Abstract
Objective
The increasing prevalence of liver disease in the UK means there is a pressing need to expand the hepatology workforce. This survey aims to evaluate current hepatology training provision, and trainee attitudes towards future careers in hepatology.
Method
An electronic survey was distributed to higher specialty gastroenterology and hepatology trainees in the UK between March and May 2022.
Results
138 trainees completed the survey covering all training grades and regions of the UK. 73.7% reported receiving adequate hepatology training currently, with 55.6% intending to become future hepatologists. Trainee preference for future hepatology consultant posts in specialist liver centres were almost threefold higher compared with district general hospitals (60.9% vs 22.6%). All trainees, irrespective of training grade reported high confidence in managing decompensated cirrhosis in both inpatient and outpatient settings. Senior trainees (grade ST6 and higher), without advanced training programme (ATP) experience reported significantly lower confidence in managing viral hepatitis, hepatocellular carcinoma and post-transplant patients compared with equivalent trainees with ATP experience. For junior trainees (IMT3–ST5), remaining in their current deanery was the most important factor when considering future hepatology training application.
Conclusions
There is a significant need to deliver widely available training on the management of complex liver disease to improve non-ATP trainee confidence. Innovative job planning strategies are required to encourage trainees to pursue careers outside of specialist liver centres. Expansion of hepatology training networks with wider geographical coverage are needed to address the growing need for more hepatologists around the UK.
Keywords: LIVER, HEALTH SERVICE RESEARCH
WHAT IS ALREADY KNOWN ON THIS TOPIC
The previous national trainee survey of hepatology training in the UK was conducted in 2010 and reported suboptimal hepatology training.
WHAT THIS STUDY ADDS
73.7% of trainees reported receiving adequate hepatology clinical experience currently and 55.6% intend to become future hepatologists.
The number of trainees intending to work as consultant hepatologists in specialist liver centres were threefold higher compared with district general hospitals.
Trainees with hepatology advanced training programme (ATP) experience were significantly more confident in managing viral hepatitis, hepatocellular carcinoma and postliver transplant complications compared with trainees without hepatology ATP experience.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
There is a need to deliver widely available training/teaching on the management of patients with; viral hepatitis, hepatocellular carcinoma and postliver transplant complications.
Innovative planning strategies are required to address the imbalance in trainees’ preference for consultant posts in specialist liver centres over district general hospitals.
Expansion of hepatology training networks with wider geographical coverage is needed to address the growing need for more hepatologists around the UK.
Introduction
Liver disease is among the leading causes of premature mortality in the UK, with a fivefold increase in mortality in people under the age of 65 and a 400% increase in overall mortality since 1970.1 It is now the second-leading cause of years of working life lost in Europe, behind only ischaemic heart disease.2 Pivotal publications from the Lancet Commission on Liver Disease in the UK and the British Society of Gastroenterology (BSG) have outlined the urgent need to expand the number of hepatologists in order to meet the rising burden of liver disease.3 4 However, there has been no recent work focusing specifically on trainees’ attitudes and concerns towards hepatology training and hepatology as a future career subspecialty, which is pertinent in view of the growing clinical unmet need.
Recent gastroenterology/hepatology trainee surveys in the UK have focused on endoscopy training,5 changes in shape of training6 and the impact of COVID-19 pandemic.7 The previous national trainee survey of hepatology training in the UK was conducted in 2010 and reported suboptimal hepatology training coupled with trainee concerns regarding lack of hepatology consultant jobs. These experiences culminated in one in three of the survey respondents being dissuaded from a career in hepatology.8
The aims of this survey are to evaluate current hepatology training and attitudes towards future careers in hepatology by assessing the experiences, and opinions of current specialist gastroenterology/hepatology trainees across the UK.
Methods
The British Association for the Study of the Liver (BASL) Trainee’s committee designed a web-based survey (Google Forms—https://docs.google.com/forms/d/1FlGmRcbZTrxt4CSXSi2G3bMVr2F-IyVOjKa-0vHeM38/edit), which was sent to higher specialty gastroenterology trainees in the UK via mailing lists from BSG, BASL, gastroenterology regional training programme directors, gastroenterology trainee research collaboratives (https://www.rcplondon.ac.uk/trainee-research-collaboratives), BASL and BSG Twitter handles. The survey contained 25 questions focusing on hepatology training, research and future consultant career planning. Trainees were asked to record self-reported confidence levels in managing a range of liver diseases in both inpatient and outpatient settings on a scale of 0–10, where 0 represented full consultant supervision required and 10 represented no consultant supervision required. Data were collected between 14 March 2022 and 6 May 2022. Continuous variables (self-reported confidence levels) were analysed using Mann-Whitney U tests (two groups) or Kruskall-Wallis test (3+ groups). Data were analysed using SPSS V.25 and GraphPad Prism V.9.1.1.
Results
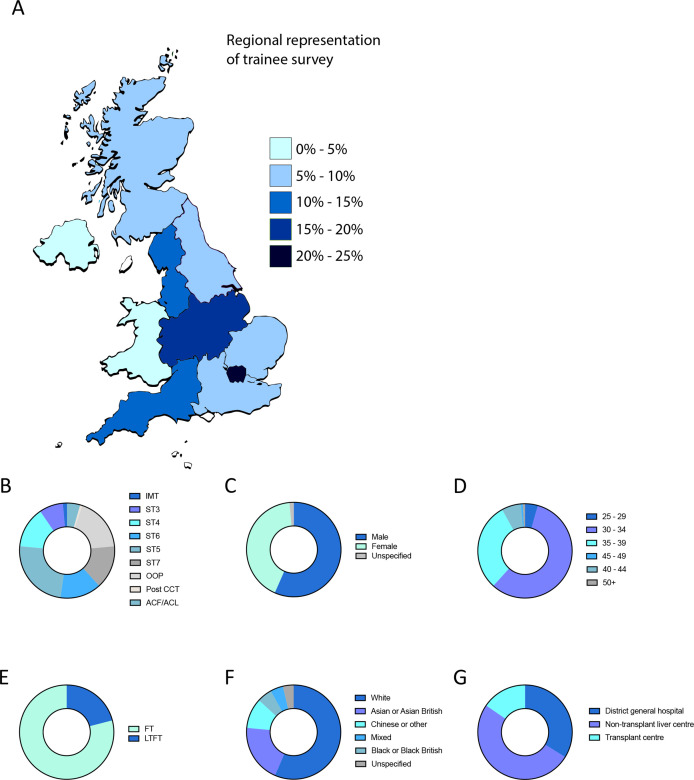
In total, 138 trainees completed the survey with representation from all National Health Service (NHS) regions across the UK (figure 1A) and across all training grades (figure 1B). Fifty-six per cent of trainees were male (figure 1C), 87% were 30–39 years old (figure 1D) and 79.4% worked full time at the time of survey (figure 1E). The most common ethnicity was white (56.6%), followed by Asian/Asian British (20.0%), Chinese/any other ethnic group (10.4%), black/black British (5.1%), mixed (4.4%) and unspecified (3.7%) (figure 1F). 33.8% of trainees worked at district general hospitals, with the remaining working in specialist liver centres (50.8% in non-transplant liver centres, 15.4% in transplant centres) (figure 1G).
Figure 1.
Trainee demographics. (A) Regional representation of trainee survey by NHS region expressed as percentage of total survey participants. (B) Trainees split by grades. (C) Trainees split by gender. (D) Trainees split by age group. (E) Trainees split by employment. (F) Trainees split by ethnicity. (G) Trainees split by liver centre designation. FT, full time; LTFT, less than full time; NHS, National Health Service.
Hepatology training
Excluding out of programme (OOP) trainees, 73.7% of trainees reported receiving adequate hepatology clinical experience in their current workplace. No significant geographical variations were observed across the UK. The majority of trainees that reported insufficient hepatology clinical experience worked in district general hospitals (82.8%) and were between IMT3 and ST5 grades (93.1%) and without previous hepatology advanced training programme (ATP) experience.
48.1% of trainees reported formal hepatology teaching availability at local hospital/trust level. Lack of regular local hepatology teaching was reported in all 10 NHS regions and was highest among district general hospitals (68.3%). At a regional level, 71.6% of trainees reported formal deanery hepatology teaching availability.
52.7% of trainees reported a dedicated hepatology component in their training programme with the majority of these trainees (91.4%) working in specialist liver centres. 45.6% of trainees reported absence of weekly hepatology ward rounds which was highest (74.5%) in trainees at district general hospitals. 19.1% of trainees reported no hepatology outpatient clinic experience in their current workplace, of which district general hospitals and non-transplant liver centres accounted for 71.4% and 23.8%, respectively.
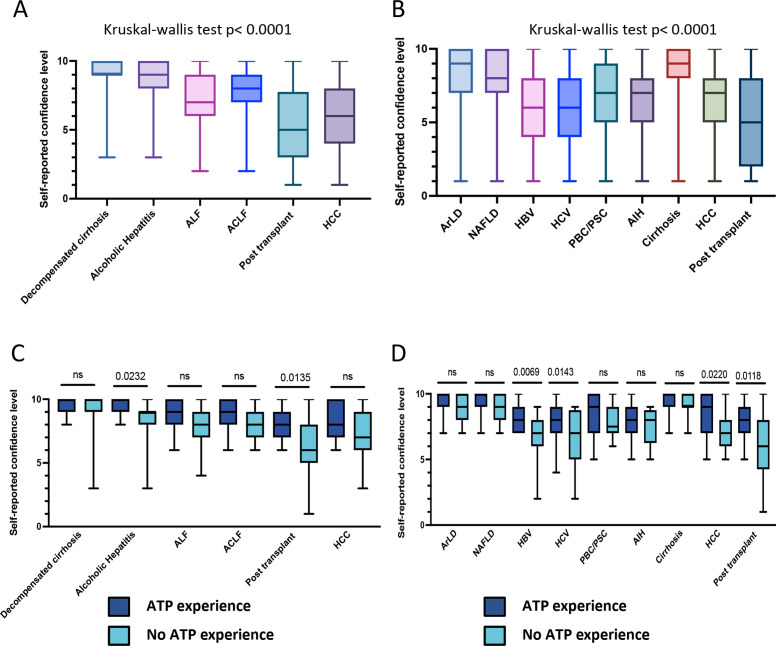
Trainees reported most confidence in managing patients with decompensated cirrhosis in both inpatient and outpatient settings. However, trainees reported least confidence in managing patients with postliver transplant complications and hepatocellular carcinoma (HCC). This was consistent for complications of both inpatients and outpatients (figure 2A,B). In terms of outpatient management, trainees were most confident in managing patients with alcohol-related liver disease (ArLD) and non-alcoholic fatty liver disease (NAFLD), but significantly lower confidence in managing patients with viral hepatitis (figure 2B). Conversely, senior trainees (ST6+) who have undertaken advanced hepatology training demonstrated significantly more confidence in managing all of these conditions (figure 2C,D).
Figure 2.
Trainee self reported confidence level in managing liver diseases. (A) Inpatient setting (all trainees). (B) Outpatient setting (all trainees). (C) Inpatient setting (senior trainee (ST6+) split by hepatology ATP experience). (D) Outpatient setting (senior trainee (ST6+) split by hepatology ATP experience). ATP, advanced training programme.
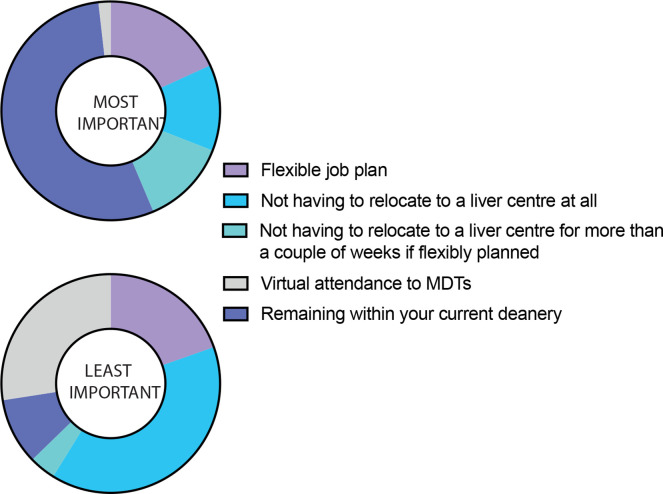
In total, 21.0% of trainees were either undertaking, or have undertaken the hepatology ATP, of whom 62.1% moved deanery in order to complete the programme. For junior trainees (grade IMT3–ST5) who have not yet to have hepatology ATP experience, remaining in current deanery was the single most important factor to trainees when considering future hepatology training application (figure 3).
Figure 3.
Factors influencing hepatology ATP application in junior trainees (IMT3 to ST5). ATP, advanced training programme.
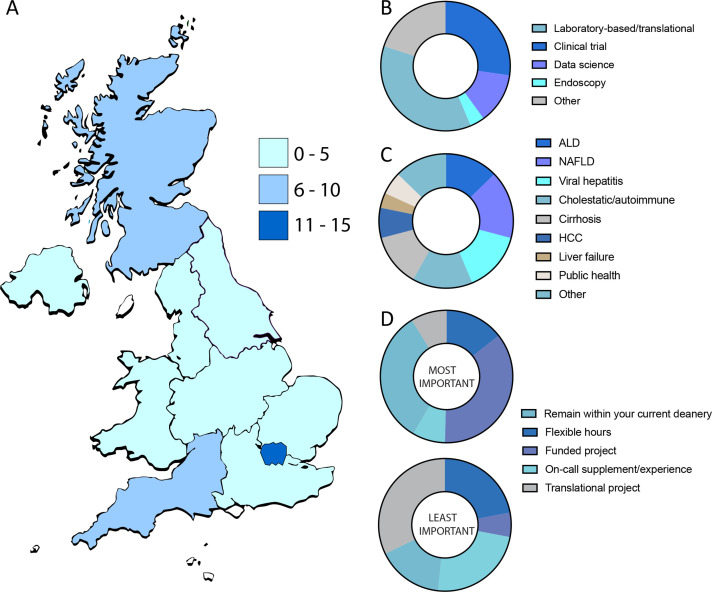
Hepatology research
In total, 39.1% of trainees reported either current or previous OOP research (OOPR) experience in hepatology with 56.4% being male. Regions with the most OOPR trainees were London, Scotland and South West England, which accounted for 58.3% of all OOPR trainees (figure 4A). Laboratory-based translational research accounted for the biggest proportion of OOPR experience (36.4%), followed by clinical trial-based research (27.3%) and data science-related research 12.7% (figure 4B). The distribution in liver research by disease aetiology was uniform with similar proportions of trainees conducting research in ArLD (12.7%), NAFLD (16.4%), viral hepatitis (14.5%), cholestatic/autoimmune liver disease (14.5%) and liver cirrhosis (12.7%). A smaller proportion of trainees conducted research in HCC (7.3%), public health (5.5%) and liver failure (3.6%) (figure 4C). Availability of funded research and remaining in the current deanery were the two most important factors when considering liver research opportunities (figure 4D). The least important factors were translational project, on-call supplementation/experience and flexible work hours.
Figure 4.
Trainee out of programme research (OOPR) experience. (A) Regional representation of total OOPR trainee numbers. (B) type of research conducted during OOPR. (C) Area of liver disease research. (D) Factors influencing hepatology research application. OOPR, out of programme research.
Future consultant career planning
In total, 55.6% of trainees across all regions in the UK intended to become a hepatologist. 21.4% of trainees had no intentions of becoming a hepatologist and the remaining 23.0% were unsure of their future career plans. In those wanting to become hepatologists, the majority (33.9%) want to work in non-transplant liver centres, followed by 22.6% in district general hospitals, 16.5% in transplant centres and 27% are unsure. Trainees who did not wish to become hepatologists stated endoscopy and luminal gastroenterology as their preferred subspecialty of interest. For trainees unsure of their future career path, the main reasons were uncertainty over changes in shape of training (40.5%) and lack of experience working in specialist liver centres (35.7%). Comparing trainees with and without OOPR experience to date, 84.6% with OOPR experience and 32.9% without OOPR experience wished to be consultant hepatologist in either non-transplant liver centres or transplant centres. 31.6% of trainees without OOPR experience wished to work as consultant hepatologists in district general hospitals compared with 5.1% of trainees with OOPR experience.
Discussion
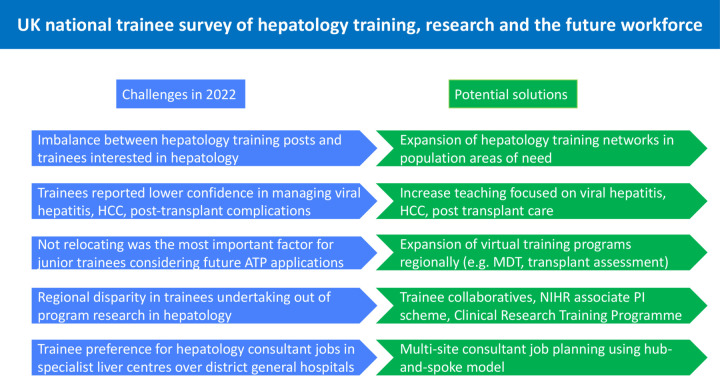
This national trainee survey illustrated the continuing high numbers of trainees wishing to pursue hepatology as a career subspecialty in the UK, while also highlighting significant challenges in hepatology workforce planning and hepatology training provision that requires urgent attention (figure 5).
Figure 5.
Infographic highlighting the current challenges and potential solutions for hepatology training, research, hepatology ATP and future hepatology consultant career planning. ATP, advanced training programme.
The survey found significant trainee preference for consultant posts in specialist liver centres over district general hospitals. The latest BSG workforce report suggests that 48% of advertised consultant jobs were unfilled, of which 49% of those were due to lack of applicants, while the proportion of unfilled hepatology consultant posts reported was unsurprisingly higher in district general hospitals.4 These findings demonstrate a paradigm shift from the 2010 training survey, which highlighted the perceived lack of consultant hepatology jobs as a major reason deterring trainees from hepatology training.8
Regional hub-and-spoke models for liver care involving networks of regional hospitals (spoke) and specialist liver centre (hub) are effective in reducing regional disparity in patient care, improve patient access to liver transplantation and reduced clinical pressure on the hub centres.9 Further work is needed to explore whether consultant job planning can be multisite and integrated within regional hub and spoke model in order to improve future specialist hepatology recruitment, particularly in district general hospitals. The NHS Long Term Plan set out in 2019, encourages NHS organisations and primary care partners to form ‘Integrated Care Systems’ to deliver services which meet the needs of local communities.10 As such, future consultant job planning integrating hepatology with primary care services may be a way to tackle liver disease in regions of greatest need and expand the hepatology workforce.
Junior trainees (grade IMT3–ST5) based predominantly in district general hospitals reported significantly less exposure to regular hepatology training and teaching compared with trainees based in other liver care settings, and this was reflected in their self-reported confidence level in management of liver diseases. With the Shape of Training reforms requiring junior trainees to decide early in their training whether they wish to pursue hepatology, increased exposure and teaching is vital during this early stage of training. Encouragingly, there has been an increasing number of online teaching resources for trainees in the UK such as the BASL School of Hepatology, which has helped to continue liver education despite the impact of COVID-19 pandemic on training. Nevertheless, all trainees irrespective of grade reported the highest confidence in managing patients with decompensated cirrhosis. This may reflect uniform increased exposure secondary to high disease burden and also the availability of tools such as the BSG/BASL decompensated cirrhosis care bundle11 to guide management. However, trainee confidence in managing patients with viral hepatitis, HCC and postliver transplant were lower across all training grades. In terms of viral hepatitis treatments, particularly hepatitis C, the treatment decisions and delivery are currently made through regional operational delivery networks, which are consultant driven and nurse led, thereby bypassing the need for trainee involvement. Similarly, lower confidence in HCC management may reflect the rapid advances in novel HCC therapies in recent12 and likely reflect limited exposure outside of specialist liver/oncology centres. More work is needed to engage trainees in the treatment decision-making process in order to improve confidence in managing viral hepatitis and HCC.
Prior to the recent Shape of Training reforms, in order to receive hepatology accreditation trainees must complete a 12 months hepatology ATP towards the latter part of their training, which are nationally recruited posts (22 in total), involving at least 3 months of training in one of seven liver transplant units around the UK. Results from this survey demonstrated a stark disconnect in the number of national hepatology ATPs and the number of trainees wishing to become hepatologists. In addition, they highlight the importance of the hepatology ATP experience in shaping senior trainees’ confidence in managing liver diseases, particularly in viral hepatitis, HCC and liver transplantation. Although more than 60% of trainees with hepatology ATP experience moved deaneries in order to complete the programme, the biggest factor influencing junior trainees’ decision to apply for future hepatology training posts was the option to remain within their current deanery, reflecting previous trainee surveys.13 Further work is needed to assess the quality of training across available hepatology ATP posts to ensure that trainees undertaking the ATP receive equivalent experience/learning.
Following Shape of Training reforms, hepatology ATP has been replaced by hepatology training pathway, which remain nationally recruited posts in the penultimate year of training. The duration of hepatology training pathway is 2 years, involving training in both specialist liver centres and district general hospitals. Increasing the number of hepatology training posts per deanery and expanding hepatology training networks in regions with poorly served liver care is needed in order to address the growing need for more hepatologists around the UK. The COVID-19 pandemic has been transformational for the uptake in innovative technology implementation in the health system. Clearly such advancements are likely to remain part of the rejuvenation of outpatient recovery programmes and remain in place for medium to long term. In the context of liver transplant centres, there is emerging evidence that virtual multidisciplinary transplant assessment is safe, and may increase patient accessibility to transplantation.14 Further work is needed to assess virtual training opportunities for trainees outside regional transplant centres. Hybrid programmes may include participation in remote or virtual ward rounds, multidisciplinary meetings, transplant assessments, with dedicated immersion attachments in regional transplant centres may help to expand regional hepatology training networks.15 Through the foundation of these expanded networks, it would be envisaged that opportunities for additional trainees to gain the required competencies across the breadth of the new 2-year hepatology curriculum would be feasible.
In terms of hepatology research, there were regional disparities in the number of OOPR trainees with higher numbers in certain regions such as London. This may reflect differences in regional research opportunities available to trainees. To address this imbalance, the National Institute for Health and Care Research associate principal investigator Scheme and Gastroenterology and Hepatology Clinical Research Training Programme16 17 should facilitate more research training, and funded liver research opportunities for trainees in previously under-represented areas of the UK. This is vital, as research-intense centres have been shown to deliver improved outcomes for patients including mortality.18 19 This is especially important as we understand that the burden of liver disease falls in those in poorer social demographics with less access to advanced hepatology services. Importantly, however, there has been an increase in the number of regional and national trainee research collaboratives in gastroenterology and hepatology in the last few years.20 21 This has enabled more trainees to be become research active, develop research skills and networking opportunities, improve well-being, and most importantly deliver projects resulting in improved patient care.
This study has several limitations. First, the number of survey participants was low compared with previous surveys and represented 20% (138/687) of all higher specialty trainees (HST) in gastroenterology and hepatology across the UK.22 However, there was representation from all regions, across training grades and the proportions of survey participants were comparable to national HST figures in terms of gender (57% male in survey participants vs 60% male national HST), age distribution (87% of survey participants vs 78% national HST between 30 and 39 years old) and training hours (79% training full time in survey participants vs 91% training full time in national HST). Second, trainee self-reported confidence levels may not be representative of their true clinical competence in those domains, thereby resulting in reporting bias. Third, trainees who participated in this survey may be a self-selected cohort already interested and engaged with hepatology as a career focus, therefore, may not be entirely representative of all trainees across the UK. However, similar proportions of trainees wanting to do hepatology have been reported in previous trainee surveys.7 8 While this is encouraging for future hepatology workforce expansion, these figures also highlight the importance of collaborative workforce planning between hepatology and gastroenterology to maintain future non-hepatology workforce recruitment.
In the first national trainee survey focusing specifically on hepatology in the UK since 2010, trainee views on hepatology training, research, hepatology ATP and future hepatology consultant career planning were explored. Several disease areas were identified that require further attention. Expansion of the hepatology training networks with wider geographical coverage is needed to address the growing demand for more specialists across the UK to reduce this glaring healthcare inequity. Further work is also required to explore ways to address the significant imbalance in trainees preferentially favouring hepatology consultant posts in specialist liver centres rather than district general hospitals, where there is a great clinical need.
Footnotes
Twitter: @drwenhaoli, @nadirabbas_x, @brennap9, @dr_robertscott, @Otavabie
Contributors: Survey design led by WL, ODT. All authors involved in survey design review. WL led on data analysis and drafting of manuscript. All other authors involved in manuscript review and editing. PNB and ODT led on final manuscript review. WL is the guarantor for the data in this study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: PNB has received an educational honorarium from Takeda. ODT has received an educational honorarium from Gilead Sciences. ODT is trainee editor for Frontline Gastroenterology.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Williams R, Aspinall R, Bellis M, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet 2014;384:1953–97. 10.1016/S0140-6736(14)61838-9 [DOI] [PubMed] [Google Scholar]
- 2. Karlsen TH, Sheron N, Zelber-Sagi S, et al. The EASL-lancet liver commission: protecting the next generation of Europeans against liver disease complications and premature mortality. Lancet 2022;399:61–116. 10.1016/S0140-6736(21)01701-3 [DOI] [PubMed] [Google Scholar]
- 3. Williams R, Ashton K, Aspinall R, et al. Implementation of the lancet standing commission on liver disease in the UK. Lancet 2015;386:2098–111. 10.1016/S0140-6736(15)00680-7 [DOI] [PubMed] [Google Scholar]
- 4. Rutter C. British Society of gastroenterology workforce report; 2021.
- 5. Segal J, Siau K, Kanagasundaram C, et al. Training in endotherapy for acute upper gastrointestinal bleeding: a UK-wide gastroenterology trainee survey. Frontline Gastroenterol 2020;11:430–5. 10.1136/flgastro-2019-101345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Clough J, FitzPatrick M, Harvey P, et al. Shape of training review: an impact assessment for UK gastroenterology trainees. Frontline Gastroenterol 2019;10:356–63. 10.1136/flgastro-2018-101168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Raju SA, Harris R, Cook C, et al. UK-wide study of the opinions of gastroenterology trainees: COVID-19, shape of training and the future workforce. Frontline Gastroenterol 2022;13:386–91. 10.1136/flgastro-2021-101965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patanwala I, Hudson M. Hepatology training in the UK. Frontline Gastroenterol 2012;3:52–6. 10.1136/flgastro-2011-100028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tai D, Dhar A, Yusuf A, et al. The royal free hospital 'hub-and-spoke network model' delivers effective care and increased access to liver transplantation. Public Health 2018;154:164–71. 10.1016/j.puhe.2017.10.012 [DOI] [PubMed] [Google Scholar]
- 10. The NHS long term plan – a summary, 2019.
- 11.BSG – BASL decompensated cirrhosis care bundle – first 24 hours.
- 12. Bruix J, Chan SL, Galle PR, et al. Systemic treatment of hepatocellular carcinoma: an EASL position paper. J Hepatol 2021;75:960–74. 10.1016/j.jhep.2021.07.004 [DOI] [PubMed] [Google Scholar]
- 13. RCP London . Medical CCT classes of 2019 and 2020
- 14. Pradeep A, Barker F, Ramos K, et al. Virtual liver transplant assessment: a novel pathway that is likely safe, effective and optimises access to transplantation. Frontline Gastroenterol 2022;13:360–2. 10.1136/flgastro-2021-101976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. FitzPatrick M, Clough J, Harvey P, et al. How can gastroenterology training thrive in a post-COVID world? Frontline Gastroenterol 2021;12:338–41. 10.1136/flgastro-2020-101601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. NIHR . Associate principal investigator (PI) scheme
- 17. Gastroenterology & Hepatology Clinical Research Training Programme (CRTP). Available: https://www.bsg.org.uk/news/gastroenterology-hepatology-clinical-research-training-programme-crtp/
- 18. Ozdemir BA, Karthikesalingam A, Sinha S, et al. Research activity and the association with mortality. PLoS One 2015;10:e0118253. 10.1371/journal.pone.0118253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jonker L, Fisher SJ. The correlation between national health service trusts' clinical trial activity and both mortality rates and care quality commission ratings: a retrospective cross-sectional study. Public Health 2018;157:1–6. 10.1016/j.puhe.2017.12.022 [DOI] [PubMed] [Google Scholar]
- 20. Trainee Collaborative for Research and Audit in Hepatology UK . ToRcH-UK: shining a light on liver disease in the UK. Frontline Gastroenterol 2022;13:2–268. 10.1136/flgastro-2021-101948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kavanagh E, Fernandes L, Li W, et al. Physician trainee research collaboratives: a mixed methods exploration of UK experience. Clin Med 2022;22:119–24. 10.7861/clinmed.2021-0511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Focus on physicians: 2018–19 census (UK consultants and higher specialty trainees)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.