The purpose of needs assessment in health care is to gather the information required to bring about change beneficial to the health of the population. It is generally, but not universally, accepted that this takes place within the context of finite resources.1 “Health gain” can therefore be achieved by reallocating resources as a result of identifying four factors:
Non-recipients of beneficial healthcare interventions (that is, unmet need);
Recipients of ineffective health care (and releasing the resources for unmet need);
Recipients of inefficient health care (and releasing resources for unmet need); and
Recipients of inappropriate health care (for whom the outcomes could be improved).
The subjects of healthcare needs assessment are the populations and patients who are recipients or potential beneficiaries of health care. Populations, of course, include individual patients. The assessment of individuals’ needs may form part of the assessment of a population’s needs, but it may be costly and it risks ignoring individuals with needs who do not present themselves for health care. Table 1 shows the circumstances favouring individual needs assessment for planning purposes.
Table 1.
Factors determining basis for assessing healthcare needs
| Individual basis | Population basis | |
|---|---|---|
| Case load | Light | Heavy |
| Cost per patient | High | Low |
| Hidden patients | Few | Many |
| Variability in case mix | High | Low |
The priority attached to different needs, whether of populations or of individuals, raises philosophical problems. For example, should the principal criterion be the benefit that could potentially be obtained for each individual, or the severity of their presenting condition?2 In other words, should greater priority (a greater assessed need) be attributed to the need for surgery of a patient with early stage colorectal cancer or to the need for hospice care of a terminally ill lung cancer patient? In practice the former, the approach that favours the greater benefit, takes precedence in formal needs assessment, but not exclusively. In either case, cost enters the equation. Some marginal benefits cannot be afforded in a publicly funded system because of the other treatments and benefits that need to be sacrificed to fund them.
New practitioners of needs assessment are emerging. The New NHS white paper requires primary care groups to contribute to health authorities’ health improvement programmes, “helping to ensure that they reflect the perspectives of the local community and the experiences of local patients.”3 More general practitioners will therefore face the dilemmas that needs assessment is intended to tackle.
Summary points
Healthcare need is the capacity to benefit from health care
The assessment of population benefit includes a measure of epidemiology (how many) and of cost effectiveness (how good)
Other sources, especially comparisons and corporate knowledge, can contribute usefully
An optimal approach requires good information gathering, clinical involvement, and a close relation to the planning process
From theory to practice
Different frameworks for healthcare needs assessment have reflected different purposes as well as different times and contexts.4 The life cycle model, for example, is a framework which encourages needs assessors to think comprehensively about different population groups of different ages.5 It is an attractive model because of its simplicity, but it does not distinguish need and demand or emphasise the pivotal theme of “capacity to benefit.”
A particular purpose of healthcare needs assessment is the spatial allocation of resources. Geographical equity of regions, districts, and even localities (such as housing estates) can be addressed by global and surrogate measures of health, particularly deprivation indices and standardised mortality ratios.6 Measuring relative deprivation is a step forward from approaches that do not distinguish need from supply and demand, but relative deprivation cannot be used to specify precise needs for service planning: measuring deprivation indicates whether Burnley is less well resourced than Belgravia but does not help in deciding the number of coronary care beds needed in either.
The definition of “need as the capacity to benefit” represents a further advance because it can be directed at specific services.7–9 It has generated new practical approaches in an area of sometimes paralysing controversy. Four points apply to needs assessment undertaken both at the level of health authority and general practice:
The population’s ability to benefit from health care equals the aggregate of individuals’ ability to benefit. For most health problems (but see table 1) this can be deduced more readily from epidemiological data than from clinical records.
The ability to benefit does not mean that every outcome will be favourable, but rather that need implies potential benefit, which on average is effective.
The benefit is not just a change in clinical status but can include reassurance, supportive care, and the relief of carers. The list of beneficiaries of care can extend beyond the patient to families and carers.
Health care includes not just treatment but also prevention, diagnosis, continuing care, rehabilitation, and palliative care.8
Such benefits are ideally assessed by an approach that combines epidemiological factors and cost effectiveness, supplemented by “corporate” and “comparative” methods.8,9 All of these methods include the enumeration of current services. But other contemporary approaches to service related assessment of needs should be noted: not just population healthcare needs assessment but also social services assessments, individual healthcare needs assessment, participatory and Oregon-style planning, population and client group surveys, expert specialty recommendations, and clinical effectiveness research.10 
The usefulness of these approaches can be assessed with the following criteria:
Is the needs assessment about populations or individuals?
Is there a clear context of allocating scarce resources (are the needs assessed in the context of priority setting among competing needs)?
Is the needs assessment exploratory or definitive (is the object to clarify what should be done or just to highlight problems that are accompanied by no obvious intervention)?
Is the determination of the most important needs based on expert knowledge or participatory methods?
Table 2 shows how other approaches compare with population healthcare needs assessment on the basis of the capacity to benefit. In population healthcare needs assessment the concern is with the health of populations with a common condition or presentation—for example, all patients with diabetes (known or not known) on a practice’s list. It recognises that resources are finite and avoids focusing on advocacy for individual groups without considering competing priorities. It is definitive rather than exploratory in that client groups are considered together with actual interventions (this is not a feature of, say, some lifestyle or disability surveys), and the needs are determined by expert appraisal of the evidence rather than principally through public participation. However, any approach that contributes information on numbers in a particular group (incidence and prevalence), the effectiveness and cost effectiveness of interventions, and the distribution of current services and their costs will be useful in practice.
Table 2.
Different approaches to healthcare needs assessment10
| Criterion | Basis | Is resource scarcity clear? | Definitive or exploratory | Expert or participatory |
|---|---|---|---|---|
| Population healthcare needs | Population | Yes | Definitive | Expert |
| Individual healthcare needs | Individual | Sometimes | Definitive | Expert |
| Social services assessments | Individual | Sometimes | Both | Both |
| Participatory planning | Population | Sometimes | Definitive | Participatory |
| Oregon-style planning | Population | Yes | Definitive | Both |
| Population surveys | Population | No | Exploratory | Expert |
| Client group surveys | Population | No | Exploratory | Both |
| Specialty recommendations | Population | No | Definitive | Expert |
| Effectiveness reviews | Population | Yes | Definitive | Expert |
Defining baseline services
Measured needs only take on meaning in relation to the existing services. Needs assessment is about change, and it is essential to know what to change from as well as what to change to. Several steps are involved. Firstly, the service under consideration has to be disaggregated into meaningful units. For example, mental health can be split up into adult, elderly, child, forensic, substance abuse, etc. Adult mental health could then be further subdivided as services for long stay, short stay, day care, community treatment, and so forth. Each of these encompasses a variety of different interventions. There follows a decision on what to measure. Structural factors such as bed capacity, staffing levels, and costs provide a powerful starting point. Measurement of process (for example, throughput) and outcomes (for example, death rate) will have little meaning unless case mix and severity are well defined. A plausible mental health baseline service specification focusing on structure and cost is set out in table 3. The emphasis is on obtaining the information needed to summarise existing levels of service as succinctly as possible.11
Table 3.
Example of table of baseline services11
| Resource name | Resource function | Capacity | Unit cost | Notes on quality and performance |
|---|---|---|---|---|
| Acute ward A | Acute assessment | Beds | £1000/bed | Nurse morale problems |
| Community team B | Community support for mild or stable conditions | Places | £1000/place | Poor coordination with general practice |
| Long stay facility C | Long stay and dementia | Beds | £1000/bed | Being run down |
Corporate approaches
The “corporate approach” involves the systematic collection of the knowledge and views of informants on healthcare services and needs. Valuable information is often available from health authority staff, provider clinicians, and general practitioners, as well as from users. The box lists possible informants. Although such an approach blurs the distinction between need and demand and between science and vested interest, the intimate, detailed knowledge of interested parties amassed over years might otherwise be overlooked. Furthermore, the corporate approach is essential if policies are to be sensitive to local circumstances. Eliciting local views is not the same as being bound by them. This approach allows sensitivity to local circumstances, particularly those consequent on historical provision. The unmet needs of discharged seriously mentally ill people from closed long stay hospitals or the absence of primary care for homeless groups may be uncovered only by speaking to people. Where cost effectiveness considerations are otherwise equal, local concerns may justifiably attach priorities to particular services. Furthermore, local experience and involvement will make any needs assessment easier to defend.
Corporate informants
General practitioners
Hospital doctors
Nurses and professions allied to medicine
Public health doctors
Commissioning managers
Trust managers
Voluntary organisations
Community health councils
General public
Patients (service users)
Comparative approaches
The “comparative approach” to needs assessment contrasts the services received by the population in one area with those received in other areas. If nothing else is known about the optimum service to be provided, there is at least reason for investigation if the level of service differs markedly from that provided elsewhere. Comparisons have proved to be powerful tools for investigating health services.12,13 For example, the need to raise renal dialysis and transplantation levels from 20 per million in the 1960s to 80 per million was indicated by comparison with European countries and subsequently confirmed epidemiologically.14 New performance indicator packages are being piloted in both primary and secondary care.15 Although they require sensitive interpretation, comparative process and outcome indicators may help identify deficiencies in provision of services.
Epidemiological and cost effectiveness approaches
The essence of needs assessment is an understanding of what is effective and for whom. Critical steps consist of:
A clear statement of the population group whose needs are to be assessed (normally a group with a particular disease). In the case of a needs assessment for diabetic services, this might include people who have not yet been diagnosed; in the case of substance misuse it would include past, present, and potential misusers;
Identifying subcategories of this population (perhaps “health benefit groups”) with particular service needs. People with insulin dependent diabetes would be distinguished from those with non-insulin dependent diabetes; current, dependent substance misusers would be distinguished from intoxicated misusers, those with comorbidities, those in recovery (at risk of relapse), and those at risk of becoming new users;
Setting out the prevalence and incidence of the subcategories: how many of each are there?
Setting out the current services available (the baseline)—all services whether in primary care, secondary care, or elsewhere;
Identifying the effectiveness and cost effectiveness of interventions and the associated services—the essence of evidence based health care; and
Setting out a model of care that apportions relative priorities.9,10
As a general rule, establishing the effectiveness of an intervention must be the most important step. There is little point in counting potential beneficiaries for an intervention which is of no benefit. Most challenging of all is the task of apportioning relative priority to different services and recipients. Cost effectiveness must be taken into consideration. The use of unitary cost-utility measures can be helpful if these are available, and decision matrices render decision making more explicit. However, flexibility around patients’ particular circumstances is often required.
Managing the task
Several challenges are commonly encountered in understanding needs assessment. Firstly, the mosaic of information required for needs assessment reflects its key components: the services already in existence, the prevalence and incidence of client groups (sub-categorised appropriately), and the effectiveness of interventions. The evidence based medicine movement has meant that information on effectiveness can more easily be obtained,16,17 but this is not true for information on epidemiology or services provided. Good quality local data on the structure and utilisation of health services can be surprisingly difficult to obtain. The absence of common disease definitions, common classification systems, and compatible software—and the partial recording of activity—limits the value of many databases.18
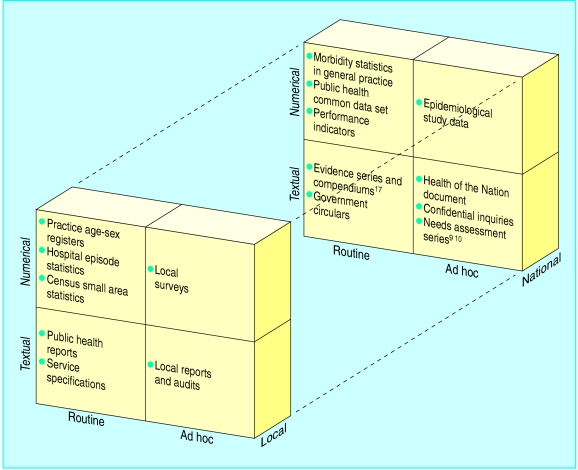
The triangulation of information sources is therefore critical. Useful information can be either local or national, either numerical or textual, and collected either routinely or ad hoc. The figure sets out key items for the needs assessors.19 The task is greatly aided by skilled librarians with access to a basic range of texts and databases. National sources of epidemiological and effectiveness data offer assessors of healthcare needs a firm starting point for their work.
A second challenge is the involvement of health professionals in healthcare needs assessment. The traditionally individualistic approach of doctors in particular may be difficult to reconcile with the utilitarian approach of planners with a population focus. This focus implies a fundamental reappraisal of the doctor’s role and the balance of power within the doctor-patient relationship.20 It is also important not to neglect the contribution of other health professionals. For example, in primary care much information is collected by community nursing staff, and health visitors’ skills in particular are easily overlooked.21 Even where doctors and nurses have a population focus, needs assessment has opportunity costs; not everyone can devote time to it. At the very least, target efficiency—directing services to the people who will potentially benefit the most—requires doctors’ involvement.
Thirdly, needs assessment is futile if it does not result in improved services to patients. A key to successful needs assessment is the proper understanding of how it is related to the rest of the planning process. Too much needs assessment is divorced from managers’ deadlines and priorities. If the information and recommendations produced are not timely, they will not be useful. The results of needs assessment therefore need to be encapsulated in strategies or business plans. These need clear definitions of objectives: describing what needs to be done, by whom, and by when.22 The key to effecting change is an understanding of the opportunities that may facilitate and the obstacles that may obstruct what is being attempted—knowing which “levers” to use. An understanding of the sources of finance, their planning cycles, and the criteria used to fund new initiatives is essential. Health authorities and health boards clearly indicate the timing of development bids and the structure of applications they wish to be submitted.
A fourth challenge is to ensure that needs assessment is not just effective but efficient and cost effective. Little is known of the cost effectiveness of needs assessment, but at least one survey found that it led to service change at little cost.23 Evaluation of different purchasing models should help clarify the population sizes for which needs assessment for different services is most efficiently undertaken.24
Conclusion
In practice, although needs assessment represents an amalgam of epidemiology, economics, and values, it has to be turned into a practical tool. But making needs assessment practical can have two unfortunate effects. Firstly, it is unhelpful to see the outcome of needs assessment as a document—the culmination of a series of easily defined, finite steps. Rather, needs assessment is an iterative, sometimes messy, process that may serve several different political purposes. The most important of these is to develop a consensus among planners, managers, and clinicians regarding priorities for service development. Secondly, needs assessment is too easily seen as some arcane preserve of public health specialists. The technical skills required can be exaggerated.25 Basic numeracy and common sense are the most important prerequisites.
The current approaches to needs assessment may be limited by time and context. Much needs assessment activity was stimulated by the advent of an internal market and by doubts about the cost effectiveness and appropriateness of care. Health authorities and general practitioners in their role as purchasers require detailed service specification for the first time. However, with increasing evidence of the equivocal efficacy of many healthcare interventions, delayed uptake of effective health care,26 unexplained geographical variations, and rising costs, the concern with capacity to benefit within finite resources is unlikely to wane. The rhetoric may change, but the demand for increasingly sophisticated approaches to needs assessment will intensify.
Figure.
Examples of sources of information
Figure.
These articles have been adapted from Health Needs Assessment in Practice, edited by John Wright, which will be published in July.
Footnotes
Funding: None.
Conflict of interest: None.
References
- 1.Dixon J, Harrison A, New B. Is the NHS underfunded? BMJ. 1997;314:58–61. doi: 10.1136/bmj.314.7073.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Culyer A. Need: the idea won’t do—but we still need it. Soc Sci Med. 1955;40:727–730. doi: 10.1016/0277-9536(94)00307-f. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. The new NHS, modern, dependable. London: HMSO; 1997. [Google Scholar]
- 4.Stevens A, Gabbay J. Needs assessment, needs assessment. Health Trends. 1991;23:20–23. [PubMed] [Google Scholar]
- 5.Pickin C. Assessment of health need using the life cycle framework. Manchester: Northwestern Regional Health Authority; 1991. [Google Scholar]
- 6.Department of Health and Social Security. Sharing resources for health in England. Report of the Resource Allocation Working Party. London: DHSS; 1976. [Google Scholar]
- 7.Culyer A. Need and the National Health Service. London: Martin Robertson; 1976. [Google Scholar]
- 8.National Health Service Management Executive. Assessing health care needs. London: Department of Health; 1991. [Google Scholar]
- 9.Stevens A, Raftery J. Health care needs assessment, the epidemiologically based needs assessment reviews. Vol. 1. Oxford: Radcliffe Medical Press; 1994. Introduction; pp. 11–30. [Google Scholar]
- 10.Stevens A, Raftery J. Health care needs assessment. Second series. Oxford: Radcliffe Medical Press; 1997. Introduction. Alternative approaches to health care needs assessment; pp. xxxii–xliv. [Google Scholar]
- 11.Stevens A, Raftery J. The purchasers’ information requirements on mental health needs and contracting for mental health services. In: Thornicroft, Brewin C, Wing J, editors. Measuring mental health needs. London: Gaskell; 1992. pp. 42–61. [Google Scholar]
- 12.Saunders D, Coulter A, McPherson K. Varieties in hospital admission rates: a review of the literature. London: King’s Fund; 1989. [Google Scholar]
- 13.Wennberg JE, Mulley AG, Hanley D, Timothy R, Fowler F, Roos N, et al. An assessment of prostatectomy for benign urinary tract obstruction. Geographic variations and the evaluation of medical care outcomes. JAMA. 1988;259:3027–3030. [PubMed] [Google Scholar]
- 14.Beech R, Gulliford M, Mays N, Melia J, Roderick P. Renal disease. In: Stevens A, Raftery J, editors. Health care needs assessment, the epidemiologically based needs assessment reviews. Vol. 1. Oxford: Radcliffe Medical Press; 1994. pp. 58–110. [Google Scholar]
- 15.NHS Executive. Consulting the NHS on a set of provisional clinical indicators. Leeds: NHSE; 1997. (EL(97)49.) [Google Scholar]
- 16.Haynes B, Sackett D, Muir Gray J, Cook D, Guyatt C. Transferring evidence from research into practice. 2. Getting the evidence straight. Evidence-Based Medicine. 1997;2:4–6. [PubMed] [Google Scholar]
- 17.Booth A. Scharr guide to evidence based practice. Sheffield: University of Sheffield, School of Health and Related Research; 1997. (Occasional paper No 97/2.) [Google Scholar]
- 18.Pringle M, Hobbs R. Large computer databases in general practice. BMJ. 1991;302:742–743. doi: 10.1136/bmj.302.6779.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NHS Management Executive. Purchasing intelligence. London: Department of Health; 1991. [Google Scholar]
- 20.Gillam S, Murray A. Needs assessment in general practice. London: Royal College of General Practitioners; 1996. (Occasional paper No 73.) [PMC free article] [PubMed] [Google Scholar]
- 21.Royal College of Nursing. The GP practice population profiles. A framework for every member of the primary health care team. London: RCN; 1993. [Google Scholar]
- 22.Spiegal N, Murphy E, Kinmonth AL, Ross F, Bain J, Coates R. Managing change in general practice: a step by step guide. BMJ. 1992;304:231–234. doi: 10.1136/bmj.304.6821.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fulop N, Henscher M. A survey of needs assessment activity in London health authorities. London: King’s Fund; 1997. [Google Scholar]
- 24.Mays N, Goodwin, Bevan G, Wike S.on behalf of TP-net. Total purchasing: a profile of national pilot projects. 1997London: King’s Fund [Google Scholar]
- 25.Gillam SJ. Assessing populations’ health needs: the general practitioners’ contribution. Br J Gen Pract. 1992;42:404. [PMC free article] [PubMed] [Google Scholar]
- 26.Antman E, Lau J, Kupelnick B, Mosteller F, Chalmers T. A comparison of results of meta-analyses of randomised control trials and recommendations of experts. JAMA. 1992;268:240–248. [PubMed] [Google Scholar]