Abstract
Evidence suggests that diabetes is on the rise in India, affecting many people’s life satisfaction. Comprehensive estimation of life satisfaction among diabetes patients does not exist in the country. This study examined the effects of socioeconomic status, depression, and diabetes symptoms severity on the life satisfaction of diabetes patients by controlling various demographic variables. It was a cross-sectional study comprising 583 diabetes patients from Punjab, India. Patients were interviewed using a multi-stage purposeful random sampling method. Descriptive analysis and partial least squares structural equation modelling were used in the study to test the hypotheses. Results revealed that socioeconomic status, depression and diabetes symptoms severity significantly influence the life satisfaction of diabetes patients. A 1% drop in diabetes symptoms severity corresponds to a 0.849% increase in life satisfaction, whereas a 1% decrease in depression results in a 0.898% increase in life satisfaction. Patients with higher diabetes symptoms severity were coping with common mental disorders. Women reported higher diabetes symptoms severity and depression than men, resulting in lower life satisfaction. An experimental evaluation of the effects of socioeconomic status, depression and diabetes symptoms severity, and numerous demographic factors on life satisfaction was reported. The findings will help policymakers understand the problem associated with life satisfaction among diabetes patients in the country.
Keywords: Diabetes, Patients, Socioeconomic status, Life satisfaction, Depression, Structural equation modelling
Subject terms: Diseases, Endocrinology, Signs and symptoms
Introduction
Diabetes, being a chronic disease, significantly impacts health and is a major global public health concern1,2. It is one of the main contributors to mortality and morbidity worldwide, especially in India3. India is known to be the “Diabetes Capital of the World”, with around 19.4 million people living with diabetes, and by 2025, that figure is anticipated to ascend to 57.2 million4,5. Such an increasing burden and the chronic nature of this disease has a multidimensional impact on the individual, family, and society6. Its multifaceted impact has been linked to several physical, psychological, and social issues that require substantial and ongoing assistance from various societal stakeholders7,8. Several studies have found that these issues are significantly associated with life satisfaction (LISAT) in diabetes patients9–13.
In this direction, Tuncay and Avcı14 in their study found that the level of LISAT varies across diabetes patients. Evidence suggests that LISAT and diabetes management are interconnected15. As a result, in the context of diabetes, LISAT, one of the oldest multidimensional concepts, appears to be more complicated than it seems16. Generally, its measures are subjective or based on the variables an individual finds personally crucial17. For instance, many studies have found that diabetes patients with a high LISAT have more fulfilling social relationships, receive more social support, and feel more satisfied than those with a low LISAT18–20.
Additional studies conducted in this area have shown that a higher LISAT is positively related to better diabetes management and helps reduce its risk factors among patients15,21–23. Patients with a high LISAT have a significantly lower risk of mortality than their low LISAT counterparts24–28. Furthermore, the low LISAT levels among patients with diabetes compared to the general population may reflect an additional burden on them19,20. With the increasing burden of diabetes, it is crucial to understand how patients’ lives are affected and the factors influencing their LISAT.
Studies conducted by various researchers, such as Baumann et al.14 in Luxembourg, Mauricio18 in Spain, and Tuncay and Avcı21 in Turkey, have shown positive results in diabetes patients with decent LISAT. A study conducted by Lee et al.19 in Taiwan suggests that improvements in LISAT positively impact diabetes management and overall mental well-being. Thus, a comprehensive study that examines the relationship between LISAT, diabetes and its related factors is important for developing countries like India. In a similar direction, this study included diabetes symptom severity (DSS) and its relationship with depression in the case of diabetes patients, and, ultimately, their LISAT. Furthermore, we have examined the effects of diabetes patients’ socioeconomic status (SES) on DSS, depression, and LISAT while controlling for gender, age, resident type, religion, social category, and household size. By gaining a deeper understanding of these factors, healthcare professionals and policymakers can develop targeted interventions and support systems to improve the LISAT of patients with diabetes. Such understanding can help them in developing effective strategies to support patients with diabetes and improve their overall well-being in the country.
Aims and objectives of the study
The LISAT measurement scale includes many essential domains such as vocational, financial and leisure situations, contacts with friends, sexual life, self-care management, family life, partner relationships, and physical and psychological health29. Evidence shows that the effects of each LISAT domain are unequal and vary between individuals30. Thus, there is a need to investigate the effect of potential factors that may significantly influence LISAT in diabetes patients31. As a result, our study aimed to assess the effect of SES, depression, and DSS on the LISAT of diabetes patients. An additional aim was to identify the potential mediating role of depression and DSS in the relationship between SES and LISAT. Both analyses were conducted while controlling for numerous demographic variables.
Methodology
Measures
This section briefly outlines the constructs and associated indicators used in our study. We have also discussed the development of measures used in survey instruments. The measures adopted in the present study are well-established and widely used scales in the literature. However, the indicators were modified as per the objectives of the study.
Socioeconomic status (SES)
SES is a complex concept that includes the living conditions, resources, and opportunities available to people within a particular society. It measures one’s combined economic and social status, often associated with health32. Therefore, from a measurement perspective, it is conventionally conceptualised as a formative latent variable rather than a reflective latent variable33. Thus, we employed several observable factors (Supplementary File 1) to establish SES as a formative latent construct while considering India’s demography34,35.
Life satisfaction (LISAT)
We used the LISAT-11 questionnaire to measure the overall LISAT level of diabetes patients. It is an extension of LISAT-9, generally treated as a reflective latent construct where several studies have employed it to assess the LISAT of different patients36–38.
Patient health questionnaire (PHQ)
The PHQ is a reflective latent construct used to assess common mental disorders in various pieces of research39. In the case of diabetes, this simple self-administered diagnostic instrument has been used extensively to detect the early stages of depression40–45.
Diabetes symptoms severity (DSS)
The DSS is constructed as a reflective latent construct based on a self-administered questionnaire designed to gauge how severe diabetes patients perceive their symptoms. The questionnaire included a list of symptoms of diabetes which have been taken from the medical literature, and the severity of each symptom was determined using a five-point Likert scale, with scores ranging from 0 (not present) to 4 (most severe)46. This questionnaire not only assesses perceived DSS but also examines the chronic progression of the disease. Since many people usually ignore the symptoms of diabetes for a substantial period and sometimes do not consider them serious because, unlike many other health conditions, the effects of diabetes does not appear immediately47. People are generally unaware that damage can begin many years before symptoms become noticeable48. Hence, by considering the asymptomatic nature of diabetes in the early stages, it is crucial to measure the chronic progression of diabetes because early recognition of symptoms can help patients get the disease under control sooner and provide protection against vascular complications49.
Control variable
In this study, Table 1 shows the demographic profiles (DP) such as resident type (DP1) (rural and urban), age group (DP2) (19–50 years, 51–60 years and 61–above years), religion (DP3) (Sikh and others including Hindu and Muslim), social category (DP4) (others and SC & OBC), gender (DP5) (women and men), and household size (DP6) (Below average and Above average) with average of 4.83 (≈ 5) persons. Previous studies have shown the importance of these variables that may affect model outcomes16,23,50,51.
Table 1.
Demographic summary.
| Characteristics | Types | Total cases (Percentage) |
|---|---|---|
| Demographic profile (DP) | ||
| Resident type (DP1) | Rural | 324 (55.6) |
| Urban | 259 (44.5) | |
| Age group (µ = 58.5 years) (DP2) | 19–50 | 169 (29.0) |
| 51–60 | 172 (29.6) | |
| 61-above | 242 (41.6) | |
| Religion (DP3) | Others (Hindu, Muslim) | 210 (36.1) |
| Sikh | 373 (64.0) | |
| Social category (DP4) | Others | 368 (63.2) |
| SC and OBC | 215 (36.9) | |
| Gender (DP5) | Women | 299 (51.3) |
| Men | 284 (48.8) | |
| Household size (µ = 4.83 person) (DP6) | Below µ | 415 (71.2) |
| Above µ | 168 (28.9) | |
µ = Mean.
Model building and hypothesis development
Diabetes and SES
Years of research have shown that SES affects diabetes disproportionately, where relatively consistent patterns are observed in the risk and prevalence of diabetes and its complications among different levels of SES52–54. Despite the interdependence of the components of SES, each has a distinct effect on diabetes. For instance, the complications and prevalence of diabetes vary significantly by the level of education and wealth55,56. However, on a broad scale, people with lower SES levels are more likely to develop diabetes, have more complications, and die earlier than those with higher SES levels57–59. Variations in SES pose unique challenges for diabetes patients in lower-middle-income nations like India. Such anomalous variation in SES across countries differentially affects the risk factors, prevalence, and burden of diabetes60.
SES and LISAT
Literature shows that people with high SES are better at controlling their diabetes than those with low SES61. Many qualitative and quantitative research studies has also demonstrated a positive association between SES and LISAT levels62–64. Accordingly, increasing LISAT is recommended not only for people with diabetes but also for the general population. Several studies have proved that a higher LISAT slows down the disease progression rate65,66. The study of Carniglia et al.67 suggests that strengthening SES can improve LISAT, which is critical in the case of diabetes as well.
SES and DSS
The major problem for any diabetes patient is managing the symptoms and the severity associated with the same68. As a result, proper diabetes management necessitates balancing the SES level of the patient69. In this direction, several studies have found SES to be a central factor in overall diabetes management, including its symptom management and associated complications57,70,71.
SES and PHQ
SES is not only linked with diabetes management but is also significantly associated with other complications of diabetes, such as depression, obesity, hypertension, etc.60,72. Furthermore, Everson et al.73 found that the least affluent bear a disproportionate amount of the disease burden, including depression, obesity and diabetes. Likewise, Leone et al.72 corroborated that a low SES is associated with a higher prevalence of depression among diabetes patients.
PHQ and LISAT
In a similar line, the level of depression among diabetes patients also has an impact on their LISAT levels19. A study by Nigeria et al.23 found that more depressed patients reported lower LISAT and vice versa. LISAT is not only associated with depression among patients with diabetes but also with complications perceived by patients due to diabetes symptoms47.
DSS and LISAT
Tekir et al.74 conducted a study on the effect of diabetes symptoms on LISAT and found that diabetes symptoms affect LISAT. The findings of Kim and Lee showed that diabetes patients with andropause symptoms experienced a low level of LISAT75. Further, Gulliford and Mahabir71 found that DSS has a negative impact on health-related quality of life. Hence, raising LISAT among diabetes patients is recommended by several studies14–16. A high level of LISAT is vital in keeping diabetes and its complications under control14.
DSS and PHQ
Further, earlier research has found that diabetes patients who have their diabetes-related problems under control are less likely to suffer from depression9. However, because most patients are unable to control their diabetes, thus, diabetes and depression occur together almost twice as often as would be predicted by chance alone76. Grootenhuis et al.77 found substantial differences in symptom severity scores among patients with diabetes to be the leading cause of depression among patients. In a similar direction, Katon78 showed an overlap between diabetes symptoms and depression. Hence, many studies have proven that the aforementioned highlighted components are essential for further analysis in the case of diabetes patients69,72,74.
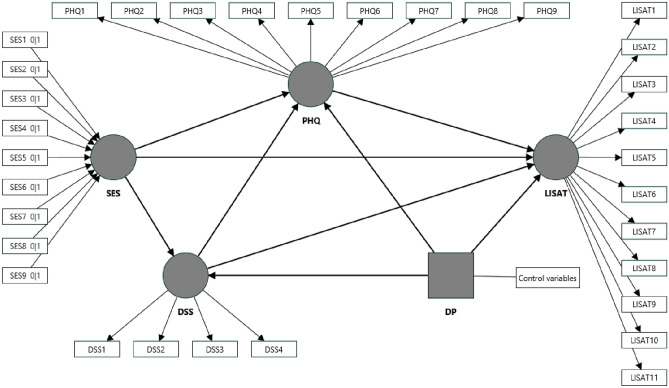
All these studies together helped in developing the following hypothesis in the present study (see Fig. 1):
Figure 1.
SEM model specification. Control variables include gender, age, resident type, religion, social category, and household size.
H1
SES has a positive relationship with LISAT among diabetes patients.
H1a
DSS mediates the relationship between SES and LISAT.
H1b
PHQ mediates the relationship between SES and LISAT.
H1c
DSS and PHQ mediate the relationship between SES and LISAT.
H2
SES has a negative relationship with DSS among diabetes patients.
H3
SES has a negative relationship with PHQ among diabetes patients.
H3a
DSS mediates the relationship between SES and PHQ.
H4
DSS has a negative relationship with LISAT among diabetes patients.
H4a
PHQ mediates the relationship between DSS and LISAT.
H5
PHQ has a negative relationship with LISAT among diabetes patients.
H6
DSS has a positive relationship with PHQ among diabetes patients.
Data and sampling methods
The present paper was based on primary cross-sectional data of diabetic patients collected through well-structured questionnaires from different districts of Punjab, India. All the data on diabetes-related symptoms were collected during diabetes, where the average duration of diagnosis was 4.75 years. A sample of households for collecting the required information was selected with the help of a multi-stage purposeful random sampling method79. We followed the WHO-STEPS methodology to prepare, design, and select the samples in the study area and used the census of 2011 as the sampling frame80,81. The target population in the study area was patients who had diabetes. The survey period was from November 2020 to February 2021 and from March 2021 to June 2021. This study was performed in line with the principles of the Declaration of Helsinki. The ethical clearance approval was obtained from the INSTITUTE ETHICAL COMMITTEE (HUMAN) of the Indian Institute of Technology Mandi, India (REF: IITM/IEC(H)/2022/RT/P1).
Statistical analysis
We have performed descriptive statistics such as frequency and percentage distribution and partial least squares structural equation modelling (PLS-SEM) using the SmartPLS4 version to calculate the results82. PLS-SEM allows the estimation of complex cause-effect relationships in path models with latent variables83.
Ethics approval
Approval was granted by the Institutional Ethics Committee of the Indian Institute of Technology Mandi on 12/01/2022 (REF: IITM/IEC(H)/2022/RT/P1).
Consent to participate
Data was collected after obtaining the informed consent from the patients. Field enumerators explained the purpose of the data collection to the subjects and obtained their approval before proceeding with the data collection.
Human and animal rights
This study was conducted in accordance with the principles of the Declaration of Helsinki. The authors did not conduct any biological experiments on human or animal subjects in this study.
Results
Table 1 shows the sample distribution of 583 diabetes patients across various demographic factors, consisting of 299 (51.3%) women and 284 (48.7%) men, categorised into three age groups: 19–50 years, 51–60 years and 61–above years, where the mean age was 58.5 years. Our results showed that the proportion of diabetes patients increased as we moved from lower to higher age groups. In our study, 55.6% of patients were from rural areas, and 44.4% were from urban areas. Also, the majority of the patients (64.0%) belonged to the Sikh community, as the state has a substantial Sikh population, accounting for 57.7% of the total population of Punjab. Furthermore, the average household size in our study was 4.83 (≈ 5) persons, which was higher than India’s average of 4.44 (≈ 4) persons.
Evaluation of reflective measurement model
Many studies highlighted the importance of reflective measurement modelling in SEM84–87. Therefore, it is crucial to perform its assessment before inclusion in the final model88. The primary goal of such an evaluation is to ensure the reliability and validity of the reflective construct measures and consequently provide support for the suitability of their inclusion in the path model. As per the criteria stated by Hair et al.89, Cronbach’s alpha and composite reliability values should lie between 0.700 and 0.950. Whereas the average variance extracted (AVE) value should be at least 0.50, indicating that the construct explains 50% or more of the variance of the indicators that make up that particular construct. Similarly, the results presented in Table 2 passed the threshold, confirming that reliability and convergent validity were achieved for the LISAT, PHQ, and DSS.
Table 2.
Reflective construct reliability and validity analysis.
| Reflective Constructs | Items | Outer loadings | Variance inflation factor (VIF) | Cronbach’s alpha | Composite reliability (rho_c) | Average variance extracted (AVE) |
|---|---|---|---|---|---|---|
| LISAT | LISAT1 | 0.935 | 1.873 | 0.921 | 0.930 | 0.563 |
| LISAT2 | 0.443 | 2.308 | ||||
| LISAT3 | 1.039 | 3.342 | ||||
| LISAT4 | 1.053 | 4.051 | ||||
| LISAT5 | 1.084 | 2.821 | ||||
| LISAT6 | 0.954 | 1.950 | ||||
| LISAT7 | 0.817 | 2.487 | ||||
| LISAT8 | 1.041 | 3.551 | ||||
| LISAT9 | 0.373 | 2.764 | ||||
| LISAT10 | 0.879 | 3.493 | ||||
| LISAT11 | 1.152 | 4.007 | ||||
| PHQ | PHQ1 | 1.043 | 1.961 | 0.926 | 0.939 | 0.631 |
| PHQ2 | 1.417 | 2.727 | ||||
| PHQ3 | 1.289 | 3.497 | ||||
| PHQ4 | 1.153 | 3.543 | ||||
| PHQ5 | 1.020 | 2.943 | ||||
| PHQ6 | 0.847 | 2.321 | ||||
| PHQ7 | 1.026 | 2.954 | ||||
| PHQ8 | 0.958 | 2.231 | ||||
| PHQ9 | 0.515 | 1.651 | ||||
| DSS | DSS1 | 0.568 | 1.180 | 0.708 | 0.817 | 0.535 |
| DSS2 | 0.893 | 1.477 | ||||
| DSS3 | 1.180 | 1.729 | ||||
| DSS4 | 1.223 | 1.585 |
After confirming the reliability and convergent validity of the LISAT, PHQ and DSS, it was necessary to establish their discriminant validity (DV) for further evaluation. Evaluating DV evaluates construct specificity, which ensures the discrimination between the measures of dissimilar constructs. Hence, to ensure that the construct is unique from the other constructs in terms of empirical criteria, Hair et al.89 presented two measures of DV, i.e., through analysing the cross-loadings of the indicators and confirming the Fornell–Larcker criterion (FLC). The cross-loading results in Table 3 show higher values in the diagonal line, confirming the DV where outer loadings of LISAT indicators were higher on the LISAT only. Similarly, PHQ indicators were also higher only on the PHQ. In addition, DSS indicators were high only for the DSS and not for the LISAT and PHQ, respectively. Concurrently, in Table 3, the FLC results show that the shared variance among LISAT, PHQ and DSS in the model did not exceed their AVE. In empirical applications, however, FLC consistently fails to reliably identify DV issues because it performs insufficiently, mainly when indicator loadings vary slightly over a construct. Thus, Henseler et al.90 stated that FLC and cross-loading criteria are inadequate methods to ensure DV, and recommended the heterotrait-monotrait (HTMT) ratio for further validation. Accordingly, in our case, the value of the HTMT ratio is below the threshold level of 0.85, indicating that the DV has been established and the model is reliable for further processing.
Table 3.
Cross loadings, Fornell–Larcker criterion and Heterotrait-monotrait ratio (HTMT).
| LISAT | PHQ | DSS | |
|---|---|---|---|
| Cross loadings | |||
| LISAT1 | 0.698 | − 0.278 | − 0.611 |
| LISAT2 | 0.340 | − 0.035 | − 0.018 |
| LISAT3 | 0.826 | − 0.368 | − 0.425 |
| LISAT4 | 0.878 | − 0.419 | − 0.600 |
| LISAT5 | 0.834 | − 0.420 | − 0.561 |
| LISAT6 | 0.684 | − 0.215 | − 0.356 |
| LISAT7 | 0.738 | − 0.353 | − 0.393 |
| LISAT8 | 0.881 | − 0.437 | − 0.485 |
| LISAT9 | 0.408 | − 0.003 | 0.035 |
| LISAT10 | 0.832 | − 0.396 | − 0.426 |
| LISAT11 | 0.890 | − 0.418 | − 0.555 |
| PHQ1 | − 0.358 | 0.748 | 0.165 |
| PHQ2 | − 0.329 | 0.772 | 0.080 |
| PHQ3 | − 0.349 | 0.821 | 0.096 |
| PHQ4 | − 0.419 | 0.875 | 0.136 |
| PHQ5 | − 0.392 | 0.838 | 0.175 |
| PHQ6 | − 0.360 | 0.792 | 0.083 |
| PHQ7 | − 0.401 | 0.846 | 0.162 |
| PHQ8 | − 0.371 | 0.768 | 0.075 |
| PHQ9 | − 0.288 | 0.667 | 0.002 |
| DSS1 | − 0.327 | − 0.033 | 0.516 |
| DSS2 | − 0.364 | 0.052 | 0.719 |
| DSS3 | − 0.434 | 0.091 | 0.803 |
| DSS4 | − 0.607 | 0.219 | 0.843 |
| Fornell–Larcker criterion | |||
| LISAT | 0.750 | ||
| PHQ | − 0.460 | 0.794 | |
| DSS | − 0.617 | 0.143 | 0.731 |
| Heterotrait-monotrait ratio | |||
| PHQ | 0.443 | ||
| DSS | 0.653 | 0.165 | |
Factor loadings for each observed variable are in bold.
Evaluation of formative measurement model
After evaluating LISAT, PHQ and DSS, the results in Table 4 show the evaluation of SES. As previously stated, SES is a formative measurement model; hence, the internal consistency perspective that supports LISAT, PHQ, and DSS assessment cannot be used in the case of SES. Since its measures do not always covary, thus its evaluation starts with convergent validity (CV). CV ensures that the entire domain of the SES and its significant attributes are covered by its indicators. As a result, we performed a redundancy analysis to ensure the CV of SES. Next, we examined the collinearity issue between indicators of SES using the Variance Inflation Factor (VIF), and the results for all indicators were below a threshold of five.
Table 4.
Formative construct assessment.
| Formative Constructs | Indicators | Convergent validity | Variance inflation factor (VIF) | Outer weights (p-values) |
|---|---|---|---|---|
| SES | SES1 | Achieved using redundancy analysis | 1.230 | 0.295 (0.000)* |
| SES2 | 1.030 | 0.361 (0.000)* | ||
| SES3 | 1.155 | 0.414 (0.000)* | ||
| SES4 | 1.054 | 0.384 (0.000)* | ||
| SES5 | 1.234 | 0.404 (0.000)* | ||
| SES6 | 1.275 | 0.277 (0.000)* | ||
| SES7 | 1.292 | 0.219 (0.000)* | ||
| SES8 | 1.179 | 0.198 (0.000)* |
*Significant at 5%.
Additionally, considering significant values of outer indicator weights ensures the validation and inclusion of SES in the final model91. We may conclude from the results of Tables 2, 3, and 4 that LISAT, PHQ, DSS and SES have a sufficient degree of measurement quality, indicating that all constructs passed the evaluation criteria presented by Hair et al.89. Thus, it is recommended to proceed with the evaluation of the structural model.
Evaluation of structural model
After establishing the outer model, Table 5 shows the results of the proposed hypotheses testing, where we found that SES plays a vital role in coping with DSS and PHQ. Further, the outcomes revealed that DSS and PHQ were negatively associated with LISAT. It implies that a 1% decrease in the DSS of diabetes patients brings a 0.849% positive change in their LISAT, while a 1% decrease in the PHQ improves the LISAT of diabetes patients by 0.898%. Additionally, diabetes patients who perceived higher symptom severity were more depressed. Similarly, our indirect path analysis demonstrated an instance of serial mediation, with DSS as a mediator variable impacting the path from SES to LISAT more than PHQ. Because the variance accounted for by DSS and PHQ were 50.73% and 30.46%, respectively, showing a case of partial mediation in our model.
Table 5.
Hypotheses testing results.
| Effect | Original sample | Sample mean | STDEV | T statistics | p-values | Decision |
|---|---|---|---|---|---|---|
| Direct effect | ||||||
| SES—> LISAT | 0.135 | 0.149 | 0.111 | 1.215 | 0.224 | Not supported |
| SES—> PHQ | − 0.280 | − 0.272 | 0.095 | 2.936 | 0.003* | Supported |
| SES—> DSS | − 0.492 | − 0.489 | 0.186 | 2.643 | 0.008* | Supported |
| DSS—> LISAT | − 0.849 | − 0.844 | 0.054 | 15.672 | 0.000* | Supported |
| PHQ—> LISAT | − 0.898 | − 0.895 | 0.070 | 12.779 | 0.000* | Supported |
| DSS—> PHQ | 0.046 | 0.044 | 0.029 | 1.606 | 0.108** | Supported |
| Indirect effect | ||||||
| SES—> DSS—> LISAT | 0.418 | 0.413 | 0.161 | 2.592 | 0.010* | Supported |
| SES—> PHQ—> LISAT | 0.251 | 0.244 | 0.088 | 2.844 | 0.004* | Supported |
| SES—> DSS—> PHQ—> LISAT | 0.020 | 0.019 | 0.014 | 1.424 | 0.154 | Not supported |
| SES—> DSS—> PHQ | − 0.023 | − 0.021 | 0.017 | 1.342 | 0.180 | Not supported |
| DSS—> PHQ—> LISAT | − 0.042 | − 0.038 | 0.024 | 1.700 | 0.089** | Supported |
*Significant at 5%, **Significant at 10%.
Results in Table 6 show the significance of control variables in our structural model. We found a significant difference in DSS among resident type and age. Patients in rural areas perceived more DSS than their urban counterparts, whereas, with increased age, patients perceived lower DSS. In the case of religion and social category, Sikh and other category patients reported significantly lower levels of LISAT. Compared to men, women patients had significantly more discomfort from DSS, and their high levels of depression may have contributed to their poorer levels of LISAT.
Table 6.
Effect of control variables.
| Effect | Original sample | Sample mean | STDEV | T statistics | p-values |
|---|---|---|---|---|---|
| DP1—> LISAT | 0.067 | 0.067 | 0.073 | 0.921 | 0.357 |
| DP1—> PHQ | 0.027 | 0.029 | 0.035 | 0.647 | 0.518 |
| DP1—> DSS | 0.183 | 0.182 | 0.063 | 2.920 | 0.004* |
| DP2—> LISAT | 0.015 | 0.015 | 0.041 | 0.359 | 0.719 |
| DP2—> PHQ | − 0.005 | − 0.006 | 0.023 | 0.231 | 0.817 |
| DP2—> DSS | − 0.089 | − 0.089 | 0.035 | 2.563 | 0.010* |
| DP3—> LISAT | 0.128 | 0.131 | 0.078 | 1.645 | 0.100** |
| DP3—> PHQ | 0.052 | 0.053 | 0.043 | 1.232 | 0.218 |
| DP3—> DSS | − 0.009 | − 0.008 | 0.066 | 0.134 | 0.893 |
| DP4—> LISAT | − 0.111 | − 0.112 | 0.068 | 1.634 | 0.102** |
| DP4—> PHQ | − 0.025 | − 0.023 | 0.043 | 0.578 | 0.563 |
| DP4—> DSS | 0.103 | 0.101 | 0.060 | 1.723 | 0.085** |
| DP5—> LISAT | − 0.085 | − 0.086 | 0.069 | 1.232 | 0.218 |
| DP5—> PHQ | 0.057 | 0.055 | 0.037 | 1.514 | 0.130 |
| DP5—> DSS | 0.175 | 0.175 | 0.054 | 3.212 | 0.001* |
| DP6—> LISAT | 0.012 | 0.008 | 0.095 | 0.129 | 0.898 |
| DP6—> PHQ | − 0.075 | − 0.076 | 0.061 | 1.239 | 0.216 |
| DP6—> DSS | 0.157 | 0.157 | 0.081 | 1.934 | 0.053* |
*Significant at 5%, **Significant at 10%.
The findings in Table 7 show the structural model’s predictive relevance results. We have used f-square, adjusted R-square, and Q-square values and calculated them for (before and after introducing) the control variables to check the predictive relevance of the structural model. VIF values for all the constructs were less than five, indicating that our model has no collinearity issues. Further, the results of the adjusted R-square (with control variable) for PHQ (0.075) and DSS (0.103) were less than 0.25, implying a weak explanatory power. In contrast, we found a substantial explanatory power in the LISAT (0.518) case because the value was more than 0.50. It means that the model’s independent variables explain 51.8% of the variability observed in LISAT. In addition, we used f-square to measure the effect of any exogenous variable on R-square when an exogenous variable is removed from the model. The analysis of the f-square (with control variable) shows that both PHQ (0.263) and DSS (0.553) have a medium and large effect on LISAT, respectively. The f-square (with control variable) for DSS (0.005 < 0.020) has a small effect on the PHQ, implying that dropping DSS would have little impact on the explanatory power of the PHQ. The results of the Q-square value for all reflective endogenous latent variables were greater than zero, indicating that our values were well reconstructed and that the model had achieved predictive relevance.
Table 7.
Predictive relevance using f-square, adjusted R-square, Q-square analysis and Cross-validated predictive ability test (CVPAT).
| LISAT f-square without control variable (with control variable) [VIF] | PHQ f-square without control variable (with control variable) [VIF] | DSS f-square without control variable (with control variable) [VIF] | Adjusted R-Square without control variable | Adjusted R-Square with control variable | Q-Square without control variable | Q-Square with control variable | |
|---|---|---|---|---|---|---|---|
| LISAT | 0.522 | 0.518 | 0.926 | 0.928 | |||
| PHQ | 0.265 (0.263) [1.096] | 0.075 | 0.075 | 0.210 | 0.208 | ||
| DSS | 0.589 (0.553) [1.134] | 0.006 (0.005) [1.128] | 0.070 | 0.103 | 0.741 | 0.746 | |
| SES | 0.003 (0.004) [1.189] | 0.059 (0.055) [1.127] | 0.077 (0.078) [1.046] |
| Average loss difference | t-values | p-values | |||||
|---|---|---|---|---|---|---|---|
| Cross-validated predictive ability test (CVPAT) | |||||||
| CVPAT without control variable | |||||||
| LISAT | − 0.060 | 2.259 | 0.024* | ||||
| PHQ | − 0.014 | 2.514 | 0.012* | ||||
| DSS | − 0.028 | 2.538 | 0.011* | ||||
| Overall | − 0.038 | 2.624 | 0.009* | ||||
| CVPAT with control variable | |||||||
| LISAT | − 0.072 | 2.386 | 0.017* | ||||
| PHQ | − 0.014 | 2.159 | 0.031* | ||||
| DSS | − 0.044 | 2.925 | 0.004* | ||||
| Overall | − 0.045 | 2.809 | 0.005* | ||||
*Significant at 5%.
In addition to the above analysis, Liengaard et al.92 extended the model’s predictive relevance using a cross-validated predictive ability test (CVPAT). CVPAT applies an out-of-sample prediction approach to calculate the structural model’s prediction error. This method also calculates the average loss value of PLS-SEM, compared with the average loss value of the indicator averages and the linear model, which are used as naive and conservative benchmarks, respectively. To substantiate better predictive capabilities of the model compared to the prediction benchmarks, CVPAT tests whether PLS-SEM’s average loss is significantly lower than the average loss of the benchmarks93. Therefore, results in Table 5 show that PLS-SEM’s average loss with and without control variables was significantly lower than the average loss of the benchmarks. A negative difference in the average loss values implies that our model has better predictive capabilities.
Discussion and policy implications
Two main theories about the LISAT exist in the current literature, namely, the bottom-up and top-down theories, first distinguished by Diener94. Bottom-up theories consider LISAT to be summary judgments of satisfaction with important life domains, while top-down theories assume that LISAT has a global halo effect on satisfaction with specific life domains95. In other words, the bottom-up theories of LISAT are based on the idea that LISAT is the sum of its parts overall. In contrast, top-down theories rest on the premise that satisfaction with domains of life is mainly a consequence of overall LISAT96. We have observed that both bottom-up and top-down theories face causality dilemmas: the problems with sorting time sequences. Despite such claims to the contrary, Tuncay and Avcı14 found that LISAT is a significant predictor of diabetes. Therefore, given the increasing burden of diabetes, it is recommended to use a mixed approach to study the causes of LISAT, and through causation, linking its multidimensional effects is suggested by several studies5,18. As a result, like many studies, we used a bottom-up approach to interpret LISAT and analysed its multivariate effects using a top-down approach for diabetes patients15,16.
Our results revealed that SES positively impacts LISAT, PHQ and DSS among diabetes patients in India. In the study area, a 1% rise in SES will improve diabetes patients’ LISAT, PHQ and DSS scores by 0.135%, 0.492%, and 0.280%, respectively. Patients with higher SES receive more diabetes care and can better manage their complications, improving their mental health and LISAT. Strengthening the SES level of the patient through its various domains helps patients cope with diabetes-related issues and reduces the overall burden on society97. Consequently, the study by Baumann et al. and Houle et al. recommends that strengthening patients’ SES can improve outcomes in diabetes patients21,98.
The outcomes showed that PHQ and DSS were negatively associated with LISAT. This implies that fragmented health policies nationwide and a lack of government support for diabetes patients prevent them from achieving high LISAT99. According to Gwozdz and Sousa-Poza’s 100 study, a higher LISAT not only enables diabetes patients to recover more quickly, preserve their lifespan and be more productive, but it also reduces the overall burden on the nation. However, India has limited diabetes treatment facilities and effective management programs, which accounts for the significant differences between LISAT, PHQ and DSS among diabetes patients9,101,102.
Furthermore, the direct effect results with control variables revealed that patients residing in rural areas perceived higher DSS than their urban counterparts. Deepa et al.103 found that knowledge and awareness about diabetes in India, particularly in rural areas, is poor compared to urban areas. At the same time, the availability and utilisation of healthcare services and diabetes-related complications vary between rural and urban areas104–106. This means that rural-specific diabetes-care planning needs to be strengthened in the study area. Besides, we found that patients with increased age perceived lower discomfort due to DSS. A study on symptoms by Tibblin et al.107 showed that self-reported symptoms generally decreased with age. In addition, biological changes that occur with ageing affect patients’ personal and social responses, which may lead to under-reporting symptoms’ severity108.
The importance of social constructs such as gender and their significant association with diabetes, LISAT and PHQ has also been highlighted by several studies51,109,110. Similarly, our study revealed a gender difference in all the endogenous variables (LISAT, PHQ and DSS), with women perceiving greater DSS and PHQ than men, which may lower their LISAT. As a result, Kim et al.50 suggest that gender disaggregated policy may provide an opportunity to increase LISAT. In line with our results, the importance of studying socioeconomic and demographic aspects in reducing the burden of diabetes has been highlighted by the study of Wang et al.111. Our research will thus assist policymakers in concentrating on those patients who actually require improvement. The results of the study may contribute to better healthcare delivery for such a large number of diabetes patients, especially those whose LISAT is affected by SES, DSS and depression.
Conclusion
This article explores the underlying association between SES and LISAT through a lens of PHQ and DSS, examining their multidimensional impact across various demographic variables. The present study’s data was collected from diabetes patients in Punjab, India, and PLS-SEM was used to test multiple hypotheses. The results showed that SES was the primary factor affecting LISAT, PHQ and DSS in the case of diabetes patients. Therefore, improving the SES of patients can lead to an overall improvement in disease management and help reduce the overall disease burden in the country. This implies that our study has practical implications for policymakers, which may assist them in doing interventions related to SES, LISAT, PHQ and DSS, perhaps resulting in multidimensional benefits to diabetes patients in India.
Additionally, we have identified breathtaking possibilities for future research in this area. Although this paper focused only on Punjab, India, it would be worthwhile to consider LISAT predictions in different states of India and various countries using cross-national data. The availability of panel data would make it possible to control unseen heterogeneity and move towards making predictions about causal relationships between LISAT and SES in the case of diabetes patients. Furthermore, this study's scope could extend to other chronic diseases such as cancer, cardiovascular diseases, etc. Since we found little research on LISAT predictors of such health conditions where the existing studies have been conducted in developed countries. Nevertheless, we found some evidence about the importance of SES in interpreting the LISAT in the literature, but their context was narrow as opposed to broad measures of SES. Despite several limitations, this study provides valuable insights for policymakers to conduct comprehensive studies on such predictors, which will help them control the disease burden and improve the overall LISAT of the patients in the country.
Supplementary Information
Acknowledgements
The authors are grateful to all the patients with diabetes who participated in this study.
Author contributions
S.R. and R.T. conceived the idea. S.R. performed the statistical analysis and prepared the initial draft of the manuscript. R.T. revised the manuscript. Both authors read and approved the final manuscript.
Funding
There is no funding involved in this study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-62814-5.
References
- 1.Jonsson B. The economic impact of diabetes. Diabetes Care. 1998;21:C7–C10. doi: 10.2337/diacare.21.3.C7. [DOI] [PubMed] [Google Scholar]
- 2.Ong KL, et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the global burden of disease study 2021. The Lancet. 2023;402:203–234. doi: 10.1016/S0140-6736(23)01301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020;10:14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandey S, Sharma V. World diabetes day 2018: Battling the emerging epidemic of diabetic retinopathy. Indian J. Ophthalmol. 2018;66:1652. doi: 10.4103/ijo.IJO_1681_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pradeepa R, Deepa R, Mohan V. Epidemiology of diabetes in India–current perspective and future projections. J. Indian Med. Assoc. 2002;100:144–148. [PubMed] [Google Scholar]
- 6.Oberoi S, Kansra P. Economic menace of diabetes in India: A systematic review. Int. J. Diabetes Dev. Ctries. 2020;40:464–475. doi: 10.1007/s13410-020-00838-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moeineslam M, et al. Diabetes in women and health-related quality of life in the whole family: A structural equation modeling. Health Qual. Life Outcomes. 2019;17:178. doi: 10.1186/s12955-019-1252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alhaik S, Anshasi HA, Alkhawaldeh J, Soh KL, Naji AM. An assessment of self-care knowledge among patients with diabetes mellitus. Diabetes Metab. Syndr.: Clin. Res. Rev. 2019;13:390–394. doi: 10.1016/j.dsx.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Mendenhall E, Narayanan G, Prabhakaran D. Depression and diabetes in India: Perspectives and recommendations: Depression and diabetes in India. Diabetic Med. 2012;29:e308–e311. doi: 10.1111/j.1464-5491.2012.03708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banker KK, et al. The impact of diabetes on productivity in India. Diabetes Care. 2021;44:2714–2722. doi: 10.2337/dc21-0922. [DOI] [PubMed] [Google Scholar]
- 11.Bansode B, Jungari DS. Economic burden of diabetic patients in India: A review. Diabetes Metab. Syndr.: Clin. Res. Rev. 2019;13:2469–2472. doi: 10.1016/j.dsx.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 12.Drivsholm T, De Fine Olivarius N, Nielsen ABS, Siersma V. Symptoms, signs and complications in newly diagnosed type 2 diabetic patients, and their relationship to glycaemia, blood pressure and weight. Diabetologia. 2005;48:210–214. doi: 10.1007/s00125-004-1625-y. [DOI] [PubMed] [Google Scholar]
- 13.Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys. Ther. 2008;88:1254–1264. doi: 10.2522/ptj.20080020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuncay FÖ, Avcı D. Association between self-care management and life satisfaction in patients with diabetes mellitus. Eur. J. Integr. Med. 2020;35:101099. doi: 10.1016/j.eujim.2020.101099. [DOI] [Google Scholar]
- 15.Hoothay F, DeStefano A, Leary E, Foley-Hartel T. Life satisfaction and coping of diabetic hemodialysis patients. ANNA J. 1990;17:361–364. [PubMed] [Google Scholar]
- 16.Priya M. A study on life satisfaction level among persons with diabetes IOSR-J. Humanit. Soc. Sci. 2017;3:51–55. [Google Scholar]
- 17.Hall A. Life satisfaction, concept of. In: Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Netherlands: Springer; 2014. pp. 3599–3601. [Google Scholar]
- 18.Mauricio D. Quality of life and treatment satisfaction are highly relevant patient-reported outcomes in type 2 diabetes mellitus. Ann. Transl. Med. 2018;6:220–220. doi: 10.21037/atm.2018.04.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee L, Hsieh C, Lin Y. Life satisfaction and emotional distress in people living with type 2 diabetes mellitus: The mediating effect of cognitive function. J. Clin. Nurs. 2021;30:2673–2682. doi: 10.1111/jocn.15740. [DOI] [PubMed] [Google Scholar]
- 20.Charzyńska E, Kocur D, Działach S, Brenner RE. Testing the indirect effect of type 1 diabetes on life satisfaction through self-compassion and self-coldness. Mindfulness. 2020;11:2486–2493. doi: 10.1007/s12671-020-01450-2. [DOI] [Google Scholar]
- 21.Baumann M, Tchicaya A, Lorentz N, Le Bihan E. Life satisfaction and longitudinal changes in physical activity, diabetes and obesity among patients with cardiovascular diseases. BMC Public Health. 2017;17:925. doi: 10.1186/s12889-017-4925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dubey A, Agarwal A. Coping strategies and life satisfaction: Chronically ill patients’ perspectives. J. Ind. Acad. Appl. Psychol. 2007;33:161–168. [Google Scholar]
- 23.Okwaraji FE, Onyebueke GC, Nduanya CU, Nwokpoku EN. Life satisfaction, self esteem and mental health in a sample of diabetic out-patients attending a Nigerian tertiary health institution. J. Med. Res. 2017;3:60–65. doi: 10.31254/jmr.2017.3207. [DOI] [Google Scholar]
- 24.Koivumaa-Honkanen H. Self-reported life satisfaction and 20-year mortality in healthy finnish adults. Am. J. Epidemiol. 2000;152:983–991. doi: 10.1093/aje/152.10.983. [DOI] [PubMed] [Google Scholar]
- 25.Rosella LC, Fu L, Buajitti E, Goel V. Death and chronic disease risk associated with poor life satisfaction: A population-based cohort study. Am. J. Epidemiol. 2019;188:323–331. doi: 10.1093/aje/kwy245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guven C, Saloumidis R. Life satisfaction and longevity: Longitudinal evidence from the German socio-economic panel. German Econ. Rev. 2014;15:453–472. doi: 10.1111/geer.12024. [DOI] [Google Scholar]
- 27.Kimm H, Sull JW, Gombojav B, Yi S-W, Ohrr H. Life satisfaction and mortality in elderly people: The Kangwha cohort study. BMC Public Health. 2012;12:54. doi: 10.1186/1471-2458-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu J, Roberts RE. The power of positive emotions: It’s a matter of life or death—Subjective well-being and longevity over 28 years in a general population. Health Psychol. 2010;29:9–19. doi: 10.1037/a0016767. [DOI] [PubMed] [Google Scholar]
- 29.Melin R, Fugl-Meyer KS, Fugl-Meyer AR. Life satisfaction in 18- to 64-year-old Swedes: In relation to education, employment situation, health and physical activity. J. Rehabil. Med. 2003;35:84–90. doi: 10.1080/16501970306119. [DOI] [PubMed] [Google Scholar]
- 30.Nakamura JS, Delaney SW, Diener E, VanderWeele TJ, Kim ES. Are all domains of life satisfaction equal? Differential associations with health and well-being in older adults. Qual. Life Res. 2022;31:1043–1056. doi: 10.1007/s11136-021-02977-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Imayama I, Plotnikoff RC, Courneya KS, Johnson JA. Determinants of quality of life in adults with type 1 and type 2 diabetes. Health Qual. Life Outcomes. 2011;9:115. doi: 10.1186/1477-7525-9-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baker EH. Socioeconomic status, definition. In: Cockerham WC, Dingwall R, Quah S, editors. The wiley blackwell encyclopedia of health, illness, behavior, and society. Chichester: Wiley; 2014. pp. 2210–2214. [Google Scholar]
- 33.Bollen KA, Bauldry S. Three Cs in measurement models: Causal indicators, composite indicators, and covariates. Psychol. Methods. 2011;16:265–284. doi: 10.1037/a0024448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramesh Masthi N, Kulkarni P. An exploratory study on socio economic status scales in a rural and urban setting. J. Family Med. Prim. Care. 2013;2:69. doi: 10.4103/2249-4863.109952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bhatnagar N, Dudeja P, Bahuguna P, Singh A. Refining a socio-economic status scale for use in community-based health research in India. J. Postgrad. Med. 2015;61:77. doi: 10.4103/0022-3859.150442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang R, Zhang T, Langhammer B. Activities of daily living and life satisfaction of persons with stroke after rehabilitation in China: A longitudinal descriptive study. Top. Stroke Rehabi. 2019;26:113–121. doi: 10.1080/10749357.2018.1550615. [DOI] [PubMed] [Google Scholar]
- 37.Ekstrand E, Lexell J, Brogårdh C. Test-retest reliability of the life satisfaction questionnaire (LiSat-11) and association between items in individuals with chronic stroke. J. Rehabil. Med. 2018;50:713–718. doi: 10.2340/16501977-2362. [DOI] [PubMed] [Google Scholar]
- 38.Hashim HM, Abd Allah ES, Ali El-Zeiny HH. Thantophobia, spirituality and life satisfaction among community dwelling elderly. Zagazig Nurs. J. 2021;17:85–99. [Google Scholar]
- 39.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolfgram P, Zhang L, Simpson P, Fiallo-Scharer R. Clinical associations of quarterly patient health questionnaire-9 depression screening results in adolescents with type 1 diabetes. Pediatr. Diabetes. 2020;21:871–877. doi: 10.1111/pedi.13017. [DOI] [PubMed] [Google Scholar]
- 41.Nouwen A, et al. Measurement invariance testing of the patient health questionnaire-9 (PHQ-9) across people with and without diabetes mellitus from the NHANES, EMHS and UK Biobank datasets. J. Affect. Disord. 2021;292:311–318. doi: 10.1016/j.jad.2021.05.031. [DOI] [PubMed] [Google Scholar]
- 42.Le Dinh T, et al. The relationship between depression and multifactorial control and microvascular complications in vietnamese with Type 2 diabetes mellitus aged 30–60 years. DMSO. 2022;15:1185–1195. doi: 10.2147/DMSO.S354443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cichoń E, et al. People with diabetes need a lower cut-off than others for depression screening with PHQ-9. PLoS ONE. 2020;15:e0240209. doi: 10.1371/journal.pone.0240209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Udedi M, Muula AS, Stewart RC, Pence BW. The validity of the patient health Questionnaire-9 to screen for depression in patients with type-2 diabetes mellitus in non-communicable diseases clinics in Malawi. BMC Psychiatry. 2019;19:81. doi: 10.1186/s12888-019-2062-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reddy P, Philpot B, Ford D, Dunbar JA. Identification of depression in diabetes: The efficacy of PHQ-9 and HADS-D. Br J. Gen. Pract. 2010;60:e239–e245. doi: 10.3399/bjgp10X502128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ramachandran A. Know the signs and symptoms of diabetes. Indian J. Med. Res. 2014;140:579–581. [PMC free article] [PubMed] [Google Scholar]
- 47.Cloete L. Diabetes mellitus: An overview of the types, symptoms, complications and management. Nurs. Stand. 2022;37:61–66. doi: 10.7748/ns.2021.e11709. [DOI] [PubMed] [Google Scholar]
- 48.Ellenberg M. Diabetic complications without manifest diabetes: Complications as presenting clinical symptoms. JAMA. 1963;183:926–930. doi: 10.1001/jama.1963.03700110058011. [DOI] [Google Scholar]
- 49.WHO. Diabetes. https://www.who.int/news-room/fact-sheets/detail/diabetes (2023).
- 50.Kim J, Lee M, Dan H. Gender differences in factors affecting life satisfaction of the elderly with multimorbidity in Korea. Nurs. Rep. 2021;11:54–63. doi: 10.3390/nursrep11010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gigantesco A, et al. The relationship between satisfaction with life and depression symptoms by gender. Front. Psychiatry. 2019;10:419. doi: 10.3389/fpsyt.2019.00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ramachandran A, Snehalatha C. Current scenario of diabetes in India: Diabetes in India. J. Diabetes. 2009;1:18–28. doi: 10.1111/j.1753-0407.2008.00004.x. [DOI] [PubMed] [Google Scholar]
- 53.Corsi DJ, Subramanian SV. Association between socioeconomic status and self-reported diabetes in India: A cross-sectional multilevel analysis. BMJ Open. 2012;2:e000895. doi: 10.1136/bmjopen-2012-000895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res. Clin. Pract. 2005;68:230–236. doi: 10.1016/j.diabres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 55.Seiglie JA, et al. Diabetes prevalence and its relationship with education, wealth, and BMI in 29 low- and middle-income countries. Diabetes Care. 2020;43:767–775. doi: 10.2337/dc19-1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mathisen J, et al. Education and incident type 2 diabetes: quantifying the impact of differential exposure and susceptibility to being overweight or obese. Diabetologia. 2020;63:1764–1774. doi: 10.1007/s00125-020-05150-3. [DOI] [PubMed] [Google Scholar]
- 57.Brown AF, et al. Socioeconomic position and health among persons with diabetes mellitus: A conceptual framework and review of the literature. Epidemiol. Rev. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 58.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. Int. J. Epidemiol. 2011;40:804–818. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 59.Williams J, et al. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J. Global Health. 2018;8:020409. doi: 10.7189/jogh.08.020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Corsi DJ, Subramanian SV. Socioeconomic gradients and distribution of diabetes, hypertension, and obesity in India. JAMA Netw. Open. 2019;2:e190411. doi: 10.1001/jamanetworkopen.2019.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shrivastava U, Misra A, Gupta R, Viswanathan V. Socioeconomic factors relating to diabetes and its management in India: 印度与糖尿病及其治疗相关的社会经济因素. J. Diabetes. 2016;8:12–23. doi: 10.1111/1753-0407.12316. [DOI] [PubMed] [Google Scholar]
- 62.Daraei M, Mohajery A. The impact of socioeconomic status on life satisfaction. Soc. Indic. Res. 2013;112:69–81. doi: 10.1007/s11205-012-0040-x. [DOI] [Google Scholar]
- 63.Mirmoghtadaee P, et al. The association of socioeconomic status of family and living region with self-rated health and life satisfaction in children and adolescents: The CASPIAN-IV study. Med. J. Islam Repub. Iran. 2016;30:423. [PMC free article] [PubMed] [Google Scholar]
- 64.Rajabi Gilan N, Khezeli M, Zardoshtian S. The effect of self-rated health, subjective socioeconomic status, social capital, and physical activity on life satisfaction: A cross-sectional study in urban western Iran. BMC Public Health. 2021;21:233. doi: 10.1186/s12889-021-10261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hsieh C. Counting importance: The case of life satisfaction and relative domain importance. Soc. Indic. Res. 2003;61:227–240. doi: 10.1023/A:1021354132664. [DOI] [Google Scholar]
- 66.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes/Metab. Res. Rev. 1999;15:205–218. doi: 10.1002/(SICI)1520-7560(199905/06)15:3<205::AID-DMRR29>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 67.Castillo-Carniglia Á, Albala C, Dangour AD, Uauy R. Factores asociados a satisfacción vital en una cohorte de adultos mayores de Santiago. Chile. Gaceta Sanitaria. 2012;26:414–420. doi: 10.1016/j.gaceta.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 68.Clark NG, Fox KM, Grandy S, for the SHIELD Study Group Symptoms of diabetes and their association with the risk and presence of diabetes. Diabetes Care. 2007;30:2868–2873. doi: 10.2337/dc07-0816. [DOI] [PubMed] [Google Scholar]
- 69.Millett C, Saxena S, Ng A, Mainous A, Majeed A. Socio-economic status, ethnicity and diabetes management: An analysis of time trends using the health survey for England. J. Public Health. 2007;29:413–419. doi: 10.1093/pubmed/fdm058. [DOI] [PubMed] [Google Scholar]
- 70.Osborn CY, Groot MD, Wagner JA. Racial and ethnic disparities in diabetes complications in the Northeastern United States: The role of socioeconomic status. J. Natl. Med. Assoc. 2013;105:51–58. doi: 10.1016/s0027-9684(15)30085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gulliford MC, Mahabir D. Relationship of health-related quality of life to symptom severity in diabetes mellitus. J. Clin. Epidemiol. 1999;52:773–780. doi: 10.1016/S0895-4356(99)00053-0. [DOI] [PubMed] [Google Scholar]
- 72.Leone T, Coast E, Narayanan S, De Graft Aikins A. Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): a mapping of the evidence. Global Health. 2012;8:39. doi: 10.1186/1744-8603-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J. Psychosom. Res. 2002;53:891–895. doi: 10.1016/S0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 74.Tekir O. The effect of diabetes symptoms on quality of life in individuals with Type 2 diabetes. Acta Endo. (Buc) 2021;17:186–193. doi: 10.4183/aeb.2021.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim J-H, Lee Y-J. A study of andropause symptoms and life satisfaction among middle-aged men. J. Korean Acad. Commun. Health Nurs. 2005;16(2):186–195. doi: 10.4040/jkan.2005.35.1.186. [DOI] [Google Scholar]
- 76.Holt RIG, De Groot M, Golden SH. Diabetes and depression. Curr. Diab. Rep. 2014;14:491. doi: 10.1007/s11892-014-0491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Grootenhuis PA, Snoek FJ, Heine RJ, Bouter LM. Development of a Type 2 diabetes symptom checklist: A measure of symptom severity. Diabetic Med. 1994;11:253–261. doi: 10.1111/j.1464-5491.1994.tb00268.x. [DOI] [PubMed] [Google Scholar]
- 78.Katon WJ. The comorbidity of diabetes mellitus and depression. Am. J. Med. 2008;121:S8–S15. doi: 10.1016/j.amjmed.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Onwuegbuzie A, Collins K. A typology of mixed methods sampling designs in social science research. TQR. 2015 doi: 10.46743/2160-3715/2007.1638. [DOI] [Google Scholar]
- 80.Government of India. Census - 2011. https://censusindia.gov.in/2011-Common/Archive.html (2011).
- 81.WHO. STEPwise approach to NCD risk factor surveillance (STEPS). https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps.
- 82.Ringle, C. M., Wende, S. & Becker, J.-M. SmartPLS 4. SmartPLS (2022).
- 83.Hair JF, Risher JJ, Sarstedt M, Ringle CM. When to use and how to report the results of PLS-SEM. EBR. 2019;31:2–24. doi: 10.1108/EBR-11-2018-0203. [DOI] [Google Scholar]
- 84.Hanafiah MH. Formative vs. reflective measurement model: Guidelines for structural equation modeling research. Int. J. Anal. Appl. 2020;18:876–889. [Google Scholar]
- 85.Murri MB, et al. The interplay between diabetes, depression and affective temperaments: A structural equation model. J. Affect. Disord. 2017;219:64–71. doi: 10.1016/j.jad.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 86.Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE. Understanding the influence of psychological and socioeconomic factors on diabetes self-care using structured equation modeling. Patient Educ. Couns. 2015;98:34–40. doi: 10.1016/j.pec.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jarvis CB, MacKenzie SB, Podsakoff PM. A critical Review of construct indicators and measurement model misspecification in marketing and consumer research. J. Consum. Res. 2003;30:199–218. doi: 10.1086/376806. [DOI] [Google Scholar]
- 88.Hair JF, et al. Partial least squares structural equation modeling (PLS-SEM) Using R: A Workbook. Cham: Springer; 2021. [Google Scholar]
- 89.Hair JF, Hult GTM, Ringle CM, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM) Melbourne: SAGE; 2022. [Google Scholar]
- 90.Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015;43:115–135. doi: 10.1007/s11747-014-0403-8. [DOI] [Google Scholar]
- 91.Cheah J-H, Sarstedt M, Ringle CM, Ramayah T, Ting H. Convergent validity assessment of formatively measured constructs in PLS-SEM: On using single-item versus multi-item measures in redundancy analyses. IJCHM. 2018;30:3192–3210. doi: 10.1108/IJCHM-10-2017-0649. [DOI] [Google Scholar]
- 92.Liengaard BD, et al. Prediction: Coveted, yet forsaken? introducing a cross-validated predictive ability test in partial least squares path modeling. Decis. Sci. 2021;52:362–392. doi: 10.1111/deci.12445. [DOI] [Google Scholar]
- 93.Sharma PN, Liengaard BD, Hair JF, Sarstedt M, Ringle CM. Predictive model assessment and selection in composite-based modeling using PLS-SEM: Extensions and guidelines for using CVPAT. EJM. 2023;57:1662–1677. doi: 10.1108/EJM-08-2020-0636. [DOI] [Google Scholar]
- 94.Diener E. Subjective well-being. Psychol. Bull. 1984;95:542–575. doi: 10.1037/0033-2909.95.3.542. [DOI] [PubMed] [Google Scholar]
- 95.Scherpenzeel A, Saris W. Causal direction in a model of life satisfaction: The top-down/bottom-up controversy. Soc. Indic. Res. 1996;38:161–180. doi: 10.1007/BF00300457. [DOI] [Google Scholar]
- 96.Headey B, Veenhoven R, Wearing A. Top-down versus bottom-up theories of subjective well-being. Soc. Indic. Res. 1991;24:81–100. doi: 10.1007/BF00292652. [DOI] [Google Scholar]
- 97.Hill-Briggs F, et al. Social determinants of health and diabetes: A scientific review. Diabetes Care. 2021;44:258–279. doi: 10.2337/dci20-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Houle J, et al. Socioeconomic status and glycemic control in adult patients with type 2 diabetes: A mediation analysis. BMJ Open Diabetes Res. Care. 2016;4:e000184. doi: 10.1136/bmjdrc-2015-000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Aarthy R, et al. Quality of life and diabetes in India: A scoping review. Indian J. Endocr. Metab. 2021;25:365. doi: 10.4103/ijem.ijem_336_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gwozdz W, Sousa-Poza A. Ageing, health and life satisfaction of the oldest old: An analysis for Germany. Soc. Indic. Res. 2010;97:397–417. doi: 10.1007/s11205-009-9508-8. [DOI] [Google Scholar]
- 101.Kumar A. India towards diabetes control: Key issues. AMJ. 2013;6:524–531. doi: 10.4066/AMJ.2013.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Das AK, et al. Health care delivery model in India with relevance to diabetes care. Heliyon. 2022;8:e10904. doi: 10.1016/j.heliyon.2022.e10904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Deepa M, et al. Knowledge and awareness of diabetes in urban and rural India: The Indian Council of Medical Research India diabetes study (Phase I): Indian Council of Medical Research India diabetes 4. Indian J. Endocr. Metab. 2014;18:379. doi: 10.4103/2230-8210.131191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tai S-Y, He J-S, Kuo C-T, Kawachi I. Urban-rural disparities in the incidence of diabetes-related complications in Taiwan: A propensity score matching analysis. JCM. 2020;9:3012. doi: 10.3390/jcm9093012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Banerjee S. Determinants of rural-urban differential in healthcare utilization among the elderly population in India. BMC Public Health. 2021;21:939. doi: 10.1186/s12889-021-10773-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shergill HS. Rural-urban disparity in the standard of living across states of India. Econ. Political Weekly. 2021;56:20220034391. [Google Scholar]
- 107.Tibblin G, Bengtsson C, Furunes B, Lapidus L. Symptoms by age and sex: The population studies of men and women in Gothenburg, Sweden. Scand. J. Prim. Health Care. 1990;8:9–17. doi: 10.3109/02813439008994923. [DOI] [PubMed] [Google Scholar]
- 108.Boss GR, Seegmiller JE. Age-related physiological changes and their clinical significance. West J Med. 1981;135:434–440. [PMC free article] [PubMed] [Google Scholar]
- 109.Fernández-Ballesteros R, Dolores Zamarrón M, Angel Ruíz M. The contribution of socio-demographic and psychosocial factors to life satisfaction. Ageing Soc. 2001;21:25–43. doi: 10.1017/S0144686X01008078. [DOI] [Google Scholar]
- 110.Ranjan S, Thakur R. Gender differential in awareness and risk factors of diabetes among diabetes patients in India. J. Public Health (Berl.) 2023 doi: 10.1007/s10389-023-01933-1. [DOI] [Google Scholar]
- 111.Wang Z, Li X, Chen M. Socioeconomic factors and inequality in the prevalence and treatment of diabetes among middle-aged and elderly adults in China. J. Diabetes Res. 2018;2018:1–12. doi: 10.1155/2018/1471808. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.