Abstract
Background:
Enhanced recovery pathways can be further improved for postoperative sore throat (POST) that occurs after surgery under general anesthesia. Medications have shown some effectiveness in preventing POST, but acupuncture or related techniques with better safety and lower cost can be used as an alternative or adjuvant therapy to treat perioperative symptoms by stimulating acupuncture point (acupoint). Therefore, we aimed to conduct a meta-analysis to assess whether acupoint stimulation helps patients prevent POST in adults undergoing tracheal intubation for general anesthesia.
Methods:
Publications in PubMed, the Cochrane Central Register, ScienceDirect, and ClinicalTrial.gov were surveyed from January 2000 through August 2020. Studies that compared interventions between true acupoint stimulation and no or sham acupoint stimulation were included. The primary outcomes were the incidence and severity of POST at 24h.
Results:
Four randomized control trials and 1 comparative study involving 1478 participants were included. Compared with the no or sham acupoint stimulation, the true acupoint stimulation was associated with a reduced incidence (risk ratio, 0.32; 95% confidence interval (CI), 0.18–0.55; P < .001) and decreased severity (standardized mean difference, −2.79; 95% CI, −4.59 to − 0.99; P = .002) of POST. There were no significant adverse events related to acupoint stimulation. The finding for POST was assured by subgroup, sensitivity, and trial sequential analyses.
Conclusions:
Acupoint stimulation may reduce the occurrence of POST. It can be considered as one of nonpharmacological methods to prevent POST in enhanced recovery pathways. Further rigorous studies are needed to determine the effectiveness of acupoint stimulation.
Keywords: acupuncture point stimulation, enhanced recovery, general anesthesia, intubation, postoperative sore throat
1. Introduction
Postoperative sore throat (POST) is a common symptom caused by tracheal intubation under general anesthesia.[1] The incidence of POST reported from university hospitals in Asia varies from 35.7% to 57.5%.[2–4] Studies have shown a higher possibility of occurrence due to some factors, such as female sex, older age, higher intracuff pressure, airway device, anesthesia time, and surgical site.[2–4] Although this postoperative symptom is often considered as a minor complication, it remains one of the most common complaints from patients after general anesthesia, second only to postoperative nausea and vomiting (PONV).[5] POST has a chance to persist for several days and may lead to potential dissatisfaction in patients after operations.[5–8] It can also cause children to delay intake[9] or cause patients to have longer postoperative stays after surgery.[10] In the past few years, there have been some ways to improve PONV in enhanced recovery after surgery (ERAS)[11]; we believe that there is room for improving ERAS pathways for POST.[12]
The etiologies of throat complications are believed to be caused by tracheal intubation that results in mucosal trauma and inflammation.[13,14] These injuries trigger a sore throat when the anesthesia wears off. Several postoperative complications, including cough, sputum, dysphagia, and hoarseness, are also likely to occur because of intubation.[15] Some studies suggest that several medications, such as dexamethasone,[16] benzylamine,[17] corticosteroids,[18] lidocaine,[19] ketamine,[20] and magnesium,[21] could be used as effective strategies to prevent or treat POST. They also report the potential benefit of the medication for other complications, such as a reduced incidence of cough,[16,19,20] to present more clinical significance.
In contrast to modern treatments, acupuncture or related techniques are also used as an alternative or adjuvant therapy in the perioperative period (e.g., the management of postoperative pain).[22] Acupuncture is a medical practice that stimulates acupuncture points (acupoints) on the body with thin needles and improves health on the theory of traditional Chinese medicine.[23] Its related techniques, including moxibustion, acupressure, acupoint application, electrical/laser/magnetic/ultrasonic acupuncture, transcutaneous electrical nerve/acupoint stimulation (TENS/TEAS), and bloodletting, are the same in principles but differ in methods.[24–26] However, the effectiveness of acupoint stimulation with various methods remains inconclusive. Therefore, in this paper, the meta-analysis aims to examine whether acupoint stimulation helps patients prevent or treat POST undergoing tracheal intubation for general anesthesia.
2. Methods
The means and reports of this systematic review followed the Cochrane Collaboration methodology[27] and PRISMA statement.[28] The protocol was registered at PROSPERO (CRD42020177480). All analyses were based on previously published studies; thus, no ethical approval and patient consent were required.
2.1. Eligibility criteria
Regarding the types of studies, we enrolled randomized controlled trials or comparative experimental trials, and excluded follow-up studies, case series, and case reports. The target participants should have the following inclusion criteria: (1) adult patients who underwent elective surgery with general anesthesia; (2) all patients received intubation by various types of airway devices. All retrieved studies were required to comprise at least 2 arms, one of which had an intervention with true acupoint stimulation and the other had an intervention with no or sham acupoint stimulation. Studies were also excluded if they had no evaluation of sore throat at 24 hours after extubation or surgery.
2.2. Search strategy
We searched 4 electronic databases, including PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), ScienceDirect, and ClinicalTrial.gov, from January 2000 to August 2020. Original articles not written in English or Chinese and not available in full-text were excluded.
The following search terms were used individually or combined: “postoperative sore throat,” “intubation complication,” “anesthesia complication,” “acupressure,” “transcutaneous electrical nerve stimulation,” “acupuncture,” “acupuncture point,” “moxibustion,” “bloodletting.” The MeSH terms were used during the search if the database system was available. Details of the search strategy are shown in Supplementary Table 1 (Supplemental Digital Content, which demonstrates the search strategy, http://links.lww.com/MD/G887).
2.3. Study selection
Two authors independently selected the included studies according to the eligibility criteria. Disagreements were resolved by discussion.
2.5. Data extraction
The same authors examined the included studies and extracted data in a predetermined form. It recorded the first author, year, study design, sample size, sex, age, American Society of Anesthesiologists (ASA) physical status classification, surgery, intervention, and outcome measurements. Detailed information about the intervention and anesthesia was also collected.
2.6. Risk of bias assessment
The risk of bias was assessed independently by the same authors using the Cochrane risk of bias assessment tool.[27] For randomized trials, the RoB 2.0 tool was used to assess 5 domains that could lead to an overall bias.[29] For nonrandomized trials, the ROBINS-I tool was used to assess 7 domains that could be ascertained to produce an overall bias.[30] The risk of bias was visualized using robvis.[31] Disagreements were resolved by discussion.
2.7. Outcome measurement
The primary outcomes were the incidence or severity of sore throat at 24 hours after surgery/extubation and adverse events in the study groups. Studies on postoperative sore throat often used the ordinal scale, such as a 4-level classification system to rate the severity of the condition (i.e., none, mild, moderate, and severe). When a study used this classification system, the incidence of sore throat was calculated from the sum of mild, moderate, and severe cases. The secondary outcomes included the incidence or severity of related complications after surgery or extubation. Continuous and dichotomous outcomes were presented as risk ratios, standardized mean differences, and 95% CIs. When trials contained zero events in either arm, continuity correction was calculated with the addition of 0.5 to each cell of 2 × 2 tables from the trial.[32] When continuous outcomes were presented as median and range, they were converted to mean and standard deviation using the methods proposed by Wan et al[33] and Luo et al.[34] If the data could not be applied to the meta-analysis, we summarized them in the text.
2.8. Data synthesis and analysis
We chose the DerSimonian and Laird random-effects model to analyze the collected data. Heterogeneity among the studies was assessed using the Higgins I 2 test; I 2 > 50% indicated substantial heterogeneity. This random-effects model was often considered with inappropriate type I error and we thus conducted sensitivity analyses by the Hartung-Knapp-Sidik-Jonkman method because it was able to work better in a limited number of included studies.[35] Subgroup analyses were also conducted to assess whether the treatment effects were changed because of the study design or the airway device. The trial sequential analysis was performed to examine the required information size and the reliability of the outcomes from our meta-analysis. According to a previous review of postoperative complications and acupoint stimulation,[36] we designed a relative risk reduction of 30% for POST that was considered clinically meaningful at a 5% risk of a type I error and a power of 80%. Nonrandomized studies were excluded from the trial sequential analysis (TSA). Statistical significance was defined as P < .05, except for the determination of publication bias, which employed P < .1. If more than 10 studies were included in the meta-analysis, publication bias was investigated using funnel plots. In addition, publication bias was tested by Egger regression. Statistical analyses were conducted using Comprehensive Meta-Analysis, version 3 (Biostat, Englewood, NJ) and the trial sequential analysis was performed using TSA software, version 0.9 beta (Copenhagen Trial Unit, Copenhagen, Denmark).
3. Results
3.1. Overview of included studies
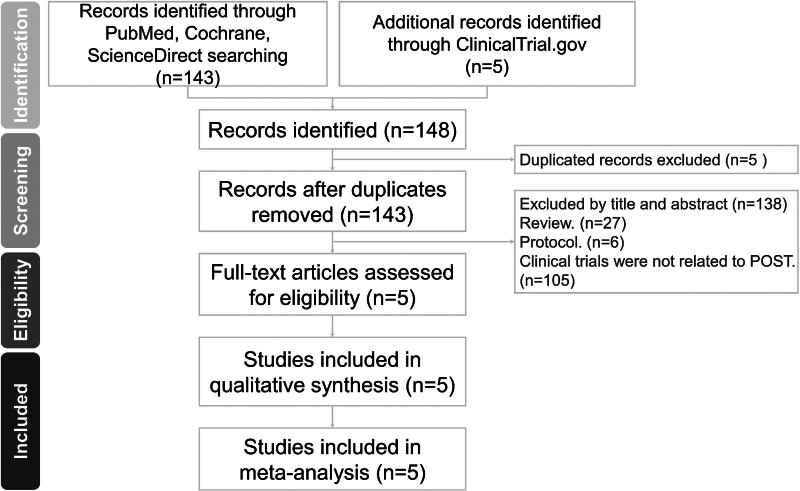
Our search yielded 148 titles and abstracts (Fig. 1). After applying the inclusion and exclusion criteria, 4 randomized controlled trials (RCTs) and 1 quasi-experimental study (QES) involving 1478 participants were included in the analysis.[37–41] The mean age of the study participants ranged from 35.69 to 58 years, and the proportion of women ranged from 33.3% to 100% (Table 1). Five trials included patients with ASA status of I–II. Four trials provided obvious types of surgery, including total abdominal hysterectomy,[37] cholecystectomy,[38] gastrointestinal,[38] herniorrhaphy,[38] mastectomy,[38] thyroid surgery[38,39] and shoulder arthroscopic surgery.[40] One trial noted that none of the patients received head or neck surgery.[41]
Figure 1.
PRISMA flow diagram for searching and identification of included studies.
Table 1.
Characteristics of included studies.
| First author (year) | Study design | Sample size (% female) |
Mean age (SD or range) |
ASA | Surgery | Intervention | Outcome measurement |
|---|---|---|---|---|---|---|---|
| Park et al (2004)[37] | RCT | True T: 50 (100%) Sham T: 50 (100%) C: 50 (100%) |
True T: 43.8 (32–59) Sham T: 44.9 (33–61) C: 42.6 (32–47) |
I, II | Total abdominal hysterectomy | True T: capsicum plasters (bilateral hand K-A20 points), placebo tape (bilateral thighs) Sham T: capsicum plasters (bilateral thighs), placebo tape (bilateral hand K-A20 points) C: placebo tape (bilateral hand K-A20 points, thighs) |
P1: incidence of POST score of sore throat P3: incidence of POST, PONV dosage of analgesic |
| Esmaeili et al (2013)[38] | QES | T: 114 (33.3%) C: 114 (38.6%) |
T: 40.54 (±14.1) C: 35.69 (±13.22) |
I, II | Cholecystectomy, gastrointestinal, thyroid, herniorrhaphy, and mastectomy | T: acupuncture with needle (bilateral wrist PC6 points) C: no acupuncture. |
P3: incidence of fever, bleeding, PONV, POST, ICU admission, sore throats needing medical care |
| Wang et al (2017)[39] | RCT | T: 50 (78%) C: 50 (84%) |
T: 44 (±10) C: 42 (±9) |
I, II | Thyroid gland lobectomy | T: active TEAS (bilateral hand LI4, wrist PC6 points) C: inactive sham TEAS (bilateral hand LI4, wrist PC6 points) |
P2: incidence of POST VAS of sore throat P3: incidence of POST VAS of sore throat |
| Pan et al (2019)[40] |
RCT | T1: 40 (55%) T2: 40 (50%) C: 40(55%) |
T1: 57(±8) T2: 58(±6) C: 58(±6) |
I, II | Shoulder arthroscopic surgery | T1: before operation, active TEAS (sham acupoints); after operation, active TEAS (hand LI4, wrist PC6 points at the affected limb) T2: before operation, active TEAS (hand LI4, wrist PC6 points at the affected limb); after operation, active TEAS (sham acupoints) C: before and after operation, active TEAS (sham acupoints) |
P2: VAS of shoulder satisfaction rate time of first use of PCIA pump P3: dosage of analgesic VAS of shoulder incidence of PONV, POST, dry month pressing number of PCIA pump |
| Lu et al (2019)[41] | RCT | T: 480 (50.8%) C: 400 (35.7%) |
T: 48.6 (±12.9) C: 47.1 (±11.1) |
I, II | All possible surgeries except head and neck | T: treatment plasters with biological waves (neck RN22 and RN23 points) in 5 experimental groups. C: blank tapes (neck RN22 and RN23 points) in 5 control groups. Groups of T and C have 5 clinical situations: SP, NSL, nonLS; PP, SSL, nonLS; SP, NSL, LS; SP, LMAS, nonLS; LD, DL, nonLS. |
P1: incidence of choking cough, sputum score of choking cough volume of sputum pH value of sputum P2: incidence of POST P3: incidence of POST, POVN |
C = control group, DL = double lumen, ICU = Intensive Care Unit, LD = lateral decubitus, LMAS = laryngeal mask, LS/nonLS = laparoscopic surgery/ non-laparoscopic surgery, NSL = normal single lumen, PACU = post-anesthesia care unit, PCIA = patient-controlled intravenous analgesia, PONV = postoperative nausea and vomiting, POST = postoperative sore throat, PP = prone position, QES = quasi-experimental study, RCT = randomized controlled trial, SP = supine position, SSL = spring single lumen, T = treatment group, TEAS = transcutaneous electrical acupoint stimulation, VAS = Visual Analogue Scale.
P1 = at the time of PACU/ recovery room, P2 = after leaving PACU/ recovery room, P3 = at 24 h.
Acupoints were stimulated by acupoint application in 2 RCTs. One used capsicum plasters and compared the true treatment with the sham treatment or the control.[37] The other used plasters with biological wave effects and compared the true treatment with the control in every subgroup.[41] Each subgroup had its own clinical situation, including different positions, airway devices, and surgical procedures. For a clearer comparison, we extracted data from these subgroups for analysis except for the groups with laryngeal mask airway, which did not totally and deeply pass through the throat as an endotracheal tube. Following the recommendation of the Cochrane handbook,[27] we combined multiple groups to create a single pair-wise comparison.
Two RCTs used TEAS to stimulate acupoints. One compared the active TEAS with the inactive, sham TEAS at the same acupoints.[39] The other compared the preoperative true-acupoint TEAS or the postoperative true-acupoint TEAS with the sham-acupoint TEAS.[40] A quasi-experimental study compared the case of body acupuncture with the case of no acupuncture.[38] Details of the anesthesia and intervention are summarized in Supplementary Table 2 (Supplemental Content, which presents detailed information on anesthesia and intervention, http://links.lww.com/MD/G887).
Two trials assessed the severity of sore throat at 24 hours with a 5-point scale[37] and a visual analog scale (VAS).[39] Ten groups within 1 trial[41] provided the incidences of choking cough and sputum immediately after extubation, but we summarized them in the text.
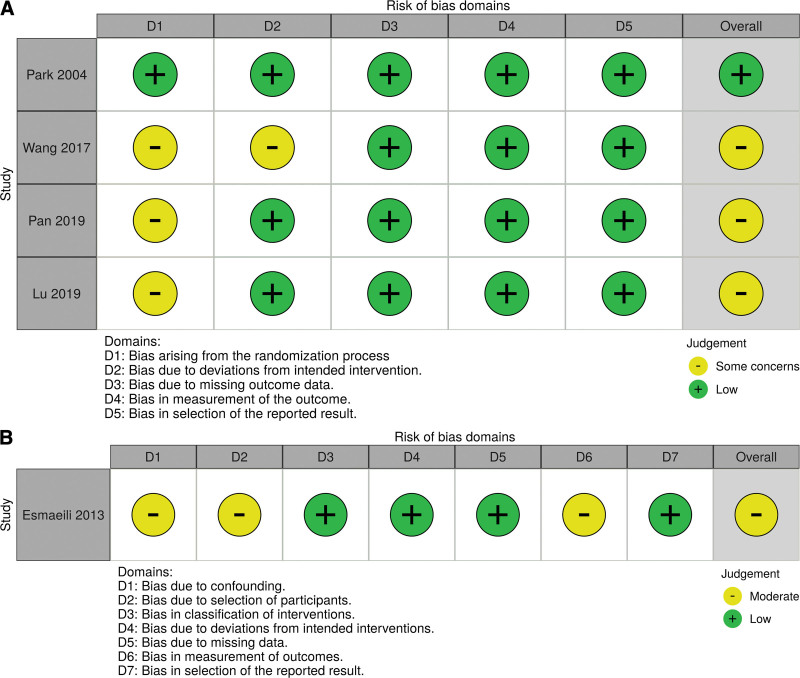
3.2. Risk of bias
The quality of randomized control trials generally needs to have some concerns according to the RoB 2.0 (Fig. 2A). Three included studies had unclear allocation concealment[39–41]; one of them did not report enough information on how to blind when participants received the intervention before anesthesia induction.[39] The quality of the quasi-experimental study also needed some concerns according to the ROBINS-I (Fig. 2B). Although all participants in the study received tubes and had intubation-related trauma, other possible undetermined causes of sore throat could generate confounding factors and lead to a vague outcome of selection or measurement.[38]
Figure 2.
Risk of bias for included studies. (A) 4 RCT with RoB 2.0; (B) 1 QES with ROBINS-I. RCT: randomized controlled trial; QES: quasi-experimental study.
3.3. Publication bias
Because there were fewer than 10 retrieved trials in our study, we did not apply a funnel plot. We performed Egger regression and found no publication bias (P = .53).
3.4. Primary outcomes
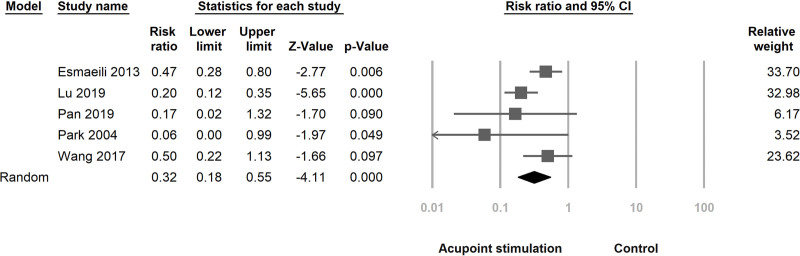
3.4.1. Incidence of postoperative sore throat.
Five studies that included 1148 participants provided data on the incidence of sore throat at 24h after surgery or extubation.[37–41] Pooled analysis in the random-effects model did not show significant statistically heterogeneity (I2 = 0%). The results indicated that acupoint stimulation was associated with a reduced incidence of postoperative sore throat (RR, 0.32; 95% CI, 0.18–0.55; P < .001; df = 4; Fig. 3).
Figure 3.
Forest plot for the incidence of POST at 24h. The plot shows the reduced incidence in patients treated with acupoint stimulation compared with control. The control involves a treatment with no or sham acupoint stimulation. The I2 value for heterogeneity was zero.
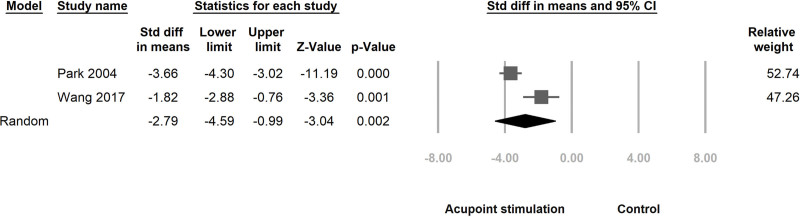
3.4.2. Severity of postoperative sore throat.
Two studies involving 121 participants reported the severity of sore throat at 24h after surgery or extubation.[37,39] One of them presented the median and range of sore throat scores[37] and we converted the median (range) to the mean (SD) in math. Pooled analysis in the random-effects model did not show significant statistically heterogeneity (I2 = 0%). The results indicated that acupoint stimulation was associated with a decreased severity of postoperative sore throat (SMD, −2.79; 95% CI, −4.59 to −0.99; P = .002; df = 1; Fig. 4).
Figure 4.
Forest plot for the severity of POST at 24h. The plot shows the decreased severity in patients treated with acupoint stimulation compared with control. The control involves a treatment with no or sham acupoint stimulation. The I2 value for heterogeneity was zero.
3.4.3. Adverse events.
One study reported that 2 patients in the true treatment group and 4 patients in the sham treatment group had plaster side effects of mild burning sensation with erythema.[37] The other did not report any adverse events developed in their study groups.[38–41]
3.5. Secondary outcomes
3.5.1. Incidence of choking cough and sputum.
Except for 1 experimental group and 1 corresponding group with a laryngeal mask airway, 4 experimental and 4 corresponding control groups with lumen tubes within the trial[41] included 640 participants. The incidence of choking cough in each experimental group was significantly lower than that in the corresponding control group and ranged from 11.4% to 18.8%. There was also a significantly lower incidence of sputum in each experimental group than in the corresponding control group and the incidence ranged from 11.3% to 18.8%.
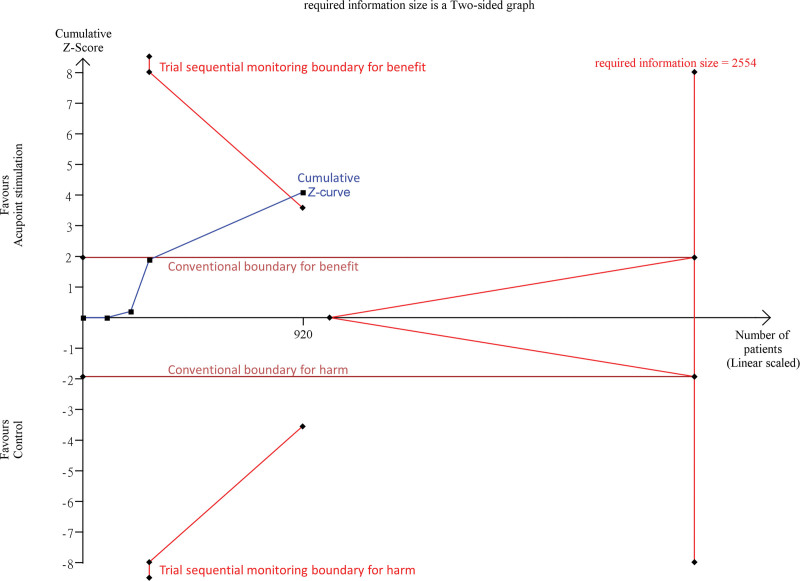
3.5.2. Subgroup, sensitivity, and trial sequential analyses.
In the subgroup analysis, for the study design, we divided all studies into RCT and QES groups. There was no significant difference between the 2 groups (Q-value, 1.91; P = .167; df = 1), but the pooled analysis with only RCTs showed a more reduced incidence of POST (RR, 0.26; 95% CI, 0.13–0.5; P < .001). For the airway device, we inferred that 4 studies used a normal single lumen from the description of the anesthesia process, tube size and surgery in the articles.[37–40] We also used subgroups with different clinical situations within the study[41] as the unit of analysis and divided the 5 studies into the groups of normal single lumen (standard single lumen tube), spring single lumen (reinforced single lumen tube), and double lumen. There was no significant difference among the 3 groups (Q-value, 2.783; P = .249; df = 2) and all tended to favor acupoint stimulation for reducing the incidence of POST.
We conducted a sensitivity analysis on the incidence of POST using the Hartung-Knapp-Sidik-Jonkman method. The summary effect in POST was consistent with the primary finding despite becoming larger range of 95% CI (RR, 0.32; 95% CI, 0.15–0.67; P < .001). When excluding QES, the TSA with RCTs suggested that the cumulative z-curve crossed both the conventional and trial sequential monitoring boundaries for benefit before reaching the required information size (2554 patients; Fig. 5), thereby recommending a positive effect of acupoint stimulation on the prevention of postoperative sore throat.
Figure 5.
The trial sequential analysis with median control event proportion of 18.7% from 4 included RCTs. The cumulative z curve (blue line) crosses the conventional boundary for benefit (horizontal brown line) and the trial sequential monitoring boundary for benefit (red line), showing a positive effect.
4. Discussion
According to limited data derived from the included trials, our study suggests that the true acupoint stimulation in adults undergoing tracheal intubation for surgery under general anesthesia is associated with a decline in POST at 24h and possibly results in less severity in comparison with the no or sham acupoint stimulation. It seems a good prophylactic effect that the number needed to treat POST (to prevent 1 case of postoperative sore throat) is 7. Limited evidence suggests that acupoint stimulation is not related to significant negative events and has a lower incidence of choking cough and sputum. Although we were not able to collect the samples with the best quality for meta-analysis, our findings are robust throughout the subgroup analysis, sensitivity analysis, and TSA, thereby confirming that acupoint stimulation prevents postoperative sore throat.
As normal, the number of patients with POST decreases within 48 hours and a few patients still have the symptom at 96 hours.[7] To improve POST, most current medications are assessed by the incidence or severity of POST at 24 hours.[16–21] The possible mechanisms of medications to prevent or treat POST are antiinflammatory, sensory-nerve suppression, and N-methyl-D-aspartic acid (NMDA) receptor antagonists.[16–21] In our view, the possible mechanisms of acupoint stimulation to prevent POST are 2 proposed possibilities. One is to regulate antiinflammatory responses, increase local blood circulation and reduce regional inflammatory-related pain.[42,43] The other is to start the neurophysiological system and induce an acupuncture-analgesic effect.[23,24,44] Five trials included in our study used different acupuncture-related techniques (acupoint application, TEAS or body acupuncture) and acupoints on different sites (neck or upper limb). It is difficult to assert which methods or acupoints are valid, especially in a limited number of current literature. However, their results basically explained the feasibility of stimulating acupoints to prevent POST.
One of the elements of enhanced recovery is to manage postoperative pain, but the ideal postoperative pain management remains a challenge.[45] According to previous articles,[17,18,20,21] topical application of ketamine, magnesium, corticosteroids, and benzydamine hydrochloride for POST at 24h were associated with a decreased incidence with a risk ratio of 0.45, 0.31, 0.39, and 0.31, respectively. The outcome of our study demonstrated that the true acupoint stimulation could create a similar preventive effect with a risk ratio of 0.32. On the other hand, these analgesics are not devoid of their pharmacological side effect. In our review, stimulating acupoints was almost in the physical methods except that using the capsicum plaster was a chemical stimulus. Because of the ingredients of capsicum, the plaster has a chance to bring about skin irritation slightly. Nevertheless, we can choose clear or sterile needles to stimulate acupoints to prevent POST and avoid pharmacological or chemical adverse events. Acupoint stimulation by acupuncture and related techniques seems to be an effective, nonpharmacological approach with better safety.[24,46,47]
ERAS pathways still require multimodal analgesia to reduce pain, improve analgesic-related adverse effects and accelerate postsurgical recovery.[48] Lu et al[49] suggested that the perioperative period under anesthesia combined with acupuncture might be beneficial to patients with less analgesic consumption, lower incidence of complications and better recovery. Both system reviews of craniotomy[50] and cardiac surgery[51] showed less analgesic consumption in general anesthesia with acupuncture therapy. Yoo et al[52] also showed that enhanced recovery in gynecological surgery with acupuncture improved gastrointestinal motility, coldness, urinary retention, PONV, and sore throat. Acupoint stimulation by acupuncture and related techniques appears to provide assisted analgesia with lower cost and better recovery.[24,47–49] The concept of “perioperative acupuncture medicine,” which was proposed by Yuan et al,[53] is the intervention of acupuncture or related techniques with acupoint stimulation before, during and after surgery to enhance recovery. Our review on the prevention of POST could serve as one of evidence-based practices in perioperative acupuncture medicine for ERAS.
This review has some limitations. First, we were unable to enroll enough good-quality studies to analyze in the absence of current trials, which limits the strength of our findings. Second, one study with multiple groups accounted for over half of the patients and may generate more relative weight in our outcome for preventing POST.[41] However, we minimized the influence of the study when using a random-effects model to adjust its relative weight and examining our outcome by 3 statistical analyses. Third, only 1 study mentions adverse events. Finally, our search was limited to English and Chinese articles only, causing a potential language bias.
5. Conclusions
In summary, the treatments with true acupoint stimulation were significantly more effective than the treatments with no or sham acupoint stimulation for the prevention of postoperative sore throat at 24 hours. Acupoint stimulation can be considered as one of nonpharmacological methods to prevent POST in ERAS. However, further clinical trials are needed to determine the effectiveness of acupoint stimulation and adverse events owing to the lack of rigorous studies.
Acknowledgements
The authors are grateful to the members of the Research Office for Health Data, Department of Education and Research, Taipei City Hospital, Taiwan, for their valuable contributions in statistical consultation.
Author contributions
All authors provided final approval and agree to be accountable for the work.
Conceptualization: Pin-Yu Jau
Data curation: Pin-Yu Jau Shang-Chih Chang
Formal analysis: Pin-Yu Jau
Investigation: Pin-Yu Jau Shang-Chih Chang
Methodology: Pin-Yu Jau Shang-Chih Chang
Writing–original draft: Pin-Yu Jau
Writing–review & editing: Shang-Chih Chang
Supplementary Material
Abbreviations:
- DL =
- double lumen
- ERAS =
- Enhanced Recovery after Surgery
- ICU =
- Intensive Care Unit
- LD =
- lateral decubitus
- LMAS =
- laryngeal mask
- LS/non-LS =
- laparoscopic surgery/ nonlaparoscopic surgery
- PACU =
- post-anesthesia care unit
- PCIA =
- patient-controlled intravenous analgesia;
- PONV =
- postoperative nausea and vomiting
- POST =
- postoperative sore throat
- PP =
- prone position
- QES =
- quasi-experimental study
- RCT =
- randomized controlled trial
- SP =
- supine position
- SSL =
- spring single lumen
- TEAS =
- transcutaneous electrical acupoint stimulation
- TENS =
- transcutaneous electrical nerve stimulation
- NSL =
- normal single lumen
- VAS =
- Visual Analogue Scale
Posted history: The earliest manuscript was previously posted to medRxiv: doi: https://doi.org/10.1101/2020.07.11.20148544
How to cite this article: Jau P-Y, Chang S-C. The effectiveness of acupuncture point stimulation for the prevention of postoperative sore throat: a meta-analysis. Medicine 2022;101:28(e29653).
Ethics approval: Not required for this study.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental Digital Content is available for this article.
The author(s) of this work have nothing to disclose.
References
- [1].McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999;54:444–53. [DOI] [PubMed] [Google Scholar]
- [2].Lee JY, Sim WS, Kim ES, et al. Incidence and risk factors of postoperative sore throat after endotracheal intubation in Korean patients. J Int Med Res. 2017;45:744–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Shrestha S, Maharjan B, Karmacharya RM. Incidence and associated risk factors of postoperative sore throat in tertiary care hospital. Kathmandu Univ Med J (KUMJ). 2017;15:10–3. [PubMed] [Google Scholar]
- [4].Piriyapatsom A, Dej-Arkom S, Chinachoti T, et al. Postoperative sore throat: incidence, risk factors, and outcome. J Med Assoc Thai. 2013;96:936–42. [PubMed] [Google Scholar]
- [5].Lehmann M, Monte K, Barach P, et al. Postoperative patient complaints: a prospective interview study of 12,276 patients. J Clin Anesth. 2010;22:13–21. [DOI] [PubMed] [Google Scholar]
- [6].Tong D, Chung F, Wong D. Predictive factors in global and anesthesia satisfaction in ambulatory surgical patients. Anesthesiology. 1997;87:856–64. [DOI] [PubMed] [Google Scholar]
- [7].Jaensson M, Gupta A, Nilsson U. Gender differences in sore throat and hoarseness following endotracheal tube or laryngeal mask airway: a prospective study. BMC Anesthesiol. 2014;14:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Myles PS, Williams DL, Hendrata M, et al. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84:6–10. [DOI] [PubMed] [Google Scholar]
- [9].Miskovic A, Johnson M, Frost L, et al. A prospective observational cohort study on the incidence of postoperative sore throat in the pediatric population. Paediatr Anaesth. 2019;29:1179–85. [DOI] [PubMed] [Google Scholar]
- [10].Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. 2002;88:582–4. [DOI] [PubMed] [Google Scholar]
- [11].Moningi S, Patki A, Padhy N, et al. Enhanced recovery after surgery: an anesthesiologist’s perspective. J Anaesthesiol Clin Pharmacol. 2019;35:S5–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Flexman AM, Duggan LV. Postoperative sore throat: inevitable side effect or preventable nuisance? Can J Anaesth. 2019;66:1009–13. [DOI] [PubMed] [Google Scholar]
- [13].Chandler M. Tracheal intubation and sore throat: a mechanical explanation. Anaesthesia. 2002;57:155–61. [DOI] [PubMed] [Google Scholar]
- [14].Combes X, Schauvliege F, Peyrouset O, et al. Intracuff pressure and tracheal morbidity: influence of filling with saline during nitrous oxide anesthesia. Anesthesiology. 2001;95:1120–4. [DOI] [PubMed] [Google Scholar]
- [15].Honarmand A, Safavi M. Beclomethasone inhaler versus intravenous lidocaine in the prevention of postoperative airway and throat complaints: a randomized, controlled trial. Ann Saudi Med. 2008;28:11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kuriyama A, Maeda H. Preoperative intravenous dexamethasone prevents tracheal intubation-related sore throat in adult surgical patients: a systematic review and meta-analysis. Can J Anaesth. 2019;66:562–75. [DOI] [PubMed] [Google Scholar]
- [17].Kuriyama A, Aga M, Maeda H. Topical benzydamine hydrochloride for prevention of postoperative sore throat in adults undergoing tracheal intubation for elective surgery: a systematic review and meta-analysis. Anaesthesia. 2018;73:889–900. [DOI] [PubMed] [Google Scholar]
- [18].Kuriyama A, Maeda H, Sun R, et al. Topical application of corticosteroids to tracheal tubes to prevent postoperative sore throat in adults undergoing tracheal intubation: a systematic review and meta-analysis. Anaesthesia. 2018;73:1546–56. [DOI] [PubMed] [Google Scholar]
- [19].Yang SS, Wang N-N, Postonogova T, et al. Intravenous lidocaine to prevent postoperative airway complications in adults: a systematic review and meta-analysis. Br J Anaesth. 2020;124:314–23. [DOI] [PubMed] [Google Scholar]
- [20].Kuriyama A, Nakanishi M, Kamei J, et al. Topical application of ketamine to prevent postoperative sore throat in adults: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 2020;64:579–91. [DOI] [PubMed] [Google Scholar]
- [21].Kuriyama A, Maeda H, Sun R. Topical application of magnesium to prevent intubation-related sore throat in adult surgical patients: a systematic review and meta-analysis. Can J Anaesth. 2019;66:1082–94. [DOI] [PubMed] [Google Scholar]
- [22].Wu M-S, Chen K-H, Chen I-F, et al. The efficacy of acupuncture in post-operative pain management: a systematic review and meta-analysis. PLoS One. 2016;11:e0150367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tan H, Tumilty S, Chapple C, et al. Understanding acupoint sensitization: a narrative review on phenomena, potential mechanism, and clinical application. Evid Based Complement Alternat Med. 2019;2019:6064358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chernyak GV, Sessler DI. Perioperative acupuncture and related techniques. Anesthesiology. 2005;102:1031–49; quiz 1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Jun M-H, Kim Y-M, Kim JU. Modern acupuncture-like stimulation methods: a literature review. Integr Med Res. 2015;4:195–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ivanov A. The analogy between the traditional Chinese acupuncture and phlebotomy in medieval bohemia. J Acupunct Meridian Stud. 2019;12:136–44. [DOI] [PubMed] [Google Scholar]
- [27].Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons, 2019. [Google Scholar]
- [28].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- [30].Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12:55–61. [DOI] [PubMed] [Google Scholar]
- [32].Sweeting MJ, Sutton AJ, Lambert PC. What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med. 2004;23:1351–75. [DOI] [PubMed] [Google Scholar]
- [33].Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Luo D, Wan X, Liu J, et al. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805. [DOI] [PubMed] [Google Scholar]
- [35].Röver C, Knapp G, Friede T. Hartung-Knapp-Sidik-Jonkman approach and its modification for random-effects meta-analysis with few studies. BMC Med Res Methodol. 2015;15:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Lee A, Chan SKC, Fan LTY. Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2015;2015:CD003281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Park HS, Kim KS, Min HK, et al. Prevention of postoperative sore throat using capsicum plaster applied at the Korean hand acupuncture point. Anaesthesia. 2004;59:647–51. [DOI] [PubMed] [Google Scholar]
- [38].Esmaeili S, Alizadeh R, Shoar S, et al. Acupuncture in preventing postoperative anaesthesia-related sore throat: a comparison with no acupuncture. Acupunct Med. 2013;31:272–5. [DOI] [PubMed] [Google Scholar]
- [39].Wang D, Ma T, Li G, et al. Effects of transcutaneous electrical acupoint stimulation on treatment and prevention of postoperative sore throat after tracheal intubation under general anesthesia. Zhongguo Zhen Jiu. 2017;37:701–4. [DOI] [PubMed] [Google Scholar]
- [40].Pan LP, Yang Y, Shao J, et al. Effects of perioperative transcutaneous electrical acupoint stimulation on postoperative analgesia in patients undergoing shoulder arthroscopic surgery. Zhongguo Zhen Jiu. 2019;39:19–23. [DOI] [PubMed] [Google Scholar]
- [41].Lu X-H, Zhang X-M, Liu S-L, et al. Clinical research on prevention and treatment of respiratory tract complications with acupoint application after operation under general anesthesia. J Craniofac Surg. 2019;30:e85–92. [DOI] [PubMed] [Google Scholar]
- [42].McDonald JL, Cripps AW, Smith PK, et al. The anti-inflammatory effects of acupuncture and their relevance to allergic rhinitis: a narrative review and proposed model. Evid Based Complement Alternat Med. 2013;2013:591796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Tsuchiya M, Sato EF, Inoue M, et al. Acupuncture enhances generation of nitric oxide and increases local circulation. Anesth Analg. 2007;104:301–7. [DOI] [PubMed] [Google Scholar]
- [44].Leung L. Neurophysiological basis of acupuncture-induced analgesia—an updated review. J Acupunct Meridian Stud. 2012;5:261–70. [DOI] [PubMed] [Google Scholar]
- [45].Joshi GP, Kehlet H. Postoperative pain management in the era of ERAS: an overview. Best Pract Res Clin Anaesthesiol. 2019;33:259–67. [DOI] [PubMed] [Google Scholar]
- [46].Liu X-L, Tan J-Y, Molassiotis A, et al. Acupuncture-point stimulation for postoperative pain control: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2015;2015:657809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Fan AY, Miller DW, Bolash B, et al. Acupuncture’s role in solving the opioid epidemic: evidence, cost-effectiveness, and care availability for acupuncture as a primary, non-pharmacologic method for pain relief and management-white paper 2017. J Integr Med. 2017;15:411–25. [DOI] [PubMed] [Google Scholar]
- [48].Kaye AD, Granier AL, Garcia AJ, et al. Non-opioid perioperative pain strategies for the clinician: a narrative review. Pain Ther. 2020;9:25–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Lu Z, Dong H, Wang Q, et al. Perioperative acupuncture modulation: more than anaesthesia. Br J Anaesth. 2015;115:183–93. [DOI] [PubMed] [Google Scholar]
- [50].Asmussen S, Maybauer DM, Chen JD, et al. Effects of acupuncture in anesthesia for craniotomy: a meta-analysis. J Neurosurg Anesthesiol. 2017;29:219–27. [DOI] [PubMed] [Google Scholar]
- [51].Asmussen S, Przkora R, Maybauer DM, et al. Meta-analysis of electroacupuncture in cardiac anesthesia and intensive care. J Intensive Care Med. 2019;34:652–61. [DOI] [PubMed] [Google Scholar]
- [52].Yoo J-E, Oh D-S. Potential benefits of acupuncture for enhanced recovery in gynaecological surgery. Forsch Komplementmed. 2015;22:111–6. [DOI] [PubMed] [Google Scholar]
- [53].Yuan W, Wang Q. Perioperative acupuncture medicine: a novel concept instead of acupuncture anesthesia. Chin Med J. 2019;132:707–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.