When, in the summer of 1994, a pilot project on prevention of drug use and transmission of HIV was launched in Hindelbank, a Swiss prison for women, not many outsiders paid attention to it. Yet only a few months later, the prison director received repeated calls from television stations, newspapers, and drug experts asking how the project was developing. We describe how this high level of public interest in a small prison (around 85 inmates, 100 entries and releases per year) came about.
Summary points
Prisons play a pivotal role in the spread of infectious diseases
Distribution of syringes reduces drug-related harm in the community, but its effect in prisons has not been reported
Automatic syringe exchange dispensers were installed in a Swiss prison for women in the framework of a pilot project on drug and HIV prevention
Ongoing evaluation provided some evidence that syringe distribution in prison did not encourage drug consumption, and syringe sharing among inmates virtually disappeared
Other prisons in Switzerland and Germany are conducting prevention projects that include syringe distribution
Provision of syringes—the cutting edge?
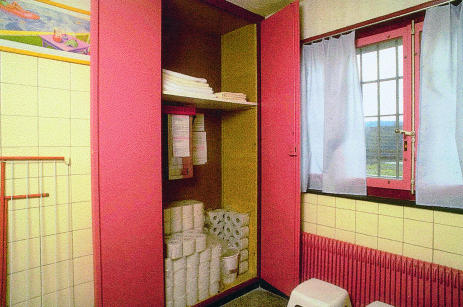
The installation of six automatic dispensers for exchange of syringes attracted special attention. The dispensers are freely accessible but hidden from general view in different wings of the prison (fig 1). Clean injection equipment is dispensed only in exchange for another (used) syringe. The first exchange is by means of a dummy syringe that is given to all inmates when they enter the prison.
To distribute equipment for illegal drug use in the framework of a penitentiary—and to provide inmates, many of whom have been sentenced for drug related crimes, with syringes—seemed paradoxical to many people. Fears abounded that inmates could misuse contaminated syringes as weapons against the prison’s staff or that improper disposal of injection equipment would provoke injuries and thus cause infections with bloodborne viruses. There was—and still is—speculation that issuing syringes to drug addicts in prison might encourage drug use.1
Development of harm reduction measures in Swiss prisons
Harm reduction is a familiar concept in Swiss prisons. The first measures for reducing drug related harm were introduced after cases of unexplained lymphadenopathy and weight loss were reported in drug misusers in some larger Swiss prisons in 1984 and tests showed HLTV-III antibodies in prisoners in 1985: information leaflets for inmates and staff and condoms for inmates have been available since 1985 in an increasing number of prisons. From 1989, a “hygiene kit” was distributed to prisoners on entry to Regensdorf penitentiary, containing condoms, disinfectant, and instructions on cleaning syringes. Oral methadone maintenance in a special section of the same prison became possible in 1989 and was introduced in 1991 in several remand prisons in Basel, Bern, Geneva, and Zurich. Since 1990, disinfectants have been available in the remand prison in Geneva.2 But when the introduction of syringe distribution in prisons was broached, the parting of the ways began. The issue became highly controversial despite sound recommendations by both the World Health Organisation and the Council of Europe postulating the principle of equivalence (providing the same health prevention and treatment in prison as is available outside).3,4
Progression of harm reduction strategies in prison—good public health policy
The need to apply the principle of equivalence emerged in the mid-80s with the first cases of HIV positivity in prisoners. The prevalence of HIV and AIDS is higher in prison than in the community in many countries, as is the prevalence of viral hepatitis, especially hepatitis C, which is increasingly recognised as a major risk for drug users.5–8 Drug misusers are overrepresented in the prison population, and prison presents a particular environment. Because of risk behaviours, such as syringe sharing and unprotected sexual contacts, the prevalence of HIV and hepatitis is higher in drug users.9–12 Studies of drug use and risk behaviours in prisons reveal worrying statistics,13 and there is evidence for HIV transmission in prison.14,15 Prisons play a pivotal role in the spread of HIV and viral hepatitis. Because there is a constant flow in and out of prison, the risks concern the whole community, not just a limited circle of prisoners.8,16 Implementing harm reduction measures in prison must be considered as an essential part of public health policy.17
The Hindelbank project
Syringe distribution in the community has been accepted for some years. In many European cities drug misusers have easy access to sterile injection equipment. Used syringes and needles can be exchanged for clean sets at pharmacies, in “shooting galleries,” or anonymously by means of automatic dispensers. Providing drug misusers with sterile injection equipment is an efficient way of reducing the risk of infection.18–24
Against this background the health service of Hindelbank prison, faced with a high level of prisoners using and sharing syringes, requested the introduction of syringe distribution in the penitentiary. The Swiss federal office of public health, which had declared the principle of equivalence to be part of its health strategy, supported this request. Initially there was determined resistance by the cantonal authorities. (In Switzerland’s decentralised structure each canton is responsible for its prison system.) But staff in the federal office of public health maintained their commitment and worked well with the prison’s management. Finally, the political reservations were overcome—less as a result of a political plan than because of the pragmatic and tireless engagement of individuals, and because the project was to be evaluated scientifically. In 1994, the prevention programme—consisting of lectures and group sessions, sociomedical counselling, and distribution of condoms and sterile syringes by exchange dispensers—was implemented in Hindelbank prison.
Evaluation was conducted parallel to the prevention programme by an independent external group of experts. The principal instrument of the evaluation was structured personal interviews with inmates. Four interview campaigns were carried out: just before the prevention programme was launched and three, six, and 12 months afterwards. Interviews were offered in German, English, Spanish, and French (instruments were developed for this study). A total of 161 inmates were asked for an interview and 137 (85%) participated at least once. The evaluation data were supplemented by results of analysis of voluntary blood samples and by data from the prison files, collected after informed consent was received from the inmates concerned.
Results
Response in regard to the feasibility of syringe distribution in prison was entirely positive. Fears turned out to be unjustified. A total of 5335 syringes were distributed within the first year (0.2 per inmate per day) without operational or security problems.
There is some evidence that drug consumption in the prison did not rise. Comparison of interviews at the beginning of the project with the two intermediate measurements showed no systematic differences in the proportion of inmates using heroin or cocaine in prison, and at the end of the one year project the proportion of users among the interviewed inmates had decreased (χ2=3.5, P<0.1; table 1). All inmates who said they were using heroin or cocaine in prison said they had previously consumed these substances regularly (three times or more per week for at least one year).
Table 1.
Use of heroin or cocaine and syringe sharing in Hindelbank prison, Switzerland. Values are numbers (percentages) of interviewed prisoners
| Variable | Time of interview after launch of the project (months)
|
|||
|---|---|---|---|---|
| 0 (n=65) | 3 (n=49) | 6 (n=33) | 12 (n=57) | |
| Drug use | 25 (38) | 24 (49) | 12 (36) | 13 (23) |
| Intravenous drug use | 19 (29) | 18 (37) | 11 (33) | 9 (16) |
| Sharing syringe | 8 (8) | 5 (10) | 2 (6) | 1 (2) |
The sharing of used syringes among inmates virtually disappeared. At the beginning of the project, eight of 19 intravenous drug users said they had shared syringes with other people in the past month spent in prison, two of them with more than one person. After three months five (of 18) and at six months two (of 11) users reported sharing syringes. At the end of the project only one women, who had been imprisoned just before the interview, reported syringe sharing in prison (table 1).
The study confirmed the gloomy picture of continuing drug misuse in prison, as well as a high prevalence of bloodborne virus infections on entry. Most of the drug misusers found access to illegal drugs after being imprisoned: 53 of the 137 women interviewed (39%) reported heroin or cocaine intake the month before incarceration, and 85% (45/137) continued taking these substances in prison (table 2), most (37/45) by intravenous injection. Drug intake was related to duration of imprisonment (table 2). Serological testing on entry to the study showed high prevalences of HIV and hepatitis infection, comparable with international findings13,25–30: of 94 inmates who voluntarily underwent blood analysis on arrival, six were HIV positive. Almost half the women (45/94) were positive for hepatitis B virus (five of them were positive for hepatitis B virus IgM) and over a third (35/94) were positive for hepatitis C. Follow up tests just before release (n=51) showed that no women had become infected with HIV or viral hepatitis.
Table 2.
Relation of duration of imprisonment to consumption of heroin or cocaine, Hindlebank prison
| Consumption of heroin or cocaine | No | Yes |
|---|---|---|
| Ever regularly (n=62) | 62 (100) | 0 |
| During month before incarceration (n=62) | 11 (18) | 51 (82) |
| While incarcerated: | ||
| Interview <1 month after incarceration (n=24) | 17 (71) | 7 (29) |
| Interview 1-5 months after incarceration (n=17) | 5 (29) | 12 (71) |
| Interview >5 months after incarceration (n=21) | 2 (10) | 19 (90) |
As syringe provision for prisoners was known to be controversial, special attention was paid to giving clear information about the project’s background and results. Reports summarising the main outcomes were produced in German, French, and English and handed out to inmates and staff.31 The results were presented and discussed by evaluators and prison authorities at a media conference. Response of the media (local radio and television stations, newspapers, and magazines) was considerable, and reports were highly objective. An evaluation of the public response to the Hindelbank project was planned. To enable deeper debate among scientists, prison authorities, and politicians from different countries, an international conference on harm reduction in prison was held in February 1996.32 These measures replaced some speculations with facts and supported development and implementation of similar projects in other prisons.
The study showed that syringe distribution in the prison was feasible and that the intervention was successful, as well as confirming the ongoing need for effective prevention measures. As a result, the programme including syringe distribution has been instituted in Hindelbank prison.
Conclusion and outlook
Our findings are linked to specific conditions. Hindelbank prison is relatively small, and it is a prison for women. The study covered a small population. Furthermore, the structures of health systems and prison systems vary from country to country. Nevertheless, a lesson can be learned from the Swiss experience: in these circumstances syringe distribution can not only minimise harm related to drug intake but also reduce drug taking. Based on this, further experience should be gained in other settings. The role of prisons in the spread of infectious diseases must be taken into account when decisions about undertaking such projects are made.
Some harm reduction measures have been implemented in other Swiss prisons as a result of the Hindelbank project. Since 1995, the medical service of the Geneva remand prison has been authorised to exchange drug users’ syringes on request. In 1995, a feasibility study including prescription of heroin for controlled intravenous injection was started in Oberschöngrün prison, Solothurn canton, in the framework of the Swiss trial on heroin prescription.1 In a prison in Basel, methadone prescription for controlled intravenous application was made available in 1996,33 and a syringe dispenser was installed in the prison in Realta, Grisons canton, in February 1997. In Germany, provision of syringes and scientific evaluation are in operation (Hamburg34; Vechta and Groß-Hespe35), and comparable projects are in preparation in several other countries.
Replacing speculations concerning syringe distribution in prison by an evidence based health policy may facilitate reconsideration of harm reduction strategies in prison. However, these decisions are political, and it remains to be seen whether politicians are prepared to apply public health criteria to an environment for which the overriding philosophies are security, punishment, and social control.
Figure.
In Hindelbank prison, syringe dispensers are freely accessible but hidden from general view
Footnotes
Funding: The evaluation study was funded by the Swiss Federal Office of Public Health.
Conflict of interest: None.
References
- 1.Nelles J, Dobler-Mikola A, Kaufmann B. Provision of syringes and prescription of heroin in prison: the Swiss experience in the prisons of Hindelbank and Oberschöngrün. In: Nelles J, Fuhrer A, editors. Harm reduction in prison. Strategies against drugs, AIDS and risk behaviour. Bern: Lang; 1997. pp. 239–262. [Google Scholar]
- 2.Nelles J. The contradictory position of HIV-prevention in prison: Swiss experiences. Intl J Drug Policy. 1997;1:2–4. [Google Scholar]
- 3.World Health Organisation. Global programme on AIDS: WHO guidelines on HIV infection and AIDS in prison. Geneva: World Health Organisation; 1993. [Google Scholar]
- 4.Council of Europe. Recommendation no. R(93)6 of the Council of Ministers. Strasbourg: Council of Europe; 1993. [Google Scholar]
- 5.Brewer TF, Derrickson J. AIDS in prison: a review of epidemiology and preventive policy. AIDS. 1992;6:623–628. [PubMed] [Google Scholar]
- 6.Thomas PA, Moerings M, editors. AIDS in prison. Aldershot: Dartmouth; 1994. [Google Scholar]
- 7.Dolan K, Wodak A, Penny R. AIDS behind bars: preventing HIV spread among incarcerated drug injectors. AIDS. 1995;9:825–832. [PubMed] [Google Scholar]
- 8.Mahon N. New York inmates’ HIV risk behaviors: the implications for preventing policy and programs. Am J Public Health. 1997;86:1211–1215. doi: 10.2105/ajph.86.9.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Des Jarlais DC, Friedmann SR, Choopanya K, Vanichseni S, Ward TP. International epidemiology of HIV and AIDS among injecting drug users. AIDS. 1992;6:1053–1068. doi: 10.1097/00002030-199210000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Myers T, Millson M, Rigby J, Ennis M, Rankin J, Mindell W, et al. A comparison of the determinants of safe injecting and condom use among injecting drug users. Addiction. 1995;80:217–226. doi: 10.1046/j.1360-0443.1995.9022177.x. [DOI] [PubMed] [Google Scholar]
- 11.Stark K, Müller R, Wirth D, Bienzle U, Guggenmoss-Holzmann GP, Guggenmoss-Holzmann I. Determinants of HIV infection and recent risk behaviour among injecting drug users in Berlin by site of recruitment. Addiction. 1995;90:1367–1375. doi: 10.1046/j.1360-0443.1995.901013678.x. [DOI] [PubMed] [Google Scholar]
- 12.Stark K, Schreier E, Müller R, Wirth D, Driesel G, Bienzle U. Prevalence and determinants of anti-HCV seropositivity and of HCV genotype among intravenous drug users in Berlin. Scand J Infect Dis. 1995;27:331–337. doi: 10.3109/00365549509032726. [DOI] [PubMed] [Google Scholar]
- 13.Dolan K. AIDS, drugs and risk behaviour in prison: state of the art. In: Nelles J, Fuhrer A, editors. Harm reduction in prison. Strategies against drugs, AIDS and risk behaviour. Bern: Lang; 1997. pp. 213–238. [Google Scholar]
- 14.Dolan K, Hall W, Wodak A, Gaughwin M. Evidence of HIV transmission in an Australian prison. Med J Aust. 1994;160:734. [PubMed] [Google Scholar]
- 15.Taylor A, Goldberg D, Cameron S, Emslie J. Outbreak of HIV infection in a Scottish prison. BMJ. 1995;310:289–292. doi: 10.1136/bmj.310.6975.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harding TW. Do prisons need special health policies and programmes? In: Nelles J, Fuhrer A, editors. Harm reduction in prison. Strategies against drugs, AIDS and risk behaviour. Bern: Lang; 1997. pp. 161–180. [Google Scholar]
- 17.Gaiter J, Doll LS. Improving HIV/AIDS prevention in prisons is good public health policy. Am J Public Health. 1996;86:1201–1203. doi: 10.2105/ajph.86.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hart GJ, Carvell ALM, Woodward N, Johnson AM, Williams P, Parry JV. Evaluation of needle exchange in central London: behaviour change and anti-HIV status over one year. AIDS. 1989;3:261–265. [PubMed] [Google Scholar]
- 19.Hartgers C, Buning EC, von Santen GW, Verster AD, Coutinho RA. The impact of the needle and syringe-exchange programme in Amsterdam on injecting risk behaviour. AIDS. 1989;3:571–576. doi: 10.1097/00002030-198909000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Martin GS, Serpelloni G, Galvan U, Rizetto A, Gomma M, Morgante S. Behavioural change in injecting drug users: evaluation of an HIV/AIDS education program. AIDS Care. 1990;2:275–279. doi: 10.1080/09540129008257740. [DOI] [PubMed] [Google Scholar]
- 21.Stephens RS, Feucht TE, Roman SW. Effects of an intervention program on AIDS-related drug and needle behavior among intravenous drug users. Am J Public Health. 1991;81:568–571. doi: 10.2105/ajph.81.5.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dubois-Arber F, Barbey P. Evaluation der AIDS-Präventionsstratgie in der Schweiz: vierter zusammenfassender Bericht 1991-1992. Im Auftrag des Bundesamtes für Gesundheitswesen. Lausanne: Institut universitaire de médecine sociale et préventive; 1994. (Evaluation report prepared on behalf of of the Swiss Federal Office of Public Health.) [Google Scholar]
- 23.Coming clean about needle exchange. Lancet. 1995;346:1397. [PubMed] [Google Scholar]
- 24.Frischer M, Taylor A, Goldberg A, Elliott L. Direct evaluation of needle and syringe exchange programmes. Lancet. 1996;347:768. doi: 10.1016/s0140-6736(96)90121-x. [DOI] [PubMed] [Google Scholar]
- 25.Gaube J, Feucht HH, Laufs R, Polywka S, Fingscheidt E, Müller HE. Hepatitis A, B und C als desmoterische Infektionen. Gesundheitswesen. 1993;55:246–229. [PubMed] [Google Scholar]
- 26.Vlahov D, Nelson KE, Quinn TC, Kending N. Prevalence and incidence of hepatitis C virus infection among male prison inmates in Maryland. Eur J Epidemiol. 1993;9:566–569. doi: 10.1007/BF00209538. [DOI] [PubMed] [Google Scholar]
- 27.Crofts N, Steward T, Hearne P, Xin YP, Breschkin AM, Locarnini SA. Spread of bloodborne viruses among Australian prison entrants. BMJ. 1995;310:285–288. doi: 10.1136/bmj.310.6975.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anon C, del Olmo JA, Llovet F, Serra MA, Gilabert S, Rodriguez F, et al. Virus C de la hepatitis entre la poblacion penitenciaria de Valencia. Rev Esp Enferm Dig. 1995;87:505–508. [PubMed] [Google Scholar]
- 29.Ford PM, White C, Kaufmann H, MacTavish J, Pearson M, Ford S, et al. Voluntary anonymous linked study of the prevalence of HIV infection and hepatitis C among inmates in a Canadian federal penitentiary for women. Can Med Assoc J. 1995;153:1605–1609. [PMC free article] [PubMed] [Google Scholar]
- 30.Polych C, Sabo D. Gender politics, pain, and illness. The AIDS epidemic in North American prisons. In: Sabo DF, Gordon F, editors. Men’s health and illness. Thousand Oaks, CA: Sage; 1995. pp. 139–157. [Google Scholar]
- 31.Nelles J, Fuhrer A. Drug and HIV prevention at the Hindelbank penitentiary. Abridged report of the evaluation results. Mandated by the Swiss Federal Office of Public Health, Bern 1995. (Also available in German and French.)
- 32.Nelles J, Fuhrer A, editors. Harm reduction in prison. Strategies against drugs, AIDS and risk behaviour. Bern: Lang; 1997. [Google Scholar]
- 33.Nelles J, Fuhrer A. Kurzevaluation des Pilotprojekts Drogen- und Aidsprävention in den Basler Gefängnissen. Bern: Bundesamtes für Gesundheit, 1997.
- 34.Pape U, Böttger A, Pfeiffer C. Hannover: Kriminologisches Forschungsinstitut Niedersachsen; 1996. Wissenschaftliche Begleitung und Beurteilung des geplanten Spritzentauschprogramms im Rahmen eines Modellversuchs der Justizbehörde der Freien Hansestadt Hamburg. Konzeption eines empirischen Forschungsprojekts. (Forschungsbericht Nr 54.) [Google Scholar]
- 35.Meyenberg R, Stöver H, Jacob J, Pospeschill M. Infektionsprophylaxe im Niedersächsischen Justizvollzug. Oldenburg: Bibliotheks- und Informationssystem der Universität Oldenburg, 1996.