Abstract
A 14-year-old male neutered domestic shorthair cat was admitted to the Veterinary Medical Center, University of Minnesota for evaluation of severe hind limb ataxia, atrophy and paresis. Diagnosis based on physical examination, neurological assessment and magnetic resonance imaging (MRI) was multifocal intervertebral disc disease (IVDD) with dorsal disc protrusion throughout the thoracic and cranial lumbar spine. The Oriental Medicine (OM) diagnosis (pattern identification) was painful obstruction (Bi) syndrome caused by phlegm-heat accumulation with blood stagnation in the spine. High dose prednisolone therapy (1.25 mg/kg PO, once daily) initially did not show any significant improvement in clinical signs. The cat was then treated with several modes of acupuncture treatment including dry needle acupuncture, electro-acupuncture and scalp acupuncture along with Tui-Na (hand manipulation in OM) and physical therapy. Significant improvements in mobility, proprioception and spinal posture were noticed and the cat was able to rise, walk and run 4 months after starting acupuncture treatments. This is the first case report of feline IVDD with multiple sites of disc compression which was successfully treated with several modes of acupuncture treatment.
A domestic shorthair neutered male cat was adopted as a stray 12 years ago. At that time, the cat tested positive for feline immunodeficiency virus, and had a slightly tilted head with mild ataxia in the hind limbs, however walking and jumping abilities were not seriously impaired. In addition, he showed a mildly prolapsed rectum. The cat had anterior uveitis in the left eye which later developed a cataract and glaucoma followed by enucleation.
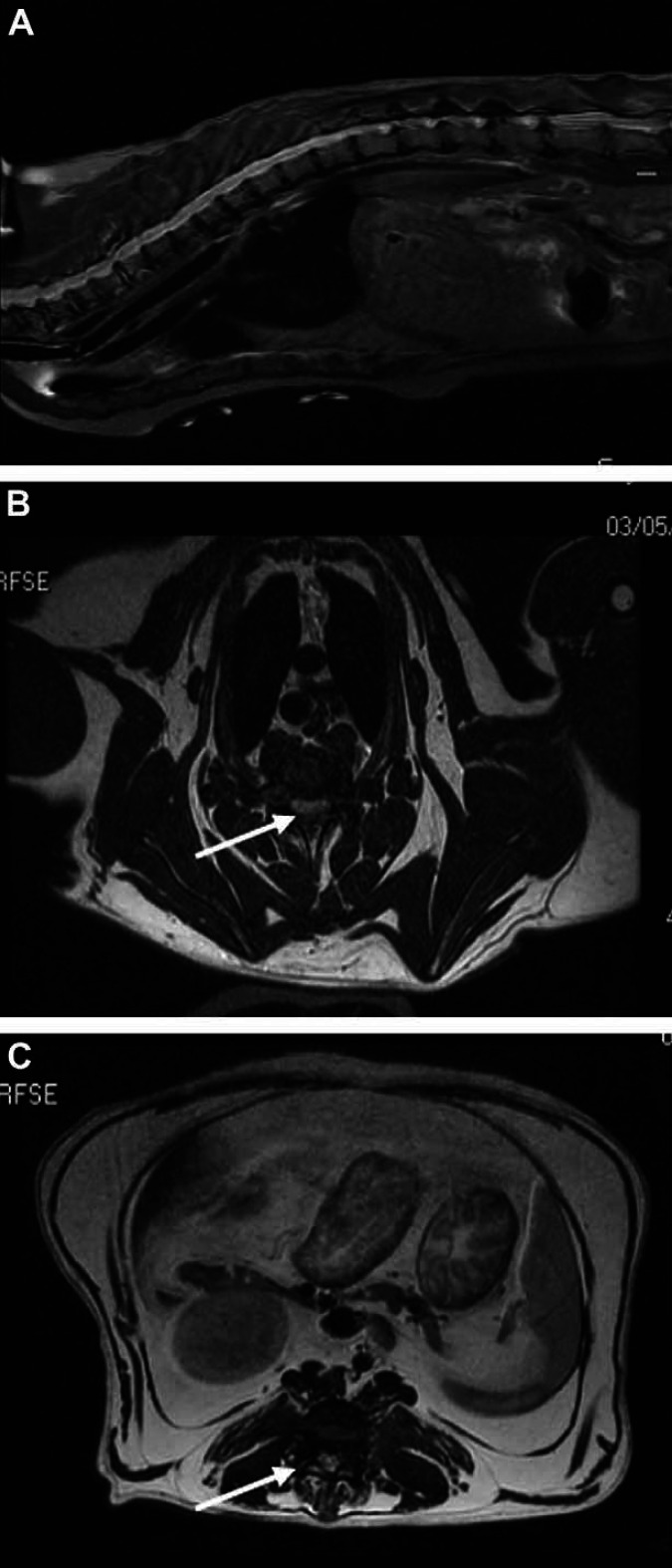
The cat developed acute onset of neurological deficits including marked ataxia, dragging of the hind limbs, inability to rise or stand, urinary accidents outside of the litter box and proprioceptive deficits 1 week before presentation to the Veterinary Medical Center, University of Minnesota. Magnetic resonance imaging (MRI) revealed loss of normal signal intensity and degeneration to most of the intervertebral discs (Fig 1A). Multiple areas of dorsal disc protrusion throughout the thoracic and cranial lumbar spine were noted. Spinal cord compression at intervertebral spaces from T2 to T6 (n=4) and from L2 to L5 (n=3) was more pronounced ( Fig 1 A). Severe compression by centrally protruding intervertebral disc material was remarkable at disc spaces T3–T4 ( Fig 1 B) and L3–L4 ( Fig 1 C).
Fig 1.
MRI of multifocal feline IVDD. (A) MRI of sagittal view at the level of the midline. (T2 SAG FS): multiples areas of disc protrusion and degeneration throughout the thoracic and cranial lumbar spine were noted. Spinal cord compression at intervertebral spaces from T2 to T6 (n=4) and from L2 to L5 (n=3) was more pronounced. (B) Transverse MRI (AX T2 FRFSE) of the most severe disc protrusion by centrally protruding intervertebral disc at T3–T4 intervertebral disc space. (C) Transverse MRI of the lumbar space disc protrusions at the L3–L4 intervertebral disc space (AX T2 FRFSE) and moderate severe compression by centrally protruding intervertebral disc from L3 to L4 was remarkable.
Due to the multiple sites of disc compression and ambiguity of specific areas contributing to the current acute onset episode, surgery was not a primary option. The cat was treated with prednisolone (1.25 mg/kg PO, once daily) in a tapering dose for alleviating spinal cord inflammation. Significant improvement was not noted within 10 days of prednisolone treatment, at which time, the cat was admitted to the Complementary and Alternative Medicine (CAM), Veterinary Medical Center, College of Veterinary Medicine, University of Minnesota for acupuncture treatment. When the cat presented to the CAM service, he was still dragging his hind limbs with severe ataxia and showed more than 90% proprioceptive deficits. The serum profiles of blood chemistry and complete blood counts were all in normal ranges. Four standard diagnostic methods in OM are observation, palpation, hearing/smelling, and inquiring. Pulse palpation and tongue profile are two unique techniques for pattern identification in OM. His femoral arterial pulse was deep in position, rapid, wiry and slightly choppy in quality bilaterally. The shape of the tongue body was puffy with a purplish red color. The tongue coating in the middle region was slightly greasy and gray in color. The physical examination, past history, MRI, palpation, and tongue and pulse profiles indicated that the cat's pattern identification, based on OM theory, was painful Bi syndrome due to phlegm-heat accumulation with blood stagnation in the spine.
Several modes of acupuncture treatment including low frequency electro-acupuncture (0.5 ms pulses, 2 Hz, 2–5 V, 1–4 mA), dry needle acupuncture using stainless steel acupuncture needle (30 gauge, 1 inch long was inserted to 0.5–1 Cun depth), and scalp acupuncture, where acupuncture needles (30 gauge, 1 inch long) are inserted transversely (15° angle) into leg motor sensory areas, 1 were performed for 5–10 min at each session once a week for 5 weeks then once every 2 weeks for six treatments. The acupuncture points included leg motor sensory areas of scalp acupuncture, Ba Feng, Yao Yan point, Hua Tuo Jia Ji points, stomach (ST)-36, ST-40, large intestine (LI)-11, governing vessel (GV)-2, GV-4, GV-14, GV-20, bladder (BL)-17, BL-35, BL-40, BL-60, gall bladder (GB)-21, GB-29, GB-30 and GB-34 (see Table 1). These acupuncture points were selected and combined differently in each session. Tui-Na using pinching the spine technique 2 was also provided for 10–15 min in each session.
Table 1.
The function and location of the selected acupuncture points
| Acupuncture points | Location | Function |
|---|---|---|
| Ba Feng | Dorsum of foot, proximal to the web margin, midway between 2nd and 3rd, 3rd and 4th, 4th and 5th toes in the depression distal to the metatarsophalangeal joint | Clears heat; alleviates pain and numbness of dorsum of foot and weakness of foot |
| BL-17 | 1.5 Cun lateral to the caudal border spinous process of T7 | Regenerates blood and dissipate blood stasis |
| BL-35 | The crease located just lateral to the tail base | Clears damp-heat, pain of coccyx, lumbar, and hind limbs |
| BL-40 | Midpoint of popliteal crease | Benefits lumbar, knees, lower limbs, sciatic pain; activates channels and alleviates pain |
| BL-60 | Depression between lateral malleolus and common calcanean tendon, level with the tip of lateral malleolus | Relaxes muscle spasm and stiff neck; strengthens lumbar spine |
| GB-21 | Midway between C7 and acromion | Alleviates pain; benefits stiffness in neck, shoulder, and back regions; eliminates phlegm; good for hemiplasia and wind-stroke |
| GB-29 | 1/3 distance between cranial/dorsal iliac spine and prominence of greater trochanter | Benefits hip and shoulder disorders; relaxes tendon or muscle spasms; relieves pain, numbness, weakness and sciatica pain |
| GB-30 | Midpoint between greater trochanter and tuber ischii | Relaxes spasms of tendons/muscles; benefits hip joints/limbs; alleviates pain, numbness, weakness, benefits atrophy/inability to flex or extend limbs |
| GB-34 | In the depression of cranial and distal to the head of fibula | Benefits sinews/joints and alleviates pain; contraction of sinews, stiffness and tightness of muscles and joints; swelling, numbness and weakness |
| GV-2 | In the sacro-coccygeal hiatue | Benefits lumbar region and hind limbs; alleviates pain and stiffness of lower back; good for muscular atrophy of lower extremities |
| GV-4 | Between dorsal spinous process of L2 and L3 | Benefits lumbar spine; stiffness and spinal rigidity |
| GV-14 | Between dorsal spinous process of C7 and T1 | Clears heat and good for pain |
| GV-20 | Midline of skull, on a line between anterior edge of base of ears, in notch between sagittal crest and frontal crest | Pacify wind, subdue yang, and good for hemiplasia |
| Hua Tuo Jia Ji | 0.3–0.5 Cun lateral to the depression below spinous process of T12–L7 | Alleviates pain, stiffness of local area, and regulates spine |
| Leg motor sensory area | From 0.5 Cun lateral to GV22 to the posteriorly 1.5 Cun, over the precruciate gyrus, postcruciate gyrus and the sensory cortex | Benefits for paralysis, numbness, and hind limb pain |
| ST-36 | 3 Cun distal to tibial tuberosity and lateral to cranial border of tibia, in the middle of cranial tibialis muscle | Resolve dampness, tonifies Qi, nourishes blood; benefits aching of stifles and hind limbs |
| ST-40 | 8 Cun proximal to the lateral malleolus, cranial to fibula, 2 Cun lateral from tibia, midline between tibialis cranials and long digital extensor muscle | Transform phlegm; improves lower extremity muscle atrophy, motor impairment, pain and paralysis |
| Yao Yan | One handbreadth on either side of lumbar, below the level of iliac crest | Benefits lumbar region and acute or chronic lumbar pain |
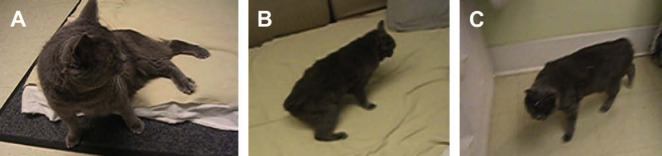
Clinical improvement started with the first acupuncture treatment using dry needle and electro-acupuncture. The duration of standing was 0 s before acupuncture treatment ( Fig 2 A). The cat was able to stand for 5 s and could move one step on his own after the first electro-acupuncture treatment with Tui-Na manipulation. Further progress was not observed after only dry needle acupuncture treatment at the second acupuncture session. At the third acupuncture session, we performed scalp acupuncture, electro-acupuncture and dry needle acupuncture together along with Tui-Na. The cat was able to rise by himself and stood for 18–20 s ( Fig 2 B). The owner mentioned that the cat could use all four limbs for walking without leaning against a wall home after the third acupuncture treatment. The cat's proprioceptive deficit was improved from a 90% deficit to 40%. However, muscle atrophy including biceps femoris, tensor fasciae latae, and gluteal muscles were still pronounced which impacted the recovery of his gait. To rebuild muscle mass, physical therapy using a land treadmill, under-water treadmill, cavaletti rails, uneven soft surfaces (cushions), leg lifts, and exercise balls started after the fourth acupuncture treatment. After the fifth acupuncture therapy including dry needle acupuncture, electro-acupuncture, scalp acupuncture, Tui-Na, and the second physical therapy session, he was able to rise and walk without falling down, and his back posture became relatively straight ( Fig 2 C). Physical therapy was continued once a week for three more times then the schedule changed to acupuncture therapy and physical therapy at alternating 2 week intervals. The dose of prednisolone was reduced from 1.25 mg/kg to 0.625 mg/kg PO daily then to 0.625 mg/kg PO every other day after the seventh and the tenth acupuncture treatment, respectively.
Fig 2.
Chronological progress of motor function following several modes of acupuncture treatment including dry needle acupuncture, electro-acupuncture and scalp acupuncture. (A) Before acupuncture treatment and 10 days after prednisolone therapy (1.25 mg/kg PO, once daily). The cat showed neurological deficits including marked ataxia, dragging of the hind limbs, and was not able to rise or stand. (B) After third acupuncture treatment. The cat was able to rise by himself and stood around 18–20 s. (C) After fifth acupuncture treatment. The cat was able to rise and walk without falling down, and his back posture was relatively straight and balanced.
Feline intervertebral disc disease (IVDD) is usually subclinical in nature. 3 To date, only 30 cases of feline IVDD have been reported in the veterinary literature. 4 Twenty-eight cats among 30 cases showed a single site of IVDD whereas two cases demonstrated two sites of IVDD in thoracolumbar and lumbosacral areas. 4 Common spinal sites of feline IVDD would be cervical or thoracolumbar areas and the ruptured disc material impinges directly on the spinal cord and nerve root. 4–7 Multiple disc extrusions are rare in the cat, especially in cranial thoracic vertebrae. 4 There are two types of IVDD: intervertebral disc extrusion (Hansen's type I) and intervertebral disc protrusion (Hansen's type II). 7 Hansen's type I might be prevalent in cats.8,9 Hansen's type II commonly appears in older cats and may be associated with fibroid disc degeneration. 6 Diagnosis is accomplished by physical signs, neurological tests, and advanced imaging techniques such as myelography, discography, epidurography, computed tomography, or MRI. Neurological signs are not always present in disc protrusions in cats. 8 In general, the clinical signs include pain, inability to walk or jump, weakness of limbs, ataxia, difficulty rising, paralysis, urinary and/or fecal incontinence or accidents and muscle atrophy.4,5,10 In western medicine, medical and surgical treatments have been used for therapeutic or palliative treatment of IVDD.3,4,9 Cats with acute intervertebral disc extrusion in a single specific area respond favorably to surgical decompression of the spinal cord.8,10
Acupuncture has been used in treating musculoskeletal and neurological disorders of humans and animals. 11–13 Pattern identification should be attained to elucidate the underlying causes for providing a proper therapy that is achieved by analyzing the collected information of tongue and pulse profiles, clinical history, observation, and palpation. In OM, IVDD could be categorized into painful obstruction (Bi) syndrome. Three general patterns of painful Bi syndrome of IVDD are: (1) cold-phlegm accumulation due to spleen yang deficiency and liver Qi stagnation, (2) heat accumulation due to kidney yin deficiency, and/or (3) blood stagnation or stasis. In this case, the pattern identification was painful Bi syndrome caused by phlegm-heat accumulation with blood stagnation in the spine based on the tongue profile, pulse diagnosis, physical examination, past history, clinical signs and MRI.
The cat was treated with several modes of acupuncture treatment including dry needle acupuncture, electro-acupuncture and scalp acupuncture along with Tui-Na and physical therapy. Significant improvements in mobility, proprioception and spinal posture were noticed and the cat was able to rise, walk and run 4 months after the initiation of acupuncture treatments. This is the first case report of feline IVDD with multiple disc compressions from cranial thoracic to lumbar area which was successfully treated with several modes of acupuncture treatment and prednisolone. The authors recognize that a single case like this cannot differentiate between the effects of acupuncture and corticosteroids. However, the cat did not respond well to the initial course of prednisolone and began to show improvement as soon as the acupuncture treatments were started. In conclusion, acupuncture treatment may provide a non-invasive complementary medical option for feline IVDD and further research is necessary to confirm the effect of acupuncture treatment for musculoskeletal and neurological disorders.
Acknowledgments
We would like to thank the Medical Imaging Service for their professional support and Dr Edward E Patterson from Department of Veterinary Clinical Sciences, College of Veterinary Medicine, University of Minnesota for his sincere advice.
References
- 1.Battistella MS. Human and small animal scalp acupuncture point comparison. Proceedings of the 13th Annual International Congress on Veterinary Acupuncture, 2004: 237–41.
- 2.Xu X.C. Chinese Tui Na massage: the essential guide to treating injuries, improving health and balancing Qi, 2002, YMAA Publishing Center: Boston, MA, USA. [Google Scholar]
- 3.King A.S., Smith R.N. Degeneration of the intervertebral disc in the cat, Acta Orthop Scand 34, 1964, 139–158. [DOI] [PubMed] [Google Scholar]
- 4.Harris J.E., Dhupa S. Lumbosacral intervertebral disc disease in six cats, J Am Anim Hosp Assoc 44, 2008, 109–115. [DOI] [PubMed] [Google Scholar]
- 5.Jaeger G.H., Early P.J., Munana K.R., Hardie E.M. Lumbosacral disc disease in a cat, Vet Comp Orthop Traumatol 17, 2004, 104–106. [Google Scholar]
- 6.Munana K.R., Olby N.J., Sharp N.J., Skeen T.M. Intervertebral disk disease in 10 cats, J Am Anim Hosp Assoc 37, 2001, 384–389. [DOI] [PubMed] [Google Scholar]
- 7.Rayward R.M. Feline intervertebral disc disease: a review of the literature, Vet Comp Orthop Traumatol 15, 2002, 137–144. [Google Scholar]
- 8.Knipe M.F., Vernau K.M., Hornof W.J., LeCouteur R.A. Intervertebral disc extrusion in six cats, J Feline Med Surg 3, 2001, 161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McConnell J.F., Garosi L.S. Intramedullary intervertebral disk extrusion in a cat, Vet Radiol Ultrasound 45, 2004, 327–330. [DOI] [PubMed] [Google Scholar]
- 10.Kathmann I., Cizinauskas S., Rytz U., Lang J., Jaggy A. Spontaneous lumbar intervertebral disc protrusion in cats: literature review and case presentations, J Feline Med Surg 2, 2000, 207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim Y.S., Chae W.S. Clinical studies on the effect of the electrical acupuncture stimulation therapy of low back pain in lumbar spondylosis, J Kor Acupunt Moxib Soc 10, 1989, 113–128. [Google Scholar]
- 12.Janssens L.A. Acupuncture for the treatment of thoracolumbar and cervical disc disease in the dog, Probl Vet Med 4, 1992, 107–116. [PubMed] [Google Scholar]
- 13.Kim Y.S., Jun H.J., Chae Y.B., et al. Review: the practice of Korean medicine: an overview of clinical trials in acupuncture, Evid Based Compl Altern Med 2, 2005, 325–352. [DOI] [PMC free article] [PubMed] [Google Scholar]