Abstract
Each year approximately 700 people die in the United States from pregnancy-related complications. We describe the characteristics of pregnancy-related deaths due to mental health conditions, including substance use disorders, and identify opportunities for prevention based on recommendations from fourteen state Maternal Mortality Review Committees (MMRCs) from the period 2008–17. Among 421 pregnancy-related deaths with an MMRC-determined underlying cause of death, 11 percent were due to mental health conditions. Pregnancy-related mental health deaths were more likely than deaths from other causes to be determined by an MMRC to be preventable (100 percent versus 64 percent), to occur among non-Hispanic White people (86 percent versus 45 percent), and to occur 43–365 days postpartum (63 percent versus 18 percent). Sixty-three percent of pregnancy-related mental health deaths were by suicide. Nearly three-quarters of people with a pregnancy-related mental health cause of death had a history of depression, and more than two-thirds had past or current substance use. MMRC recommendations can be used to prioritize interventions and can inform strategies to enable screening, care coordination, and continuation of care throughout pregnancy and the year postpartum.
Pregnancy-related complications take the lives of approximately 700 people in the US each year.1 A previous report on pregnancy-related deaths reviewed by fourteen state Maternal Mortality Review Committees (MMRCs) found that mental health conditions were a leading underlying cause of death, accounting for nearly 9 percent of such deaths.2
Rates of depressive disorder diagnoses during delivery hospitalizations increased from 4.1 per 1,000 in 2000 to 28.7 per 1,000 in 2015.3 Co-occurring depression, anxiety disorder, and substance use disorder (SUD) are also common among women of reproductive age.4 Professional and clinical organizations have issued recommendations to address screening and treatment for perinatal depression.5–7 The Council on Patient Safety in Women’s Health Care developed a consensus statement to guide the implementation of screening, intervention, referral, and follow-up care of mental health conditions in perinatal care,8 and the American Academy of Pediatrics recommends screening for postpartum depression during well-child visits.9 Yet barriers to care limit access to and use of mental health services among pregnant and postpartum people.10 Untreated perinatal mood and anxiety disorders have high societal costs11 and deleterious effects on maternal and infant outcomes.12
State and local MMRCs are uniquely positioned to evaluate the events in a pregnant or postpartum person’s life and surrounding their death. These multidisciplinary committees identify and review deaths occurring during pregnancy or within one year from the end of pregnancy. Using a standardized committee decisions form13 (which has been adapted over time), MMRCs determine pregnancy-relatedness and preventability, identify the medical and nonmedical contributors to the deaths, and make recommendations intended to eliminate preventable deaths. Through analysis of data from fourteen state MMRCs, we identify the characteristics of and factors contributing to pregnancy-related deaths caused by mental health conditions, including SUD. Based on the committees’ recommendations, we highlight opportunities for the prevention of pregnancy-related mental health deaths and for improved care during pregnancy and the postpartum year.
Study Data And Methods
We conducted a cross-sectional analysis of pregnancy-related deaths in the period 2008–17 and reviewed by MMRCs in Arizona (2016), Colorado (2008–12, 2014–15), Delaware (2009–17), Florida (2017), Georgia (2012–14), Hawaii (2015–16), Illinois (2015), Louisiana (2017), Mississippi (2016–17), North Carolina (2014–15), Ohio (2008–16), South Carolina (2014–17), Tennessee (2017), and Utah (2014–16).
Described in detail elsewhere,14,15 MMRCs convene at the local or state level to comprehensively review deaths occurring during pregnancy or within one year of the end of pregnancy. They have access to clinical and nonclinical information (from autopsy, prenatal care, law enforcement, and other reports) to more fully understand the circumstances surrounding each death and to develop recommendations to prevent similar deaths in the future. The data included in this report were voluntarily shared by the fourteen state MMRCs with the Centers for Disease Control and Prevention (CDC) through the Maternal Mortality Review Information Application.16 The application is a data system designed to facilitate and standardize MMRC functions by serving as a repository of abstracted information and committee deliberations on pregnancy-relatedness, preventability, contributing factors, and recommendations for prevention.
Specific methods for identifying deaths during or within one year of pregnancy vary by state, but in general, death records are linked to birth and fetal death records from the year of death and the year before death. Death records were also selected if the death record pregnancy checkbox indicated that the person was pregnant at the time of death or within one year of death;17 the death record included International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, cause-of-death codes related to pregnancy (A34 and O00–96 or O98–99); or the cause-of-death description indicated pregnancy. Additional deaths may be identified through other modes such as hospital reporting.
This analysis did not involve human subjects as defined in 45 CFR 46.102(e)18 and therefore was not reviewed by an Institutional Review Board. Recognizing that pregnancy-associated deaths can occur among transgender or nonbinary people, we use the term “people” to include women and other people who are pregnant or postpartum.
DEFINITIONS AND DETERMINATINS
A death was considered pregnancy-related if the MMRC determined that the death was the result of a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiologic effects of pregnancy. The CDC provided MMRCs with technical assistance, including coding of mental health conditions as the underlying cause of a pregnancy-related death. For this analysis, pregnancy-related deaths due to mental health conditions were defined as any pregnancy-related deaths for which the MMRC assigned mental health conditions, depression, or other psychiatric conditions as an underlying cause of death, including all suicides, as well as overdoses of unintentional (accidental) or unknown intent where SUD was indicated. Deaths with SUD indicated may include those with a SUD diagnosis in the abstracted records or where an expert on the MMRC (such as a psychiatrist or psychologist) felt that the criteria for a diagnosis of SUD were met based on their review of the circumstances surrounding the death. To ensure standardized methodology across states, the CDC reviewed all pregnancy-related deaths submitted by MMRCs for consistency with a standardized coding scheme (see online appendix exhibit A1).19 From this review, we identified five additional pregnancy-related suicide deaths and four additional pregnancy-related unintentional overdoses for which the state MMRCs indicated that SUD contributed to the death but did not assign mental health conditions as the underlying cause and included them in our analysis. These findings will also guide future CDC technical assistance related to the classification of pregnancy-related suicide and overdose deaths.
Among all pregnancy-related deaths classified as being due to mental health conditions, the specific manner of death was categorized as suicide, unintentional poisoning/overdose, or other causes based on MMRC determination. For deaths missing an MMRC determination, at least two coauthors independently reviewed records entered into the Maternal Mortality Review Information Application to determine the specific manner of death. Manner of death categorized as other causes included four overdoses of unknown intent, one injury of unknown intent, and one noninjury death in which the MMRC determined that mental health conditions initiated the chain of events leading directly to death and should be the underlying cause.
For each death, MMRCs document whether the death was preventable (yes or no) and whether there was no chance, some chance, or a good chance that the death could have been averted by one or more reasonable changes to patient, family, provider, facility, community, or systems factors.13 A death is considered preventable if the MMRC determines that there was at least some chance of the death being averted by one or more reasonable changes to any of these factors. In such instances, the committee selects a “yes” response to preventability or indicates on the MMRC decisions form that there was some chance or a good chance that the outcome could have been altered. Timing of death relative to pregnancy was calculated as number of days between the death record date of death and the date of delivery indicated on the linked birth or fetal death record. For deaths without a linked record, the death record pregnancy checkbox was used to assign timing. We defined leading causes as causes with at least ten deaths.
Race and ethnicity were classified as non-Hispanic White, non-Hispanic Black, Hispanic, or non-Hispanic other race, using race or ethnicity on linked birth or fetal death records (64 percent) or from death records when birth or fetal death records were not available (36 percent). (Hereafter references to race are non-Hispanic unless otherwise indicated.) Age at death was determined using death records. Specific mental health conditions (anxiety disorder, postpartum depression, preexisting or history of depressive disorder, other mood or psychotic disorder [bipolar disorder and depression, psychoses, schizophrenia, and personality disorder], and substance use disorder), life stressors (unstable housing or homelessness, history of incarceration, removal of a child from the person’s custody or Child Protective Services involvement, medication instability, adverse childhood event, unemployment, domestic violence, previous suicide attempt or attempts, and recent miscarriage), and previous or current substance use (with or without diagnosis of SUD) were identified through review of abstracted records and validated by at least two coauthors. If the abstracted records made no mention of a specific mental health condition, life stressor, or substance use, they were considered not present.
The MMRCs identified contributing factors from a list of twenty-five factors listed on the MMRC decisions form (see appendix exhibit A2);19 provided a description of each factor; and determined whether the factor should be categorized at the patient, family, provider, facility, community, or systems level. Contributing factors may be documented at multiple levels. MMRCs selected only factors that directly contributed to a death, not factors merely present in a decedent’s life. Actionable recommendations for prevention, addressing the identified contributing factors, were also made by MMRCs and documented on decision forms. Two coauthors performed a content analysis to categorize MMRC recommendations by topic area.
STATISTICAL ANALYSES
Descriptive results were calculated as counts and percentages. Chi-square or Fisher’s exact tests were used to assess differences in characteristics between pregnancy-related mental health deaths and pregnancy-related deaths from all other causes. Results were considered statistically significant at a p value less than 0.05. Percentages with a denominator of less than 10 were suppressed. All analyses were performed using SAS, version 9.4.
LIMITATIONS
These data are limited by the completeness and accuracy of the original and abstracted records. Life stressors and specific mental health conditions may be underestimated if information was not available to abstractors or documented during abstraction. Although our classification of SUD was limited to documentation in the abstracted records, MMRC experts may have determined that additional decedents met the criteria for SUD. Even so, unintentional overdoses and overdoses of unknown intent were assigned mental health conditions as an underlying cause of death only if the MMRC determined that SUD was present; these deaths may be undercounted because of underdiagnosis of SUD. Formal diagnoses for the specific mental health conditions could not always be differentiated from chart notes or self-report, and it was sometimes difficult to distinguish past versus current substance use. Data were aggregated over multiple years and jurisdictions and might not be nationally representative or reflect changes over time. Recognizing that mental health disorders (acute and chronic) are a risk factor for suicide and that treatment of these disorders is an important prevention opportunity,20 CDC guidance is for MMRCs to classify all pregnancy-related suicides as mental health deaths. It is possible that suicides not related to mental health conditions were included in our analysis. A previous report found that 66 percent of female suicide deaths had a diagnosed mental health condition.21 Recommendations made by individual MMRCs might not be applicable across jurisdictions.
Study Results
Among all deaths reviewed by the fourteen state MMRCs from 2008 to 2017, there were 421 pregnancy-related deaths with an underlying cause of death determination; 46 of them (11 percent) were due to mental health conditions. Race and ethnicity data were available for 96 percent of pregnancy-related mental health deaths. Most of the pregnancy-related mental health deaths (86 percent) occurred among White people (exhibit 1). This distribution of race and ethnicity differed significantly from that seen in pregnancy-related deaths from all other causes. Most of the pregnancy-related mental health deaths occurred among people who completed high school or less (52 percent) or who were covered by Medicaid during prenatal care or at time of delivery (63 percent). Differences in age, education, and Medicaid status distributions between pregnancy-related mental health deaths and pregnancy-related deaths from all other causes were not statistically significant.
Exhibit 1.
Characteristics of pregnancy-related deaths with a known cause of death in 14 US states, 2008–17
| Characteristics | All known causes of death (N = 421) |
Attributable to causes other than mental health conditions (n = 375) |
Attributable to mental health conditions (n = 46) |
p valuea | |||
|---|---|---|---|---|---|---|---|
| Number | Percent | Number | Percent | Number | Percent | ||
| Mother’s race/ethnicity | <0.001 | ||||||
| Hispanic | 33 | 8 | 30 | 8 | 3 | 7 | |
| Non-Hispanic Black | 158 | 38 | 157 | 43 | 1 | 2 | |
| Non-Hispanic White | 202 | 49 | 164 | 45 | 38 | 86 | |
| Non-Hispanic other | 18 | 4 | 16 | 4 | 2 | 5 | |
| Missing | 10 | —b | 8 | —b | 2 | —b | |
| Mother’s age, years | 0.51 | ||||||
| 15–24 | 102 | 25 | 88 | 24 | 14 | 31 | |
| 25–34 | 205 | 50 | 183 | 50 | 22 | 49 | |
| 35 or older | 103 | 25 | 94 | 26 | 9 | 20 | |
| Missing | 11 | —b | 10 | —b | 1 | —b | |
| Mother’s educational attainment | 0.28 | ||||||
| High school or less | 217 | 54 | 193 | 54 | 24 | 52 | |
| Some college | 78 | 19 | 68 | 19 | 10 | 22 | |
| Associate’s or bachelor’s degree | 71 | 18 | 60 | 17 | 11 | 24 | |
| Advanced degree | 35 | 9 | 34 | 10 | 1 | 2 | |
| Missing | 20 | —b | 20 | —b | 0 | —b | |
| Covered by Medicaid during prenatal | |||||||
| care or at time of delivery | 0.47 | ||||||
| Yes | 191 | 57 | 166 | 56 | 25 | 63 | |
| No | 143 | 43 | 128 | 44 | 15 | 38 | |
| Missing | 87 | —b | 81 | —b | 6 | —b | |
| Preventability of mother’s death | <0.001 | ||||||
| Preventable | 226 | 68 | 189 | 64 | 37 | 100 | |
| Not preventable | 106 | 32 | 106 | 36 | 0 | 0 | |
| Missing | 89 | —b | 80 | —b | 9 | —b | |
| Timing of mother’s death in relation | |||||||
| to pregnancy | <0.001 | ||||||
| During pregnancy | 139 | 33 | 130 | 35 | 9 | 20 | |
| Within 42 days postpartum | 183 | 44 | 175 | 47 | 8 | 17 | |
| 43–365 days postpartum | 95 | 23 | 66 | 18 | 29 | 63 | |
| Missing | 4 | —b | 4 | —b | 0 | —b | |
source Authors’ analysis of pregnancy-related deaths with known cause of death occurring during the period 2008–17 and reviewed by fourteen state Maternal Mortality Review Committees (states and years provided in the text).
For comparisons of the characteristics of people with pregnancy-related deaths attributable to mental health conditions and the characteristics of those with pregnancy-related deaths attributable to all other causes, p value calculated using chi-square test, with Fisher’s exact test used for expected cell counts less than 5.
Not applicable.
PREVENTABILITY
A preventability determination was made for 79 percent of pregnancy-related deaths with a known cause of death; 68 percent were determined to be preventable (exhibit 1). Among these 226 preventable deaths, mental health conditions were the leading underlying cause (exhibit 2).
Exhibit 2: Leading causes of pregnancy-related death among deaths determined to be preventable in 14 US states, 2008–17.
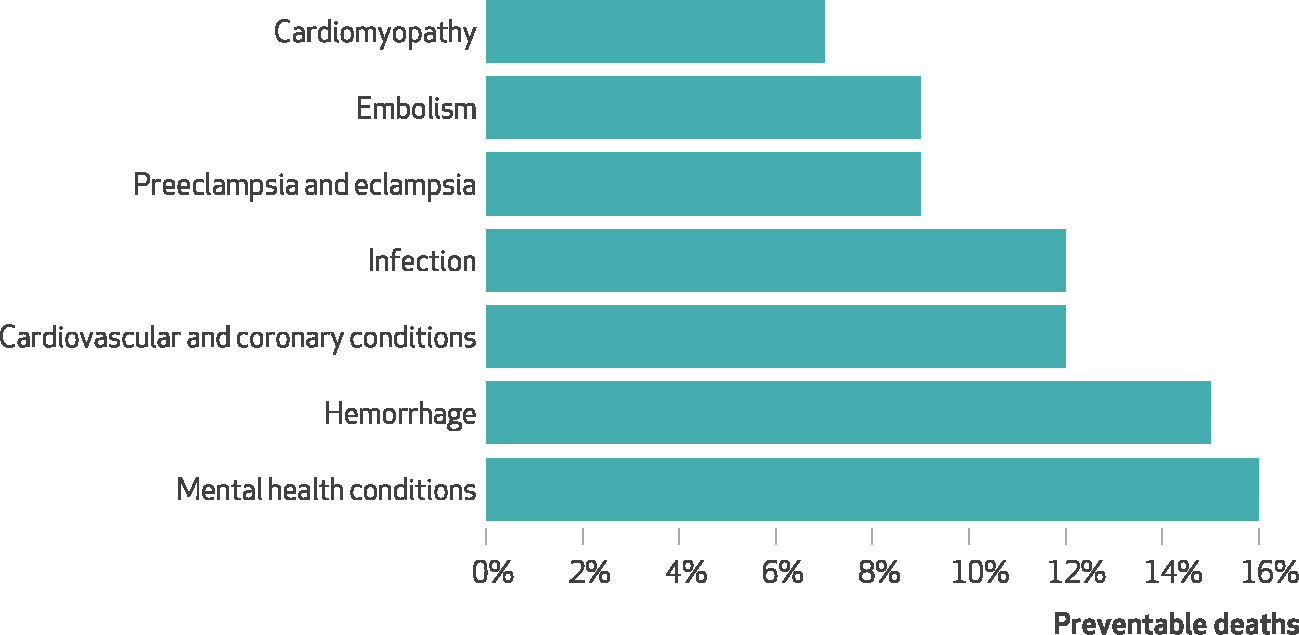
source Authors’ analysis of pregnancy-related deaths occurring during the period 2008–17 and determined by fourteen state Maternal Mortality Review Committees (as listed in the text) to be preventable. notes N = 226. Leading causes were defined as causes with at least ten deaths. Percentages do not sum to 100 percent.
Among 37 pregnancy-related mental health deaths for which an MMRC preventability determination was made, 100 percent were determined preventable. In comparison, among 295 pregnancy-related deaths from other causes and with a preventability determination, 64 percent were determined preventable (exhibit 1).
TIMING OF DEATH
Timing of death differed significantly for mental health deaths compared with other causes; 63 percent of pregnancy-related mental health deaths occurred 43–365 days postpartum, compared with 18 percent of deaths from other causes (exhibit 1).
MANNER OF DEATH
Exhibit 3 provides more detail on pregnancy-related deaths determined to have mental health causes. Among the forty-six such deaths, 63 percent were suicides, 24 percent were unintentional poisonings/overdoses, and 13 percent were classified as other causes. Among suicides, 34 percent were firearm injury deaths, 34 percent were hanging deaths, 14 percent were intentional poisonings/overdoses, and 17 percent were other means of fatal injury. In total, 41 percent of pregnancy-related mental health deaths were overdoses or poisonings: 58 percent were unintentional, 21 percent were intentional, and 21 percent were of unknown intent (data not shown).
Exhibit 3.
Manner of death, means of fatal injury among suicide deaths, mental health conditions, substance use, and life stressors recorded for pregnancy-related deaths attributable to mental health conditions in 14 US states, 2008–17
| Number | Percent | |
|---|---|---|
| manner of death | ||
| Suicide | 29 | 63 |
| Unintentional poisoning/overdose | 11 | 24 |
| Othera | 6 | 13 |
| means of fatal injury among suicide deaths | ||
| Firearm | 10 | 34 |
| Hanging | 10 | 34 |
| Intentional poisoning/overdose | 4 | 14 |
| Other | 5 | 17 |
| mental health conditions b | ||
| Preexisting or history of depressive disorder | 33 | 72 |
| Anxiety disorder | 22 | 48 |
| Substance use disorder | 10 | 22 |
| Other mood or psychotic disorder | 8 | 17 |
| Postpartum depression | 7 | 15 |
| substance use and life stressors c | ||
| Substance use with or without SUD diagnosis | 31 | 67 |
| Unstable housing or homelessness | 4 | 9 |
| History of incarceration | 7 | 15 |
| Removal of child from custody, Child Protective Services involvement | 11 | 24 |
| Medication instability | 18 | 39 |
| Adverse childhood event | 6 | 13 |
| Unemployment | 6 | 13 |
| Domestic violence | 9 | 20 |
| Previous suicide attempt or attempts | 10 | 22 |
| Recent miscarriage | 2 | 4 |
source Authors’ analysis of pregnancy-related deaths attributable to mental health conditions occurring during the period 2008–17 and reviewed by fourteen state Maternal Mortality Review Committees, as listed in the text. Definitions of selected mental health conditions, substance use, and life stressors are in appendix exhibit A4 (see note 19 in text).
Includes four overdoses of unknown intent, one injury of unknown intent, and one noninjury death for which the Maternal Mortality Review Committee determined that a mental health condition was the underlying cause.
People may have more than one condition; classification is based on information provided in the abstracted records.
People may have experienced more than one life stressor.
MENTAL HEALTH CONDITIONS
Mental health conditions noted in the abstracted records for pregnancy-related mental health deaths included preexisting or history of depressive disorder, anxiety disorder, SUD, other mood or psychotic disorder, and postpartum depression; each person could have multiple conditions (exhibit 3).
SUBSTANCE USE AND LIFE STRESSORS
History of or current substance use (with or without diagnosis of SUD) was present in 67 percent of deaths. Common life stressors among people with pregnancy-related mental health deaths included medication instability, defined as an indication that the person stopped taking psychiatric drugs or medications for treatment of SUD or had a change in medication or dosage during pregnancy or postpartum (39 percent); removal of a child from the person’s custody or Child Protective Services involvement (24 percent); and previous suicide attempt or attempts (22 percent) (exhibit 3).
CONTRIBUTING FACTORS
Among the forty-six pregnancy-related mental health deaths in our data, MMRCs identified an average of six contributing factors per death. Of 289 total contributing factors, 148 (51 percent) were classified as occurring at the patient or family level, 60 (21 percent) at the system level, 59 (20 percent) at the provider level, and 11 (4 percent) each at the facility and community levels (data not shown). At the patient or family level, the most common factors were mental health conditions (20 percent), SUD (17 percent), adherence to medical recommendations (8 percent), social support or isolation (7 percent), knowledge (7 percent), and chronic disease (7 percent) (exhibit 4). Frequent contributing factors at the system level included continuity of care (n = 21, 35 percent), access or financial factors (n = 9, 15 percent), and communication (n = 5, 8 percent). At the community level, frequent factors included cultural or religious factors (n = 3, 27 percent) and social support or isolation (n = 2, 18 percent) (data not shown).
EXHIBIT 4: Contributing factors at the patient or family level for pregnancy-related deaths attributable to mental health conditions in 14 US states, 2008–17.

source Authors’ analysis of pregnancy-related deaths attributable to mental health conditions occurring during the period 2008–17 and reviewed by fourteen state Maternal Mortality Review Committees (as listed in the text). note There were a total of 148 contributing factors classified at the patient or family level.
RECOMMENDATIONS FOR PREVENTION
MMRC recommendations for preventing pregnancy-related mental health deaths ranged from individual, patient-level changes to larger community and systems changes that address social determinants of health. Topic areas included coordination of care; access to and availability of naloxone to treat opioid overdose; access to treatment and services for SUD and mental health conditions; prescribing practices; screenings and assessments; social, family, and peer support; and education for patients, providers, and the public. Illustrative examples of MMRC recommendations are in appendix exhibit A3.19
Discussion
Using data on pregnancy-related deaths from fourteen state Maternal Mortality Review Committees, we found that nearly one in nine pregnancy-related deaths had mental health conditions as the underlying cause. Among pregnancy-related mental health deaths with a preventability determination, 100 percent were preventable. Whereas 86 percent of pregnancy-related mental health deaths occurred among White people, only 2 percent occurred among Black people. The observed racial and ethnic disparities may reflect actual differences in leading causes of death, as well as differences in screening and identification practices. For example, White people are more likely to be screened for depression at delivery than Black people.22 Our finding is consistent with prior studies showing that US suicide and overdose deaths are higher among White people than Black people.23,24
Although 43 percent of 2017 US deliveries were covered by Medicaid,25 63 percent of people with a pregnancy-related mental health death were covered by Medicaid during prenatal care or at delivery. People with lower socioeconomic status often enter prenatal care later than more advantaged people, and they experience multiple barriers to accessing mental health care.10,26 Although the American Rescue Plan Act of 2021 gives states the temporary option to extend Medicaid postpartum coverage from sixty days to one year using a state plan amendment,27 pregnancy-related Medicaid eligibility for coverage ceases sixty days after delivery in most circumstances. Coverage may be extended though state-specific waivers, state Medicaid expansion, or other Medicaid eligibility categories such as for low-income parents. However, income thresholds are generally lower than the pregnancy income threshold.28 One in five people with recent live births whose prenatal care was covered by Medicaid report not currently having insurance coverage two to six months postpartum.29 The high percentage of pregnancy-related mental health deaths occurring 43–365 days postpartum can be used to inform discussions of Medicaid coverage that extends through the year postpartum for mental health screening and treatment continuation. Research shows that reimbursement of multiple postpartum visits instead of only a single visit may help ensure continued and coordinated care during the postpartum period.30,31
The finding that most people with a pregnancy-related mental health death had a history of depression highlights the potential need for ongoing prevention and treatment. The MMRC recommendations offer suggestions for addressing gaps in mental health services, including postpartum home visiting services, increased access to crisis response and walk-in centers for people needing substance use or mental health treatment, and screening for postpartum depression during postpartum visits. We found that previous or current substance use was present among 67 percent of pregnancy-related mental health deaths. The American College of Obstetricians and Gynecologists has several recommendations to address substance use during pregnancy, including provision of medications for opioid use disorders and programs to prevent relapse during the postpartum period.32,33 Clinical recommendations also exist for providers to screen mothers for postpartum depression during well-child visits and to screen all adults for depression during primary care visits.9,34 Integration of mental health and substance use services is needed for people with comorbid conditions.4
Pregnancy-related mental health deaths were more likely to be classified as preventable compared with deaths from other causes. Although mental health conditions were previously found to be the sixth leading underlying cause of all pregnancy-related deaths,2 we found them to be the leading cause among preventable deaths. Because obstetric providers are in an ideal position to intervene and address perinatal mental health, mental health care should be integrated into obstetric care.6,8 Coordination of care between obstetric, mental health, and substance use providers, including personalized transfer of care, has been shown to be crucial for ensuring prompt follow-up and receipt of care.30 Screenings should be performed in the context of systems that ensure diagnosis, treatment, and follow-up.6,34,35
Almost a quarter of pregnancy-related mental health deaths had documentation that there was removal of a child from the person’s custody or Child Protective Services involvement. Although it is hard to distinguish the role that this involvement played in subsequent substance use or suicidal ideation, there has been documentation of greater Child Protective Services involvement among mothers with mental health diagnoses, with amplified effects among those with mental health and SUD disorders, compared to mothers without such diagnoses.36 Our finding highlights a potential missed opportunity for coordination between child welfare and obstetric or mental health providers to offer support and resources.37 Programs such as Healthy Start; Special Supplemental Nutrition Program for Women, Infants, and Children; and organizations focused on home visitation and intimate partner violence prevention may also regularly interact with pregnant and postpartum people and could consider ways to offer screening and linkage to needed care and resources.
The contributing factors and MMRC recommendations highlight opportunities to prioritize interventions to reduce pregnancy-related mental health deaths. Although most contributing factors were classified at the patient or family level, what is experienced at this level has larger societal drivers and effects. This is emphasized by the focus of the recommendations at the community or system levels, which address factors that may be beyond the control of an individual patient or provider. By continuing to broaden their understanding and reporting of social and structural factors contributing to these deaths, MMRCs can increase the information available to guide community- and system-level prevention interventions.
Conclusion
MMRC data offer the most comprehensive view of the events leading to the death of pregnant and postpartum people. Our findings show that maternal health cannot be promoted without addressing maternal mental health. As evidenced by MMRC recommendations, there are many opportunities for preventing pregnancy-related mental health deaths through improvements in coordination of care; access to and availability of naloxone; access to treatment and services for SUD and other mental health conditions; prescribing practices; screenings and assessments; social, family, and peer support; and education for patients, providers, and the public. The MMRC recommendations can be used to prioritize interventions to avoid preventable pregnancy-related deaths attributable to mental health conditions and can inform strategies that enable screening, care coordination and transition across providers, and continuation of care throughout pregnancy and the year postpartum.
Supplementary Material
Acknowledgments
This work was supported in part by funding from Merck, through an award agreement with its Merck for Mothers Program, and through federal appropriations. This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention (CDC) administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the Department of Energy and the CDC. Tiffany Moore Simas is the engagement director of the Massachusetts Child Psychiatry Access Program (MCPAP) for Moms, funded by the Massachusetts Department of Mental Health and administrated through Beacon Health Options; is a multiple principal investigator or investigator on grants funded through the CDC, National Institutes of Health, Patient-Centered Outcomes Research Institute (PCORI), American College of Obstetricians and Gynecologists (ACOG), and Perigee; performs consultancy efforts through Lifeline4Moms related to perinatal psychiatry access programs; and is a focus-group participant for Roche Diagnostics. Nancy Byatt has received PCORI Grant No. IHS-2019C2-17367, Substance Abuse and Mental Health Services Administration Grant No. 1H79SM082771-01, ACOG Grant No. 6 NU380T000287-02-01, National Institute of Mental Health Grant No. 2R42 MH113381-02, PCORI Grant No. MAT-2018C2-12891, and CDC Grant No. 5U01DP006093-05 and has a Perigee Fund Grant agreement; has consulting agreements for implementation assistance with the Georgia Department of Public Health, Montana Department of Public Health and Human Services, University of North Carolina, Florida State University, and Dignity Health Medical Foundation; and receives funding for MCPAP for Moms from the Massachusetts Department of Mental Health. She has also received salary and/or funding support from the Massachusetts Department of Mental Health via MCPAP for Moms. She is also the statewide medical director of MCPAP for Moms and the executive director of Lifeline for Families. She has served on the Medscape Steering Committee on Clinical Advances in Postpartum Depression. She received honoraria from Medscape, Miller Medical Communications, and Mathematica. She has served on advisory boards for Sage Therapeutics. She has also served as a consultant for Ovia Health, Sage Therapeutics, or their agents, and has received speaking honoraria from Sage Therapeutics. The authors acknowledge the efforts of all members of the fourteen state Maternal Mortality Review Committees included in this analysis and their dedication to reviewing each pregnancy-associated death. The authors also honor the people who are no longer living but whose deaths are reviewed to eliminate future preventable pregnancy-related deaths. Maternal Mortality Review Committee data were provided by the Arizona, Colorado, Delaware, Florida, Georgia, Hawaii, Illinois, Louisiana, Mississippi, North Carolina, Ohio, South Carolina, Tennessee, and Utah Departments of Health or agencies responsible for maternal mortality review. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC, these states’ Departments of Health, or the agencies responsible for maternal mortality review. The authors are grateful to the Maternal Mortality Prevention Team at the CDC, the CDC Foundation, and the Association of Maternal and Child Health Programs.
Footnotes
This work was presented at the 67th Annual Meeting of the Academy of Consultation-Liaison Psychiatry (virtual) in November 2020 and at the Society for Pediatric and Perinatal Epidemiologic Research Annual Meeting (virtual) in June 2021.
Contributor Information
Susanna L. Trost, Oak Ridge Institute for Science and Education Fellow in the Division of Reproductive Health, Centers for Disease Control and Prevention (CDC), in Atlanta, Georgia.
Jennifer L. Beauregard, epidemiologist in the Division of Reproductive Health, CDC, and a lieutenant in the US Public Health Service, in Rockville, Maryland.
Ashley N. Smoots, epidemiologist in the Division of Reproductive Health, CDC.
Jean Y. Ko, lead for the Maternal Health and Chronic Disease Team, Division of Reproductive Health, CDC, and a commander in the US Public Health Service.
Sarah C. Haight, graduate research assistant in the Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, in Chapel Hill, North Carolina. She was an epidemiologist in the Division of Reproductive Health, CDC, at the time of writing.
Tiffany A. Moore Simas, chair of the Department of Obstetrics and Gynecology and medical director of the Lifeline for Moms Program, University of Massachusetts Medical School/UMass Memorial Health, in Worcester, Massachusetts..
Nancy Byatt, executive director of the Lifeline for Families Center and Lifeline for Moms Program, Department of Psychiatry, University of Massachusetts Medical School/UMass Memorial Health Care..
Sabrina A. Madni, statistician with BeVera Solutions in the National Center for Immunization and Respiratory Diseases, CDC. She was an Oak Ridge Institute for Science and Education Fellow in the Division of Reproductive Health, CDC, at the time of writing.
David Goodman, lead for the Maternal Mortality Prevention Team, Division of Reproductive Health, CDC..
NOTES
- 1.Centers for Disease Control and Prevention. Pregnancy-related deaths [Internet]. Atlanta (GA): CDC; 2019. Feb 26 [cited 2021 Jul 30]. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-relatedmortality.htm [Google Scholar]
- 2.Davis NL, Smoots AN, Goodman DA. Pregnancy-related deaths: data from 14 U.S. Maternal Mortality Review Committees, 2008–2017 [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2019. [cited 2021 Jul 30]. Available from: https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/MMR-Data-Brief_2019-h.pdf [Google Scholar]
- 3.Haight SC, Byatt N, Moore Simas TA, Robbins CL, Ko JY. Recorded diagnoses of depression during delivery hospitalizations in the United States, 2000–2015. Obstet Gynecol. 2019;133(6):1216–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou J, Ko JY, Haight SC, Tong VT. Treatment of substance use disorders among women of reproductive age by depression and anxiety disorder status, 2008–2014. J Womens Health (Larchmt). 2019;28(8):1068–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American College of Nurse-Midwives. Position statement: depression in women [Internet]. Silver Spring (MD): American College of Nurse-Midwives; 2013. May [cited 2021 Jul 30]. Available from: https://www.midwife.org/acnm/files/ACNMLibraryData/UPLOADFILENAME/000000000061/Depression%20in%20Women%20May%202013.pdf [Google Scholar]
- 6.American College of Obstetricians and Gynecologists. ACOG committee opinion no. 757: screening for perinatal depression. Obstet Gynecol. 2018;132(5):e208–12. [DOI] [PubMed] [Google Scholar]
- 7.Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Interventions to prevent perinatal depression: US Preventive Services Task Force recommendation statement. JAMA. 2019;321(6):580–7. [DOI] [PubMed] [Google Scholar]
- 8.Kendig S, Keats JP, Hoffman MC, Kay LB, Miller ES, Moore Simas TA, et al. Consensus bundle on maternal mental health: perinatal depression and anxiety. Obstet Gynecol. 2017; 129(3):422–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Earls MF, Yogman MW, Mattson G, Rafferty J, Committee on Psychosocial Aspects of Child and Family Health. Incorporating recognition and management of perinatal depression into pediatric practice. Pediatrics. 2019;143(1):e20183259. [DOI] [PubMed] [Google Scholar]
- 10.Byatt N, Biebel K, Lundquist RS, Moore Simas TA, Debordes-Jackson G, Allison J, et al. Patient, provider, and system-level barriers and facilitators to addressing perinatal depression. J Reprod Infant Psychol. 2012;30(5):436–49. [Google Scholar]
- 11.Luca DL, Garlow N, Staatz C, Margiotta C, Zivin K. Societal costs of untreated perinatal mood and anxiety disorders in the United States [Internet]. Cambridge (MA): Mathematica Policy Research; 2019. Apr 29 [cited 2021 Jul 30]. Available from: https://mathematica.org/publications/societal-costs-of-untreated-perinatal-mood-and-anxiety-disorders-in-the-united-states [Google Scholar]
- 12.Slomian J, Honvo G, Emonts P, Reginster J-Y, Bruyère O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health (Lond). 2019;15:1745506519844044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Review to Action. Maternal Mortality Review Committee decisions form [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2021. [cited 2021 Jul 30]. Available from: https://reviewtoaction.org/national-resource/maternal-mortality-review-committee-decisions-form [Google Scholar]
- 14.Zaharatos J, St Pierre A, Cornell A, Pasalic E, Goodman D. Building U.S. capacity to review and prevent maternal deaths. J Womens Health (Larchmt). 2018;27(1):1–5. [DOI] [PubMed] [Google Scholar]
- 15.St Pierre A, Zaharatos J, Goodman D, Callaghan WM. Challenges and opportunities in identifying, reviewing, and preventing maternal deaths. Obstet Gynecol. 2018; 131(1):138–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Maternal Mortality Review Information Application (MMRIA, or “Maria”) [Internet]. Atlanta (GA): CDC; 2020. May [cited 2021 Jul 30]. Available from:https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/MMRIA.html [Google Scholar]
- 17.Hoyert DL, Uddin SFG, Miniño AM. Evaluation of the pregnancy status checkbox on the identification of maternal deaths. Natl Vital Stat Rep. 2020;69(1):1–25. [PubMed] [Google Scholar]
- 18.Department of Health and Human Services, Office for Human Research Protections. 45 CFR 46 [Internet]. Rockville (MD): OHRP; 2018. [last updated 2021 Mar 10; cited 2021 Jul 30]. Available from: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html [Google Scholar]
- 19.To access the appendix, click on the Details tab of the article online.
- 20.Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N. Preventing suicide: a technical package of policy, programs, and practices [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2017. [cited 2021 Jul 30]. Available from: https://www.cdc.gov/violenceprevention/pdf/suicideTechnicalPackage.pdf [Google Scholar]
- 21.Petrosky E, Ertl A, Sheats KJ, Wilson R, Betz CJ, Blair JM. Surveillance for violent deaths—National Violent Death Reporting System, 34 states, four California counties, the District of Columbia, and Puerto Rico, 2017. MMWR Surveill Summ. 2020;69(8):1–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farr SL, Denk CE, Dahms EW, Dietz PM. Evaluating universal education and screening for postpartum depression using population-based data. J Womens Health (Larchmt). 2014;23(8):657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Curtin SC, Hedegaard H. Suicide rates for females and males by race and ethnicity: United States, 1999 and 2017 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2019. [cited 2021 Jul 30].Available from: https://www.cdc.gov/nchs/data/hestat/suicide/rates_1999_2017.htm [Google Scholar]
- 24.O’Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital Signs: characteristics of drug overdose deaths involving opioids and stimulants—24 states and the District of Columbia, January–June 2019. MMWR Morb Mortal Wkly Rep. 2020;69(35):1189–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2018. Nov 7 [cited 2021 Jul 30]. Available from: https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_08-508.pdf [PubMed] [Google Scholar]
- 26.Baer RJ, Altman MR, Oltman SP, Ryckman KK, Chambers CD, Rand L, et al. Maternal factors influencing late entry into prenatal care: a stratified analysis by race or ethnicity and insurance status. J Matern Fetal Neonatal Med. 2019;32(20):3336–42. [DOI] [PubMed] [Google Scholar]
- 27.American Rescue Plan Act of 2021, Pub. L. No. 117–2, Sec. 9812. Modifications to certain coverage under Medicaid for pregnant and postpartum women. [Google Scholar]
- 28.Haley J, Johnston EM. Closing gaps in maternal health coverage: assessing the potential of a postpartum Medicaid/CHIP extension [Internet]. New York (NY): Commonwealth Fund; 2021. Jan [cited 2021 Jul 30]. Available from: https://www.commonwealthfund.org/sites/default/files/2021-01/Urban_maternal_hlt_coverage_medicaid_chip_extension_ib.pdf [Google Scholar]
- 29.Johnston EM, McMorrow S, Alvarez Caraveo C, Dubay L. Post-ACA, more than one-third of women with prenatal Medicaid remained uninsured before or after pregnancy. Health Aff (Millwood). 2021;40(4):571–8. [DOI] [PubMed] [Google Scholar]
- 30.American College of Obstetricians and Gynecologists. ACOG committee opinion no. 736: optimizing postpartum care. Obstet Gynecol. 2018;131(5):e140–50. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Medicare and Medicaid Services. Lessons learned about payment strategies to improve postpartum care in Medicaid and CHIP [Internet]. Baltimore (MD): CMS; 2019. Aug [cited 2021 Jul 30]. Available from: https://www.medicaid.gov/medicaid/quality-of-care/downloads/postpartum-payment-strategies.pdf [Google Scholar]
- 32.American College of Obstetricians and Gynecologists. Policy priorities: substance use disorder in pregnancy [Internet].Washington (DC): ACOG; [cited 2021 Jul 30]. Available from: https://www.acog.org/advocacy/policy-priorities/substance-use-disorder-in-pregnancy [Google Scholar]
- 33.American College of Obstetricians and Gynecologists. Committee opinion no. 711: opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81–94. [DOI] [PubMed] [Google Scholar]
- 34.Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(4):380–7. [DOI] [PubMed] [Google Scholar]
- 35.Wachino V. CMCS informational bulletin: maternal depression screening and treatment: a critical role for Medicaid in the care of mothers and children [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services; 2016. May 11 [cited 2021 Jul 30]. Available from: https://www.medicaid.gov/federal-policy-guidance/downloads/cib051116.pdf [Google Scholar]
- 36.Hammond I, Eastman AL, Leventhal JM, Putnam-Hornstein E. Maternal mental health disorders and reports to Child Protective Services: a birth cohort study. Int J Environ Res Public Health. 2017;14(11):1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Center on Substance Abuse and Child Welfare. The use of peers and recovery specialists in child welfare settings [Internet]. Rockville (MD): NCSACW; 2018. [cited 2021 Jul 30]. Available from: https://ncsacw.samhsa.gov/files/peer19_brief.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


