Abstract
Introduction:
Evidence suggests that psychedelics may serve as a therapeutic approach to reduce substance use; however, racial and ethnic minoritized (REM) people are often excluded from this research. We investigated whether psychedelic use affects other substance use among REM people and whether perceived changes in psychological flexibility and racial trauma mediates this association.
Methods:
REM people in the United States and Canada (N=211; 32% Black, 29% Asian, 18% American Indian/Indigenous Canadian, 21% Native Hawaiian/Pacific Islander; 57% female; mean age=33.1, SD=11.2) completed an online survey retrospectively reporting their substance use, psychological flexibility, and racial trauma symptoms 30 days before and after their most memorable psychedelic experience.
Results:
Analyses showed a significant perceived reduction in alcohol (p<.0001, d=.54) and drug use (p=.0001, d=.23) from before to after the psychedelic experience. Preliminary associations found perceived reductions in racial trauma symptoms were associated with perceived reductions in alcohol use and this association varied by race, dose, ethnic identity, and change in depressive symptoms. Specifically, Indigenous participants experienced greater perceived reductions in alcohol use relative to participants who identified as Asian, Black, or other. Those who took a high dose of psychedelics experienced greater perceived reductions in alcohol use relative to those who took a low dose. Participants with a stronger ethnic identity and those with a perceived reduction in depressive symptoms experienced a perceived reduction in alcohol use. Serial mediation indicated a perceived increase in psychological flexibility and reduction in racial trauma symptoms mediated the association between acute psychedelic effects and perceived reductions in alcohol and drug use.
Conclusion:
These findings suggest that psychedelic experiences may contribute to an increase in psychological flexibility and reduction in racial trauma symptoms and alcohol and drug use among REM people. REM people have been largely excluded from psychedelic treatment research even though psychedelic use is considered a traditional healing practice in many communities of color. Longitudinal studies of REM people should replicate our findings.
Keywords: Psychedelic, Alcohol, Drug, Racial trauma, Racial or Ethnic Minoritized
1. Introduction
Risky drug and alcohol use is a major public health concern worldwide, including in the United States and Canada (Peacock et al., 2018; World Health Organization, 2019), highlighting the importance of continued research on effective treatments for substance use disorders. Evidence suggests that psychedelics (e.g., psilocybin/mushrooms, lysergic acid diethylamide [LSD], 3,4-Methylenedioxymethamphetamine [MDMA]/ecstasy) may serve as a viable treatment. A systematic review of psychedelic clinical studies (Andersen et al., 2021) reported that administration of psilocybin resulted in significant reductions in heavy drinking days and drinking days overall. This review also reported that psilocybin resulted in significant reductions in self‐ reported daily smoking, urine cotinine, and breath carbon monoxide and that 67% of participants remained abstinent from smoking after 12 months (Andersen et al., 2021). Additional research should seek to understand the therapeutic effects of psychedelics; however, some evidence suggests that the intensity of acute subjective effects are important, such as acute mystical-type experiences (e.g., feelings of amazement; assessed using the Mystical Experience Questionnaire [MEQ]; Barrett et al., 2015; MacLean et al., 2012) and acute insight experiences related to emotions, beliefs, memories, and relationships (assessed using the Psychological Insight Questionnaire [PIQ]; Davis et al., 2021).
Despite evidence that psychedelic use may contribute to significant reductions in substance use, most prior studies have included few racial and ethnic minoritized (REM) people. A literature review of 18 randomized controlled psychedelic-assisted psychotherapy studies reported that more than 80% of participants were non-Hispanic White (Michaels et al., 2018). This trend may exist due in part to the Western world’s attempts to restrict the use of psychedelics and incarcerate those who use them, as seen with the US government’s efforts to restrict the use and cultivation of peyote and other psychedelic substances with the 1970 Controlled Substance Act (Feeney, 2017; Gray, 1994). These efforts ultimately contributed to the stigmatization of psychedelic substances and have disproportionately affected REM people, particularly those communities that have used psychedelics as a form of traditional healing like many Indigenous communities (George et al., 2019; Moore & Elkavich, 2008). Although psychedelics are slowly becoming an accepted form of treatment, REM people are often not included in research efforts to understand the effects of psychedelics on mental health and substance use.
In addition to including REM people in psychedelic research, we must include constructs particularly relevant to the experience of being a person with a REM identity, such as racial trauma. Racial trauma can be described as severely stressful experiences of racism (Williams, Metzger, et al., 2018). REM people are more likely to experience racial discrimination, which can be experienced as stressful and contribute to the development of trauma symptoms (e.g., hypervigilance, avoidance) (Bryant-Davis & Ocampo, 2005; Holmes et al., 2016; Kirkinis et al., 2018). Racial trauma is understudied and may be experienced in the form of everyday discrimination (e.g., followed in a store), major discrimination (e.g., denied a mortgage loan), as part of historical or cultural traumas including the colonization of communities of color (Gone et al., 2019), direct overt threats of violence, vicarious trauma by learning about racial trauma experienced by loved ones or of people you do not know with the same racial identity as you, and microaggressions (Williams, Metzger, et al., 2018). The US Department of Justice reported that 49.2% of Black, 10.8% of Latine, 6.8% of Asian, 6.8% of American Indian or Alaska Native, and 3.1% of multiracial people have experienced a race-based hate crime in the past year (FBI, 2019), though these are likely underestimates given that many racist events go unreported. Notably, since the global coronavirus 2019 pandemic, these numbers have increased particularly among Asian American people, from 2.7% of single incident hate crimes in 2019 to 6.8% in 2021 (Chen et al., 2020). In Canada, Indigenous, Black, Asian, Southwest Asian, Arab, Latine, other, and multiracial adults were 74% more likely than White adults to report racial discrimination (Godley, 2018). Multiple meta-analyses and systematic reviews indicate an association between experiencing racial discrimination and poor health outcomes (e.g., substance use, depression, anxiety, psychological distress; Carter et al., 2019; Paradies et al., 2015; Williams et al., in press; Pieterse et al., 2012).
Cross-sectional and prospective studies indicate racial discrimination is associated with increased substance use (Boynton et al., 2015; Carter et al., 2019; Clark et al., 2015; Currie et al., 2015; Desalu et al., 2019; Gibbons et al., 2010; Gibbons et al., 2004). A meta-analysis of the association of racial discrimination and alcohol-related behaviors among Black people found racial discrimination was associated with increased alcohol use and alcohol-related problems (Desalu et al., 2019). Further, a meta-analysis of Black, Asian, Latine, Indigenous, and multiracial individuals found that racial discrimination was associated with increased substance use (Carter et al., 2019). Given that racial discrimination can contribute to trauma symptoms and related psychopathology, it is essential to consider the mental health sequelae of racial discrimination in relation to substance use outcomes.
One study sought to address inequities in psychedelic research by specifically recruiting a racially and ethnically diverse sample across the US and Canada and found that psychedelic use was associated with perceived reductions in mental health symptoms including racial trauma (Williams et al., 2021). In addition, this research team found that perceived increases in psychological flexibility mediated the relation between acute psychedelic experiences and perceived reductions in racial trauma symptoms (Davis et al., 2021). Psychological flexibility can be described as the capacity to persist in engaging in values-consistent behaviors in the face of negative events or stressors (Gloster et al., 2017; Kashdan & Rottenberg, 2010). Evidence suggests that psychedelics can contribute to increased psychological flexibility and may be an important mechanism that results in improved outcomes (Close et al., 2020; Davis et al., 2021). Prior studies have found that an increase in psychological flexibility was a mechanism that partially explained the effectiveness of various treatments for substance use disorders (Lin et al., 2015; Marchand et al., 2018; Rosen et al., 2020). Using a subsample from prior studies (Davis et al., 2021; Williams et al., 2021), the objective of the current study is to expand prior research to elucidate whether psychedelic use contributes to perceived reductions in other substance use among REM people. We hypothesized that perceived increased psychological flexibility and a perceived reduction in racial trauma symptoms would mediate the association between psychedelic use and perceived reductions in alcohol and drug use.
2. Methods
2.1. Participants
A sample of 313 participants completed a Qualtrics survey on their psychedelic and other substance use and mental health symptoms [for more details on the sample and study procedures, see (Williams et al., 2021)]. This was a cross-sectional, observational study of participants recruited through Qualtrics survey research panels. Inclusion criteria were: 1) at least 18 years old, 2) fluent in reading and writing English, 3) reported taking a dose of a classic psychedelic (e.g. psilocybin mushrooms, LSD, ayahuasca, mescaline, DMT, 5-MeO-DMT, etc.) that produced moderate to strong effects, 4) reported experiencing relief from the negative effects of racial or ethnic discrimination, 5) resided in the United States or Canada at the time of survey completion, and 6) self-identified as a REM people person. Thirty-nine and 83 participants reported they never drank alcohol or used drugs, respectively, prior to the psychedelic experience so we removed them from the analyses leaving an overall sample of 211 participants (Table 1). Notably, to assess timing of events in this cross-sectional study, the study asked participants to retrospectively report their substance use, racial trauma symptoms, and psychological flexibility before and after their psychedelic experience. Thus, any change in these constructs are perceived changes based on retrospective report as opposed to observed measurable changes over time. The Ohio State University Institutional Review Board approved all study procedures and participants provided informed consent prior to completing the survey.
Table 1.
Demographic characteristics (N = 211)
| Race | |
| Black or African heritage | 33% |
| East Asian, South Asian, Asian American/Canadian | 29% |
| Native American or, Indigenous Canadian | 18% |
| Native Hawaiian, Pacific Islander, other | 19% |
| Sex | |
| Female | 51% |
| Male | 48% |
| Intersex | 1% |
| Gender | |
| Woman | 49% |
| Man | 46% |
| Other | 5% |
| Country | |
| United States | 46% |
| Canada | 54% |
| Latine Ethnicity | |
| Non-Latine | 87% |
| Latine | 18% |
| Age (mean, SD) | 33.28 (10.16) |
Note. Latine is being used as a gender-neutral term to describe Latin people.
2.2. Measures
Participants self-reported their demographic characteristics, including their age, sex (male, female, intersex), gender (woman, man, gender-fluid, transgender male to female, transgender female to male, other), race (White; Black; East Asian, South Asian, Asian American/Canadian; Native American, American Indian, Indigenous Canadian, or Alaskan Native; Native Hawaiian or Pacific Islander; other), ethnicity (Hispanic, non-Hispanic), and country of residence (United States, Canada).
Given prior evidence that ethnic identity (e.g., “I have a strong sense of belonging to my own ethnic group”) can be protective against the harmful effects of racial discrimination on substance use (Caldwell et al., 2004; Clifton et al., 2021; Stock et al., 2011; Zapolski et al., 2019; Zapolski et al., 2017), we assessed ethnic identity using the Multigroup Ethnic Identity Measure (MEIM-R) (Yoon, 2011). Participants answered 6 items on a scale from 1 (strongly disagree) to 5 (strongly agree). Responses ranged from 6 to 30 (mean score = 23.68, SD = 4.78), with higher scores indicating a stronger ethnic identity. Internal consistency reliability as indicated by Cronbach’s alpha was within range (α = .86).
Given a prior study using these data found that psychedelic experiences were associated with perceived reductions in anxiety, depression, and stress (Williams et al., 2021), we included these as covariates in the models as well. Depression, anxiety, and stress were assessed using the Depression, Anxiety, and Stress Scale (DASS21) (Lovibond & Lovibond, 1995), which is a 21-item measure, 7 items for each subscale of anxiety, depression, and stress. Participants were asked to retrospectively report on their anxiety, depression, and stress symptoms 30 days before and 30 days after the psychedelic experience and the change scores for each were used as the covariates in the analyses. Internal consistency reliability as indicated by Cronbach’s alphas were within range (depression before α = .89; anxiety before α = .82; stress before α = .86; depression after α = .86; anxiety after α = .83; stress after α = .87). Anxiety, depression, stress, ethnic identity, and demographic characteristics were included as covariates in the models.
2.2.1. Substance use
Alcohol and drug use were assessed and included as two separate dependent variables in the analyses. Alcohol use was assessed using the Alcohol Use Disorders Identification Test [AUDIT-C; (Dawson et al., 2005)]. The AUDIT-C is a questionnaire developed to cover the domains of alcohol consumption, drinking behavior, and alcohol-related problems. Participants answered 3-items assessing the quantity and frequency of their drinking on a 4-point scale ranging from 0 (Never; No) to 4 (4 or more times a week; Daily or almost daily; Yes, during the last year). Participants reported on their alcohol use 30 days before and 30 days after their psychedelic experience. Internal consistency was α = .81 before and after α = .81 the psychedelic experience.
The study assessed drug use using the Drug Use Disorders Identification Test [DUDIT-C; (Berman et al., 2005)]. The DUDIT-C is a self-report questionnaire developed to parallel the utility of the AUDIT-C, aiming to identify individuals with drug-related problems unrelated to alcohol use. Study staff instructed participants to report on any substance use excluding alcohol and over the counter or prescription medication unless the medication was intended to be used for recreational or nonmedical purposes. Participants answered 3 items assessing the quantity and frequency of drug use on a 4-point scale ranging from 0 (Never; No) to 4 (4 times a week or more often; Daily or almost every day; Yes, over the past year). Participants reported on their drug use 30 days before and 30 days after their psychedelic experience. Internal consistency was α = .84 before and after α = .85 the psychedelic experience.
2.2.2. Psychedelic experience
Participants reported on the psychedelic experience that was the most memorable. An 8-item multiple choice questionnaire developed for this study assessed the type of psychedelic used (Psilocybin, LSD [acid], Iboga/Ibogaine, Ayahuasca, N,N-DMT [other than Ayahuasca], 5-MeO-DMT, Mescaline, Peyote cactus, Ketamine, Cannabis, other), age of the psychedelic experience, how long ago the psychedelic experience occurred, subjective dose (endorsements of “low” and “moderate” were categorized as low and “high” and “very high” were categorized as high), route of administration, and duration of the psychedelic experience. The independent variables were psychedelic experiences, which we operationalized based on three forms of acute experiences described below. (See Table 2 in Williams et al., 2021 for more details on participants’ psychedelic use).
Psychological insight (Davis et al., 2021):
This 23-item questionnaire was developed to assess for insights had during a psychedelic experience regarding relationships, memories, emotions, and beliefs. Participants reported such insights from their psychedelic experience (e.g., “Realized ways my beliefs may be dysfunctional”) on a 6-point scale ranging from 0 (No; Not at all) to 5 (Extremely; More than ever before in my life). Internal consistency reliability as indicated by Cronbach’s alpha was within range (α = .83).
Mystical experience (Barrett et al., 2015; MacLean et al., 2012):
This 30-item questionnaire assesses for mystical-type experiences that individuals may be able to report following psychedelic experiences. Participants reported mystical-type experiences (“Loss of your usual sense of time,” “Experience of amazement”) on a 6-point scale ranging from 0 (None; Not at all) to 5 (Extremely; More than ever before in my life). Internal consistency reliability as indicated by Cronbach’s alpha was within range (α = .84).
Challenging experience (Barrett et al., 2016):
This 26-item questionnaire was developed to assess for challenging experiences that were had during a psychedelic experience, such as grief, fear, death, isolation, or paranoia. Participants reported such challenges (e.g. “I felt shaky inside”, “I felt like crying”) on a 6-point scale ranging from 0 (No; Not at all) to 5 (Extremely; More than ever before in my life). Internal consistency reliability as indicated by Cronbach’s alpha was within range (α = .92).
2.2.3. Hypothesized mediators
The study assessed racial trauma using the Trauma Symptoms of Discrimination scale [TSDS; (Williams, Printz, et al., 2018)]. This 21-item self-report measure assesses discriminatory distress related to symptoms of trauma, such as uncontrollable hyperarousal, feeling alienated, worries about future negative events, and perceiving others as dangerous. Participants reported these feelings 30 days prior to and 30 days after their psychedelic experience with consideration to past experiences of discrimination (e.g. “Due to past experiences of discrimination, I feel isolated and set apart from others”) on a 4-point scale ranging from 1 (never) to 4 (often). Internal consistency reliability as indicated by Cronbach’s alpha were within range before α = .72 and after the psychedelic experience α = .74.
The study assessed psychological flexibility using the Acceptance and Action Questionnaire-II (AAQ-II), which is a 7-item measure. The AAQ-II evaluates avoidance, emotional states, and perceptions of oneself on a 7-point scale (1=“Never true” to 7=“Always true”). Participants reported on these experiences 30 days prior to and 30 days after their psychedelic experience. We reverse scored the mean so that a decrease in score would be interpreted as an increase in psychological flexibility to aid in the interpretability of the findings. Internal consistency reliability as indicated by Cronbach’s alpha were within range before α = .89 and after the psychedelic experience α = .89.
2.3. Data analysis
We first conducted preliminary analyses to investigate the associations between variables. Specifically, bivariate correlations examined the associations between variables. Paired t-tests and Cohen’s d identified whether statistically significant (p<.05) changes in alcohol and drug use occurred from before to after the psychedelic experience based on retrospective report. We estimated change scores for alcohol and drug use, trauma symptoms, and psychological flexibility based on retrospective reports of each before and after the psychedelic experience. Analysis of covariance (ANCOVA) examined psychedelic experience (i.e., mystical, insight, and challenging experiences) and change in psychological flexibility and racial trauma symptoms as predictors of change in drug and alcohol use (two separate models), respectively while adjusting for psychedelic type and dose of the psychedelic, race, ethnicity, ethnic identity, age, and gender identity. We conducted all preliminary analyses in SAS.
To examine serial mediation, the study conducted tests of indirect effects via multiple regression analyses in Mplus to investigate whether perceived changes in psychological flexibility and racial trauma mediated the association between acute psychedelic experiences and potential perceived change in substance use (Figure 1).
Figure 1.
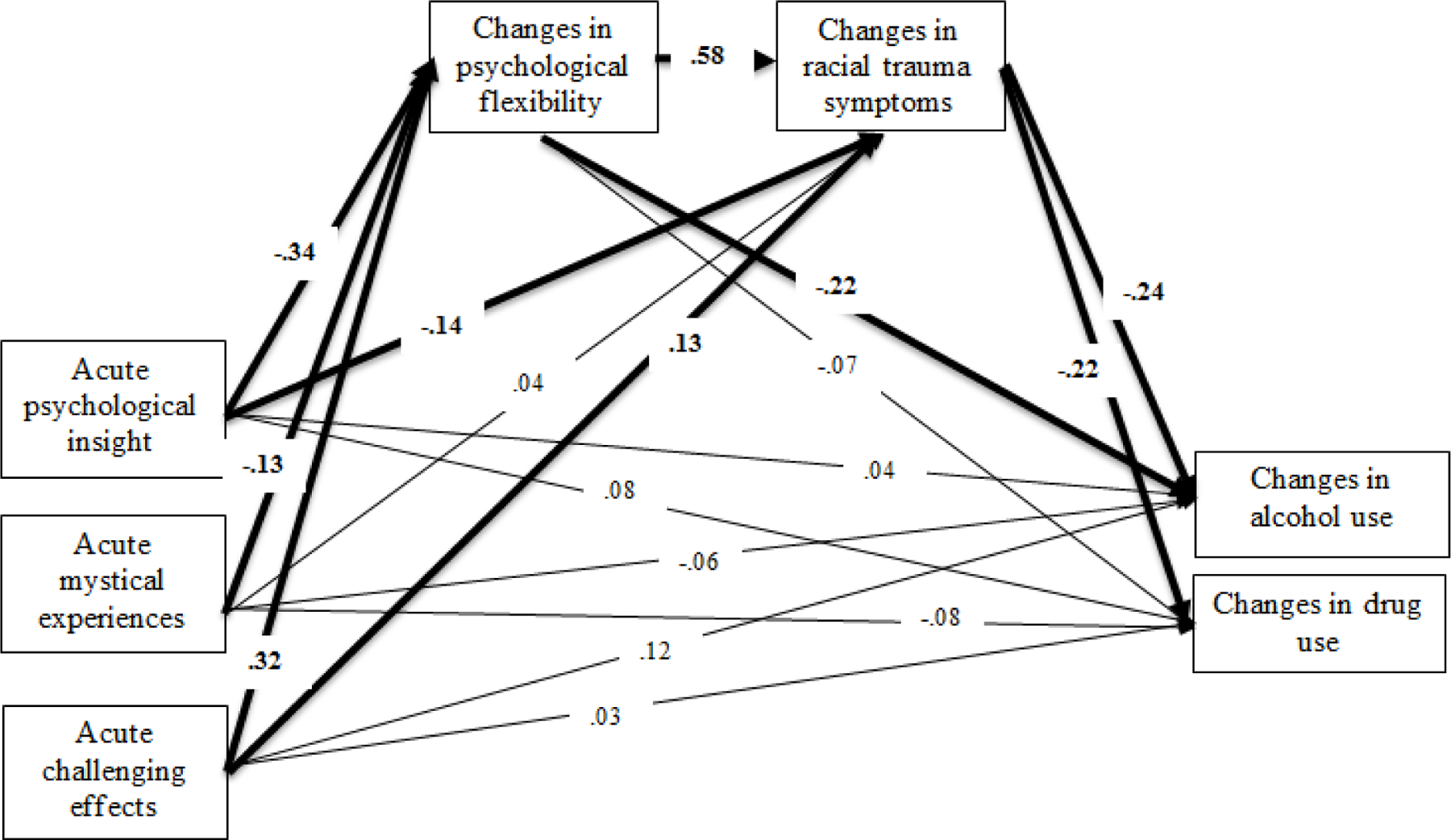
Serial mediation model testing whether perceived changes in psychological flexibility and racial trauma symptoms mediate the association between acute psychedelic experiences and perceived changes in substance use. Bold indicates significant paths (p < .05).
3. Results
3.1. Preliminary analyses
Supplemental Table 1 indicates that psychedelic effects, perceived changes in psychological flexibility and racial trauma symptoms, and alcohol use were significantly correlated with the exception that acute challenging psychedelic experiences were not associated with alcohol use. Drug use was correlated with all variables except for psychedelic effects. Paired t-tests indicated a perceived reduction in alcohol use (p<.0001, d=.54) and drug use (p=.0001, d=.23) from before to after the psychedelic experience (Table 2).
Table 2.
Change in alcohol and drug use from before to after the psychedelic experience (N = 211)
| Substance Use Measure | Before psychedelic experience Mean (SD) | After psychedelic experience Mean (SD) | t-test | Cohen’s d |
|---|---|---|---|---|
| AUDIT-C | 3.28 (.90) | 2.79 (.93) | 7.27 | .54 |
| DUDIT-C | 2.63 (.91) | 2.42 (.98) | 3.86 | .23 |
Note. AUDIT-C = Alcohol Use Disorder Identification Test, 3-item version. DUDIT-C = Drug Use Disorder Identification Test, 3-item version. Bold indicates significant at p < .05.
The overall ANCOVA model examining perceived change in alcohol use was significant (F18,167=6.96, p<.0001). We found a main effect indicating that perceived reductions in racial trauma symptoms were associated with perceived reductions in alcohol use (β=.02, SE=.01, p=.03). Acute psychedelic experiences and psychological flexibility were not associated with alcohol use. Regarding covariates, we found a main effect of race such that Indigenous participants (least squares means [LSM]=−1.23) experienced a greater perceived reduction in alcohol use relative to participants who identified as Asian (LSM=−.36), Black (LSM=−.28), or other (LSM=−.20). In addition, those who took a high dose (LSM=−.65) of the psychedelic reported perceived reductions in alcohol use than those who took a low dose (LSM=−.38). Further, those with a stronger ethnic identity (β=.24, SE=.10, p=.01) and who experienced a greater perceived reduction in depression symptoms (β=.06, SE=.02, p=.001) also experienced a greater perceived reduction in alcohol use.
The overall ANCOVA model examining change in drug use was significant (F18,167=3.12, p<.0001). Acute psychedelic effects, psychological flexibility, and racial trauma were not associated with perceived change in drug use. Regarding covariates, a greater perceived reduction in anxiety symptoms was associated with greater perceived reductions in drug use (β=.04, SE=.02, p=.04). We found a main effect of race such that a greater perceived reduction in drug use was found among participants who identified as Indigenous (LSM=−.32), other (LSM=−.32), and Asian (LSM=−.19) relative to participants who identified as Black (LSM=.06).
3.2. Serial mediation
Perceived changes in psychological flexibility and racial trauma symptoms significantly mediated the association between acute psychedelic effects and perceived changes in substance use (Figure 1). Specifically, greater psychological insight, more mystical experiences, and fewer challenging effects were associated with perceived increased psychological flexibility. Perceived increase in psychological flexibility was associated with perceived reductions in racial trauma symptoms when acute psychedelic effects are accounted for in the model. A perceived reduction in racial trauma symptoms was associated with perceived reductions in alcohol and drug use when acute psychedelic effects and perceived increase in psychological flexibility were accounted for in the model. Similarly, greater psychological insight and fewer challenging effects were associated with perceived reductions in racial trauma symptoms. Perceived increase in psychological flexibility was associated with a perceived reduction in alcohol use but the association with change in drug use was not significant. The direct effect between acute psychedelic effects and perceived changes in substance use was not significant with perceived changes in psychological flexibility and racial trauma symptoms in the model.
4. Discussion
More effective treatments are needed for substance use disorders given the major public health impact of these disorders in both the UnitedStates and Canada. Evidence suggests that psychedelics may effectively reduce substance use; however, REM people are often underrepresented in psychedelic studies and constructs especially relevant to REM people like racial trauma are not assessed. The current study aimed to address these gaps in the literature by preliminarily examining how psychedelic use impacts alcohol and other drug use and changes in psychological flexibility and racial trauma symptoms among REM people. Consistent with our hypothesis, our findings suggest that acute psychedelic effects lead to perceived increased psychological flexibility, which contributes to perceived decreased racial trauma symptoms and subsequent perceived reductions in alcohol and drug use. These findings highlight the importance of investigating the potential therapeutic effect of psychedelics in increasing psychological flexibility and reducing racial trauma symptoms and alcohol and drug use among REM people. Future longitudinal studies examining the impact of psychedelics on substance use outcomes among REM people should also assess psychological flexibility and racial trauma symptoms given that the findings from the current study suggest both are important factors in understanding how psychedelics may work to reduce substance use.
The role of psychedelics in treating mental health, including trauma, alcohol, and other drug use disorders, has been situated in communities of color the world over (George et al., 2020; Labate & Cavnar, 2018). However, these practices have often been derided within the medical community as unscientific due to a general lack of knowledge surrounding practices and history (Barnett et al., 2021). Arguably, the legality and racialization of psychedelic use (e.g., Native Americans are allowed to use peyote) has further marginalized those who would or do use psychedelics, as REM people are othered and further viewed in the context of a perceived propensity for addiction and illicit use (Jahn et al., 2021). To ensure generalizability of psychedelic research findings, and honor the millennia-old traditions and intentions of Indigenous practitioners, psychedelic researchers must acknowledge the roots of psychedelic use as a healing practice and ensure representation of REM people in their studies (Muscat et al., 2021; Smith et al., 2022).
The findings from this study also support moving beyond the conventional narratives of what constitutes trauma to include socioeconomic, environmental, community-level indictors of adversity, namely, racial trauma (Cronholm et al., 2015). Our preliminary findings suggest a reduction in racial trauma symptoms is associated with reduced alcohol and drug use after psychedelic use, highlighting the need to attend to racial trauma specifically among REM people in both our research and clinical work. Specifically, these findings indicate that attending to racial trauma may play a critical role in treating substance use disorder among REM people and that psychological flexibility may contribute to reducing racial trauma symptoms. Substance use treatment programs should strongly consider assessing racial trauma and psychological flexibility as part of their intake procedures and incorporating both in case conceptualizations and as treatment targets when appropriate. Additional research using more rigorous methodology such as clinical trials should seek to fully understand the impact of psychedelics on racial trauma among REM people, the mechanisms that underlie these associations such as increased psychological flexibility, and how these associations contribute to changes in drug and alcohol use.
The greatest reductions in alcohol use were among Indigenous participants. This is an important finding, particularly given the high prevalence of alcohol use disorder in Indigenous communities (Argento et al., 2017; Brave Heart et al., 2016; Haeny et al., 2021). Historical and contemporary race-based traumas embedded in the persistent and perpetual colonization and discrimination of Indigenous peoples of the Americas and Canada have long been viewed as the cause for alcohol and other drug problems. In terms of trauma, posttraumatic stress, and racial trauma, US and Canadian Indigenous peoples are disproportionally affected. Healing practices for traumas and myriad suffering pre- and post-colonization have been rooted in ceremonial and sacred practices that include psychedelic drug use. The finding from the current study in combination with the findings from prior studies further support the potential benefit of psychedelic use in reducing other substance use particularly among Indigenous peoples.
All participants reported a reduction in drug use except Black participants. Given the limited research on the impact of psychedelic use on other drug use among Black adults, why psychedelic experiences were associated with decreased alcohol use and no change or possibly a slight increase in drug use among Black people is unclear. This uncertainty is predicated by findings that Black people least often report psychedelic use in general, possibly resulting from hyper-criminalization for drug use or subcultural stigma (Jahn et al., 2021). These findings suggest that psychedelic use may not have the same therapeutic effect on reducing drug use among Black people relative to other REM people. Additional research should try to understand what contributes to this pattern of findings among Black people. In addition, these findings further highlight the importance of examining specific racial/ethnic groups as opposed to combining all REM people together in analyses. Although recreational (non-clinical) psychedelic use, as reported in this study, is not sufficient to reduce drug use in this population, a clinical intervention that included psychedelic drug administration may be warranted to produce clinically meaningful outcomes.
We also found that those with a stronger ethnic identity (i.e., feel a stronger connection with their racial/ethnic group) experienced a greater reduction in their alcohol use. This finding is consistent with research suggesting that a strong racial/ethnic identity can be protective against negative harms of racism on poor mental health outcomes and substance use (Clifton et al., 2021; Jackson et al., 2004; Jones & Neblett, 2017; Stock et al., 2011; Zapolski et al., 2019; Zapolski et al., 2017). Although the ultimate goal is to eliminate racism, the findings from this study support that strengthening ethnic identity can be a focus of clinical work as one means of minimizing the harms of racism on mental health and alcohol use.
4.1. Limitations
An important limitation of this study is the cross-sectional nature of the data. Although we phrased the questions to get at the timing of racial trauma and substance use before and after the psychedelic experience, they were based on retrospective report and we are unable to differentiate the directionality or specific timing of the change in psychological flexibility, racial trauma experiences, and substance use, which are important factors when testing mediation. Therefore, the findings from the mediation models should be considered preliminary given the cross-sectional nature of the data. Future research should replicate these mediation models using longitudinal data and considering a latent change score framework (Castro-Schilo & Grimm, 2018). In addition, although we were intentional about investigating changes in alcohol and drug use, we were limited in our ability to determine whether the pattern of findings would differ for specific drugs or tobacco products. We also simply assessed for alcohol and drug use and not substance use consequences or severity, which should be the focus of future research. Further, the data collected were self-reported survey responses, which are subject to response bias. Last, given the small sample sizes of those who identified as Native Hawaiian, Pacific Islander, and other, we combined these groups into an “other” category so they could be included in the analyses. Therefore, the “other” category is heterogenous and limits our ability to determine whether differences existed among those who identify as Native Hawaiian, Pacific Islander, and other.
4.2. Conclusion
This study is the first to investigate potential mediators of the association between psychedelic use and other substance use outcomes among REM people and to provide preliminary evidence that a perceived increase in psychological flexibility and reduction in racial trauma symptoms are associated with a perceived reduction in alcohol and drug use after psychedelic experiences.
Supplementary Material
Highlights.
Psychedelic treatment may reduce mental health and substance use problems
Racial and ethnic minoritized (REM) people are underrepresented in psychedelic research
We investigated the impact of psychedelics on substance use outcomes among REM people
Psychedelic use was associated with reductions in alcohol and other drug use
Racial trauma symptoms and psychological flexibility were significant mediators
5. Acknowledgements
This work was supported by the National Institutes of Health: L30 DA049246, K23 AA028515, R25 DA035163, F32 AA029627. AKD is supported by funding from Tim Ferriss, Matt Mullenweg, Craig Nerenberg, Blake Mycoskie, the Steven and Alexandra Cohen Foundation, and by the Center for Psychedelic Drug Research and Education in the College of Social Work at Ohio State University, funded by anonymous private donors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest: MW and AKD are on the board of directors at Source Research Foundation. AKD is a lead trainer at Fluence. Neither organization was financially involved in this study.
6.1 References
- Andersen KAA, Carhart-Harris R, Nutt DJ, & Erritzoe D (2021). Therapeutic effects of classic serotonergic psychedelics: A systematic review of modern-era clinical studies. Acta Psychiatrica Scandinavica, 143(2), 101–118. 10.1111/ACPS.13249 [DOI] [PubMed] [Google Scholar]
- Argento E, Strathdee SA, Tupper K, Braschel M, Wood E, & Shannon K (2017). Does psychedelic drug use reduce risk of suicidality? Evidence from a longitudinal community-based cohort of marginalised women in a Canadian setting. BMJ Open, 7(9), 1–8. 10.1136/bmjopen-2017-016025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett BS, Beaussant Y, King F, & Doblin R (2021). Psychedelic Knowledge and Opinions in Psychiatrists at Two Professional Conferences: An Exploratory Survey. Journal of Psychoactive Drugs, 00(00), 1–9. 10.1080/02791072.2021.1957183 [DOI] [PubMed] [Google Scholar]
- Barrett FS, Bradstreet MP, Leoutsakos JMS, Johnson MW, & Griffiths RR (2016). The Challenging Experience Questionnaire: Characterization of challenging experiences with psilocybin mushrooms. Journal of Psychopharmacology, 30(12), 1279–1295. 10.1016/j.paid.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett FS, Johnson MW, & Griffiths RR (2015). Validation of the revised Mystical Experience Questionnaire in experimental sessions with psilocybin. Journal of Psychopharmacology, 29(11), 1182–1190. 10.1177/0269881115609019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman AH, Bergman H, Palmstierna T, & Schlyter F (2005). Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. European Addiction Research, 11(1), 22–31. 10.1159/000081413 [DOI] [PubMed] [Google Scholar]
- Boynton MH, O’Hara RE, Covault J, Scott D, & Tennen H (2015). A Mediational Model of Racial Discrimination and Alcohol-Related Problems Among African American College Students. 10.15288/Jsad.2014.75.228, 75(2), 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brave Heart MYH, Lewis-Fernández R, Beals J, Hasin DS, Sugaya L, Wang S, Grant BF, & Blanco C (2016). Psychiatric disorders and mental health treatment in American Indians and Alaska Natives: results of the National Epidemiologic Survey on Alcohol and Related Conditions. Social Psychiatry and Psychiatric Epidemiology 2016 51:7, 51(7), 1033–1046. 10.1007/S00127-016-1225-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant-Davis T, & Ocampo C (2005). Racist Incident–Based Trauma: The Counseling Psychologist, 33(4), 479–500. 10.1177/0011000005276465 [DOI] [Google Scholar]
- Caldwell CH, Sellers RM, Bernat DH, & Zimmerman MA (2004). Racial Identity, Parental Support, and Alcohol Use in a Sample of Academically At-Risk African American High School Students. American Journal of Community Psychology, 34(2). [DOI] [PubMed] [Google Scholar]
- Carter RT, Johnson VE, Kirkinis K, Roberson K, Muchow C, Galgay C, & Kirkinis Katherine K (2019). A Meta-Analytic Review of Racial Discrimination: Relationships to Health and Culture. Race and Social Problems, 11(1), 15–32. 10.1007/s12552-018-9256-y [DOI] [Google Scholar]
- Castro-Schilo L, & Grimm KJ (2018). Using residualized change versus difference scores for longitudinal research. Journal of Social and Personal Relationships, 35(1), 32–58. 10.1177/0265407517718387 [DOI] [Google Scholar]
- Chen JA, Zhang E, & Liu CH (2020). Potential Impact of COVID-19–Related Racial Discrimination on the Health of Asian Americans. American Journal of Public Health, 110(11), 1624–1627. 10.2105/AJPH.2020.305858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark TT, Salas-Wright CP, Vaughn MG, & Whitfield KE (2015). Everyday discrimination and mood and substance use disorders: A latent profile analysis with African Americans and Caribbean Blacks. Addictive Behaviors. 10.1016/j.addbeh.2014.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifton RL, Rowe AT, Banks DE, Ashburn-Nardo L, & Zapolski TCB (2021). Examining the effects of implicit and explicit racial identity on psychological distress and substance use among Black young adults. Experimental and Clinical Psychopharmacology, 29(5), 479–486. https://psycnet.apa.org/record/2021-64108-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Close JB, Hajien EC, Watts R, Roseman L, & Carhart-Harris RL (2020). Psychedelics and psychological flexibility—results of a prospective web-survey using the Acceptance and Action Questionnaire II. Journal of Contextual Behavioral Science, 16, 37–44. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C7&q=Psychedelics+and+psychological+flexibility—results+of+a+prospective+web-survey+using+the+acceptance+and+Action+Questionnaire+II.&btnG= [Google Scholar]
- Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, Pachter LM, & Fein JA (2015). Adverse Childhood Experiences: Expanding the Concept of Adversity. American Journal of Preventive Medicine, 49(3), 354–361. 10.1016/J.AMEPRE.2015.02.001 [DOI] [PubMed] [Google Scholar]
- Currie C, Cameron Wild T, Schopflocher D, & Laing L (2015). Racial discrimination, posttraumatic stress and prescription drug problems among Aboriginal Canadians. Canadian Journal of Public Health, 106(6), 382–387. 10.17269/CJPH.106.4979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis AK, Xin Y, Sepeda ND, Garcia-Romeu A, & Williams MT (2021). Increases in Psychological Flexibility Mediate Relationship Between Acute Psychedelic Effects and Decreases in Racial Trauma Symptoms Among People of Color. Journals.Sagepub.Com, 5. 10.1177/24705470211035607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, & Ruan WJ (2005). Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction, 100(3), 281–292. 10.1111/j.1360-0443.2004.00964.x [DOI] [PubMed] [Google Scholar]
- Desalu JM, Goodhines PA, & Park A (2019). Racial discrimination and alcohol use and negative drinking consequences among Black Americans: a meta-analytical review. 10.1111/add.14578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FBI. (2019). 2019 Hate Crime Statistics. Department of Justice. https://ucr.fbi.gov/hate-crime/2019/topic-pages/victims
- Feeney K (2017). A Review of A Culture’s Catalyst: Historical Encounters with Peyote and the Native American Church in Canada. IK: Other Ways of Knowing, 76–78. 10.18113/P8IK360543 [DOI] [Google Scholar]
- George JR, Michaels TI, Sevelius J, & Williams MT (2020). The psychedelic renaissance and the limitations of a White-dominant medical framework: A call for indigenous and ethnic minority inclusion. Journal of Psychedelic Studies, 4(1), 4–15. 10.1556/2054.2019.015 [DOI] [Google Scholar]
- Gibbons FX, Etcheverry PE, Stock ML, Gerrard M, Weng C-Y, Kiviniemi M, & O’Hara RE (2010). Exploring the link between racial discrimination and substance use: What mediates? What buffers? Journal of Personality and Social Psychology, 99(5), 785–801. 10.1037/a0019880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, & Brody G (2004). Perceived Discrimination and Substance Use in African American Parents and Their Children: A Panel Study. Journal of Personality and Social Psychology, 86(4), 517–529. 10.1037/0022-3514.86.4.517 [DOI] [PubMed] [Google Scholar]
- Gloster AT, Meyer AH, & Lieb R (2017). Psychological flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science, 6(2), 166–171. 10.1016/J.JCBS.2017.02.003 [DOI] [Google Scholar]
- Godley J (2018). Everyday Discrimination in Canada. 43(2), 111–142. [Google Scholar]
- Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, & Burrage RL (2019). The Impact of Historical Trauma on Health Outcomes for Indigenous Populations in the USA and Canada : A Systematic Review. 74(1), 20–35. [DOI] [PubMed] [Google Scholar]
- Gray A (1994). Effects of the American Indian Religious Freedom Act Amendments on Criminal Law: Will Peyotism Eat Away at the Controlled Substances Act. American Journal of Criminal Law, 22. https://heinonline.org/HOL/Page?handle=hein.journals/ajcl22&id=777&div=32&collection=journals [Google Scholar]
- Haeny AM, Oluwoye O, Cruz R, Iheanacho T, Jackson AB, Fisher S, Crouch M, & O’Malley S (2021). Drug and alcohol treatment utilization and barriers among Black, American Indian/Alaskan Native, Latine, Asian/Pacific Islander/Native Hawaiian, and White adults: Findings from NESARC-III. Journal of Substance Abuse Treatment, 131, 108569. 10.1016/J.JSAT.2021.108569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes SC, Facemire VC, & Dafonseca AM (2016). Expanding Criterion A for Posttraumatic Stress Disorder: Considering the Deleterious Impact of Oppression. 10.1037/trm0000104 [DOI] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, Trierweiler SJ, & Williams DR (2004). The National Survey of American Life: a study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research, 13(4), 196–207. 10.1002/MPR.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahn ZW, Lopez J, de la Salle S, Faber S, & Williams MT (2021). Racial/ethnic differences in prevalence of hallucinogen use by age cohort: Findings from the 2018 National Survey on Drug Use and Health. Journal of Psychedelic Studies, 5(2), 69–82. 10.1556/2054.2021.00166 [DOI] [Google Scholar]
- Jones SCT, & Neblett EW (2017). Future Directions in Research on Racism-Related Stress and Racial-Ethnic Protective Factors for Black Youth. Journal of Clinical Child & Adolescent Psychology, 46(5), 754–766. 10.1080/15374416.2016.1146991 [DOI] [PubMed] [Google Scholar]
- Kashdan TB, & Rottenberg J (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878. 10.1016/J.CPR.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkinis K, Pieterse AL, Agiliga A, & Brownell A (2018). Racism, racial discrimination, and trauma: a systematic review of the social science literature. 10.1080/13557858.2018.1514453 [DOI] [PubMed] [Google Scholar]
- Labate BC, & Cavnar C (2018). Plant medicines, healing and psychedelic science : cultural perspectives. Springer. https://books.google.com/books/about/Plant_Medicines_Healing_and_Psychedelic.html?id=2PhYDwAAQBAJ [Google Scholar]
- Lin L. (Allison), Bohnert ASB, Price AM, Jannausch M, Bonar EE, & Ilgen MA (2015). Pain acceptance and opiate use disorders in addiction treatment patients with comorbid pain. Drug and Alcohol Dependence, 157, 136–142. 10.1016/j.drugalcdep.2015.10.017 [DOI] [PubMed] [Google Scholar]
- Lovibond SH, & Lovibond PF (1995). Manual for the depression anxiety & stress scales (2nd Ed.). Psychology Foundation. [Google Scholar]
- MacLean KA, Leoutsakos JMS, Johnson MW, & Griffiths RR (2012). Factor Analysis of the Mystical Experience Questionnaire: A Study of Experiences Occasioned by the Hallucinogen Psilocybin. Journal for the Scientific Study of Religion, 51(4), 721–737. 10.1111/j.1468-5906.2012.01685.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand WR, Klinger W, Block K, VerMerris S, Herrmann TS, Johnson C, Shubin E, & Sheppard S (2018). Safety and psychological impact of sailing adventure therapy among Veterans with substance use disorders. Complementary Therapies in Medicine, 40, 42–47. 10.1016/j.ctim.2018.07.013 [DOI] [PubMed] [Google Scholar]
- Michaels TI, Purdon J, Collins A, & Williams MT (2018). Inclusion of people of color in psychedelic-assisted psychotherapy: A review of the literature. BMC Psychiatry, 18(1), 1–14. 10.1186/s12888-018-1824-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LD, & Elkavich A (2008). Who’s using and who’s doing time: Incarceration, the war on drugs, and public health. American Journal of Public Health, 98, S176–S180. 10.2105/ajph.98.supplement_1.s176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat SA, Wright GD, Bergeron K, Morin KW, Crouch CR, & Hartelius G (2021). Ketamine-Assisted and Culturally Attuned Trauma Informed Psychotherapy as Adjunct to Traditional Indigenous Healing: Effecting Cultural Collaboration in Canadian Mental Health Care. Behavioral Sciences 2021, Vol. 11, Page 118, 11(9), 118. 10.3390/BS11090118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, & Gee G (2015). Racism as a determinant of health: A systematic review and meta-analysis. PLoS ONE, 10(9), e0138511. 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, & Richman LS (2009). Perceived Discrimination and Health : A Meta-Analytic Review. 135(4), 531–554. 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, Giovino GA, West R, Hall W, Griffiths P, Ali R, Gowing L, Marsden J, Ferrari AJ, Grebely J, Farrell M, & Degenhardt L (2018). Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction, 113(10), 1905–1926. 10.1111/ADD.14234 [DOI] [PubMed] [Google Scholar]
- Pieterse AL, Todd NR, Neville HA, & Carter RT (2012). Perceived Racism and Mental Health Among Black American Adults: A Meta-Analytic Review. Journal of Counsel, 59(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Rosen KD, Curtis ME, & Potter JS (2020). Pain, psychological flexibility, and continued substance use in a predominantly hispanic adult sample receiving methadone treatment for opioid use disorder. Drug and Alcohol Dependence, 206, 107681. 10.1016/j.drugalcdep.2019.107681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DT, Faber SC, Buchanan NT, Foster D, & Green L (2022). The Need for Psychedelic-Assisted Therapy in the Black Community and the Burdens of Its Provision. Frontiers in Psychiatry, 12, 2532. 10.3389/FPSYT.2021.774736/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock ML, Gibbons FX, Walsh LA, & Gerrard M (2011). Racial Identification, Racial Discrimination, and Substance Use Vulnerability Among African American Young Adults. Personality and Social Psychology Bulletin, 37(10), 1349–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MT, Davis AK, Xin Y, Sepeda ND, Grigas PC, Sinnott S, Haeny AM, & Col On Grigas P (2021). People of color in North America report improvements in racial trauma and mental health symptoms following psychedelic experiences. Drugs: Education, Prevention and Policy ISSN:, 28(3), 215–226. 10.1080/09687637.2020.1854688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MT, Metzger IW, Leins C, & DeLapp C (2018). Assessing racial trauma within a DSM–5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Practice Innovations, 3(4), 242–260. 10.1037/pri0000076 [DOI] [Google Scholar]
- Williams MT, Printz DMB, & DeLapp RCT (2018). Assessing Racial Trauma With the Trauma Symptoms of Discrimination Scale. Psychology of Violence, 8, 735–747. 10.1037/vio0000212 [DOI] [Google Scholar]
- World Health Organization. (2019). Global status report on alcohol and health 2018. https://books.google.com/books?hl=en&lr=&id=qnOyDwAAQBAJ&oi=fnd&pg=PR7&dq =%22Global+status+report+on+alcohol+and+health+2014%22&ots=a1roMEqjfl&sig=y9PlvpDyWuxdEKgWXDPgrSdM2W0#v=onepage&q=%22Global status report on alcohol and health 2014%22&f=false [Google Scholar]
- Yoon E (2011). Measuring ethnic identity in the Ethnic Identity Scale and the Multigroup Ethnic Identity Measure-Revised. Cultural Diversity and Ethnic Minority Psychology, 17(2), 144–155. 10.1037/a0023361 [DOI] [PubMed] [Google Scholar]
- Zapolski TCB, Beutlich MR, Fisher S, & Barnes-Najor J (2019). Collective ethnic–racial identity and health outcomes among African American youth: Examination of promotive and protective effects. Cultural Diversity and Ethnic Minority Psychology, 25(3), 388. https://psycnet.apa.org/journals/cdp/25/3/388/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski TCB, Fisher S, Banks DE, Hensel DJ, & Barnes-Najor J (2017). Examining the Protective Effect of Ethnic Identity on Drug Attitudes and Use Among a Diverse Youth Population. Journal of Youth and Adolescence, 46(8), 1702–1715. 10.1007/s10964-016-0605-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


