Abstract
Background Cats are the most popular pet in the United States and much of Northern Europe. Although 78% of owners consider their cats to be family members, many cats, particularly seniors, do not receive appropriate preventive care.1–3 One of the main obstacles to owner compliance is the lack of a clear recommendation by the veterinary team. 4 Guidelines can help veterinarians to minimize this obstacle, strengthen the human-pet-veterinary bond, and improve the quality of life of cats.
Goals The goals of this article are to assist veterinarians to:
Deliver consistent high-quality care to senior cats.
Promote longevity and improve the quality of life of senior cats by: recognizing and controlling health risk factors; facilitating and promoting early detection of disease; improving or maintaining residual organ function; and delaying the progression of common conditions.
Define aspects of screening, diagnosis, treatment and anesthesia of senior cats.
Aging and the older cat: what is senior?
There is no specific age at which a cat becomes ‘senior’. Individual animals and body systems age at different rates, but one convenient way to view older cats is to classify them as ‘mature’ or ‘middle-aged’ (7–10 years), ‘senior’ (11–14 years) and ‘geriatric’ (15+ years). 5 This helps to focus on the varying disease risks of the different groups (eg, obesity in the mature group, cachexia in the geriatric group). In this article, as elsewhere, the word ‘senior’ is used as a broad category for all older cats, unless otherwise noted.
With good care, many cats live into their late teens, some into their twenties; and the percentage of older cats is increasing.6,7 The inevitable biological changes associated with aging result in a progressive reduction in the ability to cope with physiologic, immunologic and environmental stresses. Along with ‘normal’ aging, the incidence of certain diseases gradually increases.
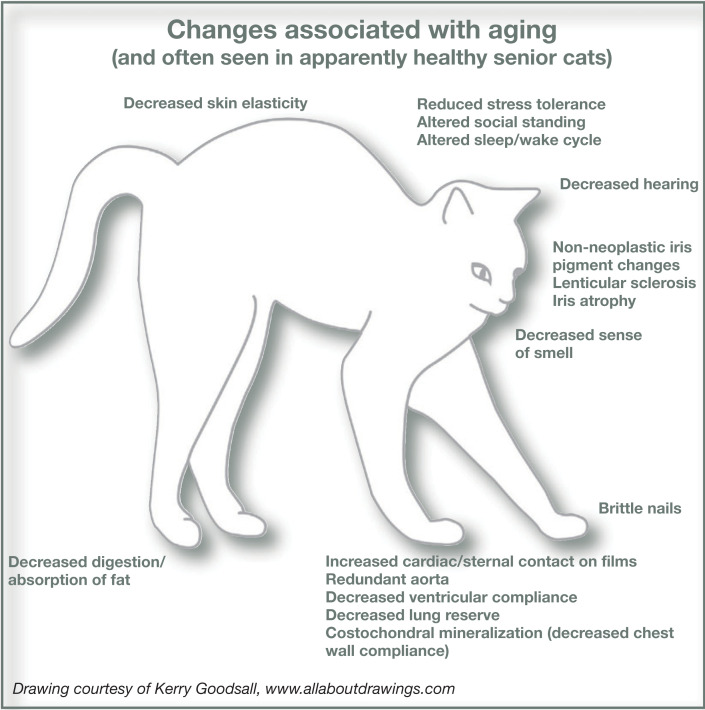
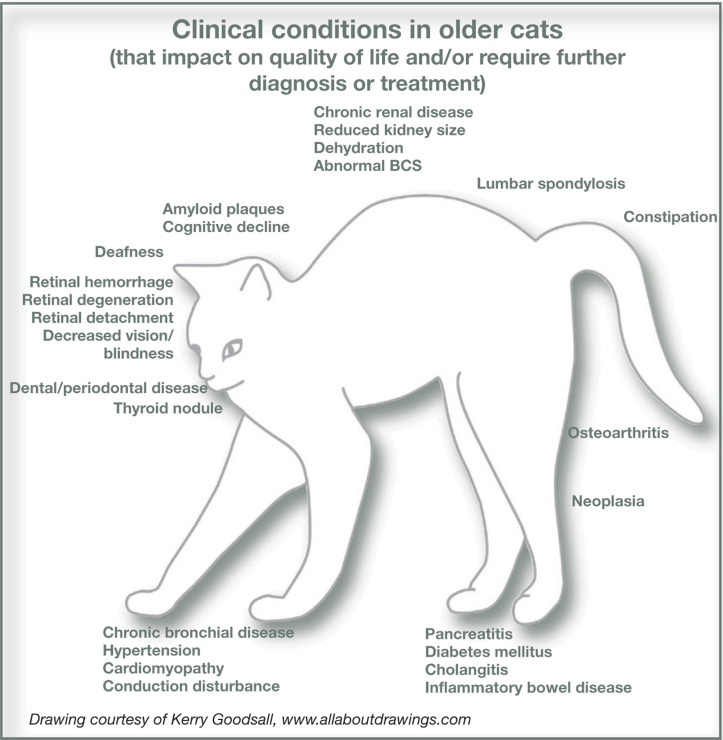
Typical changes associated with aging are shown diagrammatically on page 764. There is no clear line between ‘typical’ changes and disease. For example, many older cats have radiographic evidence of osteoarthritis (OA), and it is difficult to determine when normal aging of the joints actually becomes a pathological process; cats with radiographic evidence of OA may or may not have a clinically evident problem.8,9 For the purposes of these guidelines, we have included in the ‘typical’ changes diagram those changes that are not surprising or that one might even expect to find as common aging changes that would not necessarily result in clinical intervention.
The senior cat wellness visit
A comprehensive history helps raise the index of suspicion for early disease by uncovering relevant signs or behavior changes. Initially, open-ended questions should be asked so that the full range of client concerns is understood.10,11 Examples of open-ended questions are:
How has Max been doing since his last visit?'
What behavior changes have you noticed in the last few weeks?'
‘What else?’
These guidelines were revised in December 2008. Any questions or information requests concerning them should be addressed to the AAFP, 1-800-874-0498, or info@catvets.com
Open-ended questions can then be followed by more specific questions to ask about:
-
Changes in the cat's usual behaviors and routines. 12
For example:
— Interactions with people or other pets;
— Grooming;
— Activity (ie, sleeping patterns, jumping, wandering, reaction to being handled, and ability to navigate to preferred places);
— Vocalization;
— Litter box habits.
Eating and drinking (amount and behavior); vomiting or signs of nausea.
Stool quality (number, volume, consistency, odor, color).
Hearing or vision loss (decreased responsiveness, increased vocalization).
Current diet, medications and supplements. The physical examination allows for detection of problems that may not be obvious to owners or uncovered with laboratory testing. When performing the physical exam, particular attention should be paid to:
Observation of the cat from a distance to assess breathing patterns, gait, stance, strength, coordination, vision.
Weight and body condition score (BCS) comparisons with previous visits.
Skin and hair coat quality.
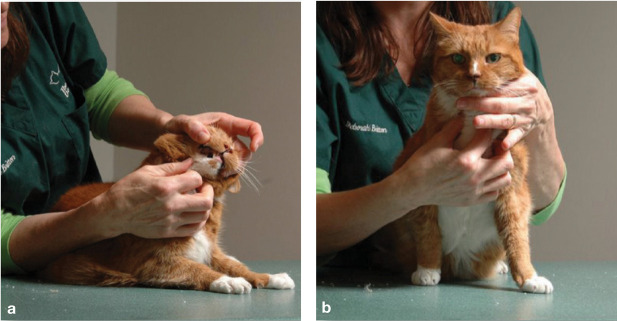
Oral cavity, including gingiva, pharynx, dentition 13 and sublingual area (Fig 1).
Retinal exam; vascular changes or ‘cotton wool spots’ as early warning of hypertension or retinal detachment.
Thyroid gland palpation (Fig 1).
Heart rate, rhythm, murmur.
Abdominal palpation; pain, masses or thickened bowel, kidney and bladder size and shape.
Joint thickening; muscle atrophy.
Changes in parameters from prior exams (eg, reduced body temperature; changed weight/BCS or heart rate).
FIG 1.
Oral cavity examination (a) and thyroid palpation (b) are essential components of a senior check. Courtesy of Deb Givin
Examination frequency in senior cats
The frequency of examinations should increase as cats age. Although there is controversy regarding the frequency of exams in younger cats, 14 panelists agree that apparently healthy senior cats should be examined every 6 months. Examining these cats at 6-month intervals is desirable because:
Many disease conditions begin to develop in cats in middle age.
Health changes occur quickly; cats age faster than humans.
Weight gain or loss can be detected and addressed earlier.
Cats may appear well despite underlying disease, compensating until they can no longer do so, then presenting as acutely ill.
Owners may not recognize the existence or importance of subtle changes.
Early detection of disease often results in easier disease management and better quality of life; it is less costly and more successful than crisis management.
Body condition score scales.
Both nine-point and five-point BCS scales are available for use:
www.purina.org/cats/health/BodyCondition.aspx
www.cvm.tamu.edu/clinicalnutrition/bcscat.shtml
The frequency of behavior problems increases with age. One study found 28% of pet cats aged 11–14 years develop at least one behavior problem, increasing to >50% for cats 15+ years of age. 15
More frequent owner contact provides opportunity for concerns to be discussed.
Examination and laboratory summary sheets allow for a quick review of trends over time. Once evidence of an age-related disease process is discovered, a more frequent monitoring schedule may be needed.
The minimum database
Regular examinations and collection of the minimum database (MDB) can help detect preclinical disease. Consider performing the recommended MDB (as indicated in Table 1) at least annually, starting at age 7–10, with the frequency increasing as cats age. Specific recommendations about age and frequency of testing depend on many factors.16,17
TABLE 1.
The minimum database
Clearly, there is high value to an individual cat to finding early disease, even when many tests yield normal results. However, routine laboratory testing of otherwise apparently normal animals increases the statistical likelihood of revealing test results that are outside of the normal range but are not clinically significant. Interpretation of these values and decisions for further work-up requires clinical judgment in the context of the specific patient. Additional work-ups are not always innocuous.
When in doubt, re-evaluate the patient to establish persistence and/or progression of the abnormality. Trends in the MDB can be significant, allowing for detection of disease earlier than interpretation of a single sample. For example, progressive increases in serum creatinine concentration over several months (even within the normal range) may be significant.
The incidence of many diseases increases as cats age. More robust data about disease incidence by age would assist practitioners in determining the value and desired frequency of testing, but such data is lacking. Veterinarians must rely on their clinical judgment and individual client discussions based on each unique cat. Regardless of the cat's age, more frequent or expansive diagnostic evaluation is indicated if:
Any abnormalities are noted in the history or physical exam, even if the MDB appears normal.
Any disease is suspected or revealed at the regular veterinary visits.
Trends or changes in the history or physical exam become apparent.
Interpretation of certain parameters is complex in senior cats. Indications for and debates about blood pressure measurement and thyroid testing are discussed later in this article.
Interpretation of the urinalysis in senior cats
Interpretation of the urinalysis, particularly the specific gravity and protein, is of particular importance in senior cats. (www.iris-kidney.com/education/en/education03.shtml).
Cystocentesis is recommended for the most accurate results.
Although it is rare, hypertension alone may induce polyuria ('pressure diuresis'), so the presence of low urine specific gravity in a patient with hypertension is not specific for kidney disease. 18
Dipstick protein measurement is inaccurate; both false negative and false positive results are possible at any specific gravity. The microalbuminuria test yields more reliable results. This test or urine protein/creatinine (UPC) ratio may be indicated: (1) for confirmation of proteinuria when the dipstick is positive; or (2) when the dipstick is negative and the cat has a disease known to promote proteinuria (eg, hypertension or chronic kidney disease (CKD).19,20
Early detection of disease often results in easier disease management and better quality of life; it is less costly and more successful than crisis management.
Proteinuria may be a sign of CKD. However, if urinary tract infection or gross hematuria is present, then reassess after resolving those problems. If proteinuria persists, measure the UPC ratio to determine if it is significant (UPC >0.4). Significant and untreated proteinuria is a poor prognostic indicator for cats with hypertension and CKD.21–25
If the urine specific gravity measurement is <1.035, repeat the measurement on a subsequent sample to evaluate persistence.
-
Bacterial infection can be present even in the absence of an inflammatory sediment. Urine culture and sensitivity is indicated under the following conditions:
Routine wellness care
Routine wellness care for older cats starts with the exam and the basic care given to cats of all ages, including parasite prevention, dental care, weight management, vaccination, and knowledge of retroviral status. 13 '28–30 Educate clients about ways they can improve comfort and manage their cats' health care, ensuring the five key resources are available (see right). Examples include providing attention, grooming, and environmental changes to ease access to food and litter, and providing a stable and predictable routine with a quiet, safe sleeping area (Figs 2 and 3). 12
FIG 2.
Routine wellness care should include grooming and nail trimming (a) to avoid problems such as ingrowing toenails (b). Courtesy of (a) Deb Givin; (b) Danielle Gunn-Moore
FIG 3.

A safe sleeping area is one of the five key resources for cats. Courtesy of Deb Givin
Five key resources for cats.
Water
Food
Litter box
Social interactions
Resting/sleeping/hiding space
Nutrition and weight management
Dietary recommendations must be individualized and will vary depending on the BCS (see page 764) and any disease present. A good diet is palatable, provides complete and balanced nutrition, and helps maintain ideal body weight, normal fecal character, and healthy skin and hair coat. Several factors must be considered in cats that are mature or older:
Feeding small meals frequently increases digestive availability. The ideal number of meals is not known, but feeding multiple (eg, three or four) small meals per day is a reasonable goal.
-
Increased water intake is important since older cats are prone to conditions that predispose to dehydration and subsequent constipation. Water intake can be increased by feeding canned food and using multiple water dishes. Note that:
— It may be difficult to convert cats from dry to canned food; starting use of canned food at a younger age could help cats become accustomed to it.
— Some cats will refuse to eat canned food; cats predisposed to dehydration that continue to eat dry food should be encouraged to increase liquid intake (eg, tuna juice ice cubes, water added to dry food, drinking fountains).
-
Dietary changes are often recommended. Note that:
— Diet changes can alter the intestinal flora, leading to diarrhea, vomiting or loss of appetite.
— Changes may need to be made gradually (over weeks or months in some cats) to be accepted, yet the presence of disease or food aversion makes a more rapid change desirable.
— Cyproheptadine may increase appetite. Mirtazapine both stimulates appetite and reduces nausea; use the lowest effective dose.
The essential B vitamins are not stored, so a diminished appetite or intestinal disease can lead to deficiencies. Oral and/or parenteral supplements may be needed as indicated by the cat's condition. Measure serum cobalamin (B12) concentration in any cat with weight loss, diarrhea or poor appetite that may have gastrointestinal (GI) disease. 31 Lifelong replacement may be required for cats with maldigestive or malabsorptive disease.
If urinary stones are a problem in seniors, non-acidified prescription diets can be used that prevent both triple phosphate and calcium oxalate stone formation. This helps avoid excess systemic acidification or low sodium diets which can contribute to progressive potassium loss and lead to a hypokalemic nephropathy. 32
A cat that is overweight or underweight has a problem that must be managed as a disease (see boxes). Monitor both increased and decreased weight, comparing serial body weights and evaluating the BCS. 33
A cat that is overweight or underweight has a problem that must be managed as a disease.
Underweight/loss of body mass.
Cats in the ‘senior’ and ‘geriatric’ age groups often become underweight with a low BCS. This may be due to underlying disease, changes in metabolism and hormones with increasing age, and/or a decrease in the ability to adequately digest protein.
Loss of normal body mass is a clinical sign that is an indication of chronic disease and a predictor of mortality; when possible, identify and correct the underlying health problem.33–35
Recognize and investigate the cause of changes in muscle mass. Muscle atrophy is typically secondary to chronic OA or nerve damage; muscle wasting is typically associated with lack of exercise, poor diet, severe kidney disease or neoplasia.
Cats admitted to veterinary clinics are more likely than dogs to be underweight (median BCS 4/9) with −60% having recently lost weight. 36 Attend to adequate and proper feeding while in the hospital; balance the need for hospitalization with the cat's willingness to eat, treating at home if possible.
Protein wasting and loss of muscle mass can result from inadequate protein intake or digestibility. Kidney or intestinal disease may further negatively affect this balance. Thus, the key is to feed the cat sufficient high-quality protein without exacerbating any pre-existing or new conditions. In general, if a higher protein diet is desired, canned foods will provide a wider selection of choices.
Placement of a feeding tube allows administration of proper nutritional support and can ease administration of fluids or medications.

Underweight senior cat. Courtesy of Daniélle Gunn-Moore
Obesity.
Since obesity often begins in young cats, ‘mature’ and older cats should receive continuing weight management.37–39
Obesity is a metabolic disease with hormonal, metabolic and inflammatory changes that requires immediate attention. It is a risk factor for diabetes, OA, respiratory distress, lower urinary tract diseases and early mortality. 40
Obesity is caused by increased overall caloric intake relative to energy expenditure. Metabolism also plays a part; feline carbohydrate metabolism differs from that of non-obligate carnivores.38,41
In cats with specific conditions requiring other diets (eg, CKD), the weight loss plan must be modified, which may complicate weight management.
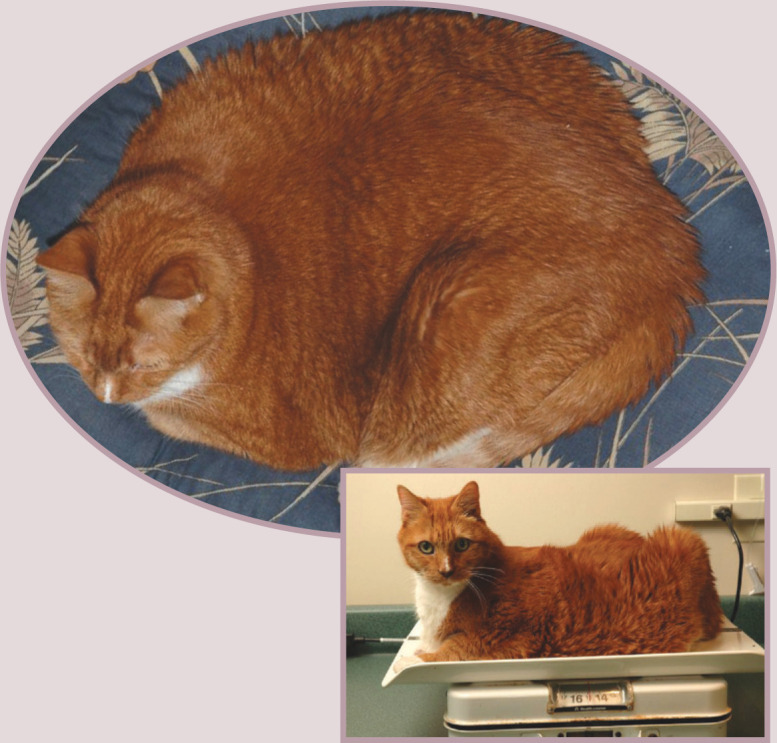
Fergie, pictured in 2006 (above), severely overweight and (right) slimming down over subsequent months. Courtesy of Deb Givin
Although increasing age, poor health status and extremes of weight are identified risk factors during anesthesia, mature and older cats can be successfully anesthetized.
Dental care
Oral cavity disease is an often overlooked cause of significant morbidity in the older cat and can contribute to a general decline in attitude and overall health. 17 A complete oral exam, plus the owner's observation of eating behavior, will elucidate dental problems. Cats with oral pain may be thin, drop their food, chew on one side, eat more slowly, eat less, or show less interest in food. Age or the presence of other chronic conditions should not exclude the treatment of dental disease, which can be undertaken when the cat is stabilized. Avoiding treatment of painful dental conditions such as odontoclastic resorptive lesions, periodontal disease or broken teeth contributes to diminished quality of life.13,17 The American Animal Hospital Association (AAHA) has published comprehensive dental care guidelines for dogs and cats. 13
Anesthesia
Although increasing age, poor health status and extremes of weight are identified risk factors during anesthesia, mature and older cats can be successfully anesthetized.42–43 Various precautions and considerations will help ensure a safe recovery, which include (but are not limited to) the following:
Tailor the preanesthetic testing and preparation to the individual cat's clinical condition. Begin correction of underlying abnormalities pre-operatively whenever possible. For example, cats with CKD may need prehydration and / or fluids in the immediate postoperative period, as well as maintenance fluid therapy during the procedure, to prevent hypovolemia and hypotension.
Provide and monitor intravenous fluids for all anesthetic patients. Decreased ventricular compliance and cardiac reserve make older cats less tolerant to changes in intravascular volume, making them more susceptible to fluid overload or volume depletion complications.
Recall the changes in drug metabolism with overweight or underweight cats, and with certain disease states. Reduce dosages of drugs with a significant effect on heart rate (eg, ketamine or alpha-2 agonists) and, in cats with renal compromise, reduce dosages of anesthetic drugs eliminated by renal excretion (eg, ketamine).
Monitor blood pressure throughout anesthesia, with careful attention to cats receiving antihypertensive medication. 44
Poor lung compliance and decreased lung reserve capacity increase susceptibility to hypoxia in the perianesthetic period. Pre-oxygenation and more frequent bagging may be necessary. 45
Since hypothermia is common, evaluate body temperature every 15 mins, continuing postoperatively until the cat is ambulatory or normothermic. Support body temperature by using tools such as a heated cage, hot air blankets, water-circulating heating pad, and/or booties. 43
Ensure appropriate pain management is provided for all dental and surgical procedures. Pre-surgical analgesics (eg, buprenorphine) decrease the necessary amount of injectable or inhalation anesthesia, thereby lowering the risk of anesthetic or drug adverse reactions. Attend to comfort and gentle handling, particularly for cats with OA or muscle wasting.
Monitoring and managing disease
Chronic diseases typically start to develop in mature cats but may not manifest fully for some years. These guidelines will not attempt to review all aspects of diseases, but will highlight new or crucial information about those diseases that are most common in senior cats (see below).
Hypertension
Hypertension appears to be recognized most often among cats over 10 years of age. 46
Hypertension is potentially damaging to the eyes, brain, heart, kidneys and central nervous system.
Hypertension may be idiopathic or secondary (ie, associated with a variety of disease states; Table 2). Most cats have an identifiable cause for their elevated blood pressure (BP), but idiopathic increases in BP may occur in a substantial subpopulation of older cats (possibly ranging from 17–55% in one study). 46
Cats have a significant incidence of anxiety-associated hypertension.
Treat when the BP is 180/120 mmHg or, in cats with CKD, when the BP is 160–179/100–119 mmHg. A reasonable treatment goal is to reduce BP to below 150/95 mm (no lower than 120 mmHg for systolic). 47
The American College of Veterinary Internal Medicine (ACVIM) has created excellent, detailed guidelines about measuring and interpreting BP and diagnosing and treating hypertension. 18
TABLE 2.
Diseases and drugs associated with secondary hypertension 18
| Diseases | Drugs |
|---|---|
| Kidney disease | Glucocorticoids |
| Hyperthyroidism | Erythropoietin |
| Hyperaldosteronism | Mineralocorticoids |
| Phaeochromocytoma | Sodium choride |
| Non-steroidal anti-inflammatory drugs |
Chronic kidney disease
While kidney disease is most common in older cats, it most likely begins in middle age (Pet Protect insurance company, data on file 2008). While diagnosis and management are extensively described elsewhere,20,48 a few specifics deserve mention:
Blood pressure measurement.
Experts agree that increased BP may significantly affect feline health and thus BP should be measured at least annually in cats in the ‘senior’ and ‘geriatric’ age groups.
There is some debate about the indications for or frequency of measuring BP in cats in the ‘mature’ age group. Some recommend routine BP measurement only in mature cats with hyper-tension-associated diseases or signs consistent with target organ damage. Their concern is accuracy, since ‘white coat hypertension’ is a significant problem in cats; widespread screening could lead to overtreating or performance of unnecessary tests. Others recommend monitoring BP with every MDB collection, thus providing baseline measurements for future comparison. Taking precautions to reduce anxiety can increase accuracy.
One approach is to obtain one or more baseline values for mature cats and then to measure at increasingly frequent intervals as cats age and their risk of hypertension-associated disorders such as kidney disease increases. Obtaining an accurate BP requires a consistent approach with attention to detail (see below). 18 It is not necessary to shave the hair to get good Doppler contact using alcohol and gel.
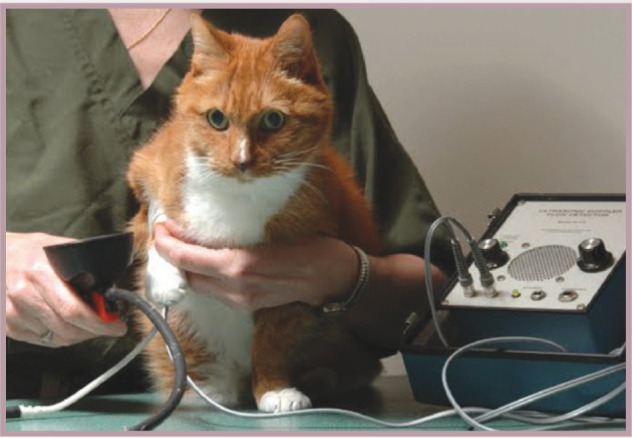
Blood pressure should be measured at least annually in ‘senior’ and ‘geriatric’ cats. Courtesy of Deb Givin
Ways to improve measurement accuracy.
Use the most accurate machine available (currently Doppler)
Measure BP with the owner present, in a quiet room. Allowing the cat to acclimate to the room for 5–10 mins can decrease anxiety-associated hypertension up to 20 mmHg
Train staff to minimize stress, including minimizing restraint, which would potentially cause anxiety-induced BP increases
Monitor sequential measurements to detect trends; base treatment decisions on multiple measurements
Use proper cuff size (30–40% of circumference of cuff site) and a consistent location on the cat's body
-
Routine MDB screening and evaluation of trends may reveal early disease.
Often, CKD-induced polyuria and polydipsia are not noted by cat owners. Signs that are sometimes overlooked include constipation, inappetence, nausea, change in drinking frequency or location, poor hair coat, and muscle wasting or weight loss.
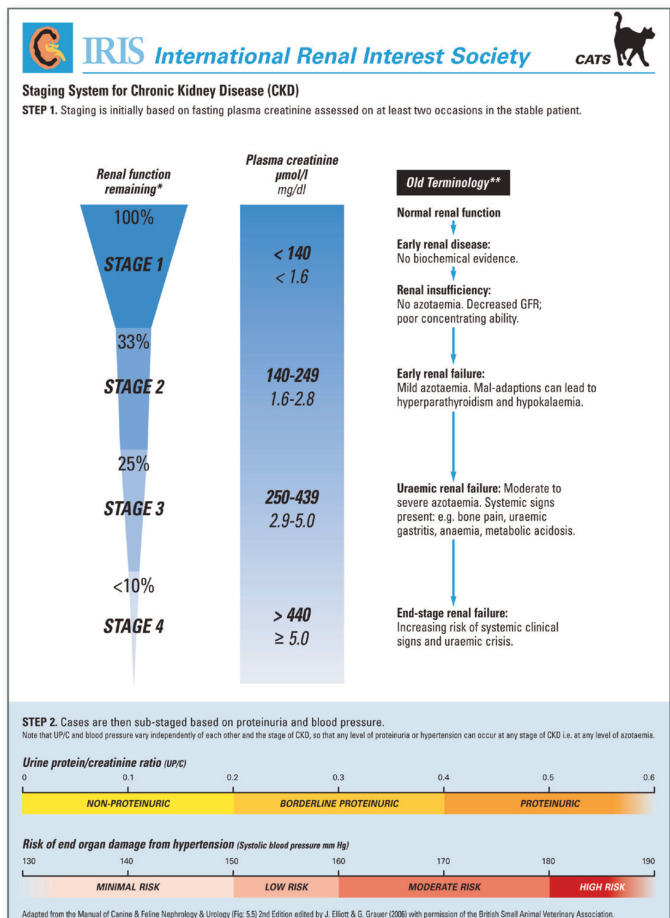
Some patients with serum creatinine values within published reference ranges may actually have CKD. Evaluating urine concentrating ability is essential. In the absence of urinary obstruction or non-renal causes of polyuria, serum creatinine values >1.6 mg/dl (140 μmol/l) with urine specific gravity persistently <1.035 are likely to indicate kidney disease in a hydrated patient.
The International Renal Interest Society (IRIS) provides detailed guidelines for the management of CKD. 20 Once CKD has been diagnosed and the patient is stable and hydrated, determine the patient's UPC ratio and BP. IRIS stage to aid in management. The IRIS stage is assigned using the serum creatinine concentration, UPC ratio and BP (see below). 20
Investigate and treat electrolyte abnormalities such as hypokalemia, hyperphosphatemia and acidosis. Maintain potassium at >4 MEq/dl (>4 mmol/l), regardless of reference range normals. 49 Treatment goals for phosphorus restriction are below normal reference values: <4.5 mg/dl (<1.45 mmol/l) for stage 2, <5 mg/dl (<1.6 mmol/l) for stage 3, <6 mg/dl (<1.9 mmol/l for stage 4). 50
Monitor BP, since CKD is the leading cause of secondary hypertension.
Perform a urine culture as part of the MDB for cats with CKD, even in the absence of inflammatory sediment. 26
Evaluate for proteinuria, a marker for severity of kidney disease that has been shown to be a negative predictor of survival and may play a role in progression of kidney injury. Finding a raised UPC (>0.4) warrants consideration of treatment.23,24
Feeding a ‘renal’ prescription diet has been shown to reduce uremic episodes, decrease phosphorus retention, prevent muscle wasting and increase survival times. The composition of renal diets is more complex than just providing low protein, and their beneficial effects may not be down to their low protein content alone.48,51-55 Canned diets provide the benefit of improving hydration.
If the cat will not eat a commercial renal diet, home-prepared, nutritionally balanced lower protein diets may be a reasonable compromise. 56 Alternatively, a feeding tube may be used to provide optimum nutrition.
Once the patient is stabilized, continue monitoring every 3–6 months, or more often if indicated; the frequency depends on several factors outlined in the IRIS guidelines. 20
This IRIS chart is reproduced according to the IRIS Guidelines 2006, with permission of IRIS and Novartis Animal Health
Thyroid testing.
A T4 should be run any time hyperthyroidism is suspected, including (but not limited to): noting signs of inappropriate defecation or urination, weight loss, polyphagia, polydipsia, inappetence, hypertension, heart murmur or a thyroid nodule.
Panelists debate about the age at which the T4 measurement should become part of the annual MDB for healthy-appearing cats. Some think this should begin at age 7, whereas others prefer to wait until age 10. Preliminary data from the UK show an overall incidence of hyperthyroidism of around 0.5%, with the vast majority of cases occurring in senior cats (Pet Protect insurance company, UK, unpublished data).

Hyperthyroidism
Approximately 40% of cats with early hyperthyroidism have only mild clinical signs. Early hyperthyroid disease can be diagnosed 1–2 years prior to obvious signs.57–59
Thyroid nodules may or may not be functional so diagnosis cannot be made solely on the presence or absence of a thyroid nodule. 60
The total T4 is the appropriate screening test. An elevated result indicates hyperthyroidism is present, but a normal result does not rule out hyperthyroidism. 61
Should total T4 results be equivocal or normal, but hyperthyroidism is suspected, rule out other illness. Then concurrently evaluate a second total T4 plus a free T4 by equilibrium dialysis.
Since free T4 can be elevated in cats with non-thyroidal illness, interpret free T4 in conjunction with total T4 and clinical signs. 61
A high free T4 with total T4 in the upper range of normal supports the diagnosis.
Thyroid scintigraphy, if available, is important in treatment planning for I131 therapy, can be used to assess poor response, and is helpful if malignant disease is suspected.62,63 Scintigraphy is a good test for localizing the source of thyroid hormone production and may assist in diagnosing hyperthyroidism.
-
Monitor affected cats for kidney disease and hypertension. Note that:
— Hypertension may persist or even develop after treatment.21,64,65
— Hypertension secondary to hyperthyroidism alone may self-correct when a euthyroid state is achieved. 18
-
— Renal function should be monitored.
Creatinine levels post-treatment can rise due to unmasking of existing kidney disease. Even cats with a urine specific gravity >1.035 are at risk of developing unmasked kidney disease following treatment. 21
Transdermal methimazole is an alternative for cats with vomiting or inappetence secondary to oral methimazole. Differences in efficacy and side effects are still being studied.66–69
Early hyperthyroid disease can be diagnosed 1–2 years prior to obvious signs.
Diabetes mellitus
Diabetes mellitus is an increasingly common disease, most commonly diagnosed in middle-aged, obese male cats.70–72 It remains a significant disease in senior cats, with almost half of all diabetics being 10–15 years old.73,74
Interpretation of blood glucose curves remains a challenge due to stress responses in the hospital setting. Introduction of home monitoring by owners (blood collection via ear veins) may help mitigate the problem associated with stress.75–77
-
Although most cats are insulin dependent at the time of diagnosis, early glycemic control may lead to clinical remission. Recent advances in treatment that can facilitate earlier and/or tighter glycemic control include:
— Feeding a canned low carbohydrate, high protein diet. 78
— The availability of new insulins such as long acting insulin glargine, which can help achieve ideal mean blood glucose concentrations. 70
— Portable blood glucose monitors, which can allow clients to perform blood glucose curves at home. Choose a monitor shown to be accurate with cats, since accuracy varies greatly.75,79
Of particular importance for senior cats is the effect of concurrent disease, such as chronic pancreatitis, on their health status.
Corticosteroids can cause increased insulin resistance, further complicating disease management.70,80
Inflammatory bowel disease and associated disease
Inflammatory bowel disease (IBD) begins in adult cats and may require lifelong treatment. Increased vomiting or poor appetite may be more common or have a greater impact in older cats, so medication changes may be needed.
The clinical signs of IBD are non-specific and may be confused with many diseases of older cats. Additionally, IBD may influence the diagnostic and/or treatment approach to other diseases when it is present.
Rule out a disorder causing digestion/absorption problems in euthyroid, non-diabetic cats with unexplained weight loss, vomiting, diarrhea, increased appetite and thirst. The history may reveal that the cat is ingesting more calories than should be necessary for normal metabolism.
In addition to the MDB, initial evaluation should include measurement of feline pancreatic lipase immunoreactivity (fPLI), feline trypsin-like immunoreactivity (fTLI), B12 and folate concentration, which help create a specific treatment plan.31,81-84 Correct interpretation of the results is available at the Texas A&M University, GI Lab website (www.cvm.tamu.edu/gilab/index.aspx).
-
Differentiation of IBD from small cell lymphoma can be challenging:
— Endoscopically obtained samples are not always sufficient for definitive diagnosis since lymphoma lesions often lie deep to the mucosal layer. Full thickness biopsy is ideal, but does not always provide the definitive diagnosis. 85
— Since the treatment for both diseases can be the same, the risk of surgical biopsy has to be weighed against the potential benefits for each patient.
— Biopsy is recommended for cats that do not respond well to treatment for IBD or have ultrasound changes that lead to suspicion of severe intestinal disease or concurrent illness.
Because of the close anatomic relationship between the pancreatic and bile ducts in cats, it is important to recognize that IBD, pancreatitis and cholangiohepatitis may occur separately or together (see later section on complex disease management).
Cancer
Weight loss, in the absence of other identifiable causes, is a common sign of cancer. The paraneoplastic syndrome of cancer cachexia causes a loss of fat and muscle mass and can occur even in cats that eat well.
Pursuing a diagnosis before body condition deteriorates may affect outcome. A recent study found a positive correlation between BCS, remission rate and median survival time. Cats with a BCS <5/9 had a significantly shorter median survival time (3.3 months) than cats with a BCS >5/9 (16.7 months). 86
Many cancers are treatable or manageable. High remission rates and extended survival times are achievable for many cats with the most common cancer, lymphoma.87,88
-
Educate clients about the differences between human and animal chemotherapy:
— Treatment goals are to control the cancer and to improve the cat's quality of life, with less frequent and less severe side effects than those seen in people.
— Owners who pursue chemotherapy are usually satisfied with their decision; they perceive their cat's quality of life as being higher than prior to treatment. 89
Palliative therapy, designed to improve quality of life without necessarily increasing survival time, remains a mainstay of therapy in many cats. Critical components of all cancer therapy include pain management, 90 anti-nausea medication (eg, ondansetron, dolasetron, maropitant citrate) and nutritional support.
Osteoarthritis
Osteoarthritis is a common but under-recognized condition in senior cats. In radiographic studies, prevalence rates have varied from 22% in cats of all ages up to 90% in cats ≥12 years of age.8,9,91,92 Radiographic evidence is not always consistent with clinical signs; there may be radiographic changes with no clinical signs, as well as clinical signs with no radiographic changes.91,92
Improving access to key resources.
Provide food and water at floor level, raised slightly, to reduce the need for jumping or bending.
Add ramps or steps to allow easier access to favored sleeping areas.
Use deep, comfortable bedding.
Provide large litter boxes with a low entry for easy access, and high sides to help cats that cannot squat (eg, a dog litter box). A fine-consistency litter is easier on the paws.
Signs are often subtle behavioral and lifestyle changes mistaken for ‘old age’. 93 Use a mobility questionnaire to help with diagnosis (Table 3). Palpate for joint thickening, swelling or pain; crepitus or limited range of motion are not routinely noted, and pain does not always correlate with radiographic signs of disease. 8
Management is ideally holistic in scope, attending to both the cat and its environment. 91 Improve access to key resources (see below), and manage obesity to reduce the stress on the cat's joints and facilitate exercise.
-
Treatment decisions depend on the degree of OA and the existence of concurrent diseases. A multimodal or staged approach may be needed. Note that:
— Diets created for management of OA may improve joint mobility and comfort. These may include a variety of supplements for which there is varying evidence of efficacy.
— Chondroprotective agents and nutraceuticals may be useful in patients with mild to moderate OA. 94
— Additional pain medication can be added at times of acute flare-up, or continually as progression occurs. Pain management guidelines have been published. 90 Medication choices include opiates (eg, transmucosal or subcutaneous buprenorphine, tramadol), gabapentin or NSAIDs (eg, meloxicam). 9 Recent studies have shown good efficacy and safety with oral low dose meloxicam. 95 However, in the United States, meloxicam has not been approved for use beyond a one-time injection; obtain informed client consent for any off-label use. Take appropriate precautions, including laboratory monitoring, if using any NSAID.
Non-drug interventions include surgery, acupuncture, electroacupuncture, passive motion exercises and massage. While they may be of benefit in individual cases, little published data is currently available relating to their use in cats. 96
TABLE 3.
Mobility/cognitive dysfunction questionnaire∗
| My cat: | Yes | Maybe | No |
| is less willing to jump up or down | |||
| will only jump up or down from lower heights | |||
| shows signs of being stiff at times | |||
| is less agile than previously | |||
| cries when lifted | |||
| shows signs of lameness or limping | |||
| has difficulty getting in or out of the cat flap/cat door | |||
| has difficulty going up or down stairs | |||
| has more accidents outside the litter box | |||
| spends less time grooming | |||
| is more reluctant to interact with me | |||
| plays less with other animals or toys | |||
| sleeps more and/or is less active | |||
| cries out loudly for no apparent reason | |||
| has become more fearful and/or more aggressive | |||
| appears forgetful |
Ensure there have been no environmental reasons for the change. Table provided courtesy of Danielle Gunn-Moore
Cognitive disorders
When considering brain aging in cats and humans, the age at which 50% of cats and 50% of humans have signs of cognitive dysfunction (dementia) is 15 years for cats and 85 years for humans.97–99
Signs of cognitive disorders include altered behavior, inappropriate elimination, spatial or temporal disorientation, altered interaction with the family, changes in sleep/wake cycles, changes in activity, and/or inappropriate vocalization (often displayed as loud crying at night) (Table 3). 15
Cognitive changes may result from systemic illness (eg, hyperthyroidism, hypertension), organic brain disease (eg, brain tumor), true behavioral problems (eg, separation anxiety), or cognitive dysfunction syndrome, a neurodegenerative disorder that is believed to result from compromised cerebral blood flow, chronic free radical damage and amyloid deposition.100,101
Rule out all medical illnesses to diagnose a primary cognitive disorder.
Feline treatments are extrapolated from studies of humans and dogs. Diets enriched with antioxidants and other supportive compounds (eg, vitamin E, beta carotene, and essential omega-3 and 6 fatty acids) are believed to reduce oxidative damage and amyloid production, and improve cognitive function.102,103
Environmental management, particularly surrounding litter box issues, can help the cat and owner maintain good quality of life. Because these cats are easily stressed, change should be kept to a minimum or incorporated gradually.
No drugs are licensed for the treatment of cognitive dysfunction syndrome in cats. Anti-anxiety medication may be useful in some cases. 104 Selegiline, propentofylline and nicergoline have all been used with varying degrees of success.105–108
Complex disease management.
As cats get older, the likelihood of developing more than one disease increases, often with complex effects on diagnosis and treatment. Explore options to help clients manage their pet with multiple diseases. Educate clients about administering and scheduling medications, asking about their abilities and limitations. Multiple treatments can be difficult for the patient and the client; it is important that the quality of the human-animal bond is maintained despite multiple treatments. Educate clients on ways to administer medications in a calm manner that is comfortable for the cat. Explore new routes for oral medications, such as treats made to hold pills, food the cat likes, or reformulation of medications into treats, liquids or pastes. Consider complementary treatments, such as nutraceuticals, acupuncture, massage therapy and physical therapy. Listen to clients, asking how treatments are going and exploring their expectations, desires and needs.
When expected therapeutic results are not obtained, search for additional disease processes. While any diseases may occur concurrently, certain ones occur together more often, confounding diagnosis and treatment.
Be aware of issues surrounding multiple diseases in senior cats:
Treatment of some diseases may worsen other, concurrent diseases (eg, treatment of hyperthyroidism can unmask the severity of kidney disease).
The effect of polypharmacy or drug interactions.
The effect of diet on body condition, GI function, kidney function and overall health
-
The cumulative impact of multiple diseases.
— CKD, OA, diabetes mellitus and IBD, when present in any combination, can result in significant inappropriate elimination.
-
The risk of diagnosing one disease while missing another, or assuming a single disease is severe when signs are actually due to multiple diseases. Note, for example, that:
— When cholangitis, pancreatitis and/or IBD occur together, one or more may be missed. 109
— Chronic pancreatitis may be missed in a diabetic patient.110,111
— Hyperthyroidism may be missed in cats with kidney or liver disease, or cancer because typical signs are masked and T4 may be suppressed back into the top of the normal range.112,113
— Hyperthyroidism may also be missed in cats with diabetes | mellitus since signs are usually similar.
— The diagnosis of urinary tract infection in cats with kidney disease, hyperthyroidism or diabetes can be complicated, since signs of lower urinary tract disease, pyuria and/or active urine sediment are not always present. Diagnosis can only be confirmed by performing a urinalysis and bacterial culture (see MDB, Table 1). 26
— Hyperthyroidism and cardiac disease may occur together, with only one being recognized.
Hyperthyroidism and concurrent DM.
T4 concentrations may be lower than expected in hyperthyroid cats with DM.112,114 Insulin requirement may change after treatment of hyperthyroidism.
Hyperthyroidism can confuse diagnosis of diabetes mellitus because it can increase serum glucose concentrations while reducing serum fructosamine concentrations. 115
Hyperthyroidism and concurrent CKD.
Hyperthyroidism may cause an increased glomerular filtration rate and thus a decreased BUN and creatinine, with under-diagnosis of CKD. Creatinine may also be low from low muscle mass with hyperthyroidism. Repeat laboratory evaluation following hyperthyroid treatment to reassess CKD and the need for treatment changes.
CKD may mask hyperthyroidism. 112 Measuring free T4 concentration is often needed to diagnose hyperthyroidism in these cases. 113
The veterinarian must act as a patient advocate when counseling clients about decisions regarding use and/or continuation of treatment.
Quality of life
Hand in hand with the management of chronic illness in senior patients comes the responsibility to control pain and distress, assess quality of life, and provide guidance to the owner in end-of-life decisions.
Veterinarians can assist clients in managing home care, changing the environment as necessary to ensure comfort and access to the five key resources (see page 773). The veterinarian must act as a patient advocate when counseling clients about decisions regarding use and/or continuation of treatment. 116 Using published quality-of-life scales or an individualized list of behaviors (see right) as objective tools can aid tremendously in determining ‘when it's time’.
Quality-of-life assessment tools.
RSPCA Five Freedoms Fact Sheet www.wspa-international.org/wspaswork/education/downloads_resources.aspx
Alice Villalobos' Quality of Life Scale Available online in multiple sites including: www.veterinarypracticenews.com/vet-practice-news-columns/bond-beyond/quality-of-life-scale.aspx
Relevant questions might include:
Is pain well controlled?
Is the cat able to eat, albeit with support?
Can the cat navigate to its key resources, albeit with supportive changes?
Does the cat have more good days than bad days?
Does the cat follow its former predictable routines for sleeping, resting, grooming, eating, playing and socializing?
Hospitalized cats may become depressed; therefore, allow clients to keep cats at home whenever possible. If hospitalization is needed, it should be for the shortest time possible, and with visiting available for the clients.
Hospice care patients and their owners benefit from examination every 2–4 weeks, or as deemed necessary to assess comfort, quality of life, and quality of the relationship. Discussion about what to expect during the process of euthanasia and options for aftercare can help alleviate owner anxiety when the time does come. Helping owners prepare for loss and grief is a valuable and memorable service that veterinarians can offer. 117
Where next?
The authors deliberated at length about some aspects of this article. Many recommendations are not as definite as some would desire. The creation of these Senior Care Guidelines has elucidated areas where further clinical investigation and more evidence are needed to create clearer recommendations for optimal health of senior cats.
Acknowledgements
Supported by grants from: Nestlé Purina, Merial Ltd, IDEXX Laboratories, Inc, Nutramax Laboratories, Inc, and Abbott Laboratories. Thanks also to Pet Protect for allowing access to its database in order to generate UK prevalence data for kidney disease and hyperthy-roidism.
Disclaimer: Dr Gunn-Moore, Dr Polzin and Dr Zoran have received funding for previous work from Nestlé Purina. Dr Taboada has received funding for previous work from Merial Ltd and Nutramax Laboratories, Inc.
In memoriam
Dedicated to our friend, colleague and coauthor of the original AAFP Senior Care Guidelines, Dr Jim Richards. A passionate cat lover, he was particularly fond of his older ‘kitty’, Dr Mew. Two of Dr Richards’ favorite sayings were: ‘Cats are masters at hiding illness’ and ‘Age is not a disease.’
KEY POINTS.
While age itself is not a disease, the aging process induces complex and interrelated metabolic changes that complicate health care.
Management decisions should not be based solely on the age of the patient, as many conditions that affect older cats can be controlled, if not cured.
Veterinarians treating senior cats must be adept at recognizing, managing and monitoring chronic disease and, when possible, preventing disease progression, while ensuring a good quality of life.
With prevention, early detection and treatment of health care problems, the human-pet-veterinary for cats improved.
References
- 1.Pew Research Center Publications. Gauging family intimacy: dogs edge cats (dads trail both). March 7, 2006. http://pewresearch.org/pubs/303/gauging-family-intimacy (accessed Dec 1, 2008).
- 2.Cohen SP. Can pets function as family members? West J Nurs Res 2002; 24: 621–38. [DOI] [PubMed] [Google Scholar]
- 3.Adams CL, Bonnett BN, Meek AH. Predictors of owner response to companion animal death in 177 clients from 14 practices in Ontario. J Am Vet Med Assoc 2000; 217:1303–9. [DOI] [PubMed] [Google Scholar]
- 4.AAHA. The path to high quality care: practical tips for improving compliance, 2003.
- 5.FAB. Feline Advisory Bureau, UK. Well Cat for Life. www.fabcats.org/wellcat/publications/index.php (accessed Dec 1, 2008).
- 6.Broussard JD, Peterson ME, Fox PR. Changes in clinical and laboratory findings in cats with hyperthyroidism from 1983 to 1993. J Am Vet Med Assoc 1995; 206: 302–5. [PubMed] [Google Scholar]
- 7.Wolf A. Proceedings of the BSAVA Pedigree Pet Foods lecture tour, 2005.
- 8.Hardie EM, Roe SC, Martin FR. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994–1997). J Am Vet Med Assoc 2002; 220: 628–32. [DOI] [PubMed] [Google Scholar]
- 9.Clarke SP, Bennett D. Feline osteoarthritis: a prospective study of 28 cases. J Small Anim Pract 2006; 47: 439–45. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz S, Silverman J, Draper J. Teaching and learning communication in medicine. Oxon, UK: Radcliffe Medical Press, 1998. [Google Scholar]
- 11.Frankel RM, Stein T. Getting the most out of the clinical encounter: the four habits model. Perman J 1999; 3(3): 79–88. [PubMed] [Google Scholar]
- 12.Overall K, Rodan I, Beaver B, et al. AAFP feline behavior guidelines. www.catvets.com (accessed Dec 1, 2008).
- 13.Holmstrom S, Bellows J, Colmery B, Conway ML, Knutson K, Vitoux J. AAHA dental care guidelines. J Am Anim Hosp Assoc 2005; 41: 277–83. www.aahanet.org (accessed Dec 1, 2008). [DOI] [PubMed] [Google Scholar]
- 14.AAHA. AAHA issues position statement on frequency of veterinary visits. AAHA ‘Member Connection’, 2008.
- 15.Moffat KS, Landsberg GM. An investigation of the prevalence of clinical signs of cognitive dysfunction syndrome (CDS) in cats. J Am Anim Hosp Assoc 2003; 39: 512. [Google Scholar]
- 16.Epstein M, Kuehn N, Landsberg G. AAHA senior care guidelines for dogs and cats. J Am Anim Hosp Assoc 2005; 41: 81–91. www.aahanet.org (accessed Dec 1, 2008). [DOI] [PubMed] [Google Scholar]
- 17.Richards J, Rodan I, Beekman G, et al. AAFP senior care guidelines for cats, 1st edn, 1998. www.catvets.com (accessed Dec 1, 2008).
- 18.Brown S, Atkins C, Bagley R, et al. Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. ACVIM consensus statement. J Vet Intern Med 2007; 21: 542–58. www.acvim.org/websites/acvim/index.php?p=94 (accessed Dec 1, 2008). [DOI] [PubMed] [Google Scholar]
- 19.Mardell EJ, Sparkes AH. Evaluation of a commercial in-house test kit for the semi-quantitative assessment of microalbuminuria in cats. J Feline Med Surg 2006; 8: 269–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Renal Interest Society (IRIS). www.iris-kidney.com/ (accessed Dec 1, 2008).
- 21.Riensche MR, Graves TK, Schaeffer DJ. An investigation of predictors of renal insufficiency following treatment of hyperthy-roidism in cats. J Feline Med Surg 2008; 10: 160–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elliott J, Syme HM. Proteinuria in chronic renal failure in cats-prognostic marker or therapeutic target? [editorial]. J Vet Intern Med 2006; 20: 1052–53. [DOI] [PubMed] [Google Scholar]
- 23.Syme HM, Markwell PJ, Pfeiffer D, Elliott J. Survival of cats with naturally occurring chronic renal failure is related to severity of proteinuria. J Vet Intern Med 2006; 20: 528–35. [DOI] [PubMed] [Google Scholar]
- 24.Lees GE, Brown SA, Elliott J, Grauer GE, Vaden SL, American College of Veterinary Internal Medicine Assessment and management of proteinuria in dogs and cats: the 2004 ACVIM forum consensus statement (small animal). J Vet Intern Med 2005; 19: 377–85. [DOI] [PubMed] [Google Scholar]
- 25.King JN, Tasker S, Gunn-Moore DA, Strehlau G, BENRIC Study Group Prognostic factors in cats with chronic renal disease. J Vet Intern Med 2007; 21: 906–16. [PubMed] [Google Scholar]
- 26.Mayer-Roenne BM, Goldstein RE, Erb HN. Urinary tract infections in cats with hyperthyroidism, diabetes mellitus, and chronic kidney disease. J Feline Med Surg 2007; 9: 124–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chew J, DiBartola S. Recent concepts in feline lower urinary tract disease. Vet Clin North Am Small Anim Pract 2005; 35: 147–70. [DOI] [PubMed] [Google Scholar]
- 28.Companion Animal Parasite Council CAPC guidelines. www.capcvet.org/ (accessed Dec 1, 2008).
- 29.Levy J, Crawford C, Hofmann-Lehmann R, Little S, Sundahl E, Thayer V. AAFP retrovirus guidelines. J Feline Med Surg 2008; 10: 300–16. www.catvets.com (accessed Dec 1, 2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Richards JR, Elston TH, Ford R, et al. AAFP feline vaccine guidelines. J Am Vet Med Assoc 2006; 29: 1405–11. www.catvets.com (accessed Dec 1, 2008). [DOI] [PubMed] [Google Scholar]
- 31.Simpson KW, Fyfe J, Cornetta A, et al. Subnormal concentrations of serum cobalamin (vitamin B12) in cats with gastrointestinal disease. J Vet Intern Med 2001; 15: 26–32. [DOI] [PubMed] [Google Scholar]
- 32.Buranakarl C, Mathur S, Brown SA. Effects of dietary sodium chloride intake on renal function and blood pressure in cats with normal and reduced renal function. Am J Vet Res 2004; 65: 620–27. [DOI] [PubMed] [Google Scholar]
- 33.LaFlamme DP. Nutrition for aging cats and dogs and the importance of body condition. Vet Clin North Am Small Anim Pract 2005; 35: 713–42. [DOI] [PubMed] [Google Scholar]
- 34.Doria-Rose VP, Scarlett JM. Mortality rates and causes of death among emaciated cats. J Am Vet Med Assoc 2000; 216: 347–51. [DOI] [PubMed] [Google Scholar]
- 35.Galanos AN, Pieper CF, Kussin PS, et al. Relationship of body mass index to subsequent mortality among seriously ill hospitalized patients. Crit Care Med 1997; 25: 1962–68. [DOI] [PubMed] [Google Scholar]
- 36.Chandler ML, Gunn-Moore DA. Nutritional status of canine and feline patients admitted to a referral veterinary internal medicine service. J Nutr 2004; 134 (suppl 8): 2050–52. [DOI] [PubMed] [Google Scholar]
- 37.Fettman MJ, Stanton CA, Banks LL, et al. Effects of neutering on bodyweight, metabolic rate and glucose tolerance of domestic cats. Res Vet Sci 1997; 62: 131–36. [DOI] [PubMed] [Google Scholar]
- 38.Hoenig M, Thomaseth K, Waldron M, Ferguson DC. Insulin sensitivity, fat distribution, and adipocytokine response to different diets in lean and obese cats before and after weight loss. Am J Physiol Regul Integr Comp Physiol 2007; 292: R227–34. [DOI] [PubMed] [Google Scholar]
- 39.Martin LJM, Siliart B, Dumon HJW, et al. Spontaneous hormonal variations in male cats following gonadectomy. J Feline Med Surg 2006; 8: 309–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lund EM, Armstrong PJ, Kirk CA, Klausner JS. Prevalence and risk factors for obesity in adult cats from private US veterinary practices. Intern J Appl Res Vet Med 2005; 3: 88–96. [Google Scholar]
- 41.Morris JG. Idiosyncratic nutrient requirements of cats appear to be diet induced evolutionary adaptations. Nutr Rev 2002; 15: 153–68. [DOI] [PubMed] [Google Scholar]
- 42.Robertson SA. Anesthesia for the elderly cat. AAFP Fall Meeting Proceedings; 2006. Oct 22–24; Toronto, Canada.
- 43.Brodbelt DC, Pfeiffer DU, Young LE, Wood JL. Risk factors for anaesthetic-related death in cats: results from the confidential enquiry into perioperative small animal fatalities (CEPSAF). Br J Anaesth 2007; 99: 606–8. [DOI] [PubMed] [Google Scholar]
- 44.Lefebvre HP, Toutain PL. Angiotensin converting enzyme inhibitors in the therapy of renal diseases. J Vet Pharmacol Ther 2004; 27: 265–81. [DOI] [PubMed] [Google Scholar]
- 45.Carpenter RE, Pettifer GR, Tranquilli WJ. Anesthesia for geriatric patients. Vet Clin North Am Small Anim Pract 2005; 35: 571–80. [DOI] [PubMed] [Google Scholar]
- 46.Maggio F, DeFrancesco TC, Atkins CE, Pizzirani S, Gilger BC, Davidson MG. Ocular lesions associated with systemic hypertension in cats: 69 cases (1985–1998). J Am Vet Med Assoc 2000; 217: 695–702. [DOI] [PubMed] [Google Scholar]
- 47.Jepson RE, Elliott J, Brodbelt D, Syme HM. Effect of control of systolic blood pressure on survival in cats with systemic hypertension. J Vet Intern Med 2007; 21: 402–9. [DOI] [PubMed] [Google Scholar]
- 48.Polzin DJ. Guidelines for conservatively treating chronic kidney disease. Vet Med 2007; Dec: 788–99. [Google Scholar]
- 49.Sparkes AH. Chronic renal failure in the cat. Proceedings of the WSAVA Congress, 2006. www.ivis.org/proceedings/wsava/2006/lecture11/sparkes1.pdf.
- 50.Polzin DJ, Osborne CA, Ross SJ. Evidence-based management of chronic kidney disease. In: Bonagura J, ed. Current veterinary therapy XIV. Philadelphia, WB Saunders, 2009: 872–79. [Google Scholar]
- 51.Ross J, Osborne C, Kirk C, Lowry S, Koehler L, Polzin D. Clinical evaluation of dietary modification for treatment of spontaneous chronic kidney disease in cats. J Am Vet Med Assoc 2006; 229: 949–57. [DOI] [PubMed] [Google Scholar]
- 52.Plantinga EA, Everts H, Kastelein A, Beynen AC. Retrospective study of the survival of cats with acquired chronic renal insufficiency offered different commercial diets. Vet Rec 2005; 157: 185–87. [DOI] [PubMed] [Google Scholar]
- 53.Elliott DA. Nutritional management of chronic renal disease in dogs and cats. Vet Clin North Am Small Anim Pract 2006; 36: 1377–84. [DOI] [PubMed] [Google Scholar]
- 54.Elliott J, Rawlings JM, Markwell PJ, Barber PJ. Survival of cats with naturally occurring chronic renal failure: effect of dietary management. J Small Anim Pract 2000; 41: 235–42. [DOI] [PubMed] [Google Scholar]
- 55.Harte JG, Markwell PJ, Moraillon R, Gettinby GG, Smith BH, Wills JM. Dietary management of naturally occurring chronic renal failure in cats. J Nutr 1994; 124: 2660S. [DOI] [PubMed] [Google Scholar]
- 56.Strombeck D. Home-prepared dog and cat diets: the healthful alternative. Iowa State Press, 1999. [Google Scholar]
- 57.Peterson ME. Diagnostic methods for hyperthyroidism. In: August J. Consultations in feline internal medicine, 5th edn. St Louis, Elsevier Saunders, 2005: 191–97. [Google Scholar]
- 58.Norsworthy GD, Adams VJ, McElhaney MR, Milios JA. Relationship between semi-quantitative thyroid palpation and total thyroxine concentration in cats with and without hyperthyroidism. J Feline Med Surg 2002; 4: 139–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Norsworthy GD, Adams VJ, McElhaney MR, Milios JA. Palpable thyroid and parathyroid nodules in asymptomatic cats. J Feline Med Surg 2002; 4: 145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ferguson DC, Freedman R. Goiter in apparently euthyroid cats. In August J. Consultations in feline internal medicine, 5th edn. St Louis, Elsevier Saunders, 2005: 207–15. [Google Scholar]
- 61.Peterson ME, Melián C, Nichols R. Measurement of serum concentrations of free thyroxine, total thyroxine, and total triiodothy-ronine in cats with hyperthyroidism and cats with nonthyroidal disease. J Am Vet Med Assoc 2001; 218: 529–36. [DOI] [PubMed] [Google Scholar]
- 62.Broome MR. Thyroid scintigraphy in hyperthyroidism. Clin Tech Small Anim Pract 2007; 21: 10–16. [DOI] [PubMed] [Google Scholar]
- 63.Bruyette D. Choosing the best tests to diagnose feline hyper-thyroidism. Vet Med 2004; Nov: 956–62. [Google Scholar]
- 64.Becker TJ, Graves TK, Kruger JM, Braselton WE, Nachreiner RF. Effects of methimazole on renal function in cats with hyperthyroidism. J Am Anim Hosp Assoc 2000; 36: 215–23. [DOI] [PubMed] [Google Scholar]
- 65.Graves TK, Olivier NB, Nachreiner RF, Kruger JM, Walshaw R, Stickle RL. Changes in renal function associated with treatment of hyperthyroidism in cats. Am J Vet Res 1994; 55: 1745–49. [PubMed] [Google Scholar]
- 66.Sartor LL, Trepanier LA, Kroll MM, Rodan I, Challoner L. Efficacy and safety of transdermal methimazole in the treatment of cats with hyperthyroidism. J Vet Intern Med 2004; 18: 651–55. [DOI] [PubMed] [Google Scholar]
- 67.Lécuyer M, Prini S, Dunn ME, Doucet MY. Clinical efficacy and safety of transdermal methimazole in the treatment of feline hyperthyroidism. Can Vet J 2006; 47: 131–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Trepanier L. Transdermal drugs: what do we know? Proceedings of the ABVP practitioners' symposium; 2005. April 29-May 1; Washington DC, USA.
- 69.Trepanier LA. Pharmacologic management of feline hyper-thyroidism. Vet Clin North Am Small Anim Pract 2007; 37: 775–88. [DOI] [PubMed] [Google Scholar]
- 70.Rand JS, Marshall R. Diabetes mellitus in cats. Vet Clin North Am Small Anim Pract 2005; 35: 211–24. [DOI] [PubMed] [Google Scholar]
- 71.Weaver KE, Rozanski EA, Mahony OM, Chan DL, Freeman LM. Use of glargine and lente insulins in cats with diabetes mellitus. J Vet Intern Med 2006; 20: 234–38. [DOI] [PubMed] [Google Scholar]
- 72.Behrend EN. Update on drugs used to treat endocrine disease in small animals. Vet Clin North Am Small Anim Pract 2006; 36: 1087–105. [DOI] [PubMed] [Google Scholar]
- 73.Prahl A, Guptill L, Glickman NW, Tetrick M, Glickman LT. Time trends and risk factors for diabetes mellitus in cats presented to veterinary teaching hospitals. J Feline Med Surg 2007; 9: 351–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McCann TM, Simpson KE, Shaw DJ, Butt JA, Gunn-Moore DA. Feline diabetes mellitus in the UK: the prevalence within an insured cat population and a questionnaire-based putative risk factor analysis. J Feline Med Surg 2007; 9: 289–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Reusch C, Kley S, Casella M. Home monitoring of the diabetic cat. J Feline Med Surg 2006; 8: 119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Casella M, Reusch CE. Home monitoring of blood glucose in cats with diabetes mellitus; evaluation over a 4-month period. J Feline Med Surg 2005; 7: 163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alt N, Kley S, Haessig M, Reusch CE. Day-to-day variability of blood glucose concentration curves generated at home in cats with diabetes mellitus. J Am Vet Med Assoc 2007; 230: 1011–17. [DOI] [PubMed] [Google Scholar]
- 78.Bennett N, Greco DS, Peterson ME, Kirk C, Mathes M, Fettman MJ. Comparison of a low carbohydrate-low fiber diet and a moderate-high fiber diet in the management of feline diabetes mellitus. J Feline Med Surg 2006; 8: 73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reusch C, Wess G, Casella M. Home monitoring of blood glucose. Proceedings of the 20th Annual ACVIM Forum; 2002. May 29-June 1; Dallas, Texas, USA.
- 80.Stumpf JL, Lin SW. Effect of glucosamine on glucose control. Ann Pharmacother 2006; 40: 694–98. [DOI] [PubMed] [Google Scholar]
- 81.Forman A, Marks SL, de Cock HEV, et al. Evaluation of serum feline pancreatic lipase immunoreactivity and helical computed tomography versus conventional testing for the diagnosis of feline pancreatitis. J Vet Intern Med 2004; 18: 807–15. [DOI] [PubMed] [Google Scholar]
- 82.Steiner JM, Williams DA. Serum feline trypsin-like immunoreac-tivity in cats with exocrine pancreatic insufficiency. J Vet Intern Med 2000; 14: 627–29. [DOI] [PubMed] [Google Scholar]
- 83.Parent C, Washabau RJ, Williams DA. Serum trypsin-like immunoreactivity, amylase and lipase in the diagnosis of feline acute pancreatitis [abstract]. J Vet Intern Med 1995; 9: 194. [Google Scholar]
- 84.Salvadori C, Cantile C, De Ambrogi G, Arispici M. Degenerative myelopathy associated with cobalamin deficiency in a cat. J Vet Med A Physiol Pathol Clin Med 2003; 50: 292–96. [DOI] [PubMed] [Google Scholar]
- 85.Day MJ, Bilzer T, Mansell J, et al. Histopathological standards for the diagnosis of GI inflammation in endoscopic biopsy samples from the dog and cat: a report from the WSAVA GI Standardization Group. J Comp Pathol 2008; 138 (suppl 1): 1–43. [DOI] [PubMed] [Google Scholar]
- 86.Baez JL, Michel KE, Sorenmo K, Shofer FS. A prospective investigation of the prevalence and prognostic significance of weight loss and changes in body condition in feline cancer patients. J Feline Med Surg 2007; 9: 411–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kiselow MA, Rassnick KM, McDonough SP, et al. Outcome of cats with low-grade lymphocytic lymphoma: 41 cases (1995–2005). J Am Vet Med Assoc 2008; 232: 405–10. [DOI] [PubMed] [Google Scholar]
- 88.Milner RJ, Peyton J, Cooke K, et al. Response rates and survival times for cats with lymphoma treated with the University of Wisconsin-Madison chemotherapy protocol: 38 cases (1996–2003). J Am Vet Med Assoc 2005; 7: 1118–22. [DOI] [PubMed] [Google Scholar]
- 89.Tzannes S, Hammond MF, Murphy S, Sparkes A, Blackwood L. Owners' perception of the cats' quality of life during COP chemotherapy for lymphoma. J Feline Med Surg 2008; 10: 73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hellyer P, Rodan I, Brunt J, Downing R, Hagedorn J, Robertson S. AAHA-AAFP pain management guidelines for dogs and cats. J Am Anim Hosp Assoc 2007; 43: 235–48. [DOI] [PubMed] [Google Scholar]
- 91.Godfrey DR. Osteoarthritis in cats: a retrospective radiological study. J Small Anim Pract 2005; 46: 425–29. [DOI] [PubMed] [Google Scholar]
- 92.Clarke SP, Mellor D, Clements DN, et al. Prevalence of radiographic signs of degenerative joint disease in a hospital population of cats. Vet Rec 2005; 157: 793–99. [DOI] [PubMed] [Google Scholar]
- 93.Ingelheim Boehringer. New survey highlights behavioural changes are key to identifying arthritis in cats. UK Vet 2007; 12(6): 26–7. [Google Scholar]
- 94.Beale BS. Use of nutraceuticals and chondroprotectants in osteoarthritic dogs and cats. Vet Clin North Am Small Anim Pract 2004; 34: 271–89. [DOI] [PubMed] [Google Scholar]
- 95.Gunew MN, Menrath VH, Marshall RD. Long-term safety, efficacy and palatability of oral meloxicam at 0.01–0.03 mg/kg for treatment of osteoarthritic pain in cats. J Feline Med Surg 2008; 10: 235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sparkes A. Feline osteoarthritis - an important, but under-recognised, condition. Hill's Clinical Update, Issue 6, 2006: 3–6.
- 97.Head E, Das P, Sarsoza F, Poon W, et al. b-Amyloid deposition and tau phosphorylation in clinically characterized aged cats. Neurobiol Aging 2005; 26: 749–63. [DOI] [PubMed] [Google Scholar]
- 98.Porter VR, Buxton WG, Fairbanks LA, et al. Frequency and characteristics of anxiety among patients with Alzheimer's disease and related dementias. J Neuropsychiatry Clin Neurosci 2003; 15: 180–86. [DOI] [PubMed] [Google Scholar]
- 99.Landsberg G. Behavior problems of older cats. In: Schaumburg I, ed. Proceedings of the 135th annual meeting of the American Veterinary Medical Association, 1998: 317–20. [Google Scholar]
- 100.Gunn-Moore DA, McVee J, Bradshaw JM, Pearson GR, Head E, Gunn-Moore FJ. b-Amyloid and hyper-phosphorylated tau deposition in cat brains. J Feline Med Surg 2006; 8: 234–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gunn-Moore DA, Moffat K, Christie LA, Head E. Cognitive dysfunction and the neurobiology of aging in cats. J Small Anim Pract 2007; 48: 546–53. [DOI] [PubMed] [Google Scholar]
- 102.Milgram NW, Head E, Zicker SC, Ikeda-Douglas C. Long-term treatment with antioxidants and a program of behavioral enrichment reduces age-dependent impairment in discrimination and reversal learning in beagle dogs. Exp Gerontol 2004; 39: 753–65. [DOI] [PubMed] [Google Scholar]
- 103.Milgram NW, Head E, Zicher SC. Learning ability in aged Beagle dogs is preserved by behavioural enrichment and dietary fortification: a two year longitudinal study. Neurobiol Aging 2005; 26: 77–90. [DOI] [PubMed] [Google Scholar]
- 104.Crowell-Davis SL. Cognitive dysfunction in senior pets. Compend Contin Educ Pract Vet 2008; 30: 106–10. [PubMed] [Google Scholar]
- 105.Landsberg G. Therapeutic options for cognitive decline in senior pets. J Am Anim Hosp Assoc 2006; 42: 407–13. [DOI] [PubMed] [Google Scholar]
- 106.Landsberg G, Araujo JA. Behavior problems in geriatric pets. Vet Clin North Am Small Anim Pract 2005; 35: 675–98. [DOI] [PubMed] [Google Scholar]
- 107.Landsberg GL, Hunthausen W, Ackerman L. The effects of aging on behavor in senior pets. In: Handbook of behavior problems in the dog and cat, 2nd edn. London: WB Saunders, 2003: 269–304. [Google Scholar]
- 108.Studzinski CM, Araujo JA, Milgram NW. The canine model of human cognitive aging and dementia: pharmacological validity of the model for assessment of human cognitive-enhancing drugs. Prog Neuropsychopharmacol Biol Psychiatry 2005; 29: 489–98. [DOI] [PubMed] [Google Scholar]
- 109.Mansfield CS, Jones BR. Review of feline pancreatitis part two: clinical signs, diagnosis and treatment. J Feline Med Surg 2001; 3: 125–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Forcada Y, German AJ, Noble PJ, et al. Determination of serum fPLI concentrations in cats with diabetes mellitus. J Feline Med Surg 2008; 10: 480–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xenoulis PG, Suchodolski JS, Steiner JM. Chronic pancreatitis in dogs and cats. Compend Contin Educ Pract Vet 2008; 30: 166–80. [PubMed] [Google Scholar]
- 112.Peterson ME, Gamble DA. Effect of nonthyroidal illness on serum thyroxine concentrations in cats: 494 cases. J Am Vet Med Assoc 1990; 197: 1203–8. [PubMed] [Google Scholar]
- 113.Wakeling J, Moore K, Elliott J, Syme H. Diagnosis of hyper-thyroidism in cats with mild chronic kidney disease. J Small Anim Pract 2008; 49: 287–94. [DOI] [PubMed] [Google Scholar]
- 114.Crenshaw KL, Peterson ME. Pretreatment clinical and laboratory evaluation of cats with diabetes mellitus: 104 cases (1992–1994). J Am Vet Med Assoc 1996; 209: 943–49. [PubMed] [Google Scholar]
- 115.Reusch CE, Tomsa K. Serum fructosamine concentration in cats with overt hyperthyroidism. J Am Vet Med Assoc 1999; 215: 1297–300. [PubMed] [Google Scholar]
- 116.Rollin BE. Ethical issues in geriatric feline medicine. J Feline Med Surg 2007; 9: 326–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chun R, Garret L. Communicating with oncology clients. Vet Clin North Am Small Anim Pract 2007; 37: 1013–22. [DOI] [PubMed] [Google Scholar]