Little strong evidence exists to explain the sustained growth in demand for hospital services shown in the table, but changes in population structure, numbers of people living alone, pressures on primary care, risk management, patient expectations, and an increased ability to treat are frequently cited as possible reasons for this seemingly inexorable rise.1
The desire to reduce, or at least contain, demand in the hospital sector is undoubtedly related to this growth and to the need to control costs. There is also a concern about the appropriateness of hospital care for many conditions, and there are growing opportunities to provide modes of care which may better meet patients’ needs and may, in some circumstances, be cheaper.
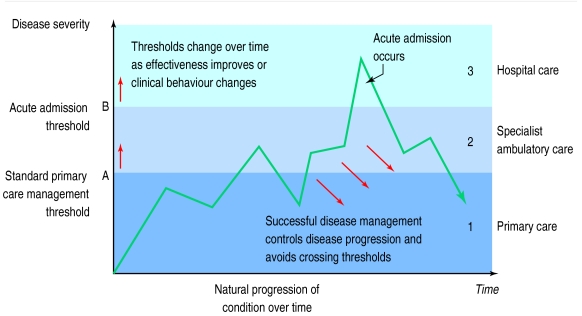
The previous paper in this series discussed demand management at the interface between primary care and secondary care. Attempts to segment primary and secondary care are inevitably somewhat artificial. Figure 1, however, shows a highly simplified representation of the relation over time between the natural progression of a chronic illness and the thresholds between different healthcare sectors.
Summary points
There has been a sustained growth in demand for hospital services, which has been accommodated despite a decline in bed numbers
Further ways of managing demand for secondary care include condition-specific waiting lists, medical assessment units, use of protocols, and a single point of access to non-hospital alternatives
Once patients are in hospital protocols can help limit their stay, but the biggest impact will come from discharging patients to other forms of care
We need a new currency for secondary care, couched in terms of what needs to be done, rather than where it is done
Figure 1.
Schematic model of relation between disease severity and management thresholds over time
Below a certain degree of severity (threshold A) a patient’s condition can be managed within primary care alone; beyond it, some specialist ambulatory care input is required—for example, outpatient referral or specialist home nursing. As a condition becomes more severe, hospitalisation may become necessary (threshold B). The focus of this paper is on demand management within and beyond secondary care. This includes patients’ arrival at the admission threshold (B), their subsequent inpatient episode, and the management of their demand for resources after discharge.
Supply and demand for hospital care
Although the presumption often exists that many of the options for managing demand may have been exhausted once the patient has reached hospital, opportunities for managing demand for hospital services do exist at this stage. Three types of intervention are available (see box). The least sophisticated is to restrict the supply of beds. Roemer’s law, which states that “a bed built is a bed filled,” suggests that increasing supply will increase admissions or length of stay.2 This seems to be confirmed by the work of Carr-Hill et al, who found that supply had a positive impact on hospital use.3 The demand for and supply of hospital services and beds therefore seem to be intimately linked, and it seems that the level of supply may act directly on the demand for admission to hospital.
Approaches to managing demand for hospital care
Supply side measures
(Raising admission threshold B by constricting supply)
Closing beds or departments, reducing staffing, etc
Preadmission policies
(Preventing or deferring a patient from crossing threshold B)
Waiting lists (including condition-specific waiting lists)
Protocols for referral
User charges
Measures to prevent or divert admissions on presentation
Policies within the hospital
(Reducing resource use once a patient has crossed threshold B)
Reducing the length of time patients spend in hospital
Controlling consumption of resources in hospital
Reductions in supply might therefore be expected to reduce demand and length of stay. In 1995-6 there were 21% fewer beds in England than in 1985 but 18% more inpatients were treated.4 Effective demand had apparently increased, while supply had reduced. In fact productivity had increased faster than reductions in supply—acute length of stay fell by 3.7% per year on average while the bed stock shrank by only 2.3% per year.4 Thus closing beds had not actually reduced supply capacity.
Policies at the admission threshold
Waiting lists have long been held to be a key method of rationing and demand management in NHS. Waiting lists are not, however, as direct a method of demand management as is often supposed, as most patients placed on a waiting list do generally go on to receive treatment. Nevertheless, some studies have found that, after a period of waiting, some patients no longer require surgery. Sometimes, conditions may indeed be self limiting, but in others this amounts to a crude method of triage at the expense of those who require treatment.5 In the case of cardiac surgery, for instance, the reason for not requiring surgery is higher mortality among waiting patients.6
If waiting lists do reduce demand, it is probably because of their effect on the expectations and referral practices of general practitioners. This effect is unpredictable, particularly if Frankel and West are correct in suggesting that waiting lists may sometimes protect “patients and practitioners from being forced to acknowledge . . . the triviality or the intractability of particular conditions.”7 Using waiting lists without explicit criteria for referral and inclusion can be inequitable, while delaying treatment may result in an emergency presentation, with increased risk to the patient and a higher cost of treatment.
An implicit assumption often exists that elective cases are less important than medical emergencies because we tend to equate abruptness of presentation with urgency of need. In fact many elective cases are urgent, while a significant proportion of emergency cases do not need to be admitted to hospital. An important innovation in emergency care in recent years has been the introduction of short stay observation or medical assessment units within or alongside accident and emergency departments, which aim safely to identify “borderline” patients who will not actually require admission—for example, by ruling out acute myocardial infarction.8 Meanwhile, admissions units are increasingly used to provide more intensive investigaton and active treatment for up to 48 hours to allow early discharge or transfer to less acute wards.9
Typically, such units will have a higher ratio of senior doctors than conventional accident and emergency departments, working more systematically to protocols of care for key conditions. Perhaps not surprisingly, more experienced staff, working at a more deliberate pace than their junior colleagues in the chaotic environment of accident and emergency, will display substantially higher admission thresholds. Another important feature of such models is their ability to provide a single point of timely access to non-hospital alternatives. A range of services which aim explicitly to prevent admission through provision of nursing and treatment in the home or in intermediate care facilities has been implemented in Britain, often with some success (but see box for discussion).
Changing the currency of demand: substitutes for hospital care
Despite their increasing popularity and clinical viability, evidence on the demand management potential of most of the established or proposed models of intermediate care remains unclear. As such substitutes for hospital care become more widespread, their very success may undermine the usefulness of existing currencies of demand for hospital care—that is, admissions and bed days. In future, effective demand management will require a currency that encompasses both hospital care and substitutes for hospital—for example, a “secondary care therapeutic episode”—without specifying demand for care in terms of institutions or buildings. Failure to do so might open the possibility of inadvertently expanding supply and demand through uncontrolled opening of intermediate care alternatives. Key challenges for future demand management in intermediate care include the following.
Substitutes for hospital admission
The specificity of admission avoidance substitutes must be closely monitored, as their key risk is that they may accept patients who otherwise would not have been admitted to hospital
If the aim of such substitutes is to treat a constant level of demand at a reduced cost, then their introduction must be accompanied by closure of acute capacity. Failure to close capacity will lead to increased supply, cost, and effective demand. They may, however, represent the most cost effective means of meeting an expanding demand
Substitutes for hospital stay (early discharge models)
To tackle effectively the key source of demand for bed days, intermediate care must target the long stay bed blockers—that is, the hardest target group to move out of hospital
Considerable care must be taken to compare fully the incremental costs of intermediate care and the acute care it seeks to replace
The provision of intermediate care that is not accompanied by reductions in acute capacity will, again, increase supply, costs, and effective demand
A final set of demand management tools operating on the admission threshold involves the use of financial incentives. Such incentives can apply to healthcare purchasers, providers, or users. A few studies from the United States have considered the impact of charging direct user fees to inpatients. Siu et al found that increasing levels of cost sharing by patients did indeed reduce admissions—but did so by reducing both inappropriate and clinically appropriate admissions alike, suggesting that this approach is something of a blunt instrument.10
Changing the incentives of purchasers and providers will change organisational behaviour. Crucially, transferring financial risk to health care providers will tend to lead them to manage demand for their own services more robustly. The abandonment of contracting and a move to longer term fixed funding agreements11 will represent a return to providers bearing greater financial risk, and this may reduce incentives to increase activity levels.
Post-admission policies
Once patients have been admitted to hospital two sets of strategies can be used to improve the appropriateness with which they use resources: improving efficiency, and earlier discharge of patients who have ceased to benefit from hospital care.
Successfully managing the demand for resources generated by patients once in a hospital bed relies critically on the use of protocols and guidelines. Their use improves the speed of decision making and organisation of care, reducing the number of interactions with professionals and minimising variations in patterns of care. As well as reducing length of stay, protocols have also been credited with having an impact on the use of drugs and other inputs such as nursing or therapy time12 and achieve important benefits by reducing duplication or unecessary use of investigations.
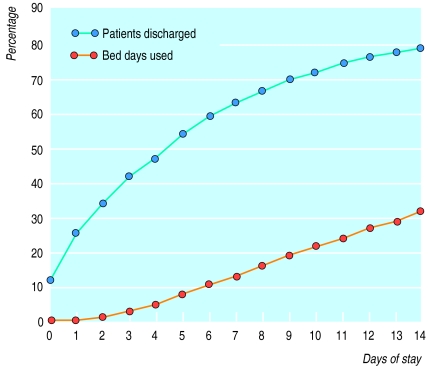
The biggest gains in managing demand for bed days are probably to be made from changing the model of care for the many inpatients who have ceased to benefit from the services of the acute hospital. In several specialties a relatively small number of patients account for a very high proportion of total bed days. Figure 2 shows the cumulative distribution of length of stay for general medicine and care of the elderly for a general hospital. After 14 days all but 20% of patients have been discharged—but these patients account for almost 70% of the bed days generated. Many of these patients will have ceased to benefit from acute hospital care, and their reasons for being in hospital will often only tangentially relate to their reason for admission.
Figure 2.
Cumulative use of beds and discharges by day of discharge in general medicine and care of the elderly, Burton General Hospital 1996-7 (source: South Staffordshire Health Authority)
Published data suggest that 4.4-62% of bed days in acute care are inappropriate,13 depending on the specialties studied, the country in which the study was conducted, and the instrument used. The greatest opportunities for change are in the medical specialties, particularly care of the elderly, and orthopaedics. Clarke reviewed studies of the effect of length of stay on outcome, and, although noting methodological problems in almost every study, she confirms that “all studies reported find no important effect of shorter stay on health outcome.”14
Nursing homes, residential care, and home care services generally are necessary to allow these “ceased to benefit” patients to be discharged. Overall, there is increasing consensus among clinicians, managers, and policymakers that intermediate care through models such as community hospitals, “step down” beds, nursing homes, and “hospital at home” is clinically effective and acceptable to patients. However, policy questions remain over the extent to which such alternatives can help with the management of overall demand for health care (see box).
Tertiary referral
Purchasers of health care have long been interested in tertiary referrals because of their high cost. There is also a suspicion that some of this work could be done more cost effectively locally. Any analysis of demand management in tertiary care is hampered by the absence of a meaningful definition. “Tertiary” referrals are no longer simply consultant to consultant referrals and, except in undisputed tertiary specialties such as cardiac surgery or neurosurgery, tertiary services often treat diseases with identical diagnostic codes to those seen in secondary care. Distance and the supply of health services seem to have an impact on demand, but attempts by policymakers to control demand do not seem to have succeeded.
Conclusions
Successfully managing demand for secondary care in a changing health care system requires attention to several lessons. The use of effective access filters at key thresholds will remain crucial. It will be important to ensure that, as the range of alternatives to admission grows, new access filters are inserted for these hospital substitutes. It is not hard to imagine a situation in which direct access by general practitioners to community hospital beds leads to substantial increases in overall hospitalisation—quite the reverse of what was intended. To ensure that the incentives to manage demand remain properly aligned with changing models of service delivery, thought will need to be given to a new currency for secondary care which captures its diagnostic and therapeutic qualities, rather than its institutional qualities.
Within secondary care, the important role of protocols in managing demand for healthcare resources will continue to grow. Initiatives such as the establishment of the National Institute for Clinical Excellence11 could have a profound influence on improving the quality, appropriateness, equity, and efficiency of care. The challenge here, however, is to guard against the ossification of practice: adherence to obsolete protocols remains a key driver of the substantial excess demand for hospital care in the former Soviet Union and Eastern Europe.
For these tools to be effective, they must be acceptable to individuals—both as patients and as citizens. Most crucially, patients and their families will increasingly be expected to accept home or intermediate care in place of admission, and to accept ever earlier discharge. In fact, the day surgery revolution of the late 1980s and early 1990s and long term changes in maternity care provide clear success stories. Nevertheless, more is required to change expectations than slick marketing and worthy exhortations to the public to accept the tenets of evidence based medicine. Crucially, expectations will adapt and changing patterns of care will be most readily accepted if patients’ trust is won through positive experiences. If alternatives to hospital care are not properly resourced and well managed, patients will see only “cuts,” shifting the burden of care on to them and their carers.
Table.
Hospital activity (thousands) in England 1991-2 to 1996-7
| 1991-2 | 1992-3 | 1993-4 | 1994-5 | 1995-6 | 1996-7 | |
|---|---|---|---|---|---|---|
| Ordinary admissions (total acute) | 5 404 | 5 460 | 5 573 | 5 662 | 5 844 | 5 864 |
| Accident and emergency attendances (total) | 13 305 | 13 070 | 13 289 | 13 812 | 14 234 | 14 080 |
| Outpatient attendances (total acute) | 31 825 | 32 595 | 33 362 | 34 452 | 35 398 | 36 057 |
| Day case admissions (total acute) | 1 530 | 1 781 | 2 076 | 2 433 | 2 806 | 2 910 |
Source: Department of Health. Statistical Bulletin 1997/20.
Acknowledgments
We thank Rachel Stokes for her help in assembling materials and commenting on drafts of this paper.
References
- 1.NHS Confederation; Royal College of Physicians. Tackling emergency admisions: policy into practice. Birmingham: NHS Confederation; 1997. [Google Scholar]
- 2.Van Doorslaer EKA, van Vliet RCJA. A built bed is a filled bed? An empirical re-examination. Soc Sci Med. 1989;28:155–164. doi: 10.1016/0277-9536(89)90143-3. [DOI] [PubMed] [Google Scholar]
- 3.Carr-Hill RA, Hardman G, Martin S, Peacock S, Sheldon TA, Smith P. A formula for distributing NHS revenues based on small area use of hospital beds. York: Centre for Health Economics, University of York; 1994. [Google Scholar]
- 4.Department of Health. Hospital activity statistics: England 1986 to 1996/97. Statistical Bulletin 1997:20.
- 5.Naylor CD, Slaughter PM. A stitch in time: case for assessing the burden of delayed surgery. Quality in Health Care. 1994;3:221–224. doi: 10.1136/qshc.3.4.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marber M, MacRae C, Joy M. Delay to invasive investigation and revascularisation for coronary heart disease in South West Thames region: a two tier system? BMJ. 1991;302:1189–1191. doi: 10.1136/bmj.302.6786.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frankel S, West R. What is to be done? In: Frankel S, West R, editors. Rationing and rationality in the NHS. The persistence of waiting lists. London: Macmillan; 1993. pp. 115–131. [Google Scholar]
- 8.Gaspoz JM, Lee TH, Weinstein MC, Cook EF, Goldman P, Komaroff AL, et al. Cost-effectiveness of a new short-stay unit to “rule out” acute myocardial infarction in low risk pateints. J Am Coll Cardiol. 1994;24:1249–1259. doi: 10.1016/0735-1097(94)90106-6. [DOI] [PubMed] [Google Scholar]
- 9.Audit Commission. Lying in wait: the use of medical beds in acute hospitals. London: HMSO; 1992. [Google Scholar]
- 10.Siu AL, Sonnenberg FA, Manning WG, Goldberg GA, Bloomfield ES, Newhouse JP, et al. Inappropriate use of hospitals in a randomized trial of health insurance plans. N Engl J Medicine. 1986;315:1259–1266. doi: 10.1056/NEJM198611133152005. [DOI] [PubMed] [Google Scholar]
- 11.Secretary of State for Health. The new NHS. London: Stationery Office; 1997. (Cm 3807). [Google Scholar]
- 12.Poole P, Johnson S. Integrated care pathways: an orthopaedic experience. Physiotherapy. 1996;82:28–30. [Google Scholar]
- 13.Coast J, Inglis A, Morgan K, Gray S, Kammerling M, Frankel S. The hospital admissions study in England: are there alternatives to emergency hospital admission? J Epidemiol Comm Health. 1995;49:194–199. doi: 10.1136/jech.49.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clarke A. Why are we trying to reduce length of stay? Evaluation of the costs and benefits of reducing time in hospital must start from the objectives that govern the change. Quality in Health Care. 1996;5:172–179. doi: 10.1136/qshc.5.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]