Abstract
BACKGROUND
High out-of-pocket prescription drug costs contribute to financial toxicity, medication nonadherence, and adverse cardiovascular (CV) outcomes. Policymakers recently passed the Inflation Reduction Act, which will cap Medicare out-of-pocket drug costs at $2,000/year and expand full low-income subsidies (LIS). It is unclear how these provisions will affect Medicare beneficiaries with CV risk factors and/or conditions.
OBJECTIVES
The authors sought to characterize the population of Medicare beneficiaries with CV risk factors/conditions experiencing out-of-pocket prescription drug costs >$2,000/year and estimate their potential savings under the Inflation Reduction Act’s spending cap; identify sociodemographic characteristics associated with out-of-pocket costs >$2,000/year; and characterize beneficiaries newly eligible for LIS under the Inflation Reduction Act.
METHODS
This was a cross-sectional study of Medicare beneficiaries aged ≥65 years with ≥1 CV risk factor/condition from 2016 to 2019.
RESULTS
An annual estimated 34,056,335 ± 855,653 Medicare beneficiaries (mean ± SE) had ≥1 CV risk factor/condition, of whom 1,020,484 ± 77,055 experienced out-of-pocket drug costs >$2,000/year. The likelihood of experiencing out-of-pocket drug costs >$2,000/year was lower among adults ≥75 years vs 65 to 74 years (adjusted OR: 0.67; 95% CI: 0.49–0.93) and for low-income vs higher-income adults. Among beneficiaries currently spending >$2,000/year, estimated median out-of-pocket drug savings would be $855/year and total annual savings $1,723,031,307 ± $91,150,609 under the Inflation Reduction Act. An estimated 1,289,861 beneficiaries would also become newly eligible for LIS.
CONCLUSIONS
More than 1 million older adults with CV risk factors and/or conditions spend >$2,000/year out-of-pocket on prescription drugs and will likely benefit from the Inflation Reduction Act’s cap, with estimated total out-of-pocket savings of $1.7 billion/year, while another 1.3 million will also become newly eligible for LIS.
Keywords: cardiovascular disease, cardiovascular risk factors, low-income subsidies, Medicare, medications, out-of-pocket costs, Part D, prescription drugs
High and rising prescription drug costs in the United States contribute to financial toxicity among adults with cardiovascular (CV) risk factors or conditions.1–3 Moreover, recent evidence has shown that high out-of-pocket drug costs lead to medication nonadherence,4–6 which can worsen morbidity and mortality,7 especially among those with chronic conditions such as hypertension, diabetes, and CV disease. As a result, addressing prescription drug costs in patients with CV risk factors or conditions—a population at risk of high out-of-pocket costs and financial toxicity—has become a national priority.
In response to these growing concerns, federal policymakers passed the Inflation Reduction Act on August 16, 2022, which aims to address high out-of-pocket drug costs for adults enrolled in Medicare Part D, the primary source of prescription drug insurance for older U.S. adults. Two specific provisions of the Inflation Reduction Act could have major implications for Medicare beneficiaries who receive Part D drug benefits: 1) a $2,000 annual cap on out-of-pocket prescription drug costs; and 2) expanding eligibility for full Part D low-income subsidies (LIS) to individuals with incomes >135% to <150% of the federal poverty level (FPL), which will reduce deductible costs and prescription copayments to zero or minimal amounts.8 However, little is known about how these provisions will impact Medicare beneficiaries with CV risk factors or conditions, who are at risk of high out-of-pocket prescription drug costs, and as a result, cost-related medication nonadherence and adverse health outcomes.9–11
Therefore, in this study, we used data from the Medical Expenditure Panel Survey (MEPS) to answer 3 questions. First, how many Medicare beneficiaries age ≥65 years with CV risk factors and/or conditions would benefit from the Inflation Reduction Act’s $2,000 annual spending cap, and what is the estimated out-of-pocket amount that they would save annually under this cap? Second, what sociodemographic factors are associated with out-of-pocket spending >$2,000/year in this population and how do self-reported measures of affordability compare with those in adults spending ≤$2,000/year? Third, how many beneficiaries with CV risk factors and/or conditions would become newly eligible under the Inflation Reduction Act for full Part D LIS, which further reduce prescription drug deductibles and copayments?
METHODS
DATA SOURCES AND STUDY POPULATION.
We used data from MEPS, an annual cross-sectional study of the noninstitutionalized U.S. population by the Agency for Healthcare Research and Quality (AHRQ) that collects data on individual demographic and socioeconomic characteristics, medical conditions, health insurance coverage, access to and use of medical care services, and health care expenditures. We pooled 2016 to 2019 data collected by the Household Component of MEPS, which uses an overlapping panel design to randomly sample households annually based on respondents from the previous year’s National Health Interview Survey. Response rates ranged from 40% to 46% in the years 2016 to 2019.12 To account for nonresponders, MEPS assigns person-weights that are adjusted for individual and household nonresponse rates and national population totals.
Our study population included adults age 65 years or older with Medicare prescription drug coverage (Part D) who reported ≥1 CV risk factor (high blood pressure, high cholesterol, diabetes) and/or CV condition (coronary heart disease, angina, myocardial infarction, stroke, other heart disease). The MEPS Household Component directly asks individuals whether they have been diagnosed with “priority medical conditions,” which includes high blood pressure, high cholesterol, diabetes, coronary heart disease, angina, myocardial infarction, stroke, and other heart disease (heart murmur, heart arrhythmia/irregular heartbeat, blocked or clogged artery, congestive heart failure, atrial fibrillation, mitral valve prolapse, enlarged heart, heart valve problems, etc), which we used to identify individuals with CV risk factors and/or conditions. Fewer than 0.2% of respondents included in our study had missing data for CV risk factors and/or conditions. A flow diagram of our final study population (unweighted n = 13,631) after applying the aforementioned inclusion criteria is shown in Supplemental Figure 1.
MEPS reports survey respondents’ annual out-of-pocket prescription drug costs as a sum of self-reported out-of-pocket costs for each prescribed medication over the course of a calendar year, which MEPS verifies by requesting records of out-of-pocket payments directly from pharmacies for each pre-scribed medication. As a result of this verification process, MEPS prescription drug spending data for Medicare patients have been shown to closely correlate with Medicare Part D claims data.13
This study was based on secondary analyses of publicly available data; therefore, no further Institutional Review Board approval was sought from Beth Israel Deaconess Medical Center, in accordance with institutional policy.
OUTCOMES.
We examined 3 outcomes: 1) annual number of Medicare beneficiaries with out-of-pocket prescription medication costs >$2,000/year and their demographic and socioeconomic characteristics, to characterize individuals who would potentially benefit from the Inflation Reduction Act’s out-of-pocket spending cap; 2) median annual out-of-pocket prescription costs and the estimated out-of-pocket savings if the $2,000 spending cap were applied; and 3) annual number of beneficiaries who would be newly eligible for full Part D LIS under the Inflation Reduction Act’s expanded income criteria, along with their demographic and socioeconomic characteristics.
STATISTICAL ANALYSIS.
We used survey-specific methods that accounted for the multistage sampling design of the MEPS, including the stratified sampling and clustering of the data within sampling units, and used appropriate person-weights to obtain nationally representative estimates. Among Medicare beneficiaries age ≥65 years enrolled in Part D with ≥1 CV risk factor or condition, we calculated the annual number of beneficiaries with out-of-pocket drug spending >$2,000/year. We compared sociodemographic (age, sex, self-reported race and ethnicity, poverty level) and clinical characteristics of beneficiaries spending >$2,000/year to those spending ≤$2,000/year using Rao-Scott chi-square tests for categorical variables and survey-specific linear regression models for continuous variables. A similar approach was used to compare self-reported difficulty affording medical care and prescription medications between these groups using the subset of years (2018–2019) that captured these data.
We then fit a multivariable logistic regression model to identify sociodemographic characteristics (age [65–74 vs ≥75 years], sex, race and ethnicity [non-Hispanic White; non-Hispanic Black; non-Hispanic Asian; Hispanic; and other, which includes American Indian/Alaska Native and multiple races], poverty [<200% FPL vs ≥200% FPL]) associated with out-of-pocket drug costs >$2,000/year, after adjustment for clinical comorbidities.
Next, we calculated median annual out-of-pocket drug costs and weighted IQR for all beneficiaries and compared median costs of those spending >$2,000/year vs ≤$2,000/year using survey-specific linear regression as described in the preceding text. In order to estimate median annual out-of-pocket savings under the Inflation Reduction Act, we calculated the difference (with IQR) between median observed out-of-pocket costs among individuals spending >$2,000/year and $2,000 (the Inflation Reduction Act’s annual spending cap). To estimate total annual savings (with mean ± SE) for all beneficiaries spending >$2,000/year, we summed the difference between observed out-of-pocket costs and $2,000 for each individual included in our study population, and applied appropriate person-weights to calculate mean total annual savings over the survey period.
Finally, we estimated the annual number of beneficiaries with ≥1 CV risk factor or condition who would be newly eligible for full LIS (income >135% and <150% FPL) under the Inflation Reduction Act, and their sociodemographic characteristics. We also estimated the number of beneficiaries newly eligible for full LIS who spend >$2,000/year, as these individuals will also benefit from the annual spending cap.
ADDITIONAL ANALYSES.
We performed several additional analyses. First, we repeated our main analyses described in the preceding text after stratifying the study population into 2 subgroups: 1) Medicare beneficiaries with CV risk factors (high blood pressure, high cholesterol, and/or diabetes), but no CV conditions; and 2) Medicare beneficiaries with CV conditions (coronary heart disease, angina, myocardial infarction, stroke, and/or other heart disease). Because >87% of all Medicare beneficiaries in our initial sample had at least 1 CV risk factor or condition, we were unable to fit a model for the subgroup without any risk factors or conditions due to the small sample size. Second, to understand whether income was an effect modifier in regard to the association between sociodemographic characteristics and likelihood of spending >$2,000/year out-of-pocket, we repeated our main analysis after stratifying the study population by income levels (poor/near-poor/low-income [<200% FPL]; middle-income [≥200% to <400% FPL]; high-income [≥400% FPL]). Third, because we hypothesized that beneficiaries not qualifying for full LIS would experience the highest burden of out-of-pocket drug costs, we fit an additional multivariable logistic regression model to determine sociodemographic predictors of spending >$2,000/year among those not eligible for full LIS (individuals with income ≥150% FPL).
All analyses were performed using SAS 9.4 (SAS Institute). Our approach followed best practices for analysis of survey data, as described in similar studies using MEPS data.2,3 Two-sided P < 0.05 was used for statistical significance.
RESULTS
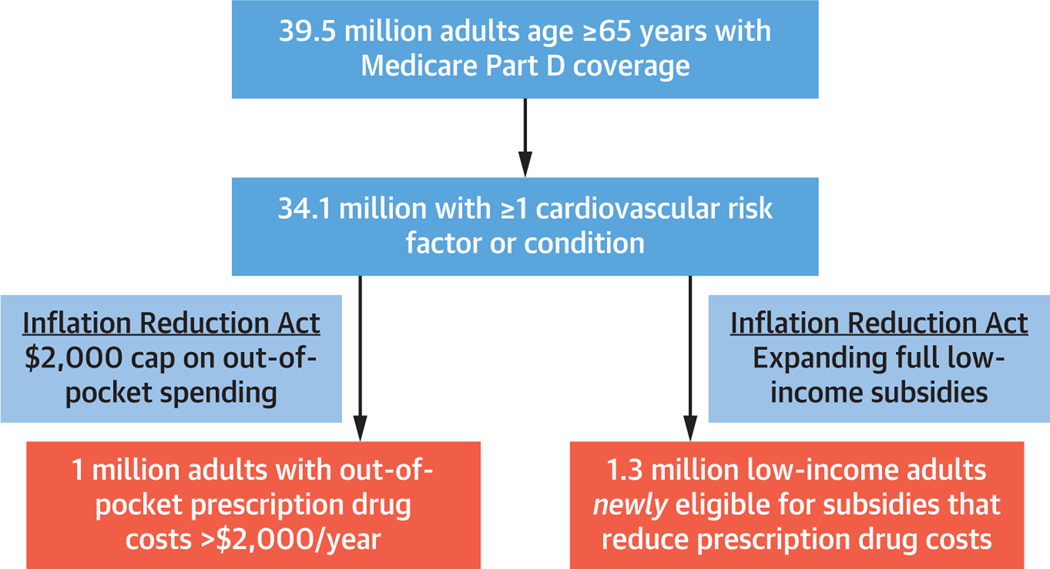
The annual weighted population of U.S. adults 65 years or older with Medicare Part D coverage was 39,484,261 ± 992,334 (mean ± SE). An estimated 34,056,335 ± 855,653 Medicare beneficiaries 65 years or older reported at least 1 CV risk factor or condition (mean age 74.5 years, 55.7% female), of whom 1,020,484 ± 77,055 (3.0%) experienced out-of-pocket drug costs >$2,000/year (Central Illustration). Beneficiaries who spent >$2,000/year were younger (mean age 73.4 vs 74.5 years; P = 0.03), more likely to be White (85.3% vs 74.1%; P < 0.001), and middle- or high-income (75.3% vs 66.6%; P = 0.001), but less likely to be Black (5.9% vs 9.9%; P < 0.001) or Hispanic (4.2% vs 9.5%; P < 0.001) than those who spent ≤$2,000/year (Table 1). Beneficiaries who spent >$2,000/year also had a higher burden of CV risk factors and conditions (Table 1).
CENTRAL ILLUSTRATION. Estimated Impact of the Inflation Reduction Act on Medicare Beneficiaries.
An estimated 1.02 million Medicare beneficiaries age ≥65 years with cardiovascular risk factors and/or conditions currently experience out-of-pocket drug costs >$2,000/year and would therefore benefit from the Inflation Reduction Act’s $2,000 annual spending cap. In addition, another 1.3 million beneficiaries would be newly eligible for full low-income subsidies (LIS) that reduce deductible costs and prescription copayments due to expansion of the income criteria to <150% federal poverty level (FPL) under the Inflation Reduction Act.
TABLE 1.
Baseline Characteristics of Beneficiaries With Cardiovascular Risk Factors and/or Conditions by Level of Annual Out-of-Pocket Drug Costs
| Out-of-Pocket Costs >$2,000 | Out-of-Pocket Costs ≤$2,000 | P Value | |
|---|---|---|---|
| Weighted population (annual)a | 1,020,484 ± 77,055 | 33,035,851 ± 835,217 | |
| Median annual out-of-pocket costs | $2,855 [$2,356-$3,795] | $145 [$40-$397] | <0.001 |
| Mean age, y | 73.4 ± 0.5 | 74.5 ± 0.1 | 0.03 |
| Female, % | 53.0 (46.6–59.5) | 55.8 (54.6–56.9) | 0.41 |
| Race/ethnicity, % | |||
| White | 85.3 (81.1–89.6) | 74.1 (72.4–75.8) | <0.001 |
| Hispanic | 4.2 (1.9–6.5) | 9.5 (8.3–10.7) | |
| Black | 5.9 (3.4–8.4) | 9.9 (8.9–10.9) | |
| Asian | 1.4 (0.1–2.8) | 4.7 (4.0–5.5) | |
| Other | 3.2 (1.4–5.0) | 1.8 (1.5–2.2) | |
| Poverty, % | |||
| Poor, <100% FPL | 6.1 (3.7–8.4) | 11.0 (10.2–11.8) | 0.001 |
| Near-poor, ≥100%-<125% FPL | 0.9 (0.0–2.0) | 5.6 (5.1–6.1) | |
| Low-income, ≥125%-<200% FPL | 17.7 (12.2–23.1) | 16.9 (15.8–17.9) | |
| Middle-income, ≥200%-<400% FPL | 31.1 (25.3–36.9) | 28.3 (26.9–29.6) | |
| High-income, ≥400% FPL | 44.2 (36.5–52.0) | 38.3 (36.6–40.0) | |
| Cardiovascular risk factor/condition, % | |||
| High blood pressure | 84.2 (79.2–89.2) | 76.8 (75.7–78.0) | 0.01 |
| High cholesterol | 76.2 (70.2–82.2) | 71.4 (70.1–72.7) | 0.15 |
| Diabetes | 51.1 (43.7–58.5) | 26.4 (25.2–27.7) | <0.001 |
| Coronary heart disease | 31.3 (24.7–37.8) | 18.7 (17.6–19.8) | <0.001 |
| Angina | 11.9 (6.9–16.8) | 7.3 (6.6–8.0) | 0.03 |
| Myocardial infarction | 18.9 (13.6–24.2) | 12.5 (11.6–13.4) | 0.01 |
| Stroke | 15.5 (10.8–20.2) | 14.0 (13.1–14.8) | 0.51 |
| Other heart disease | 43.5 (36.7–50.3) | 28.9 (27.7–30.2) | < 0.001 |
Values are mean ± SE, median [IQR], or % (95% CI).
Weighted population based on an unweighted sample of n = 13,477 beneficiaries.
FPL = federal poverty level.
OUT-OF-POCKET PRESCRIPTION DRUG COSTS AND AFFORDABILITY.
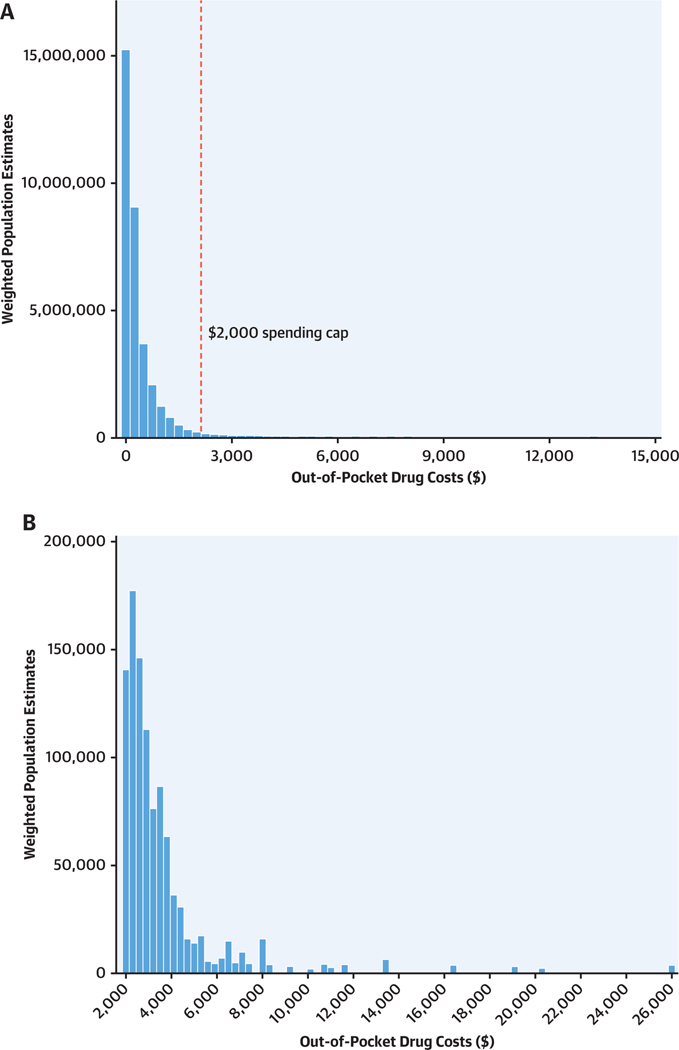
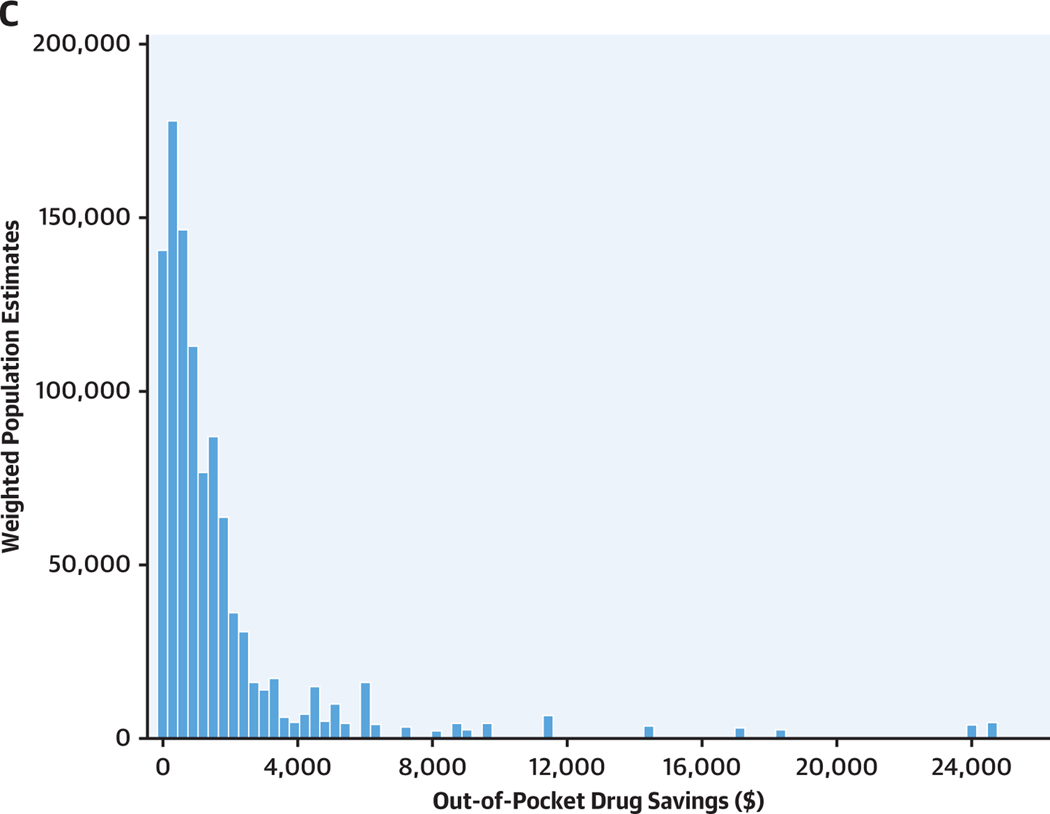
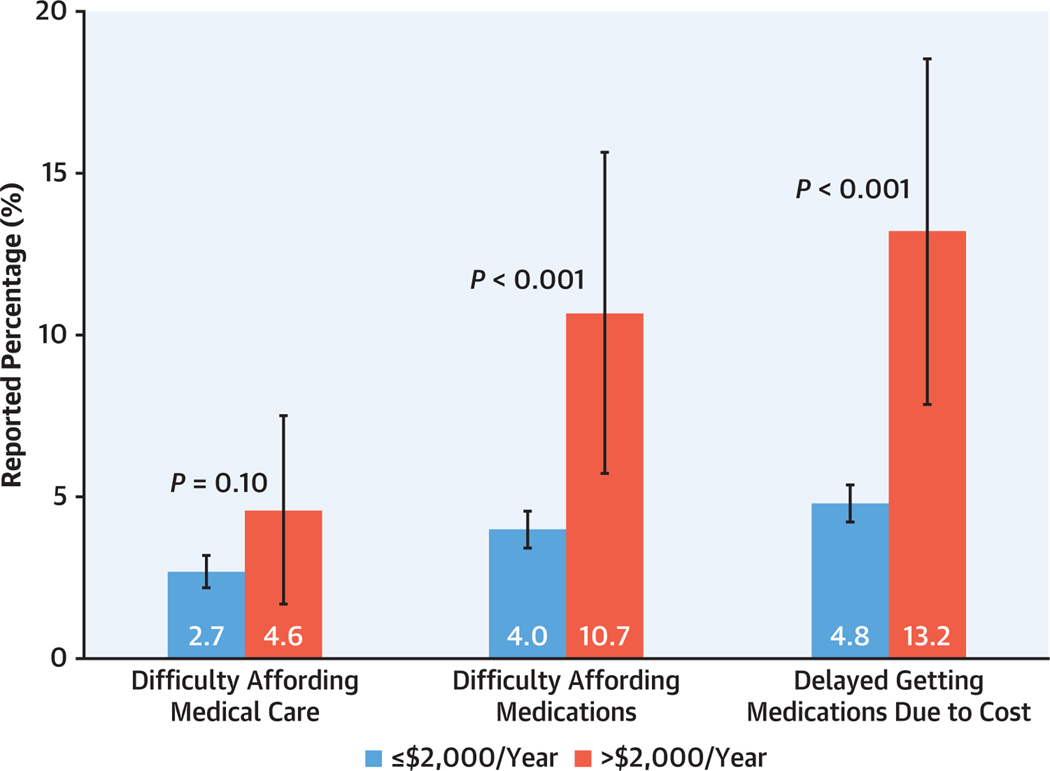
Among all Medicare beneficiaries with ≥1 CV risk factor or condition, median out-of-pocket drug costs were estimated at $153/year (IQR: $41-$440), and for those filling at least 1 prescription medication per year (N = 32,591,796), $168/year (IQR: $51-$462). Among beneficiaries spending >$2,000/year, median out-of-pocket costs were $2,855 (IQR: $2,356-$3,795); for those spending ≤$2,000/year, median costs were $145 (IQR: $40-$397) (P < 0.001) (Table 1). The distributions of annual out-of-pocket drug costs for all beneficiaries with CV risk factors/conditions and those with out-of-pocket costs >$2,000/year are shown in Figure 1. Medicare beneficiaries with CV risk factors or conditions who spent >$2,000/year, compared with those who spent ≤$2,000/year, were more likely to self-report difficulty affording prescription medications (10.7% vs 4.0%; P < 0.001) and delaying getting prescription medications due to cost (13.2% vs 4.8%; P < 0.001) (Figure 2, Supplemental Table 1).
FIGURE 1. Annual Out-of-Pocket Drug Costs and Savings for Beneficiaries.
The figure shows (A) distribution of annual out-of-pocket prescription drug costs for all Medicare beneficiaries, (B) distribution of annual out-of-pocket prescription drug costs for beneficiaries spending >$2,000/year, and (C) estimated distribution of annual out-of-pocket drug savings for beneficiaries spending >$2,000/year under the Inflation Reduction Act. The dotted line in A corresponds to the $2,000 annual spending cap under the Inflation Reduction Act. The estimated annual total out-of-pocket drug savings was $1,723,031,307 (SE ± $91,150,609) for beneficiaries spending >$2,000/year. In (A), 5 outliers for out-of-pocket costs ($16,458, $18,977, $20,429, $26,036, and $26,540) are not shown due to the upper-bound of the x-axis.
FIGURE 2. Out-of-Pocket Drug Costs and Difficulty Affording Medications and Medical Care.
The figure shows cost-related barriers to prescription medication use and medical care among Medicare beneficiaries with out-of-pocket prescription drug costs >$2,000/year (red) compared with those with costs ≤$2,000/year (blue).
SOCIODEMOGRAPHIC CHARACTERISTICS ASSOCIATED WITH ANNUAL OUT-OF-POCKET DRUG COSTS >$2,000.
After multivariable adjustment, Medicare beneficiaries age ≥75 years were less likely than those age 65 to 74 years to experience out-of-pocket drug costs >$2,000/year (adjusted OR: 0.67; 95% CI: 0.49–0.93) (Figure 3). Lower-income (<200% FPL) adults were less likely than higher-income (≥200% FPL) adults to have out-of-pocket costs >$2,000/year (adjusted OR: 0.63; 95% CI: 0.45–0.89). In addition, Hispanic (adjusted OR: 0.36; 95% CI: 0.20–0.65), Black (adjusted OR: 0.49; 95% CI: 0.31–0.78), and Asian (adjusted OR: 0.25; 95% CI: 0.09–0.68) adults were all less likely than White adults to experience out-of-pocket drug costs >$2,000/year.
FIGURE 3. Sociodemographic Characteristics Associated With Out-of-Pocket Spending >$2,000 Per Year.
The forest plot shows sociodemographic characteristics associated with out-of-pocket prescription drug spending >$2,000/year (vs ≤$2,000/year) among Medicare beneficiaries age ≥65 years with cardiovascular risk factors and/or conditions. Adjusted ORs and 95% CIs from the multivariable logistic regression model are shown. Age ≥75 years (compared with age 65–74 years); Hispanic, Black, and Asian race (compared with White race); and lower income were all associated with lower likelihoods of spending >$2,000/year. FPL = federal poverty level; LCL = lower control limit; UCL = upper control limit.
OUT-OF-POCKET SAVINGS UNDER THE INFLATION REDUCTION ACT’S $2,000 SPENDING CAP.
Under the Inflation Reduction Act’s annual spending cap, median out-of-pocket drug savings among beneficiaries who spend >$2,000/year were estimated to be $855 (IQR: $356-$1,795)/year, or roughly 30% of their median annual out-of-pocket drug costs (Figure 1). The estimated sum of annual out-of-pocket drug savings for all beneficiaries spending >$2,000/year was $1,723,031,307 ± $91,150,609.
BENEFICIARIES NEWLY ELIGIBLE FOR FULL LOW-INCOME SUBSIDIES UNDER THE INFLATION REDUCTION ACT.
An annual estimated 1,289,861 ± 60,962 Medicare beneficiaries age ≥65 years with CV risk factors or conditions would be newly eligible for full Part D LIS under the Inflation Reduction Act (ie, income >135% to <150% FPL) (Central Illustration). Among these beneficiaries, 37,125 ± 8,198 experienced out-of-pocket drug costs >$2,000/year, and would therefore also benefit from the $2,000 annual spending cap. The demographic and clinical characteristics of newly eligible beneficiaries are shown in Supplemental Table 2. Notably, nearly 33% of newly eligible beneficiaries would be from racial and ethnic minority subpopulations (14.9% Hispanic, 11.6% Black, 1.9% Asian, and 3.9% other races).
ADDITIONAL ANALYSES.
We performed several additional analyses. First, we repeated our main analyses after stratifying the study population into beneficiaries with no CV risk factors/conditions, CV factors (but no conditions), and beneficiaries with CV conditions (Supplemental Table 3). Among those spending >$2,000/year out-of-pocket, median costs were $2,738 (IQR $2,266-$3,547) for those with CV risk factors only, and higher among those with CV conditions (median $2,967 [IQR: $2,362-$3,840]). Our analysis of sociodemographic factors associated with spending >$2,000/year for each subgroup were largely similar to the main findings (Supplemental Figure 2). Second, we repeated our main analysis after stratifying the study population by income levels (low, middle, high). Baseline characteristics, median out-of-pocket spending, and multivariable regression models are shown in Supplemental Table 4 and Supplemental Figure 3. Third, among beneficiaries not qualifying for full LIS (individuals with incomes ≥150% FPL) (Supplemental Table 5), we fit an additional multivariable logistic regression model to determine sociodemographic predictors of spending >$2,000/year, and our findings were similar to our main analysis (Supplemental Figure 4).
DISCUSSION
In this nationally representative study, we found that more than 1 million Medicare beneficiaries with CV risk factors and/or conditions experience out-of-pocket prescription drug costs >$2,000/year, and will likely benefit from the Inflation Reduction Act’s cap on out-of-pocket costs. We estimate that this population would save approximately $1.7 billion annually in total out-of-pocket costs as a result of the spending cap. Additionally, an estimated 1.3 million adults with CV risk factors/conditions will be newly eligible to receive full LIS that further reduce drug costs, based on the Inflation Reduction Act’s expanded income criteria. Overall, our findings suggest that this landmark policy—the largest change to Medicare prescription drug costs since the creation of Medicare Part D in 2006—will have major implications on out-of-pocket costs for patients with CV risk factors and conditions.
Out-of-pocket prescription drug costs have risen steadily in the United States for more than a decade, raising concern among patients, clinicians, and policymakers.14,15 Prior studies of patients with CV risk factors/conditions (eg, diabetes, hypertension, coronary artery disease) have shown that higher out-of-pocket drug costs are associated with lower rates of medication adherence,4–6,16–18 consistent with our finding that patients spending >$2,000/year were >2 times more likely to report difficulty affording medications, as well as delays in obtaining medications, than those spending ≤$2,000/year. Increasingly, patients with CV disease are prescribed multiple brand-name or specialty medications that improve health outcomes but may incur prohibitively high prescription copayments.19 Reducing or eliminating copayments for CV medications has been shown to improve patient and health care system outcomes.20,21 By capping out-of-pocket prescription drug costs and expanding LIS, the Inflation Reduction Act could lead to improvements in medications adherence, and ultimately, health outcomes in Medicare beneficiaries with CV risk factors or conditions.
Although Medicare beneficiaries who spent >$2,000/year out-of-pocket on prescription drugs had a higher burden of CV risk factors and conditions than those who did not, we found that Black and Hispanic adults were less likely to experience high out-of-pocket costs compared with White adults. There are several potential explanations for this finding. First, Black and Hispanic adults are more likely to have lower incomes,22 and therefore, more likely to qualify for Part D LIS that reduce prescription drug costs. However, racial and ethnic differences persisted even after even adjusting for poverty in our main analysis and after excluding adults who would qualify for LIS in our secondary analysis. Second, racial and ethnic minority beneficiaries may be less likely to be prescribed or use medications due to systemic factors independent of income, including differences in usual sources of medical care, access to specialist care, differences in provider quality, or other factors such as structural racism experienced by these groups in health care settings.23 Third, it is possible that Black and Hispanic adults are more likely to face competing demands, such as food insecurity and housing instability,24–26 and that concerns about cost-sharing (eg, copayments, coinsurance, deductibles) dissuade these individuals from filling high-cost prescriptions that might worsen financial toxicity.15 Our finding that lower-income adults (<200% FPL) were less likely to spend >$2,000/year than higher-income adults on out-of-pocket on prescription drugs supports this hypothesis. Therefore, it is possible that the $2,000 annual spending cap (once in effect) may mitigate concerns about financial toxicity imposed by prescription drugs, resulting in increased prescription utilization among racial and ethnic minority groups. Overall, our findings highlight the importance of ongoing assessment of the equity implications of the Inflation Reduction Act in the years after its implementation.27
We also found that approximately 1.3 million Medicare beneficiaries with CV risk factors or conditions will newly qualify for Part D LIS due to expansion of income eligibility criteria (from <135% to <150% of the federal poverty level) under the Inflation Reduction Act. Nearly one-third of this population will be individuals from racial and ethnic minority backgrounds. The expansion of full LIS is critically important, as enrolled beneficiaries do not have to pay premium or deductible costs and prescription copayments (including for brand-name drugs) are generally zero or minimal.28
STUDY LIMITATIONS.
First, data on CV risk factors and conditions were self-reported by survey participants. Second, we only included data through 2019, because the onset of the COVID-19 pandemic in 2020 impacted prescription drug utilization in the United States.29,30 Third, our findings are estimates based on recent retrospective data and are limited to Medicare Part D beneficiaries, the target population of the Inflation Reduction Act. It is possible that we underestimated the total number of beneficiaries who might benefit from the Inflation Reduction Act’s provisions, as individuals who have historically had poor access and faced cost-related barriers to filling prescriptions may be more likely to use much-needed prescription medications in response to the spending cap. Fourth, our study estimates the impact of the Inflation Reduction Act’s $2,000 out-of-pocket spending cap, but did not evaluate other provisions (eg, negotiation of prescription drug prices, cap on out-of-pocket costs for insulin) that might also influence out-of-pocket drug costs for patients. Future quasiexperimental studies will need to assess the full effects of the Inflation Reduction Act on out-of-pocket drug costs and medication adherence for Part D beneficiaries, as well as the potential spillover effects (eg, cost shifting) of this policy on commercially insured patient populations.
CONCLUSIONS
In the United States, more than 1 million Medicare beneficiaries with CV risk factors and/or conditions experience out-of-pocket prescription drug costs >$2,000/year, and will likely benefit from the Inflation Reduction Act’s cap on out-of-pocket costs. This population would save an estimated $1.7 billion annually in total out-of-pocket drug costs as a result of the spending cap. In addition, another 1.3 million beneficiaries with CV risk factors would become newly eligible for LIS that reduce drug costs under the Inflation Reduction Act’s expanded income criteria. Overall, our findings suggest that this landmark policy will have major implications on out-of-pocket drug costs for Medicare beneficiaries with CV risk factors and/or disease, which could ultimately impact medication adherence and CV outcomes in the United States.
Supplementary Material
PERSPECTIVES.
COMPETENCY IN SYSTEMS-BASED PRACTICE:
More than 1 million Medicare beneficiaries with cardiovascular risk factors and/or conditions experience out-of-pocket prescription drug costs >$2,000 per year, and will likely benefit from the 2022 Inflation Reduction Act’s out-of-pocket spending cap, amounting to an estimated annual out-of-pocket savings of $1.7 billion. Approximately 1.3 million beneficiaries would be newly eligible for full low-income subsidies that significantly reduce drug costs.
TRANSLATIONAL OUTLOOK:
Following full implementation of the Inflation Reduction Act’s prescription drug provisions by 2026, implementation and surveillance efforts by health care providers and health systems to improve medication access for eligible patients will be integral to improving clinical outcomes.
FUNDING SUPPORT AND AUTHOR DISCLOSURES
This research project was supported by National Heart, Lung, and Blood Institute grant R01HL164561 (Dr Wadhera), who also receives research support from the National Heart, Lung, and Blood Institute, National Institutes of Health, grant K23HL148525. Dr Yeh has received consulting fees and research grants from AstraZeneca. Dr Wadhera has been a consultant for Abbott and CVS Health, outside the submitted work. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
ABBREVIATIONS AND ACRONYMS
- CV
cardiovascular
- FPL
federal poverty level
- LIS
low-income subsidies
- MEPS
Medical Panel Expenditure Survey
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the AuthorCenter.
REFERENCES
- 1.Khera R, Valero-Elizondo J, Nasir K. Financial toxicity in atherosclerotic cardiovascular disease in the United States: current state and future directions. J Am Heart Assoc. 2020;9(19):e017793. 10.1161/JAHA.120.017793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khera R, Valero-Elizondo J, Okunrintemi V, et al. Association of out-of-pocket annual health expenditures with financial hardship in low-income adults with atherosclerotic cardiovascular disease in the United States. JAMA Cardiol. 2018;3(8):729–738. 10.1001/jamacardio.2018.1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang SY, Valero-Elizondo J, Ali H, et al. Out-of-pocket annual health expenditures and financial toxicity from healthcare costs in patients with heart failure in the United States. J Am Heart Assoc. 2021;10(14):e022164. 10.1161/JAHA.121.022164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khera R, Valero-Elizondo J, Das SR, et al. Cost-related medication nonadherence in adults with atherosclerotic cardiovascular disease in the United States, 2013 to 2017. Circulation. 2019;140(25):2067–2075. 10.1161/CIRCULATIONAHA.119.041974 [DOI] [PubMed] [Google Scholar]
- 5.Kang H, Lobo JM, Kim S, Sohn MW. Cost-related medication non-adherence among U.S. adults with diabetes. Diabetes Res Clin Pract. 2018;143:24–33. 10.1016/j.diabres.2018.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel MR, Piette JD, Resnicow K, Kowalski-Dobson T, Heisler M. Social determinants of health, cost-related non-adherence, and cost-reducing behaviors among adults with diabetes: findings from the National Health Interview Survey. . Med Care. 2016;54(8):796–803. 10.1097/MLR.0000000000000565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandra A, Flack E, Obermeyer Z. The health costs of cost-sharing. NBER Working Paper No. 28439. National Bureau of Economic Research. February 2021. Accessed November 6, 2022. http://www.nber.org/papers/w28439 [Google Scholar]
- 8.H.R.5376 – 117th Congress (2021–2022): Inflation Reduction Act of 2022. August 16, 2022. Accessed November 6, 2022. https://www.congress.gov/bill/117th-congress/house-bill/5376
- 9.Gagne JJ, Choudhry NK, Kesselheim AS, et al. Comparative effectiveness of generic and brand-name statins on patient outcomes. Ann Intern Med. 2014;161(6):400–407. 10.7326/M13-2942 [DOI] [PubMed] [Google Scholar]
- 10.Hsu J, Price M, Huang J, et al. Unintended consequences of caps on Medicare drug benefits. N Engl J Med. 2006;354(22):2349–2359. 10.1056/NEJMsa054436 [DOI] [PubMed] [Google Scholar]
- 11.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence. Circulation. 2009;119(23):3028–3035. 10.1161/CIRCULATIONAHA.108.768986 [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality. MEPS-HC Response Rates by Panel. Accessed January 13, 2023. https://meps.ahrq.gov/survey_comp/hc_response_rate.jsp
- 13.Hill SC, Zuvekas SH, Zodet MW. Implications of the accuracy of MEPS prescription drug data for health services research. Inq J Health Care Organ Provis Financ. 2011;48(3):242–259. 10.5034/inquiryjrnl_48.03.04 [DOI] [PubMed] [Google Scholar]
- 14.Tarazi W, Finegold K, Sheingold S, De Lew N, Sommers BD. Prescription drug affordability among Medicare beneficiaries. Issue Brief No. HP-2022–03 Office of the Assistant Secretary for Planning and Evaluation. U.S. Department of Health and Human Services; January 2022. [Google Scholar]
- 15.Rector TS, Venus PJ. Do drug benefits help Medicare beneficiaries afford prescribed drugs? Health Aff (Millwood). 2004;23(4):213–222. 10.1377/hlthaff.23.4.213 [DOI] [PubMed] [Google Scholar]
- 16.Osborn CY, Kripalani S, Goggins KM, Wallston KA. Financial strain is associated with medication nonadherence and worse self-rated health among cardiovascular patients. J Health Care Poor Underserved. 2017;28(1):499–513. 10.1353/hpu.2017.0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marcum ZA, Zheng Y, Perera S, et al. Prevalence and correlates of self-reported medication non-adherence among older adults with coronary heart disease, diabetes mellitus, and/or hypertension. Res Soc Adm Pharm RSAP. 2013;9(6). 10.1016/j.sapharm.2012.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rome BN, Gagne JJ, Avorn J, Kesselheim AS. Non-warfarin oral anticoagulant copayments and adherence in atrial fibrillation: a population-based cohort study. Am Heart J. 2021;233:109–121. 10.1016/j.ahj.2020.12.010 [DOI] [PubMed] [Google Scholar]
- 19.Sandhu AT, Heidenreich PA. The affordability of guideline-directed medical therapy. Circulation. 2021;143(11):1073–1075. 10.1161/CIRCULATIONAHA.120.053291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choudhry NK, Bykov K, Shrank WH, et al. Eliminating medication copayments reduces disparities in cardiovascular care. Health Aff (Millwood). 2014;33(5):863–870. 10.1377/hlthaff.2013.0654 [DOI] [PubMed] [Google Scholar]
- 21.Choudhry NK, Fischer MA, Avorn JL, et al. The impact of reducing cardiovascular medication copayments on health spending and resource utilization. J Am Coll Cardiol. 2012;60(18):1817–1824. 10.1016/j.jacc.2012.06.050 [DOI] [PubMed] [Google Scholar]
- 22.Wadhera RK, Wang Y, Figueroa JF, Dominici F, Yeh RW, Joynt Maddox KE. Mortality and hospitalizations for dually enrolled and nondually enrolled Medicare beneficiaries aged 65 years or older, 2004 to 2017. JAMA. 2020;323(10):961–969. 10.1001/jama.2020.1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gaskin DJ, Briesacher BA, Limcangco R, Brigantti BL. Exploring racial and ethnic disparities in prescription drug spending and use among Medicare beneficiaries. Am J Geriatr Pharmacother. 2006;4(2):96–111. 10.1016/j.amjopharm.2006.06.008 [DOI] [PubMed] [Google Scholar]
- 24.Coleman-Jensen A, Gregory C, Singh A. Household Food Security in the United States in 2013. ERR-173. US Department of Agriculture, Economic Research Service; September 2014. [Google Scholar]
- 25.Fusaro VA, Levy HG, Shaefer HL. Racial and ethnic disparities in the lifetime prevalence of homelessness in the United States. Demography. 2018;55(6):2119–2128. 10.1007/s13524-018-0717-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson DA, Boadu O, Jones AL, et al. Analysis of initiating anticoagulant therapy for atrial fibrillation among persons experiencing homelessness in the veterans affairs health system. JAMA Netw Open. 2022;5(7):e2223815. 10.1001/jamanetworkopen.2022.23815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Essien UR, Dusetzina SB, Gellad WF. A policy prescription for reducing health disparities—achieving pharmacoequity. JAMA. 2021;326(18): 1793–1794. 10.1001/jama.2021.17764 [DOI] [PubMed] [Google Scholar]
- 28.Shapiro JR. 2023 Resource and Cost-Sharing Limits for Low-Income Subsidy (LIS). Centers for Medicare & Medicaid Services; 2022. [Google Scholar]
- 29.Ismail H, Marshall VD, Patel M, Tariq M, Mohammad RA. The impact of the COVID-19 pandemic on medical conditions and medication adherence in people with chronic diseases. J Am Pharm Assoc. 2022;62(3):834–839.e1. 10.1016/j.japh.2021.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159–169. 10.1016/j.jacc.2020.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.