Introduction
Cutaneous collagenous vasculopathy (CCV) is an uncommon yet likely underreported idiopathic microangiopathy, first described in 2000 [1]. The disorder is characterized by progressive, asymptomatic cutaneous telangiectasias associated with collagen IV deposition around the affected vessels in the superficial dermis [1]. CCV may mimic other telangiectatic disorders, particularly generalized essential telangiectasia (GET) or pigmented purpuric dermatoses.
Case Presentation
A 50-year-old male presented with progressive patchy erythematous/telangiectatic non-atrophic macules symmetrically distributed over extensor aspects of arms and forearms that had developed over the previous three years (Figure 1A, B). He had no history of sunburns, occupational sun exposure, radiation, topical glucocorticosteroid application, hypertension, alcohol abuse, or of taking any medications. However, he has been a car parts reseller and thus, reportedly frequently used lacquer thinner (toluene-acetone solution) and vehicle paint.
Figure 1.
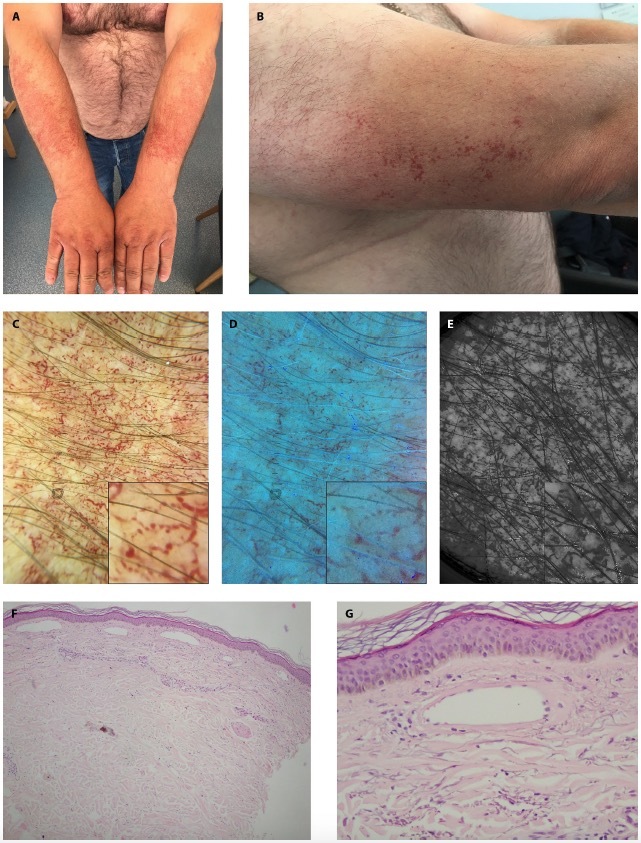
Clinical presentation of erythematotelangiectatic macules distributed over extensor surfaces of the arms and forearms in 50-year-old male (A, B).
Contact polarized dermatoscopic image (DL5, Dermlite, US) of the lesion displays a vascular pattern of thick linear serpentine vessels with alternating regions of constrictions and dilations (a sausage-string appearance) of reticular/polygonal arrangement (better seen in the box) (C).
Ultraviolet-induced fluorescence dermatoscopy (365nm) (DL5, Dermlite, US) demonstrates vascular constrictions and dilations (a sausage-string appearance) of reticular/polygonal arrangement along with darkening of perivascular structureless areas (higher absorption of UV spectrum by hemoglobin) suggestive of underlying endothelial dysfunction and erythrocyte extravasation (better seen in the box) (D).
Sub-ultraviolet reflectance dermatoscopy (405nm)(DZ-D100, Casio, Japan) exhibits hyporeflective linear serpentine reticular/polygonal vessels with indistinct contours (higher absorption of UV spectrum by hemoglobin) suggestive of underlying endothelial dysfunction and erythrocyte extravasation (better seen in the box) (E).
Pathology displays thinned epidermis with reduced papillomatosis, numerous dilated vessels of the superficial vascular plexus (no perivascular infiltrate noted), and fragmented elastin fibers in the upper dermis that could support the diagnosis of both generalized essential telangiectasia and cutaneous collagenous vasculopathy (F), but thickened hyalinized walls of the vessels support the diagnosis of the CCV (G).
Figure 2.
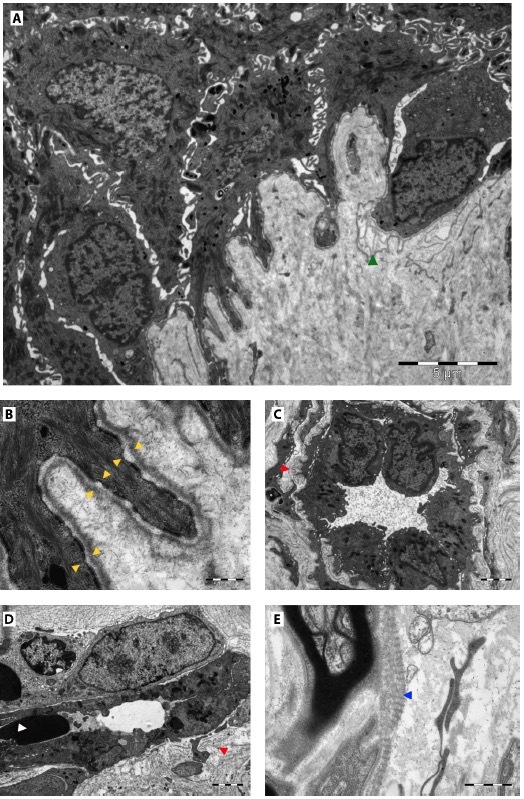
Electron microscopy reveals focally disrupted hemidesmosomal internal/external plates in the basal layer (yellow arrowheads) with focal multiplication of basal lamina (green arrowhead) (A, B), mild dilation of superficial dermal vessels exhibiting multi-laminated and focally deformed basal laminas (suggestive for cutaneous collagenous vasculopathy) (red arrowheads) (C), and increased activity of endothelial cells. Perivascular lymphocytes and single extravasated erythrocytes can be noted (white arrowhead) (D). Focal abnormally banded (long-spaced) collagen (Luse-like bodies) in the vicinity of sensory receptors is suggestive for the diagnosis of CCV (blue arrowhead) (E).
Based on the clinical presentation, GET (bilateral nevoid variant), telangiectasia macularis eruptiva perstans, and CCV were considered as possible differentials.
Complete blood count, ESR, aminotransferases, fasting glucose, lipid profile, serum tryptase levels, thyroid hormones, estrogen and progesterone levels, and abdominal ultrasound were within the normal limits.
Contact polarized conventional, ultraviolet-induced fluorescence (UVFD) and sub-ultraviolet reflectance dermatoscopic (sUVRD) imaging were performed (Figure 1C). Diagnostic biopsy was evaluated with pathology (Figure 1D, E) and electron microscopy (Figure 1F, G).
Discussion
There is a certain clinical and pathological overlap between CCV and GET. Thus, the diagnosis can only be made with electron microscopy (CCV featuring multiplication and deformation of vascular basal lamina and the presence of Luse-like bodies) [1, 3], as was in our case. Here we describe a dermatoscopic pattern of alternated vascular constrictions and dilations (sausage-like appearance) which has not yet been observed in CCV [1, 4] and which may hint at endothelial instability [2]. Although non-contact polarized dermatoscopy is a gold standard in inflammoscopy, contact mode with 70% alcohol solution produced a crisper image of the vessels in all dermatoscopy subtypes due to the reduction of stratum corneum reflection. Although there were no dermatoscopic or histopathologic clues to erythrocyte extravasation, UVFD and sUVRD could support it with perivascular hyporeflective areas, which was confirmed with electron microscopy. We hypothesize that disruption of vascular integrity in the reported patient could possibly result from prolonged exposure to aromatic volatile organic chemical compounds present in paint thinners, especially toluene. This substance, constituting 80% of paint thinner, has been reported to upregulate TNFα levels [5] responsible for the production of reactive oxygen species. Abrupt cutoff of telangiectatic macules sparing the hands was likely associated with the use of protective gloves.
Conclusions
CCV is a clinically challenging entity associated with endothelial damage. Even though the diagnosis can be reached with electron microscopic studies, it is possible that it may present characteristic dermatoscopic, UVFD, and sUVRD clues that may aid the diagnosis and make it technically easier and affordable.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Sartori DS, Almeida HL, Jr, de Dorn TV, Ruas CP. Cutaneous collagenous vasculopathy: light and transmission electron microscopy. An Bras Dermatol. 2019;94(2):211–3. doi: 10.1590/abd1806-4841.20198166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobsen JC, Beierholm U, Mikkelsen R, Gustafsson F, Alstrøm P, Holstein-Rathlou NH. “Sausage-string” appearance of arteries and arterioles can be caused by an instability of the blood vessel wall. Am J Physiol Regul Integr Comp Physiol. 2002;283(5):R1118–30. doi: 10.1152/ajpregu.00006.2002. [DOI] [PubMed] [Google Scholar]
- 3.Salama SS. Cutaneous collagenous vasculopathy: a new case series with clinicopathologic and ultrastructural correlation, literature review, and insight into the pathogenesis. Am J Dermatopathol. 2015 May;37(5):368–75. doi: 10.1097/DAD.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 4.Knöpfel N, Martín-Santiago A, Saus C, Escudero-Góngora MM, Del Pozo LJ, Gómez C. Extensive Acquired Telangiectasias: Comparison of Generalized Essential Telangiectasia and Cutaneous Collagenous Vasculopathy. Actas Dermosifiliogr. 2017;108(3):e21–e26. doi: 10.1016/j.ad.2016.02.020. English, Spanish. [DOI] [PubMed] [Google Scholar]
- 5.Abouee-Mehrizi A, Rasoulzadeh Y, Kazemi T, Mehdipour A, Mesgari-Abbasi M. Toxicopathological changes induced by combined exposure to noise and toluene in New Zealand White rabbits. Arh Hig Rada Toksikol. 2022;73(1):31–42. doi: 10.2478/aiht-2022-73-3602. [DOI] [PMC free article] [PubMed] [Google Scholar]


