Anaphylaxis and anaphylactic death are becoming more common and particularly affect children and young adults. Anaphylaxis can be frightening to deal with because of its rapid onset and severity. Doctors in many fields, but particularly those working in general practice and in accident and emergency departments, need to know how to treat it.
Features of anaphylaxis
Erythema
Pruritus (generalised)
Urticaria
Angio-oedema
Laryngeal oedema
Asthma
Rhinitis
Conjunctivitis
Itching of palate or external auditory meatus
Nausea, vomiting, abdominal pain
Palpitations
Sense of impending doom
Fainting, lightheadedness
Collapse
Loss of consciousness
Definition
Anaphylaxis means a severe systemic allergic reaction. No universally accepted definition exists because anaphylaxis comprises a constellation of features, and the argument arises over which features are essential features. A good working definition is that it involves one or both of two severe features: respiratory difficulty (which may be due to laryngeal oedema or asthma) and hypotension (which can present as fainting, collapse, or loss of consciousness). Other features are usually present.
The confusion arises because systemic allergic reactions can be mild, moderate, or severe. For example, generalised urticaria, angio-oedema, and rhinitis would not be described as anaphylaxis, as neither respiratory difficulty nor hypotension—the potentially life threatening features—is present.
Mechanism
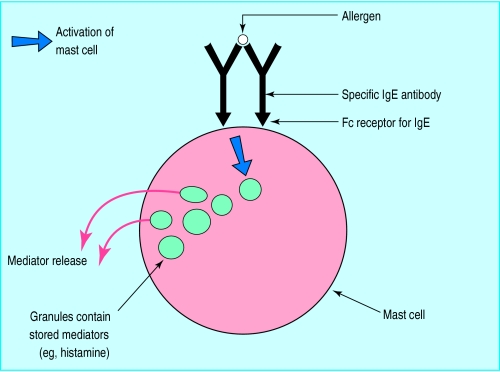
An allergic reaction results from the interaction of an allergen with specific IgE antibodies, bound to Fc receptors for IgE on mast cells and basophils. This leads to activation of the mast cell and release of preformed mediators stored in granules (including histamine), as well as of newly formed mediators, which are synthesised rapidly. These mediators are responsible for the clinical features. Rapid systemic release of large quantities of mediators will cause capillary leakage and mucosal oedema, resulting in shock and asphyxia.
Effects of mast cell mediators
| Physiological effect | Clinical expression | Danger |
| Capillary leakage | Urticaria | |
| Angio-oedema | ||
| Laryngeal oedema | Asphyxia | |
| Hypotension | Shock | |
| Mucosal oedema | Laryngeal oedema | Asphyxia |
| Rhinitis | ||
| Asthma | Respiratory arrest | |
| Smooth muscle contraction | Asthma | Respiratory arrest |
| Abdominal pain |
Anaphylactoid reactions are caused by activation of mast cells and release of the same mediators, but without the involvement of IgE antibodies. For example, certain drugs act directly on mast cells. For practical purposes (management) it is not necessary to distinguish an anaphylactic from an anaphylactoid reaction. This difference is relevant only when investigations are being considered.
Incidence
Hardly any data exist on the overall incidence of anaphylaxis. One recent study examining cases of anaphylaxis presenting to an accident and emergency department in Cambridge (to which all cases from a defined area would be brought) found that 1 in 1500 patients attending the department had anaphylaxis with loss of consciousness or collapse (equivalent to 1 in 10 000 a year in the population) and that the rate almost trebled when systemic allergic reactions with respiratory difficulty were included. Most other data relate to specific causes—for example, anaphylaxis due to allergy to penicillin or to anaesthetic drugs—and are quite variable.
Aetiology
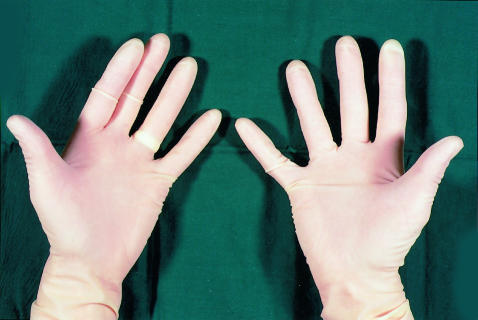
Foods are the commonest cause of anaphylaxis, and evidence suggests that this is an increasing problem, now documented for allergies to peanuts and other nuts. Insect venom is the next most common cause of anaphylaxis. A rapidly increasing problem is allergy to latex rubber. This is probably related to the enormous increase in the use of latex rubber gloves by medical and paramedical staff, as well as to the increase in atopy. Rare causes include exercise, vaccines, and semen. Allergen immunotherapy (desensitisation) may induce anaphylaxis.
Common causes of anaphylaxis
Foods
Bee and wasp stings
Drugs
Latex rubber
Foods commonly causing anaphylaxis
Peanuts
Tree nuts (eg, brazil nut, almond, hazelnut)
Fish
Shellfish
Egg
Milk
Sesame
Pulses (other than peanuts)
Drugs causing anaphylaxis or anaphylactoid reactions
Antibiotics (especially penicillin)
Intravenous anaesthetic drugs
Aspirin
Non-steroidal anti-inflammatory drugs
Intravenous contrast media
Opioid analgesics
Clinical features
It is important to recognise that the picture will vary with the cause. When an allergen is injected systemically (insect stings, intravenous drugs) cardiovascular problems, especially hypotension and shock, predominate. This is especially true when large boluses are given intravenously, as at induction of anaesthesia. Foods that are absorbed transmucosally (from the oral mucosa down) seem especially to cause lip, facial, and laryngeal oedema. Respiratory difficulty therefore predominates. With severe reactions onset occurs soon after exposure (within minutes), and progression is rapid.
Four brief case histories
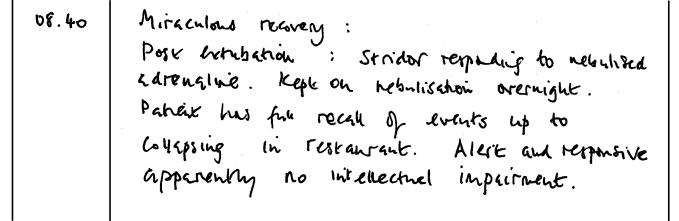
| Case 1—Woman aged 30, six months pregnant | |
| • Trigger: Chinese meal | Case 2—Woman aged 30 |
| • Symptoms and treatment: one hour after start of meal felt faint; mild asthma; severe dyspnoea and laryngeal oedema; loss of consciousness; taken to accident and emergency department after 10 minutes; on arrival cyanosed, respiratory arrest; periorbital oedema; salbutamol infusion; cardiac arrest four minutes later; adrenaline given; intubated with difficulty and ventilated | • Trigger: one teaspoonful muesli |
| • Recovered (see figure next page) | • Symptoms and treatment: immediate itching of mouth; throat swollen and uncomfortable inside; vomited; dyspnoea (could not breathe, different from her asthma); laryngeal oedema (obstruction in throat); lightheaded; no loss of consciousness; used her own salbutamol inhaler (no effect); taken to accident and emergency department; respiratory distress; intense erythema and generalised urticaria; given intramuscular adrenaline and chlorpheniramine |
| • Cause: allergy to green pepper | • Rapid recovery |
| Case 3—Boy aged 8 months | • Cause: allergy to brazil nuts and hazelnuts |
| • Trigger: Tiny quantity of peanut butter | Case 4—Woman aged 26 |
| • Symptoms: blisters around mouth; distressed; vomiting; dyspnoea; urticaria | • Trigger: vaginal examinations during labour |
| • Cause: allergy to peanuts | • Symptoms: itching of vulva; oedema of labia; generalised urticaria and pruritus; mild dyspnoea; felt woozy, lightheaded, odd, shaking |
Latex rubber anaphylaxis—unusually—develops more slowly (30 minutes or longer from the time of exposure), as the allergen has to be absorbed through the skin or mucosa (for example, during abdominal or gynaecological surgery, vaginal examination, dental work, or simply contact with, or wearing, rubber gloves). Healthcare workers are especially at risk.
Investigations
The only immediate test that is useful at the time of reaction is mast cell tryptase. Tryptase is released from mast cells in both anaphylactic and anaphylactoid reactions. It is an indicator of mast cell activation but does not distinguish mechanisms or throw light on causes. It is usually but not always raised in severe reactions but may not be in less severe systemic reactions. As mast cell tryptase is only raised transiently, blood should be taken when it peaks at about an hour after the onset of the reaction. This test remains to be fully evaluated.
Management
Adrenaline (epinephrine) is the most important drug for anaphylaxis and should be given intramuscularly. It is almost always effective.
Do not give adrenaline intravenously except in special circumstances (see text)
Drug treatment of anaphylaxis in adults
Intramuscular adrenaline 0.5 ml (500 μg), 1 in 1000 solution (1 mg/ml)
Intramuscular or slow intravenous chlorpheniramine 10 mg
Intramuscular or slow intravenous hydrocortisone 200 mg
This should be followed by chlorpheniramine and hydrocortisone (intramuscular or slow intravenous). This is usually all that is required, provided that treatment is started early. Treatment failure is more likely if administration of adrenaline is delayed. Biphasic reactions have been described but are probably rare; administration of hydrocortisone should minimise the risk of late relapse.
Difficulties may arise if the clinical picture is evolving when the patient is first assessed. Adrenaline should be given to all patients with respiratory difficulty or hypotension. If these features are absent but there are other features of a systemic allergic reaction, it is appropriate to give chlorpheniramine and hydrocortisone and reassess. If in doubt, give 500 μg adrenaline intramuscularly in an adult or the appropriate dose in a child.
Doses of intramuscular adrenaline in children
| Age (years) | Volume of 1 in 1000 | Dose (μg) |
| strength (1 mg/ml) | ||
| 1 | 0.1 ml | 100 |
| 2-3 | 0.2 ml* | 200 |
| 4-7 | 0.3 ml* | 300 |
| 8-11 | 0.4 ml* | 400 |
| >11 | 0.5 ml* | 500 |
This is a guide based on average weight for different age bands. No evidence exists for particular doses for different age bands, and published schedules therefore differ.
*Reduce dose in children of below average height.
There can be risks associated with intravenous adrenaline. Adrenaline should not be given intravenously except under special circumstances: profound shock (which is immediately life threatening) or during anaesthesia. Even then, if intravenous adrenaline is given, a dilute solution (1 in 10 000) must be administered very slowly in aliquots (with a maximum initial dose of 100 μg (that is, 1 ml)) with cardiac monitoring. Such treatment therefore is rarely indicated outside hospital.
Although myocardial infarction has been reported in the literature as being associated with the use of adrenaline, this reflects a bias in reporting, as the effective and safe use of adrenaline is not considered worth reporting. Those with wide experience of its use find adrenaline extremely safe.
β Blockers may increase the severity of an anaphylactic reaction and may antagonise some of the beneficial actions of adrenaline. However, if a patient with anaphylaxis is taking β blockers this should not prevent the use of adrenaline.
Supporting treatments
If the patient has hypotension then he or she should lie flat with the legs raised, but if respiratory difficulty is the dominant problem it may be better for the patient to sit up. Oxygen should be administered.
Key to management of anaphylaxis
Awareness
Recognise it (consider in differential diagnosis)
Treat quickly
Deaths in otherwise healthy young people could then be avoided
Anaphylaxis is easily treatable, and patients can make a complete recovery
An inhaled β2 agonist should be given if there is asthma. Inhaled adrenaline is effective for mild to moderate laryngeal oedema but would not be given if intramuscular adrenaline had already been given as first line treatment, and it is not a substitute for intramuscular adrenaline. If drugs are not rapidly effective for shock, intravenous fluids should be given rapidly.
Long term management
Patients are commonly sent home from accident and emergency departments without further advice. Patients are not infrequently given an ampoule of adrenaline or a preloaded adrenaline syringe without instruction. This is of little or no value and frightens patients.
What to do after an anaphylactic reaction
| Action | Aim |
| Take blood at 1-5 hours for measurement of mast cell tryptase | To confirm anaphylaxis or anaphylactoid reaction |
| Refer to an allergy clinic to determine cause | To prevent further attacks |
| Organise self treatment of future reactions (best done by an allergist) | To prevent morbidity (early treatment is the key) |
It is important to refer patients to an allergist— ideally, one with expertise in anaphylaxis. The cause should be determined, and advice given on avoidance to prevent further attacks. The cause is determined by taking a detailed and structured allergy history, then, in the case of IgE mediated reactions, confirmed (for most allergens) by skin prick tests. The cause is sometimes obvious from the history (as in case 3, previous page, where a typical reaction immediately followed ingestion of peanut butter). In case 1 the cause was also indicated by the history as there had been two allergic reactions, the first milder one after a “ploughman’s lunch” with few ingredients and the second after a large Chinese meal containing at least six suspected allergens. Green pepper was the common factor. Skin tests (directly through the flesh of green pepper and also with an aqueous extract of green pepper that we prepared) were strongly positive, confirming the diagnosis.
Early self treatment is highly effective, and reactions can usually be stopped easily. Syringes preloaded with adrenaline are easy for patients to use and readily available. They deliver fixed intramuscular doses and are available in two strengths: for adults (containing 0.3 ml of 1 in 1000 strength (that is, 300 μg)) and for children (0.3 ml of 1 in 2000 (150 μg)). The appropriate self treatment varies and may include other drugs. This should be determined by a specialist as, once a cause is determined and avoidance measures are in place, further reactions after inadvertent exposure are usually less severe. A written treatment plan should be provided by the allergist, and the patient (and relatives) should be taught how and when to use the treatments provided—for example, trainer syringes are available.
Some patients who have had an anaphylactic reaction wear a Medic Alert bracelet or necklace—with an inscription endorsed by a doctor that alerts other doctors to the possible cause of any future reaction
To be of help to children, schools and nurseries need training. Some allergists have developed links with community paediatricians, whose teams are best placed to deliver training. This requires expertise, which is now developed in only a few centres. The team in Cambridge is therefore coordinating the production of national guidelines.
Further reading
Stewart AG, Ewan PW. The incidence, aetiology and management of anaphylaxis presenting to an accident and emergency department. Q J Med 1996;89:859-64
Fisher MMcD, Baldo BA. The incidence and clinical features of anaphylactic reactions during anaesthesia in Australia. Ann Fr Anesth Reanim 1993;12:97-104
Ewan PW. Clinical study of peanut and nut allergy in 62 consecutive patients: new features and associations. BMJ 1996;312:1074-8
Turjanmaa K, Alenius H, Makinen-Kiljunen S, Reunala T, Palosuo T. Natural rubber latex allergy. Allergy 1996;51:593-602
Vickers DW, Maynard L, Ewan PW. Management of children with potential anaphylactic reactions in the community: a training package and proposal for good practice. Clin Exp Allergy 1997;27:898-903
If there is no local allergist the general practitioner or the doctor in the accident and emergency department should provide the drugs for self treatment, but it is essential that these are given with advice and training. Practice nurses should have trainer syringes for this purpose.
Figure.
Activation of mast cells by allergen crosslinking of adjacent IgE on cell surface in a type I allergic reaction
Figure.
Allergy to latex rubber is common in healthcare workers
Figure.
Entry in patient’s hospital notes (case 1, box previous page) 9 hours after anaphylaxis with cardiorespiratory arrest, showing effectiveness of prompt treatment
Figure.
Preloaded adrenaline syringes are available for self treatment of anaphylaxis
Footnotes
Pamela W Ewan is a Medical Research Council clinical scientist and honorary consultant in allergy and clinical immunology at Addenbrooke’s Hospital, Cambridge.
The ABC of allergies is edited by Stephen Durham, honorary consultant physician in respiratory medicine at the Royal Brompton Hospital, London. It will be published as a book later in the year.