Children are important users of health services, accounting for up to a quarter of general practitioner consultations1 and 30% of the workload in accident and emergency departments.2 However, their needs are given insufficient priority by policy makers and health service professionals. Last year a report of the British government’s health committee stressed that a change in attitude was needed and that it was important to listen to children and to take their views into account.3
Although consumers have an important role in reforming health care,4 the paternalistic attitude still prevailing among health professionals when it comes to consumer involvement in health care and research can make this difficult.5 Patient passivity begins early in life6 so we should not be surprised that adult users acquiesce. In this article we discuss why children should be consulted directly, how this is to be achieved, and finally what may be required to bring about change.
Summary points
Children are major users of health services but are rarely consulted as healthcare consumers
Although parents are extensively used as proxies for children, their accounts may not always accurately reflect children’s perceptions
Large numbers of children are cared for and treated by staff who have no paediatric training and abilities to communicate cannot be assumed
Children’s concepts of hospital care and illness differ greatly from those of adults
Children may be able to express their opinions if they are sought using appropriate methods
Staff need to be trained to enable the child’s voice to be heard and may need to consult colleagues in departments of child and family psychiatry and clinical psychology and develop closer contacts with teachers and social workers
Current situation
Parent as proxy
In Britain, although there has been an increasing emphasis on obtaining the views of health service users, children are rarely included. This probably reflects social attitudes and confusion about an appropriate approach for children. Some adults may have little interest in what children think, while others regard the need to protect them as paramount. The children’s charter on health was essentially a parents’ charter and reflects a common belief that children’s views may be represented by their parents.7
It cannot be assumed, however, that parents’ perception of their child’s response will accurately reflect the child’s feelings and needs, especially as the child becomes more independent. A study of quality of life in young children with asthma argued that reporting by proxy may lead to measurement of the impact of the child’s illness on the proxy rather than on the child, as shown in the the case of quality of life in young children with asthma.8 Jessop et al found a relation between the mother’s mental health and her ratings of the degree of disability of the child.9 Furthermore, mothers and staff have been found to have divergent opinions on a child’s likely perceptions. For example, in a recent study only 24% of mothers thought that their young children worried about being in hospital whereas 91% of staff believed this to be the case.10
Staff know best
Healthcare staff are often assumed to be able to communicate effectively with children, but it may not be easy for those without paediatric training, even though many will be parents. This is important since large numbers of children are seen outside paediatric settings. Sixteen per cent of children aged 5-15 years are admitted to hospital each year.11 In 1994 half the children admitted to English hospitals were not cared for by nurses qualified in nursing children. In Wales one quarter were admitted to adult wards.12
Staff training in communication lags behind good intentions, and the General Medical Council’s report on reforming medical education makes no specific reference to communicating with children.13 It is also assumed that staff know how children think and feel about treatment and care. A recent study, however, found that most children (75%) could understand the concept of localising their pain yet less than half the staff (41%) thought that young children could do this.10
Children’s concepts of hospitals and illness
Children differ greatly from adults in their understanding about the cause of illness and its treatment and prevention as well as in their perceptions of hospitals. Preschool children may believe that doctors or nurses deliberately set out to hurt them.14 Although it is difficult to generalise, children below the age of 7 years often see illness as occurring by contagion as if by magic or as a punishment for bad behaviour.15 From the ages of 7 to 11 children have a better knowledge and understanding, though their views are not those of an adult. They often see illness as caused by a single factor—often a “germ”—and therefore contagious. They do not correctly infer the reasons for treatment. From 11 years children have a more detailed understanding and become aware that illness can become aggravated by psychological factors. They understand the notion of drug related side effects and the possibility of delay before responding to treatment.16 Children with chronic illness, contrary to expectation, may not have a more mature understanding of their illness than those with little experience of hospitals. Especially little is known about children’s understanding of mental health.17 Medical terms may also be misinterpreted by children—for instance, a diagnosis of diabetes may be understood by a child in terms that they will “die of betes” or mention of oedema as a sign equated to a “demon in my belly.”15 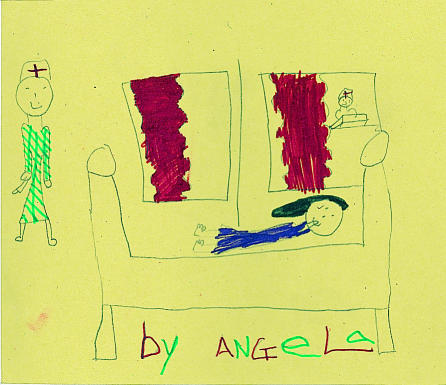
Although research on children’s views on hospital care and treatment is sparse, American studies have yielded some unexpected findings. Schoffstall discovered that children in hospital perceived the greatest stressors to be missing their families, being afraid of surgery, pain from their illness, infection, and being touched by people they did not know. They rated “sleeping with someone they didn’t know in their room” the eighth most stressful variable.18 Unless children’s perceptions are known, services cannot respond to their needs and improvements to achieve high quality care cannot be instigated.
Methods of consultation
Research methods for use with children are still unrefined. Although it has been suggested that children may need to be over the age of 8 to provide their views, children as young as 5 with emotional and behavioural problems were able to express their opinions on being in hospital.17 Alderson contends that rigidly controlled methods are seldom helpful.19 Thus validated measures, such as the metro assessment of child satisfaction (MACS), which can be used with children from the age of 6,20 may be of limited value. Clearly even basic tools such as questionnaires need modification for children, and activity booklets have been recommended. Questions can be incorporated with games and space provided for pictures to be drawn relating to experience.2
King maintains that using “talking pictures” to elicit opinions is a safer, easier, less threatening and less confusing method for children while also being more enjoyable for them.21 He believes that the type of information he obtained from drawings would probably not have been obtained by any other method. Martin contends that emotions repressed from children’s conscious minds are often expressed in their drawings in a non-threatening way; interpretation is not wild, mystical speculation but a rational way of gaining insight based on firm research.22 Bach’s work with spontaneous drawings by severely ill children often informed her of the somatic as well as the psychological condition of the patient.23 Where children may have difficulties drawing or communicating their views directly—for example, those with learning disabilities—photographs may be helpful.24 Account has to be taken of the child’s understanding together with his or her age and stage of emotional and cognitive development.17 A major difficulty with direct interviews, however, is that children’s responses to healthcare staff may reflect what the child thinks the professional wants to hear rather than the child’s true feelings.25 The gratitude barrier may be as prevalent in children as adults.
In recent years several indirect methods of consulting children have developed, particularly in the context of trauma. Dent-Read communicated with children in hospital by eliciting metaphors for body functioning and symptoms.26 Many of the methods used to help children describe distressing events and express their feelings, such as puppet play in the case of abused children,27 may also be appropriate and valuable means of learning what children are thinking.
How is change to be brought about?
In 1959 a government report recommended that children should be treated as children and not “mini adults” in hospital and emphasised the need for staff training in paediatrics. Thirty years later the Department of Health advocated that health needs must be met by those specifically qualified in child health and that staff training in the developmental and emotional needs of children is essential to a high quality service.28 These recommendations have yet to be implemented. Targets need to be set with timescales for meeting them if progress is to be made.
Communication skills with children need to be specifically included in the undergraduate curriculums of doctors and nurses. Health professionals could also benefit from closer liaison with those who possess expertise in child development and communication. For instance, greater use could be made of colleagues in departments of child and family psychiatry and clinical psychology. Specialist knowledge and experience could be exploited. Contact also needs to be extended with other non-health professionals such as teachers and social workers, who also work closely with children, as recommended by the report of the National Commission of Inquiry into the Prevention of Child Abuse.29 The report highlights the general practitioner’s role in identifying children at risk from abuse,30 for which doctors must be able to help children to express themselves.
To suggest that service providers should consult children does not mean that parents’ views should be ignored. Parents need to have the opportunity to express their expectations, which are likely to differ from children and will be based on many years’ experience of health services. Parents’ knowledge may be vital to understanding how best their child may be approached to avoid causing unnecessary distress. But parents have to recognise that children need to develop responsibility for their own health and health care. Children are not possessions but individuals with rights and developing responsibilities.29 Parents may need to be encouraged to stand back and enable children’s voices to be heard.
Conclusions
Healthcare professionals will not be able to allay children’s fears and respond to their needs unless they are prepared to develop effective means by which children can communicate with them. Seeking children’s views appropriately is important not only for the individual child and his or her family but also for the future of the NHS. Consumer participation is a prerequisite in bargaining assertively for quality health care.
Figure.
Research methods need refining
Figure.
Children’s views matter, too
References
- 1.Palmer KT. Notes for the MRCGP. Oxford: Blackwell Scientific; 1988. [Google Scholar]
- 2.McIver S. Obtaining the views of users of health services. London: King’s Fund; 1991. [Google Scholar]
- 3.House of Commons Health Committee. The specific health needs of children and young people. Vol. 1. London: Stationery Office; 1997. [Google Scholar]
- 4.Donabedian A. Quality assurance in health care: the consumer’s role. Quality in Health Care. 1992;1:247–251. doi: 10.1136/qshc.1.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liberati A. Consumer participation in research and health care. BMJ. 1997;315:499. doi: 10.1136/bmj.315.7107.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pittman KP. Awakening child consumerism in health care. Paediatr Nurs. 1992;18:132–136. [PubMed] [Google Scholar]
- 7.Department of Health. The patient’s charter: services for children and young people. London: HMSO; 1996. [Google Scholar]
- 8.Osman L, Silverman M. Measuring quality of life for young children with asthma and their families. Eur Resp J. 1996;9 (suppl 21):35–41. s. [PubMed] [Google Scholar]
- 9.Jessop DJ, Reissman CK, Stein RE. Chronic childhood illness and maternal mental health. J Dev Behav Pediatrics. 1988;9:147–156. [PubMed] [Google Scholar]
- 10.Gillies ML, Parry-Jones WL, Smith LN. Postoperative pain in children under five years. Health Bull. 1994;52:193–195. [Google Scholar]
- 11.Department of Health. Health and personal social services statistics for England. London: HMSO; 1993. [Google Scholar]
- 12.Lansdown R. Children in hospital. Oxford: Oxford University Publications; 1996. [Google Scholar]
- 13.General Medical Council. Tomorrow’s doctors: recommendations on undergraduate medical education. London: Kiek and Read; 1993. [Google Scholar]
- 14.Brewster AB. Chronically ill hospitalized children’s concepts of their illness. Pediatrics. 1982;69:355–362. [PubMed] [Google Scholar]
- 15.Perrin EC, Gerrity PS. There’s a demon in your belly: children’s understanding of illness. Pediatrics. 1980;67:841–849. [PubMed] [Google Scholar]
- 16.Bibace R, Walsh M. Children’s conceptions of health, illness and bodily functions. San Francisco, CA: Jossey-Bass; 1981. [Google Scholar]
- 17.Chesson R, Harding L, Hart C, O’Loughlin V. Do parents and children have common perceptions of admission, treatment and outcome in a child psychiatric unit? Clin Child Psychol Psychiatry. 1997;2:251–270. [Google Scholar]
- 18.Schoffstall MC. Children’s perceptions of hospital stressors. Nursing Times. 1988;84:60. [Google Scholar]
- 19.Alderson P. Children’s consent to surgery. Oxford: Oxford University Press; 1993. [Google Scholar]
- 20.Simonion S, Tarnowski K, Park A, Bekeny P. Child, parent and physician perceived satisfaction with paediatric out-patient visits. Dev Behav Paediatrics. 1993;14:8–12. [PubMed] [Google Scholar]
- 21.King P. Talking pictures: triggered pictures to help children talk about themselves. London: British Association for Adoption and Fostership; 1992. [Google Scholar]
- 22.Martin J. A channel from the subconscious. Understanding drawing interpretation. Professional Nurse. 1994;10:14–19. [PubMed] [Google Scholar]
- 23.Bach S. Life paints its own span: on the significance of spontaneous pictures by severely ill children. Zurich: Daimon Verlq; 1991. [Google Scholar]
- 24.Joy D, Harvais V, Young A, Chesson R. The use of photographs in surveying children with learning disabilities views of occupational therapy. Br J Occup Therapy. 1998;61:116–120. [Google Scholar]
- 25.Parish L. Communicating with hospitalised children. Canadian Nurse. 1986;82:21–24. [PubMed] [Google Scholar]
- 26.Dent-Read CH. Communicating with hospitalized children by eliciting metaphors for body functioning and symptoms. Chicago: Midwestern Psychological Association; 1991. [Google Scholar]
- 27.Geldard K, Geldard D. Counselling children: a practical introduction. London: Sage; 1997. [Google Scholar]
- 28.Department of Health. The welfare of children and young people in hospital. London: HMSO; 1991. [Google Scholar]
- 29.Childhood matters—the report of the National Commission of Inquiry into the Prevention of Child Abuse. Vols 1 and 2. London: Stationery Office, 1996.
- 30.Hobbs CJ, Heywood PL. Childhood matters. BMJ. 1997;314:622. doi: 10.1136/bmj.314.7081.622. [DOI] [PMC free article] [PubMed] [Google Scholar]




