Abstract
Colorectal cancer, the third most common cancer worldwide, affects 40–45% of patients on the right side. Surgery, especially minimally invasive methods such as laparoscopic and robotic procedures, is the preferred treatment. However, these techniques present technical complications. The anatomical complexity and variations in vessel branching patterns pose challenges, particularly for less experienced surgeons. The CoDIG 2 is a nationwide observational study involving 76 specialized Italian general surgery departments focused on colorectal surgery. The centres were directed to maintain their standard surgical and clinical practices. The aim of this study was to analyse the intraoperative vascular anatomy of Italian patients who underwent laparoscopic right colectomy and explore the ligature techniques used by Italian surgeons. Surgeons reported information about vascularization of the right colon for 616 patients and about surgical anatomy of RCA for 368 patients. Fifty-three patients (10.8%) showed no RCA intraoperatively. The right colic artery (RCA) was categorized according to the Yada classification (types 1–4) during evaluation, and intraoperative assessments revealed that Yada type 1 was the most common type (55.2%), while radiologic evaluations revealed a higher prevalence of type 2. Furthermore, compared with the superior mesenteric vein (SMV), the RCA is more often located anteriorly according to intraoperative and contrast-enhanced CT examination; 59.9% were found in the anterior position during intraoperative examination, while 40.1% were found in the same position on preoperative contrast-enhanced CT. Vascularization of the right colon, including missing branches, additional branches, shared trunks, and retro-superior courses of the mesenteric vein, exhibited notable variations. To understand vascular variations, a preoperative radiological study is necessary; although there was no concordance between the intraoperative and radiological evaluations, this is a limitation of preinterventional radiological evaluation (PII) because it is always needed for oncological staging. This approach is especially critical for inexperienced surgeons to avoid potential complications, such as problematic bleeding.
Keywords: Vascular anatomy, Right colic artery, Superior mesenteric artery, Yada classification, Right hemicolectomy, Laparoscopy
Introduction
According to the estimated 2020 incidence in the Global Cancer Observatory database (GLOBOCAN), colorectal cancer is the third most common cancer in the world, with 1.931.590 new cases (10%), and the second most common cause of death, with 935.173 deaths (9.4%) [1]. An analysis of the Surveillance, Epidemiology, and End Results (SEER) database revealed that 40–45% of all colon-rectal cancers are located on the right side [2, 3] .
During right colectomy, surgeons usually search for anatomical variations in vessels in common clinical practice to attempt correct central vessel ligation [4, 5]. Currently, laparoscopic identification is easier than intraoperative identification [6, 7]. In high-volume centres, this technical step is a requirement [8, 9]; in fact, correct central vessel ligation is associated with a high number lymph node dissections. For these reasons, some surgical groups aim to standardize the technique for right-sided colon cancer [10, 11].
In some cases, anatomical complexity and anatomical variations in vessel branching patterns pose challenges for young surgeons during laparoscopic or robotic right hemicolectomy [12, 13]. Consequently, accurate knowledge of possible anatomical variations is very important for safe oncological identification and dissection of vessels in the right colon [14, 15].
The aim of our study was to analyse the anatomical variations in the vessels of Italian patients who underwent laparoscopic right colectomy; we hope that the findings of our study will be added to the literature to improve the standardization of colorectal surgical procedures.
Methods/design
The CoDIG2 (ColonDxItalian Group – Italian Right Colon Group) study (ClinicalTrials.gov; ID: NCT05943951) was a 6-month multicentre prospective observational study (01/04/2022 to 30/09/2022) concerning “laparoscopic right hemicolectomy” for cancer treatment. The aim of the present study was to report the steps Italian surgeons perform during “laparoscopic right hemicolectomy”, namely, ligature of vessels and extension of lymphadenectomy. Furthermore, a section of the study is dedicated to presenting intraoperative data about the anatomical variability of the vascularization of the right colon. Regarding the lymphadenectomy, our working group has recently published an article on the subject [16].
The CoDIG2 was designed based on relevant guidelines and regulations applicable to research involving human subjects, such as the World Medical Association Declaration of Helsinki and the Medical Research Involving Human Subjects Act. Written informed consent was obtained from all participants.
For this study, a prospective patient questionnaire was administered at the University of Ferrara and was submitted to all members of the SICE (Società Italiana di Chirurgia Endoscopica e Nuove Tecnologie).
Outcomes
Anatomical variants of the superior mesenteric artery were categorized into types according to Yada’s classification [17].
The principal outcome was the absence of the right colic artery (RCA) (reported as type 4 according to the Yada classification) on evaluation during surgical dissection.
The secondary outcomes were:
- The RCA was categorized according to the Yada classification (Fig. 1) on evaluation during surgical dissection and on preinterventional (PII) radiological evaluation via computed tomography (CT):
- The RCA arises independently from the superior mesenteric artery (SMA) (Yada Type 1).
- The RCA and middle colic artery (MCA) have a common trunk (Yada Type.
- The RCA and ileocolic artery (ICA) have a common trunk (Yada Type 3).
Topographic relationship between the RCA and SMV on evaluation during surgical dissection and, on preinterventional (PII) radiological evaluation, the RCA was located anterior or posterior to the SMV (Fig. 2).
Fig. 1.
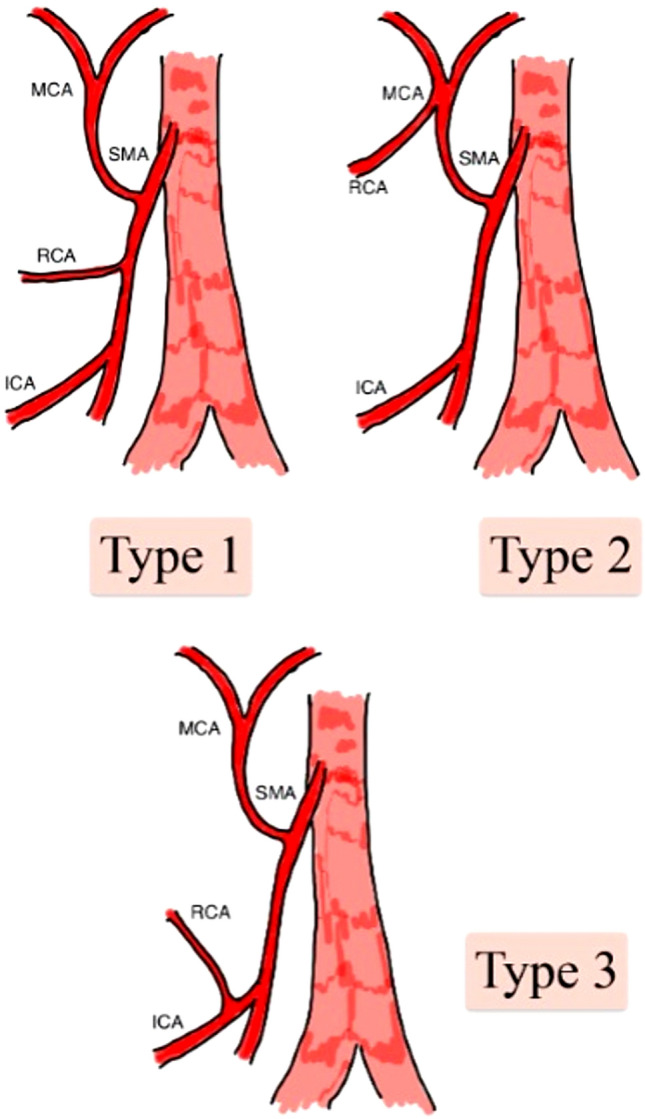
Yada classification of RCA variations. SMA superior mesenteric artery, MCA middle colic artery, RCA right colic artery, ICA ileocolic artery
Fig. 2.
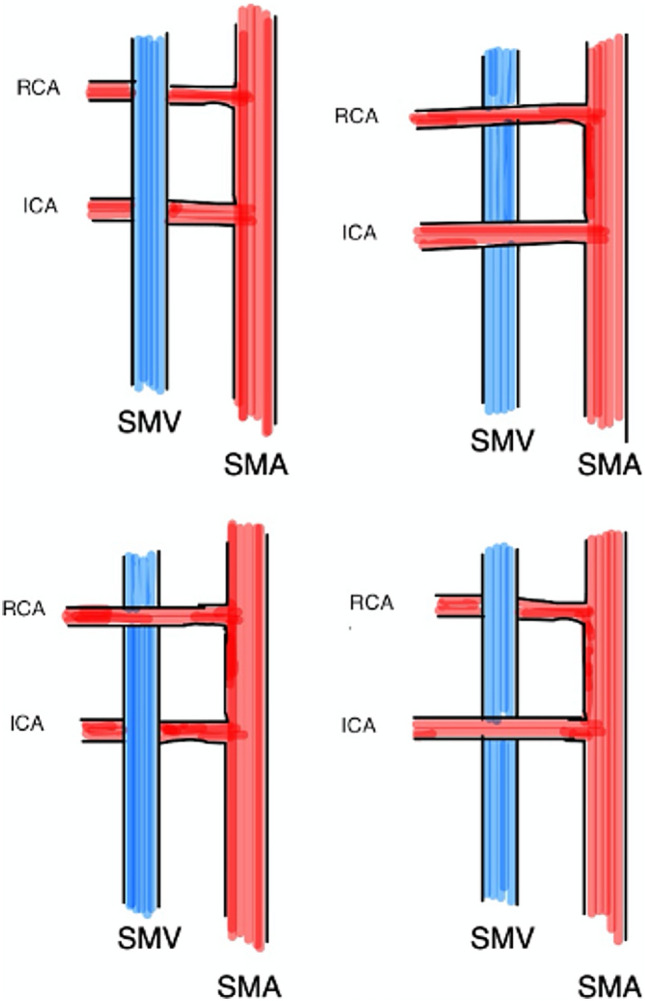
Topographic relationship between the RCA and SMV
Data collection
A member of each participating centre prospectively enrolled data for consecutive patients on a website sponsored by SICE for smart access through personal computers, tablets and smartphones. Consequently, we collected baseline data (sex, age, BMI, Charlson comorbidity index (BMI), American Society of Anaesthesiologists (ASA) score, preoperative diagnosis, TNM stage, histologic diagnosis, surgical technique, operative time, type of anastomosis, intraoperative complications, tumour-free margin, terminal ileum length, vascular ligature, mesocolon sail integrity and area, total lymph nodes/positive lymph nodes, ERAS protocol adherence, length of postoperative hospital stay, and postoperative complications) from the hospital electronic medical records system in our electronic database. A consultant recognized the vessel anatomy intraoperatively; subsequently, the same expert surgeons completed the questionnaire.
The inclusion criteria were as follows: all consecutive patients aged >18 years who underwent elective laparoscopic or robotic right colectomy. The exclusion criteria were emergency surgery, laparotomic right colectomy, ASA > IV, and pregnancy.
All patients underwent standard laparoscopic or robotic right colectomy with D2 lymphadenectomy.
In the PII evaluation, all patients underwent dynamic CT, and a senior radiologist reviewed the contrast-enhanced images.
Statistical methods
Frequencies and crosstabulations were conducted with SPSS 27.0 software for artery location (anterior or posterior), evaluation type (intraoperative or contrast-enhanced CT), and Yada classification (Type 1 through Type 4). Bootstrap 95% confidence intervals were computed using 1000 bootstrapped samples. Following the recommendations of the American Statistical Association, we report 95% confidence intervals instead of p values from null hypothesis tests. Differences in N between analyses were due to patients with missing data for the variables being investigated [18].
Results
In the CoDIG2 cohort, 788 patients were enrolled from 76 participating centres over a period of 6 months from April 2022 to October 2022; surgeons reported the vascularization of the right colon for only 368 patients. All patients were Caucasian (100%).
Fifty-three patients had no RCA intraoperatively (10.8%), which is reported as type 4 according to the Yada classification (Fig. 3).
Fig. 3.
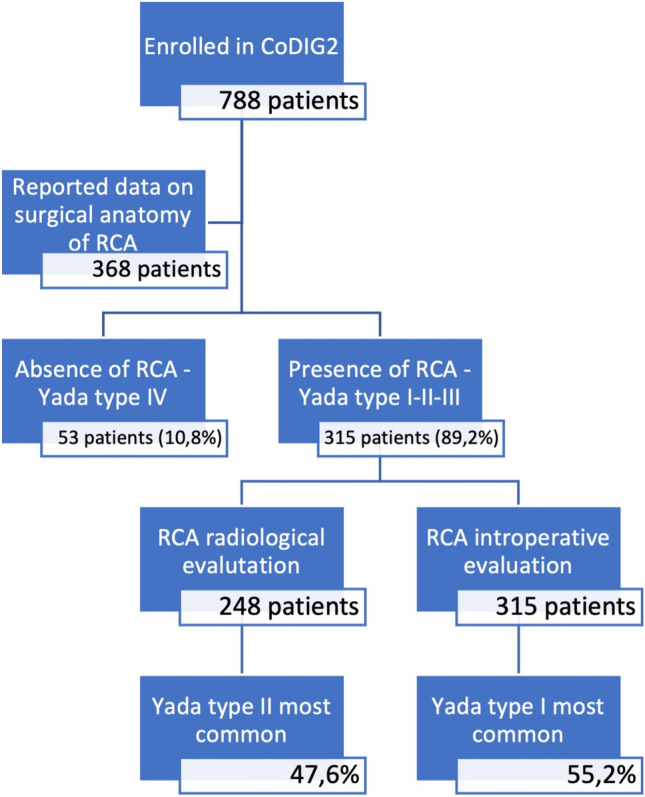
Absence of the RCA
For the other 315 patients (89.2%), vascularization of the right colon artery was categorized through the Yada classification and disaggregated by evaluation type. Among the same patients, radiological and intraoperative findings were reported for 248 patients and 315 patients, respectively.
This analysis revealed that intraoperatively, Type 1 was the most common condition (55.2%). In contrast, radiological preoperative evaluation (contrast-enhanced CT) revealed that Type 2 was most common (47.6%) (Table 1).
Table 1.
Frequencies and percentages of arterial vascularization from the superior mesenteric artery based on evaluation type and Yada’s classification
| Evaluation type | Yada classification | Frequency | % | 95% CI lower % | 95% CI upper % |
|---|---|---|---|---|---|
| Intraoperative | Type 1 | 174 | 55.2 | 49.5 | 60.3 |
| Type 2 | 112 | 35.6 | 30.5 | 41.0 | |
| Type 3 | 29 | 9.2 | 6.3 | 12.4 | |
| Total | 315 | 100.0 | 100.0 | 100.0 | |
| Contrast-enhanced CT | Type 1 | 99 | 39.9 | 33.9 | 46.0 |
| Type 2 | 118 | 47.6 | 41.5 | 54.0 | |
| Type 3 | 31 | 12.5 | 8.5 | 16.9 | |
| Total | 248 | 100.0 | 100.0 | 100.0 |
The RCA arises independently from the SMA (superior mesenteric artery) (Yada type 1). This variation was the most common finding during intraoperative dissection (55.2%), but the rate was lower during radiological preoperative evaluation (contrast-enhanced CT) (33.9%). In type 1 patients, the RCA was located in the anterior position to the superior mesenteric vein (SMV) (55.04% of the patients).
Common trunk of the RCA and MCA (middle colic artery) (Yada type 2). This variation was the most common finding during radiological preoperative evaluation (contrast-enhanced CT) (47.6%), but the rate was lower for intraoperative dissection (35.6%). Among those classified as type 2, the common trunk anterior to the SMV was the most common location (66.39%).
Common trunk of the RCA and ICA (ileo-colic artery) (Yada type 3). This variation was the most uncommon, and the rates of radiological preoperative evaluation (contrast-enhanced CT) (12.5%) and intraoperative dissection (9.2%) were the same. In type 3 patients, the posterior position to the SMV was the most common location of the common trunk (66.39%).
Furthermore, the topographic location between the RCA and SMV (Figure 2) was evaluated intraoperatively in 315 patients, and it was evaluated preoperatively via contrast-enhanced CT in 248 patients. The evaluation of tumour type stratified by artery location revealed a different trend; in fact, for the intraoperative and contrast-enhanced CT images, 59.9% of the intraoperative cases were located in the anterior position, while 40.1% were located in the same position on preoperative contrast-enhanced CT images (Table 2).
Table 2.
Frequencies and percentages of the different types of superior mesenteric arteries according to evaluation type and Yada classification
| Artery location | Evaluation type | Frequency | % | 95% CI lower % | 95% CI upper % |
|---|---|---|---|---|---|
| Anterior | Intraoperative | 190 | 59.9 | 54.7 | 65.0 |
| Contrast-enhanced CT | 127 | 40.1 | 35.0 | 45.3 | |
| Total | 317 | 100.0 | 100.0 | 100.0 | |
| Posterior | Intraoperative | 125 | 50.8 | 44.5 | 57.7 |
| Contrast-enhanced CT | 121 | 49.2 | 42.3 | 55.5 | |
| Total | 246 | 100.0 | 100.0 | 100.0 |
Discussion
In this prospective observational study, we reported the results of vascular variations during intraoperative and radiological evaluations performed on patients enrolled in CODIG 2 who underwent laparoscopic right colectomy.
Currently, laparoscopic and robotic evaluations routinely reveal anatomical details that were not commonly visualized; consequently, there is increasing knowledge of vascular variations.
The evaluation of these anatomical vascular variants is a basic step for the standardization of oncological right hemicolectomy. In fact, these new anatomical data have thus made this technique safer because it is associated with a reduction in postoperative morbidity related to ligatures [14].
In addition, the presence of arterial variants seems to be associated with better outcomes in terms of oncological radicality; recently, Efetov et al. reported the results of a large comparative study of 260 Russian and Chinese patients. They suggested that in Western countries, increased complexity in performing D3 lymph node dissection is associated with an increased prevalence of surgically challenging anatomic variations in the right colon vessels [19].
Currently, CODIG 2 is the largest study in the literature in which an intraoperative description of the arteries of the right colon has been reported; to date, only eight articles have been published on the topic, and they have included a total of 930 patients [13, 20–26].
Furthermore, in our study, anatomical evaluation was always performed during laparoscopic right hemicolectomy; only Wu [20], Ohsawa [25] and Lee [22] reported performing laparoscopic evaluation during right hemicolectomy, but the numbers of patients were lower 60, 205 and 116, respectively. Furthermore, Alsabilah reported performing a laparoscopic evaluation but did not differentiate the number of patients examined laparoscopically or via open approaches [13]. All the studies in which anatomical analysis was performed were conducted in Asia (Korea, Japan and China); however, the data in our study were based only on the Italian population.
Our results do not agree with the findings of an extensive systematic review of international literature based on 41 studies (n = 4691 patients) [27].
Regarding the absence of an RCA, our results (absence in 10.4% of patients) differed from those of the aforementioned systematic review and meta-analysis, which reported absence in 27.4% of patients [27]; this very obvious difference was also present in laparoscopic studies conducted in Asia (Wu 45%, Ohsawa 48.8%, Lee 67.3%) [20, 22, 25], which could suggest that ethnic factors may be the basis of this difference. In addition, the origin of the RCA was evaluated and categorized according to the Yada classification:
Yada type 1 (an RCA that originates independently of the SMA) was the most common type according to the intraoperative evaluation in our study (55.2%) and in the systematic review, where the percentage was greater (68.9%).
Yada type 2 (common branch for the RCA and MCA) was the second variant by frequency according to the intraoperative analysis of our study (35.6%) and systematic review, where the percentage was lower (17.7%).
Yada type 3 (common branch for the RCA and ICA) was the rarest variant according to the intraoperative evaluation (9.2%) and the systematic review (13.2%).
In patients with anatomical variations of the RCA, there is a great surgical risk of not recognizing a type 2 or 3 Yada variant; this is of great surgical importance because, in some cases, the MCA can be confused with the RCA and cut/ligated. This could impair the blood supply to the distal transverse colon [28].
For these reasons, the importance of a preoperative radiological study has been supported by numerous surgeons [29], who argue that right colon vascularization can be delineated radiologically, and that preoperative vascular mapping is a necessary component of the CME technique.
In addition, another critical point related to the anatomical variants of the vascularization of the right colon is the correct understanding of the relationship between the SMV and the branches of the SMA. Knowledge of such topographic reports is of paramount importance for preventing iatrogenic lesions of the SMV, which are serious and potentially fatal during vascular dissection of right hemicolectomies [30].
This condition represents a very important risk because these topographic relationships are highly variable. In our study, 59.9% of variants located in the anterior course of the RCA were found via intraoperative evaluation, whereas 40.1% were found via preoperative contrast-enhanced CT analyses (Table 2). This result is not in line with the literature in which the RCA precedes the SMV in 53.04% of patients.
The learning curve of laparoscopic and robotic techniques for right colectomy was evaluated. A risk-adjusted cumulative sum (CUSUM) model was used from Tekkis et al. to evaluate the learning curve for right colon cancer treatment; this study reported that 55 patients were needed to prove proficiency for right colectomy. During the learning curve, the most common mistake is dissection of the wrong surgical layers, which is common in the deep retroperitoneal space, especially for a lesion in Gerota's fascia or an injury to deep retroperitoneal structures [31, 32].
Identification and central ligation of the main mesocolic vessels can be difficult for novice surgeons; for this reason, several surgeons have suggested the usefulness of three-dimensional printing of superior mesenteric vessels for determining the course of the superior mesenteric vessels [33, 34].
In fact, right colectomies performed by novice surgeons are commonly prolonged procedures with increased bleeding and decreased lymph node resection [34].
This study is limited by the difficulty of identifying vascular anatomy during laparoscopic or robotic surgery. According to Kuzu et al., it is practically impossible to trace each vessel to its origin in real-time surgery, especially within the fatty mesocolon, thereby increasing the risk of severe complications. Additionally, it is challenging to ascertain the names of each tributary of the superior mesenteric artery (SMA) and superior mesenteric vein (SMV) until all tributaries are centrally ligated and when the specimen is removed [15].
Nonetheless, our study has several limitations, most of which involved subjective evaluation by surgeons or radiologists. In fact, differences in anatomical knowledge for surgical proficiency can lead to differences in opinions about the vessels. For this reason, SICE has a new ongoing study in which the researchers aim to reduce this bias [36, 37]:
The surgeon photographed the vessels during intraoperative dissection and sent the photos to three consultants to check the correctness of the identification.
The radiologist extracted the CT photogram and sent the images to three consultants to check the correctness of the identification.
Accurate identification of anatomical structures involved in surgical intervention is a crucial component of the undergraduate medical curriculum and frequently difficult, as time constraints often limit the depth of instruction. [37]. We hope that this new research can resolve this “information gap” for right minimally invasive colectomy regarding poor knowledge of vascular variants. In fact, vascular variations are still the cause of bias in surgical training that cannot be resolved from surgical anatomy dissection courses [38].
Conclusion
Right colectomy performed with minimally invasive surgical techniques (laparoscopy or robotic) and hemicolectomy with complete mesocolic excision are the treatment of choice for colorectal cancer. The purpose of minimally invasive surgery is to achieve better oncological outcomes while minimizing the incidence of postoperative complications.
The vascularization of the right colon showed considerable variation, i.e., the absence of some branches, supernumerary branches, common trunks and retro-superior courses of the mesenteric vein. To understand vascular variations, a preoperative radiological study is necessary; although there was no concordance between the intraoperative and radiological evaluations, this is a limitation of radiological PII because it is always needed for oncological staging.
It is therefore crucial to increase the knowledge and study of changes in the vascular anatomy of the right colon during surgical resection, particularly during minimally invasive surgery.
We hope that our study can support young surgeons in mastering the learning curve for right colectomy in terms of accurately identifying, exposing, and dissecting right colonic arterial vessels. As previously reported by Wu, knowledge of these variations can help residents reduce the risk of damaging arterial vessels in the right colon and thus avoid troublesome bleeding.
Acknowledgements
The study was approved by the Ethical Committee of the province of Ferrara, authorized by the Azienda Ospedaliero-Universitaria of Ferrara with the Protocol CE 890/2020/OSS/AOUFe, and registered on clinicaltrials.gov (NCT05943951).
SICE CoDIG 2 (ColonDx Italian Group)*: *Adamo V. (Vercelli), *Ammendola M. (Catanzaro), *Angelini P. (Napoli), *Annecchiarico M. (Benevento), *Aprea G. (Napoli), *Autuori F. (Iglesias, SU), *Baldazzi G. (Legnano, MI), *Balla A. (Civitavecchia, Roma), *Baronio G. (Esine, BS), *Bellio G. (Piove di Sacco, PD), *Bertelli G. (Bolzano), *Bima C. (Torino), *Bonomo L.D. (Borgosesia, VC), *Borreca D. (Torino), *Botteri E (Montichiari), *Brescia A. (Roma), *Cafagna L. (Andria), *Capelli P. (Piacenza), *Caracino V. (Pescara), *Caricato M. (Roma), *Carlini M. (Roma), *Cassinotti E. (Milano), *Catarci M. (Roma), *Chiaro P. (Torino), *Cillara N. (Cagliari), *Clementi M. (Aquila), *Contul R.B. (Aosta), *Curro G. (Catanzaro), *De Manzini N. (Trieste), *Degiuli M. (Orbassano, TO), *Delogu D. (Sassari), *Di Leo A. (Trento), *Elmore U. (Milano), *Ercolani G. (Forlì), *Festa F. (Torino), *Galleano R. (Savona), *Gambino G. (Trapani), *Gelmini R. (Modena), *Giordano A. (Prato), *La Mendola R. (Rovigo), *Laface L. (Carate Brianza, MB), *Masoni L. (Roma), *Maurizi A. (Jesi), *Memeo R. (Acquaviva delle Fonti, Bari), *Mercantini P. (Roma), *Merola G. (Frattamaggiore, NA), *Milone M. (Napoli), *Montuori M. (Ponte San Pietro, BG), *Morelli L. (Pisa), *Muttillo I.A. (Roma), *Nascimbeni R. (Brescia), *Nelli T. (Firenze), *Olmi S. (Bergamo), *Ortenzi M. (Ancona), *Patriti A. (Pesaro), *Pavone G. (Foggia), *Pisano M. (Cagliari), *Polastri R. (Biella), *Rega D. (Napoli), *Rottoli M. (Bologna), *Saladino E. (Messina), *Santarelli M. (Torino), *Santoro R. (Viterbo), *Sartori A. (Montebelluna, TV), *Scatizzi M. (Bagno a Ripoli, FI), *Sica G. (Roma), * Silecchia G.(Roma), *Siquini W. (Macerata), *Sorrentino M. (Latisana, UD), *Staderini F. (Firenze), *Vincentini L. (Castellana Grotte, BA),Abate E. (Carate Brianza, MB), Aizza G. (Trieste), Amodio P. (Viterbo), Aquilino F. (Castellana Grotte, BA), Argenio G. (Benevento), Avanzolini A. (Forlì), Baldari L. (Milano), Banchini F. (Piacenza), Benedetti M. (Roma), Bertino V. (Trapani), Bianco A. (Biella), Blasi F. (Roma), Bonariol L. (Montebelluna), Bono D. (Borgosesia, VC), Bottari A. (Firenze), Buscemi S. (Palermo), Calini G. (Bologna), Campagnacci R. (Jesi), Cantafio S. (Prato), Capolupo G.T. (Roma), Capuano M. (Napoli), Carannante F. (Roma), Casati M. (Carate Brianza, MB), Cassini D. (Legnano, MI), Castiglioni S. (Macerata), Cecconi C. (Piove di Sacco, PD), Cestino L. (Torino), Chetta N. (Acquaviva delle fonti, BA), Chiappetta F. M. (Ponte San Pietro, BG), Cinelli L. (Milano), Cojutti A. (Latisana, UD), Coletta D. (Pesaro), Corallino D. (Pesaro), Crepaz L. (Trento), Curcio S. (Catanzaro), Cuticone G. (Papardo, ME), D'Agostino F. (Cagliari), De Luca M. (Rovigo), De Palma G.D. (Napoli), De Stefano N. (Torino), De Rosa C. (Vercelli), De Serra A. (Cagliari), Del Giudice R. (Esine, BS), Di Franco G. (Pisa), Delrio P. (Napoli), Fedele S. (Castellana Grotte, BA), Foglio F. (Roma), Fontani G. (Firenze), Fortuna L. (Firenze), Fortunato M.R. (Aosta), Frazzini D. (Pescara), Furbetta N. (Pisa), Gambino E. (Savona), Garosio I. (Brescia), Germani P. (Trieste),, Ghazouani O. (Savona), Giannotti D. (Viterbo), Gibin E. (Torino), Gozzini L. (Milano), Grasso A. (L'Aquila), Grieco M. (Roma), Izzo D. (Napoli), Laracca G.G. (Roma), Lauteri G. (Roma), Lepiane P. (Civitavecchia), Li Causi F.S. (Roma), Locci E. (Cagliari), Madaro A. (Acquaviva delle fonti, BA), Madeddu F. (Iglesias, SU), Maggi F. (Roma), Maiello F. (Biella), Manigrasso M. (Napoli), Marcellinaro R. (Roma), Marinello P. (Bolzano), Mattei M.S. (Roma), Mazzarella G. (Roma), Moroni F. (Prato), Murgese A. (Torino), Muttillo E.M. (Roma), Oldani A. (Bergamo), Paicilli M. (Foggia), Palmieri M. (Ancona), Palomba G. (Napoli), Paolini G. (Firenze), Parini D. (Rovigo), Paroli G.M. (Bagno a Ripoli, FI), Pellicciaro M. (Roma), Petrucciani N. (Roma), Picardi B. (Roma), Piccolo R. (Latisana, UD), Pinotti E. (Ponte San Pietro, BG), Pisanu A. (Cagliari), Reddavid R. (Orbassano, TO), Reggio S. (Napoli), Resendiz A. (Orbassano, TO), Romano G. (Palermo), Rossi E.G. (Modena), Saracco R. (Napoli), Scaramuzzo R. (Civitavecchia), Scognamillo F. (Sassari), Serra F. (Modena), Sgotto E. (Torino), Solaini L. (Forlì), Spalluto M. (Legnano, MI), Taglietti L. (Esine, BS), Tartaglia E. (Napoli), Tartaglia N. (Foggia), Torre B. (Bologna), Tutino R. (Torino), Varesano M. (Andria), Vettoretto N. (Montichiari), Villamaina E. (Frattamaggiore, NA), Viora T. (Torino), Yusef M. (Roma), Zago M. (Borgosesia, VC), Zerbinati A. (Piove di Sacco, PD)
Author contributions
RC, GA, AC, MC conceived the study; GA, AC, MC, GR, SM, SP designed and performed the research; JR, RC analyzed the data; RC, GA, AC wrote the paper; RC, GA, AC, MC, AA, DC reviewed and supervised the paper; all authors read and approved the final manuscript.
Funding
Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement. The authors have not received any funding.
Data availability
The dataset generated and/or generated during the current study is not publicly available due to the principle of confidentiality.
Declarations
Conflict of interest
Gabriele Anania, Alberto Campagnaro, Matteo Chiozza, Justus Randolph; Giuseppe Resta; Serafino Marino; Sabrina Pedon, Antonino Agrusa, Diego Cuccurullo and Roberto Cirocchi have no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration and its later amendments.
Research involving human participants and/or animals
This study does not contain any studies performed with animals.
Informed consent
Informed consent was obtained from the patients before the surgical procedure.
Consent for publication
All the authors approved the publication of the manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Global Cancer Observatory: Graph production, Globocan (2020) [Online]. Available: https://gco.iarc.fr
- 2.Wang Y, Yang L, Zhou M, Shen L, Zhang J, Deng W, et al. Disparities in survival for right-sided vs. left-sided colon cancers in young patients: a study based on the surveillance, epidemiology, and end results database (1990–2014) Cancer Manag Res. 2018;10:1735–1747. doi: 10.2147/CMAR.S163302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tadros M, Mago S, Miller D, Ungemack JA, Anderson JC, Swede H. The rise of proximal colorectal cancer: a trend analysis of subsite specific primary colorectal cancer in the SEER database. Ann Gastroenterol. 2021;34(4):559–567. doi: 10.20524/aog.2021.0608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arezzo A, Passera R, Ferri V, Gonella F, Cirocchi R, Morino M. Laparoscopic right colectomy reduces short-term mortality and morbidity. Results of a systematic review and meta-analysis. Int J Colorectal Dis. 2015;30(11):1457–72. doi: 10.1007/s00384-015-2304-9. [DOI] [PubMed] [Google Scholar]
- 5.Bosker RJI, Van'tRiet E, de Noo M, Vermaas M, Karsten TM, Pierie JP. Minimally invasive versus open approach for right-sided colectomy: a study in 12,006 patients from the Dutch surgical colorectal audit. Dig Surg. 2019;36(1):27–32. doi: 10.1159/000486400. [DOI] [PubMed] [Google Scholar]
- 6.Zarnescu EC, Zarnescu NO, Sanda N, Costea R. Risk factors for severe postoperative complications after oncologic right colectomy: unicenter analysis. Medicina (Kaunas) 2022;58(11):1598. doi: 10.3390/medicina58111598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Society of Coloproctology Collaborating Group Predictors for anastomotic leak, postoperative complications, and mortality after right colectomy for cancer: results from an international snapshot audit. Dis Colon Rectum. 2020;63(5):606–618. doi: 10.1097/DCR.0000000000001590. [DOI] [PubMed] [Google Scholar]
- 8.Cuk P, Simonsen RM, Sherzai S, Buchbjerg T, Andersen PV, Salomon S, et al. Surgical efficacy and learning curves of laparoscopic complete mesocolic excision with intracorporeal anastomosis for right-sided colon cancer: a retrospective two-center cohort study. J Surg Oncol. 2023;127(7):1152–1159. doi: 10.1002/jso.27230. [DOI] [PubMed] [Google Scholar]
- 9.Giani A, Veronesi V, Bertoglio CL, Mazzola M, Bernasconi DP, Grimaldi S, et al. Multidimensional evaluation of the learning curve for laparoscopic complete mesocolic excision for right colon cancer: a risk-adjusted cumulative summation analysis. Colorectal Dis. 2022;24(5):577–586. doi: 10.1111/codi.16075. [DOI] [PubMed] [Google Scholar]
- 10.Grüter AAJ, Coblijn UK, Toorenvliet BR, Tanis PJ, Tuynman JB (2023) Right collaborators Group. National implementation of an optimal standardised technique for right-sided colon cancer: protocol of an interventional sequential cohort study (Right study). Tech Coloproctol 27(11):1083–1090. 10.1007/s10151-023-02801-6 [DOI] [PMC free article] [PubMed]
- 11.Strey CW, Wullstein C, Adamina M, Agha A, Aselmann H, Becker T, et al. Laparoscopic right hemicolectomy with CME: standardization using the "critical view" concept. Surg Endosc. 2018;32(12):5021–5030. doi: 10.1007/s00464-018-6267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Taher M, Okamoto N, Mutter D, Stassen LPS, Marescaux J, Diana M, Dallemagne B. International survey among surgeons on laparoscopic right hemicolectomy: the gap between guidelines and reality. Surg Endosc. 2022;36(8):5840–5853. doi: 10.1007/s00464-022-09044-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alsabilah J, Kim WR, Kim NK. Vascular structures of the right colon: incidence and variations with their clinical implications. Scand J Surg. 2017;106(2):107–115. doi: 10.1177/1457496916650999. [DOI] [PubMed] [Google Scholar]
- 14.Smalbroek BP, Smits AB, Khan JS. Safe oncological and standardised ("SOS") right hemicolectomy for colon cancer. Tech Coloproctol. 2023;27(3):169–170. doi: 10.1007/s10151-022-02749-z. [DOI] [PubMed] [Google Scholar]
- 15.Kuzu MA, İsmail E, Çelik S, Şahin MF, Güner MA, Hohenberger W, et al. Variations in the vascular anatomy of the right colon and implications for right-sided colon surgery. Dis Colon Rectum. 2017;60(3):290–298. doi: 10.1097/DCR.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 16.Anania G, Chiozza M, Campagnaro A, Bagolini F, Resta G, Azzolina D, Silecchia G, Cirocchi R, Agrusa A, Cuccurullo D, Guerrieri M, et al. Laproscopic right hemicolectomy: a SICE (Società Italiana di Chirurgia Endoscopica e Nuove Tecnologie) network prospective study on the approach to right colon lymphadenectomy in Italy: is there a standard?—CoDIG2 (ColonDx Italian Group) Surg Endosc. 2023 doi: 10.1007/s00464-023-10607-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yada H, Sawai K, Taniguchi H, Hoshima M, Katoh M, Takahashi T. Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg. 1997;21(1):109–15. doi: 10.1007/s002689900202. [DOI] [PubMed] [Google Scholar]
- 18.Wasserstein RL, Schirm AL, Lazar NA (2019) Moving to a World Beyond “p < 0.05”. Am Stat 73(sup1): 1-19. 10.1080/00031305.2019.1583913
- 19.Efetov S, Jiang J, Liu Z, Tulina I, Kim V, Schegelski V, et al. Superior mesenteric vessel anatomy features differ in Russian and Chinese patients with right colon cancer: computed tomography-based study. Chin Med J (Engl) 2021;134(20):2495–2497. doi: 10.1097/CM9.0000000000001566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu C, Ye K, Wu Y, Chen Q, Xu J, Lin J, Kang W. Variations in right colic vascular anatomy observed during laparoscopic right colectomy. World J Surg Oncol. 2019;17(1):16. doi: 10.1186/s12957-019-1561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao Y, Lu JY, Xu L, Zhang GN. Clinical anatomy study of superior mesenteric vessels and its branches. Zhonghua Wai Ke Za Zhi. 2019;57(9):673–680. doi: 10.3760/cma.j.issn.0529-5815.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Lee SJ, Park SC, Kim MJ, Sohn DK, Oh JH. Vascular anatomy in laparoscopic colectomy for right colon cancer. Dis Colon Rectum. 2016;59(8):718–24. doi: 10.1097/DCR.0000000000000636. [DOI] [PubMed] [Google Scholar]
- 23.Nesgaard JM, Stimec BV, Bakka AO, Edwin B, Ignjatovic D, RCC study group Navigating the mesentery: a comparative pre- and per-operative visualization of the vascular anatomy. Colorectal Dis. 2015;17(9):810–8. doi: 10.1111/codi.13003. [DOI] [PubMed] [Google Scholar]
- 24.Tajima Y, Ishida H, Ohsawa T, Kumamoto K, Ishibashi K, Haga N, et al. Three-dimensional vascular anatomy relevant to oncologic resection of right colon cancer. Int Surg. 2011;96(4):300–4. doi: 10.9738/cc20.1. [DOI] [PubMed] [Google Scholar]
- 25.Ohsawa T (2010) Pattern of arterial branches crossing the superior mesenteric vein: its relevance to laparoscopic right hemicolectomy, SAGES, SAGES Abstract Archives. [Online]. Available: https://www.sages.org/meetings/annual-meeting/abstracts-archive/pattern-of-arterial-branches-crossing-the-superior-mesenteric-vein-its-relevance-to-laparoscopic-right-hemicolectomy/
- 26.Peters JH, Kronson JW, Katz M, DeMeester TR. Arterial anatomic considerations in colon interposition for esophageal replacement. Arch Surg. 1995;130(8):858–62. doi: 10.1001/archsurg.1995.01430080060009. [DOI] [PubMed] [Google Scholar]
- 27.Cirocchi R, Randolph J, Davies RJ, Cheruiyot I, Gioia S, Henry BM, Carlini L, Donini A, Anania G. A systematic review and meta-analysis of variants of the branches of the superior mesenteric artery: the Achilles heel of right hemicolectomy with complete mesocolic excision? Colorectal Dis. 2021;23(11):2834–2845. doi: 10.1111/codi.15861. [DOI] [PubMed] [Google Scholar]
- 28.Murono K, Kawai K, Ishihara S, Otani K, Yasuda K, Nishikawa T, et al. Evaluation of the vascular anatomy of the right-sided colon using three-dimensional computed tomography angiography: a single-center study of 536 patients and a review of the literature. Int J Colorectal Dis. 2016;31(9):1633–8. doi: 10.1007/s00384-016-2627-1. [DOI] [PubMed] [Google Scholar]
- 29.Haywood M, Molyneux C, Mahadevan V, Srinivasaiah N. Right colic artery anatomy: a systematic review of cadaveric studies. Tech Coloproctol. 2017;21(12):937–943. doi: 10.1007/s10151-017-1717-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Surgical anatomy of the superior mesenteric vessels related to colon and pancreatic surgery: a systematic review and meta-analysis. Sci Rep. 2018;8(1):4184. doi: 10.1038/s41598-018-22641-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005;242(1):83–91. doi: 10.1097/01.sla.0000167857.14690.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bakula B. Is non-mentored initiation of laparoscopic colorectal surgery safe? Single surgeon initial experience with the first 40 cases. Front Surg. 2023;10:1196037. doi: 10.3389/fsurg.2023.1196037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luzon JA, Andersen BT, Stimec BV, Fasel JHD, Bakka AO, Kazaryan AM, et al. Implementation of 3D printed superior mesenteric vascular models for surgical planning and/or navigation in right colectomy with extended D3 mesenterectomy: comparison of virtual and physical models to the anatomy found at surgery. Surg Endosc. 2019;33(2):567–575. doi: 10.1007/s00464-018-6332-8. [DOI] [PubMed] [Google Scholar]
- 34.Chen Y, Bian L, Zhou H, Wu D, Xu J, Gu C, et al. Usefulness of three-dimensional printing of superior mesenteric vessels in right hemicolon cancer surgery. Sci Rep. 2020;10(1):11660. doi: 10.1038/s41598-020-68578-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Barros N, Rodrigues CJ, Rodrigues AJ, Jr, de NegriGermano MA, Cerri GG. The value of teaching sectional anatomy to improve CT scan interpretation. Clin Anat. 2001;14(1):36–41. doi: 10.1002/1098-2353(200101)14:1<36::AID-CA1006>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 36.Fletcher J, Ilangovan R, Hanna G, Miskovic D, Lung P. The impact of three-dimensional reconstruction and standardised CT interpretation (AMIGO) on the anatomical understanding of mesenteric vascular anatomy for planning complete mesocolic excision surgery: a randomised crossover study. Colorectal Dis. 2022;24(4):388–400. doi: 10.1111/codi.16041. [DOI] [PubMed] [Google Scholar]
- 37.Priyadharshini NA, Dinesh KV, Rajprasath R, Rema D. Relevance of learning anatomy to clinical practice: perceptive of medical students, interns, and clinicians. Natl J Clin Anat. 2019;8(1):32–37. doi: 10.1055/s-0039-1688893. [DOI] [Google Scholar]
- 38.Selcuk İ, Tatar I, Huri E. Cadaveric anatomy and dissection in surgical training. Turk J Obstet Gynecol. 2019;16(1):72–75. doi: 10.4274/tjod.galenos.2018.15931. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and/or generated during the current study is not publicly available due to the principle of confidentiality.


