily living.
Another important finding of our systematic review is that concomitant wrist pathology is common in this patient population and should be suspected, studied, and considered in the surgical management. Associated injuries were identified by arthroscopy in more than half of the patients included in recent series. 9 14 16 With the data gathered in our review it seems reasonable to either have an advanced imaging study preoperatively or to perform a wrist diagnostic arthroscopy at the time of surgical treatment to avoid missing injuries that might warrant further reoperation. Given that there has been some concerns with MRI diagnostic properties for the study of ulnar-side wrist pain conditions, surgeons might consider routine concurrent arthroscopic assessment to identify and manage commonly associated pathology at the time of surgery. 17 18 19
Several potential intraoperative considerations arise from the nature of the identified complications and their subsequent management. First, prevention of constrained postoperative tendinitis may be facilitated by care to avoid excessively tighten the reconstructed or repaired sheath, allowing the tendon to glide without resistance after the repair/reconstruction is performed. The use of Wide-Awake Local Anesthesia No Tourniquet (WALANT) 20 surgery can be beneficial to decrease tension-related problems in this patient subgroup. Further, the dorsal sensory cutaneous branch of the ulnar nerve should be identified and protected throughout the surgery to prevent postoperative painful neuromas requiring reinterventions. 13 14
Limitations
There are several limitations to this systematic review. The main limitation is that the included studies were all classified as low levels of evidence that included case series or retrospective reviews of relatively small sample sizes. Unfortunately, when dealing with unusual conditions like this injury, to successfully conduct higher-level prospective studies can be very challenging.
Another limitation is the inability to perform subgroup analysis to account for the different variations in surgical techniques and presence/absence of associated injuries. This is especially true for concomitant injuries of the TFCC and ECU tendon, which may potentially negatively impact the end outcome. There were also variations regarding the time from injury to surgery, and degree of injury, which impede broad generalization. Moreover, outcomes reported among the studies varied, with some studies missing validated instruments to quantify functional outcome and with a lack of instruments to account for minor deficits which might not be captured in this high-demand population with traditional patient-reported outcomes but that might still be very important for this group.
Future Directions
Data from this systematic review suggests that the operative management of ECU posttraumatic instability yields favorable results with low complication rates. Early detection of ECU instability and concomitant pathology may further improve outcomes and alter the surgical management. However, data extricated from this review highlights the need for larger standardized prospective studies to reveal the implications of different operative techniques, the role of primary repair versus reconstructive alternatives, and the ability of patients to restore their preinjury level given the high-demand population who suffer from this injury. Furthermore, information gathered by surgical registries may be of potential benefit as these injuries are still quite uncommon and adequate prospective collection of data can be difficult to achieve.
Conclusion
Patients undergoing operative treatment of posttraumatic ECU instability can expect good postoperative outcomes with a potentially low complication rate. However, due to the heterogeneity in the patient population, injuries, time to surgery, and different surgical techniques, it is difficult to draw firm conclusions on the superiority of different surgical techniques and their outcomes.
Funding Statement
Funding This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest None declared.
Authors' Contributions
All authors have agreed to the submission of the current version of the manuscript and that all authors have made substantial contributions to the work submitted in the forms of; design, data acquisition, analysis, writing, editing, reviewing, and final approval of the version to be published.
Ethical Approval
No ethical approval was required for the purpose of this study.
Authors' Declaration
We, the authors of this submission confirm that we have not published the same or a very similar study with the same or very similar results and major conclusions in any other journals. These include English or non-English language journals and journals that are indexed or not indexed in PubMed, regardless of different words being used in the article titles, introduction, and discussion.
References
- 1.Omokawa S, Gumpangseth T, Komutrattananont P, Inchai C, Mahakkanukrauh P. Anatomical study of stabilizing structures of the extensor carpi ulnaris tendon around the wrist. J Hand Surg Am. 2021;46(10):9300–9.3E11. doi: 10.1016/j.jhsa.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Spinner M, Kaplan E B. Extensor carpi ulnaris. Its relationship to the stability of the distal radio-ulnar joint. Clin Orthop Relat Res. 1970;68(68):124–129. [PubMed] [Google Scholar]
- 3.Ghatan A C, Puri S G, Morse K W, Hearns K A, von Althann C, Carlson M G. Relative contribution of the subsheath to extensor carpi ulnaris tendon stability: implications for surgical reconstruction and rehabilitation. J Hand Surg Am. 2016;41(02):225–232. doi: 10.1016/j.jhsa.2015.10.024. [DOI] [PubMed] [Google Scholar]
- 4.Campbell D, Campbell R, O'Connor P, Hawkes R. Sports-related extensor carpi ulnaris pathology: a review of functional anatomy, sports injury and management. Br J Sports Med. 2013;47(17):1105–1111. doi: 10.1136/bjsports-2013-092835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montalvan B, Parier J, Brasseur J L, Le Viet D, Drape J L.Extensor carpi ulnaris injuries in tennis players: a study of 28 cases Br J Sports Med 20064005424–429., discussion 429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sole J S, Wisniewski S J, Newcomer K L, Maida E, Smith J. Sonographic evaluation of the extensor carpi ulnaris in asymptomatic tennis players. PM R. 2015;7(03):255–263. doi: 10.1016/j.pmrj.2014.08.951. [DOI] [PubMed] [Google Scholar]
- 7.Erpala F, Ozturk T. “Snapping” of the extensor carpi ulnaris tendon in asymptomatic population. BMC Musculoskelet Disord. 2021;22(01):387. doi: 10.1186/s12891-021-04271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inoue G, Tamura Y. Surgical treatment for recurrent dislocation of the extensor carpi ulnaris tendon. J Hand Surg [Br] 2001;26(06):556–559. doi: 10.1054/jhsb.2001.0615. [DOI] [PubMed] [Google Scholar]
- 9.Oh B-S, Choi Y-R, Ko I-H, Oh W-T, Eom N-G, Kang H-J. Operative treatment for extensor carpi ulnaris tendon dislocation. J Korean Orthop Assoc. 2018;53(03):256–263. [Google Scholar]
- 10.Page M J, McKenzie J E, Bossuyt P M et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(09):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 12.Inoue G, Tamura Y. Recurrent dislocation of the extensor carpi ulnaris tendon. Br J Sports Med. 1998;32(02):172–174. doi: 10.1136/bjsm.32.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fram B, Wall L B, Gelberman R H, Goldfarb C A. Surgical transposition for chronic instability of the extensor carpi ulnaris tendon. J Hand Surg Eur Vol. 2018;43(09):925–930. doi: 10.1177/1753193418773036. [DOI] [PubMed] [Google Scholar]
- 14.Verhiel S HWL, Özkan S, Chen N C, Jupiter J B. Long-term outcomes after extensor carpi ulnaris subsheath reconstruction with extensor retinaculum. Tech Hand Up Extrem Surg. 2020;24(01):2–6. doi: 10.1097/BTH.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 15.MacLennan A J, Nemechek N M, Waitayawinyu T, Trumble T E. Diagnosis and anatomic reconstruction of extensor carpi ulnaris subluxation. J Hand Surg Am. 2008;33(01):59–64. doi: 10.1016/j.jhsa.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Peter K, Luzian H, Markus G, Ansgar R, Andrea K, Arora R. Mid-term outcome (11-90 months) of the extensor retinaculum flap procedure for extensor carpi ulnaris tendon instability. Arch Orthop Trauma Surg. 2019;139(09):1323–1328. doi: 10.1007/s00402-019-03227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Öztürk T, Burtaç Eren M. Is it really safe to evaluate symptomatic extensor carpi ulnaris tendon instability by magnetic resonance imaging (MRI)? Acta Orthop Belg. 2021;87(02):227–234. [PubMed] [Google Scholar]
- 18.Omar N N, Mahmoud M K, Saleh W R et al. MR arthrography versus conventional MRI and diagnostic arthroscope in patients with chronic wrist pain. Eur J Radiol Open. 2019;6:265–274. doi: 10.1016/j.ejro.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Torres-de Torres E, Hernández M O, Corella Montoya F. Visualization of the extensor carpi ulnaris and its subsheath using standard wrist arthroscopy. J Hand Surg Eur Vol. 2021;46(02):208–209. doi: 10.1177/1753193420948404. [DOI] [PubMed] [Google Scholar]
- 20.Lalonde D. Wide awake local anaesthesia no tourniquet technique (WALANT) BMC Proc. 2015;9(03):1–2. [Google Scholar]
- 21.Allende C, Le Viet D. Extensor carpi ulnaris problems at the wrist--classification, surgical treatment and results. J Hand Surg Br. 2005;30(03):265–272. doi: 10.1016/j.jhsb.2004.12.007. [DOI] [PubMed] [Google Scholar]


