Abstract
Bisphosphonates are effective for the treatment of osteoporosis despite recent reports of safety concerns such as atypical femur fracture. We conducted an ecological analysis of relevant media reports, oral bisphosphonate use, and fracture outcomes in the United States. Trends in media reports and public interest of bisphosphonates were quantified using data from Google Trends. Data from the Medical Expenditure Panel Survey (MEPS) and the National Inpatient Sample (NIS) were used to estimate the trends in oral bisphosphonate use among patients aged 55 years and older and hospitalizations for intertrochanteric and subtrochanteric fractures, respectively. These trends in the prevalence of oral bisphosphonate use and the age-adjusted incidence rate of intertrochanteric and subtrochanteric fractures were examined from 1996 to 2012. A series of spikes in Internet search activity for alendronate (Fosamax) occurred between 2006 and 2010 immediately following media reports of safety concerns. Oral bisphosphonate use declined by greater than 50% between 2008 and 2012 (p < 0.001) after increasing use for more than a decade. The decline was more common in patients with lower education levels. Intertrochanteric hip fractures declined from 1996 through 2006 (p < 0.001) and continued to decline from 2008 to 2012 (p < 0.05). Subtrochanteric and diaphyseal fractures showed a steady and significant increase from 2002 to 2011 (p < 0.05). However, the incidence decreased from a peak of 30.5 per 100,000 in 2011 to 26.7 per 100,000 in 2012. The plateauing and subsequent decline in oral bisphosphonate use since 2006 coincided with reports of safety concerns of bisphosphonates, despite the fact that U.S. Food and Drug Administration (FDA) and American Society of Bone and Mineral Research (ASBMR) reports did not recommend any safety restrictions on their use. This decline in oral bisphosphonate use was followed by the decline in the incidence of subtrochanteric and diaphyseal fractures.
Keywords: OSTEOPOROSIS, FRACTURE PREVENTION, ANTIRESORPTIVES, GENERAL POPULATION STUDIES, EPIDEMIOLOGY, BISPHOSPHONATE
Introduction
Fosamax was the first bisphosphonate to be approved by the U.S. Food and Drug Administration (FDA) for postmenopausal osteoporosis. It is currently FDA-approved for the treatment and prevention of postmenopausal osteoporosis, osteoporosis in men, glucocorticoid-induced osteoporosis, and Paget’s disease of the bone. More than 50% of patients who have sustained a fracture of the hip are institutionalized and up to 20% die within 1 year of injury.(1) Incidence and mortality from hip fractures declined from 1995 to 2005, corresponding to the period after Fosamax was first approved.(2) Bisphosphonate use is widespread and as many as one in seven postmenopausal women in the United States have been treated with a bisphosphonate at some time.(3)
However, several reports of adverse effects from bisphosphonates have surfaced since their approval, including atypical fracture of the femur, osteonecrosis of the jaw, and esophageal cancer.(4–7) These safety concerns prompted the FDA to perform a systematic review of long-term bisphosphonate safety and efficacy in 2012. The meeting culminated in a recommendation that bisphosphonate labeling be updated—“The optimal duration of use has not been determined. All patients on bisphosphonate therapy should have the need for continued therapy re-evaluated on a periodic basis”—although there was consensus that the data did not support a regulatory restriction on the duration of drug use.(8)
Associations of increase in subtrochanteric fractures with increase in oral bisphosphonate use and adherence have been reported in our previous studies.(9,10) A recent study suggested bisphosphonate use declined from 2007 to 2012.(11) We hypothesized that recent reports of safety concerns may have had an impact on bisphosphonate prescription prevalence. To test this, we studied the trends in bisphosphonate use from 1996 to 2012 and attempted to temporally correlate these trends with reports regarding safety concerns in both popular and scientific media.
Materials and Methods
Data sources and samples
In order to study the frequency of Internet searches, data from Google Trends for brand names and generic names for bisphosphonates were examined in a method similar to Skeldon and colleagues.(12) Google Trends reports relative search activity for specified search terms from January 2004 to the present. Data before 2004 are not available through Google Trends. In 2009 and 2010, approximately 65% of all United States Internet searches were through Google.(13) Data from Google Trends are normalized and scaled from 0 to 100 with the highest week of search activity given a value of 100. We searched brand and generic names of bisphosphonates and found Fosamax to be the most searched term consistently from 2004 to 2015. Results were scaled to the highest week of activity (week of March 7, 2010). News articles regarding Fosamax and bisphosphonates correlating to the dates of major spikes in search frequency were identified.
The Medical Expenditure Panel Survey (MEPS) is an annual survey of families and individuals, their medical providers, and their employers across the United States.(14) It has a main household component (HC) that collects nationally representative data from a subsample of households that participated in the prior year’s National Health Interview Survey conducted by the National Center for Health Statistics. The MEPS uses both household interviews and pharmacy surveys for its prescribed medicine files. It contains information about respondents’ demographic characteristics, health conditions, health status, access to care, insurance status, and prescription drug use. MEPS is conducted as a national probability survey using a complex stratified multistage area probability design with certain groups (including racial minorities and low-income households) being oversampled. Weights provided in the MEPS pooled-estimation file allow researchers to calculate national estimates of prescription drug use. We used the database to study national utilization of medications used for osteoporosis, such as oral bisphosphonates, selective estrogen receptor modulators, denosumab, and teriparatide. We calculated the proportion of patients with at least one prescription for bisphosphonate in annual surveys from 1996 to 2012 among responders aged 55 years and older.
The National (Nationwide) Inpatient Sample (NIS) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).(15) The NIS is the largest publicly available all-payer inpatient health care database in the United States, yielding statistically valid national estimates of hospital inpatient stays. Beginning with 2012 data, the NIS was redesigned to improve national estimates. It is now a sample of discharge records from all HCUP-participating hospitals rather than a sample of hospitals from which all discharges were retained. Around 8 million hospital stays were sampled each year, and weighted according to the sampling scheme to represent a total of approximate 36 million hospitalizations nationally. The database contains clinical and nonclinical data elements for each hospital stay including primary and secondary diagnoses and procedures, patient demographic characteristics, hospital characteristics, expected payment source, total charges, discharge status, total length of stay, and severity and comorbidity measures.
Outcome measures
Hip fractures require hospitalizations and were captured in the NIS data with the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes. We excluded open hip fractures because they are more commonly a result of high-energy trauma. After exclusion of open hip fractures, closed hip fractures constitute more than 99.5% of all hospitalizations for hip fractures and are likely to be osteoporotic in nature. We defined closed intertrochanteric fractures (ICD-9-CM: 820.00, 820.01, 820.02, 820.03, 820.09, 820.21, and 820.8), subtrochanteric (ICD-9-CM: 820.22), and diaphyseal (ICD-9-CM: 821.01) fractures.
Furthermore, we limited the records to those with a concurrent primary ICD-9-CM procedure code for primary surgical treatment (7855, 7905, 7915, 7925, 7935, 7945, 7955, 7965, 7975, 7985, and 7995) or replacement (0074, 0075, 0076, 0077, 0085, 0086, 0087, 8151, 8152, and 8169). In this way, we captured over 90% of original records and estimated incidences of hip fractures and excluded discharges for follow-up visits, procedures for periprosthetic fractures, and revision procedures. We abstracted data on annual discharge records pertaining to specific types of hip fractures for patients aged 55 years and older, excluding those with missing data on gender (<0.01%).
As a sensitivity analysis, we studied the incidence of “non-hip” major osteoporotic fractures of the distal radius and proximal humerus that required hospitalization among adults aged 55 years and older. We defined proximal humerus fractures (ICD-9-CM: 812.00, 812.01, 812.02, 812.03, and 812.09) and distal radius fracture (ICD-9-CM: 813.40, 813.41, 813.42, 813.43, and 813.44). We then limited records to those with a concurrent primary ICD-9-CM procedure code for primary surgical treatment (79.01, 79.11, 79.21, and 79.91 for proximal humerus fracture; 79.02, 79.12, 79.22, and 79.92 for distal radius fracture).
Data analysis
To calculate annual hospitalization rates, we used weighted frequencies of hip fractures as the numerator and annual, mid-year census population estimates for the older adult population (55 years and over) as the denominator. Trends in hip fracture rates were stratified by gender and adjusted to the 2000 population in 5-year age groups (55–59, 60–64, 65–69, 70–74, 75–79, 80–84, and 85+ years old). Standard errors were calculated along with age standardization.(16)
We used SAS 9.3 (SAS Institute, Inc., Cary, NC, USA). All estimates of fracture rate and medication use took into consideration the stratified survey design of both NIS and MEPS. To compare national estimates and demographics, Z test and chi-square tests were used, respectively. Statistical tests were performed at a two-sided significance level ≤0.05. Changes in adjusted rates or proportions were normalized by the differences between the minimum and maximum values for these annual estimates, respectively.
The study was exempted by the Institutional Review Board at National Institutes of Health (NIH) because the database used is publicly available and contained only deidentified information. The Agency for Healthcare Research and Quality (AHRQ) granted the use of MEPS database.
Results
Frequency of “Fosamax” as a search term
A study of relative search activity of different term equivalents for bisphosphonates revealed “Fosamax” to be by far the most used search term. The frequency of Fosamax as an Internet search term from January 2004 to January 2015 showed a series of spikes from 2006 to 2010 mirroring media reports of safety concerns (Fig. 1). The first prominent spike was noted in 2006 when the first lawsuit was filed against Merck and Co. Inc. for osteonecrosis of the jaw. The second spike was seen in 2008 after a study published in the Archives of Internal Medicine showed an increased risk of atrial fibrillation with use of alendronate.(17) A small spike is seen in 2010 when jury deliberations began for the first Fosamax trial.
Fig. 1.
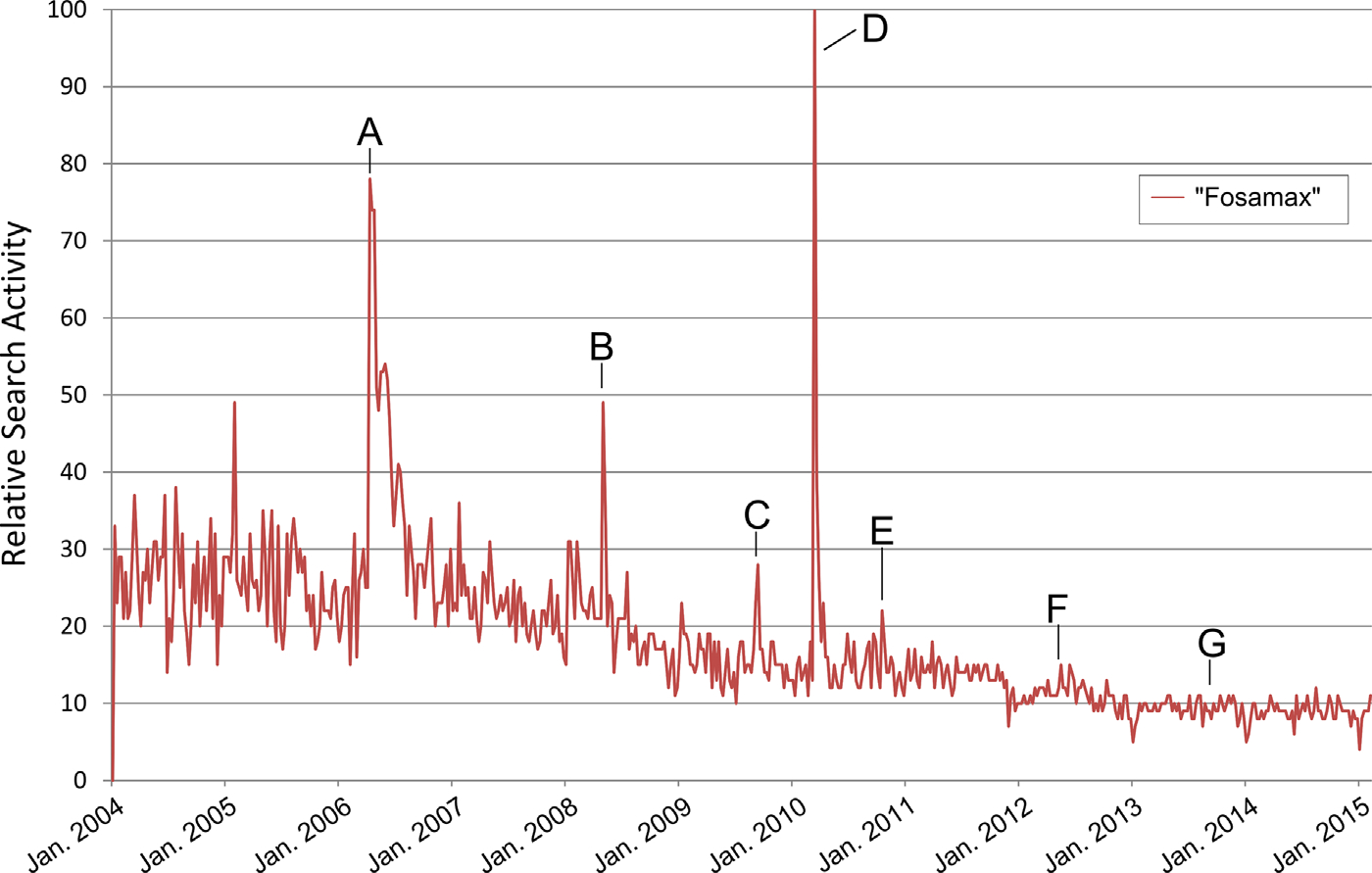
U.S. Google search activity for the term “Fosamax” from January 2004 to January 2015. Search activity is relative to the highest peak which is given a value of 100. Labeled events: A = Lawsuit filed against Merck for Fosamax causing osteonecrosis of the jaw. B = Study in Archives of Internal Medicine published associating Fosamax with atrial fibrillation. C = Jury deliberations start for first Fosamax trial. D = ABC World News runs feature segment on Fosamax and atypical femoral fractures. E = First ASBMR task force report on atypical femoral fractures published. F = FDA Advisory Committee findings on bisphosphonates and fracture risk published in New England Journal of Medicine. G = Second ASBMR task force report on atypical femoral fractures published. Data source: Google Trends (www.google.com/trends).
A sharp increase in use of Fosamax as a search term occurred in 2010 when ABC World News aired a segment on Fosamax and atypical femur fractures. This broadcast was based on findings of two studies which was to be presented at the upcoming American Academy of Orthopaedic Surgeons (AAOS) conference.(18,19) Three much smaller spikes occurred in 2011, 2012, and 2014, coinciding with publications of the first American Society for Bone and Mineral Research (ASBMR) Task Force Report, recommendations of the FDA Advisory Committee, and the second ASBMR Task Force Report, respectively.(8,20,21) The spikes in Internet activity seen from the lay press were four times higher than the spikes generated from scientific consensus reports.
Medication use
The prevalence of oral bisphosphonate use among women older than age 55 years increased from 2.7% in 1996 to nearly three times at 7.8% in 2001 (Fig. 2). Prevalence plateaued in 2005 at 15.1% and stayed in that range until 2008 at 15.8%. However, the prevalence of oral bisphosphonate use showed a steady decline since 2008 to a low of 7.3% in 2012; nearly the same as in 2001. Among males, the trend parallels the pattern among females. Prevalence of oral bisphosphonate use among males increased from 0.1% in 1996 to 0.9% in 2001. Thereafter, it increased to 1.5% in 2005, peaking at 1.9% in 2010 and declining to 0.8% in 2012.
Fig. 2.
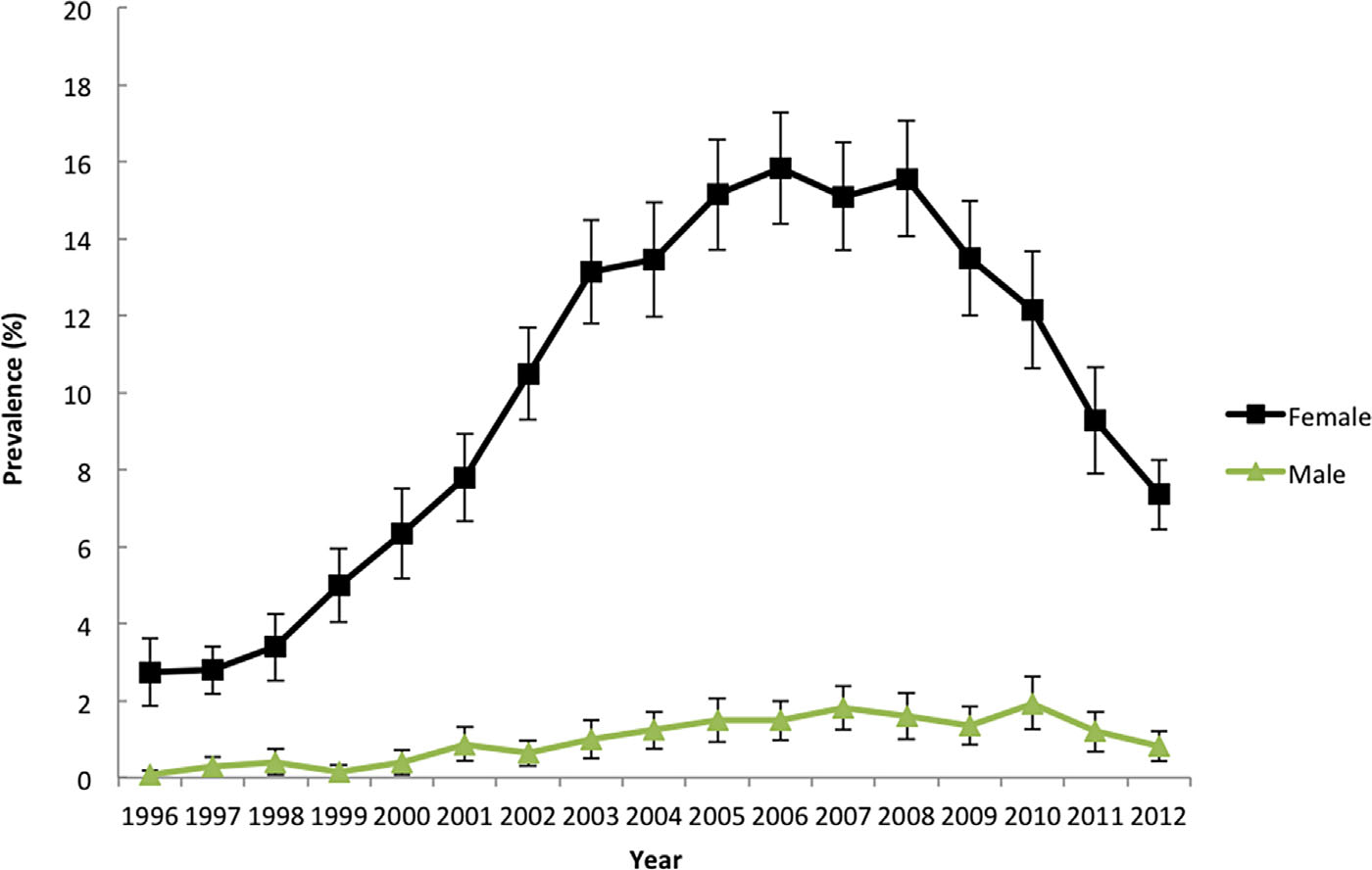
Prevalence of bisphosphonate use among females and males aged 55 years and older from 1996 to 2012. Data source: Medical Expenditure Panel Survey (MEPS).
Demographic data showed that certain subpopulations experienced a shift in oral bisphosphonate use (Table 1 Q4). The decline in the prevalence of oral bisphosphonate use was predominantly seen among white women (86.4% in 2008 down to 78.1% in 2012; p < 0.009). Twice as many Asian women are using oral bisphosphonates in 2012 (7.2%) as compared to 2008 (3.5%). The prevalence of oral bisphosphonate use also seems to have increased among Hispanic and black women. Women with education levels less than high school showed a significant decline in oral bisphosphonate use (15.3% in 2008 down to 11.8% in 2012; p < 0.01) in contrast to women with college education. The decrease in oral bisphosphonate use is also significant in the rural population (17.2% in 2005 to 12.6% in 2008; p < 0.03) as compared to the urban population. No significant difference in trends through the time points was noted among responders based on age, gender, marital status, smoking status, region, employment status, or subjects with a primary care physician.
Table 1.
Demographic Characteristics of Subjects Who Used Bisphosphonates
| Variable | 2001 (%) | 2005 (%) | p | 2008 (%) | p | 2012 (%) | p |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age (years) | |||||||
| 55–64 | 21.8 | 28.2 | 0.17 | 25.6 | 0.32 | 26.4 | 0.24 |
| 65–74 | 37.5 | 32.4 | 30.1 | 36.1 | |||
| 75+ | 40.8 | 39.4 | 44.3 | 37.5 | |||
| Gender | |||||||
| Female | 92.4 | 92.8 | 0.85 | 92.5 | 0.86 | 91.7 | 0.72 |
| Male | 7.6 | 7.2 | 7.5 | 8.3 | |||
| Race/ethnicity | |||||||
| White | 89.2 | 88.4 | 0.73 | 86.4 | 0.77 | 78.1 | 0.009* |
| Black | 3.1 | 2.2 | 2.4 | 3.8 | |||
| Hispanic | 4.3 | 4.8 | 6.3 | 9.4 | |||
| Asian | 2.9 | 3.5 | 3.5 | 7.2 | |||
| Other | 0.5 | 1.1 | 1.4 | 1.5 | |||
| Marital status | |||||||
| No | 50.6 | 48.5 | 0.69 | 48.7 | 0.96 | 46.6 | 0.61 |
| Yes | 49.4 | 51.5 | 51.3 | 53.4 | |||
| Current smoker | |||||||
| Yes | 8.8 | 9.7 | 0.69 | 7.1 | 0.13 | 7.4 | 0.88 |
| No | 91.2 | 90.3 | 92.9 | 92.6 | |||
| Education level | |||||||
| Less than high school | 23.5 | 18.6 | 0.29 | 15.3 | 0.32 | 11.8 | 0.01* |
| High school | 34.0 | 35.5 | 37.6 | 27.5 | |||
| College | 42.5 | 46.0 | 47.1 | 60.7 | |||
| Poverty line | |||||||
| Poor | 9.5 | 7.1 | 0.04* | 6.6 | 0.11 | 9.9 | 0.27 |
| Near poor | 5.9 | 4.3 | 7.0 | 5.8 | |||
| Low income | 14.4 | 11.6 | 15.2 | 13.5 | |||
| Middle income | 35.4 | 30.6 | 30.5 | 24.7 | |||
| High income | 34.9 | 46.4 | 40.7 | 46.2 | |||
| Employment status | |||||||
| No | 77.0 | 70.3 | 0.06 | 68.6 | 0.59 | 74.8 | 0.17 |
| Yes | 23.0 | 29.7 | 31.5 | 25.2 | |||
| Insurance status | |||||||
| Any private | 63.8 | 70.8 | 0.02* | 58.9 | 0.001* | 59.1 | 0.93 |
| Public only | 35.7 | 27.5 | 39.6 | 39.7 | |||
| Uninsured | 0.5 | 1.7 | 1.6 | 1.2 | |||
| Has primary care provider | |||||||
| Yes | 95.5 | 96.4 | 0.50 | 95.0 | 0.28 | 95.2 | 0.91 |
| No | 4.5 | 3.6 | 5.0 | 4.8 | |||
| MSA | |||||||
| Non-MSA | 19.6 | 17.2 | 0.54 | 12.6 | 0.03* | 13.2 | 0.86 |
| MSA | 80.4 | 82.8 | 87.4 | 86.8 | |||
| Region | |||||||
| Northeast | 20.9 | 21.9 | 0.96 | 23.4 | 0.05 | 18.3 | 0.17 |
| Midwest | 22.8 | 24.1 | 18.4 | 20.2 | |||
| South | 34.2 | 32.8 | 38.3 | 36.2 | |||
| West | 22.1 | 21.3 | 19.8 | 25.4 | |||
Year 2001 represents the initial phase of bisphosphonate use, 2008 represents the year of peak use, and 2012 represents the decline in use. Source: Medical Expenditure Panel Survey. MSA = Metropolitan Statistical Area
Statistically significant.
We also studied the use of alternate osteoporotic drugs such as estrogen, teriparatide, denosumab, and calcitonin for the year 2011 to see if these medications accounted for an increasing share of antiosteoporotic therapy. We found that bisphosphonates continue to be the most commonly prescribed medication in spite of the noted decrease in use in recent years.
Effect on age-adjusted hip fracture rates
The hospitalization rate of intertrochanteric hip fracture declined from 478.9 per 100,000 (95% CI, 477.0 to 480.7) in 1996 to 355.3 per 100,000 (95% CI, 353.9 to 356.7) in 2006, decreasing further to 305.8 per 100,000 (95% CI, 304.5 to 307.0) in 2012 (Fig. 3). Among women, the hospitalization rates of intertrochanteric hip fracture decreased from 653.7 per 100,000 (95% CI, 650.8 to 656.6) in 1996 to 476.9 per 100,000 (95% CI, 474.6 to 479.1) in 2006, showing a further decrease to 412.3 per 100, 000 (95% CI, 410.4 to 414.4) in 2012. The hospitalization rate of intertrochanteric hip fracture among men was 253.7 per 100,000 (95% CI, 251.6 to 255.7) in 1996, which decreased to 205.9 per 100,000 (95% CI, 204.3 to 207.5) in 2006 then decreased further to 181.0 per 100,000 (95% CI, 179.6 to 182.4) in 2012.
Fig. 3.
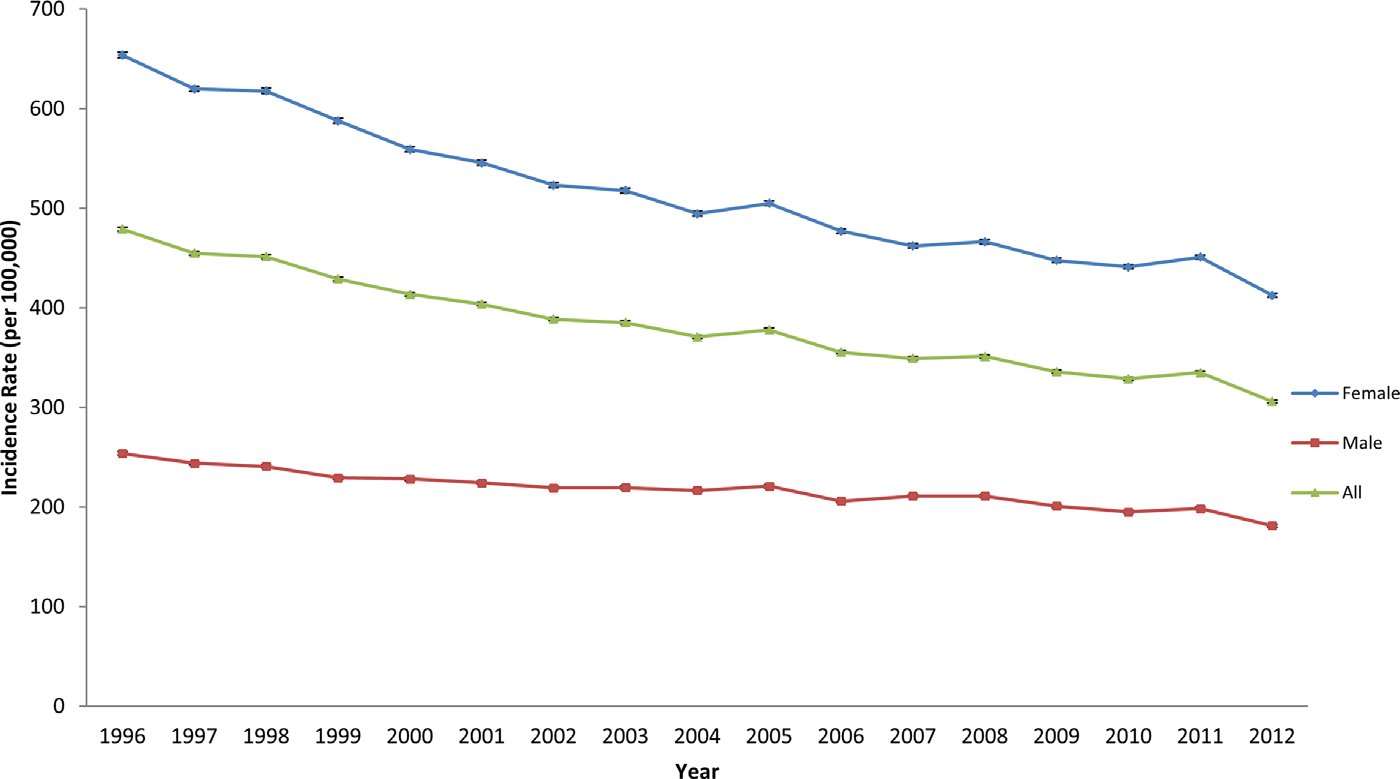
National estimates of intertrochanteric fractures from 1996 to 2012 in patients aged 55 years and older. Source: National Inpatient Sample (NIS). Error bars indicate 95% CI.
The overall incidence of subtrochanteric and diaphyseal fractures was 25.6 per 100,000 (95% CI, 25.2 to 26.0) in 1996 and increased to a maximum of 30.5 per 100,000 (95% CI, 30.1 to 30.9) in 2011, but decreased to 26.7 per 100,000 (95% CI, 26.3 to 27.0) in 2012 (Fig. 4). Among females, the hospitalization rate for subtrochanteric and diaphyseal fractures was 33.9 per 100,000 (95% CI, 33.2 to 34.5) in 1996, increasing to a peak of 43.4 per 100,000 (95% CI, 42.8 to 44.1) in 2011. It decreased thereafter to 37.9 per 100,000 (95% CI, 37.3 to 38.5) in 2012. The hospitalization rate for subtrochanteric and diaphyseal fractures among men increased from 14.9 per 100,000 (95% CI, 14.4 to 15.4) in 1996 to 16.9 per 100,000 (95% CI, 16.5 to 17.3) in 2010. It decreased thereafter to 13.6 per 100,000 (95% CI, 13.2 to 14.0) in 2012.
Fig. 4.
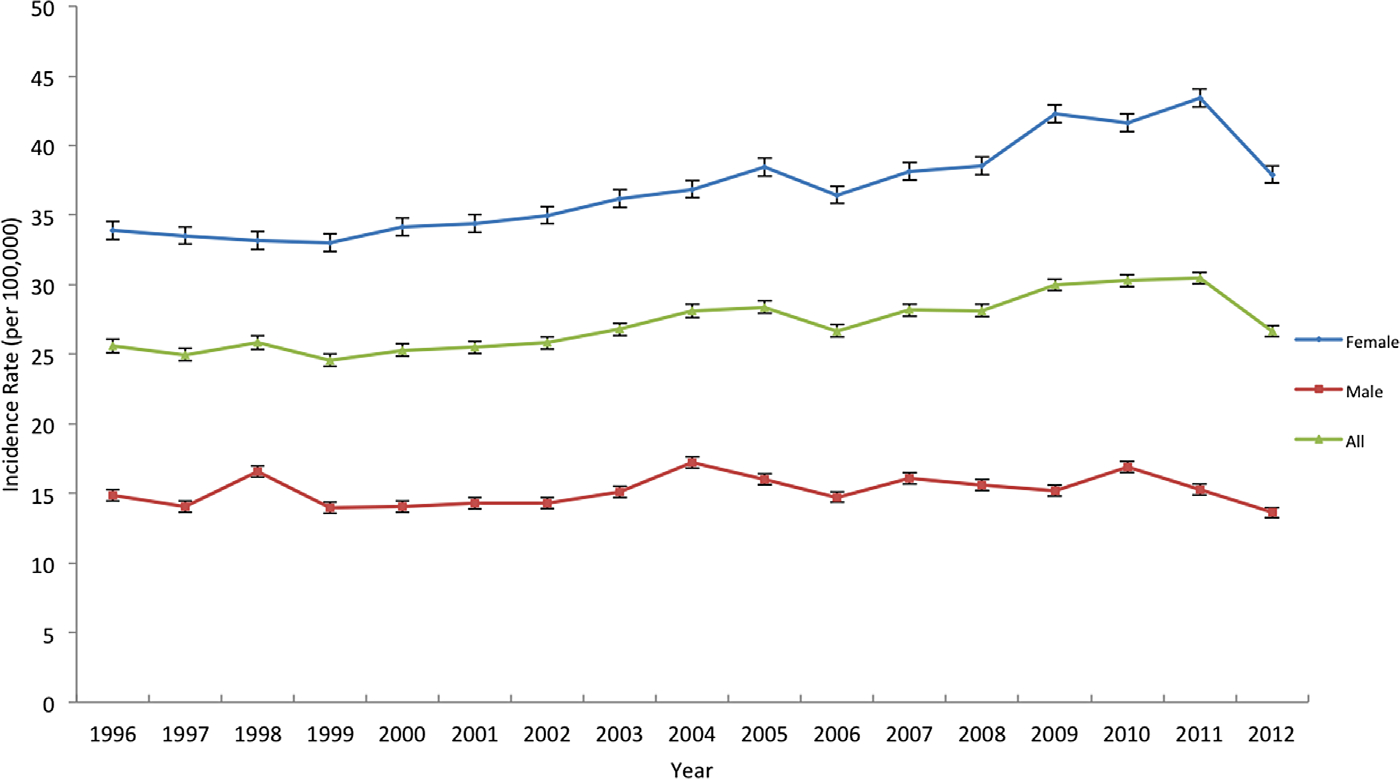
National estimates of subtrochanteric fractures from 1996 to 2012 in patients aged 55 years and older. Source: National Inpatient Sample (NIS). Error bars indicate 95% CI.
The incidence of hospitalization for “non-hip” major osteoporotic fractures of the distal radius and proximal humerus among subjects aged 55 years and older was also studied for comparison. Our results show a decline toward less inpatient treatment of these fractures, suggesting a possible decline in osteoporotic fractures overall (Supporting Fig. 1). Importantly, no rise of distal radius or proximal humerus fractures was seen, unlike that of subtrochanteric femur fractures.
The normalized rate of increase in subtrochanteric fractures seems to parallel that of the increase in bisphosphonate prescriptions, albeit with a delay (Fig. 5). The significant drop in subtrochanteric fractures from 2011 to 2012 was more precipitous than the gradual decrease in bisphosphonate use. This may be explained by the 70% decrease in risk of atypical femur fracture per year since the last use after drug withdrawal.(4)
Fig. 5.

Percentage normalized changes of bisphosphonate prescription and subtrochanteric and diaphyseal fractures. BIS = bisphosphonate; FX = fractures.
Discussion
Our study shows that oral bisphosphonate use increased for over a decade then declined significantly between 2008 and 2012, which follows media reports of safety concerns. This finding highlights an important change in patient behavior as being “active” consumers of the drug market. Osteoporosis is a public health concern. Thirty percent of all postmenopausal women have osteoporosis in the United States and in Europe.(22) The aging population is expected to cause a major increase in the incidence of osteoporosis worldwide. Despite the availability of guidelines for its diagnosis and treatment, osteoporosis remains undertreated, with consequent fragility fractures even in patients with a prior history of fragility fracture.(23) Hip fracture is largely used as a proxy for the incidence of osteoporosis and the decrease in the incidence of intertrochanteric hip fractures because the availability of bisphosphonates is believed to be proof of their efficacy. However, one must remember that multiple other factors could have contributed to the decline in hip fractures—increase in the average number of reproductive years and exposure to endogenous hormones in females, improvements in calcium and vitamin D intake, physical activity, fall prevention, decline in smoking, and the obesity epidemic.(24,25)
Although several reports of adverse effects related to bisphosphonates have surfaced since their approval about two decades ago, these events are very rare.(26) Neither the FDA nor the ASBMR consensus committee recommends any safety restrictions on the use of bisphosphonates. Despite the rarity of adverse outcomes and the lack safety restrictions, our findings showed a decline in the use of oral bisphosphonates by as much as 50% from 2008 to 2012.
This study documents an interesting interaction between patient behavior and popular media in comparison to scientific publications. It appears that media reports have much more impact than journal reports. A recent shift in the ways in which patients consume health information, with more patients looking for information online before speaking to their physicians, has been documented.(27) Although research goes through a rigorous process of peer-review before it is published in scientific literature, which could take months, popular media is exempted from such review and typically operates on a weekly to daily cycle. It has been shown that news media stories about medications may include inadequate or incomplete information about the benefits, risks, and costs of the drug, as well as financial ties between study groups or experts and pharmaceutical manufacturers.(28,29) Marketing by big pharmaceutical industries (eg, in this case by makers of alternate antiosteoporotic therapy) may segment the population at risk. However, popular media also has its own benefits; for example, in the case of breast cancer, a two-way concurrent relationship between breast cancer funding and media coverage has been shown. The study also showed a two-way concurrent relationship between breast cancer incidence and TV coverage.(30)
Although our data are limited to the use of oral bisphosphonates, we know that the use of intravenous bisphosphonates also shows a trend toward decreasing use.(11) One should not ignore the fact that many bone experts had expressed concern about the unlimited use of bisphosphonate and recommended a “drug holiday” even prior to the FDA recommendations or the media coverage. It is suggested that relatively better bone mineral density may be a risk for atypical femur fractures and, hence, bisphosphonates should be discontinued when bone mineral density is sufficiently improved in order to prevent adverse effects.(20)
The decline in bisphosphonate use may at least partially represent better targeting of therapy. In 2008, the World Health Organization (WHO) developed the Fracture Risk Assessment Tool (FRAX) to include non-bone mineral density (non-BMD) clinical risk factors into treatment decisions. FRAX helps calculate the 10-year probability of a hip fracture or a major osteoporosis-related fracture to help make treatment decisions in untreated patients. Based on FRAX, only patients with osteopenia who meet a certain cutoff (country-specific; based on cost-benefit ratio) for 10-year risk of a hip or a major osteoporotic fracture should be offered pharmaceutical intervention. According to the FRAX website, it appears that nearly 3.5 million U.S. whites with fracture risk have been assessed since June 1, 2011, providing credence to its wide use.
The decline in the prevalence of oral bisphosphonate use is skewed toward individuals with lower education levels. Patients with lower educational levels may not understand the intricacies of scientific studies and thus rely more on media reports. The decline in oral bisphosphonate use has been seen only among white women who still account for nearly 80% of the bisphosphonate users in 2012, despite the overall decline.
The decrease in oral bisphosphonate use did not alter the long continuing decline in the incidence of intertrochanteric fracture. Our findings show decreasing incidence of intertrochanteric hip fractures since the approval of Fosamax—declining by 26% between 1996 to 2006 and an additional 14% between 2006 and 2012. The continued decline in intertrochanteric fractures despite the decrease in the prevalence of bisphosphonate use may represent better targeting of bisphosphonate therapy with the availability of alternate treatment options and the advent of FRAX scores. Alternately, the long half-life of oral bisphosphonates may be associated with ongoing decline in the incidence of intertrochanteric fracture notwithstanding their discontinuation. It is also plausible that trends in other factors, particularly calcium and vitamin D repletion, could have contributed to this continued decline.
Our study further supports the association between bisphosphonate use and subtrochanteric fractures of the femur. Subtrochanteric fracture rates increased during the period of increasing bisphosphonate use and then decreased as bisphosphonate use became less prevalent. The incidence of subtrochanteric and diaphyseal fractures increased by 4% between 1996 and 2006; however, it decreased by 12% in 2012 from its peak incidence in 2011.
Fisher and colleagues(31) showed that in Australia the decline in the use of bisphosphonate in 2007 to 2008 compared to 2005 was associated with an increase in the incidence of hip fractures in women. The reason for this difference in findings is unclear but may be explained by longer periods of observation or differences in ecology.
Our study has strengths with its large sample, nationwide sampling, extended duration of observation, and high sensitivity. Both MEPS and NIS, with their large sample sizes, allowed us to estimate the rare incidence of subtrochanteric fractures. However, the study has certain limitations. First, MEPS and NIS may not represent the same segment of the U.S. population, so it may not be prudent to compare trends. Given the disparate nature of the three datasets, a formal interrupted time-series analysis is beyond the scope of the data and this work. Second, this is an ecological analysis and hence prone to the possibility of “ecological fallacy”—the declines and increases observed may be occurring, but have no actual relation to each other. Third, trends in lifestyle factors, such as physical activity, dietary modifications, and smoking cessation, or medical factors, such as adequacy of vitamin D stores in the body, were not studied, which could have contributed to these trends. Trends cannot account for physician-driven prescribing drug tendencies such as planned drug holidays and one cannot ascertain if this decrease in bisphosphonate use is largely accounted for by decrease in new users or discontinuation among previous users. Fourth, radiographs of the studied subtrochanteric fractures were not available to assess if these fractures had the characteristic radiographic “atypical” findings as defined by ASBMR. Furthermore, the sampling scheme of NIS has changed over time, which could affect data trends. According to the NIS website, a onetime decrease of about 4% to historical trends for discharge counts could be expected because of this redesign. Because this trend of decrease in subtrochanteric fracture is noted only in a single data point of 2012 thus far, the next few years will further our understanding of its association with bisphosphonate use. In addition, the use of such an inpatient search strategy limits our ability to include incomplete subtrochanteric fractures. One could speculate that with increased awareness of “atypical femur fractures” among providers and patients alike, we may be diagnosing more such fractures prior to completion now as compared to a few years ago, which could potentially explain the decrease in the hospitalization trend for subtrochanteric fracture. The data also do not account for heightened vigilance in case finding and accuracy reporting/coding that followed recognition of “atypical” femur fractures. Coding and reporting of such “atypical” femur fractures were clearly inaccurate when these fractures were first appreciated. Our data are also limited to the use of oral bisphosphonates alone, and we are unable to account for switching among different bisphosphonates, trends in the use of intravenous bisphosphonate, duration of use among responders, patient adherence, or characteristics of prescribing physicians. In addition, we lack information on the use of other concurrent drugs that may have contributed to such trends by drug-drug interactions. Additionally, MEPS is a self-reported survey and the indication for the prescription of bisphosphonate was not ascertained. It is plausible that the use of bisphosphonates for osteopenia (and not necessarily osteoporosis or other indications) has decreased much more dramatically than others.
Conclusion
A significant decrease in the use of oral bisphosphonates is noted from 1996 to 2012, which follows reports of safety concerns in popular media despite consensus reports documenting their safety in the scientific literature. As members of the scientific community, clearly we need to do better in disseminating and translating our message to the community at large. Continued decrease in the incidence of intertrochanteric fracture has been seen in spite of decreasing use of oral bisphosphonates, possibly due to long residence of bisphosphonates in bones, better targeting of therapy, and trends in vitamin D repletion, physical activity, etc. A decrease in the incidence of subtrochanteric fracture is also noted in the period, supporting the association between bisphosphonates and subtrochanteric fractures. Because this decrease is only noted in 2012, more longitudinal follow-up will help enhance our understanding of the association between bisphosphonate use and subtrochanteric fracture.
Supplementary Material
Acknowledgments
This research was supported by the Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health (NIH).
Footnotes
Disclosures
All authors state that they have no conflicts of interest.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Farley JF, Blalock SJ. Trends and determinants of prescription medication use for treatment of osteoporosis. Am J Health Syst Pharm. 2009;66(13):1191–201. [DOI] [PubMed] [Google Scholar]
- 2.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fracture in the United States. JAMA. 2009;302-(14):1573–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black DM, Bauer DC, Schwartz AV, Cummings SR, Rosen CJ. Continuing bisphosphonate treatment for osteoporosis—for whom and for how long? N Engl J Med. 2012;366(22):2051–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schilcher J, Michaelsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364-(18):1728–37. [DOI] [PubMed] [Google Scholar]
- 5.Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62(5):527–34. [DOI] [PubMed] [Google Scholar]
- 6.Wysowski DK. Reports of esophageal cancer with oral bisphosphonate use. N Engl J Med. 2009;360(1):89–90. [DOI] [PubMed] [Google Scholar]
- 7.Black DM, Delmas P, Eastell R, et al. HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of post-menopausal osteoporosis. N Engl J Med. 2007;356(18):1809–22. [DOI] [PubMed] [Google Scholar]
- 8.Whitaker M, Guo J, Kehoe T, Benson G. Bisphosphonates for osteoporosis—where do we go from here? N Engl J Med. 2012;366(22):2048–51. [DOI] [PubMed] [Google Scholar]
- 9.Wang Z, Ward MM, Chan L, Bhattacharyya T. Adherence to oral bisphosphonates and the risk of subtrochanteric and femoral shaft fractures among female Medicare beneficiaries. Osteoporos Int. 2014;25(8):2109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Z, Bhattacharyya T. Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996–2007. J Bone Miner Res. 2011;26(3):553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wysowski DK, Greene P. Trends in osteoporosis treatment with oral and intravenous bisphosphonates in the United States, 2002–2012. Bone. 2013;57(2):423–8. [DOI] [PubMed] [Google Scholar]
- 12.Skeldon SC, Kozhimannil KB, Majumdar SR, Law MR. The effect of competing direct-to-consumer advertising campaigns on the use of drugs for benign prostatic hyperplasia: time series analysis. J Gen Intern Med. 2015;30(4):514–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nielsen Company. Bing Overtakes Yahoo as The #2 U.S. Search Engine [Internet]. New York: Nielsen Company; 2010. Sep 14 [cited 2015 Jun 8]. Available from: http://www.nielsen.com/us/en/insights/news/2010/bing-overtakes-yahoo-as-the-2-search-engine.html. [Google Scholar]
- 14.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2015. [cited 2015 Jun]8. Available from: http://meps.ahrq.gov/mepsweb. [Google Scholar]
- 15.HCUP NIS Database Documentation. Healthcare Cost and Utilization Project (HCUP) [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2015. [updated 18th July, 2014; cited 2015 Jun 8]. Available from: http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp [Google Scholar]
- 16.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998. Oct 7;47(3):1–16, 20. [PubMed] [Google Scholar]
- 17.Heckbert SR, Cummings SR, Smith NL, Psaty BM. Use of alendronate and risk of incident atrial fibrillation in women. Arch Intern Med. 2008;168(8):826–31. [DOI] [PubMed] [Google Scholar]
- 18.ABC News. Osteoporosis Drugs, Like Fosamax May Increase Risk of Broken Bones in Some Women [Internet]. 2010. Mar 8 [cited 2015 Jun 8]. Available from: http://abcnews.go.com/WN/WorldNews/osteoporosis-drugs-fosamax-increase-risk-broken-bones-women/story?id=10044066. [Google Scholar]
- 19.Lane JM. Bisphosphonate use for ≥5 years increased risk for subtrochanteric or femoral shaft fractures. J Bone Joint Surg Am. 2011;93(16):1546. [DOI] [PubMed] [Google Scholar]
- 20.Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010;25(11):2267–94. [DOI] [PubMed] [Google Scholar]
- 21.Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29(1):1–23. [DOI] [PubMed] [Google Scholar]
- 22.Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. How many women have osteoporosis? JBMR Anniversary Classic. JBMR, Volume 7, Number 9, 1992. J Bone Miner Res. 2005;20(5):886–92. [DOI] [PubMed] [Google Scholar]
- 23.Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35(2):375–82. [DOI] [PubMed] [Google Scholar]
- 24.Leslie WD, O’Donnell S, Jean S, et al. Osteoporosis Surveillance Expert Working Group. Trends in hip fracture rates in Canada. JAMA. 2009;302(8):883–9. [DOI] [PubMed] [Google Scholar]
- 25.Jean S, O’Donnell S, Lagace C, et al. Osteoporosis Surveillance Expert Working Group. Trends in hip fracture rates in Canada: an age-period-cohort analysis. J Bone Miner Res. 2013;28(6):1283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McClung M, Harris ST, Miller PD, et al. Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med. 2013;126-(1):13–20. [DOI] [PubMed] [Google Scholar]
- 27.Hesse B, Nelson D, Kreps G, Croyle R, Arora N, Rimer B, et al. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165-(22):2618–24. [DOI] [PubMed] [Google Scholar]
- 28.Moynihan R, Bero L, Ross-Degnan D, et al. Coverage by the news media of the benefits and risks of medications. N Engl J Med. 2000. Jun 1;342(22): 1645–50. [DOI] [PubMed] [Google Scholar]
- 29.Korownyk C, Kolber MR, McCormack J, et al. Televised medical talk shows—what they recommend and the evidence to support their recommendations: a prospective observational study. BMJ. 2014. Dec 17;349:g7346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corbett J, Mori M. Medicine, media and celebrities: news coverage of breast cancer, 1960–1995. Journal Mass Commun Q. 1999;76(2):229–49. [Google Scholar]
- 31.Fisher A, Martin J, Srikusalanukul W, Davis M. Bisphosphonate use and hip fracture epidemiology: ecologic proof from the contrary. Clin Interv Aging 2010;5:355–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


