Abstract
Background/aims
This retrospective multicentric panel study provides absolute numbers, types of and indications for corneal transplantation in Germany from 2011 to 2021 and sets them into the international context.
Methods
A questionnaire was sent to the 104 German ophthalmologic surgery departments and 93 (89%) provided their data.
Results
The number of reported keratoplasties more than doubled from 2011 (n=4474) to 2021 (n=8998). Lamellar keratoplasties (49% posterior (n=2883), 4% anterior (n=231)) surpassed penetrating keratoplasty (PKP, 47%, n=2721) for the first time in 2014. Since 2016, Descemet’s membrane endothelial keratoplasty (DMEK) has become the predominant keratoplasty procedure in Germany. Its number increased by 1.5-fold from 3850 (2016) to 5812 (2021). Main indications in 2021 were Fuchs’ endothelial corneal dystrophy (FECD, 43%), pseudophakic corneal decompensation (12%), repeated keratoplasty (11%), infections (7%), keratoconus (6%) and corneal scarring (4%, others: 9%). The PKP percentage decreased from 70.2% in 2011 (n=3141) to 31.7% in 2021 (n=2853). Descemet’s stripping (automated) endothelial keratoplasties (DSAEKs) decreased to 1% in 2021 (n=74). 98.6% of all posterior lamellar keratoplasties were DMEKs in Germany in 2021. The number of deep anterior lamellar keratoplasties (DALKs) remained comparable from 2011 (n=269) to 2021 (n=251, 2.8%).
Conclusion
Main indications for corneal transplantation in Germany (2021) were FECD and pseudophakic corneal decompensation. DMEK is by far the predominant corneal transplantation procedure since 2016 followed by PKP, whose absolute number decreased only slightly during the decade from 2011 to 2021. DALK proportions remain low, but stable, whereas DSAEK decreased annually and plays a minor role in Germany.
Trial registration number
Keywords: cornea, treatment surgery
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Lamellar keratoplasty procedures are on the rise. However, there exist different trends in the application of lamellar keratoplasty techniques worldwide.
WHAT THIS STUDY ADDS
This report summarises developments in Germany from 2011 to 2021 and sets them into the international context.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This report underlines the importance of Descemet’s membrane endothelial keratoplasty as a relatively novel surgical technique which is likely to become more widely adopted internationally.
Introduction
The beginnings of penetrating keratoplasty (PKP) date back to 1905 when Eduard Zirm performed the first successful full-thickness corneal transplantation1 and PKP became the gold standard of corneal transplantation during the twentieth century. However, refined lamellar grafting techniques adapted to the wide range of indications for corneal transplantation that are precisely tailored to the individual corneal disease patterns have been introduced and set new standards in the last two decades.2
Deep anterior lamellar keratoplasty (DALK) consists of a corneal donor transplantation without endothelium after complete removal of the pathological stroma down to Descemet’s membrane.3 4 Descemet’s stripping (automated) endothelial keratoplasty (DSAEK) is a posterior lamellar corneal transplantation applied in endothelial corneal diseases, and comprises the preparation and transplantation of an endothelial donor tissue that was prepared using a microkeratome and includes a stromal layer, Descemet’s membrane and the endothelium.5–7 Descemet’s membrane endothelial keratoplasty (DMEK) is defined by the isolated preparation and transplantation of Descemet’s membrane and corneal endothelium.8 Recent approaches that are designated as ‘Descemet’s stripping only’ (DSO) or ‘Descemetorhexis without endothelial keratoplasty’ (DWEK) aim to remove only the central Descemet’s membrane and endothelium without any transplantation.
This study aimed to assess and analyse the absolute numbers, percentages, surgical techniques of and indications for corneal transplantations performed in Germany during the decade from 2011 to 2021 as raised by data from the German Keratoplasty Registry of the Cornea Section of the German Ophthalmological Society (Deutsche Ophthalmologische Gesellschaft, DOG).
Methods
Data about keratoplasties performed in Germany have been collected by the Cornea Section of the German Ophthalmological Society (DOG, http://www.dog.org/die-dog/sektionen-dog-kornea) annually. A questionnaire asking for absolute numbers, surgical techniques of and indications for corneal transplantation has been sent each year to 104 ophthalmologic departments in Germany out of which 93 (89%) responded and provided their data in 2022.9 The 93 responses consisted of 36 (95%) of the 38 contacted chairmen of German university departments and 57 (86%) of the 66 contacted non-university-based heads of ophthalmologic departments in Germany. The study is a retrospective panel study (ideally) including all German patients treated with corneal transplantation from 2011 to 2021. It was registered at the public database ClinicalTrials.gov maintained by the U.S. National Institutes of Health and follows the principles of the declaration of Helsinki.
Results
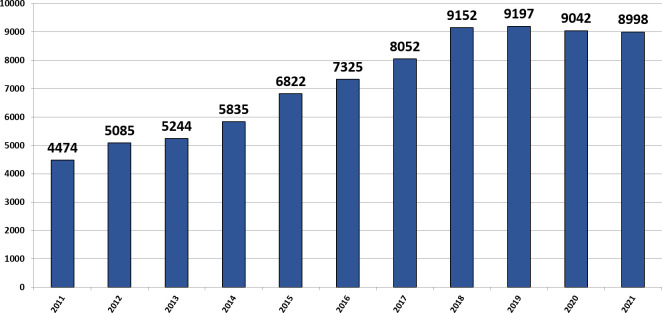
The number of reported keratoplasties increased from 4474 in 2011 to a maximum of 9197 in 2019 and slightly decreased to 8998 in 2021 (figure 1). The proportion of PKP performed annually decreased by more than half from 2011 (70.2%) to 2021 (31.7%, figure 2). Nevertheless, the absolute number of PKP decreased only slightly from 3141 (2011) to 2853 (2021) during the same period because of the overall increase of the number of corneal transplantations (figure 3).
Figure 1.
Absolute number of keratoplasties in Germany from 2011 to 2021. Increasing number of reported keratoplasties in Germany from 2011 (n=4474) to a maximum of n=9197 in 2019 followed by a slight decrease to n=8998 in 2021. The x-axis shows year; y-axis, number of reported corneal transplantations.
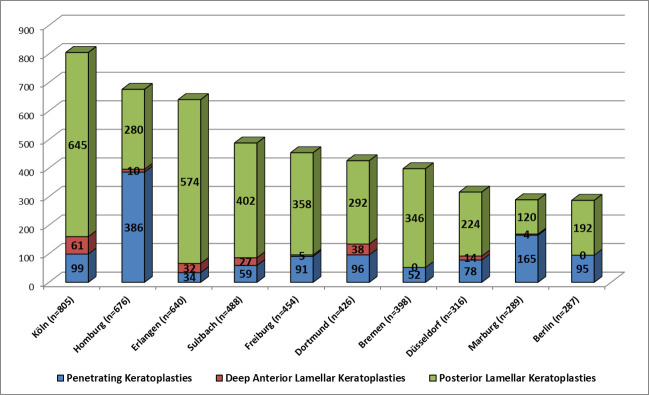
Figure 2.
Proportions of penetrating, anterior and posterior lamellar keratoplasties in Germany from 2011 to 2021. Proportions of penetrating keratoplasties (blue), deep anterior lamellar keratoplasties (red) and posterior lamellar keratoplasties (green) in Germany from 2011 to 2021. The x-axis shows year; y-axis, proportions of keratoplasty techniques.
Figure 3.
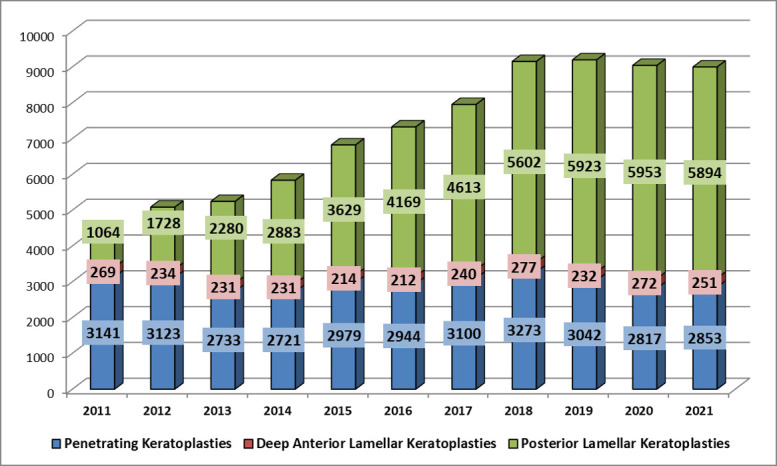
Absolute number of penetrating, anterior and posterior lamellar keratoplasties in Germany from 2011 to 2021. Absolute number of penetrating keratoplasties (blue), deep anterior lamellar keratoplasties (red) and posterior lamellar keratoplasties (green) in Germany from 2011 to 2021. The x-axis shows year; y-axis, absolute number of keratoplasties.
Lamellar procedures (49% posterior (n=2883) and 4% anterior (n=231)) surpassed PKP (47%, n=2721) from 2014 on (figures 2 and 3). The proportion of DALK remained comparatively low each year, with a minimum of 212 (2016) and a maximum of 277 (2018, figure 3). Overall, there was no major change from 2011 (n=269) to 2021 (n=251, figure 3) concerning anterior lamellar keratoplasties.
The number of DSAEK decreased from 10% in 2013 (n=507) to 1% in 2021 (n=77, figure 4). In contrast, the number of DMEK increased by 3.3-fold from 34% in 2013 (n=1773) to 65% in 2021 (n=5812, figure 4). Since 2016, DMEK has become the predominant keratoplasty procedure in Germany with 53%, 54%, 59%, 63%, 65% and 65% in 2016, 2017, 2018, 2019, 2020 and 2021, respectively (figure 4). Moreover, 98.6% of all posterior lamellar keratoplasties were performed as DMEKs in 2021 in Germany. With two exceptions, this development was reflected in the proportional distribution of the surgical procedures within the ten most active corneal transplantation centres in Germany (figure 5).
Figure 4.
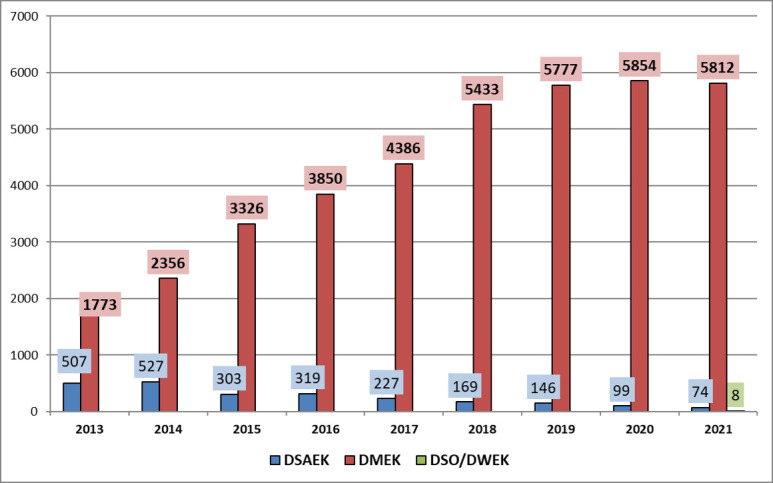
Absolute number of posterior lamellar keratoplasties in Germany from 2013 to 2021. Absolute number of Descemet's stripping automated endothelial keratoplasty (DSAEK, blue) vs Descemet’s membrane endothelial keratoplasty (DMEK) from 2013 to 2021 in Germany. DSAEK decreasing from 507 (10%) in 2013 to 74 (1%) in 2021. DMEK increasing by 3.3-fold from 1773 (34%) in 2013 to 5812 (65%) in 2021. DSO (Descemet’s stripping only) and DWEK (Descemetorhexis without endothelial keratoplasty) were reported in 2021 for the first time.
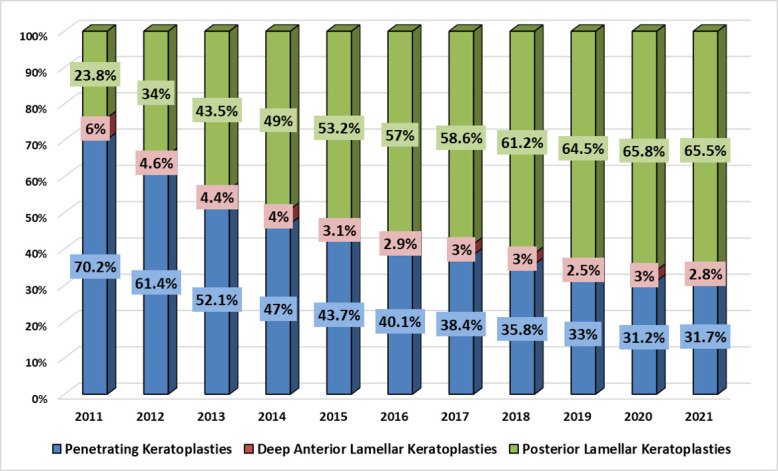
Figure 5.
Ten most active corneal transplantation centres in Germany (2021). The 10 most active corneal transplantation centres in Germany (2021) show a preponderance of posterior lamellar keratoplasties (exceptions: Homburg and Marburg).
Main indications for corneal transplantation in 2021 were Fuchs’ endothelial corneal dystrophy (FECD, 43%, increasing tendency since 2017), pseudophakic corneal decompensation (12%, stable), repeated keratoplasty (11%, increasing tendency since 2017), infections (7%, increasing tendency since 2017), keratoconus (6%, stable) and corneal scarring (4%, stable, others: 9%, figure 6).
Figure 6.
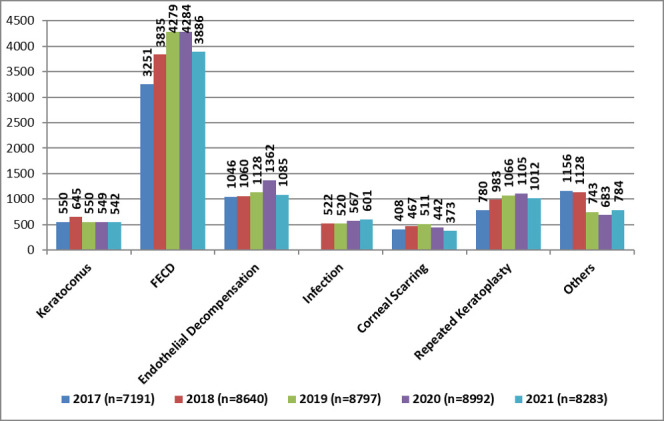
Main indications for keratoplasties in Germany from 2017 to 2021. Reported main indications for penetrating and lamellar corneal transplantations in Germany from 2017 to 2021. FECD, Fuchs’ endothelial corneal dystrophy.
The number of patients on German waiting lists for corneal transplantation reached a maximum in 2018 (n=5313) and decreased to 4627 in 2020 (figure 7). Based on the responses to the questionnaire for 2021, the average waiting time for PKP in Germany was 9 weeks (n=57 centres reported the waiting time), for DMEK 12 weeks (n=52 reported) and for DALK 13 weeks (n=22 reported).
Figure 7.
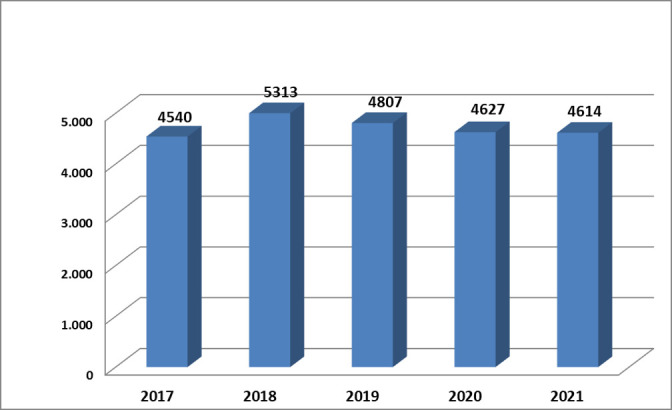
Waiting lists for corneal transplantation in Germany. Patients on waiting lists for corneal transplantation in Germany from 2017 to 2021, maximum of 5313 in 2018.
Discussion
This retrospective panel study summarises the developments in corneal transplantation in Germany during the decade from 2011 to 2021. FECD has become the major indication and DMEK is the most commonly applied transplantation procedure followed by PKP, which decreased only slightly (in absolute numbers) during this decade. The DALK and the posterior lamellar DSAEK procedure turned out to play minor roles in Germany.
These developments shall be put into the worldwide context in the following. For this purpose, published manuscripts and reports from cornea bank associations with data about corneal transplantation published from 2017 onwards were reviewed. A PubMed research was performed using the keywords ‘corneal transplant registry’ and ‘eye bank report’ for each country (each country was added after these keywords). It is therefore possible that existing reports not listed in PubMed or not written in English have been missed and were not included.
Europe
The European Cornea and Cell Transplantation Registry (ECCTR) collects data on corneal transplantation throughout Europe and published its first report in 2021 with 12 913 registered corneal transplantations in Europe in 2019.10 11 This report did not include data from Germany but data from 10 other European Union Member States, the UK and Switzerland,10 11 with the UK (n=7491) and the Netherlands (n=3083) reporting the highest number of corneal transplantations.10 11 Because of the limited participation among European Union Member States, the authors assumed a total of approximately 30 000 corneal transplantations for the reported period.10 11 The main diagnoses that required corneal transplantation were FECD (n=5325, 41%) followed by repeated graft (n=2108, 16%), pseudophakic bullous keratopathy (n=1594, 12%) and keratoconus (n=1506, 12%).10 11 These results present a similar distribution of the indication spectrum as in our report for Germany. Differences arise when looking at the corneal transplantation procedures. Whereas DMEK has been the predominant corneal transplantation procedure in Germany since 2016, the ECCTR report stated that the predominant corneal transplantation procedure in its European survey was DS(A)EK (n=5918, 46%), followed by PKP (n=3886, 30%) and DMEK only in third place (n=1838, 9%).10 11 In view of these results, one could conclude that Germany would have a certain pioneering role in Europe with regard to the introduction and application of DMEK. However, such interpretations must consider that this ECCTR report with data from 10 out of 27 European Union Member States cannot (yet) provide a complete and representative picture of corneal transplantation trends in Europe.
The Great Britain Organ and Tissue Donation and Transplantation Activity Report 2019/2020 stated accordingly that DS(A)EK (33%) was the predominant corneal transplantation procedure followed by PKP (29%), DMEK (25%) and (D)ALK (10%).12 The Italian Eye Bank Report 2020 reported similar results to our survey with more posterior lamellar than penetrating keratoplasties since 2016 and 1785 posterior lamellar, 1046 penetrating and 191 anterior lamellar keratoplasties in 2020 (total=3023).13
To satisfy the need of corneal transplantations, Europe also relies on the import of corneal grafts: The Eye Banking Statistical Report of the Eye Bank Association of America reported, for 2019, that a total of 1849 corneal grafts were exported to Europe (the majority of them to Germany, n=1290).14
North America
The Eye Banking Statistical Report of the Eye Bank Association of America reported 51 336 keratoplasties during 2019, composed of 30 650 posterior lamellar, 17 409 penetrating and 745 anterior lamellar keratoplasties.14 The proportion of posterior lamellar keratoplasty represented the majority (60%) and was composed of 17 428 DS(A)EK and 13 215 DMEK.14 For 2021, the majority of corneal transplantations were also posterior lamellar keratoplasties with the number of DMEK (n=14 128) gradually approaching, but not (yet) exceeding that of DS(A)EK (n=15 935).15 Although there were fewer corneal transplantations reported in 2021 (n=49 110) than 2019 (n=51 336) probably as a side-effect of the COVID-19 pandemic, the proportion of PKP remained almost the same (n=16 269, 33%).15 Despite a smaller total number of corneal transplantations in 2021, these numbers reveal a gradual trend towards DMEK (2019: 13 215; 2021: 14 128) and away from DSAEK (2019: 17 428; 2021: 15 935) for the USA.
As in the USA and in Germany, the Canadian Eye and Tissue Banking Statistics also reported the majority of corneal transplantations to be posterior lamellar procedures for 2020 (n=2264) followed by 845 penetrating and 106 anterior lamellar keratoplasties (total=3215).16 However, like in the USA, DSAEK dominated with 59% (n=1327) versus 41% DMEK (n=937) in view of posterior lamellar keratoplasty procedures.16
South America
The Organ Transplantation in Brazil Report indicated 14 943 corneal transplantations in Brazil for 2019 without, however, providing more detailed information on the transplantation techniques.17 An earlier study from Brazil reported a 2.3-fold increase of corneal transplantations from 6193 (2001) to 14 641 (2016) and the main indications for corneal transplantation to be keratoconus, followed by infectious keratitis, post-infectious scarring and pseudophakic bullous keratopathy during this period.18 Similar results for main indications were stated in a report from Colombia covering the period from 2010 to 2017. These were corneal ectasias, followed by pseudophakic bullous keratopathy and repeated graft.19 The most common technique was PKP (90%); however, a trend towards lamellar grafts was reported.19 A report from Mexico reported 4729 corneal transplantions from March 2019 to February 2021 without providing information about indications and techniques.20
Although there are fewer recent reports on corneal transplantation for the other South American countries, the export statistics of the USA can be used to draw conclusions about their transplantation activity: A total of 1499 corneal grafts were imported by South American countries, most of them to Argentina (n=377).14
Asia
A similar spectrum of indications as in South America was reported in a survey from the Islamic Republic of Iran covering the period from 1991 to 2017. It reported 95 057 corneal transplants with the underlying diagnoses keratoconus (40%) followed by pseudophakic bullous keratopathy (19%), corneal scarring (16%) and graft failure (8%).21 The most common transplant technique was PKP (70%) which decreased slightly in favour of DSAEK (12%) until 2017, while DMEK played almost no role until 2017 (<0.1%)21 as opposed to the development in Germany with DMEK being the most frequently applied corneal transplantation procedure at that time (54.4%). Anterior lamellar keratoplasty accounted for 14%, which is probably attributable to the main indication of corneal ectasia.21 An early report of the eye banks in India from 2013 to 2014 reported the main indications for corneal transplantation to be infections (n=3023) followed by pseudophakic bullous keratopathy (n=934).22 Furthermore, the predominant transplantation technique in this report was PKP (n=7920), followed by DS(A)EK (n=1245) and DALK (n=437).22 The absence of DMEK in this survey may be due to the timing of the survey. In comparison, however, there was no major change in the distribution of transplantation techniques in a single eye bank in Hyderabad (India) in 2018: PKP continued to be the predominant technique (n=2955) followed by 1508 posterior lamellar and 164 anterior lamellar keratoplasties,23 indicating that there had not yet been a transition towards lamellar procedures in this Indian eye bank equivalent to American or European conditions by the year 2018.
A survey from China reported an increase of corneal transplantations from 2014 (n=5377) to 2018 (n=8980) with main indications leukoma (21%), followed by bacterial keratitis (11%), dystrophies (11%), keratoconus (10%) and corneal perforation (8%).24 The authors attributed the differing spectrum of indications compared with the aforementioned countries and continents to the large agricultural population and lower cataract surgery rates, resulting in a higher susceptibility to corneal scarring and infections, which in turn led to the predominant technique of PKP (54%), followed by anterior lamellar (38%) and a quite small proportion of posterior lamellar keratoplasties (7%).24
The Eye Banking Statistical Report of the Eye Bank Association of America reported that 12 207 corneal grafts were exported to Asia in 2019 and that the largest importer was Japan (n=1999), followed by Pakistan (n=1800) and Saudi Arabia (n=1363).14
Australia
Like in South America and the Middle East (Iran), the main indication for corneal transplantation in New Zealand was keratoconus from 2010 to 2018 and was surpassed by repeated graft in 2019.25 During this period, the main surgical procedure was PKP (n=1703), followed by DS(A)EK (n=888), (D)ALK (n=266) and DMEK (n=98).25 Since nine times more DS(A)EK than DMEK have been carried out by 2020, this contrasts with the reverse development in Germany. The Australian Corneal Graft Registry 2020 reported 1831 conducted keratoplasties out of which 30% were PKP, 30% DMEK, 29% DS(A)EK, 8% DALK and 3% tectonic,26 indicating that DMEK has just surpassed DS(A)EK whereas it has not exceeded PKP. Main indications were keratoconus followed by repeated graft and pseudophakic bullous keratopathy and the authors stated that the number of corneal grafts for FECD tends to increase rapidly27 which might influence the ranking of the main indications in the years to come.
Africa
The basic problem in Africa is the lack of necessary infrastructure including cornea banks (apart from exceptions as, eg, the Gauteng Cornea and Eye Bank in South Africa).28 For this reason, corneal transplants have to be imported, which in turn raises the threshold for the indication and performance of keratoplasty and results in a lower number of corneal transplantations overall.29 30 Since the corneal transplants are to be imported and not every African country published reports about corneal transplantations, conclusions about the number of corneal transplantations in Africa can be drawn from the exporters’ data, for example, the Eye Banking Statistical Report of the Eye Bank Association of America. For 2019, it reported 10 711 donor corneas exported to Africa and the three most active countries in corneal transplantation were Egypt (n=5935), Djibouti (n=1409) and South Africa (n=851).14 Only a few recent reports exist from the individual African countries. One first survey reported 32 full-thickness grafts performed in Nigeria from 2008 to 2011.31 A second reported 118 PKP in Kenya from 2012 to 2014, which were mainly conducted because of keratoconus (66%) and corneal scarring (22%) with all donor tissues imported from the USA.29 One more recent survey reported 75 corneal transplantations in Ghana from 2014 to 2018 (n=60 PKP, 14 DS(A)EK, 1 DALK) after import of all transplants and the main underlying diagnoses stated were pseudophakic bullous keratopathy and keratoconus.30
Transition to DMEK in a global context
A worldwide review of PKP indications during the period of 1980 to 2014 reported FECD to be the fourth most common indication in North America and Europe.32 Much has changed since then and the proportion of posterior lamellar keratoplasties (mainly due to FECD) has already surpassed the number of PKP in many parts of the world, for example, in Germany (2021: 65%), in Europe (2019: 55%),10 11 in the USA (2021: 61%)15 and in Australia (2020: 59%),26 which is why the twenty-first century is sometimes being referred to as the lamellar age or century27 with regard to corneal transplantations techniques. While visual acuity may be affected after DSAEK by the shape and thickness of the graft or the stroma–stroma interface,33 DMEK is reported to result in better visual acuity outcomes and an even lower hyperopic shift.34 35 In terms of 5-year survival rates and endothelial cell loss rates, both procedures seem to be comparable.36 The American Academy of Ophthalmology confirmed a faster visual recovery and better visual outcome with DMEK when compared with DSAEK with an even lower endothelial rejection rate after DMEK than after DSAEK.37 Since DMEK donor preparation and transplantation in the recipient eye may be technically more challenging, the question arises why DSAEK is constantly underrepresented in Germany. In the German-language literature, it has been suggested that DSAEK should be used especially in eyes with a shallow anterior chamber,38 complex anterior segment pathologies (such as aphakia, larger iris defects, glaucoma implants, hypotonic eyes, eyes with silicone oil filling)39 or in children38 since the DSAEK lamella unfolds quasi-autonomously due to its inherent rigidity.40 For the treatment of endothelial corneal diseases, DMEK has been considered the standard of care in Germany,2 although the most important factor in deciding between DMEK and DSAEK remains the experience of the microsurgeon with one or the other surgical procedure.41 In view of these aspects, a further increase in the spread and number of DMEK conducted worldwide at the expense of DSAEK can be expected. However, prevalence and genetic studies about FECD found a higher frequency of FECD in Caucasians when compared with Asians.42 Geographical and ethnic differences in FECD prevalence may therefore affect the relative proportions of indications for and techniques of corneal transplantations throughout the world. One recent study concluded that DMEK became the leading technique for the cure of endothelial corneal diseases in Spain.33 Another reported 58% of keratoplasties in the Singapore National Eye Center to be endothelial keratoplasties with equal proportions of DSAEK (50%) and DMEK (50%).42 A survey among Canadian corneal surgeons revealed DMEK to be the preferred surgery method for endothelial corneal diseases.43 When comparing DMEK and DSAEK for the treatment of FECD and pseudophakic bullous keratopathy, patients with DMEK showed a better graft survival and fewer rejections than patients treated with PKP or DSAEK receiving the same medical postoperative therapy.44 A meta-analysis yielded better postoperative outcomes for DMEK in terms of best corrected visual acuity (BCVA), patient satisfaction and rejection rates.45 In the direct comparison of DMEK and DSAEK, a distinction must be made in the DSAEK group between DSAEK, MT-(microthin, <130 µm graft thickness)46 DSAEK and UT-(ultrathin <100 µm graft thickness)40 DSAEK. The trend towards further reduced DSAEK graft thickness results from the fact that thinner grafts with the thinnest possible stromal lamella are associated with faster visual recovery.47 Randomised controlled trials on the treatment of FECD or pseudophakic bullous keratopathy with DMEK or MT-DSAEK or UT-DSAEK concluded that DMEK leads to better visual outcomes after 3, 6 and 12 months,46 48–50 whereas both techniques lead to a minimal hyperopic shift and do not differ in terms of endothelial cell loss.50 In addition, DMEK resulted in lower posterior corneal higher order aberrations compared with UT-DSAEK.51 Contrast and scatter sensitivity also recovered faster after DMEK.51 Although these studies document a superiority of DMEK, there exist also randomised controlled trials that showed comparable results between DMEK and UT-DSAEK in terms of postoperative BCVA, complication rates, endothelial loss and patient-reported quality-of-life scores.52 Finally, the growing number of posterior lamellar procedures is probably also attributable to the decreasing clinical threshold for surgery in corneal endothelial diseases.53
The increasing use of sophisticated tomographic and biomechanical measurements54–56 helping to diagnose keratoconus at its very early stages and corneal crosslinking providing efficient keratoconus stabilisation57 may contribute to decreasing numbers of keratoplasties (PKP and DALK). Although DALK aims to preserve the patient’s own endothelium and is thus not threatened by endothelial rejection, it is technically challenging and may be considered still on its way to becoming the standard procedure for corneal pathologies located in the (anterior) corneal stroma.38 Visual outcomes after DALK and PKP may show similar results,58 yet there are several factors that contribute to the fact that DALK has not become widespread in Germany. First, corneal crosslinking increasingly succeeds in halting keratoconus progression, thus obviating at least in part the need for keratoplasty. Second, DALK does not always achieve the desired separation between Descemet’s membrane and the corneal stroma59 resulting in an average BCVA of 20/4060–62 in young patients with keratoconus or stromal corneal dystrophies. In Germany, the well-established eximer laser-assisted PKP technique may achieve a BCVA up to 20/28 on average.63 64 Third, a frustrated separation of Descemet’s membrane and the corneal stroma may result in opacities in the interface between Descemet’s membrane and the posterior corneal stroma.59 Fourth, the rate of patients requiring intraoperative conversion from DALK to PKP (in Germany between 10%65 66 and 15%67) may discourage the use of DALK as a routine technique in the patients with keratoconus.68
Repeated keratoplasty was again the third most common indication for corneal transplantation in Germany in 2021. Unfortunately, the German Keratoplasty Registry did not collect data on the underlying diagnoses of repeated keratoplasty up to now. It is known that posterior lamellar procedures in abnormal anterior chamber anatomy subsequent to previous surgery have a higher failure rate.69 70 Detailed data about repeated keratoplasty in Germany are still to be collected and should be the main topic of the next German Keratoplasty Registry report. A recent German multicentre (n=7) study about 3200 DMEKs conducted to treat FECD or pseudophakic bullous keratopathy reported 3% graft failure (n=67) and a graft rejection rate of 1.5% (n=48), respectively.2 Thus, (1) repeated PKP after graft failure, (2) repeated DMEK/DSAEK after graft failure, but also (3) DMEK on the PKP graft (also in case of transplanted guttae on the PKP graft71 or if a toric intraocular lens has been implanted earlier to correct corneal astigmatism) in previously well-functioning penetrating grafts are to be subsumed under the heading of repeated keratoplasty.72
Conclusions
As in many other countries, the most common corneal transplantation in Germany is the posterior lamellar keratoplasty. Germany stands out in international comparison because of the high proportion of DMEK and very low proportion of DSAEK. Penetrating keratoplasty continues to be the second most frequent corneal transplantation procedure, although its number decreased proportionally from 2011 to 2021. The number of PKP is yet almost stable because of the increasing number of overall corneal transplantations. DALK seems to be underrepresented in Germany with about 3% and might further decrease due to an early and stage-appropriate therapy of keratoconus.
Footnotes
Collaborators: German Keratoplasty Registry (GeKeR) Study Members and thereby contributing collaborators are in alphabetical order: Julita Adamiak-Kalinowska (Klinikum Frankfurt/Oder, Germany), Professor Dr Sabine Aisenbrey (Vivantes Klinikum, Neukölln, Germany), Dr Nasser Al Ashi (Oberlausitz-Kliniken gGmbh, Bautzen, Germany), Professor Dr Gerd Auffarth (Universitätsaugenklinik Heidelberg, Germany), Professor Dr Holger Baatz (Aurelios Augenzentrum Recklinghausen, Germany), Claudia Baier (HELIOS Klinikum Pforzheim, Germany), Dr Dirk Bahlmann (Universitätsaugenklinik Göttingen, Germany), Professor Dr Karl U Bartz-Schmidt (Universitätsaugenklinik Tübingen, Germany), Professor Dr Nikolaos E Bechrakis (Universitätsaugenklinik Essen, Germany), Professor Dr Marcus Blum (HELIOS Klinikum Erfurt GmbH, Germany), Professor Dr Andreas G Böhm (Elblandklinikum Radebeul, Germany), PD Dr Thorsten Böker (Klinikum Dortmund GmbH, Germany), Dr Simone Brandtner (Klinikum Bremen Mitte, Germany), Dr Christian K Brinkmann (Klinikum Dietrich Bonhoeffer Neubrandenburg GmbH, Germany), Professor Dr Reinhard Burk (Klinikum Bielefeld Rosenhöhe, Germany), Dr Erik Chankiewitz (Städisches Klinikum Braunschweig, Germany), Professor Dr Claus Cursiefen (Universitätsaugenklinik Köln, Germany), Professor Dr Burkhard Dick (Universitätsaugenklinik Bochum, Germany), Dr Dirk Ehrich (HELIOS Vogtland Kliniken, Germany), Professor Dr Karl-Heinz Emmerich (Klinikum Darmstadt, Germany), Professor Dr Katrin Engelmann (Klinikum Chemnitz gGmbH, Germany), Professor Dr Nicole Eter (Universitätsaugenklinik Münster, Germany), Professor Dr Carsten Framme (Medizinische Hochschule Hannover, Germany), PD Dr Ulrich Fries (Johanniter-Krankenhaus Bonn, Germany), Professor Dr Thomas A Fuchsluger (Universitätsaugenklinik Rostock, Germany), Professor Dr Matthias Fuest (Universitätsaugenklinik Aachen, Germany), Professor Dr Gerd Geerling (Universitätsaugenklinik Düsseldorf, Germany), Professor Dr Florian Gekeler (Klinikum Stuttgart-Katharinenhospital, Germany), Professor Dr Christos Haritoglou (Augenklinik Herzog Carl Theodor München, Germany), Professor Dr Lars-Olof Hattenbach (Klinikum Ludwigshafen gGmbH, Germany), Professor Dr Horst Helbig (Universitätsaugenklinik Regensburg, Germany), Professor Dr Fritz Hengerer (Bürgerhospital Frankfurt, Germany), Professor Dr Lutz Hesse (SLK-Kliniken Heilbronn GmbH, Germany), Professor Dr Konrad Hille (Ortenau Klinikum Offenburg, Germany), Professor Dr Jost Hillenkamp (Universitätsklinikum Würzburg, Germany), PD Dr Fabian Höhn (Marienhospital Osnabrück, Germany), Professor Dr Frank G Holz (Universitätsaugenklinik Bonn, Germany), Professor Dr Antonia M Joussen (Charité Universitätsaugenklinik Berlin, Germany), Dr Bernd Junker (Maximilians-Augenklinik, Nürnberg, Germany), Dr Susanne Kaskel-Paul (Klinikum Lüdenscheid, Germany), Professor Dr Marcus Knorr (HELIOS Klinikum Krefeld, Germany), Professor Dr Leon Kohen (Helios Klinikum Aue, Germany), Professor Dr Markus Kohlhaas (St. Johannes-Hospital Dortmund, Germany), Professor Dr Thomas Kohnen (Universitätsaugenklinik Frankfurt, Germany), PD Dr Lothar Krause (Städtisches Klinikum Dessau, Germany), Professor Dr Friedrich E Kruse (Universitätsaugenklinik Erlangen, Germany), Dr Markus S Ladewig (Klinikum Saarbrücken gGmbH, Germany), Dr Catharina Latz (Augenklinik Dardenne Bonn, Germany), Professor Dr Wolfgang E Lieb (Vincentus-Diakonissen-Kliniken gAG Karlsruhe, Germany), Professor Dr Anja Liekfeld (Klinikum Ernst von Bergmann gGmbH Potsdam, Germany), Professor Dr Mathias Maier (Klinikum rechts der Isar, Technische Universität München, Germany), Dr Joachim Magner (Park-Klinik Manhagen, Germany), Professor Dr Daniel Meller (Universitätsaugenklinik Jena, Germany), Dr Andreas Mohr (St. Joseph-Stift Bremen, Germany), Dr Markus Motschmann (AMEOS Klinikum Haldensleben, Germany), Prof Dr Arthur Mueller (Universitätsaugenklinik Augsburg, Germany), Professor Dr Thomas Neuhann (MVZ Thomas Neuhann GmbH, München, Germany), Dr Tobias Neuhann (Ophthalmologikum Neuhann MVZ GmbH, München, Germany), Dr Thomas Pahlitzsch (Augenklinik im Ring-Center GmbH, Berlin, Germany), Professor Dr Lutz E Pillunat (Universitätsaugenklinik Dresden, Germany), Dr Uwe P Press (Krankenhaus der Barmherzigen Brüder Trier, Germany), Professor Dr Siegfried G Priglinger (Universitätsaugenklinik München, Germany), Igor Prusiecki (Städtisches Klinikum Görlitz, Germany), PD Dr Mahdy Ranjbar (Universitätsaugenklinik Lübeck, Germany), Professor Dr Matus Rehak (Universitätsaugenklinik Giessen, Germany), Professor Dr Thomas Reinhard (Universitätsaugenklinik Freiburg, Germany), Professor Dr Peter Rieck (Schlosspark-Klinik Berlin, Germany), Professor Dr Johann B Roider (Universitätsaugenklinik Kiel, Germany), Professor Dr Helmut Sachs (Carl-Thiem-Klinikum gGmbH, Cottbus, Germany), Professor Dr Gangolf Sauder (Charlottenklinik Stuttgart, Germany), Dr Hubert Scharf (Südharz-Klinikum gGmbH, Nordhausen, Germany), Professor Dr Marc Schargus (Asklepios Klinik Nord-Heidberg, Hamburg, Germany), Dr Armin Scharrer (MVZ Fürth, Germany), PD Dr Ulrich Schaudig (Asklepios Klinikum Barmbek, Hamburg, Germany), Dr Christian Scheib (Diakonissenkrankenhaus Karlsruhe, Germany), Professor Dr Andreas Scheider (Evangelisches Krankenhaus Essen-Werden, Germany), Professor Dr Josef Schmidbauer (Klinikum Nürnberg, Germany), Professor Dr Stefan Schrader (Universitätsklinikum Oldenburg, Germany), Professor Dr Norbert Schrage (Kliniken der Stadt Köln gGmbH, Germany), Dr Jens Schrecker (Rudolf Virchow Klinikum Glauchau gGmbH, Germany), Dr Frank Schröder (Universitätsaugenklinik Marburg, Germany), Dr Jörg Seewald (SRH Waldklinikum GmbH, Gera, Germany), Professor Dr Martin Spitzer (Universitätsaugenklinik Hamburg, Germany), Professor Dr Andreas Stahl (Universitätsaugenklinik Greifswald, Germany), Dr Annette Sturm (Städtisches Klinikum Brandenburg GmbH, Germany), Professor Dr Peter Szurman (Knappschaftsklinikum Saar GmbH Sulzbach, Germany), Professor Dr Hagen Thieme (Universitätsaugenklinik Magdeburg, Germany), Professor Dr Felix Treumer (Klinikum Kassel, Germany), Professor Dr Arne Viestenz (Universitätsaugenklinik Halle, Germany), Dr Burkhard von Jagow (Klinikum Barnim GmbH Eberswalde, Germany), Professor Dr Joachim Wachtlin (St. Gertrauden Krankenhaus, Berlin, Germany), PD Dr Joanna Wasielica-Poslednik (Universitätsaugenklinik Mainz, Germany), PD Dr Christopher Wirbelauer (Augenklinik Berlin-Marzahn GmbH, Germany), Professor Dr Armin Wolf (Universitätsaugenklinik Ulm, Germany) and Professor Dr Focke Ziemssen (Universitätsaugenklinik Leipzig, Germany).
Contributors: EF is guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Collaborators: GeKeR Study Group, Julita Adamiak-Kalinowska, Sabine Aisenbrey, Nasser Al Ashi, Gerd Auffarth, Holger Baatz, Claudia Baier, Dirk Bahlmann, Karl U Bartz-Schmidt, Nikolaos E Bechrakis, Marcus Blum, Andreas G Böhm, Thorsten Böker, Simone Brandtner, Christian K Brinkmann, Reinhard Burk, Erik Chankiewitz, Claus Cursiefen, Burkhard Dick, Dirk Ehrich, Karl-Heinz Emmerich, Katrin Engelmann, Nicole Eter, Carsten Framme, Ulrich Fries, Thomas A Fuchsluger, Matthias Fuest, Gerd Geerling, Florian Gekeler, Christos Haritoglou, Lars-Olof Hattenbach, Horst Helbig, Fritz Hengerer, Lutz Hesse, Konrad Hille, Jost Hillenkamp, Fabian Höhn, Frank G Holz, Antonia M Joussen, Bernd Junker, Susanne Kaskel-Paul, Marcus Knorr, Leon Kohen, Markus Kohlhaas, Thomas Kohnen, Lothar Krause, Friedrich E Kruse, Markus S Ladewig, Catharina Latz, Wolfgang E Lieb, Anja Liekfeld, Mathias Maier, Joachim Magner, Daniel Meller, Andreas Mohr, Markus Motschmann, Arthur Mueller, Thomas Neuhann, Tobias Neuhann, Thomas Pahlitzsch, Lutz E Pillunat, Uwe P Press, Siegfried G Priglinger, Igor Prusiecki, Mahdy Ranjbar, Matus Rehak, Thomas Reinhard, Peter Rieck, Johann B Roider, Helmut Sachs, Gangolf Sauder, Hubert Scharf, Marc Schargus, Armin Scharrer, Ulrich Schaudig, Christian Scheib, Andreas Scheider, Josef Schmidbauer, Stefan Schrader, Norbert Schrage, Jens Schrecker, Frank Schröder, Martin Spitzer, Andreas Stahl, Annette Sturm, Peter Szurman, Hagen Thieme, Felix Treumer, Arne Viestenz, Burkhard von Jagow, Joachim Wachtlin, Joanna Wasielica-Poslednik, Christopher Wirbelauer, Armin Wolf, Focke Ziemssen, and Jörg Seewald
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The local ethics committee of Saarland (Ethikkommission bei der Ärztekammer des Saarlandes) was informed and decided to exempt this study because it does not contain individual-related data.
References
- 1. Zirm EK. Eine erfolgreiche totale keratoplastik (a successful total keratoplasty). Albrecht von Graefes Archiv Für Ophthalmologie 1906;64:580–93. 10.1007/BF01949227 [DOI] [Google Scholar]
- 2. Spaniol K, Hellmich M, Borgardts K, et al. DMEK outcome after one year-results from a large multicenter study in Germany. Acta Ophthalmol 2023;101:e215–25. 10.1111/aos.15257 [DOI] [PubMed] [Google Scholar]
- 3. Sugita J, Kondo J. Deep lamellar keratoplasty with complete removal of pathological stroma for vision improvement. Br J Ophthalmol 1997;81:184–8. 10.1136/bjo.81.3.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Anwar M, Teichmann KD. Big-bubble technique to bare Descemet’s membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 2002;28:398–403. 10.1016/s0886-3350(01)01181-6 [DOI] [PubMed] [Google Scholar]
- 5. Melles GRJ, Wijdh RHJ, Nieuwendaal CP. A technique to excise the Descemet membrane from a recipient cornea (descemetorhexis). Cornea 2004;23:286–8. 10.1097/00003226-200404000-00011 [DOI] [PubMed] [Google Scholar]
- 6. Price FW, Price MO. Descemet’s stripping with endothelial keratoplasty in 50 eyes: a refractive neutral corneal transplant. J Refract Surg 2005;21:339–45. 10.3928/1081-597X-20050701-07 [DOI] [PubMed] [Google Scholar]
- 7. Gorovoy MS. Descemet-stripping automated endothelial Keratoplasty. Cornea 2006;25:886–9. 10.1097/01.ico.0000214224.90743.01 [DOI] [PubMed] [Google Scholar]
- 8. Melles GRJ. Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea 2006;25:879–81. 10.1097/01.ico.0000243962.60392.4f [DOI] [PubMed] [Google Scholar]
- 9. Flockerzi E, Maier P, Böhringer D, et al. Trends in corneal transplantation from 2001 to 2016 in Germany: a report of the dog-section cornea and its keratoplasty registry. Am J Ophthalmol 2018;188:91–8. 10.1016/j.ajo.2018.01.018 [DOI] [PubMed] [Google Scholar]
- 10. The European Cornea and Cell Transplantation Registry . Summary final report of the ECCTR project. Available: https://ec.europa.eu/research/participants/documents/downloadPublic?documentIds=080166e5c9dc9246&appId=PPGMS [Accessed 1 Jun 2022].
- 11. Dunker SL, Armitage WJ, Armitage M, et al. Practice patterns of corneal transplantation in Europe: first report by the European cornea and cell transplantation registry. J Cataract Refract Surg 2021;47:865–9. 10.1097/j.jcrs.0000000000000574 [DOI] [PubMed] [Google Scholar]
- 12. National Health Service of the United Kingdom Health Departments . Organ and tissue donation and transplantation activity report; Available: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/24053/activity-report-2020-2021.pdf [Accessed 1 Jun 2022].
- 13. Fondazione banca degli occhi del veneto onlus; Available: https://www.fbov.org/images/Report/Report2020/fbov_web_.pdf [DOI] [PMC free article] [PubMed]
- 14. Eye Bank Association of America . Eye banking statistical report. 2019. Available: https://restoresight.org/wp-content/uploads/2020/04/2019-EBAA-Stat-Report-FINAL.pdf
- 15. Eye Bank Association of America . Eye banking statistical report. 2021. Available: https://restoresight.org/statistical-report/
- 16. Canadian Blood Services . Canadian Eye and Tissue Data Committee Report; 2020. Available: https://profedu.blood.ca/sites/default/files/2021-12/2020%20ETDC%20Report_EN%20FINAL.pdf
- 17. Brazilian Transplantation Registry . Organ transplantation in Brazil 2012–2019. n.d. Available: https://site.abto.org.br/wp-content/uploads/2020/09/rbt-ingles-2019-leitura.pdf
- 18. Almeida HG, Hida RY, Kara-Junior N. Trends in corneal transplantation from 2001 to 2016 in Brazil. Arq Bras Oftalmol 2018;81:529–38. 10.5935/0004-2749.20180096 [DOI] [PubMed] [Google Scholar]
- 19. Mora M, Cortés M, Plata M, et al. Corneal transplant epidemiology in a reference center in Bogotá, Colombia (2010–2017). Pan Am J Ophthalmol 2021;3:39. 10.4103/pajo.pajo_108_21 [DOI] [Google Scholar]
- 20. Servin-Rojas M, Olivas-Martinez A, Ramirez Del Val F, et al. Transplant trends in Mexico during the COVID-19 pandemic: disparities within healthcare sectors. Am J Transplant 2021;21:4052–60. 10.1111/ajt.16801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ali Javadi M, Kanavi MR, Safi S. A 27-year report from the Central Eye Bank of Iran. J Ophthalmic Vis Res 2020;15:149–59. 10.18502/jovr.v15i2.6731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sharma N, Arora T, Singhal D, et al. Procurement, storage and utilization trends of eye banks in India. Indian J Ophthalmol 2019;67:1056–9. 10.4103/ijo.IJO_1551_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chaurasia S, Mohamed A, Garg P, et al. Thirty years of eye bank experience at a single centre in India. Int Ophthalmol 2020;40:81–8. 10.1007/s10792-019-01164-y [DOI] [PubMed] [Google Scholar]
- 24. Gao H, Huang T, Pan Z, et al. Survey report on keratoplasty in China: a 5-year review from 2014 to 2018. Plos one 2020;15:e0239939. 10.1371/journal.pone.0239939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhang J, Patel DV, McGhee CNJ. The rapid transformation of transplantation for corneal endothelial diseases: an evolution from penetrating to lamellar to cellular transplants. Asia PAC J Ophthalmol 2019;8:441–7. 10.1097/APO.0000000000000265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. The Australian Corneal Graft Registry 2020 annual report; Available: https://www.flinders.edu.au/content/dam/documents/research/fhmri-eye-and-vision/australian-corneal-graft-registry-2020-annual-report.pdf
- 27. Williams KA, Keane MC. Outcomes of corneal transplantation in Australia, in an era of lamellar keratoplasty. Clin Exp Ophthalmol 2022;50:374–85. 10.1111/ceo.14089 [DOI] [PubMed] [Google Scholar]
- 28. Makgotloe AM, Carmichael TR. Plummeting corneal donations at the Gauteng Cornea and Eye Bank. South African medical Journal = Suid-Afrikaanse Tydskrif VIR Geneeskunde 2009;99:797. [PubMed] [Google Scholar]
- 29. Chen MC, Kunselman AR, Stetter CM, et al. Corneal transplantation at Tenwek hospital, Kenya, East Africa: analysis of outcomes and associated patient socioeconomic characteristics. Plos one 2017;12:e0187026. 10.1371/journal.pone.0187026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lartey S, Antwi-Adjei EK, Mohammed AK, et al. Indications and outcomes of corneal transplant surgery in Ghana. Ann Afr Surg 2021;18:137–42. 10.4314/aas.v18i3.3 [DOI] [Google Scholar]
- 31. Ulasi II, Ijoma CK. Organ transplantation in Nigeria. Transplantation 2016;100:695–7. 10.1097/TP.0000000000001149 [DOI] [PubMed] [Google Scholar]
- 32. Matthaei M, Sandhaeger H, Hermel M, et al. Changing indications in penetrating keratoplasty: a systematic review of 34 years of global reporting. Transplantation 2017;101:1387–99. 10.1097/TP.0000000000001281 [DOI] [PubMed] [Google Scholar]
- 33. Palma-Carvajal F, Morales P, Salazar-Villegas A, et al. Trends in corneal transplantation in a single center in Barcelona, Spain. Transitioning to DMEK. J Fr Ophtalmol 2020;43:1–6. 10.1016/j.jfo.2019.06.026 [DOI] [PubMed] [Google Scholar]
- 34. Ham L, Dapena I, Moutsouris K, et al. Refractive change and stability after Descemet membrane endothelial keratoplasty. Effect of corneal dehydration-induced hyperopic shift on intraocular lens power calculation. J Cataract Refract Surg 2011;37:1455–64. 10.1016/j.jcrs.2011.02.033 [DOI] [PubMed] [Google Scholar]
- 35. van Dijk K, Ham L, Tse WHW, et al. Near complete visual recovery and refractive stability in modern corneal transplantation: Descemet membrane endothelial keratoplasty (DMEK). Cont Lens Anterior Eye 2013;36:13–21. 10.1016/j.clae.2012.10.066 [DOI] [PubMed] [Google Scholar]
- 36. Price DA, Kelley M, Price FW, et al. Five-year graft survival of Descemet membrane endothelial keratoplasty (EK) versus Descemet stripping EK and the effect of donor sex matching. Ophthalmology 2018;125:1508–14. 10.1016/j.ophtha.2018.03.050 [DOI] [PubMed] [Google Scholar]
- 37. Deng SX, Lee WB, Hammersmith KM, et al. Descemet membrane endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology 2018;125:295–310. 10.1016/j.ophtha.2017.08.015 [DOI] [PubMed] [Google Scholar]
- 38. Cursiefen C, Schaub F, Bachmann BO. Update minimally invasive lamellar keratoplasty: DMEK, DSAEK and DALK. Klin Monbl Augenheilkd 2016;233:1033–42. 10.1055/s-0041-110448 [DOI] [PubMed] [Google Scholar]
- 39. Cursiefen C, Steven P, Roters S, et al. Komplikationsvermeidung und -management bei „Descemet membrane endothelial keratoplasty'' (DMEK) und „Descemet stripping automated endothelial keratoplasty'' (DSAEK). Ophthalmologe 2013;110:614–21. 10.1007/s00347-012-2679-8 [DOI] [PubMed] [Google Scholar]
- 40. Bachmann B, Schaub F, Cursiefen C. Treatment of corneal endothelial disorders by DMEK and UT-DSAEK. indications, complications, results and follow-up. Ophthalmologe 2016;113:196–203. 10.1007/s00347-016-0221-0 [DOI] [PubMed] [Google Scholar]
- 41. Bachmann B, Schrittenlocher S, Matthaei M, et al. „Descemet membrane endothelial keratoplasty'' in komplexen augen. Ophthalmologe 2019;116:228–35. 10.1007/s00347-018-0818-6 [DOI] [PubMed] [Google Scholar]
- 42. Soh YQ, Kocaba V, Pinto M, et al. Fuchs endothelial corneal dystrophy and corneal endothelial diseases: East meets West. Eye (Lond) 2020;34:427–41. 10.1038/s41433-019-0497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kisilevsky E, Srikumaran D, Chew HF. Surgeon preferences for endothelial keratoplasty in Canada. Cornea 2021;40:1420–5. 10.1097/ICO.0000000000002639 [DOI] [PubMed] [Google Scholar]
- 44. Woo JH, Ang M, Htoon HM, et al. Descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty and penetrating keratoplasty. Am J Ophthalmol 2019;207:288–303. 10.1016/j.ajo.2019.06.012 [DOI] [PubMed] [Google Scholar]
- 45. Marques RE, Guerra PS, Sousa DC, et al. DMEK versus DSAEK for Fuchs’ endothelial dystrophy: a meta-analysis. Eur J Ophthalmol 2019;29:15–22. 10.1177/1120672118757431 [DOI] [PubMed] [Google Scholar]
- 46. Matsou A, Pujari R, Sarwar H, et al. Microthin Descemet stripping automated endothelial keratoplasty versus Descemet membrane endothelial keratoplasty: a randomized clinical trial. Cornea 2021;40:1117–25. 10.1097/ICO.0000000000002601 [DOI] [PubMed] [Google Scholar]
- 47. Dapena I, Ham L, Melles GRJ. Endothelial keratoplasty: DSEK/DSAEK or DMEK – the thinner the better? Curr Opin Ophthalmol 2009;20:299–307. 10.1097/ICU.0b013e32832b8d18 [DOI] [PubMed] [Google Scholar]
- 48. Chamberlain W, Lin CC, Austin A, et al. Descemet endothelial thickness comparison trial: a randomized trial comparing ultrathin Descemet stripping automated endothelial keratoplasty with Descemet membrane endothelial keratoplasty. Ophthalmology 2019;126:19–26. 10.1016/j.ophtha.2018.05.019 [DOI] [PubMed] [Google Scholar]
- 49. Hirabayashi KE, Chamberlain W, Rose-Nussbaumer J, et al. Corneal light scatter after ultrathin Descemet stripping automated endothelial keratoplasty versus Descemet membrane endothelial keratoplasty in Descemet endothelial thickness comparison trial: a randomized controlled trial. Cornea 2020;39:691–6. 10.1097/ICO.0000000000002256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dunker SL, Dickman MM, Wisse RPL, et al. Descemet membrane endothelial keratoplasty versus ultrathin Descemet stripping automated endothelial keratoplasty: a multicenter randomized controlled clinical trial. Ophthalmology 2020;127:1152–9. 10.1016/j.ophtha.2020.02.029 [DOI] [PubMed] [Google Scholar]
- 51. Dunker SL, Dickman MM, Wisse RPL, et al. Quality of vision and vision-related quality of life after Descemet membrane endothelial keratoplasty: a randomized clinical trial. Acta Ophthalmol 2021;99:e1127–34. 10.1111/aos.14741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pujari R, Matsou A, Kean J, et al. A randomized controlled trial comparing microthin Descemet stripping automated endothelial keratoplasty with Descemet membrane endothelial keratoplasty: two-year report. Cornea 2022;41:1519–24. 10.1097/ICO.0000000000003024 [DOI] [PubMed] [Google Scholar]
- 53. Chilibeck CM, Brookes NH, Gokul A, et al. Changing trends in corneal transplantation in Aotearoa/New Zealand, 1991 to 2020: effects of population growth, cataract surgery, endothelial keratoplasty, and corneal cross-linking for keratoconus. Cornea 2022;41:680–7. 10.1097/ICO.0000000000002812 [DOI] [PubMed] [Google Scholar]
- 54. Belin MW, Duncan JK. Keratoconus: the ABCD grading system. Klin Monbl Augenheilkd 2016;233:701–7. 10.1055/s-0042-100626 [DOI] [PubMed] [Google Scholar]
- 55. Vinciguerra R, Ambrósio R, Elsheikh A, et al. Detection of keratoconus with a new biomechanical index. J Refract Surg 2016;32:803–10. 10.3928/1081597X-20160629-01 [DOI] [PubMed] [Google Scholar]
- 56. Flockerzi E, Vinciguerra R, Belin MW, et al. Combined biomechanical and tomographic keratoconus staging: adding a biomechanical parameter to the ABCD keratoconus staging system. Acta Ophthalmol 2022;100:e1135–42. 10.1111/aos.15044 [DOI] [PubMed] [Google Scholar]
- 57. Xanthopoulou K, Milioti G, Daas L, et al. Accelerated corneal crosslinking causes pseudoprogression in keratoconus within the first 6 weeks without affecting posterior corneal curvature. Eur J Ophthalmol 2022;32:2565–76. 10.1177/11206721221099257 [DOI] [PubMed] [Google Scholar]
- 58. Reinhart WJ, Musch DC, Jacobs DS, et al. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty. Ophthalmology 2011;118:209–18. 10.1016/j.ophtha.2010.11.002 [DOI] [PubMed] [Google Scholar]
- 59. Cursiefen C, Siebelmann S, Bachmann B. Complications of deep anterior lamellar keratoplasty. Avoid, recognize and treat. Der Ophthalmologe 2015;112:961–8. 10.1007/s00347-015-0164-x [DOI] [PubMed] [Google Scholar]
- 60. Bahar I, Kaiserman I, Srinivasan S, et al. Comparison of three different techniques of corneal transplantation for keratoconus. Am J Ophthalmol 2008;146:905–12. 10.1016/j.ajo.2008.06.034 [DOI] [PubMed] [Google Scholar]
- 61. Kubaloglu A, Sari ES, Koytak A. Deep anterior lamellar keratoplasty in eyes previously treated with collagen crosslinking for keratoconus: 3-year results. Graefes Arch Clin Exp Ophthalmol 2020;258:821–7. 10.1007/s00417-019-04587-6 [DOI] [PubMed] [Google Scholar]
- 62. Feizi S, Javadi MA, Karimian F, et al. Penetrating keratoplasty versus deep anterior lamellar keratoplasty for advanced stage of keratoconus. Am J Ophthalmol 2023;248:107–15. 10.1016/j.ajo.2022.11.019 [DOI] [PubMed] [Google Scholar]
- 63. Seitz B, Langenbucher A, Kus MM, et al. Nonmechanical corneal trephination with the excimer laser improves outcome after penetrating keratoplasty. Ophthalmology 1999;106:1156–64. 10.1016/S0161-6420(99)90265-8 [DOI] [PubMed] [Google Scholar]
- 64. Seitz B, Hager T, Langenbucher A, et al. Reconsidering sequential double running suture removal after penetrating keratoplasty: a prospective randomized study comparing excimer laser and motor trephination. Cornea 2018;37:301–6. 10.1097/ICO.0000000000001420 [DOI] [PubMed] [Google Scholar]
- 65. Heindl LM, Riss S, Bachmann BO, et al. Split cornea transplantation for 2 recipients: a new strategy to reduce corneal tissue cost and shortage. Ophthalmology 2011;118:294–301. 10.1016/j.ophtha.2010.05.025 [DOI] [PubMed] [Google Scholar]
- 66. Cursiefen C, Heindl LM. Perspectives of deep anterior lamellar keratoplasty. Ophthalmologe 2011;108:833–9. 10.1007/s00347-011-2331-z [DOI] [PubMed] [Google Scholar]
- 67. Riss S, Heindl LM, Bachmann BO, et al. Pentacam-based big bubble deep anterior lamellar keratoplasty in patients with keratoconus. Cornea 2012;31:627–32. 10.1097/ICO.0b013e31823f8c85 [DOI] [PubMed] [Google Scholar]
- 68. Cursiefen C, Schaub F, Bachmann B. Update: deep anterior lamellar keratoplasty (DALK) for keratoconus. When, how and why. Ophthalmologe 2016;113:204–12. 10.1007/s00347-015-0204-6 [DOI] [PubMed] [Google Scholar]
- 69. Cohen E, Mimouni M, Sorkin N, et al. Risk factors for repeat Descemet membrane endothelial keratoplasty graft failure. Am J Ophthalmol 2021;226:165–71. 10.1016/j.ajo.2021.01.004 [DOI] [PubMed] [Google Scholar]
- 70. Kiel M, Bu JB, Gericke A, et al. Comparison of DMEK and DSAEK in eyes with endothelial decompensation after previous penetrating keratoplasty. Cornea 2021;40:1218–24. 10.1097/ICO.0000000000002786 [DOI] [PubMed] [Google Scholar]
- 71. Schönit S, Maamri A, Zemova E, et al. Prevalence and impact of cornea guttata in the graft after penetrating keratoplasty in Germany. Cornea 2022;41:1495–502. 10.1097/ICO.0000000000002971 [DOI] [PubMed] [Google Scholar]
- 72. Seitz B, Daas L, Wykrota AA, et al. Graft failure after PKP and DMEK: what is the best option? Klin Monbl Augenheilkd 2022;239:775–85. 10.1055/a-1774-4862 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable.