Abstract
BACKGROUND
Robotic surgery (RS) is gaining popularity; however, evidence for abdominoperineal resection (APR) of rectal cancer (RC) is scarce.
AIM
To compare the efficacy of RS and laparoscopic surgery (LS) in APR for RC.
METHODS
We retrospectively identified patients with RC who underwent APR by RS or LS from April 2016 to June 2022. Data regarding short-term surgical outcomes were compared between the two groups. To reduce the effect of potential confounding factors, propensity score matching was used, with a 1:1 ratio between the RS and LS groups. A meta-analysis of seven trials was performed to compare the efficacy of robotic and laparoscopic APR for RC surgery.
RESULTS
Of 133 patients, after propensity score matching, there were 42 patients in each group. The postoperative complication rate was significantly lower in the RS group (17/42, 40.5%) than in the LS group (27/42, 64.3%) (P = 0.029). There was no significant difference in operative time (P = 0.564), intraoperative transfusion (P = 0.314), reoperation rate (P = 0.314), lymph nodes harvested (P = 0.309), or circumferential resection margin (CRM) positive rate (P = 0.314) between the two groups. The meta-analysis showed patients in the RS group had fewer positive CRMs (P = 0.04), lesser estimated blood loss (P < 0.00001), shorter postoperative hospital stays (P = 0.02), and fewer postoperative complications (P = 0.002) than patients in the LS group.
CONCLUSION
Our study shows that RS is a safe and effective approach for APR in RC and offers better short-term outcomes than LS.
Keywords: Robotic surgery, Laparoscopic surgery, Abdominoperineal resection, Postoperative complications, Propensity score
Core Tip: This study compared the efficacy of robotic surgery (RS) and laparoscopic surgery (LS) in abdominoperineal resection (APR) for rectal cancer (RC). Our results showed that RS patients had fewer positive circumferential resection margins, less estimated blood loss, shorter postoperative hospital stays, and fewer postoperative complications than did LS patients. Our findings demonstrate that RS is a safe and effective approach for APR in RC and offers better short-term outcomes than LS. This study contributes to the existing evidence base and can assist surgeons and healthcare providers in making informed decisions on using RS in APR for RC.
INTRODUCTION
Colorectal cancer is the third most common cancer and one of the most common causes of cancer-related deaths worldwide. Nearly 40% of colorectal cancers occur in the rectum[1]. Surgery is the primary treatment for rectal cancer (RC)[2]. Common surgical procedures for RC include intersphincteric resection, low anterior resection (LAR), anterior resection, and abdominoperineal resection (APR)[3]. APR, also known as Miles’s procedure, was first reported by Miles[4] in 1908. With the increasing use of LAR for lower RC, the application of APR has gradually declined. However, APR remains the best choice for RC cases in lower locations, cases with perianal muscle invasion, or cases where sphincter-preserving techniques are unsuitable for radical resection[5].
Laparoscopic minimally invasive surgery for colorectal cancer was first reported in the 1990s[5]. Compared with traditional open surgery, laparoscopic surgery (LS) has been widely used in RC surgery due to its advantages of shorter hospital stays, reduced blood loss, and faster postoperative recovery[6,7]. However, some limitations of LS, such as a two-dimensional field of view, amplification of operative tremors, and poor flexibility, may affect its efficacy in radical surgery[6,8]. These limitations are further amplified in the narrow pelvic cavity. However, robotic surgery (RS) offers a three-dimensional view, a stable camera platform, and flexible operating instruments[9]. The development of RS provides a potential approach that overcomes the limitations of LS. Several studies have compared the efficacy of laparoscopic and robotic APR for RC. However, the benefits of robotic APR remain controversial. Feng et al[10] showed that robotic APR significantly reduced the incidence of postoperative complications, rate of conversion to laparotomy, and length of hospital stay. However, some retrospective studies[11,12] have shown no significant difference in postoperative complication rates between robotic and laparoscopic APR.
Therefore, we conducted a retrospective cohort study to evaluate the effects of RS on postoperative complications, pathological findings, and postoperative recovery in RC patients undergoing APR. Propensity score matching (PSM) was performed to reduce the influence of imbalanced factors between the two groups. In addition, we performed a meta-analysis of all previous studies evaluating the efficacies of robotic and laparoscopic APR for RC surgery and combined the results of this trial.
MATERIALS AND METHODS
Study population
This retrospective study included 133 patients with pathologically confirmed RC who underwent APR via RS or LS at the First Affiliated Hospital of Chongqing Medical University from April 2016 to June 2022. This study was ethically approved by the Institutional Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. All patients provided informed consent. Patients undergoing surgery for local recurrence after rectal resection, with malignant melanoma, younger than 18 years, or undergoing combined resection of other organs were excluded.
Patient demographics [age, sex, body mass index (BMI), the American Society of Anesthesiologists physical status classification (ASA) scores, comorbidity, tumor distance from the anal verge, and neoadjuvant therapy], surgical information (surgical approach, operative time, blood loss, and conversion to open surgery), postoperative outcomes [length of stay, reoperation, complications within 30 d, readmissions, mortality, time to first flatus, first defecation time, lymph nodes harvested, circumferential resection margin (CRM), and cost] were obtained from the electronic medical record system.
Surgical procedure
All laparoscopic and robotic procedures were performed by the same experienced surgeon. Robotic and laparoscopic approaches were used only for abdominal procedures. The perineal portion of the procedure was performed manually by the surgeon. All surgical procedures were performed in accordance with the principle of total mesorectal excision, which included resection of the entire mesorectum to the pelvic floor, ligation of the inferior mesenteric artery at the origin of the inferior mesenteric artery, and lymph node dissection. Perineal resection involved the removal of the internal and external anal sphincters and a part of the levator ani muscle. Extended resection of the levator ani muscle, posterior vaginal wall, and surrounding tissues was performed, if necessary, for tumor invasion. No procedure was taken to fill the pelvic cavity.
Primary and secondary endpoints
The primary endpoint was postoperative complications within 30 postoperative days. The secondary endpoints included operative time, blood loss, time to first flatus and defecation, conversion rate, intensive care rate, histological examination, morbidity, reoperation rate, transfusion rate, and length of hospital stay.
Statistical analysis
Data were presented as frequencies (percentages), means (standard deviation), or medians (interquartile range). Differences in categorical variables between the groups were examined by the Pearson χ2 test. Meanwhile, differences in continuous variables between the two groups were analyzed using the Student's t-test or Mann-Whitney U test, as appropriate. PSM analysis based on patient demographics (male, age, BMI, neoadjuvant therapy, tumor location, and stage) and comorbidities (chronic obstructive pulmonary disease, hypertension, diabetes mellitus, coronary artery disease, and ASA) was performed to reduce potential confounders resulting from differences in baseline characteristics between the groups. The matching ratio was established as 1:1 using the nearest neighbor matching algorithm. Calipers were set to 0.05 times the standard deviation of the logarithm of the estimated propensity score. All statistical analyses were performed with IBM SPSS version 26. A P-value < 0.05 was considered statistically significant.
Meta-analysis
We conducted a meta-analysis of all published cohort studies, case-control studies, and randomized controlled trials (RCTs) following the PRISMA guidelines, comparing RS with LS in APR for RC. The PubMed, Embase, Web of Science, and Cochrane databases were searched from inception until December 7, 2022. Studies were included if they met the following criteria: (1) Patients undergoing APR for RC; (2) intervention with RS; (3) comparison with LS; (4) outcomes included postoperative complications, completeness of resection, operative time, length of hospital stay, mortality, conversion rate, lymph nodes harvested, and blood loss; and (5) cohort studies, case-control studies, or RCTs. The risk of bias in RCTs was assessed independently by two authors (Tang G and Song L) based on the Cochrane risk-of-bias tool. The quality of non-RCTs was assessed based on the Newcastle-Ottawa Scale. Data extracted from each eligible study were as follows: First author, year, country, study design, sample, age, sex, and outcomes. Heterogeneity between studies was assessed using the I² statistic[13]. Mean differences (MD) or odds ratios (OR) across studies were combined using the random effects model[14]. One-study exclusion test was used to examine the impact of each study on the pooled effect size. Analyses were conducted using Review Manager (RevMan) Version 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration 2014; Copenhagen, Denmark). A P-value < 0.05 was considered statistically significant.
RESULTS
Patient characteristics
In total, 133 patients (96 males and 37 females) who underwent APR for RC were included. The median (interquartile range: 25th-75th percentile) age and mean BMI of the patients were 63.0 (55.5-70.0) years and 22.53 ± 2.43 kg/m2, respectively. Robotic APR was performed in 49 patients and laparoscopic APR in 84 patients. There were no significant differences in the ASA grade, sex, age, diabetes mellitus, chronic obstructive pulmonary disease, coronary artery disease, BMI, and tumor stage between the two groups. However, the proportion of patients with hypertension was higher in the RS group than in the LS group (P = 0.011).
Surgical results
After matching, 42 patients were included in each group (Table 1). Operative times were similar between the two groups (P = 0.564), with a median of 245 min for RS and 230 min for LS. The estimated blood loss was significantly lower in the RS group than in the LS group (P = 0.012). No significant differences in the rate of intraoperative blood transfusion were observed between the two groups (P = 0.314). In addition, there was no conversion to open surgery in either group (Table 2).
Table 1.
Baseline characteristics after propensity score matching, n (%)
|
|
Group RS (n = 42)
|
Group LS (n = 42)
|
P value
|
| Age (yr)1 | 63.5 (55-69) | 65 (57.8-72.3) | 0.211 |
| Sex | 1.000 | ||
| Male | 32 (76.2) | 32 (76.2) | |
| Female | 10 (23.8) | 10 (23.8) | |
| BMI2 | 22.5 (2.03) | 22.6 (2.41) | 0.815 |
| COPD | 8 (19) | 8 (19) | 1.000 |
| Hypertension | 11 (26.2) | 9 (21.4) | 0.608 |
| Diabetes mellitus | 2 (4.8) | 4 (9.5) | 0.397 |
| Coronary artery disease | 1 (2.4) | 2 (4.8) | 0.557 |
| ASA Grade | 0.890 | ||
| 1 | 5 (11.9) | 4 (9.5) | |
| 2 | 22 (52.4) | 24 (57.1) | |
| 3 | 15 (35.7) | 14 (33.3) | |
| Neoadjuvant therapy received | 9 (21.4) | 8 (19) | 0.786 |
| Distance between tumor and AV (cm)1 | 3 (2-5) | 3 (2.5-4) | 0.996 |
| Stage | 0.969 | ||
| I | 10 (23.8) | 10 (23.8) | |
| II | 16 (38.1) | 15 (35.7) | |
| III | 16 (38.1) | 17 (40.5) |
Values are median (interquartile range: 25th-75th percentile).
Values are mean (SD).
Values in parentheses are percentages, unless indicated otherwise. ASA: American Society of Anesthesiologists physical status classification; AV: Anal verge; BMI: Body mass index; COPD: Chronic obstructive pulmonary disease; RS: Robotic surgery; LS: Laparoscopic surgery.
Table 2.
Operative outcomes and postoperative complication after propensity score matching, n (%)
|
|
Group RS (n = 42)
|
Group LS (n = 42)
|
P value
|
| Duration of surgery (min)1 | 245 (191.5-295) | 230 (200-286.3) | 0.564 |
| Intraoperative blood loss (ml)1 | 60 (50-100) | 100 (50-200) | 0.012 |
| Transfusion | 1 (2.4) | 0 (0) | 0.314 |
| Days to first flatus1 | 2 (1-2) | 2 (2-3) | 0.023 |
| Days to first defecation1 | 3 (2.8-4.3) | 3 (2.8-4.3) | 0.679 |
| Reoperation | 0 (0) | 1 (2.4) | 0.314 |
| Mortality | 0 (0) | 0 (0) | - |
| Intensive care | 0 (0) | 2 (4.8) | 0.152 |
| Conventional open | 0 (0) | 0 (0) | - |
| Circumferential resection margin positive | 0 (0) | 1 (2.4) | 0.314 |
| Lymph nodes harvested1 | 15 (11-18) | 13 (9-18.3) | 0.309 |
| Perineural invasion | 1 (2.4) | 1 (2.4) | 1.000 |
| Lymphovascular invasion | 2 (4.8) | 2 (4.8) | 1.000 |
| Hospital stay (d)1 | 9 (7.8-13) | 11 (8-18) | 0.044 |
| Postoperative complications | 17 (40.5) | 27 (64.3) | 0.029 |
| Urinary infection | 2 (4.8) | 1 (2.4) | 0.557 |
| Pneumonia | 1 (2.4) | 1 (2.4) | 1.000 |
| Ileus | 3 (7.1) | 3 (7.1) | 1.000 |
| Wound infection | 5 (11.9) | 12 (28.6) | 0.057 |
| Intraabdominal infection | 5 (11.9) | 8 (19) | 0.365 |
| Urinary retention | 1 (2.4) | 2 (4.8) | 0.557 |
| Hospital charge (RMB)1 | 81886.5 (70540.5-109854.2) | 70102.8 (60308.6-109415.4) | 0.040 |
Values are median (interquartile range: 25th-75th percentile).
Values in parentheses are percentages, unless indicated otherwise. RS: Robotic surgery; LS: Laparoscopic surgery.
Postoperative complication rate was significantly lower in the RS group (17/42, 40.5%) than in the LS group (27/42, 64.3%) (P = 0.029). There were no significant differences observed in pneumonia (P = 1.000), urinary infection rate (P = 0.557), ileus rate (P = 1.000), wound infection rate (P = 0.057), abdominal infection rate (P = 0.365), reoperation rate (P = 0.314), urinary retention (P = 0.557), or intensive care rate (P = 0.152) between the two groups, and no deaths were recorded in both groups. There was no significant difference between the two groups in the number of examined lymph nodes (P = 0.309) and CRM positive rate (P = 0.314). Median hospitalization costs were significantly higher in the RS group (81886.5 RMB) than in the LS group (70102.8 RMB; P = 0.040).
Regarding intestinal function recovery, the time to first flatus in the robotic group (P = 0.023) was significantly shorter than that in the laparoscopic group. However, there was no significant difference in the time to first defecation between the two groups (P = 0.679). In addition, the median postoperative hospital stay was significantly shorter in the RS group (9.0 d) than in the LS group (11.0 d; P = 0.044).
Meta-analysis
Our literature search yielded 810 potential records, of which 11 published articles were completely reviewed. In addition to our study, six trials[10-12,15-17] published between 2015 and 2022 were included. Details of the seven eligible trials are summarized in Table 3. The risk of bias was low in all seven studies included in the review.
Table 3.
Characteristics of trials included in the meta-analysis
|
Ref.
|
Country
|
Study design
|
Sample
|
Age
|
Gender (M/ F)
|
Outcomes
|
NOS
|
| Moghadamyeghaneh et al[15], 2015 | United States | Retrospective cohort study | R: 872; L: 4737 | R: 64; L: 62 | R: 556/316; L: 2844/1893 | Hospital stay, postoperative complications, mortality | 7 |
| Kamali et al[16], 2017 | United Kingdom | Retrospective case-control study | R: 11; L: 11 | R: 71; L: 57 | R: 7/4; L: 9/2 | Postoperative complications, mortality, CRM, operating time, hospital stay, lymph nodes harvested, conversion rate | 8 |
| Gavrila et al[17], 2021 | Romania | Retrospective case-control study | R: 46; L: 63 | R: 62; L: 62 | R: 34/12; L: 32/31 | Postoperative complications, mortality, operating time, blood loss, hospital stay, conversion rate, reoperation rate | 8 |
| Kasai et al[11], 2022 | Japan | Retrospective cohort study | R: 33; L: 20 | R: 74; L: 78 | R: 20/13; L: 16/4 | Postoperative complications, CRM, operating time, blood loss, hospital stay, conversion rate, lymph nodes harvested | 8 |
| Feng et al[10], 2022 | China | Randomized controlled trial | R: 174; L: 173 | R: 58; L: 60 | R: 108/66; L: 113/60 | Postoperative complications, mortality, CRM, operating time, blood loss, hospital stay, conversion rate, reoperation rate, lymph nodes harvested | - |
| Gorgun et al[12], 2022 | United States | Retrospective PSM | R: 34; L: 34 | R: 66; L: 66 | R: 25/9; L: 25/9 | Postoperative complications, CRM, operating time, blood loss, hospital stay, conversion rate, reoperation rate, lymph nodes harvested | 9 |
| Current study, 2022 | China | Retrospective PSM | R: 34; L: 34 | R: 34; L: 34 | R: 34; L: 34 | Lymph nodes harvested, postoperative complications, mortality, CRM, operating time, blood loss, hospital stay, conversion rate, reoperation rate | 9 |
CRM: Circumferential resection margin; F: Female; L: Laparoscopic abdominoperineal resection; M: Male; NOS: Newcastle-Ottawa Scale; PSM: Propensity score matching; R: Robotic abdominoperineal resection.
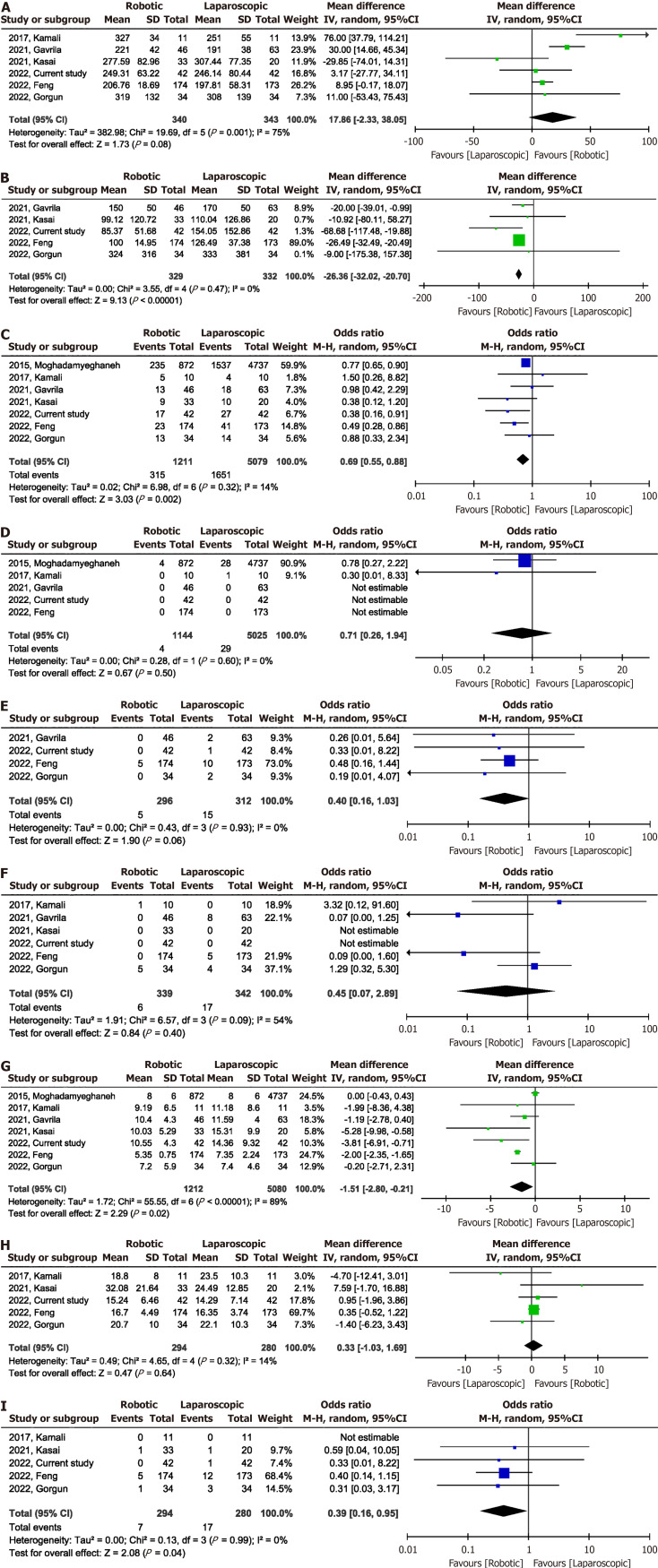
Meta-analysis of the six studies[10-12,16,17] showed no significant difference in operative time [MD = 17.86 min; 95%CI: -2.33 to 38.05; P = 0.08, with high heterogeneity (I2 = 75%)] (Figure 1A and Table 4). Intraoperative blood loss was significantly lower in the RS group than in the LS group (MD -26.36 mL, 95%CI: -32.02 to -20.70; I2 = 0%, P = 0.47) (Figure 1B). A total of 6290 participants in the seven studies[10-12,15-17] had postoperative complications. The incidence of postoperative complications was lower in the RS group than in the LS group (OR 0.69, 95%CI: 0.55-0.88; I2 = 14%, P = 0.32) (Figure 1C). There was no significant difference (OR, 0.71; 95%CI: 0.26-1.94; P = 0.50) in the postoperative mortality between the RS and LS groups, with low heterogeneity between studies (I2 = 0%, P = 0.60) (Figure 1D). Data on reoperation rates were reported in four studies[10,12,17]. The RS and LS groups were comparable in terms of reoperation rate (OR, 0.40; 95%CI: 0.16-1.03; P = 0.06; I2 = 0%) (Figure 1E). Furthermore, no significant differences were observed between RS and LS in terms of conversion to open surgery (OR, 0.45; 95%CI: 0.07-2.89; P = 0.40; I2 = 54%), estimated at 1.8% for RS and 5.0% for LS (Figure 1F). The overall effect of the seven studies[10-12,15-17] reporting the length of stay showed that RS was associated with reduced length of hospital stay (MD -1.51 d; 95%CI: -2.80 to -0.21), with significant heterogeneity (I2 = 89%, P < 0.00001) between studies (Figure 1G). Five studies[10-12,16] described the number of lymph nodes harvested, and there was no significant difference in the number of lymph nodes harvested between the RS and LS groups, with low heterogeneity (MD, 0.33; 95%CI: -1.03 to 1.69; P = 0.64; I2 = 14%) (Figure 1H). Data on CRM positive rates were reported in five studies[10-12,16]. Surgery with the robotic-assisted technique for APR reduced the CRM positive rate (OR, 0.39; 95%CI: 0.16-0.95; P = 0.04; I2 = 0%) (Figure 1I).
Figure 1.
Forest plots. A: Forest plots of the operation time for robotic vs laparoscopic abdominoperineal resection; B: Forest plots of the intraoperative blood loss for robotic vs laparoscopic abdominoperineal resection; C: Forest plots of postoperative complications for robotic vs laparoscopic abdominoperineal resection; D: Forest plots of postoperative mortality for robotic vs laparoscopic abdominoperineal resection; E: Forest plots of the reoperation rates for robotic vs laparoscopic abdominoperineal resection; F: Forest plots of the rate of conversion to open surgery for robotic vs laparoscopic abdominoperineal resection; G: Forest plots of the length of stay for robotic vs laparoscopic abdominoperineal resection; H: Forest plots of the number of lymph nodes harvested for robotic vs laparoscopic abdominoperineal resection; I: Forest plots of the circumferential resection margin positive rates for robotic vs laparoscopic abdominoperineal resection.
Table 4.
Summary of results from all outcomes
|
Indicators
|
No. of studies
|
Events for RS
|
Events for LS
|
Effect size
|
95%CI
|
| Operative time | 6 | - | - | 17.86 min | -2.33, 38.05 |
| Intraoperative blood loss | 5 | - | - | -26.36 mL | -32.02, -20.70 |
| Postoperative complications | 7 | 315/1211 | 1651/5079 | 0.69 | 0.55, 0.88 |
| Postoperative mortality | 5 | 4/1144 | 29/5025 | 0.71 | 0.26, 1.94 |
| Reoperation | 4 | 5/296 | 15/312 | 0.40 | 0.16, 1.03 |
| Conversion to open surgery | 6 | 6/339 | 17/342 | 0.45 | 0.07, 2.89 |
| The length of stay | 7 | - | - | -1.51 d | -2.80, -0.21 |
| Lymph nodes harvested | 5 | - | - | 0.33 | -1.03, 1.69 |
| Circumferential resection margin positive | 5 | 7/294 | 17/280 | 0.39 | 0.16, 0.95 |
RS: Robotic surgery; LS: Laparoscopic surgery.
The results of the sensitivity analysis showed that the total effect size of intraoperative blood loss, postoperative complications, postoperative mortality, reoperation rate, conversion to open surgery, and number of lymph nodes harvested was not affected by the elimination of any one study. However, the total effect size for operative time changed (MD, 24.05 min; 95%CI: 3.71-44.40; I2 = 0%, P = 0.47) when the study by Kasai et al[11] was excluded. Sensitivity analysis indicated that studies by Gorgun et al[12] (OR, 0.41; 95%CI: 0.16-1.06; I2 = 0%, P = 0.96) and Feng et al[10] (OR, 0.38; 95%CI: 0.08-1.84; I2 = 0%, P = 0.94) and the present study (OR, 0.40; 95%CI: 0.16-1.00; I2 = 0%, P = 0.94) prominently affected the total effect size of the CRM positive rate. The total effect size of the length of hospital stay was changed by the exclusion of the study by Kasai et al[11] (MD, -1.27 d; 95%CI: -2.59 to 0.05), the present study (MD, -1.24 d; 95%CI: -2.60 to 0.12), and the study by Feng et al[10] (MD, -1.28 d; 95%CI: -2.68 to 0.12).
DISCUSSION
With advancements in technology, LS is gradually becoming the preferred technique for colorectal surgery. LS is safe and effective in the short and long term[9]. However, laparoscopic RC surgery has some inherent limitations, especially in patients with low RC[18]. In addition, neoadjuvant use can lead to pelvic tissue fibrosis, which increases the difficulty of surgery and affects the efficacy of LS[9]. RS is another surgical technique that is under development. Compared with LS, RS has several major advantages, including a wider surgical field, more flexible surgical instruments, and less fatigue for doctors[19]. In addition, LS is difficult to perform on the pelvic floor and requires a long learning curve, whereas RS has a shorter learning period, making this technique easier for younger doctors to learn[20,21]. A recently published meta-analysis[21] showed that robotic rectal surgery had similar long-term outcomes as LS, with shorter operative time, lower incidence of postoperative complications, shorter hospital stays, and lower conversion to open surgery rates. However, there are few related studies on RS for APR, and the efficacy is still controversial. Postoperative complications of minimally invasive surgery for RC are as high as 27%[3]. In addition, the incidence of postoperative complications was higher with APR than with LAR[22]. The overall complication rate after APR in our study was 31%. Our retrospective study and meta-analysis showed that RS was effective in reducing the overall incidence of complications after APR. This result is consistent with that of a previous RCT involving patients undergoing LAR and APR procedures[23]. Postoperative complications not only increase the cost and length of hospital stay but also negatively affect long-term prognosis[24,25]. Gamboa et al[26] found that major complications after proctectomy were associated with shortened overall and recurrence-free survival. Thus, our findings have significant clinical implications, as we provide evidence supporting the benefit of RS in reducing complications after APR.
In addition, the advantages of the RS could theoretically bring benefits in terms of conversion to open surgery. A meta-analysis of 42 studies[21] showed that RS reduced the conversion rate. A recent large RCT[23] showed that robotics was associated with a lower conversion rate. However, in our study, there was no difference in the rate of conversion to open surgery between the RS and LS groups. After meta-analysis, conversion rates between RS and LS groups remained comparable. However, our analysis included a limited number of studies; more high-quality studies are needed to evaluate the effect of robotics on conversion to open surgery in APR. In addition, our meta-analysis showed that RS did not reduce the reoperation rate.
In RC surgery, surgeons focus on the quality of tumor resection. The number of harvested lymph nodes is related to the accuracy of tumor staging and oncologic radicality. In addition, it affects the patient's oncologic prognosis[27]. Being CRM positive, defined as having a minimum distance between the tumor and the CRM of 1 mm or less[28], is associated with tumor recurrence and shorter survival[18]. Studies have reported that being CRM positive leads to a 1- to 5-fold increased risk of local recurrence and a 1- to 4-fold increased risk of distant metastasis[23,29-32]. In traditional LS, surgical instruments need to enter the pelvic cavity in a nearly vertical direction, and their operation in the horizontal direction is limited. In addition, the narrow space in the pelvic cavity can lead to interference between instruments. Lower rectal surgery requires the cooperation of experienced assistants[23]. These factors may affect the quality of LS. RS has better three-dimensional vision and more flexible tools. In addition, the operating arm of the robot can be controlled by the surgeon, which can replace the role of the assistant in LS. These factors allow the robot to perform precise surgical manipulations in a narrow space and improve the quality of tumor specimens[21,23]. Although there was no benefit of RS in terms of the number of lymph nodes harvested, our meta-analysis showed that RS significantly reduced the CRM positive rate. However, the sensitivity analysis showed that the total effect of the CRM positive rate was not robust. More studies are needed to explore the effect of RS on the quality of APR in the future.
Minimally invasive surgery is characterized by a rapid recovery of bowel function and a short hospital stay[19]. Postoperative recovery of gastrointestinal function is an important part of enhanced recovery after gastrointestinal tumor surgery, which has important clinical significance. The time to first flatus and time to first defecation after surgery are key indicators of gastrointestinal dysfunction[33]. Our study showed that although RS, compared to LS, did not shorten the time to first defecation, it reduced the time to first flatus. This is similar to the results of a recent meta-analysis[21] in which the time to first flatus after RC surgery was significantly shorter in the RS group (2.5 ± 1.4 d) than in the LS group (2.9 ± 2.0 d). In addition, our retrospective study and meta-analysis observed a significantly shorter hospital stay in the RS group than that in the LS group. This may be related to the faster recovery of intestinal function and fewer incidences of complications.
Regarding safety, some researchers have expressed concerns that RS will lead to longer operation times[3]. However, our retrospective study and meta-analysis suggest that RS does not lead to longer operation times. This is similar to the results of several previous studies[23,34,35]. In addition, we found that intraoperative blood loss was significantly lower in the RS group than that in the LS group. This may be due to the technical advantages of the robotic system providing a better surgical field of view, clearer anatomy, and easier suture manipulation, helping to prevent more bleeding[15,18].
A significant limitation of RS is its high cost[23]. Moghadamyeghaneh et al[15] used the nationwide inpatient sample database from 2009 to 2012 and found that the average total hospitalization cost of robotic APR was 37% higher than that of laparoscopy. Similar to previous studies, in the present study, we found a 17% increase in median hospitalization costs in the RS group compared with that in the LS group. Recently, Gorgun et al[12] reported an increase in direct costs of robotic APR compared with those of laparoscopic APR (26% increase in mean cost and 43% increase in median cost); however, the difference was not significant. The increase in hospitalization costs is an important factor hindering the routine application of RS[12]. Increased complication rates and longer hospital stays are associated with increased treatment costs[11]. Compared with LS, the lower complications and shorter hospital stays observed in the robotic group may be beneficial in reducing the high costs of RS treatment. Furthermore, as the use of RS becomes more widespread and the volume of such procedures increases, the cost of robotic devices will likely decrease over time. In the future, conducting further research to explore the cost-effectiveness of RS compared to that of LS will be important.
Our study had some limitations. First, our study was retrospective and may have been subject to some confounding factors. Therefore, we performed a PSM analysis, and the post-PSM RS and LS groups had similar underlying characteristics. Second, it was difficult to compare the effects of the two surgical techniques on long-term survival because the postoperative follow-up time was too short. However, given the concern about the impact of postoperative complications on survival and the lower incidence of postoperative complications in the RS group compared with that in the LS group, it is necessary to evaluate the long-term efficacy of the two surgical methods. Finally, this study was a single-center study, and all operations were performed by the same surgeon, which was not representative of the skill level of most colorectal surgeons. Therefore, we conducted a meta-analysis of data from other previous studies to further confirm the reliability of the results. To the best of our knowledge, this is the first meta-analysis comparing the short-term efficacy of robotic vs laparoscopic APR.
CONCLUSION
RS is a safe and effective treatment for APR in RC. Although RS is more expensive than LS, RS offers better short-term outcomes including fewer complications, fewer positive CRMs, less blood loss, and a faster postoperative recovery. More high-quality prospective studies are warranted to confirm the benefits of RS in APR.
ACKNOWLEDGEMENTS
We would like to express our gratitude to all those who contributed to the study.
Footnotes
Institutional review board statement: The study was reviewed and approved by the First Affiliated Hospital of Chongqing Medical University Institutional Review Board (Approval No. 2022-K533).
Informed consent statement: Considering that the research was retrospective, the need for patients’ informed written consent was waived.
Conflict-of-interest statement: All the authors have no conflict of interest related to the manuscript.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade A
Creativity or Innovation: Grade B
Scientific Significance: Grade A
P-Reviewer: Vyshka G, Albania S-Editor: Yan JP L-Editor: A P-Editor: Xu ZH
Contributor Information
Li Song, Department of Gastrointestinal Surgery, Chengdu Fifth People's Hospital, Chengdu 610000, Sichuan Province, China.
Wen-Qiong Xu, Department of Nephrology, Chengdu Fifth People's Hospital, Chengdu 610000, Sichuan Province, China.
Zheng-Qiang Wei, Department of Gastrointestinal Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400000, China.
Gang Tang, Division of Biliary Tract Surgery, Department of General Surgery, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China. gangtang2017@163.com.
Data sharing statement
The original anonymous dataset is available on request from the corresponding author at gangtang2017@163.com.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Su WC, Huang CW, Ma CJ, Chen PJ, Tsai HL, Chang TK, Chen YC, Li CC, Yeh YS, Wang JY. Feasibility of robot-assisted surgery in elderly patients with rectal cancer. J Minim Access Surg. 2021;17:165–174. doi: 10.4103/jmas.JMAS_154_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, Jimenez-Rodriguez RM, Gurrado A, Strippoli GFM. Robotic Versus Laparoscopic Minimally Invasive Surgery for Rectal Cancer: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann Surg. 2018;267:1034–1046. doi: 10.1097/SLA.0000000000002523. [DOI] [PubMed] [Google Scholar]
- 4.Miles WE. A method of performing abdomino-perineal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon (1908) CA Cancer J Clin. 1971;21:361–364. doi: 10.3322/canjclin.21.6.361. [DOI] [PubMed] [Google Scholar]
- 5.Zhang X, Wu Q, Hu T, Gu C, Bi L, Wang Z. Laparoscopic Versus Conventional Open Abdominoperineal Resection for Rectal Cancer: An Updated Systematic Review and Meta-Analysis. J Laparoendosc Adv Surg Tech A. 2018;28:526–539. doi: 10.1089/lap.2017.0593. [DOI] [PubMed] [Google Scholar]
- 6.Tang B, Lei X, Ai J, Huang Z, Shi J, Li T. Comparison of robotic and laparoscopic rectal cancer surgery: a meta-analysis of randomized controlled trials. World J Surg Oncol. 2021;19:38. doi: 10.1186/s12957-021-02128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Liu Y, Han G, Yi B, Zhu S. The severity of postoperative complications after robotic versus laparoscopic surgery for rectal cancer: A systematic review, meta-analysis and meta-regression. PLoS One. 2020;15:e0239909. doi: 10.1371/journal.pone.0239909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu G, Zhang S, Zhang Y, Fu X, Liu X. Robotic Surgery in Rectal Cancer: Potential, Challenges, and Opportunities. Curr Treat Options Oncol. 2022;23:961–979. doi: 10.1007/s11864-022-00984-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qiu H, Yu D, Ye S, Shan R, Ai J, Shi J. Long-term oncological outcomes in robotic versus laparoscopic approach for rectal cancer: A systematic review and meta-analysis. Int J Surg. 2020;80:225–230. doi: 10.1016/j.ijsu.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Feng Q, Tang W, Zhang Z, Wei Y, Ren L, Chang W, Zhu D, Liang F, He G, Xu J. Robotic versus laparoscopic abdominoperineal resections for low rectal cancer: A single-center randomized controlled trial. J Surg Oncol. 2022;126:1481–1493. doi: 10.1002/jso.27076. [DOI] [PubMed] [Google Scholar]
- 11.Kasai S, Kagawa H, Shiomi A, Hino H, Manabe S, Yamaoka Y, Kato S, Hanaoka M, Kinugasa Y. Advantages of robotic abdominoperineal resection compared with laparoscopic surgery: a single-center retrospective study. Surg Today. 2022;52:643–651. doi: 10.1007/s00595-021-02359-6. [DOI] [PubMed] [Google Scholar]
- 12.Gorgun E, Cengiz TB, Ozgur I, Dionigi B, Kalady MF, Steele SR. Outcomes and Cost Analysis of Robotic Versus Laparoscopic Abdominoperineal Resection for Rectal Cancer: A Case-Matched Study. Dis Colon Rectum. 2022;65:1279–1286. doi: 10.1097/DCR.0000000000002394. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration 2011. Available from: https://onlinelibrary.wiley.com/doi/book/10.1002/9780470712184 .
- 15.Moghadamyeghaneh Z, Phelan M, Smith BR, Stamos MJ. Outcomes of Open, Laparoscopic, and Robotic Abdominoperineal Resections in Patients With Rectal Cancer. Dis Colon Rectum. 2015;58:1123–1129. doi: 10.1097/DCR.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 16.Kamali D, Reddy A, Imam S, Omar K, Jha A, Jha M. Short-term surgical outcomes and patient quality of life between robotic and laparoscopic extralevator abdominoperineal excision for adenocarcinoma of the rectum. Ann R Coll Surg Engl. 2017;99:607–613. doi: 10.1308/rcsann.2017.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gavrila D, Bitere O, Droc G, Lacatus M, Minciuna C, Ilie V, Trandafir B, Herlea V, Tudor S, Vasilescu C. Abdominoperineal Resection for Rectal Cancer: Open, Laparoscopic or Robotic Approach. Chirurgia (Bucur) 2021;116:573–582. doi: 10.21614/chirurgia.116.5.573. [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Cao G, Mao W, Lao W, He C. Robot-assisted versus laparoscopic surgery for rectal cancer: A systematic review and meta-analysis. J Cancer Res Ther. 2020;16:979–989. doi: 10.4103/jcrt.JCRT_533_18. [DOI] [PubMed] [Google Scholar]
- 19.Cheong C, Kim NK. Minimally Invasive Surgery for Rectal Cancer: Current Status and Future Perspectives. Indian J Surg Oncol. 2017;8:591–599. doi: 10.1007/s13193-017-0624-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Araujo SE, Seid VE, Klajner S. Robotic surgery for rectal cancer: current immediate clinical and oncological outcomes. World J Gastroenterol. 2014;20:14359–14370. doi: 10.3748/wjg.v20.i39.14359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Safiejko K, Tarkowski R, Koselak M, Juchimiuk M, Tarasik A, Pruc M, Smereka J, Szarpak L. Robotic-Assisted vs. Standard Laparoscopic Surgery for Rectal Cancer Resection: A Systematic Review and Meta-Analysis of 19,731 Patients. Cancers (Basel) 2021;14 doi: 10.3390/cancers14010180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang XT, Li DG, Li L, Kong FB, Pang LM, Mai W. Meta-analysis of oncological outcome after abdominoperineal resection or low anterior resection for lower rectal cancer. Pathol Oncol Res. 2015;21:19–27. doi: 10.1007/s12253-014-9863-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng Q, Yuan W, Li T, Tang B, Jia B, Zhou Y, Zhang W, Zhao R, Zhang C, Cheng L, Zhang X, Liang F, He G, Wei Y, Xu J REAL Study Group. Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): short-term outcomes of a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol. 2022;7:991–1004. doi: 10.1016/S2468-1253(22)00248-5. [DOI] [PubMed] [Google Scholar]
- 24.Tang G, Pi F, Zhang DH, Qiu YH, Wei ZQ. Novel surgical procedure for preventing anastomotic leakage following colorectal cancer surgery: A propensity score matching study. Front Oncol. 2022;12:1023529. doi: 10.3389/fonc.2022.1023529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Kooten RT, Elske van den Akker-Marle M, Putter H, Meershoek-Klein Kranenbarg E, van de Velde CJH, Wouters MWJM, Tollenaar RAEM, Peeters KCMJ. The Impact of Postoperative Complications on Short- and Long-Term Health-Related Quality of Life After Total Mesorectal Excision for Rectal Cancer. Clin Colorectal Cancer. 2022;21:325–338. doi: 10.1016/j.clcc.2022.07.004. [DOI] [PubMed] [Google Scholar]
- 26.Gamboa AC, Lee RM, Turgeon MK, Varlamos C, Regenbogen SE, Hrebinko KA, Holder-Murray J, Wiseman JT, Ejaz A, Feng MP, Hawkins AT, Bauer P, Silviera M, Maithel SK, Balch GC. Impact of Postoperative Complications on Oncologic Outcomes After Rectal Cancer Surgery: An Analysis of the US Rectal Cancer Consortium. Ann Surg Oncol. 2021;28:1712–1721. doi: 10.1245/s10434-020-08976-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tonini V, Birindelli A, Bianchini S, Cervellera M, Bacchi Reggiani ML, Wheeler J, Di Saverio S. Factors affecting the number of lymph nodes retrieved after colo-rectal cancer surgery: A prospective single-centre study. Surgeon. 2020;18:31–36. doi: 10.1016/j.surge.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Baik SH, Kim NK, Lee YC, Kim H, Lee KY, Sohn SK, Cho CH. Prognostic significance of circumferential resection margin following total mesorectal excision and adjuvant chemoradiotherapy in patients with rectal cancer. Ann Surg Oncol. 2007;14:462–469. doi: 10.1245/s10434-006-9171-0. [DOI] [PubMed] [Google Scholar]
- 29.Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008;26:303–312. doi: 10.1200/JCO.2007.12.7027. [DOI] [PubMed] [Google Scholar]
- 30.Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, Abbott CR, Scott N, Finan PJ, Johnston D, Quirke P. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg. 2002;235:449–457. doi: 10.1097/00000658-200204000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA, Peters WR Jr, Maun DC, Chang GJ, Herline A, Fichera A, Mutch MG, Wexner SD, Whiteford MH, Marks J, Birnbaum E, Margolin DA, Larson DW, Marcello PW, Posner MC, Read TE, Monson JRT, Wren SM, Pisters PWT, Nelson H. Disease-free Survival and Local Recurrence for Laparoscopic Resection Compared With Open Resection of Stage II to III Rectal Cancer: Follow-up Results of the ACOSOG Z6051 Randomized Controlled Trial. Ann Surg. 2019;269:589–595. doi: 10.1097/SLA.0000000000003002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Wilson K, Hague W, Simes J Australasian Gastro-Intestinal Trials Group (AGITG) ALaCaRT investigators. Disease-free Survival and Local Recurrence After Laparoscopic-assisted Resection or Open Resection for Rectal Cancer: The Australasian Laparoscopic Cancer of the Rectum Randomized Clinical Trial. Ann Surg. 2019;269:596–602. doi: 10.1097/SLA.0000000000003021. [DOI] [PubMed] [Google Scholar]
- 33.Tang G, Huang W, Tao J, Wei Z. Prophylactic effects of probiotics or synbiotics on postoperative ileus after gastrointestinal cancer surgery: A meta-analysis of randomized controlled trials. PLoS One. 2022;17:e0264759. doi: 10.1371/journal.pone.0264759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baik SH, Ko YT, Kang CM, Lee WJ, Kim NK, Sohn SK, Chi HS, Cho CH. Robotic tumor-specific mesorectal excision of rectal cancer: short-term outcome of a pilot randomized trial. Surg Endosc. 2008;22:1601–1608. doi: 10.1007/s00464-008-9752-z. [DOI] [PubMed] [Google Scholar]
- 35.Tang B, Gao GM, Zou Z, Liu DN, Tang C, Jiang QG, Lei X, Li TY. [Efficacy comparison between robot-assisted and laparoscopic surgery for mid-low rectal cancer: a prospective randomized controlled trial] Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23:377–383. doi: 10.3760/cma.j.cn.441530-20190401-00135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original anonymous dataset is available on request from the corresponding author at gangtang2017@163.com.