Abstract
Retrospective study.
The purpose of this study was to investigate the clinical symptomatology of discopathies before and 7 days after treatment with one of the following: intravenous dexamethasone, selective nerve root block (SNRB), and systemic treatment with different nonsteroidal antiinflammatory drugs (NSAIDs).
Radiculopathy is a clinical condition in which dysfunction of one or more nerves occurs due to mechanical compression and/or chemical irritation of the nerve roots. Most often located in the lumbar spine, radiculopathy remains one of the most common complaints in primary health. Some patients responded well to conservative treatment. However, those who show no improvement may benefit from more invasive treatment options, such as intravenous corticosteroids, spinal injections, and surgical procedures.
We conducted a retrospective study of 81 male and female patients aged 18 years and above who had radicular pain and were referred to our facility over a 7-year period. Of the 100 patients assessed for eligibility, 19 patients were not included in the study due to malignancy or surgical intervention, 32 patients received intravenous dexamethasone, 24 patients received SNRB, and 25 received various NSAIDs as the control group. The visual analog scale, straight leg raise test and neurological deficits were assessed to evaluate the patients before and after receiving treatment. All patients underwent spinal computed tomography to confirm the diagnosis of disc herniation. Pearson chi-squared test, Kruskal–Wallis test, and Mann–Whitney test were used to evaluate the results.
Visual analog scale scores and the ability to perform straight leg raise test significantly improved after treatment with dexamethasone, SNRB, and NSAIDs. However, clinical improvement was significantly better in both the dexamethasone and SNRB groups than in the control group. Motor deficits improved significantly after dexamethasone treatment alone.
Dexamethasone and SNRB are useful and safe treatment options for treating patients with acute radicular pain. Randomized, double-blinded, control studies are warranted.
Keywords: dexamethasone, NSAID drugs, pain, phospholipase A2, radiculopathies, SNRB
1. Introduction
Approximately two-thirds of adults suffer from neck and low-back pain. Axial spine pain is often accompanied by radicular pain or radiculopathy, which is defined as spinal nerve root dysfunction causing dermatomal pain and paresthesia, weakness of muscles innervated by the affected root, and/or impaired deep tendon reflexes.[1] This common neurological syndrome is an important source of disability and a costly medical condition due to the expenditure associated with repeated treatments, long-term absence from work, and the need for social support.[2–4]
Radiculopathies can affect any level of the spinal column; however, the most common locations are the lumbar and cervical spine. Radiculopathies are precipitated by chemical irritation, chronic pressure, or mechanical compression exerted on the root in or bordering the spinal column, which can also lead to inadequate blood supply.[5] The intervertebral disc has been identified as the leading cause of low-back pain with radiculopathy.[6]
General risk factors for radiculopathy usually include activities with excessive or repetitive loads on the spine, such as lifting heavy loads, improper lifting techniques, or contact sports. Prolonged and repetitive sitting, especially while driving, may lead to disc compression along with vibrational damage. Over time, the accumulated damage can evolve into disc herniation. Smoking, chronic cough, and pregnancy are also risk factors.[7]
Radiculopathies are usually characterized by sharp and burning pain that is difficult to localize, numbness, tingling, muscle weakness, impaired reflexes, and limited motion.[2]
To establish the diagnosis and management, patients with radicular symptoms are usually investigated using computed tomography (CT) or magnetic resonance imaging (MRI) of the affected area. Clinicians must be aware of asymptomatic disc herniation, which is a common incidental imaging finding. Therefore, a correlation between symptoms and radiographic abnormalities is required before considering any invasive procedures.[8]
Lumbar disc herniation remains among the most common diagnoses encountered in clinical practice. The incidence of symptomatic lumbar disc herniations in the American population has been estimated to be 1% to 2%, for which approximately 200,000 lumbar discectomies are performed annually.[9] The lifetime prevalence of low-back pain is reported to be >70% in industrialized countries (1-year prevalence 15%–45%, adult incidence 5% per year). Peak prevalence occurs between the ages of 35 and 55 years.[10] Despite the frequency of lumbar disc herniation, there is substantial controversy regarding its pathophysiology. From the standpoint of basic science, mounting evidence suggests that both biochemical and mechanical factors are responsible for the development of symptomatic radiculopathy; however, their involvement in the pathophysiology of radiculopathy remains poorly understood.[7] Radicular pain seems to be mediated by inflammatory mechanisms involving substances such as phospholipase A2 (PLA2), nitric oxide, and prostaglandin E2. PLA2 has been demonstrated to be released by intervertebral discs following injury. This enzyme acts on cell membranes to release arachidonic acid, a precursor to other prostaglandins and leukotrienes, which further promotes the inflammatory response.[11,12]
The rationale for using noninvasive procedures in the treatment of radiculopathies is that radicular pain is caused by local inflammation secondary to disc injury or herniation, and that accurate injection of corticosteroids directly into the affected nerve should theoretically suppress the function of PLA2, thereby decreasing the inflammation around the nerve roots and relieving pain.[12,13] While many adverse effects are associated with systemic steroid use, these are more frequently encountered in the setting of prolonged administration.[14]
Radiculopathies treatment is divided into 3 phases according to the severity of the clinical and neurological presentations. In the case of tolerable symptoms, conservative medical treatment including oral medications [acetaminophen, nonsteroidal antiinflammatory drugs (NSAIDs)] and physical measures such as immobilization, heat and cold therapy, electrical stimulation, and stretching exercises are sufficient. Invasive procedures, such as epidural steroid injection, are performed if neurologic deficits are progressive or severe. Nevertheless, there is no agreed standard therapy for radiculopathy.
Immediate surgical intervention (discectomy, laminectomy) should be conducted if the spinal cord is compressed, such as in patients with cauda equina syndrome and those with radiculopathy causing marked or progressive muscle weakness. In most other cases, surgery is advised only after rest, physical therapy, and medications have failed to adequately relieve the symptoms over a significant period of time.[2]
The purpose of this study was to retrospectively assess the clinical symptomatology of discopathies before and after receiving one of the following treatments: intravenous administration of dexamethasone, selective nerve root block (SNRB), or NSAIDs.
2. Methods
2.1. Data assessment
Cases were selected over a 7-year period (2013–2020) from computerized medical files of patients comprising men and women aged 18 and above attending the emergency department due to radicular pain. Patients were assessed in emergency department by an orthopedic surgeon or a neurologist. As there is no standard treatment protocol for radiculopathy except criteria for surgical treatment, the treatment they received was based on a case-by-case clinical decision of the treating doctors in emergency room and/or orthopedic or neurologist in the departments concerning their treatment. Personal details remained confidential. This retrospective study was conducted at the Ziv Medical Center after obtaining approval from our institutional review board (0100-16-ZIV). This study adhered to the STROBE statement. All relevant data are within the paper and its supporting information files.
2.2. Outcomes to be measured
The clinical symptomatology of discopathies was evaluated before and after receiving treatment with one of the following: NSAIDs were given to all patients presenting to the emergency room. In addition to NSAIDs, some patients were administered intravenous dexamethasone (30 mg for 3 days, tapering off 10 mg daily) or SNRB, based on a case-by-case decision. Therefore, we considered patients who received NSAIDs only (diclofenac 100 mg once a day or ibuprofen 200 mg twice a day) as a control group. SNRB [Depomedrol (80 mg methylprednisolone) + 0.5% bupivacaine] was injected to the implicated root using X-Ray device (Siemens Arcadis Orbic 3D, C-arm) scan imaging. The inclusion criteria included patients aged 18 years and older who were examined in the emergency room due to lower back pain with acute radicular features. All included patients underwent spinal CT, which confirmed the herniated discopathy. Only patients with L4-L5 and L5-S1 discopathy were included. Patients with active malignancy, infection, discopathy at a different level or penetrating trauma were excluded from the study. Patients who met the indications for surgical treatment (patients with cauda equina syndrome and those with radiculopathy causing marked or progressive muscle weakness) were also excluded.
Visual analog scale (VAS) and straight leg raise (SLR) are simple and frequently used methods for assessing variations in pain intensity variations. The VAS is a validated scale used to measure the practice, and the percentage of pain relief is a measure of the efficacy of treatment. In the SLR test, radicular leg pain produced between 30° and 70° of leg elevation is a strong indicator of herniated disc as the generator of pain. The pain was especially worsened by ankle dorsiflexion. This examination is approximately 91% sensitive to a herniated disc.[15] Neurological deficits (motor, sensory, and reflex) were also measured to evaluate the patients before and after treatment. Patients with motor weakness more severe than 4 of 5 degrees of strength were excluded as they were candidates for surgical treatments. All patients included in this study were examined twice: prior to treatment and 7 days following treatment.
2.3. Statistical analysis
For categorical variables, summary tables provide sample sizes and frequencies, and arithmetic mean (M) and standard deviation for continuous variables. The Pearson chi-squared test was used to test the correlations between the study groups for categorical parameters. Kruskal–Wallis nonparametric tests were applied to measure the differences between the study groups (control, dexamethasone, and SNRB), while Mann–Whitney nonparametric tests were applied to measure the differences between the time of measurement in each group (before vs after). Differences between the 3 groups in VAS and SLR were measured overall and stratified by age (45 and under and over 45). A P-value of ≤5% or less was considered statistically to be significant. Data were analyzed using SPSS version 25 (SPSS Inc., Chicago, IL).
3. Results
Demographics, clinical symptomatology, prior medical history including outpatient medications, prior level of renal function, comorbidities, length of mechanical ventilation, and hospital stay were collected.
Of the 100 patients assessed for eligibility, 19 were not included in the study due to malignancy or surgical intervention. Eighty-one patients aged 18 years and older, who were transferred to the emergency department due to radicular pain, met the eligibility criteria and have been included in the study: 32 patients received i.v. dexamethasone, 24 patients received SNRB, and 25 received various NSAIDs as control group.
No significant differences in age and/or sex were found between the 3 groups. A statistically significant effect was found in the duration of disease symptoms; both groups treated with SNRB or with dexamethasone had a longer duration of symptoms compared to the NSAIDs group, while the longest duration was observed in those treated with SNRB (Table 1).
Table 1.
Demographic and clinical characteristics of the patients.
| Variables | Control (n = 25) | Dexamethasone (n = 32) | SNRB (n = 24) | P |
|---|---|---|---|---|
| Gender, male (n, %) | 16, 64.0 | 24, 75.0 | 18, 75.0 | .598 |
| Age, y (mean ± SD) | 45.5 ± 11.3 | 44.3 ± 12.4 | 45.0 ± 11.6 | .929 |
| Duration days (mean ± SD) | 10.3b ± 15.5 | 22.3ab ± 23.4 | 36.8a ± 33.1 | .002 |
a-b: different letters in each row represent significant differences between the means.
SD = standard deviation, SNRB = selective nerve root block.
The VAS score and the ability to perform SLR after treatment with dexamethasone, SNRB, and NSAIDs greatly improved (P < .001) (Table 2).
Table 2.
Clinical characteristics of the patients.
| Variables and group | Time | Control | Dexamethasone | SNRB | P |
|---|---|---|---|---|---|
| VAS score, 1–10 (mean ± SD) | |||||
| All ages | Before | 7.6 ± 1.6 | 7.7 ± 1.7 | 7.3 ± 1.6 | .681 |
| After | 4.7a ± 2.4 | 2.8b ± 2.3 | 2.3b ± 1.9 | .001 | |
| P * | <.001 | <.001 | <.001 | ||
| Age ≤ 45 y | Before | 7.1 ± 2.1 | 7.9 ± 1.7 | 7.3 ± 1.6 | .141 |
| After | 4.1 ± 2.6 | 2.9 ± 2.4 | 2.2 ± 1.9 | .225 | |
| P * | .005 | <.001 | .003 | ||
| Age > 45 y | Before | 8.0 ± 0.8 | 7.5 ± 1.7 | 7.4 ± 1.6 | .775 |
| After | 5.3a ± 2.3 | 2.7b ± 2.4 | 2.5b ± 1.9 | .017 | |
| P * | .041 | <.001 | .001 | ||
| SLR score (mean ± SD) | |||||
| All ages | Before | 34.8 ± 16.1 | 32.2 ± 15.9 | 40.2 ± 18.0 | .204 |
| After | 44.8b ± 18.1 | 66.7a ± 18.7 | 72.3a ± 14.0 | <.001 | |
| P * | <.001 | <.001 | <.001 | ||
| Age ≤ 45 y | Before | 36.7 ± 16.7 | 34.4 ± 16.9 | 40.0 ± 19.4 | .624 |
| After | 47.5b ± 21.7 | 70.6a ± 19.4 | 71.8a ± 18.3 | .006 | |
| P * | .003 | <.001 | .001 | ||
| Age > 45 y | Before | 33.1 ± 16.0 | 29.7 ± 14.7 | 40.4 ± 17.6 | .264 |
| After | 42.3b ± 14.2 | 62.3a ± 17.4 | 72.7a ± 9.7 | <.001 | |
| P * | .006 | <.001 | .002 | ||
a-b: different letters in each row represent significant differences between the means.
SD = standard deviation, SLR = straight leg raise test, SNRB = selective nerve root block, VAS = visual analog scale.
Comparison between time of measurement in each group.
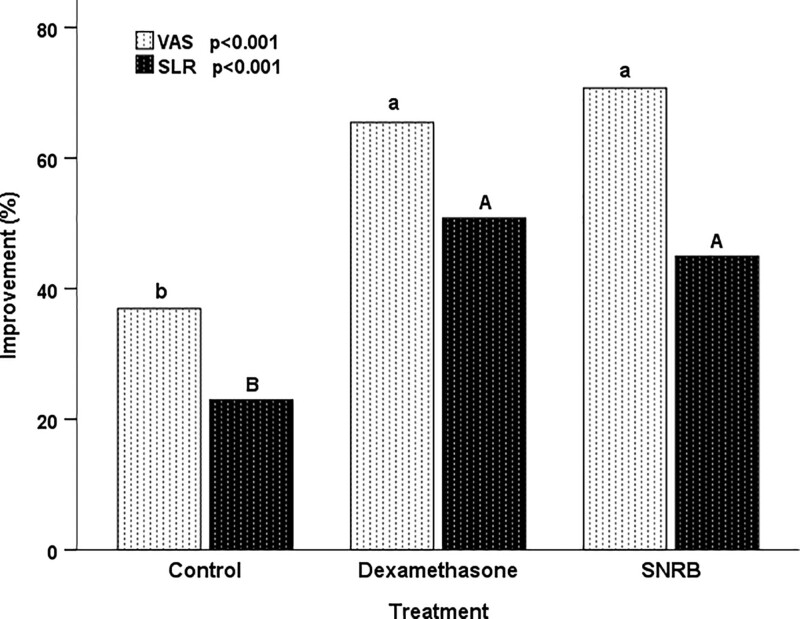
Both groups treated with SNRB and dexamethasone showed an improvement in VAS and SLR compared to the control (P < .001) (Fig. 1). For SLR this was the case for both age groups while for VAS it was only the case in those over the age of 45 (Table 2).
Figure 1.
Improvement in VAS and SLR in the study population. Both groups treated with SNRB and dexamethasone showed an improvement in VAS and SLR compared to the control (P < .001). SLR = straight leg raise, VAS = visual analog scale.
There were no changes before and after treatment in the proportion experiencing sensory or reflexes deficits, but 10 of 15 patients in the group of dexamethasone who had motor deficits greatly improved (Table 3).
Table 3.
Distribution of neurological deficits in the study population.
| Variables and group | Time | Control | Dexamethasone | SNRB | P |
|---|---|---|---|---|---|
| Motor, yes (n, %) | |||||
| All ages | Before | 6, 24.0 | 15, 46.9* | 8, 33.3 | .193 |
| After | 7, 28.0 | 5, 15.6 | 8, 33.3 | .283 | |
| Age ≤ 45 y | Before | 2, 16.7 | 9, 52.9 | 5, 45.5 | .140 |
| After | 3, 25.0 | 3, 17.6 | 5, 45.5 | .298 | |
| Age > 45 y | Before | 4, 30.8 | 6, 40.0 | 3, 23.1 | .645 |
| After | 4, 30.8 | 2, 13.3 | 3, 23.1 | .575 | |
| Sensory, yes (n, %) | |||||
| All ages | Before | 21, 84.0 | 24, 75.0 | 17, 70.8 | .540 |
| After | 21, 84.0 | 24, 75.0 | 15, 62.5 | .238 | |
| Age ≤ 45 y | Before | 8, 66.7 | 12, 70.6 | 6, 54.5 | .678 |
| After | 8, 66.7 | 12, 70.6 | 5, 45.5 | .382 | |
| Age > 45 y | Before | 13, 100 | 12, 80.0 | 11, 84.6 | .343 |
| After | 13, 100 | 12, 80.0 | 10, 76.9 | .279 | |
| Reflexes, yes (n, %) | |||||
| All ages | Before | 6, 24.0 | 7, 21.9 | 5, 20.8 | .963 |
| After | 6, 24.0 | 6, 18.8 | 5, 20.8 | .890 | |
| Age ≤ 45 y | Before | 3, 25.0 | 2, 11.8 | 2, 18.2 | .868 |
| After | 3, 25.0 | 2, 11.2 | 2, 18.2 | .868 | |
| Age > 45 y | Before | 3, 23.1 | 5, 33.3 | 3, 23.1 | .823 |
| After | 3, 23.1 | 4, 26.7 | 3, 23.1 | .967 | |
SNRB = selective nerve root block.
P = .015, comparison between time of measurement in the dexamethasone group.
4. Discussion
Low-back pain combined with radicular pain remains one of the most challenging musculoskeletal problems for its diagnostic and therapeutic management because multilevel abnormalities are common, and a number of spinal and paraspinal structures may contribute to the pain syndrome. The facet joints, vertebral bodies, nerve roots, and local nociceptors are potential pain generators. Discogenic pain due to degenerative lumbar disc disease is recognized as another cause of low-back pain.[16] Conservative treatment, percutaneous spine interventions, and surgery have all been used as treatment options. The treatment approach depends on the severity of clinical and neurological presentations. Any surgical decision should be based on clinical symptoms and corroborate the results of the diagnostic testing. Indications for surgical referral include the following: cauda equina syndrome, progressive neurologic deficit, profound neurologic deficit, and severe and disabling pain refractory to 4 to 6 weeks of conservative treatment.[17] All patients for whom surgical intervention was indicated were excluded from this study. As there is no agreed standardization for radiculopathy treatment, we intended to perform this study.
This retrospective study provides an encouraging picture of the effectiveness of intravenous dexamethasone and SNRB for the treatment of diseases, as there is currently no other validated alternative.[18]
A particular focus has been given to the use of nonsurgical procedures as the first treatment option for radiculopathies. In fact, without any surgery, pain decreases in approximately 87% of patients within 3 months, and CT often reveals a significant reduction in herniation size and even complete resolution in 1 year.[6] Therefore, choosing surgical intervention as an initial treatment should be evaluated carefully.[19] Finding noninvasive treatments that alleviate pain and improve functional abilities may prevent unnecessary surgical interventions, thus allowing the herniation to regress.[20]
Many suggestions regarding the benefits of corticosteroids have been proposed. First, it is postulated that corticosteroids reduce inflammation either by inhibiting the synthesis or release of a number of proinflammatory substances or by causing a reversible local anesthetic effect.[21] Second, the administration of epidural solutions clears or dilutes chemical irritants. Corticosteroids are postulated to exert their effects through multiple modes, including membrane stabilization, inhibition of neural peptide synthesis or action, blockade of PLA2 activity, prolonged suppression of ongoing neuronal discharge, and suppression of sensitization of dorsal horn neurons.[22]
The philosophy of epidural steroid injections (ESIs) is based on the principle that the corticosteroid delivered into the epidural space achieves some higher local concentrations over an inflamed nerve root and will be more effective than a steroid administered either orally or by intramuscular injection.[23] Moreover, SNRB, which contains local anesthetic combined with corticosteroids, demonstrates even higher efficacy than epidural injections in the management of radiculopathy.[24]
The role of corticosteroids in the treatment of radiculopathy from disc herniation is to significantly improve the disabling symptoms and neuroprotective effects on the involved nerve roots.[25,26] This documented efficacy, with a high safety margin, justifies their frequent use.[27] Controversies regarding the effectiveness of intravenous administration of dexamethasone in the treatment of radiculopathy have been reported. A prospective double-blind study showed that dexamethasone is not superior to placebo for either short- or long-term relief of lumbosacral radicular pain.[28] However, due to inconsistencies, internal contradictions, and lack of statistical value, their study cannot be conclusive. Myelograms were not performed on all patients, analgesics were received by both the dexamethasone and placebo groups, and the number of patients was too small. In a recent systematic review, the recommendation to treat systemic steroids was determined to be of low level of evidence and weak strength of recommendation. This is attributed to the paucity of well-designed randomized controlled trials, a small number of patients, variable follow-up periods, conflicting results regarding pain reduction versus functional improvement, and the heterogeneity of subjects across the selected randomized controlled trials.[29]
With the injection of long-acting anesthetic and steroids, SNRB can provide pain relief of variable duration in most patients with nerve root compression, typically in the setting of acute herniated nucleus pulposus. Radicular pain may be exacerbated by injection adjacent to the target nerve root, and concordant-elicited pain predicts a high likelihood of success with therapeutic injection. Peripheral numbness may occur, but should resolve within 2 to 3 hours as the effect of the long-acting anesthetic diminished. Motor weakness is rare with 0.25% bupivacaine and is still uncommon with 0.50% bupivacaine. If this occurs, motor weakness should also resolve within 2 to 3 hours. Patients are usually discharged 30 to 60 minutes after SNRB if they have no motor weakness. None of our patients experienced motor weakness during or after SNRB.
Our study challenges the current prevalent perception, in which treatment with systemic corticosteroids for acute radiculopathy is considered uncommon in clinical practice due to previous inconclusive data.[29–31] We demonstrated that both intravenous dexamethasone and SNRB are useful and safe treatment options for acute radicular pain as they lead to significant improvement in VAS and SLR compared to NSAIDs (Fig. 1). Furthermore, i.v. dexamethasone was superior to SNRB in the motor neurological deficit domain (Table 3).
The key strengths of our study include the correlation of both clinical and radiological findings for effective and accurate diagnosis, high adherence to the intervention and follow-up, and the use of several different assessment tools to evaluate treatment efficacy.
There are several potential limitations to this study. First, the outcomes will be more validated and accurate with a larger sample size. Second, long-term follow-up is required to further evaluate treatment efficacy in the long term. Randomized, double-blinded control studies based on pathologic and therapeutic homogenous groups, are warranted to determine the immediate and late effects of these treatments.
Author contributions
Individual contribution to the manuscript: Radi Shahien designed the study. Karine Beiruti Wiegler wrote the protocol and the manuscript. Saad Abu Saleh and Lior Dekel managed the literature searches and conducted the clinical part of the study. Adi Sharabi-Nov took care of the statistical analysis. Radi Shahien and Karine Beiruti Wiegler reviewed the manuscript.
Abbreviations:
- CT =
- computed tomography
- M =
- mean
- MRI =
- magnetic resonance imaging
- NSAIDs =
- nonsteroidal antiinflammatory drugs
- PLA2 =
- phospholipase A2
- SD =
- standard deviation
- SLR =
- straight leg raise test
- SNRB =
- selective nerve root block
- VAS =
- visual analog scale
The datasets generated during and/or analyzed during the current study are publicly available.
The study was approved by the Ethics Committee of Ziv Medical Center (0100-16-ZIV). The authors state that the study was performed at the hospital without any external help. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors declare no conflicts of interest.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Shahien R, Wiegler KB, Dekel L, Sharabi-Nov A, Abu Saleh S. Retrospective study assessing the efficacy of i.v. dexamethasone, SNRB and nonsteroidal treatment for radiculopathy. Medicine 2022;101:28(e29272).
Contributor Information
Karine Beiruti Wiegler, Email: 8082424@gmail.com.
Lior Dekel, Email: liordekel3@gmail.com.
Adi Sharabi-Nov, Email: adi_nov@hotmail.com.
Saad Abu Saleh, Email: saadabusaleh@ziv.gov.il.
References
- [1].Richter KJ, Chodoroff G. Steroids for lumbar radiculopathy. Neurology. 1987;37:1689–1689. [PubMed] [Google Scholar]
- [2].Atlas SJ, Nardin RA. Evaluation and treatment of low back pain: an evidence-based approach to clinical care. Muscle Nerve. 2003;27:265–84. [DOI] [PubMed] [Google Scholar]
- [3].Corwell BN. The emergency department evaluation, management, and treatment of back pain. Emerg Med Clin North Am. 2010;28:811–39. [DOI] [PubMed] [Google Scholar]
- [4].Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007;25:387–405. [DOI] [PubMed] [Google Scholar]
- [5].O’Connor RC, Andary MT, Russo RB, et al. Thoracic radiculopathy. Phys Med Rehabil Clin N Am. 2002;13:623–44, viii. [DOI] [PubMed] [Google Scholar]
- [6].Huang R, Meng Z, Cao Y, et al. Nonsurgical medical treatment in the management of pain due to lumbar disc prolapse: a network meta-analysis. Paper presented at: Seminars in arthritis and rheumatism. 2019;45:303–13. [DOI] [PubMed] [Google Scholar]
- [7].Rhee JM, Schaufele M, Abdu WA. Radiculopathy and the herniated lumbar disc. Controversies regarding pathophysiology and management. J Bone Joint Surg Am. 2006;88:2070–80. [DOI] [PubMed] [Google Scholar]
- [8].Carragee EJ, Barcohana B, Alamin T, et al. Prospective controlled study of the development of lower back pain in previously asymptomatic subjects undergoing experimental discography. Spine (Phila Pa 1976). 2004;29:1112–7. [DOI] [PubMed] [Google Scholar]
- [9].Taylor VM, Deyo RA, Cherkin DC, et al. Low back pain hospitalization. Recent United States trends and regional variations. Spine (Phila Pa 1976). 1994;19:1207–12; discussion 13. [DOI] [PubMed] [Google Scholar]
- [10].Andersson G. The adult spine: principles and practice JW F, ed. In: The Epidemiology of Spinal Disorders. New York: Raven Press, 1997:93–141. [Google Scholar]
- [11].Derby R, Chen Y, Lee SH, et al. Non-surgical interventional treatment of cervical and thoracic radiculopathies. Pain Physician. 2004;7:389–94. [PubMed] [Google Scholar]
- [12].Kang JD, Georgescu HI, McIntyre-Larkin L, et al. Herniated cervical intervertebral discs spontaneously produce matrix metalloproteinases, nitric oxide, interleukin-6, and prostaglandin E2. Spine (Phila Pa 1976). 1995;20:2373–8. [DOI] [PubMed] [Google Scholar]
- [13].Furusawa N, Baba H, Miyoshi N, et al. Herniation of cervical intervertebral disc: immunohistochemical examination and measurement of nitric oxide production. Spine (Phila Pa 1976). 2001;26:1110–6. [DOI] [PubMed] [Google Scholar]
- [14].Malanga G, Nadler S, Lipetz J. Pharmacologic treatment of low back pain. Physical medicine and rehabilitation. 1999;13:531–50. [Google Scholar]
- [15].Devillé WL, van der Windt DA, Dzaferagic A, et al. The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine. 2000;25:1140–7. [DOI] [PubMed] [Google Scholar]
- [16].Zoarski GH, Johnson BA, Ortiz AA, et al. Treating low back pain with spinal injections. Practic Approaches Comm Clinical Cond. 2010;194:194–205. [Google Scholar]
- [17].Humphreys SC, Eck JC. Clinical evaluation and treatment options for herniated lumbar disc. Am Fam Physician. 1999;59:575–82, 587. [PubMed] [Google Scholar]
- [18].Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bush K, Chaudhuri R, Hillier S, et al. The pathomorphologic changes that accompany the resolution of cervical radiculopathy. A prospective study with repeat magnetic resonance imaging. Spine (Phila Pa 1976). 1997;22:183–6; discussion 187. [DOI] [PubMed] [Google Scholar]
- [20].Nozawa S, Nozawa A, Kojima H, et al. Spontaneous disappearance of lumbar disk herniation within 3 months. Orthopedics. 2009;32:852. [DOI] [PubMed] [Google Scholar]
- [21].Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician. 2002;5:182–99. [PubMed] [Google Scholar]
- [22].Botwin KP, Gruber RD, Bouchlas CG, et al. Complications of fluoroscopically guided caudal epidural injections. Am J Phys Med Rehabil. 2001;80:416–24. [DOI] [PubMed] [Google Scholar]
- [23].Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000;3:374–98. [PubMed] [Google Scholar]
- [24].Dhakal GR, Hamal PK, Dhungana S, et al. Clinical efficacy of selective nerve root block in lumbar radiculopathy due to disc prolapse. J Nepal Health Res Counc. 2019;17:242–6. [DOI] [PubMed] [Google Scholar]
- [25].Carette S, Leclaire R, Marcoux S, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336:1634–40. [DOI] [PubMed] [Google Scholar]
- [26].DePalma MJ, Bhargava A, Slipman CW. A critical appraisal of the evidence for selective nerve root injection in the treatment of lumbosacral radiculopathy. Arch Phys Med Rehabil. 2005;86:1477–83. [DOI] [PubMed] [Google Scholar]
- [27].Manchikanti L, Singh V, Kloth D, et al. Interventional techniques in the management of chronic pain: part 2.0. Pain Physician. 2001;4:24–96. [PubMed] [Google Scholar]
- [28].Haimovic IC, Beresford HR. Dexamethasone is not superior to placebo for treating lumbosacral radicular pain. Neurology. 1986;36:1593–4. [DOI] [PubMed] [Google Scholar]
- [29].Lee HM, Weinstein JN, Meller ST, et al. The role of steroids and their effects on phospholipase A2. An animal model of radiculopathy. Spine (Phila Pa 1976). 1998;23:1191–6. [DOI] [PubMed] [Google Scholar]
- [30].Finckh A, Zufferey P, Schurch M-A, et al. Short-term efficacy of intravenous pulse glucocorticoids in acute discogenic sciatica. A randomized controlled trial. Spine. 2006;31:377–81. [DOI] [PubMed] [Google Scholar]
- [31].Roncoroni C, Baillet A, Durand M, et al. Efficacy and tolerance of systemic steroids in sciatica: a systematic review and meta-analysis. Rheumatology. 2011;50:1603–11. [DOI] [PubMed] [Google Scholar]