Abstract
Climate change, particularly increasing temperature, changes in rainfall, extreme weather events and changes in vector ecology, impacts the transmission of many climate-sensitive infectious diseases. Asia is the world’s most populous, rapidly evolving and diverse continent, and it is already experiencing the effects of climate change. Climate change intersects with population, sociodemographic and geographical factors, amplifying the public health impact of infectious diseases and potentially widening existing disparities. In this narrative review, we outline the evidence of the impact of climate change on infectious diseases of importance in Asia, including vector-borne diseases, food- and water-borne diseases, antimicrobial resistance and other infectious diseases. We also highlight the imperative need for strategic intersectoral collaboration at the national and global levels and for the health sector to implement adaptation and mitigation measures, including responsibility for its own greenhouse gas emissions.
Keywords: Climate change, greenhouse gas emissions, health systems response, infectious diseases, vector-borne diseases
INTRODUCTION
Climate change is among the most significant global health threats of the century, with profound implications for infectious diseases transmission. Greenhouse gas (GHG) emissions have reached unprecedented concentrations,[1] and global warming continues unabated. At the time of writing in 2023, several countries globally have experienced record-breaking temperatures, heat waves with heat-related health impacts, storm and flood events necessitating evacuation of populations and at times, post-flood rise in infectious diseases. Singapore’s annual mean temperature rose by 1.1°C in just 40 years; sea levels in the Straits of Singapore rose 1.2–1.7 mm per year from 1975 to 2009, and the annual rainfall has increased by 67 mm per decade since 1980.[2]
Climate change poses several other risks to human health beyond heat stress through three main pathways: first, through more frequent extreme weather events such as heat waves, droughts and increased precipitation; second, through natural systems such as changes in disease vector ecology and air quality, and lastly, through interactions with social institutions, public infrastructure, and phenomena such as health systems, global food markets and civil conflict.[3] These impact not just climate-sensitive infectious diseases, but also cardiorespiratory health, allergic diseases, metabolic diseases, nutritional status, pregnancy outcomes and mental health.[4] Climate change adversely impacts healthcare through extreme weather events causing injury, displacement and death, as well as damage to healthcare infrastructure and transportation.
Asia — the world’s most populous and largest continent, highly connected to the world via trade and travel — offers a unique perspective on climate change. The continent exhibits a wide range of climates and geographical settings, which include the Middle East’s deserts, South Asia’s Himalayan mountains, Central Asia’s grasslands, and South and East Asia’s monsoon climates. Climate shifts critically affect agriculture and water security through complex pathways affecting not only the quantity and yield, but also the quality and nutritional value of food.
Many Asian countries are also confronted by compounded impacts due to urbanisation, population growth and migration, land use changes and deforestation. Asia’s sociodemographic and economic landscape is diverse; large metropolitan, densely populated areas often coexist with informal urban settlements with inadequate water, sanitation and hygiene (WASH) and access to healthcare. Comprising lower- and middle-income countries (LMICs) and high-income countries, Asia is experiencing fast-ageing populations and rapidly evolving healthcare systems. These dynamics are accelerating increases in healthcare expenditure and attendant carbon emissions. Ironically, these changes in Asia threaten to exacerbate the climate change pressure and disparities it faces with far-reaching effects, and the healthcare sector has the responsibility to lead the building of climate-resilient health systems.
We focus on the nexus of climate change and infectious diseases in this review for several compelling reasons: (a) infectious diseases have a significant burden on human health, (b) infections are highly sensitive to changes in climactic conditions, (c) there is a potential for climate change to trigger the emergence and re-emergence of these diseases, and (d) infectious diseases have a disproportionate effect in the region, exacerbating health disparities. The evidence base in this field lays a strong foundation for advancing climate adaptation strategies to shape climate-resilient public health policy and health systems.
METHODS
This review employed a detailed search strategy encompassing English-language peer- and non-peer-reviewed articles from 1 January 2000 to 30 June 2023, with the aim to elucidate the link between climate change and infectious diseases that are the most relevant to Asia. PubMed and Google Scholar databases were searched with keyword search terms including ‘climate’, ‘climate change’, ‘Asia’, ‘South Asia’, ‘Southeast Asia’, ‘Middle East’, ‘China’, ‘infection’ and ‘infectious disease’ that encompassed the impact of climate change on infectious diseases and regional specificities. Specific disease terms like ‘dengue’, ‘malaria’ and ‘vector-borne disease’, and ‘diarrheal disease’ in the context of Asia were also included. Additional references were sourced from article citations. We incorporated data from relevant publicly available governmental epidemiological/surveillance such as the Epidemiological News Bulletin from the Ministry of Health, Singapore, and international guidance documents.
CLIMATE CHANGE AND ITS PATHWAYS AFFECTING INFECTIOUS DISEASES EPIDEMIOLOGY
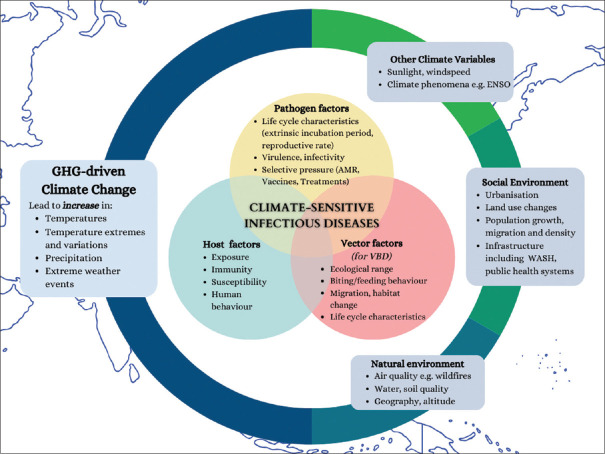
Over half of the known human diseases caused by pathogens are projected to be exacerbated by climate change.[5] A summary framework of the interacting factors that may amplify infectious disease risk is shown in Figure 1, including GHG-driven climate change, other climactic variables, and the social/demographic and natural environment.
Figure 1.
A framework of how climate change interacts with other natural and human variables that may amplify the risk of infectious diseases. AMR: antimicrobial resistance, ENSO: El Niño–Southern Oscillation, WASH: water, sanitation and hygiene, VBD: vector-borne disease
Climate change is predicted to increase zoonotic spillover events driven by novel mammal–virus interactions and cross-species transmission (particularly by bats, and in biodiversity-rich areas such as Asia and Africa), possibly fuelling the next pandemic.[6] Microbes may also be exposed by thawing permafrost leading to outbreaks, as has been seen, for example, in an anthrax outbreak in Siberia in 2016.[7] Climate hazards may catalyse a sequence of secondary events arising from other population vulnerabilities impacting infectious diseases in Asia, further amplifying health inequities.[8]
Temperature rise increases the duration of transmission season of many vector-borne diseases. Climate change-induced temperature rise and irregular rainfall influence pathogen propagation, dispersal and distribution, human behaviour and vector ecology, and thus can enhance disease transmission.[9] Its incidence in relation to climactic factors is a complex, non-linear interplay with temperature, rainfall and humidity. Rainfall likewise influences vector/larval breeding sites, but may affect transmission in urban environments less predictably, such as in Singapore, where mosquitoes breed indoors, particularly in low-rise housing, and around corridors in apartment blocks.[10,11]
Extreme weather events and flooding may not only wash out vector habitats, but also increase new breeding sites, leading to higher risk of dengue and increase in food- and water-borne diseases (FWBD) such as leptospirosis and cholera. Flooding events compromise clean drinking water sources, particularly in settings of suboptimal WASH infrastructure, leading to FWBD outbreaks. Poor air quality, exacerbated by rising global temperatures through increased ground-level ozone and wildfire incidence, adversely affects respiratory health, increasing the risk of respiratory infections.[12,13] Weather disasters and climate migration may also impact access to health services such as vaccination programmes, exacerbating the burden of vaccine-preventable diseases.[14]
EFFECTS OF CLIMATE CHANGE ON SPECIFIC INFECTIOUS DISEASES IN ASIA
Vector-borne diseases
Arthropods are ectothermic; their larvae require humidity or water for development. Temperature impacts mosquito survival, flying distance and biting behaviour.[15] Vector-biting rates rise with temperatures to a threshold, beyond which they decline. Higher temperatures speed up the pathogen’s extrinsic incubation period.[16] Host and carrier ecology, population immunity, along with temperature, precipitation and humidity chiefly influence vector-borne disease transmission. Climate change-related floods typically lead to increases in mosquito-borne disease after an initial decrease.[17]
In addition, major climactic phenomena, such as the El Niño–Southern Oscillation (ENSO),[18] and human factors, such as urbanisation, population growth, travel, public health infrastructure, all interact with climate change to influence transmission. Overall, climate change is likely to exacerbate risk and pose significant challenges for disease control and public health planning.
Dengue
Dengue is the most important arboviral disease in Asia. It is transmitted by Aedes spp. mosquitoes (Ae. aegypti and Ae. albopictus), which are also the chief vectors of other arboviruses such as chikungunya, yellow fever and Zika. Seasonal incidence of dengue is well described in Asia, with correlations established with temperature, relative humidity and rainfall.[19,20,21]
Dengue vector abundance has increased by 9.5% over the past 110 years, largely due to climate change, and further increases are expected, potentiated in densely populated regions like South Asia.[22] If GHG emissions continue to rise, annual dengue transmission duration in South China is predicted to increase, while areas susceptible to year-round dengue epidemics will significantly expand.[23]
Climate change has increased the vectorial capacity for dengue transmission and the potential for dengue transmission in parts of China based on vectorial capacity and public health surveillance and response capacity.[24] Several studies also predict the geographical expansion of dengue due to climate change.[25] Every 1°C rise in temperature approximately doubled the population at risk for dengue in Taiwan.[26] However, this relationship is non-linear; beyond a temperature threshold, dengue incidence may not increase further.[27] This appears to hold true for precipitation as well, across some time lag.[28] Studies in Singapore and Bangladesh have demonstrated high variable temperature as the best predictor for a spike in dengue cases.[29,30]
Weather extremes like heatwaves, extreme rainfall and tropical cyclones can all further drive transmission.[31] Droughts may drive more water storage, creating potential breeding grounds; heavy rainfall increases water ponding, producing breeding sites.[32] Conversely, Seah et al.[27] observed a parabolic effect of maximum temperature and dengue, with negative effect of extreme heat on dengue risk. In the Pearl River Delta, China, in 2013–2018, dengue infection risk increased by 62% five days after a tropical cyclone.[33] In contrast, strong, multifaceted responses by numerous national and international organisations in the immediate aftermath of typhoon Haiyan in the Philippines in 2015 were successful in preventing a large dengue outbreak.[34] Kao et al.[35] found that dengue outbreaks in Taiwan were influenced not only by typhoon-induced precipitation, but also by typhoon trajectory, suggesting the degree of wind destruction may affect the amount of debris created, hence influencing mosquito habitat suitability. These findings reflect the strong influence of environmental conditions on dengue transmission.
Malaria
Malaria, transmitted by Anopheles spp. mosquitoes, is caused by Plasmodium spp. protozoa. Plasmodium spp. relevant to Asia are P. falciparum, P. vivax and P. knowlesi. Despite strides in malaria eradication and control, malaria remains prevalent in Asia, second only to Africa. Climate change threatens this progress; significant challenges persist, including vector resistance to insecticides and parasite multidrug resistance.
Like dengue, increased rainfall could drive mosquito breeding but may also wash away mosquito larvae, reducing transmission. Droughts may drive mosquito populations down, but increased water storage may increase mosquito breeding sites. Areas with reduced rainfall may observe seasonal rather than year-round transmission.[5] Rising temperatures may expand the geographical range of Anopheles mosquitoes and bring malaria polewards to previously naïve regions, such as the highlands, at the borders of endemic malaria areas.[36] In endemic areas, further temperature rise may reduce the vector capacity instead.[37]
In Asia, climate suitability for malaria is expected to decrease in India, southern Myanmar, southern Thailand, eastern Borneo and parts of Cambodia, Malaysia and Indonesia; it is anticipated to increase in parts of China, Taiwan and Nepal,[38,39] potentially outside designated at-risk areas and, therefore, lacking targeted vector control interventions.[40] Land use changes also influence zoonotic malaria, which has been demonstrated in Malaysian Borneo, where Fornace et al.[41] developed a model incorporating mosquito and human space use data that predicted the majority (>90%) of infectious bites in surrounding residential household areas at forest edges. This has implications for vector control programmes and strategies, to focus not only on indoor but also outdoor transmission.
Other vector-borne diseases
Japanese encephalitis virus, Zika virus, chikungunya virus, and Rickettsia spp. infections are well recognised in the region. While global transmissibility of Zika and chikungunya viruses is expected to increase due to climate change, the specific impact on Asia remains uncertain. The implications of other important potentially climate-sensitive vector-borne diseases not yet endemic in Asia, such as yellow fever and Rift Valley fever, have not been thoroughly researched.[42]
Food- and water-borne diseases
The FWBD, caused by Vibrio spp., Shigella spp., Campylobacter spp. and Escherichia coli, account for substantial morbidity and mortality, and are projected to increase with climate change, not just due to climactic factors, but also compounded by food and water security issues and population factors, including population displacement.[43] The World Health Organization (WHO) projects that under a fossil fuel-intensive emissions scenario, climate change will cause an additional 48,000 and 33,000 deaths due to diarrhoeal disease in children under 15 years of age by 2030 and 2050, respectively. One-third and one-quarter of these deaths are predicted to occur in Asia in 2030 and 2050, respectively, even after considering improvements in child health. Impacts are particularly concentrated in South Asia, alongside eastern Africa. This is largely due to water scarcity intensified by climate change.[44] Several studies in Japan, China, Taiwan, Bangladesh and Nepal have found that diarrhoeal disease morbidity risk increases by 4%–10% per 1°C rise in temperature.[45,46,47]
Seasonal trends in FWBD are related to environmental conditions and climatic factors, particularly in environments where WASH infrastructure may be overwhelmed or compromised and where open defaecation is practised. Climate change dynamics are likely to impact multiple WASH factors, which will in turn influence cholera transmission.[48] Floods may compromise sewerage systems, thereby contaminating drinking sources or water used for irrigation, leading to disease outbreaks of enteric pathogens. Droughts drive water rationing, thereby affecting both water quantity and quality.[49] El Niño–Southern Oscillation catalyses changes in global weather patterns and has been linked to rates of enteric illness, including cholera in Bangladesh.[49]
Vibrio species including Vibrio cholerae
Climate affects the ecology of Vibrio spp.,which are abundant in estuarine ecosystems with warm waters of moderate salinity. Estuarine waters have warmed more rapidly than oceans due to climate change, providing ideal environmental conditions for Vibrio spp. proliferation.[44] Human infection transmission occurs via the faecal–oral route from the ingestion of improperly handled or contaminated raw seafood or water. Vibrio cholerae, the aetiological agent of cholera, is causing significant global outbreaks in the ongoing seventh cholera pandemic, extending beyond areas of conflict and humanitarian crises. Vibrio parahaemolyticus and V. vulnificus can also cause life-threatening skin/soft tissue infections in wounds contaminated by water containing these microbes.
Climate is a major threat to global cholera disease rates, particularly in coastal areas such as Bangladesh and India.[50] Cholera is highly influenced by factors such as rainfall, temperature, sea surface temperature and ENSO. Average temperature, ocean temperature, ocean salinity, precipitation and humidity have influenced the incidence of V. parahaemolyticus in Taiwan.[51] A V. vulnificus outbreak in Israeli fish market workers coincided with the hottest summers recorded in Israel, suggesting extreme heat from climate change may have affected local ecology and triggered emergence of the disease.[52] Projections predict substantial climate change-related increases in Vibrio-friendly areas globally, particularly in Southeast Asia and China. This coincides with the Vibrio season extension and a growing coastal population, hence a predicted rise in infections.[53]
National food security, threatened by climate change, also affects cholera incidence. There is an independent inverse relationship between national food security and cholera incidence in LMICs, including Asian countries.[54] Multiple potential pathways explain this, including changes in human behaviours and malnutrition affecting susceptibility to cholera infection.[55,56] A worldwide shortage of cholera vaccine is likely to exacerbate these predictions and underscore the need for strong public health response/preparedness plans.
Salmonellosis
Salmonellosis is among the most important causes of diarrhoeal disease globally, causing considerable morbidity in young children and economic impact. Seasonal trends are associated with climatic factors.[57] Weather changes may lead to microbial contamination of leafy vegetables and other food produce and rise in pests and insects in agricultural areas, transferring microbes. Higher temperature and rainfall is associated with Salmonella cases in Singapore and Hong Kong.[58]
Other water-borne diseases
Water-borne diseases also include those transmitted via contact, ingestion, inhalation and skin penetration, such as leptospirosis, typhoid fever, melioidosis and schistosomiasis. Leptospirosis is endemic in many countries in Asia, especially in settings where water is contaminated by rodent urine, and transmission is known to coincide with rainy seasons.[59] Burkholderia pseudomallei, the causative agent of melioidosis, causes serious infections, particularly in immunocompromised hosts. Found in water and soil, it is endemic in Southeast Asia and northern Australia. Rainfall intensity is a clear predictor of melioidosis incidence. High wind speeds in tropical storms/cyclones can cause aerosolisation (and inhalation) of B. pseudomallei.[60] Schistosomiasis, a parasitic blood fluke infection transmitted via contact with water contaminated by infective cercariae released from freshwater snails, is prevalent in Asia, notably due to Schistosoma japonicum and S. mekongi. Outbreaks are linked to floods, as seen in the Yangtze River region.[61]
Other notable infectious diseases
Tuberculosis
The incidence of tuberculosis (TB) is the highest in Southeast Asia, accounting for 44% of the global burden.[62] Tuberculosis continues to be a leading cause of death worldwide.[63] Climate changes, through diverse pathways, are likely to hamper TB eradication efforts. The transmission of TB increases with temperature and decreases with altitude.[64] The spatial distribution of TB in China has moved southwards, with climate and air quality variables being significant factors at play.[65] Climate change also increases susceptibility to TB infection, through increasing prevalence of underlying risk factors such as malnutrition, poverty and indoor air pollution, especially in developing countries.[66]
Hand, foot and mouth disease
Hand, foot and mouth disease (HFMD), largely a paediatric disease, is commonly caused by human enterovirus A71 and coxsackieviruses 10 and 16. Severe or prolonged manifestations are rare, but the socioeconomic burden of HFMD on children and their families is substantial.[67] Many Asian countries report increasing numbers of HFMD, including Singapore, where annual HFMD case numbers have risen.[68] Summer outbreaks strongly connotate a relationship with weather patterns.[69] Temperature and relative humidity increases are associated with increasing HFMD cases in East and Southeast Asia,[70,71] with climate change likely to exacerbate HFMD incidence. Warmer and humid conditions are thought to provide a more suitable environment for enteroviruses to multiply in food and water and survive in the environment.
OTHER EFFECTS OF CLIMATE CHANGE ON INFECTIOUS DISEASES
The interplay between climate change and antimicrobial resistance (AMR) is generally understudied, albeit gaining traction in recent years. Multiple factors resulting from climate change may contribute to AMR. Increasing temperature accelerates bacterial growth, horizontal transfer of mobile genetic elements and AMR, for example, the population prevalence of carbapenem-resistant Gram negatives.[72] In addition, microplastics, which increase GHGs via perturbations of the soil and marine microbiome and affect climate factors like precipitation and temperature,[73] also facilitate gene exchange, including resistance determinants, in bacteria.[74] A case in point is ‘coronavirus disease 2019 pollution’, where Asia, the most populous continent, generated the most plastic waste from disposable facemasks in the world during the pandemic.[75] Beyond personal protective equipment (PPE) and cleaning-related and general waste, significant sources of biomedical waste-related microplastics arise from pharmaceuticals and the laboratory/diagnostics. Climate change-driven food insecurity will increase pressure for food production, affecting land use patterns and possibly increasing pressure for the use of adjuncts, such as antimicrobials for agriculture and farming, exacerbating the AMR issue.[76] In addition, extreme weather events may disrupt and overwhelm routine healthcare, including immunisation services, and may lead to outbreaks of vaccine-preventable diseases, increased antimicrobial use and AMR.
LIMITATIONS AND BIAS
Research trends in climate change and infectious disease demonstrate taxonomic bias, with an emphasis on the study of specific organisms. Vector-borne diseases have dominated this field. However, there are substantial knowledge gaps in other infectious diseases.[77] Insufficient research in non-human taxa may limit our capacity to understand and predict emerging diseases. In addition, there is a complex interplay and interdependency of various factors mediating the impact of climate change on infectious diseases, and the nuances may not be easily extrapolated to specific contexts. For example, most studies on climate change and infectious diseases have been in temperate rather than tropical areas, reflecting spatial bias against more vulnerable areas.[78] While a detailed search strategy was used for this review’s aim to illustrate the evidence of impact of climate change on infectious diseases of importance to Asia from peer-reviewed and suitable non-peer-reviewed literature, it was limited to English-language articles, which may introduce some bias. There remain significant uncertainties in accurately quantifying climate impacts on health. The impact of infectious diseases on climate change depends on how much GHG emissions are reduced. Various emission scenarios and respective warming will alter projections and modelling. Inherent uncertainties highlight the need for enhanced resilience, adaptive capacity and flexibility in public health climate adaptation strategies.[79]
HEALTH SYSTEM RESPONSE: ADAPTATION AND MITIGATION
The evidence of climate change impacting infectious diseases highlights its role as a significant public health threat. In anticipation of climate change significantly straining health systems and exacerbating global health inequities, it is crucial to address climate change from a health perspective.
Widespread consensus highlights two key strategies for climate action necessary to counteract the health risks of climate change, as outlined in the action agenda agreed upon at the Second WHO Global Conference on Health and Climate in 2016[80] — firstly, climate adaptation, focused on strengthening the resilience of health systems and supply chains against ‘locked-in’ climate change, referring to anticipated continued temperature rise due to past, current and near-future GHG emissions,[81] and secondly, climate mitigation, which aims to reduce emissions of climate pollutants to safeguard environmental and social determinants of health. The WHO has proposed broad principles for these strategies, which we have applied specifically to infectious disease risks, outlined in Table 1.[82]
Table 1.
Strategies for climate resilience in infectious diseases according to WHO guidance.
| Strategy | Deployment of strategy to respond to infectious diseases risks from climate change in Asia |
|---|---|
| Adopt a comprehensive approach to integrating and mainstreaming the management of climate risks into health systems | • Enhanced surveillance and monitoring of emerging infectious diseases by integrating climate data into early warning systems, particularly for vector-borne diseases. |
|
| |
| Show leadership and engage in intersectoral governance | • Enhance collaboration between public health professionals and policymakers to boost health contributions to national climate resilience plans. |
| • Embed infection control teams into sustainability workgroups at hospitals and balance pandemic preparedness and energy efficiency. | |
|
| |
| Develop the capacity of the health workforce to address climate risks | • Enhance health professional training to recognise and address climate-sensitive health risks as well as to educate communities accordingly. |
|
| |
| Enhance health information systems | • Encourage research on regional climate modelling for infectious diseases to improve predictive early warning systems. |
| • Adopt a One Health approach for integrated surveillance across human, animal and environmental sectors, for example, enhanced vector-borne disease tracking in animal reservoirs can help predict and prevent outbreaks in humans. | |
|
| |
| Promote climate-resilient and sustainable infrastructure and technologies | • Advocate for a green standard for healthcare infrastructure and procurement that balances infection control needs, energy efficiency, climate resilience and health co-benefits for patients. For example, hospitals may need to balance the transition to open ventilation ward systems to reduce energy intensity, with the need to have closed spaces to protect patients from mosquito bites and, in turn, vector-borne diseases. |
| • Leverage emerging technologies to optimise energy use for cooling/ventilation needs and hospital sterilisation processes. | |
|
| |
| Strengthen the management of environmental determinants of health, climate-informed health programming and emergency preparedness | • Develop emergency response plans that consider the potential impacts of climate change on infectious diseases — this may involve planning for increased healthcare service delivery during anticipated disease outbreaks, training healthcare workers, especially primary care professionals, to respond to climate-related health emergencies. |
| • Balance health benefits of outdoor activities with the risks of vector-borne and other climate-sensitive diseases when designing health interventions. | |
|
| |
| Scale up financial investments to develop and sustain health resilience to climate change | • Invest more in research for climate-sensitive infectious diseases and climate resilience strategies in infectious disease prevention and control. |
WHO: World Health Organization
Adaptation measures in Asia
Systems such as the Asia Pacific Strategy for Emerging Diseases and Public Health Emergencies[83] and China’s Infectious Disease Automated-alert and Response System (CIDARS)[84] recognise the role of climate change in disease emergence. The CIDARS uses climactic variables to predict and manage diseases like avian influenza and dengue. In Singapore, an early warning system incorporating various data streams, including recent cases, meteorological data and vector surveillance data, outperformed other methods in forecasting the 2013 dengue outbreak and has shown promise in enhancing response preparedness to dengue outbreaks.[85]
The modelling techniques used for projections and decision-making need to be more rigorous and sophisticated. For instance, dengue outbreak prediction models are incorporating more robust modelling techniques such as machine learning and autoregressive time series, underscoring the importance of considering a variety of factors affecting transmission, adjusting for time lags in disease dynamics and conducting rigorous validation of model performance in real-world settings. However, key shortcomings in current models include reliance on secondary predictor data, exclusion of non-climate variables and inadequate reporting of methodology, validation and performance measures.[86]
The public health implications for anticipated rise in climate-driven food-borne infections include food agencies reviewing temperature control guidance and food hygiene for commercial and home food preparation; food importation regulations and surveillance; and interdisciplinary measures to mitigate risk to food safety.[87] Ensuring integrity of drinking water supply, WASH infrastructure and disease surveillance is important to mitigate the risk of water-borne diseases.
Mitigation measures
Improving healthcare’s resilience to climate-sensitive trends in infectious diseases is only one aspect of the challenge. Equally crucial is the need to manage the significant carbon footprint associated with addressing these diseases. Healthcare contributes 5%–8% of global GHG emissions,[88,89] which is more than that of shipping and aviation industries. However, data on the healthcare carbon footprint in Asia are sparse and lack robustness. Longitudinally measuring and tracking GHG emissions associated with healthcare and healthcare-related activities, such as education and biomedical research with implemented interventions, is an urgent need. Greening our energy grid alone will only reduce this footprint by approximately one fifth. The remaining carbon footprint is embedded within clinical practice — a domain over which healthcare professionals have a unique voice.
While top-down systematic transformation, leadership and organisational emphasis on sustainable practices is necessary for mitigating healthcare carbon emissions, bottom-up approaches, led by healthcare professionals who are most familiar with direct healthcare delivery, are equally vital. Excellent examples in Singapore include recent initiatives championed by anaesthetists to reduce their use of desflurane, an inhaled anaesthetic with a disproportionately large carbon footprint,[90] and recycling of polyvinyl chloride single-use ward items like intravenous fluid bags, oxygen tubings and oxygen masks.[91] Simply practising ‘good medicine’ can be a good first step to reduce our professional carbon and ecological footprints. Key drivers of sustainable healthcare practice include encouraging disease prevention, empowering patients and adopting lean methodologies and low-carbon alternatives that do not impact patient safety.[92] For example, rational prescribing of antimicrobials and improved infection prevention and control practices can collectively significantly reduce unnecessary prescriptions, combat the spread of AMR and reduce antibiotic-related adverse events. Responsible and rational use of single-use items and PPE, including safe and extended use of PPE,[93] advocating for reusables where the risk of infection transmission from reusing PPE (or other items) that has been used for patient care is negligible, can also lower the carbon footprint associated with waste.
Eliminating unnecessary testing and investigations, where it will not change clinical management, can streamline practice and increase value. Embracing telemedicine and other remote care models can decrease the carbon footprint linked to patient travel, which contributes about 5% of the United Kingdom’s National Health Service carbon footprint.[94]
While medico-legal risks can make it tempting to over-investigate and overtreat, the medical principle of ‘primum non nocere’ (first, do no harm) should serve as a reminder. It is an ethical imperative to practise medicine in a way that protects the well-being of not just today’s population, but also future generations. Here, strengthening diagnostic and therapeutic stewardship programmes in healthcare will be key. Lastly, there is a need to build an investment and economic case for policymakers to address the health impacts of climate change and to enable and advocate for building of climate-resilient health systems, where GHG emission reduction and climate action are projected to yield economic benefits and increase value.[95]
CONCLUSION
Climate change exerts a substantial influence on many infectious diseases, with important implications for Asia. It is critical that the healthcare sector strengthens its adaptive strategies to handle climate-sensitive emerging and endemic diseases, including robust public health preparedness and disease prediction systems. The healthcare sector must also take responsibility for its role in global emissions and mitigate its own GHG emissions. This requires strategic change at a systemic level and sustainable healthcare delivery, underscoring the duality of healthcare’s response to climate change.
Financial support and sponsorship
Nil.
Conflicts of interest
Vasoo S is a member of the SMJ Editorial Board and was thus not involved in the peer review and publication decisions of this article.
REFERENCES
- 1.Liu Z, Deng Z, Davis S, Ciais P. Monitoring global carbon emissions in 2022. Nat Rev Earth Environ. 2023;4:205–6. doi: 10.1038/s43017-023-00406-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Climate Change Secretariat. Global impact of climate change. Available from: https://www.nccs.gov.sg/about-climate-cha nge/global-impact-of-climate-change/
- 3.Wheeler N, Watts N. Climate change: From science to practice. Curr Environ Health Rep. 2018;5:170–8. doi: 10.1007/s40572-018-0187-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Climate change and health. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health .
- 5.Romanello M, Di Napoli C, Drummond P, Green C, Kennard H, Lampard P, et al. The 2022 report of the Lancet Countdown on health and climate change: Health at the mercy of fossil fuels. Lancet. 2022;400:1619–54. doi: 10.1016/S0140-6736(22)01540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson CJ, Albery GF, Merow C, Trisos CH, Zipfel CM, Eskew EA, et al. Climate change increases cross-species viral transmission risk. Nature. 2022;607:555–62. doi: 10.1038/s41586-022-04788-w. [DOI] [PubMed] [Google Scholar]
- 7.Ezhova E, Orlov D, Suhonen E, Kaverin D, Mahura A, Gennadinik V, et al. Climatic factors influencing the anthrax outbreak of 2016 in Siberia, Russia. Ecohealth. 2021;18:217–28. doi: 10.1007/s10393-021-01549-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Semenza JC, Rocklöv J, Ebi KL. Climate change and cascading risks from infectious disease. Infect Dis Ther. 2022;11:1371–90. doi: 10.1007/s40121-022-00647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yi L, Xu X, Ge W, Xue H, Li J, Li D, et al. The impact of climate variability on infectious disease transmission in China: Current knowledge and further directions. Environ Res. 2019;173:255–61. doi: 10.1016/j.envres.2019.03.043. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez SA, Sun H, Dickens BL, Ng LC, Cook AR, Lim JT. Features of the urban environment associated with Aedes aegypti abundance in high-rise public apartments in Singapore: An environmental case-control study. PLoS Negl Trop Dis. 2023;17:e0011075. doi: 10.1371/journal.pntd.0011075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seidahmed OME, Lu D, Chong CS, Ng LC, Eltahir EAB. Patterns of urban housing shape dengue distribution in singapore at neighborhood and country scales. GeoHealth. 2017;2:54–67. doi: 10.1002/2017GH000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhai G, Zhang L. Impact of fine particulate matter 2.5 on hospitalization for upper respiratory tract infections in Lanzhou urban industrial area, China. Ann Agric Environ Med. 2023;30:462–7. doi: 10.26444/aaem/171499. [DOI] [PubMed] [Google Scholar]
- 13.Brugha R, Grigg J. Urban air pollution and respiratory infections. Paediatric Respir Rev. 2014;15:194–9. doi: 10.1016/j.prrv.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Zhu YG, Johnson TA, Su JQ, Qiao M, Guo GX, Stedtfeld RD, Hashsham SA, et al. Diverse and abundant antibiotic resistance genes in Chinese swine farms. Proc Natl Acad Sci U S A. 2013;110:3435–40. doi: 10.1073/pnas.1222743110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li C, Lu Y, Liu J, Wu X. Climate change and dengue fever transmission in China: Evidences and challenges. Sci Total Environ. 2018;622623:493–501. doi: 10.1016/j.scitotenv.2017.11.326. [DOI] [PubMed] [Google Scholar]
- 16.Caminade C, McIntyre KM, Jones AE. Impact of recent and future climate change on vector-borne diseases. Ann N Y Acad Sci. 2019;1436:157–73. doi: 10.1111/nyas.13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coalson JE, Anderson EJ, Santos EM, Madera Garcia V, Romine JK, Dominguez B, et al. The complex epidemiological relationship between flooding events and human outbreaks of mosquito-borne diseases: A scoping review. Environ Health Perspect. 2021;129:96002. doi: 10.1289/EHP8887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martinez PP, Reiner RC, Jr, Cash BA, Rodó X, Mondal MS, Roy M, et al. Cholera forecast for Dhaka, Bangladesh, with the 2015-2016 El Niño: Lessons learned. PLoS One. 2017;12:e0172355. doi: 10.1371/journal.pone.0172355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen SC, Hsieh MH. Modeling the transmission dynamics of dengue fever: Implications of temperature effects. Sci Total Environ. 2012;431:385–91. doi: 10.1016/j.scitotenv.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 20.Lee H, Kim JE, Lee S, Lee CH. Potential effects of climate change on dengue transmission dynamics in Korea. PLoS One. 2018;13:e0199205. doi: 10.1371/journal.pone.0199205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pham HV, Doan HT, Phan TT, Minh NN. Ecological factors associated with dengue fever in a Central Highlands province, Vietnam. BMC Infect Dis. 2011;11:172. doi: 10.1186/1471-2334-11-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu-Helmersson J, Brännström Å, Sewe MO, Semenza JC, Rocklöv J. Estimating past, present, and future trends in the global distribution and abundance of the Arbovirus Vector Aedes aegypti under climate change scenarios. Front Public Health. 2019;7:148. doi: 10.3389/fpubh.2019.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao-dong D, Hua W, Xiao-xuan W. Change in temperature in South China and its impact on the potential epidemic duration of dengue fever. Chin J Ecol. 2015;34:3174–81. [Google Scholar]
- 24.Cai W, Zhang C, Zhang S, Bai Y, Callaghan M, Chang N, et al. The 2022 China report of the Lancet Countdown on health and climate change: Leveraging climate actions for healthy ageing. Lancet Public Health. 2022;7:e1073–90. doi: 10.1016/S2468-2667(22)00224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kraemer MU, Sinka ME, Duda KA, Mylne AQ, Shearer FM, Barker CM, et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. Elife. 2015;4:e08347. doi: 10.7554/eLife.08347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu PC, Lay JG, Guo HR, Lin CY, Lung SC, Su HJ. Higher temperature and urbanization affect the spatial patterns of dengue fever transmission in subtropical Taiwan. Sci Total Environ. 2009;407:2224–33. doi: 10.1016/j.scitotenv.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 27.Seah A, Aik J, Ng LC, Tam CC. The effects of maximum ambient temperature and heatwaves on dengue infections in the tropical city-state of Singapore-A time series analysis. Sci Total Environ. 2021;775:145117. doi: 10.1016/j.scitotenv.2021.145117. doi: 10.1016/j.scitotenv. 2021.145117. [DOI] [PubMed] [Google Scholar]
- 28.Servadio JL, Rosenthal SR, Carlson L, Bauer C. Climate patterns and mosquito-borne disease outbreaks in South and Southeast Asia. J Infect Public Health. 2018;11:566–71. doi: 10.1016/j.jiph.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Pinto E, Coelho M, Oliver L, Massad E. The influence of climate variables on dengue in Singapore. Int J Environ Health Res. 2011;21:415–26. doi: 10.1080/09603123.2011.572279. [DOI] [PubMed] [Google Scholar]
- 30.Hossain S, Islam MM, Hasan MA, Chowdhury PB, Easty IA, Tusar MK, et al. Association of climate factors with dengue incidence in Bangladesh, Dhaka City: A count regression approach. Heliyon. 2023;9:e16053. doi: 10.1016/j.heliyon.2023.e16053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y, Wei Y, Li K, Jiang X, Li C, Yue Q, et al. Impact of extreme weather on dengue fever infection in four Asian countries: A modelling analysis. Environ Int. 2022;169:107518. doi: 10.1016/j.envint.2022.107518. [DOI] [PubMed] [Google Scholar]
- 32.Banu S, Hu W, Hurst C, Tong S. Dengue transmission in the Asia-Pacific region: Impact of climate change and socio-environmental factors. Trop Med Int Health. 2011;16:598–607. doi: 10.1111/j.1365-3156.2011.02734.x. [DOI] [PubMed] [Google Scholar]
- 33.Li C, Zhao Q, Zhao Z, Liu Q, Ma W. The association between tropical cyclones and dengue fever in the Pearl River Delta, China during 2013-2018: A time-stratified case-crossover study. PLoS Negl Trop Dis. 2021;15:e0009776. doi: 10.1371/journal.pntd.0009776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aumentado C, Cerro BR, Olobia L, Suy LL, Reyes A, Kusumawathie PH, et al. The prevention and control of dengue after Typhoon Haiyan. Western Pac Surveill Response J. 2015;6(Suppl 1):60–5. doi: 10.5365/WPSAR.2015.6.3.HYN_018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kao B, Lin CH, Wen TH. Measuring the effects of typhoon trajectories on dengue outbreaks in tropical regions of Taiwan: 1998-2019. Int J Biometeorol. 2023 doi: 10.1007/s00484-023-02498-0. doi: 10.1007/s00484-023-02498-0. [DOI] [PubMed] [Google Scholar]
- 36.Martens WJ, Niessen LW, Rotmans J, Jetten TH, McMichael AJ. Potential impact of global climate change on malaria risk. Environ Health Perspect. 1995;103:458–64. doi: 10.1289/ehp.95103458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murdock CC, Sternberg ED, Thomas MB. Malaria transmission potential could be reduced with current and future climate change. Sci Rep. 2016;6:27771. doi: 10.1038/srep27771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khormi HM, Kumar L. Future malaria spatial pattern based on the potential global warming impact in South and Southeast Asia. Geospat Health. 2016;11:416. doi: 10.4081/gh.2016.416. [DOI] [PubMed] [Google Scholar]
- 39.Wang Z, Liu Y, Li Y, Wang G, Lourenço J, Kraemer M, et al. The relationship between rising temperatures and malaria incidence in Hainan, China, from 1984 to 2010: A longitudinal cohort study. Lancet Planet Health. 2022;6:e350–8. doi: 10.1016/S2542-5196(22)00039-0. [DOI] [PubMed] [Google Scholar]
- 40.Bhattarai S, Blackburn JK, Ryan SJ. Malaria transmission in Nepal under climate change: Anticipated shifts in extent and season, and comparison with risk definitions for intervention. Malar J. 2022;21:390. doi: 10.1186/s12936-022-04417-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fornace KM, Alexander N, Abidin TR, Brock PM, Chua TH, Vythilingam I, et al. Local human movement patterns and land use impact exposure to zoonotic malaria in Malaysian Borneo. Elife. 2019;8:e47602. doi: 10.7554/eLife.47602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wasserman S, Tambyah PA, Lim PL. Yellow fever cases in Asia: Primed for an epidemic. Int J Infect Dis. 2016;48:98–103. doi: 10.1016/j.ijid.2016.04.025. [DOI] [PubMed] [Google Scholar]
- 43.Cissé G. Food-borne and water-borne diseases under climate change in low- and middle-income countries: Further efforts needed for reducing environmental health exposure risks. Acta Trop. 2019;194:181–8. doi: 10.1016/j.actatropica.2019.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pachauri R. K., Meyer L. A., editors. IPCC 2014: Climate Change 2014: Synthesis Report. IPCC; Geneva, Switzerland: Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; p. 151. [Google Scholar]
- 45.Onozuka D, Gasparrini A, Sera F, Hashizume M, Honda Y. Modeling future projections of temperature-related excess morbidity due to infectious gastroenteritis under climate change conditions in Japan. Environ Health Perspect. 2019;127:77006. doi: 10.1289/EHP4731. doi: 10.1289/ehp4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Y, Bi P, Hiller JE. Weather and the transmission of bacillary dysentery in Jinan, northern China: A time-series analysis. Public Health Rep. 2008;123:61–6. doi: 10.1177/003335490812300109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dhimal M, Bhandari D, Karki KB, Shrestha SL, Khanal M, Shrestha RRP, et al. Effects of climatic factors on diarrheal diseases among children below 5 years of age at National and Subnational Levels in Nepal: An ecological study. Int J Environ Res Public Health. 2022;19:6138. doi: 10.3390/ijerph19106138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jones N, Bouzid M, Few R, Hunter P, Lake I. Water, sanitation and hygiene risk factors for the transmission of cholera in a changing climate: Using a systematic review to develop a causal process diagram. J Water Health. 2020;18:145–58. doi: 10.2166/wh.2020.088. [DOI] [PubMed] [Google Scholar]
- 49.Asadgol Z, Mohammadi H, Kermani M, Badirzadeh A, Gholami M. The effect of climate change on cholera disease: The road ahead using artificial neural network. PLoS One. 2019;14:e0224813. doi: 10.1371/journal.pone.0224813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Asadgol Z, Badirzadeh A, Niazi S, Mokhayeri Y, Kermani M, Mohammadi H, et al. How climate change can affect cholera incidence and prevalence? A systematic review. Environ Sci Pollut Res Int. 2020;27:34906–26. doi: 10.1007/s11356-020-09992-7. [DOI] [PubMed] [Google Scholar]
- 51.Hsiao H-I, Jan M-S, Chi H-J. Impacts of climatic variability on vibrio parahaemolyticus outbreaks in Taiwan. Int J Environ Res Public Health. 2016;13:188. doi: 10.3390/ijerph13020188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paz S, Bisharat N, Paz E, Kidar O, Cohen D. Climate change and the emergence of Vibrio vulnificus disease in Israel. Environ Res. 2007;103:390–6. doi: 10.1016/j.envres.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 53.Trinanes J, Martinez-Urtaza J. Future scenarios of risk of Vibrio infections in a warming planet: A global mapping study. Lancet Planet Health. 2021;5:e426–35. doi: 10.1016/S2542-5196(21)00169-8. [DOI] [PubMed] [Google Scholar]
- 54.Richterman A, Azman AS, Constant G, Ivers LC. The inverse relationship between national food security and annual cholera incidence: A 30-country analysis. BMJ Glob Health. 2019;4:e001755. doi: 10.1136/bmjgh-2019-001755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharkey JR. Diet and health outcomes in vulnerable populations. Ann N Y Acad Sci. 2008;1136:210–7. doi: 10.1196/annals.1425.020. [DOI] [PubMed] [Google Scholar]
- 56.Jones AD. Food insecurity and mental health status: A global analysis of 149 countries. Am J Prev Med. 2017;53:264–73. doi: 10.1016/j.amepre.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 57.Akil L, Ahmad HA, Reddy RS. Effects of climate change on Salmonella infections. Foodborne Pathog Dis. 2014;11:974–80. doi: 10.1089/fpd.2014.1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang P, Goggins WB, Chan EYY. Associations of Salmonella hospitalizations with ambient temperature, humidity and rainfall in Hong Kong. Environ Int. 2018;120:223–30. doi: 10.1016/j.envint.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 59.Davies GI, McIver L, Kim Y, Hashizume M, Iddings S, Chan V. Water-borne diseases and extreme weather events in Cambodia: Review of impacts and implications of climate change. Int J Environ Res Public Health. 2014;12:191–213. doi: 10.3390/ijerph120100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Birnie E, Biemond JJ, Wiersinga WJ. Drivers of melioidosis endemicity: Epidemiological transition, zoonosis, and climate change. Curr Opin Infect Dis. 2022;35:196–204. doi: 10.1097/QCO.0000000000000827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu XH, Zhang SQ, Xu XJ, Huang YX, Steinmann P, Utzinger J, et al. Effect of floods on the transmission of schistosomiasis in the Yangtze River valley, People's Republic of China. Parasitol Int. 2008;57:271–6. doi: 10.1016/j.parint.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 62.Furin J, Cox H, Pai M. Tuberculosis. Lancet. 2019;393:1642–56. doi: 10.1016/S0140-6736(19)30308-3. [DOI] [PubMed] [Google Scholar]
- 63.Programme GT. Global Tuberculosis Report 2021. Geneva: 2021. [Google Scholar]
- 64.Gelaw YA, Yu W, Magalhães RJS, Assefa Y, Williams G. Effect of temperature and altitude difference on tuberculosis notification: A systematic review. J Glob Infect Dis. 2019;11:63–8. doi: 10.4103/jgid.jgid_95_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li H, Ge M, Zhang M. Spatio-temporal distribution of tuberculosis and the effects of environmental factors in China. BMC Infect Dis. 2022;22:565. doi: 10.1186/s12879-022-07539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kharwadkar S, Attanayake V, Duncan J, Navaratne N, Benson J. The impact of climate change on the risk factors for tuberculosis: A systematic review. Environ Res. 2022;212:113436. doi: 10.1016/j.envres.2022.113436. [DOI] [PubMed] [Google Scholar]
- 67.Wang ZL, Xia AM, Li YF, Su HL, Zhan LW, Chen YP, et al. Socioeconomic burden of hand, foot and mouth disease in children in Shanghai, China. Epidemiol Infect. 2016;144:138–43. doi: 10.1017/S0950268815001569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Min N, Ong YHB, Han AX, Ho SX, Yen EWP, Ban KHK, et al. An epidemiological surveillance of hand foot and mouth disease in paediatric patients and in community: A Singapore retrospective cohort study, 2013-2018. PLoS Negl Trop Dis. 2021;15:e0008885. doi: 10.1371/journal.pntd.0008885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Coates SJ, Davis MDP, Andersen LK. Temperature and humidity affect the incidence of hand, foot, and mouth disease: A systematic review of the literature-a report from the International Society of Dermatology Climate Change Committee. Int J Dermatol. 2019;58:388–99. doi: 10.1111/ijd.14188. [DOI] [PubMed] [Google Scholar]
- 70.Abdul Wahid NA, Suhaila J, Rahman HA. Effect of climate factors on the incidence of hand, foot, and mouth disease in Malaysia: A generalized additive mixed model. Infect Dis Model. 2021;6:997–1008. doi: 10.1016/j.idm.2021.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cheng Q, Sun A, Liu X, Chen QL, Bi L, Ren PX, et al. Ambient temperature, humidity and hand, foot, and mouth disease: A systematic review and meta-analysis. Sci Total Environ. 2018;625:828–36. doi: 10.1016/j.scitotenv.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 72.Li Z, Sun A, Liu X, Chen QL, Bi L, Ren PX, et al. Climate warming increases the proportions of specific antibiotic resistance genes in natural soil ecosystems. J Hazard Mater. 2022;430:128442. doi: 10.1016/j.jhazmat.2022.128442. [DOI] [PubMed] [Google Scholar]
- 73.Chia RW, Lee JY, Lee M, Lee GS, Jeong CD. Role of soil microplastic pollution in climate change. Sci Total Environ. 2023;887:164112. doi: 10.1016/j.scitotenv.2023.164112. [DOI] [PubMed] [Google Scholar]
- 74.Yuanze S, Jie W. How microplastics and nanoplastics shape antibiotic resistance? How microplastics and nanoplastics shape antibiotic resistance? Water Emerg Contam Nanoplastics. 2022;1:8. https://doi.org: 10.20517/wecn.2022.09. [Google Scholar]
- 75.Benson NU, Bassey DE, Palanisami T. COVID pollution: Impact of COVID-19 pandemic on global plastic waste footprint. Heliyon. 2021;7:e06343. doi: 10.1016/j.heliyon.2021.e06343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang MS, Li W, Zhang WG, Li YT, Li JY, Gao Y, et al. Agricultural land-use change exacerbates the dissemination of antibiotic resistance genes via surface runoffs in Lake Tai Basin, China. Ecotoxicol Environ Saf. 2021;220:112328. doi: 10.1016/j.ecoenv.2021.112328. [DOI] [PubMed] [Google Scholar]
- 77.Ryan SJ, Lippi CA, Caplan T, Diaz A, Dunbar W, Grover S, et al. The current landscape of software tools for the climate-sensitive infectious disease modelling community. Lancet Planet Health. 2023;7:e527–36. doi: 10.1016/S2542-5196(23)00056-6. [DOI] [PubMed] [Google Scholar]
- 78.Allen T, Murray KA, Zambrana-Torrelio C, Morse SS, Rondinini C, Di Marco M, et al. Global hotspots and correlates of emerging zoonotic diseases. Nat Commun. 2017;8:1124. doi: 10.1038/s41467-017-00923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wardekker JA, de Jong A, van Bree L, Turkenburg WC, van der Sluijs JP. Health risks of climate change: An assessment of uncertainties and its implications for adaptation policies. Environ Health. 2012;11:67. doi: 10.1186/1476-069X-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.World Health Organization. Second Global Conference Health &Climate-Conference Conclusions and Action Agenda. Paris: 2016. [Google Scholar]
- 81.UN Environment Programme. Temperature rise is “locked in” for the coming decades in the Arctic. 2019 [Google Scholar]
- 82.Operational Framework for building climate resilient health systems. Geneva: World Health Organization; 2015. [[Last accessed on 2023 Nov 15]]. Available from: https://apps.who.int/iris/bitstream/handle/10665/189951/9789241565073_eng.pdf . [Google Scholar]
- 83.World Health Organization. Regional Office for the Western Pacific. Asia Pacific strategy for emerging diseases and public health emergencies (APSED III): Advancing implementation of the International Health Regulations (2005): Working together towards health security. 2017:75. [Google Scholar]
- 84.Yang W. Elsevier/Academic Press; 2017. Early warning for infectious disease outbreak: Theory and practice; pp. 133–61. [Google Scholar]
- 85.Shi Y, Liu X, Kok SY, Rajarethinam J, Liang S, Yap G, et al. Three-month real-time dengue forecast models: An early warning system for outbreak alerts and policy decision support in Singapore. Environ Health Perspect. 2016;124:1369–75. doi: 10.1289/ehp.1509981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Leung XY, Islam RM, Adhami M, Ilic D, McDonald L, Palawaththa S, et al. A systematic review of dengue outbreak prediction models: Current scenario and future directions. PLoS Negl Trop Dis. 2023;17:e0010631. doi: 10.1371/journal.pntd.0010631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Aik J, Heywood AE, Newall AT, Ng LC, Kirk MD, Turner R. Climate variability and salmonellosis in Singapore-A time series analysis. Sci Total Environ. 2018;639:1261–7. doi: 10.1016/j.scitotenv.2018.05.254. [DOI] [PubMed] [Google Scholar]
- 88.Connor A, Lillywhite R, Cooke MW. The carbon footprint of a renal service in the United Kingdom. QJM. 2010;103:965–75. doi: 10.1093/qjmed/hcq150. [DOI] [PubMed] [Google Scholar]
- 89.Eckelman MJ, Sherman JD, MacNeill A. J. Life cycle environmental emissions and health damages from the Canadian healthcare system: An economic-environmental-epidemiological analysis. PLOS Med. 2018;15:e1002623. doi: 10.1371/journal.pmed.1002623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ying LL. Singapore: SPH Media Limited; 2023. The Straits Times. [Google Scholar]
- 91.Hong L. Singapore: SPH Media Limited; 2023. The Straits Times. [Google Scholar]
- 92.Mortimer F, Isherwood J, Wilkinson A, Vaux E. Sustainability in quality improvement: Redefining value. Future Healthc J. 2018;5:88–93. doi: 10.7861/futurehosp.5-2-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tan GSE, Linn KZ, Soon MML, Vasoo S, Chan M, Poh BF, et al. Effect of extended use N95 respirators and eye protection on personal protective equipment (PPE) utilization during SARS-CoV-2 outbreak in Singapore. Antimicrob Resist Infect Control. 2020;9:86. doi: 10.1186/s13756-020-00753-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, et al. Health care's response to climate change: A carbon footprint assessment of the NHS in England. Lancet Planetary Health. 2021;5:e84–92. doi: 10.1016/S2542-5196(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Perera FP. Multiple threats to child health from fossil fuel combustion: Impacts of air pollution and climate change. Environ Health Perspect. 2017;125:141–8. doi: 10.1289/EHP299. [DOI] [PMC free article] [PubMed] [Google Scholar]